Documente Academic
Documente Profesional
Documente Cultură
Ojog20110300015 35650094
Încărcat de
Nurholis MajidTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Ojog20110300015 35650094
Încărcat de
Nurholis MajidDrepturi de autor:
Formate disponibile
Open Journal of Obstetrics and Gynecology, 2011, 1, 90-93
OJOG
doi:10.4236/ojog.2011.13016 Published Online September 2011 (http://www.SciRP.org/journal/ojog/).
Perinatal transmission of dengue virus in Puerto Rico: a case
report
Janice Prez-Padilla1*, Rafael Rosario-Casablanca2, Luis Prez-Cruz2, Carmen Rivera-Dipini2,
Kay Marie Tomashek1
1
Dengue Branch, Division of Vector-Borne Diseases, Centers For Disease Control and Prevention, San Juan, Puerto Rico;
HIMA San Pablo Hospital, Fajardo, Puerto Rico.
E-mail: *jpq9@cdc.gov
Received 17 June 2011; revised 14 July 2011; accepted 25 July 2011.
ABSTRACT
We report a laboratory confirmed case of vertical
transmission of dengue in a mother-child pair in the
eastern part of Puerto Rico. The clinical course of the
pregnant female suggested a GBS infection, but laboratory tests confirmed it was dengue infection, one
week after delivery. The male infant was healthy at
birth, but one week after birth developed clinical
complications related to vertical transmission of dengue. This report targets physicians in dengue endemic
countries like Puerto Rico to be aware of the possibility of vertical transmission of dengue in symptomatic
pregnant patients, especially around the time of delivery.
Keywords: Dengue; Perinatal Transmission; Bloodborne
1. INTRODUCTION
Dengue is caused by four related dengue viruses (DENV)
1, 2, 3, and 4, and infection with one DENV is
thought to provide lifelong immunity to that virus-type
and partial short term protection to other DENVs. Most
DENV infections are asymptomatic especially first infections. The clinical spectrum of disease ranges from a
mild, non-specific acute febrile illness, to classic dengue
fever (DF) to severe, life-threatening disease including
dengue hemorrhagic fever (DHF) and dengue shock
syndrome (DSS) [1]. Second and subsequent DENV
(secondary) infections have been associated with more
severe disease.[2]
DENV transmission is primarily between humans
through infected Aedes mosquitoes. The incubation period in the human host is typically one week (range 3 to
14 days) with viremia occurring 1 to 2 days before symptom onset and lasting approximately one week. During
this period of viremia, DENV can also be transmitted as
a bloodborne infection which has been observed from re-
ceipt of donor organs or tissue, blood transfusion [3-6],
after occupational accidents in healthcare settings, and
perinatal transmission [7,8].
Historically, dengue was thought to be primarily a
childhood disease; however, an increasing proportion of
cases are now being reported among adults [2,9,10]. In
Puerto Rico, half of all reported dengue cases are
adults >20 years of age while adolescents 15 to 19 years
old have the highest incidence of laboratory-confirmed
den- gue; a group whose infants make up nearly one-fifth
of the birth cohort [11]. Because of this, women of childbearing age are now increasingly at risk of acquiring
DENV infection while pregnant and may be more likely
to develop severe disease as second infections occur later
in life. Here we describe a unique case of perinatal
DENV transmission involving a teenage mother and her
infant.
2. CASE SUMMARY
2.1. Mother
A 17 year old woman, Grava: 1 Para: 1 Abortions: 0
Stillbirth: 0, who regularly attended prenatal care clinic
since 17 weeks gestation, presented to the Emergency
Department (ED) on 16 June 2010. She was 38 4/7
weeks gestation with a chief complaint of fever for one
day, headache, and nausea. The patient had recently
moved to Puerto Rico from Pennsylvania. She had one
previous hospitalization for appendectomy at age 7 and
no chronic medical conditions. The patient denied tobacco, alcohol or illicit drug use, and she was HIV, HBV
and RPR non-reactive and Group B Streptococcus (GBS)
positive at 34 weeks gestation. At initial presentation, she
had a temperature of 38.3C, a heart rate of 140 bpm,
respiratory rate of 18 bpm, and blood pressure of 109/46
mm Hg. She was alert, active and in moderate distress
with complaints of pelvic pain. On physical examination,
her cervix was two centimeters dilated and she was
thought to be in early labor. Laboratory studies included
Published Online September 2011 in SciRes. http://www.scirp.org/journal/OJOG
J. Prez-Padilla et al. / Open Journal of Obstetrics and Gynecology 1 (2011) 90-93
a complete blood count (CBC) with leukocyte count of
9500 mm3 and a normal differential, hematocrit of 31.7%,
and a platelet count of 105,000 mm3. She was mildly
hyponatremic with serum sodium of 134.0 meq/L. Blood
and urine cultures were taken and the patient was admitted for intravenous hydration and empiric treatment with
ampicillin and gentamicin for GBS. After intravenous
hydration, the decision was made to transfer the patient
to the delivery room were an amniotomy was
1
performed to promote active labor. After 5 hours of
2
active labor, the patient delivered a male infant at 16:13
on 17 June 2010 by spontaneous vaginal delivery. She
did not have any abnormal bleeding during labor or delivery, and did not require any blood products.
The patient continued to have fever and headache for 5
more days, and admission blood and urine cultures, and
placental cultures were all negative. Her platelet count
declined further to a low of 59,000 mm3 on the day of
fever defervescence. That day a serum sample was sent
to the Centers for Disease Control and Prevention (CDC)
Dengue Branch Laboratory in San Juan, Puerto Rico for
dengue diagnostic testing. The patient did not develop
any evidence of plasma leakage as indicated by hemoconcentration, ascites, pleural effusions, or hypoalbuminemia. She did not develop any hemorrhagic manifestations other than moderate post partum vaginal bleeding that lasted about two weeks. The patient did not have
any other signs or symptoms associated with dengue.
However, her aspartate aminotransferase (AST) and alanine aminotranferase (ALT) were slightly elevated at 95
and 46 IU/L, respectively on 22 June 2010, while her
total bilirubin (0.6 mg/dl) remained normal during the
hospital stay. The patient was discharged home on 23
June 2010 with a platelet count of 118,000 mm3, an AST
of 53 IU/L, ALT of 31 IU/L, and a hematocrit of 32.5%.
When evaluated 2 weeks later, she had fully recovered
without any complications.
2.2. Infant
The infant weighted 2,892 grams, and had a length of 20
inches and a head circumference of 13 inches. APGAR
scores were 8 and 9 at one and five minutes after birth,
respectively. The infant was transferred immediately to
the Neonatal Intensive Care Unit (NICU) to be evaluated
for GBS sepsis. Upon admission, the infant had a temperature of 36.5C, a heart rate of 141 bpm, a respiratory
rate of 35 bpm, and a blood pressure of 60/43 mm Hg.
Blood and urine cultures were taken and the infant was
given ampicillin and gentamycin empirically. Physical
examination was unremarkable. Laboratory studies showed
a leukocyte count of 11,000 mm3 and a normal differential, a platelet count of 260,000 mm3, and a hematocrit of
Copyright 2011 SciRes.
91
43.5%. Blood and urine cultures taken at birth were
negative.
The infant remained stable with no changes observed
in his physical examination, vital signs or behavior until
the evening of June 23, when he became hypoactive and
unable to suck and feed. On physical examination, the
infant had a temperature of 36.5C and a heart rate of
130 bpm, respiratory rate of 46 bpm and BP 64/39 mm
Hg. He was pale and had a fine reticular rash. The remainder of his examination was unremarkable. The patient had no lymphadenopathy, petechiae, ecchymosis,
purpura, or hepatomegaly. Laboratory studies showed a
leukocyte count of 4900 mm3 , a platelet count of 116,000
mm3 and a hematocrit of 36.6%; he was hyponatremic
with a sodium of 130 meq/L. Blood and urine cultures
were taken, and the possibility of a fungal infection was
entertained as there had been recent cases in the hospital.
Antibiotics were changed to vancomycin and imipenem,
and amphotericin was added.
The next day on 24 June, the infant remained hypoactive, pale, and unable to suck. He had a leukocyte
count of 4600 mm3, a platelet count of 84,000 mm3, and
a hematocrit of 35.6%. No bleeding was observed, and
there was no change in his physical examination or vital
signs. At this point, the mothers serum was reported as
positive for DENV-1 by reverse transcriptase-polymerase
chain reaction (RT-PCR). The possibility of vertical
transmission was entertained, and a serum sample was
sent to CDC for diagnostic testing. The infants platelet
count decreased to a low of 36,000 mm3 on June 26, and
he was given a platelet transfusion. No bleeding was
observed, a head ultrasound was normal, and stool and
urine analyses were negative for red blood cells. On June
27, laboratory studies showed a prothrombin time (PT)
of 11.4 seconds; partial thromboplastin time (PTT) of
63.3 seconds, and international normalized ratio (INR) of
1.05, and the infant was given fresh frozen plasma and
evaluated for disseminated intravascular coagulation
(DIC). His coagulation profile normalized on June 28.
An abdominal ultrasound found prehepatic and perisplenic free fluid, suggesting ascites.
Dengue diagnostic results were received on June 29,
which were positive for DENV-1 by RT-PCR. The next
day, the infant was more active and his sucking improved.
A CBC showed a leukocyte count of 7100 mm3, a platelet count of 98,000 mm3, and a hematocrit of 28.7%. He
was given a packed red blood cell transfusion for symptomatic anemia with hypoxia (O2 saturation 93%). On
July 7, his platelet count reached normal values for age
(168,000 mm3). The patient had no other complications
and he was discharged home on 18 July 2010.
3. DISCUSSION
This case illustrates the importance of considering denOJOG
92
J. Prez-Padilla et al. / Open Journal of Obstetrics and Gynecology 1 (2011) 90-93
gue as a cause of acute febrile illness in pregnant women
residing in, or traveling to endemic countries, and suggests that perinatal DENV transmission is likely to be
under-recognized. Unlike other cases reported in the literature [12-31] the infant we described never developed
fever. Newborn infants often do not mount a febrile response to an infection, and consequently cases of perinatal DENV transmission may be missed if the mother is
not identified as having dengue. This infant had nonspecific findings consistent with congenital dengue including hyponatremia, leucopenia, and thrombocytopenia, an elevated PTT, and ascites. However, he was diagnosed as having dengue because DENV-1 was detected by RT-PCR in his mothers serum. Perinatal transmission of DENV was supported by the fact that the mother was acutely febrile at the time of delivery, the infant
never left the hospital after an uneventful delivery and
was unlikely to have had mosquito-borne DENV transmission and all cultures were negative for GBS.
Perinatal dengue, as this case illustrates, may result in
severe dengue and prolonged hospital stays [22]. Of the
33 cases of perinatal DENV transmission reported with
clinical data, all developed fever and thrombocytopenia
in the first two weeks after birth, and 39% had a hemorrhagic manifestations, 24% developed hypotension, and
33% had hepatomegaly.
Our case and all of the perinatal transmission cases
described in the literature involved a woman who was
acutely ill with dengue at or near the time of delivery. It
has been hypothesized that when this happens, there is an
insufficient level of protective maternal anti-DENV IgG
to transfer to the fetus as the women is at or near the
peak of DENV viremia. In dengue endemic areas, women with intrapartum or post partum fever and a negative evaluation for bacterial or other causes should be
tested for dengue and informed of the risk of perinatal
dengue. Special attention should be paid to their infants
who if infected, might become ill in the first two weeks
of life. As with other diseases, this may mean that the
infant presents with a change in their level of activity,
responsiveness, muscle tone, or ability to suck and swallow, and they may not develop classic signs of dengue
such as fever and rash.
For nearly four decades, the Puerto Rico Department
of Health and CDC have monitored dengue incidence in
Puerto Rico via a passive surveillance system. Even
though dengue has been endemic since the late 1960s
and it is a reportable condition by law, cases are thought
to be under-recognized and under-reported. Pregnancyassociated dengue cases may not always be reported as
such. Pregnant women with dengue may be diagnosed
with other febrile illnesses or HELLP syndrome, especially if they present with elevated liver enzymes and a
Copyright 2011 SciRes.
low platelet count. Since there is no rapid diagnostic test
for dengue, physicians need to have a high index of suspicion and test for dengue while ruling out these other
etiologies.
Future studies should aim to determine the incidence
of perinatal DENV transmission, risk factors for dengue
in the neonate, and poor outcomes among infants born to
women with dengue during pregnancy. Increased awareness of the possibility of maternal dengue and perinatal
transmission is important to prevent complications in
both the mother and the newborn.
REFERENCES
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
[10]
[11]
[12]
[13]
Gregory, C.J., Santiago, L.M., Arguello, D.F., Hunsperger, E. and Tomashek, K.M. (2010) Clinical and laboratory features that differentiate dengue from other febrile
illnesses in an endemic areaPuerto rico, 2007 - 2008.
American Journal Tropical Medicine and Hygiene, 82,
922-929. doi:10.4269/ajtmh.2010.09-0552
Ooi, E.E., Hart, T.J., Tan, H.C. and Chan, S.H. (2001)
Dengue seroepidemiology in Singapore. Lancet, 357, 685686. doi:10.1016/S0140-6736(00)04137-4
Chuang, V.W., Wong, T.Y. and Leung, Y.H., et al. (2008)
Review of dengue fever cases in Hong Kong during 1998
to 2005. Hong Kong Medical Journal, 14, 170-177.
Mohammed, H., Linnen, J.M. and Munoz-Jordan, J.L., et
al. (2008) Dengue virus in blood donations, Puerto Rico,
2005. Transfusion, 48, 1348-1354.
doi:10.1111/j.1537-2995.2008.01771.x
Tambyah, P.A., Koay, E.S., Poon, M.L., Lin, R.V. and
Ong, B.K. (2008) Dengue hemorrhagic fever transmitted
by blood transfusion. New England Journal of Medicine,
359, 1526-1527. doi:10.1056/NEJMc0708673
Wilder-Smith, A., Chen, L.H., Massad, E. and Wilson,
M.E. (2009) Threat of dengue to blood safety in dengueendemic countries. Emerging Infectious Diseases, 15,
8-11. doi:10.3201/eid1501.071097
Pouliot, S.H., Xiong, X., Harville, E., et al. (2010)
Maternal dengue and pregnancy outcomes: A systematic
review. Obstetrics and Gynecology Survey, 65, 107-118.
Wiwanitkit, V. (2010) Unusual mode of transmission of
dengue. Journal of Infection in Developing Countries, 4,
51-54. doi:10.3855/jidc.145
Guha-Sapir, D. and Schimmer, B. (2005) Dengue fever:
New paradigms for a changing epidemiology. Emerging
Themes in Epidemiology, 2, 1.
doi:10.1186/1742-7622-2-1
Ooi, E.E., Goh, K.T. and Gobbler, D.J. (2006) Dengue
Prvention and 35 years of vector control in Singapore.
Emerging Infectious Diseases, 12, 887-893.
Martin, J.A., Hamilton, B.E., Sutton, P.D., Ventura, S.J.
and Mathews-Osterman, M.J.K. (2010) Births: Final data
for 2008. National Vital Statistics Report, National Center
for Health Statistics, 59.
Boussemart, T., Babe, P., Sibille, G., Neyret, C. and Berchel, C. (2001) Prenatal transmission of dengue: Two
new cases. Journal of Perinatology, 21, 255-257.
doi:10.1038/sj.jp.7200530
Bunyavejchevin, S., Tanawattanacharoen, S., Taecha-
OJOG
J. Prez-Padilla et al. / Open Journal of Obstetrics and Gynecology 1 (2011) 90-93
[14]
[15]
[16]
[17]
[18]
[19]
[20]
[21]
[22]
krai-chana, N., Thisyakorn, U., Tannirandorn, Y. And
Limpa-Phayom, K. (1997) Dengue hemorrhagic fever
during pregnancy: Antepartum, intrapartum and postpartum management. Journal of Obstetrics and Gynaecology
Research, 23, 445-448.
Carroll, I.D., Toovey, S. and Van, G.A. (2007) Dengue
fever and pregnancyA review and comment. Travel
Medicine and Infectious Diseases, 5, 183-188.
doi:10.1016/j.tmaid.2006.11.002
Chotigeat, U., Kalayanarooj, S. and Nisalak, A. (2003)
Vertical transmission of dengue infection in Thai infants:
Two case reports. Journal of the Medical Association
Thai, 86, 628-632.
Chye, J.K., Lim, C.T., Ng, K.B., Lim, J.M., George, R.
and Lam, S.K. (1997) Vertical transmission of dengue.
Clinical Infectious Diseases, 25, 1374-1377.
doi:10.1086/516126
Fatimil, L.E., Mollah, A.H., Ahmed, S. and Rahman, M.
(2003) Vertical transmission of dengue: First case report
from Bangladesh. Southeast Asian Journal Tropical Medicine and Public Health, 34, 800-803.
Fernandes, C., Silami, V.N., Brasil, P., Herdy, M.E.,
Coelho. J. and Ribeiro, R.M. (2009) Dengue during pregnancy: A study of thirteen cases. American Journal of
Infectious Disease, 5, 298-303.
Janjindamai, W. and Pruekprasert, P. (2003) Perinatal
dengue infection: A case report and review of literature.
Southeast Asian Journal of Tropical Medicine and Public
Health, 34, 793-796.
Kerdpanich, A., Watanaveeradej, V. and Samakoses, R.,
et al. (2001) Perinatal dengue infection. Southeast Asian
Journal of Tropical Medicine and Public Health, 32, 488493.
Poli, L., Chungue, E., Soulignac, O., Gestas, P., Kuo, P.
and Papouin-Rauzy, M. (1991) Materno-fetal dengue.
Apropos of 5 cases observed during the epidemic in
Tahiti (1989). Bulletin de la Societe de Pathologie Exotique,
84, 513-521.
Sirinavin, S., Nuntnarumit, P., Supapannachart, S., Boon-
Copyright 2011 SciRes.
[23]
[24]
[25]
[26]
[27]
[28]
[29]
[30]
[31]
93
kasidecha, S., Techasaensiri, C. and Yoksarn, S. (2004)
Vertical dengue infection: Case reports and review. Pediatric Infectious Disease Journal, 23, 1042-1047.
doi:10.1097/01.inf.0000143
Tan, P.C., Rajasingam, G., Devi, S. and Omar, S.Z
(2008) Dengue infection in pregnancy: Prevalence, vertical transmission, and pregnancy outcome. Obstetrics &
Gynecology, 111, 1111-1117.
doi:10.1097/AOG.0b013e31
Basurko, C., Carles, G., Youssef, M. and Guindi, W.E.
(2009) Maternal and fetal consequences of dengue fever
during pregnancy. European Journal of Obstetrics &
Gynecology and Reproductive Biology, 147, 29-32.
doi:10.1016/j.ejogrb.2009.06.028
Berberian, G., Fari, D., Rosanova, M.T., et al. (2011)
Dengue perinatal. Arch Argent Pediatr, 109, 232-236.
Castellanos-Morfn, J., Hernndez-Prez, P., ArellanoCorts, B., Newton-Snchez, O.A. and Espinoza-Gmez,
F. (2006) Reporte de un caso de dengue neonatal. Boletin
Medico del Hospital Infantil Mexico, 63, 202-206.
Silva-Delgado, H., Ruiz-Rios, J.C., Vela-Barbaran, E.L.,
et al. (2011) Dengue neonatal en el Per: Reporte de un
caso. Revista Peruana de Medicina Experimental y Salud
Publica, 28, 140-144.
Fonseca-Becerra, C.E. and Bayona-Ospina, M.A. (2010)
Dengue en embarazadas y en recin nacidos: Presentacin de dos casos en Neiva (Huila, Colombia) y revisin
de la literatura. Revista Colombiana de Obstetricia y
Ginecologia, 61, 72-77.
Restrepo, B.N., Isaza, D.M. and Salazar, C.L., et al.
(2004) Dengue y embarazo en antioquia, colombia. Revista
de la Facultad Nacional de Salud Publica, 22, 7-14.
Carrasco, J.R. and Avila, G.A. (2009) Transmisin vertical
de dengue en honduras: Primer reporte de caso en centro
Amrica. Revista Medica Honduras, 77, 20-22.
Gonzlez, G., Guerra, A., Malav, L. and Prez, P. (2001)
Dengue neonatal: A propsito de un caso. Archivos
Venezolanos de Puericultura y Pediatria, 64, 219.
OJOG
S-ar putea să vă placă și
- Renal Stones A Clinical Review PDFDocument6 paginiRenal Stones A Clinical Review PDFNurholis MajidÎncă nu există evaluări
- Renal Stones A Clinical Review PDFDocument6 paginiRenal Stones A Clinical Review PDFNurholis MajidÎncă nu există evaluări
- Keratosis TopografiDocument6 paginiKeratosis TopografiNurholis MajidÎncă nu există evaluări
- How Recover+wbiDocument1 paginăHow Recover+wbiLandry LisdiantoÎncă nu există evaluări
- Vancouver Citation StyleDocument7 paginiVancouver Citation StyleGerardo Alberto Padilla MartínezÎncă nu există evaluări
- Renal Stones A Clinical Review PDFDocument6 paginiRenal Stones A Clinical Review PDFNurholis MajidÎncă nu există evaluări
- External Ear Canal Cholesteatoma and Keratosis Obturans 20070328Document8 paginiExternal Ear Canal Cholesteatoma and Keratosis Obturans 20070328Nurholis MajidÎncă nu există evaluări
- Bilirubin Tinggi CountDocument13 paginiBilirubin Tinggi CountNurholis MajidÎncă nu există evaluări
- Liken AmiloidDocument2 paginiLiken AmiloidNurholis MajidÎncă nu există evaluări
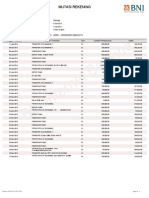
- Mutasi Rekening: Kriteria PencarianDocument2 paginiMutasi Rekening: Kriteria PencarianNurholis MajidÎncă nu există evaluări
- Dorl andDocument1 paginăDorl andNurholis MajidÎncă nu există evaluări
- Pengaruh Konseling Terhadap Pengetahuan, Sikap, Dan Tindakan Ibu Hamil Tentang Upaya Pencegahan Anemia Masa Kehamilan Di BPS Wilayah Mojo SurabayaDocument1 paginăPengaruh Konseling Terhadap Pengetahuan, Sikap, Dan Tindakan Ibu Hamil Tentang Upaya Pencegahan Anemia Masa Kehamilan Di BPS Wilayah Mojo SurabayaNurholis MajidÎncă nu există evaluări
- Dengue in PregnancyDocument4 paginiDengue in PregnancyEirna Syam Fitri IIÎncă nu există evaluări
- KLP No Nma Umur JK Bb1 Bb2-5 TB Lp1 Lp2-5Document1 paginăKLP No Nma Umur JK Bb1 Bb2-5 TB Lp1 Lp2-5Nurholis MajidÎncă nu există evaluări
- REFERENSIDocument1 paginăREFERENSINurholis MajidÎncă nu există evaluări
- REFERENSIDocument1 paginăREFERENSINurholis MajidÎncă nu există evaluări
- Bagian Akhir Food RecallDocument4 paginiBagian Akhir Food RecallNurholis MajidÎncă nu există evaluări
- BV ReferenceDocument1 paginăBV ReferenceNurholis MajidÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Barry Jones Post-Conviction Review PetitionDocument30 paginiBarry Jones Post-Conviction Review Petitionelliott602azÎncă nu există evaluări
- 2007 Nov 07 CompleteDocument62 pagini2007 Nov 07 CompleteKay BristolÎncă nu există evaluări
- Disseminated Intravascular CoagulationDocument1 paginăDisseminated Intravascular CoagulationAnn Justine OrbetaÎncă nu există evaluări
- TXADocument8 paginiTXACashim cashimÎncă nu există evaluări
- TP4Document14 paginiTP4Asdfghjl0% (1)
- Dengue 2Document56 paginiDengue 2Eliz Codilla-SyÎncă nu există evaluări
- FCPS Surgery 25 Aug 2023 (M)Document20 paginiFCPS Surgery 25 Aug 2023 (M)Tauseef AfridiÎncă nu există evaluări
- Issva Classification 2014 Final TrialDocument20 paginiIssva Classification 2014 Final TrialFrancis MunguíaÎncă nu există evaluări
- Actual Nursing Care Plan GT DisorderDocument3 paginiActual Nursing Care Plan GT DisordermandzkievonnieÎncă nu există evaluări
- Path NotesDocument111 paginiPath NotesNirav Patel100% (1)
- RECALLS 3 - Nursing Practice 1: SituationDocument45 paginiRECALLS 3 - Nursing Practice 1: Situationray raisÎncă nu există evaluări
- Comprehensive Hesi Review 1Document68 paginiComprehensive Hesi Review 1Tamara Smith-Williams100% (26)
- Disseminated Intravascular Coagulation in PregnancyDocument8 paginiDisseminated Intravascular Coagulation in Pregnancydr_asaleh100% (1)
- PancitopeniasDocument34 paginiPancitopeniasJuan Pablo Fuentes ArriagadaÎncă nu există evaluări
- Hematologic: DisordersDocument32 paginiHematologic: DisordersSomeshÎncă nu există evaluări
- Platelet IndicesDocument17 paginiPlatelet IndicesNarendra Bhattarai0% (1)
- AdfgDocument9 paginiAdfgicha shafiraÎncă nu există evaluări
- Lecture 16 - Bleeding Tendency DiseasesDocument64 paginiLecture 16 - Bleeding Tendency Diseasesapi-3703352100% (1)
- Ciesla 15264Document368 paginiCiesla 15264Razvan Mihalcea100% (14)
- Blood Disorders Seminar No 7Document142 paginiBlood Disorders Seminar No 7Hysum Mushtaq100% (1)
- Chapter 23 ContinuationDocument7 paginiChapter 23 ContinuationArabelle GO100% (1)
- MY Hematology MasterclassDocument32 paginiMY Hematology Masterclassabdul qayyumÎncă nu există evaluări
- Perinatal Asphyxia in Term and Late Preterm Infants - UpToDateDocument31 paginiPerinatal Asphyxia in Term and Late Preterm Infants - UpToDateRocio GÎncă nu există evaluări
- Acl CurveDocument24 paginiAcl Curvepieterinpretoria391100% (2)
- Fluid and Hemodynamic DisordersDocument19 paginiFluid and Hemodynamic DisordersapplesncoreÎncă nu există evaluări
- Guidelines For The Rational Use of Blood Blood ProductsDocument120 paginiGuidelines For The Rational Use of Blood Blood ProductsHafiz Hamidi100% (1)
- Disseminated Intravascular Coagulation (DIC)Document2 paginiDisseminated Intravascular Coagulation (DIC)JoyyÎncă nu există evaluări
- KGMU Pathology (2000-2020)Document10 paginiKGMU Pathology (2000-2020)Prepladder ChyÎncă nu există evaluări
- MCQ Haemato (DivC)Document6 paginiMCQ Haemato (DivC)Muhammad Nazif0% (2)
- How To Manage Coagulopathies in Critically Ill Patients: ReviewDocument18 paginiHow To Manage Coagulopathies in Critically Ill Patients: ReviewDaniel Balderas Anzures100% (2)