Documente Academic
Documente Profesional
Documente Cultură
Study of HLA Class I and Class II by (PCR-SSP) and the role of salivary TNF-α in Iraqi patients with Recurrent Aphthous Stomatitis
Încărcat de
Stephanie LyonsDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Study of HLA Class I and Class II by (PCR-SSP) and the role of salivary TNF-α in Iraqi patients with Recurrent Aphthous Stomatitis
Încărcat de
Stephanie LyonsDrepturi de autor:
Formate disponibile
J Bagh College Dentistry
Vol. 24(1), 2012
Study of HLA Class I
Study of HLA Class I and Class II by (PCR-SSP) and the
role of salivary TNF- in Iraqi patients with Recurrent
Aphthous Stomatitis
Mustafa M. Salah MSc. (1)
Batool H. Al-Ghurabei MSc. Ph.D
(2)
ABSTRACT
Background: Until today, the etiology of recurrent aphthous stomatitis remains unknown, although hints of its etiologic
basis lay on genetic susceptibility, infectious agents and alterations in immune mechanics. Current study was
established to shed light on the possible association of human leukocyte antigen class I and II alleles with recurrent
aphthous stomatitis, and to investigate the possible alterations in salivary tumor necrosis factor-alpha level in patients
and its relation with clinical types of disease.
Subjects and Methods: The study included 55 subjects: 30 recurrent aphthous stomatitis patients and 25 apparently
healthy subjects as control. Polymerase chain reaction-specific sequence primers assay was conducted to assess
human leukocyte antigen-typing whereas salivary tumor necrosis factor-alpha level was estimated by enzyme-linked
immunosorbent assay.
Results: The present study showed a significant association of HLA-Cw*12:02:01-and DQB1*02:01:01- alleles with
recurrent aphthous stomatitis as compared with healthy control, and there was significant low frequency of
DQB1*05:01:01- allele in patients when compared with healthy control. Furthermore, high frequency of
DQB1*02:01:01- alleles was observed among patients with minor type of recurrent aphthous stomatitis when
compared with healthy control. Another interesting finding in this study was the significant elevation of salivary tumor
necrosis factor-alpha level in patients than in healthy controls, as well as strong association of high salivary tumor
necrosis factor-alpha level among patients who expressed DQB1*02:01:0-allell was observed.
Conclusion: Cw*12:02:01- and DQB1*02:01:01-alleles may played a role in the etiology of the disease, whereas
DQB1*05:01:01-05 may confer protective effects against recurrent aphthous stomatitis. Moreover; salivary tumor
necrosis factor-alpha may play an important role in pathogenesis of disease, and may also have an important role in
the search of new treatments for disease.
Keywords: RAS, HLA allele, PCR, Salivary TNF-. (J Bagh Coll Dentistry 2012;24(1):151-157).
INTRODUCTION
However it was not confirmed by other
authors (5,6). In groups of patients of different
ethnical origin, a significant association between
HLA-DR2 and RAS was noticed (3, 7).
The ulcerative process in RAS is initiated by
an unknown antigenic stimulation of the mucosal
keratinocytes which leads to T-lymphocyte
stimulation, the liberation of cytokines such as
tumor necrosis factor-alpha (TNF-) and different
interleukins, and the migration of other
lymphocytes, neutrophils and Langerhans cells.
Some cytokines like TNF- could stimulate the
expression of MHC class I and II antigens in
epithelial basal cells. These cells are recognized
by T-lymphocytes triggering a cytotoxic response
and causing the ulceration of the mucosa (8).
Recently, TNF- is considered to be one of the
most important cytokines implied in the
development of new lesions in RAS patients (9).
Several studies have reported an increase in
salivary and serological TNF-, especially during
the active phase of the disease (8,10). RAS is
common oral cavity disease in Iraq, yet no
available data on the association of HLA-alleles
with RAS. This prompted us to carry out this
study in order to shed light on the association
between HLA-class I and -class II alleles with
The precise etiology of recurrent aphthous
stomatitis (RAS) remains unknown, although
genetic susceptibility, infections and alteration in
immune system has been considered as etiologic
factors. The disease usually has three clinical
forms, based on the aspect and size of the
ulcerations: minor, major and herpetiform. Family
history seems to be relevant in the genesis of
RAS, and reports of cases in the same family are
found in 24% to 46% of the times (1). Moreover,
patients with family history of RAS can develop
ulcers earlier on and have more severe
manifestations than those without family history
(2)
. Numerous associations and non-associations of
HLA and RAS antigen have been reported in the
medical literature. The association between the
disease and HLAB12 was described by Lehner
and colleagues (3) and Malmstrm et al., (4).
(1) MSc. student /College of Dentistry/ University of Baghdad
(2) Assistant Professor, Department of Basic Science, College of
Dentistry, University of Baghdad.
Basic Sciences
151
J Bagh College Dentistry
Vol. 24(1), 2012
variations between patients and controls were
further presented in terms of odds ratio (OR) and
etiological fraction (EF). The significance of these
differences was assessed by fishers exact
probability (P). Regarding levels of TNF- was
assessed using P (Mann-Whitney-test), P
(Bonferroni-test) and (Kruskal-Wallis-test). P
values of P<0.001and P<0.05 were considered
significant (14).
RAS, as well as to provide information about
genotypes that confer susceptibility or resistance
to develop the disease, and to investigate the
possible alterations in salivary TNF- level in
patients and its relation with clinical types of
disease in Iraqi patients.
SUBJECTS AND METHODS
Thirty Iraqi Arab patients with RAS (16
females and 14 males) were included in this study.
They were among patients attending to the
teaching hospital dentistry college in
Baghdad, during the period between September
2009 till March 2010. Their age ranged from 1840 years. Diagnosis was made by specialized
dentists in the hospital. All the cases had received
no treatment with no complain of chronic or
systemic diseases. Apparently healthy volunteers
their ethnic, ages, and gender were matched,
consisted of 25 individuals who were considered
as control. All of them have no history or clinic
evidence of RAS lesions. Their age ranged from
18-31years.
Two ml of venous blood with EDTA as
anticoagulant were collected from each subject.
Extraction of DNA from peripheral blood was
done according to the modified method of Miller
(11)
, using the EXTRA-GENE-I kit (BAGGermany).
HLA-genotyping
was
performed
by
polymerase chain reaction-specific sequence
primers (PCR-SSP) according to a method
presented by Olerup and Zetterquist (12, 13), using
low resolution typing kits (HISTO TYPE / DNASSP Kits-BAG- Germany). In the PCR-SSP
method, HLA-A, HLA-Cw, HLA-DR and HLADQ specific primer mixes were employed as well
as, a negative control and ladder mixes.
Appropriate amounts of DNA (50-100 ng/l) and
Taq polymerase (Recombinant Taq polymerase 5u
/ l from QIAGEN-company) were added to prealiquoted primers and PCR conditions were set
according to the manufacturer instructions. PCR
products were loaded in 2 % agarose gel
containing 0.5 g/ml ethidium bromide,
electrophoresed for 25 min at 12 V/cm, and
examined under ultraviolet light. The individual
alleles were assigned for the specific pattern of
appropriately sized bands.
Two ml of saliva were also collected from
each subject for estimating levels of TNF- by
using enzyme-linked immunosorbent assay
(ELISA) and performed as recommended in
leaflet with kit. [Human TNF- kit/ DRG
International, Inc., USA].
Statistical analysis were presented in terms of
percentage frequencies, and alleles showing
Basic Sciences
Study of HLA Class I
RESULTS
The current results showed that the age of
patients ranged between 16-40 years with a mean
age of 23.1 years. Successful amplification was
resulted in the generation of a DNA fragment of
defined length as a positive internal control band
in all lanes except the negative control lane, when
there was no amplification, the band was missed.
A positive specific amplification was resulted in
the generation of a positive specific amplification
band in addition to an internal positive control
band, as show in figures (1 &2). The frequency of
distribution of various HLA- alleles for thirty
patients with RAS were typed for HLAgenotyping class I and class II. These frequencies
for two studied groups were presented in tables (1,
2, 3 and 4). Comparison between patients and
control group showed several alleles deviations in
their frequencies. Regarding HLA-A alleles, the
statistical analysis revealed no significant
association was found in patients as compared
with control, table (1). Concerning C-locus
alleles, the Cw*12:02:01-alleles were revealed
higher frequencies (17.2%) in RAS patients than
healthy control with OR of (11.00), table (2). A
survey of the distribution of HLA-DRB1 alleles
frequencies yielded no evident association
between DR alleles and RAS patients, table (3).
Among DQB alleles that have significant risk
effect in a disease, there was DQB1*02:01:0
which noticed in high frequency among patients
(48.3% vs. 20.8%) with significant differences in
comparison with healthy control (P<0.05), table
(4). On the contrary, there was significant
decrease in the frequency of DQB1*05:01:0
among RAS cases with (P=0.036), this allele
acted as protective against the development of
RAS, therefore this allele present in high
frequency in healthy control group as clearly
shown in table (4).
When RAS patients were divided according to
the type of aphtha, the prevalence of
DQB1*02:01:0 allele frequency in the group with
minor RAS remained statistically significant
higher than those of control group (OR = 0.21 and
P = 0.016), p < 0.05, table (5). But the differences
in DQB1*02:01:0 allele frequency between major
152
J Bagh College Dentistry
Vol. 24(1), 2012
compared to controls.
Furthermore, the result obtained from the present
study revealed that HLA- DQB1*02:01:0 allele
frequency in the patients with MiRAS type
remained higher. Correspondingly, Wilhelmsen
and colleagues, found that patients with RAS
showed increase frequencies of HLA-A33 and
HLA-B35 alleles, and when analyzed in relation
to the subtypes of RAS the same HLA-A33 and
HLA-B35 frequency was statistically significant
only for patients with MiRAS (15). This might in
part, resulted from the limited number of
investigated patients in this study, as well as
reduction in the number of patients after the
subdivision could be attributed to the lack the
association of HLA-alleles with other types of
disease. In line with present findings, high levels
of TNF-, have also been reported by other
studies (8,9,10) have observed increased levels of
TNF- in saliva and serum of RAS patients. This
result underlines the importance of this cytokine
in the pathogenesis of RAS. In study conducted
by Valle and associates, how studied 20 patients
with RAS, they observed that saliva levels of
TNF- was significantly higher in patients with
active lesions of RAS compared with controls (9).
Guimaraes and colleagues have related the high
production of some cytokines, such as TNF-, IL1, IL-10 or IL-6 in RAS patients to some genetic
polymorphisms. This fact could explain the family
history frequently observed in some RAS patients
(18)
. In conclusion these findings demonstrated that
HLA-Cw*12:02:01- and HLA-DQB1*02:01:01alleles may played a role in the etiology of the
disease, whereas HLA-DQB1*05:01:01-05 may
confer protective effects against RAS. Moreover;
salivary TNF- may play an important role in
pathogenesis of this disease and it may also have
an important role in the search of new treatments
for this disease.
RAS patients and control group were statistically
not significant (p > 0.05).
The current study revealed a significant
elevation in median salivary level of TNF-
among RAS patients (0.15pg/ml) in comparison
to that of healthy control (0.131 pg/ml),
(p<0.001), according to table (6). Moreover, the
level of TNF- was significantly increased in
minor type of disease than in major and
herptiform types (p<0.05), as shown in table (7).
An anticipated, the current study revealed strong
association of high salivary TNF- level among
RAS patients who expressed DQB1*02:01:0-allell
(P<0.05), as clearly shown in table (8).
DISCUSSION
The role of genetic factors in the etiology of RAS
was documented many decades ago. As a result,
the investigative efforts were focused on the
genetic markers of susceptibility to this disease.
Moreover, the high familial incidence of RAS
suggests the possibility of a linkage or an
association of disease with HLA.
The present work revealed a significant
association of HLA- Cw*12:02:01-alleles with
RAS patients (p= 0.041), as compared with
healthy control. Different results regarding this
association was reported, results differ in different
population. In Brazilian study conducted by
Wilhelmsen and colleagues (15), observed that high
frequencies of HLA-A33, HLA-B35 and HLA-B8
were found in patients with RAS as compared to
healthy control. Correspondingly Malmstrm and
co-workers also noticed that HLA- HLA-B12
frequency was higher when they studied 14 Finish
patients with RAS (4). In 2001, twenty two Israeli
Arab patients with RAS were studied, a
statistically significant increase in HLA-B52 and
B44 molecules in patients with this disease was
observed when compared to the control group (16).
An anticipated, another finding in this study was
the higher expression of HLA- DQB1*02:01:0- in
RAS patients. This results is at variance with
some other studies (5,6,17) which lack such
association between HLA- DQ and this disease,
while reporting positive association with other
antigens of HLA- class II. For instance Gallina
and colleagues, (5) studied a sample of 26 Sicilian
patients with RAS, they found a statistically
significant increased value for HLA-DR7
frequency.
It is very important to point out that, as
mentioned by Louzada-Junior and associates (17)
the reduced frequency of HLA typing could be
considered as a protective factor for RAS. The
current study found decrease frequency of HLADQB1*05:01:0 allele in RAS patients when
Basic Sciences
Study of HLA Class I
REFERENCES
1. Gallo CB, Mimura MA, Sugaya NN. Recurrent Aphthous
Stomatitis. Clinics 2009; 64 (7):645-8.
2. Miller MF, Ship II, Ram C. A retrospective study of
factors associated with recurrent aphthous ulcers in a
professional population. Oral Surg 1977;43:532-7.
3. Lehner T, Welsh KL, Batchelor JR. The relationship of
HLA-B and DR phenotypes to Behets syndrome,
recurrent oral ulceration and the class of immune
complexes. Immunology 1982;47:581-7.
4. Malmstrm M, Salo OP, Fyhrquist F. Immunogenetic
markers and immune response in patients with recurrent
oral ulceration. Int J Oral Surg 1983;12:23-30.
5. Gallina G, Cumbo V, Messina P, Caruso C. HLA-A, B, C,
DR, MT, and MB antigens in recurrent aphthous
stomatitis. Oral Surg Oral Med Oral Pathol
1985;59(4):364-70.
6. Ozbakir F, Yazici H, Mat C, Tuzun Y, Yurdakul S,
153
J Bagh College Dentistry
Vol. 24(1), 2012
Yilmazer S. HLA antigens in recurrent oral ulceration:
evidence against a common disease spectrum with
Behcets syndrome. Clin Exp Rheumatol 1987;5:263-5.
7. Albanidou-Farmaki A, Kayavis IG, Polymenidis Z,
Papanayotou P. HLA-A, B, C and DR antigens in
recurrent oral ulcers. Ann Dent 1988;47(1):5-8.
8. Natah SS, Hyrinen-Immonen R, Hietanen J, Malmstrm
M, Konttinen YT. Immunolocalization of tumor necrosis
factor-alpha expressing cells in recurrent aphthous ulcer
lesions . J Oral Pathol Med 2000; 29:19-25.
9. Valle E, Llamosas RC, Vicente JL, Etxebarria AU, Urizar
JA. Salivary levels of Tumour Necrosis Factor-alpha in
patients with recurrent aphthous stomatitis. Med Oral
Patol Oral Cir Bucal 2011;16 (1): 33-6.
10.
Boras VV, Lukac J, Brailo V, Picek P, Kordi
D, Zili IA. Salivaryinterleukin-6 and tumor necrosis
factor-alpha in patients with recurrent aphthous
ulceration. J Oral Pathol Med 2006;35:241-3 .
11.
Miller SA, Dykes DD, Polesky IF. Asimple salting
out procedure for extracting DNA from human nucleated
cells. Nucl Acid Res 1988; 16:1215.
12.
Olerup O, Zetterquist H. HLA-DR typing by PCR
amplification with PCR-SSP in two hours. Tissue
Antigens 1992; 39:225-235.
Study of HLA Class I
13.
Olerup O, Zetterquist H.DR low-resolution PCR-SSP
typing-a correction and an update. Tissue Antigens 1993;
41:55-56.
14.
Sorlie DE. Medical biostatistics and epidemiology:
Examination and Board review First ed, Norwalk,
Connecticut, Appleton and Lange 1995; 47-88.
15.
Wilhelmsen NS, Weber R, Monteiro F, Kalil J,
Miziara ID.Correlation between histocompatibility
antigens andrecurrent aphthous stomatitis in the brazilian
population. Brazil J Otorhinolaryngology 2009; 75 (3).
16.
Jaber L, Weinberger A, Klein T, Yaniv I,
Mukamel M. Close association of HLA-B52 and HLAB44 antigens in Israeli Arab adolescents with recurrent
aphthous stomatitis. Arch Otolaryngol Head Neck Surg
2001;127:184-7.
17.
Louzada-Junior P, Smith AG, Hansen JA,
Donadi EA. HLA-DRB1 and -DQB1 alleles in the
Brazilian population of the northeastern region. Tissue
Antigen 2001;57:158-62.
18.
Guimares AL, Correia-Silva Jde F, S AR,
Victria JM, Diniz MG, Costa Fde O. Investigation of
functional gene polymorphisms IL-1beta, IL-6, IL-10 and
TNF-alpha in individuals with recurrent aphthous
stomatitis. Arch Oral Biol 2007; 52:268-72.
Table 1: HLA-A alleles genotyping in RAS cases in comparison to healthy control group.
A*01:13,17:
A*02:01:01:
A*03:01:01:
A*03:30
A*11:43
A*23:03:01
A*24:02:01:
A*24:77
A*24:94
A*25:01:01,01
A*25:05
A*26:09
A*29:01:01:01
A*31:03,04
A*31:07,10
A*32:17
A*33:01:01-01
A*33:19
A*34:07
A*36:01-05
A*66:01,04,06
A*66:03
A*68:29
Total
Basic Sciences
Controls
N
%
2
8.3
1
4.2
2
8.3
2
8.3
1
4.2
2
8.3
4 16.7
0
0
0
0
0
0
0
0
1
4.2
0
0
2
8.3
0
0
0
0
2
8.3
1
4.2
1
4.2
1
4.2
0
0
0
0
1
4.2
25 30
Cases (RAS)
N
%
2
6.9
1
3.4
0
0
1
3.4
1
3.4
3
10.3
3
10.3
1
3.4
2
6.9
1
3.4
1
3.4
0
0
1
3.4
0
0
1
3.4
1
3.4
1
3.4
0
0
0
0
0
0
1
3.4
2
6.9
0
0
29
100
154
OR
0.81
0.82
0.15
0.39
0.82
1.27
0.58
2.58
4.45
2.58
2.58
0.27
2.58
0.15
2.58
2.58
0.39
0.27
0.27
0.27
2.58
4.45
0.27
EF
**
**
**
**
**
0.022
**
0.021
0.054
0.021
0.021
**
0.021
**
0.021
0.021
**
**
**
**
0.021
0.054
**
P (Fisher's exact)
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
J Bagh College Dentistry
Vol. 24(1), 2012
Study of HLA Class I
Table 2: HLA-Cw alleles genotyping in RAS cases in comparison to healthy control group.
C*01:17
C*02:27
C*03:03:04,13,18
C*03:04:02,04:06
C*03:27,38:01
C*03:38:02
C*04:01:01:01
C*05:10 C*05:23
C*05:26
C*06:02:01:0
C*06:17/*12:09
C*07:02:01:01-02
C*07:05,08,14,
C*07:07
C*07:09
C*07:12,41
C*08:01:0102:2
C*08:05,21
C*08:28
C*12:02:01C*12:14:02
C*12:21,28
C*15:02:01-0
C*16:02:01,02:0
B*40:76
C 87
Total
Controls
N
%
1
4.2
2
8.3
1
4.2
1
4.2
1
4.2
2
8.3
0
0
3 12.5
2
8.3
1
4.2
1
4.2
0
0
0
0
1
4.2
0
0
1
4.2
1
4.2
0
0
0
0
0
0
1
4.2
1
4.2
1
4.2
1
4.2
0
0
2
8.3
25 100
Cases (RAS)
N
%
1
3.4
0
0
0
0
0
0
0
0
1
3.4
1
3.4
5
13.8
2
6.9
1
3.4
1
3.4
1
3.4
1
3.4
2
6.9
1
3.4
1
3.4
0
0
1
3.4
1
3.4
5
17.2
0
0
1
3.4
1
3.4
0
0
1
3.4
1
3.4
30
100
OR
0.82
0.15
0.27
0.27
0.27
0.39
2.58
1.12
0.81
0.82
0.82
2.58
2.58
1.70
2.58
0.82
0.27
2.58
2.58
11.00
0.27
0.82
0.82
0.27
2.58
0.39
EF
**
**
**
**
**
**
0.021
0.015
**
**
**
0.021
0.021
0.029
0.021
**
**
0.021
0.021
0.156
**
**
**
**
0.021
**
P (Fisher's exact)
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
0.041
P<0.05
NS
NS
NS
NS
NS
NS
Table 3: HLA-DR alleles genotyping in RAS cases in comparison to healthy control group.
DRB1*01:03
DRB1*01:23w,
DRB1*16:01:
DRB1*04:01:0
DRB1*04:02,1
DRB1*08:01:0
DRB1*09:01:0
DRB1*11:01:0
DRB1*11:45
DRB1*13:01:0
DRB1*13:01:0
DRB1*13:05:0
DRB1*13:37,7
DRB1*13:55
DRB1*13:60,8
DRB1*14:01:0
DRB1*14:19
DRB1*14:24.3
Total
Basic Sciences
Controls
N
%
4 16.7
0
0
1
4.2
0
0
2
8.3
2
8.3
3 12.5
1
4.2
3 12.5
0
0
0
0
1
4.2
1
4.2
2
8.3
1
4.2
1
4.2
1
4.2
1
4.2
25 100
Cases (R AS)
N
%
6
20.7
1
3.4
2
6.9
1
3.4
2
6.9
3
10.3
2
6.9
1
3.4
1
3.4
1
3.4
1
3.4
1
3.4
1
3.4
0
0
3
10.3
1
3.4
1
3.4
1
3.4
30
100
155
OR
1.30
2.58
1.70
2.58
0.81
1.27
0.52
0.82
0.25
2.58
2.58
0.82
0.82
0.15
2.65
0.82
0.82
0.82
EF
0.048
0.021
0.029
0.021
**
0.022
**
**
**
0.021
0.021
**
**
**
0.064
**
**
**
P (Fisher's exact)
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
NS
J Bagh College Dentistry
Vol. 24(1), 2012
Study of HLA Class I
Table 4: HLA-DQ alleles genotyping in RAS cases in comparison to healthy control group.
Controls
N
%
4 16.7
2
8.3
3 12.5
5 20.8
3 12.5
3 12.5
2
8.3
0
0
2
8.3
0
0
25 100
DQB1*05:01:0
DQB1*06:01:0
DQB1*06:02:0
DQB1*02:01:0
DQB1*03:01:0
DQB1*03:02:0
DQB1*03:03:0
DQB1*03:04,1
DQB1*03:10
DQB1*04:01:0
Total
Cases (RAS)
N
%
0
0
3
10.3
2
6.9
14
48.3
2
6.9
2
6.9
3
10.3
1
3.4
0
0
2
6.9
30
100
OR
0.08
1.27
0.52
3.55
0.52
0.52
1.27
2.58
0.15
4.45
EF
**
0.022
**
0.347
**
**
0.022
0.021
**
0.054
P (Fisher's exact)
0.036
P<0.05
NS
NS
0.028
P<0.05
NS
NS
NS
NS
NS
NS
Table 5: HLA-allele in minor and major RAS cases in comparison to healthy control group.
Controls Cases (RAS)
Inverse OR
N %
N
% OR
EF
Minor RAS
Cw*12:02:01- 0
5 20.8
DQB1*02:01:0
Major RAS
Cw*12:02:01- 1 4.3
DQB1*02:01:0 5 20.8
5.2
2.58
**
10
45.1 0.21
4.7
0
4
0
0.27
30.7 1.27
3.8
**
PF
P (Fisher's exact) Adjusted P
0.021 **
** 0.314
**
**
0.022 **
0.547
NS
0.016
P<0.05
0.453
0.351
NS
NS
Table 6: Case-control difference in median salivary TNF- (pg/ml) concentration.
Controls
Cases (RA S) P (Mann-Whitney)
salivary TNF-
(0.116 - 0.213) (0.12 - 0.201)
Range
0.131
0.15
P<0.001
Median
Inter-quartile range (0.125 - 0.142) (0.135 - 0.153)
25
30
No.
Table 7: The difference in levels of TNF- (pg/ml) according to the clinical types of disease.
Type of RAS Number
1- Minor
2- Major
3- Herptiform
16
13
1
Median of
P (Kruskall-Wallis)
salivary TNF-
0.150*
0.128
0.136
P<0.05
Table 8: The median salivary TNF- (pg/ml) concentration by HLA genotype.
Salivary TNF
Median Inter-quartile range N P (Mann-Whitney)
0.71[NS]
Cw*12:02:01
0.142
(0.136 - 0.153)
24
Negative
0.135
(0.132 - 0.176)
6
Positive
Basic Sciences
0.94[NS]
DQB1*05:01:0
0.142
Negative
0.138
Positive
(0.135 - 0.152)
(0.132 - **)
26
4
DQB1*02:01:0
0.138
Negative
0.146
Positive
(0.132 - 0.153)
(0.135 - 0.153)
11
19
0.034
156
J Bagh College Dentistry
Vol. 24(1), 2012
Study of HLA Class I
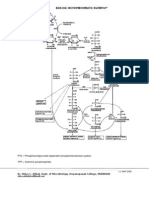
Figure1: Electrophoresis of HLA-DQ alleles amplified by PCR-SSP of RAS patient. Lane M
represent 1 kb DNA ladar, lanes (1-8) represent class-II HLA-DQB alleles. Lanes (3,4) represent
positive bands.
Figure 2: Electrophoresis of HLA-DR alleles amplified by PCR-SSP of RAS patient. Lane M
represent [DNA-lenth standard (x174-HaeIII)] DNA ladar, lanes (1-24) represent class-II HLADR alleles. Lanes (5,7,19,23) represent positive bands.
Basic Sciences
157
S-ar putea să vă placă și
- AACR 2022 Proceedings: Part A Online-Only and April 10De la EverandAACR 2022 Proceedings: Part A Online-Only and April 10Încă nu există evaluări
- NPC Examiners SyllabusDocument7 paginiNPC Examiners SyllabusAnirban DasÎncă nu există evaluări
- A Comparison of The Pattern of Liver Involvement in Dengue Hemorrhagic Fever With Classic Dengue FeverDocument5 paginiA Comparison of The Pattern of Liver Involvement in Dengue Hemorrhagic Fever With Classic Dengue FeverMichelle Rayvi J. SumampouwÎncă nu există evaluări
- Genotyping of HLA-class-I by PCR-SSP of Iraqi Breast Cancer PatientsDocument8 paginiGenotyping of HLA-class-I by PCR-SSP of Iraqi Breast Cancer PatientsAli MahdiÎncă nu există evaluări
- Plasma Histamine and Tumour Necrosis Factor-Alpha Levels in Crohn'S Disease and Ulcerative Colitis at Various Stages of DiseaseDocument8 paginiPlasma Histamine and Tumour Necrosis Factor-Alpha Levels in Crohn'S Disease and Ulcerative Colitis at Various Stages of DiseaseNejc KovačÎncă nu există evaluări
- BJBMS 10 282 PDFDocument5 paginiBJBMS 10 282 PDFRoman MamunÎncă nu există evaluări
- Prognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergDocument11 paginiPrognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergStephania SandovalÎncă nu există evaluări
- 8 - Ap 170219 0493Document8 pagini8 - Ap 170219 0493hoshikoongÎncă nu există evaluări
- 1443 3 FullDocument2 pagini1443 3 FullmuamarrayÎncă nu există evaluări
- Laboratory Features of Systemic Lupus Erythematosus (SLE)Document6 paginiLaboratory Features of Systemic Lupus Erythematosus (SLE)AmrKamalÎncă nu există evaluări
- TLR2 and TLR4 As A Biomarker of BacteriaDocument6 paginiTLR2 and TLR4 As A Biomarker of Bacteriafaraz.mirza1Încă nu există evaluări
- Drug-Induced Liver Injury: A Meta-Analysis: NAT2 Polymorphisms and Susceptibility To Anti-TuberculosisDocument9 paginiDrug-Induced Liver Injury: A Meta-Analysis: NAT2 Polymorphisms and Susceptibility To Anti-TuberculosisSherif EdrisÎncă nu există evaluări
- Hyperbilirubinemia: A Risk Factor For Infection in The Surgical Intensive Care UnitDocument14 paginiHyperbilirubinemia: A Risk Factor For Infection in The Surgical Intensive Care UnitChristian Karl B. LlanesÎncă nu există evaluări
- APJCP - Volume 23 - Issue 4 - Pages 1285-1290Document6 paginiAPJCP - Volume 23 - Issue 4 - Pages 1285-1290davidÎncă nu există evaluări
- Tse 2014Document5 paginiTse 2014Ke XuÎncă nu există evaluări
- Programmed Death Ligand-1 Expression Is Associated With Poorer Survival in Anal Squamous Cell CarcinomaDocument8 paginiProgrammed Death Ligand-1 Expression Is Associated With Poorer Survival in Anal Squamous Cell CarcinomaAnu ShaÎncă nu există evaluări
- Clinical and Genetic Risk Factors For Acute PancreatitisDocument8 paginiClinical and Genetic Risk Factors For Acute PancreatitisNermeen Mostafa ElhawaryÎncă nu există evaluări
- Plasma Vitamin D Levels and Vitamin D Receptor Polymorphisms Are Associated With Survival of Non-Small Cell Lung CancerDocument5 paginiPlasma Vitamin D Levels and Vitamin D Receptor Polymorphisms Are Associated With Survival of Non-Small Cell Lung CancerDaniel AriasÎncă nu există evaluări
- The Clinical and Immunologic Effects of AcetylcystDocument2 paginiThe Clinical and Immunologic Effects of Acetylcystفرجني موغÎncă nu există evaluări
- Genetic Polymorphisms of Long Non-Coding RNA GAS5 PredictDocument12 paginiGenetic Polymorphisms of Long Non-Coding RNA GAS5 PredictprototyposÎncă nu există evaluări
- Clinical Features and Major Histocompatibility Complex Genes As Potential Susceptibility Factors in Pediatric Immune ThrombocytopeniaDocument24 paginiClinical Features and Major Histocompatibility Complex Genes As Potential Susceptibility Factors in Pediatric Immune ThrombocytopeniaMerlin Margreth MaelissaÎncă nu există evaluări
- Acute Myeloid Leukemia With Mutated NPM1 Mimics Acute Promyelocytic Leukemia PresentationDocument9 paginiAcute Myeloid Leukemia With Mutated NPM1 Mimics Acute Promyelocytic Leukemia PresentationMunawwar SaukaniÎncă nu există evaluări
- 5TOAUTOJDocument5 pagini5TOAUTOJRika FitriaÎncă nu există evaluări
- Thalassemia IndiaDocument4 paginiThalassemia IndiaDr Laxmikant Basavraj DamaÎncă nu există evaluări
- Research Article: Correlations Between Iron Load and CD4 in Adult Transfusion-Dependent Beta ThalassemiaDocument5 paginiResearch Article: Correlations Between Iron Load and CD4 in Adult Transfusion-Dependent Beta ThalassemiaHyacinth A RotaÎncă nu există evaluări
- Lupus ActiveDocument5 paginiLupus ActivedeliaÎncă nu există evaluări
- 02 - Hav 2006Document6 pagini02 - Hav 2006sunilpkumar18Încă nu există evaluări
- Interferon Gamma Production in The Course of Mycobacterium Tuberculosis InfectionDocument9 paginiInterferon Gamma Production in The Course of Mycobacterium Tuberculosis InfectionAndia ReshiÎncă nu există evaluări
- 1 s2.0 S1098360021011758 MainDocument5 pagini1 s2.0 S1098360021011758 Main4-005-กิตติ์การต์ วีราพิสิษฐ์Încă nu există evaluări
- 1 s2.0 S0168827804905533 MainDocument1 pagină1 s2.0 S0168827804905533 Maindjafer maryaÎncă nu există evaluări
- Relationship of Hla-Dw3 HLA-B8 To Sjogren'S Syndrome: (P (P F PDocument6 paginiRelationship of Hla-Dw3 HLA-B8 To Sjogren'S Syndrome: (P (P F PMohmed AttiaÎncă nu există evaluări
- Anticorpos Resumo DM1Document4 paginiAnticorpos Resumo DM1rafaelplÎncă nu există evaluări
- Parik H 2016Document35 paginiParik H 2016Jose Angel AbadíaÎncă nu există evaluări
- Acinic Cell Carcinoma of The Salivary Glands: An Immunohistochemical Study of Angiogenesis in 12 CasesDocument10 paginiAcinic Cell Carcinoma of The Salivary Glands: An Immunohistochemical Study of Angiogenesis in 12 CaseselisasusantiÎncă nu există evaluări
- Konsensus AkiDocument10 paginiKonsensus AkiSatrya MillyanÎncă nu există evaluări
- Ankle1 N - Methyladenosine-Related Variant Is Associated With Colorectal Cancer Risk by Maintaining The Genomic StabilityDocument13 paginiAnkle1 N - Methyladenosine-Related Variant Is Associated With Colorectal Cancer Risk by Maintaining The Genomic Stabilitytirasi1214Încă nu există evaluări
- Ksienski 2021Document15 paginiKsienski 2021tim yuÎncă nu există evaluări
- Jayaram 2021Document5 paginiJayaram 2021Tuan NguyenÎncă nu există evaluări
- Sharma 2002Document4 paginiSharma 2002wosen wondÎncă nu există evaluări
- Response of Severe HIV-Associated Thrombocytopenia To Highly Active Antiretroviral Therapy Including Protease InhibitorsDocument6 paginiResponse of Severe HIV-Associated Thrombocytopenia To Highly Active Antiretroviral Therapy Including Protease InhibitorsMaharani Ni Luh PutuÎncă nu există evaluări
- Methylenetetrahydrofolate Reductase Gene Polymorphisms and Recurrent Pregnancy Loss in China - A Systematic Review and Meta-Analysis PDFDocument8 paginiMethylenetetrahydrofolate Reductase Gene Polymorphisms and Recurrent Pregnancy Loss in China - A Systematic Review and Meta-Analysis PDFmpm8471Încă nu există evaluări
- ABo Blood Group, Helicobacter Pylori Soropositivity, and A Risk of Pancreatic Cancer - A Case-Control StudyDocument4 paginiABo Blood Group, Helicobacter Pylori Soropositivity, and A Risk of Pancreatic Cancer - A Case-Control StudyDaniel OlyveiraÎncă nu există evaluări
- Aqac126 303Document2 paginiAqac126 303Starix UkrÎncă nu există evaluări
- The Mucosal Immune Response To Laryngopharyngeal Reflux: at A Glance CommentaryDocument11 paginiThe Mucosal Immune Response To Laryngopharyngeal Reflux: at A Glance CommentaryElisa Vina JayantiÎncă nu există evaluări
- 2.Applied-Elevated Serum Acid Phosphatase-Mamta YadavDocument4 pagini2.Applied-Elevated Serum Acid Phosphatase-Mamta YadavImpact JournalsÎncă nu există evaluări
- Ref TNF-a - Karplus, 2002Document7 paginiRef TNF-a - Karplus, 2002louisehip UFCÎncă nu există evaluări
- RematologyDocument5 paginiRematologyKilroy Vincent SterlingÎncă nu există evaluări
- Drug-Resistant Candida Glabrata Infection in Cancer PatientsDocument8 paginiDrug-Resistant Candida Glabrata Infection in Cancer PatientsGarryÎncă nu există evaluări
- Nejmoa 1917246Document12 paginiNejmoa 1917246AmitShettyÎncă nu există evaluări
- Genetic Association Between IL-21 Polymorphisms and Cryptorchidism in A Chinese Han PopulationDocument4 paginiGenetic Association Between IL-21 Polymorphisms and Cryptorchidism in A Chinese Han PopulationHugo AlvesÎncă nu există evaluări
- 2017 Article 2601 PDFDocument11 pagini2017 Article 2601 PDFzihanÎncă nu există evaluări
- Thrombosis Research: Full Length Article TDocument7 paginiThrombosis Research: Full Length Article TAnonymous 4XKNqMÎncă nu există evaluări
- Etm 11 6 2300 PDFDocument5 paginiEtm 11 6 2300 PDFLalan HolalaÎncă nu există evaluări
- Sars-Cov-2 Cellular Immune Response in Uninfected Health Care Workers With Prolonged and Close Exposure To Covid-19 PatientsDocument14 paginiSars-Cov-2 Cellular Immune Response in Uninfected Health Care Workers With Prolonged and Close Exposure To Covid-19 PatientsAlexis Guevara QuijadaÎncă nu există evaluări
- Prevalence of Mutations Conferring Resistance Among Multi-And Extensively Drug-Resistant Mycobacterium Tuberculosis Isolates in ChinaDocument4 paginiPrevalence of Mutations Conferring Resistance Among Multi-And Extensively Drug-Resistant Mycobacterium Tuberculosis Isolates in ChinaKartikeya SinghÎncă nu există evaluări
- Souza 2003Document5 paginiSouza 2003MariaLyNguyễnÎncă nu există evaluări
- Tropical Doctor YayınımızDocument6 paginiTropical Doctor Yayınımıztayibe balÎncă nu există evaluări
- AdherenceDocument8 paginiAdherenceAbdurhman SeidÎncă nu există evaluări
- Advpub 1201160351Document18 paginiAdvpub 1201160351hoshikoongÎncă nu există evaluări
- Genetics of Hypertension: The Lack of EvidenceDocument11 paginiGenetics of Hypertension: The Lack of EvidenceInternational Medical PublisherÎncă nu există evaluări
- SepsisDocument7 paginiSepsisrifkizidnyÎncă nu există evaluări
- Disinfection Procedures: Their Efficacy and Effect On Dimensional Accuracy and Surface Quality of An Irreversible Hydrocolloid Impression MaterialDocument8 paginiDisinfection Procedures: Their Efficacy and Effect On Dimensional Accuracy and Surface Quality of An Irreversible Hydrocolloid Impression MaterialStephanie LyonsÎncă nu există evaluări
- Article WMC003626Document29 paginiArticle WMC003626Stephanie LyonsÎncă nu există evaluări
- Morphology and Properties of Denture Acrylic Resins Cured by Microwave Energy and Conventional Water BathDocument9 paginiMorphology and Properties of Denture Acrylic Resins Cured by Microwave Energy and Conventional Water BathStephanie LyonsÎncă nu există evaluări
- A Cephlalometric Study of North American Black Patients With Anterior Open BiteDocument8 paginiA Cephlalometric Study of North American Black Patients With Anterior Open BiteStephanie LyonsÎncă nu există evaluări
- Bilateral Adenomatoid Odontogenic Tumour of The Maxilla in A 2-Year-Old Female-The Report of A Rare Case and Review of The LiteratureDocument7 paginiBilateral Adenomatoid Odontogenic Tumour of The Maxilla in A 2-Year-Old Female-The Report of A Rare Case and Review of The LiteratureStephanie LyonsÎncă nu există evaluări
- Introduction Blok 17Document15 paginiIntroduction Blok 17Stephanie LyonsÎncă nu există evaluări
- Animals of The Desert RegionDocument13 paginiAnimals of The Desert RegionpradeepsrecÎncă nu există evaluări
- Transgenic Fly Lab Worksheet StudentDocument10 paginiTransgenic Fly Lab Worksheet Studentluisfula0% (1)
- MCQ Cell Cycle N ChromosomeDocument3 paginiMCQ Cell Cycle N ChromosomeHenary Chongtham100% (2)
- Ethics of Sex ChangeDocument20 paginiEthics of Sex ChangeSoraj HongladaromÎncă nu există evaluări
- Colorful Handwritten About Me Blank Education PresentationDocument27 paginiColorful Handwritten About Me Blank Education PresentationDevone Claire Bolanos GonzalesÎncă nu există evaluări
- COVID-19 Vaccine Development - Milestones, Lessons and ProspectsDocument32 paginiCOVID-19 Vaccine Development - Milestones, Lessons and Prospectsnadhia rahdaÎncă nu există evaluări
- Chapter 50 Principles of PharmacologyDocument47 paginiChapter 50 Principles of PharmacologyTee WoodÎncă nu există evaluări
- Cell Division and Genetic Inheritance - FormattedDocument24 paginiCell Division and Genetic Inheritance - FormattedAISHA MUHAMMADÎncă nu există evaluări
- Biology Chapter 6Document5 paginiBiology Chapter 6emilyÎncă nu există evaluări
- Mark Scheme (Results) : Pearson Edexcel International GCSE in Human Biology (4HB0) Paper 1Document14 paginiMark Scheme (Results) : Pearson Edexcel International GCSE in Human Biology (4HB0) Paper 1Joseph LAU [11D]Încă nu există evaluări
- Age of Onset of Schizophrenia: Perspectives From Structural Neuroimaging StudiesDocument10 paginiAge of Onset of Schizophrenia: Perspectives From Structural Neuroimaging StudiesFrontiersÎncă nu există evaluări
- 978 3 642 65923 2 - 3Document2 pagini978 3 642 65923 2 - 3faraza adindaÎncă nu există evaluări
- Biomems PaperDocument16 paginiBiomems PaperpratiharmukeshÎncă nu există evaluări
- Mendelian GeneticsDocument52 paginiMendelian Geneticshengst librandoÎncă nu există evaluări
- Microbiology Parasitology OBE Syllabus Final 1Document16 paginiMicrobiology Parasitology OBE Syllabus Final 1Ryzette Angela MorañaÎncă nu există evaluări
- New Insight Into The Role of Exosomes in VitiligoDocument18 paginiNew Insight Into The Role of Exosomes in VitiligoAndrea AguirrePerezÎncă nu există evaluări
- Natural Science. Level 6. Unit 3. ReproductionDocument3 paginiNatural Science. Level 6. Unit 3. ReproductionAna Rosa Camacho Cornejo50% (2)
- Hexose Monophosphate Pathway PathwayDocument3 paginiHexose Monophosphate Pathway PathwayShiva100% (6)
- Food and You: Feeding The World With Modern Agricultural BiotechnologyDocument36 paginiFood and You: Feeding The World With Modern Agricultural BiotechnologyAmerican Council on Science and HealthÎncă nu există evaluări
- Goat Cryptosporidiosis and Its Importance at Goat Production Pathology - I. Pavlović, S. Ivanović, M. Žujović, Z. TomićDocument6 paginiGoat Cryptosporidiosis and Its Importance at Goat Production Pathology - I. Pavlović, S. Ivanović, M. Žujović, Z. TomićCk_psihÎncă nu există evaluări
- HiMedia Hugh Leifson Medium M826 Technical DatasheetDocument2 paginiHiMedia Hugh Leifson Medium M826 Technical DatasheetTimotius Candra KusumaÎncă nu există evaluări
- De Barros 2018Document36 paginiDe Barros 2018Eletícia SousaÎncă nu există evaluări
- Genetic RecombinationDocument25 paginiGenetic RecombinationChandrashekhar UnakalÎncă nu există evaluări
- DR - Tjok. Istri Anom Saturti, Sppd. MarsDocument16 paginiDR - Tjok. Istri Anom Saturti, Sppd. MarsYogiswara KarangÎncă nu există evaluări
- Project Manager Biotech Pharmaceutical Healthcare in Boston MA Resume Katinka SteniusDocument3 paginiProject Manager Biotech Pharmaceutical Healthcare in Boston MA Resume Katinka SteniusKatinkaSteniusÎncă nu există evaluări
- 1 s2.0 S0022282816302176 MainDocument85 pagini1 s2.0 S0022282816302176 MainNia Rukman100% (1)
- Biology STD 12: Biology MCQ: Section A //X Choose Correct Answer From The Given Options. (Each Carries 1 Mark)Document19 paginiBiology STD 12: Biology MCQ: Section A //X Choose Correct Answer From The Given Options. (Each Carries 1 Mark)Darshil MakwanaÎncă nu există evaluări
- Pablo Borbon Main II Batangas City: Republic of The Philippines Batangas State UniversityDocument5 paginiPablo Borbon Main II Batangas City: Republic of The Philippines Batangas State UniversityChichiri NomiÎncă nu există evaluări
- Pharmacogenetics Case StudyDocument9 paginiPharmacogenetics Case Studyapi-256755409Încă nu există evaluări