Documente Academic
Documente Profesional
Documente Cultură
Science
Încărcat de
Pety Tunjung Sari0 evaluări0% au considerat acest document util (0 voturi)
129 vizualizări1 paginăENJOY IT ;)
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentENJOY IT ;)
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
129 vizualizări1 paginăScience
Încărcat de
Pety Tunjung SariENJOY IT ;)
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 1
144
SCIENCE & PRACTICE
Pre-eclampsia:
than
pregnancy-induced
hypertension
more
and eclampsia are the most important
of maternal death in the USA, Scandinavia, Iceland,
Finland, and the UK.1-3 They occupy the same prime
position as they did nearly 40 years ago.4
Pre-eclampsia is not only common and dangerous for
both mother and baby, but also unpredictable in onset and
progression, and incurable except by termination of the
pregnancy. Because the pathogenesis is unclear there is no
specific diagnostic test; the disorder is recognised by the
concurrence of pregnancy-induced changes that regress
after delivery, of which hypertension and proteinuria are the
easiest to recognise and the signs by which the maternal
syndrome is defined.
Several classification schemes have been proposed to aid
clinical recognition of pre-eclampsia. The scheme
advocated by the US National Institutes of Health working
group on hypertension in pregnancy is outlined in table 1.5 It
emphasises, as do other similar classifications, the
distinction between a woman whose hypertension antedates
pregnancy and one with increased blood pressure as a sign of
pre-eclampsia. This classification helps greatly in
recognition of the patient with the disorder but has had the
of overemphasising
the
undesirable
consequence
importance of hypertension in the pathophysiology. As a
result, patients with other signs of pre-eclampsia but
without an increase in blood pressure may be mismanaged.
The recognition of the HELLP (haemolysis, elevated liver
enzyme activity, low platelets) variant of the disorder
emphasises how important it is to look at the whole
pathophysiological picture in diagnosing and managing
pre-eclampsia. Conversely, the emphasis on raised blood
pressure leads to the conclusion that all women whose blood
pressure increases during pregnancy have a single disorder.
Although appropriate for clinical management, this concept
has hindered understanding of the pathophysiology and
natural history of the disease. Epidemiological studies have
shown at least two forms of pregnancy-related
hypertension—pre-eclampsia, which increases fetal and
maternal mortality and morbidity but in which the
Pre-eclampsia
causes
cardiovascular abnormalities completely disappear aft
pregnancy, and transient hypertension, which predicts fix
hypertension in later life but has no acute consequenc
Unfortunately, research to find out the pathophysiologic
mechanisms of pre-eclampsia has been guided by strategi
useful in the understanding of hypertension. Thus, studi
have concentrated on measuring pressor agents a
mineralocorticoids and investigating renal pathophysiolog
Here we review the pathological and physiological chang
of pre-eclampsia that show that this syndrome is more th
pregnancy-induced hypertension.
Pathological changes
The
pathological changes present in women dying wi
eclampsia are listed in table 11. The widespread presence
haemorrhage and necrosis suggests reduced perfusi
rather than the gross vascular disruption that would
expected with mechanical damage from high blo
pressure. In the brain, the most frequent lesion is petechi
haemorrhage (perhaps agonal), and the subendocardi
necrosis found in this disorder is identical
hypovolaemic shock.6
to
that
seen
The
changes observed in renal and decidual vessels
with pre-eclampsia and eclampsia provide spec
insights. Electron-microscopic examination of renal biop
samples from pre-eclamptic women reveals changes seen
no other form of hypertension .7 The primary pathologi
change is in the glomerular capillary endothelial cells. T
cells are greatly increased in size, with electron-de
cytoplasmic inclusions that may occlude the capill
lumen. These changes support the idea that pre-eclampsi
a unique disease of pregnancy and direct attention
vascular endothelial damage in this disorder.
In normal pregnancy, as a result of trophoblastic invasi
there are striking changes in the arteries supplying
women
ADDRESSES:
Department of Obstetrics, Gynecology,
Reproductive Sciences, Magee Womens Hospital, Universit
Pittsburgh, Forbes Avenue, Pittsburgh, Pennsylvania 152
USA (Prof J. M. Roberts, MD); and Nuffield Department
Obstetrics and Gynaecology, John Radcliffe Hospital, Oxfo
UK (Prof C. W. G. Redman, FRCP). Correspondence to Prof James
Roberts.
S-ar putea să vă placă și
- Maternal Mortality Remains Major Challenge To Health Systems WorldwideDocument2 paginiMaternal Mortality Remains Major Challenge To Health Systems WorldwidePety Tunjung SariÎncă nu există evaluări
- Appendicitis Medication - Penicillins, Cephalosporins, Aminoglycosides, Carbapenems, Fluoroquinolones, Anti-Infective Agents, AnalgesicsDocument5 paginiAppendicitis Medication - Penicillins, Cephalosporins, Aminoglycosides, Carbapenems, Fluoroquinolones, Anti-Infective Agents, AnalgesicsPety Tunjung SariÎncă nu există evaluări
- Appendicitis Clinical Presentation - History, Physical Examination, Appendicitis and PregnancyDocument6 paginiAppendicitis Clinical Presentation - History, Physical Examination, Appendicitis and PregnancyPety Tunjung SariÎncă nu există evaluări
- Appendicitis Differential DiagnosesDocument5 paginiAppendicitis Differential DiagnosesPety Tunjung SariÎncă nu există evaluări
- Maternal Mortality Remains Major Challenge To Health Systems WorldwideDocument2 paginiMaternal Mortality Remains Major Challenge To Health Systems WorldwidePety Tunjung SariÎncă nu există evaluări
- CandidiasisDocument6 paginiCandidiasisyorlandaÎncă nu există evaluări
- Effect of Removable Partial Denture On Periodontal HealthDocument3 paginiEffect of Removable Partial Denture On Periodontal HealthAlex KwokÎncă nu există evaluări
- Anxiety Disorders (Risk Factors)Document3 paginiAnxiety Disorders (Risk Factors)Pety Tunjung SariÎncă nu există evaluări
- Anxiety Disorders (Risk Factors)Document3 paginiAnxiety Disorders (Risk Factors)Pety Tunjung SariÎncă nu există evaluări
- Bacterial and Viral Etiology of Childhood Diarrhea in OuagadougouDocument15 paginiBacterial and Viral Etiology of Childhood Diarrhea in OuagadougouPety Tunjung SariÎncă nu există evaluări
- Treatment of InfertilityDocument12 paginiTreatment of InfertilityPety Tunjung SariÎncă nu există evaluări
- Anatomi Fisiologi Kardiovaskular 2013Document64 paginiAnatomi Fisiologi Kardiovaskular 2013Sally WirawanÎncă nu există evaluări
- What Is Cerebral PalsyDocument2 paginiWhat Is Cerebral PalsyPety Tunjung SariÎncă nu există evaluări
- Chord Dan Kunci GitarDocument19 paginiChord Dan Kunci GitarPety Tunjung SariÎncă nu există evaluări
- Oral Rehydration Salts (ORS)Document3 paginiOral Rehydration Salts (ORS)Pety Tunjung SariÎncă nu există evaluări
- P 285Document7 paginiP 285Pety Tunjung SariÎncă nu există evaluări
- Chord Dan Kunci GitarDocument19 paginiChord Dan Kunci GitarPety Tunjung SariÎncă nu există evaluări
- WHO CDD SER 85.8 pp1-60Document62 paginiWHO CDD SER 85.8 pp1-60Pety Tunjung SariÎncă nu există evaluări
- Long Distance LyricsDocument3 paginiLong Distance LyricsPety Tunjung SariÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Dialog Bahasa InggirsDocument2 paginiDialog Bahasa InggirsKeRtha NeghaRaÎncă nu există evaluări
- Report - IvatanDocument28 paginiReport - IvatanJohara Winel PerezÎncă nu există evaluări
- QuantAssay Software Manual 11-Mar-2019Document51 paginiQuantAssay Software Manual 11-Mar-2019LykasÎncă nu există evaluări
- Properties of Matter ReviewDocument8 paginiProperties of Matter Reviewapi-290100812Încă nu există evaluări
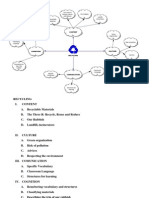
- Recycling Mind MapDocument2 paginiRecycling Mind Mapmsole124100% (1)
- PAG7.1 Student The Effects of Antibiotics On Microbial Growth - v0.3Document3 paginiPAG7.1 Student The Effects of Antibiotics On Microbial Growth - v0.3Habib UddinÎncă nu există evaluări
- 2 Contoh Narative TextDocument9 pagini2 Contoh Narative TextRini RienzÎncă nu există evaluări
- Fama Fraternitatis Rosae Crucis PDFDocument2 paginiFama Fraternitatis Rosae Crucis PDFJudy50% (2)
- Industrial Internet of Things: Presented To-Presented byDocument18 paginiIndustrial Internet of Things: Presented To-Presented byGaurav RaturiÎncă nu există evaluări
- Reactive Dyes For Digital Textile Printing InksDocument4 paginiReactive Dyes For Digital Textile Printing InksDHRUVÎncă nu există evaluări
- Abnormalities of Placenta, Amniotic Fluid and Cord: Prepared By, B. Ezhilarasi, Nursing TutorDocument21 paginiAbnormalities of Placenta, Amniotic Fluid and Cord: Prepared By, B. Ezhilarasi, Nursing TutorGopala KrishnanÎncă nu există evaluări
- Relationsh Between EM and Young S ModuliDocument7 paginiRelationsh Between EM and Young S ModuliDwight AndersonÎncă nu există evaluări
- Earth Sciences Notes Csir-Ugc Net JRFDocument57 paginiEarth Sciences Notes Csir-Ugc Net JRFmanas773Încă nu există evaluări
- Five Star Hotel and ResortDocument9 paginiFive Star Hotel and ResortAISHÎncă nu există evaluări
- Index PDFDocument159 paginiIndex PDFHüseyin IşlakÎncă nu există evaluări
- History of Flash Part - 2Document7 paginiHistory of Flash Part - 2YOGESHWER NATH SINGHÎncă nu există evaluări
- Opex and CapexDocument5 paginiOpex and CapexATM Shafiq Ul AlamÎncă nu există evaluări
- Sch3u Exam Review Ws s2018 PDFDocument4 paginiSch3u Exam Review Ws s2018 PDFwdsfÎncă nu există evaluări
- SCIENCEEEEEDocument3 paginiSCIENCEEEEEChristmae MaganteÎncă nu există evaluări
- ST 36Document4 paginiST 36ray72roÎncă nu există evaluări
- Nutrient DeficiencyDocument8 paginiNutrient Deficiencyfeiserl100% (1)
- JHS 182Document137 paginiJHS 182harbhajan singhÎncă nu există evaluări
- Aluminium Alloy - Wikipedia, The Free EncyclopediaDocument12 paginiAluminium Alloy - Wikipedia, The Free EncyclopediaAshishJoshi100% (1)
- Serial Analysis of Gene Expression (SAGE)Document34 paginiSerial Analysis of Gene Expression (SAGE)Rohit PhalakÎncă nu există evaluări
- Product Stock Exchange Learn BookDocument1 paginăProduct Stock Exchange Learn BookSujit MauryaÎncă nu există evaluări
- Chemical Bonds WorksheetDocument2 paginiChemical Bonds WorksheetJewel Mae MercadoÎncă nu există evaluări
- Reloved - October 2015Document116 paginiReloved - October 2015Barron Fields67% (3)
- TS SR Chemistry Imp Questions PDFDocument5 paginiTS SR Chemistry Imp Questions PDFUnknown Khan100% (3)
- Intro Slow Keyofg: Em7 G5 A7Sus4 G C/G D/F# AmDocument2 paginiIntro Slow Keyofg: Em7 G5 A7Sus4 G C/G D/F# Ammlefev100% (1)
- Unnatural Selection BiologyDocument2 paginiUnnatural Selection BiologyAlexa ChaviraÎncă nu există evaluări