Documente Academic
Documente Profesional
Documente Cultură
Preparation and Evaluation of Curcumin Invasomes: International Journal of Drug Delivery 6 (2014) 113-120
Încărcat de
nophadonTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Preparation and Evaluation of Curcumin Invasomes: International Journal of Drug Delivery 6 (2014) 113-120
Încărcat de
nophadonDrepturi de autor:
Formate disponibile
International Journal of Drug Delivery 6 (2014) 113-120
http://www.arjournals.org/index.php/ijdd/index
Original Research Article
ISSN: 0975-0215
Preparation and Evaluation of Curcumin Invasomes
Lakshmi PK1, Mounica V1, Manoj Kumar Y1, Prasanthi D1
*Corresponding author:
Lakshmi PK
1Department
of Pharmaceutics, G.Pulla
Reddy College of Pharmacy,
Hyderabad, India.
Abstract
Curcumin has poor aqueous solubility and has bioavailability problems. Hence in the present study
the solubility of curcumin was increased by complexing with cyclodextrin (CD) and Hydroxy propyl
cyclodextrin(HPCD). This complex is incorporated in to invasomes and then into HPMC gel to
prepare as a transdermal formulation.Curcumin cyclodextrin complexes were prepared by physical
mixture and co-precipitation method. Different formulations of invasomes containing 0.5, 1.0, 1.5 %
of limonene, fenchone, nerolidol individually were prepared using mechanical dispersion technique.
Invasomes were characterized for vesicular size, surface morphology, zeta potential, entrapment
efficiency and percutaneous permeation.Formulations CHL1 and CHL2 were optimized for further
studies. It was found in the study that complex with HPCD in 1:2 proportion prepared by coprecipitation method was found to bind 90% of curcumin.Invasomal preparation with 0.5% limonene,
4% ethanol was found to enhance permeation by 8.11 times the control.In vivo diffusion studies
were conducted using franz diffusion cell, ex vivo skin permeation studies of CHL1using rat
abdominal skin showed cumulative drug permeated (Q24)of 70.32 g/cm2, steady state transdermal
flux of 3.344 g/cm2/hr-1, permeability coefficient of 5.35 cm/hr and lag time of 1 hr when compared
with control formulation. From the results it was concluded that the solubility of curcumin increased
by complexing with HPCD and invasomal preparation with 0.5% limonene has improved
permeation through the skin.
Keywords: - Curcumin, Cyclodextrin, Invasomes, HPMCK4M gel
Introduction
Curcumin known as diferuloylmethane a yellow polyphenol is an
extract from rhizomes of Curcuma longa lin. This compound has
potency against many diseases such as cough, diabetes, anorexia,
alzheimer disease, rheumatism, hepatic disorders, antioxidant,
anti-inflammatory, anti carcinogenic, hypocholesterolemic,
antibacterial, antispasmodic, anticoagulant, anti tumor etc.
[1].Although therapeutic properties of curcumin have been the topic
of several studies widespread clinical applications of curcumin is
limited due to its poor aqueous solubility, degradation at alkaline
pH, photodegradation, low systemic bioavailability. Cyclodextrins
are 1,4 linked cyclic oligosaccharides produced by enzymatic
conversion of starch and contain atleast 6 D - (+) glucopyranose
units. -CDsare insufficient in size for many drugs while -CDsare
expensive. Usually -CD has been used extensively for many
studies because of its ready availability, cavity size and use with
wide range of drugs. Cyclodextrins are used pharmaceutically for
drug complexation, as solubilizers, diluents, bioavailability
enhancers for poorly soluble drug [2]. Serum plasma levelswere
found to be only 2.25g/ml by intra peritoneal route and 0.36g/ml
by intravenous route [3, 4]. Curcumin was complexed with cyclodextrin using co-precipitation method to increase the
solubility[5]. Anand et al., coated that nanoparticles, liposomes,
phospholipid complexes are promising novel formulations which
improve the bioavailability [6]. Transdermal route is the alternate
pathway for localized or systemic pharmacological effects.
Although advantageous in avoiding problems of poorly absorbable
drugs and enzymatic degradation, penetration through the stratum
corneum (SC) of epidermis an efficient barrier is the major
problem. Hence several techniques and carrier systems were
developed to cross this barrier.Liposomes,phospholipid vesicles
are used as drug carriers. Traditional liposomes can be used only
for topical application but they cannot deeply penetrate the skin
and are restricted to upper layers of SC [7].Hence a series of
vesicular carriers transferosomes with edge activators,
ethosomes with high amounts of ethanol, invasomes with ethanol
and terpenes were developed. Elastic vesicles have shown to be
superior in enhancing the penetration than conventional gel state
and even liquid state vesicles [8]. Terpenes like cineole, citral and
limonene are widely used for hydrophilic and lipophilic drugs.
Dragicevic-Curic et al., 2009preparedsemisolid liposomal
formulation by mixing with carbomer hydrogel to avoid leaky
behavior of liposomes on application site [8].Two proposed
mechanisms of penetration enhancement of terpenes observed are
permeation as intact vesicles and disruption of intercellular lipid
lamellae, forming channels[9].
Hence the present study deals with improving the solubility of
curcumin by complexing with CD or HPCD and then incorporating
This work is licensed under a Creative Commons Attribution 3.0 License.
Lakshmi et al. International Journal of Drug Delivery 6 (2) 113-120 [2014]
this complex mixture into vesicular carrier invasomes. This
vesicular carrier is then incorporated into HPMC K4M gel.
Invasomes are characterized for size, morphology, zeta potential,
stability. Invasomal gels are investigated for ex vivo permeation
studies.
entrapped is calculated indirectly from the amount of free drug from
the formula.
100
Materials and methods
Surface morphology
Materials
Surface morphology was studied by placing a drop of preparation
on a clear glass slide, air dried, coated with gold using sputter
coater (Polaron E5100, Watford, UK) and visualized under
Scanning electron microscope (Joel 5400, Japan).
Curcumin was procured from Sanat Products Limited, New Delhi,
Soya phosphatidylcholine-70 from Sonic-Biochem extractions,
limonene, fenchone and nerolidol procured from Alfa aesar, HPMC
K4M procured from Sigma labs, HPCD from Otto Kemi and other
analytical reagents.
Ex Vivo permeation studies
Ex vivo studies were approved by institutional animal ethics
1:1
43%
comittee. Abdominal skin section of male wistar rat was prepared
and permeation studies were performed using Franz diffusion cell.
Effective surface area of cell was 2.0 cm2 and has a receptor
volume of 20ml. Donor compartment was applied with invasomal
preparation and 20 ml of pH 7.4 phosphate buffer saline
maintained at 37C was used as receptor medium. Aliquot
amounts were withdrawn and replaced by fresh media to maintain
sink condition. Samples were analyzed using UV
spectrophotometer, steady state transdermal flux (g/cm2/hr),
permeability coefficient (cm/hr), enhancement ratio were
calculated.
1:2
61%
Preparation of Gel
1:1
65%
1:2
90%
1:1
24%
1:2
36%
Aqueous gel of 2% HPMC K4M was prepared by soaking the
polymer overnight, appropriate amounts of propylene glycol was
added and mixed until gel was formed. To this gel base optimized
invasomal suspension was added such that 500 mg of gel contains
12.5% curcumin.
1:1
43%
Speradability studies
1:2
54%
Spreadability was determined by measuring the spreading
diameter of 1g of gel between 20X20 cm glass plates for 1 min.
Mass of upper plate was standardized at 150g. It is calculated by
using the formula
Complexation of Curcumin
Curcumin was complexed with CD and HPCD according to the
formula (Table
1) by Physical Mixture and Co-precipitation
method (Zaibunnisa A.H et al., 2011)[5].
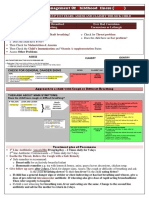
Table 1: Preparation and optimization of curcumin CD complex.
Drug:
Percentage
Carrier
Method
Carrier
bound
Physical Mixture
HPCD
Co-precipitation
Physical Mixture
CD
Co-precipitation
Preparation of invasomes
Optimized 1:2 co-precipitated complex of Curcumin and HPCD
was loaded in to invasomes by mechanical dispersion technique.
Soya Phosphotidylcholine (1 3% w/v) was added to ethanol and
vortexed for 5 minutes. Curcumin HPCD complex and different
terpenes (0.5 1.5%) were added under constant vortexing, this
mixture was sonicated for 5 minutes. Fine stream of Phosphate
buffer saline (upto 10%w/v) was added with syringe under constant
vortexing. It was vortexed for additional 5 minutes to obtain final
invasomal preparation.
Where S is spreadability, M is weight tied on upper glass plate, L is
length of glass slide, T is time in sec.
Extrudability
Extrudability was carried out by Pfizer hardness tester. 15g of gel
was filled in aluminium tube and plunger was adjusted to hold the
tube properly. Pressure of 1 Kg/cm2 was applied for 30 sec and the
mass of gel extruded was measured. This procedure is repeated at
three equidistance places of tube.
Entrapment efficiency
Skin irritant studies
Entrapment efficiency was studied by ultracentrifugation method.
1ml of invasomal suspension was transferred to Ephendroff tubes,
centrifuged at 15000 rpm, 4C for 15 min in two cycles to separate
the unentrapped drug and invasomes. Clear fraction was analyzed
for free drug at 430 nm spectrophotometrically. Percentage
Skin irritant studies were performed on 3 healthy rabbits.
Unbraided skin was cleaned with rectified spirit, control formulation
was placed on left dorsal surface and test formulation on right
dorsal surface. The formulation was removed after 24 hrs and the
114
Lakshmi et al. International Journal of Drug Delivery 6 (2) 113-120 [2014]
skin was examined for erythema/edema and scored according to
primary dermal irritation index classification.
Stability studies
Optimized invasomal gel was sealed in 10 ml glass vial and stored
at refrigeration temperature (4 - 8C) and room temperature for one
month. Entrapment efficiency, physical appearance was
determined at regular intervals.
Results and Discussion
Characterization of curcumin complex
Physical mixture, co-precipitation methods using CD, HPCD in
two ratios 1:1 and 1:2 were used for complex preparation.
Complexes prepared by co-precipitation method showed more
bonding/ complexing than the physical method. It was found that
complexation in 1:1 ratio showed 43, 65% bonding by coprecipitation method with CD and HPCD respectively which
was more than 24, 43% prepared by physical mixing method.
Similarly with 1:2 ratio it was found to be 54, 90% with CD and
HPCD by co-precipitation method where as only 36, 61% by
physical mixing method. Complex prepared by co-precipitation
method in 1:2 ratio with CD showed complexation of only 54%,
where as HPCD showed 90%. Hence co-precipitation method
showed more bonding than physical method [5] and more bonding
was observed with 1:2 proportion.
Solubility of pure curcumin was found to be 2.98X10-11M and
increased to 1.63X10-8M in HPCD whereas only 0.21X10-8M with
CD. This is accounted because of hydrophilic nature of CD
derivative HPCD which enhanced the solubility of poorly water
soluble curcumin when compared to parent CD [10]. Hence
curcumin- cyclodextrin complexes prepared by co-precipitation
method using HPCD in 1:2 proportion was optimized.
Figure 1: Comparision of FTIR spectra.
FTIR spectral studies
Compatibility studies were performed using Fourier Transform
Infrared spectrophotometer (FTIR 8400s, Shimadzu, Japan) in the
range of 4000 400 cm-1 using potassium bromide pellet method.
Pure curcumin showed absorption peaks at 3504.46 cm-1
characteristic to hydroxyl ( OH) group, peak at 1601 cm-1
characteristic to C=C of benzene ring, 1506.31 cm-1 characteristic
to C=O, C=C, peaks at 1000 1260cm-1 for C-O and are found to
be near to the absorption bands [11]. The complexed mixture with
HPCD also showed peaks in the region of 3503.84, 1601.39,
1506.73cm-1(figure 1). Retention of the peak in the region 1601
shows that complexes were not formed with carbonyl group of
curcumin and increase in intensity around the region of C-O ether
bond shows that complexation was due to this C-O bond of
curcumin [5].
Figure 2: DSC of curcumin alonend curcumin complex
DSC studies
DSC studies were performed and exothermic peaks were observed
around the region of 170 180C [12] this was because of melting
of curcumin. The reduced intensity of the peak in complex of
curcumin with HPCD indicates complexation of curcumin (figure
2).
115
Lakshmi et al. International Journal of Drug Delivery 6 (2) 113-120 [2014]
Characterization of invasomes
In vitro studies
Entrapment efficiency
In vitro diffusion studies were carried out using dialysis membrane
to evaluate release from invasomes. Release profile for 24 hrs
study is shown in figure 3.Three terpene formulations CHL1, CHL2,
CHF2 showed good release rate of 22.313.0, 20.892.8,
15.251.9
respectively. In previous studies 1% terpene formulations showed
better release [13] but the results show that 0.5% limonene showed
good release than 1% formulation this may be attributed to
presence of ethanol in the formulations. These three formulations
were selected for ex vivo studies. Although CHF1 showed good
entrapment efficiency of 88.4 0.11 because of its release rate
compared to CHF2 it was not selected for further studies.
Invasomes were prepared by mechanical dispersion method.
Preliminary studies were conducted and 1% soya
phosphotidylcholine was optimized for further studies as it showed
maximum entrapment efficiency. Curcumin-HPCD was taken as
equivalent to 5mg and incorporated into invasomes with different
terpenes limonene, fenchone, nerolidol at 3 levels 0.5, 1, 1.5%
individually and 4% of ethanol was added to all the
formulations(table 2). Entrapment efficiency of each formulation
was calculated and it was found to be maximum inCHL193.50.08%, 88.40.11 in CHF1, 87.40.12 in CHL2, 76.80.07 in
CHF2 and least in CHN3 - 58.40.06. Entrapment efficiency with
different terpenes was found in the order limonene > fenchone
>nerolidol. Limonene showed highest entrapment efficiency which
is attributed due to the presence of hydrocarbon group.
Ex vivo skin permeation studies
Ex vivo studies were approved by IAEC. Permeation studies were
conducted using excised male wistar rat abdominal skin and were
performed usingFranz diffusion cell. Cumulative drug permeated
was found to be 70.321.98 for CHL1, 60.582.61 for CHL2,
51.83.02 for CHF2 which was found to be more than control
22.892.08. D. D. Verma et al., observed increase in permeation
with increase in ethanol [14],many literatures discusses the
increase in permeation with terpene loaded vesicles when
compared with liposome vesicles. Increased permeation in
formulation with terpenes than conventional liposomes (control)
may be attributed to synergistic effect of ethanol and terpenes as
formulation CE prepared without terpenes also showed increase in
permeation of 40.322.76 [7](table 2).
Surface morphology
Characterization of invasomes
Vesicular size
Vesicle size was determined using Microtel X100 Leeds & Northrup
particle size analyzer, UK and it was observed to be 134.7nm and
poly dispersity index was < 0.2 for CHL1.
Zeta potential
Zeta potential was measured at Malvern Instruments Ltd using
Zeta sizer and was found to be -33.7mv for CHL1. Negative charge
may be imparted due to the presence of ethanol [7,12].
90
80
%drugrelease
70
60
CHL1
CHL2
50
CHL3
CHF1
40
CHF2
CHF3
30
CHN1
CHN2
20
CHN3
10
0
0
10
15
Time(Hours)
20
25
30
Figure 3: Release profile of prepared invasomal formulations.
with CHL1 3.34 0.08 and increased flux of 3.02 0.07 with CHL2
and 2.28 0.16 with CHF2.
Penetration parameters like steady state transdermal flux and
permeability coefficient were calculated. Control formulation
showed flux of 0.410.14 g/cm2/hr, maximum flux was observed
116
Lakshmi et al. International Journal of Drug Delivery 6 (2) 113-120 [2014]
JSS steady state flux, dM amount of drug permeated, S unit of
cross section, t time, CV total concentration in the donar
compartment, Kp permeability coefficient.
Permeability coefficient was found to be 5.350.03 X10-3 with
CHL1, 4.830.07X10-3, 3.660.06X10-3 with CHL2 and CHF2,
where as only 0.320.04X10-3 with control and 0.980.09 CE (with
out terpenes).
Enhancement ratio
Permeability
Coefficient
cm/hr)
ND
ND
22.89 2.08
0.41 0.14
0.32 0.04
3.6 0.12
CE
ND
ND
40.322.76
1.730.19
0.980.09
4.2
2.40.5
CHL1
0.5
93.5 0.08
22.31 3.0
70.32 1.98
3.34 0.08
5.35 0.03
8.11
1 0.2
CHL2
87.4 0.12
20.89 2.8
60.58 2.64
3.02 0.07
4.83 0.07
7.33
1.2 0.1
CHL3
1.5
82.2 0.06
19.34 2.4
ND
ND
ND
ND
ND
CHF1
0.5
88.4 0.11
14.26 1.0
ND
ND
ND
ND
Lag time
hrs
Nerolidol
(%)
Control
SSTF
g/cm2/hr
Fenchone
(%)
Cumulative
permeated
(Q24)g/cm2
(X10-3
drug
rate
Release
g/cm2/hr1/2
Entrapment efficiency
SD
Limonene
(%)
Formulation code
Table 2: Formulation and Evaluation results of Invasome preparations
CHF2
76.8 0.07
15.25 1.9
51.8 3.02
2.28 0.16
3.66 0.06
5.55
ND
1.9 0.6
CHF3
1.5
68.7 0.13
10.33 2.0
ND
ND
ND
ND
ND
CHN1
0.5
76.5 0.08
12.98 2.8
ND
ND
ND
ND
ND
CHN2
64.8 0.12
14.86 2.7
ND
ND
ND
ND
ND
CHN3
1.5
58.4 0.06
8.79 2.7
ND
ND
ND
ND
ND
CNT G
7.98 1.86
0.28 0.03
0.450.02
4.20.2
CHL1G
52.8 2.32
2.21 0.27
3.530.08
7.78
2.5 0.1
CHL2G
42.32 2.52
1.77 0.08
2.840.04
6.25
20.05
Curcumin Hydroxy propyl cyclodextrin complex 5 mg (5% w/v), Soya lecithin
Fenchone, N- nerolidol, ND- not determined, SSTF - Steady state transdermal flux.
1%, Ethanol
4% in all formulations except control, L-limonene, F-
The optimized invasomal suspension CHL1, CHL2 was
incorporated in to 2% HPMC K4M which was optimized by
preliminary trials. Prepared gel was inspected under black and
white background and was found very clear and without any
aggregates.
The pH of the gel was determined using digital pH meter LI 127
Elico. 0.5g of gel was dispersed in 100 ml of pH 7.4 Phosphate
buffer and checked for its pH. It was found to be 6.9, 7.0 for CHL1,
CHL2 respectively.
Spreadability and Extrudability were performed as mentioned
earlier and spreadability was found to be 27.07cm, 24.96cm for
CHL1, CHL2 respectively, and extrudability was found to be
excellent.
Viscosity was measured using LV DV-II+Pro Brookfield
programmable viscometer with spindle 64, and was found to be
39822cp, 38961cp with CHL1, CHL2 respectively.
Enhancement ratio was calculated by comparing the formulations
CHL1, CHL2, CHF2 with Control. CHL1 was found to enhance by
8.11 time and only 7.33, 5.55 times with CHL2, CHF2 respectively.
T. Subongkot et al. also reported enhancement of 6.8 8 folds in
ultradeformable vesicles compared to liposomes [9]. Lag time
decreased with the use of terpenes when compared with control
from 3.60.12 for control to 10.2, 1.20.1, 1.90.6 for CHL1,
CHL2, CHF2 respectively owing to increased permeation effect of
terpenes. Permeation enhancement of present study are in
controversy with other authors but are according to the results of
work of A. F. El-kattan et al., 2001 [16] where limonene showed
high entrapment with lipophilic drugs. The increase in the
permeation observed with limonene may be due to its lipophilicity
and low boiling point [17] and lipophilic nature of curcumin.
Organoleptic characterization of gel
117
Lakshmi et al. International Journal of Drug Delivery 6 (2) 113-120 [2014]
Statistical analysis
Ex vivo studies were conducted for prepared gels and were
compared with control. Release profile is shown in figure 4.
Cumulative drug permeated was found to be 52.82.32,
42.322.52g/cm2for CHL1G, CHL2G but with control it was just
7.981.86g/cm2. Steady state transdermal flux was found to be
2.210.27, 1.770.08g/cm2/hr for CHL1G, CHL2G respectively
and 0.280.03 g/cm2/hr for control. Permeability coefficient was
3.530.08X10-3, 2.840.04X10-3 for CHL1G, CHL2G and
0.450.02X10-3 cm/hr. Enhancement ratio was found to be 7.78,
6.25 times for CHL1G,CHL2G. Lag time decreased from 4.20.2
for control to 2.50.11, 20.05 hrs for CHL1G, CHL2G
respectively. Drug permeation, flux, enhancement ratio and lag
time was observed to be high for gel preparation with CHL1G
The results obtained were analyzed statistically using one way
ANOVA (Tukeys multiple comparison test) and is depicted in (table
3).Results of control and CHL1 were significant (p<0.001) in SSTF,
Q24, permeability coefficient, enhancement ratio and lag time,
CHL1 and CHL2 were significant (p<0.001) in permeability
coefficient and enhancement ratio but Q24, SSTF and lag time
were not significant (p>0.05). CHL1 and CHF2 were significant
(p<0.01) in permeability and enhancement, Q24 and SSTF but lag
time was not significant (p.0.05). Comparing CHL2 with control
showed significance of p<0.001 for SSTF, Q24, permeability
coefficient, enhancement ratio, lag time. CHL2 and CHF2 are
significant in permeability, enhancement (p<0.001), Q24 and SSTF
were not significant. Comparing CHF2 with control Q24,
permeability coefficient, enhancement ratio showed significance of
p<0.01, SSTF with significance of P<0.005 and significance of
p<0.01 in lag time.
SSTF, Q24, permeability coefficient, enhancement ratio and lag
time were observed to be significant to p<0.001 in CHL1G and
CHL2G with control but lag time was not significant in CHL2G.
SSTF, Q24, permeability coefficient, enhancement ratio were
significant but lag time was not significant (p>0.05) when
comparing CHL1G, CHL2G.
From this analysis it is observed that terpenes shows significant
effect on permeability coefficient and flux was influenced by
permeability enhancer. Least lag time was observed with CHL2G
60
40
CHL1
CHL2
20
CNT
0
0
10
Time(hrs)
20
30
Figure 4: Ex vivo permeation studies
Table 3: Statistical analysis by ANOVA (Tukeys multiple comparison test)
CNT vs CHL1
Cumulative amount
permeated (Q24)
***
CNT vs CHL2
***
Permeability
coefficient
***
Enhancement
ratio
***
***
***
***
***
***
***
CNT vs CHF2
***
***
***
**
F value
61.26
17.88
9640
18610
23.94
CHL1 vs CHL2
NS
NS
***
***
NS
CHL1 vs CHF2
**
***
***
NS
CHL2 vs CHF2
NS
NS
***
***
NS
F Value
61.26
17.88
9640
18610
23.94
CNT vs CHL1G
***
***
***
***
NS
CNT vs CHL2G
***
***
***
***
CHL1G vs CHL2G
***
***
***
***
NS
3.565e+006
5.922
SSTF
Gel
Invasomes
Control vs Other
formulations
Parameters
Comparision with in formulations
Cummulativeamount
permeated(g/cm2)
Ex vivo studies of gel
F value
1.031e+006
191731
488463
n = 2; *** (p<0.001); ** (p<0.01); * (p<0.005); NS non significant (p>0.05)
118
Lag time
Lakshmi et al. International Journal of Drug Delivery 6 (2) 113-120 [2014]
CHL1
Table 4: release kinetics of prepared invasomes and gel.
Zero order
First order
Higuchi
Peppas
r2
r2
r2
r2
n
0.990
0.9068
0.952
0.982
0.434
Fickian diffusion
CHL2
0.996
0.7341
0.936
0.923
0.471
Fickian diffusion
CHF2
0.995
0.8202
0.939
0.969
0.472
Fickian diffusion
CHL1G
0.992
0.9078
0.962
CHL2G
0.986
0.7641
0.926
Release kinetics of optimized 0 order kinetics, fickian n<0.5
0.982
0.943
0.454
0.431
Fickian diffusion
Fickian diffusion
Ge
Invasomes
l
Formulations
Release mechanism
Release kinetics
Conclusion
Release kinetics was observed by fitting the data in to Zero order,
First order, Higuchis, Korsemeyer peppas equations and was
found to follow zero order release with Fickian diffusion
mechanism.Table-4
Skin irritation studies were performed on depilated rabbit and was
assessed and scored according to primary dermal irritation index
classification. Gel formulation CHL1G was applied on to depilated
skin and was confirmed that there was no sign of erythema or
edema.
Because of its poor solubility, its instability in alkaline pH curcumin
is formulated as transdermal formulation. Curcumin was
complexed with CD and HPCD. Improved solubility and stability
was observed with HPCD prepared by co-precipitation method
than physical mixture method. Optimized complex ie., 1:2
proportion complex is incorporated into invasomes with limonene,
fenchone, nerolidol as terpenes which acted as phospholipid
membrane flexibilizers, penetration enhancers. 1% soya
phosphotidylcholine, 0.5% limonene was optimized which showed
Q24 of 70.32 g/cm2, SSTF of 3.34 g/cm2/hr-1, permeability
coefficient of 5.35 cm/hr, and decreased lag time of 1 hr.
formulation CHL1 was found to be better in all characteristics and
was incorporated into 2% HPMC K4M gel formulation. Further in
vivo studies are to be carried out to assess the pharmacokinetics of
curcumin invasomal formulations.
Stability studies
Stability studies of optimized formulation was carried out by sealing
the formulation in 10 ml glass vial and refrigerated at 4 - 8C and at
room temperature for 1 month. Drug content was determined and
there was a decrease of only 10 % of entrapped drug after 1 month
when stored at refrigeration. But when stored at room temperature
the loss was upto 50%. Hence curcumin loaded invasomes are
stored at 4 - 8C as aggravated temperatures causes leaking by
transition of lipid bilayer or chemical degradation of lipids.
Abbreviations
HPMC- Hydroxy propyl methyl cellulose
References
[1]. Moin K. Modasiya, Vishnu M. Patel.
Curcumin: Properties and medicinal
applications. American Journal of
PharmTech Research. 2011; 1(3):
39 56.
[2]. G. Astray, C. Gonzalez-Barreiro,
J.C. Mejuto, R. Rial-Otero, J. SimalGandara. A review on the use of
cyclodextrins in foods. Food
Hydrocolloids. 2009;23(7): 1631
1640.
[3]. Pan MH, Huang TM, Lin JK.
Biotransfromatin
of
curcumin
through
reduction
and
glucuronidation in mice. Drug
Metabolism
and
Disposition.
1999;27: 486 494.
[4]. Kuo-Yi Yang, Lei-Chewen Lin, TingYu Tseng, Shau-Chun Wang, TungHu Tsai. Oral bioavailability of
curcumin in rat and the herbal
analysis from Curcuma longa by LCMS/MS. Journal of Chromatography
B. Analytical Technologies in the
Biomedical and Life Sciences.
2007;853(1-2): 183 -189.
[5]. Zaibunnisa A. H., Siti Rashmima R.
Nur Ain A. H. Stabilisation of
curcumin with -cyclodextrin: phase
solubility
study
and
its
characterization.
International
Proceedings of Chemical, Biological
and Environmental Engineering.
2011; 7: 9 13.
[6]. Preetha Anand, Ajaikumar B,
Kunnumakkara, Robert A. Newman,
119
Bharat B. Aggarwal. Bioavailability
of Curcumin: Problems and
Promises. Molecular Pharmaceutics;
4(6): 807 818.
[7]. Mohamed Badran, Gamal Shazly,
Mohmoud El-Badry. Effect of
terpene
liposomes
on
the
transderamal
delivery
of
hydrophobic
model
drug,
nimesulide:
Characterization,
stability and in vitro skin permeation.
African Journal of Pharmacy and
Pharmacology. 2012; 6(43): 3018
3026.
[8]. Nina Dragicevic-Curic, Dietrich
Scheglmann, Volker Albrecht, Alfred
Fahr. Development of different
temoporfin-loaded invasomes-novel
nanocarriers
of
temoporfin:
Lakshmi et al. International Journal of Drug Delivery 6 (2) 113-120 [2014]
Characterizatrion, stability and
invitro skin penetration studies.
Colloids
and
Surfaces
B:
Biointerfaces. 2009; 70: 198 206.
[9]. Thirapit Subongkot, Sureewan
Duangjit, Theerasak Rojanarata,
Praneet Opanasopit, and Tanasait
Ngawhirunpat.
Ultradeformable
liposomes with terpenes for delivery
of hydrophilic compound. Journal of
Liposome Research. 2012; 22(3):
254 262.
[10]. Hajime Matsuda, Hidetoshi Arima.
Cyclodextrins in transdermal and
rectal delivery. Advanced Drug
Delivery Reviews. 1999; 36: 81
89.
[11]. Murali Mohan Yallapu, Meena Jaggi,
Subhash
C.
Chauhan.
Cyclodextrin-curcumin self assembly
enhances curcumin delivery in
prostate cancer cells. Colloids and
surfaces B: Biointerfaces. 2010; 79:
113 125.
Journal of Controlled Release. 2004;
97: 55 66.
[12]. Anant Paradkar, Anushuman A.
Ambike, Bhimrao K. Jadhav, K.R.
Mahadik.
Characterization
of
curcumin
PVP solid dispersion
obtained
by
spray
drying.
International
Journal
of
Pharmaceutics. 2004; 271: 281
286.
[15]. Boddupalli Bindu Madhavi, Kallem
Siri Vennela, Prasad Masana,
Bhavana Madipoju. Enhanced
transdermal drug penetration of
curcumin via ethosomes. Malaysian
Journal of Pharmaceutical Sciences.
2013; 11(1): 49 58.
[13]. Nina Dragicevic-Curic, Dietrich
Scheglmann, Volker Albrecht, Alfred
Fahr.
Temoporfin-loaded
invasomes:
Development,
characterization and in vitro skin
permeation studies. Journal of
Controlled Release. 2008; 127: 59
69.
[14]. D.D. Verma, A. Fahr. Synergistic
penetration enhancement effect of
ethanol and phospholipids on the
topical deliver of cyclosporine A.
120
[16]. Ayman F. El-Kattan, Charles S.
Asbill, Nanhye Kim, Bozena B.
Michniak. The effects of terpene
enhancers on the percutaneous
permeation of drugs with different
lipophilicities. International Journal
of Pharmaceutics. 2001; 215: 229
240.
[17]. Kalpana B, Lakshmi P K.
Transdermal
permeation
enhancement of Tolterodine tartrate
through
invasome
and
iontophoresis.
Der Pharmacia
Lettre, 2013; 5(6): 119 126.
S-ar putea să vă placă și
- Parenteral Products: The Preparation and Quality Control of Products for InjectionDe la EverandParenteral Products: The Preparation and Quality Control of Products for InjectionÎncă nu există evaluări
- Formulation and Evaluation of Glimepiride Oral CapsulesDocument13 paginiFormulation and Evaluation of Glimepiride Oral CapsulesinventionjournalsÎncă nu există evaluări
- A Comprehensive Book on Experimental PharmaceuticsDe la EverandA Comprehensive Book on Experimental PharmaceuticsEvaluare: 5 din 5 stele5/5 (1)
- Formulation and Evaluation of Transdermal Patch of Repaglinide PDFDocument9 paginiFormulation and Evaluation of Transdermal Patch of Repaglinide PDFapa menÎncă nu există evaluări
- Gel AnDocument5 paginiGel AnerikÎncă nu există evaluări
- Formulation and Evaluation of Sublingual Tablets of Asenapine Maleate by 32 Full Factorial DesignDocument15 paginiFormulation and Evaluation of Sublingual Tablets of Asenapine Maleate by 32 Full Factorial DesignPRASANTA KUMAR MOHAPATRAÎncă nu există evaluări
- Tds 4Document4 paginiTds 4Neha YadavÎncă nu există evaluări
- Pandit Et Al HPMC Karbopol 2%Document6 paginiPandit Et Al HPMC Karbopol 2%kristinedp92Încă nu există evaluări
- Curcuminoid in Curcuma Xanthoriza PDFDocument5 paginiCurcuminoid in Curcuma Xanthoriza PDFFajarRachmadiÎncă nu există evaluări
- Cucumber MucilageDocument18 paginiCucumber Mucilagesaicharan88417Încă nu există evaluări
- Literature ReviewDocument10 paginiLiterature Review006giriÎncă nu există evaluări
- Shiv IJCRRDocument10 paginiShiv IJCRRnavodaya9Încă nu există evaluări
- Comparison Effect of Penetration Enhancer On Drug Delivery SystemDocument7 paginiComparison Effect of Penetration Enhancer On Drug Delivery SystemSanjesh kumar100% (1)
- Drug DeliveryDocument8 paginiDrug DeliveryHarry SetiawanÎncă nu există evaluări
- Development and Evaluations of Transdermal Delivery of Selegiline HydrochlorideDocument14 paginiDevelopment and Evaluations of Transdermal Delivery of Selegiline HydrochlorideInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Formulation and Evaluation of in Situ Gels Containing Clotrimazole For Oral CandidiasisDocument7 paginiFormulation and Evaluation of in Situ Gels Containing Clotrimazole For Oral CandidiasisAndika DikaÎncă nu există evaluări
- Formulation and Design of Sustained Release Matrix Tablets of Metformin Hydrochloride - Influence of Hypromellose and Polyacrylate PolymersDocument10 paginiFormulation and Design of Sustained Release Matrix Tablets of Metformin Hydrochloride - Influence of Hypromellose and Polyacrylate PolymersDIKAÎncă nu există evaluări
- FlubiprofenDocument5 paginiFlubiprofenPradeep BhimaneniÎncă nu există evaluări
- JPSR 03110106Document9 paginiJPSR 03110106sunilpdÎncă nu există evaluări
- Formulation and Evaluation of Buccal Patches of Simvastatin by Using Different PolymersDocument6 paginiFormulation and Evaluation of Buccal Patches of Simvastatin by Using Different PolymersIsrawan AzisÎncă nu există evaluări
- 1223-Article Text-4692-1-10-20081006 PDFDocument6 pagini1223-Article Text-4692-1-10-20081006 PDFJosé RojasÎncă nu există evaluări
- MMR 15 03 1109Document8 paginiMMR 15 03 1109SoniaÎncă nu există evaluări
- International Journal of Pharma and Bio Sciences V1 (2) 2010Document10 paginiInternational Journal of Pharma and Bio Sciences V1 (2) 2010Richard MoralesÎncă nu există evaluări
- Formulation Development and Evaluation of TransferDocument10 paginiFormulation Development and Evaluation of TransferOktavia Rahayu AÎncă nu există evaluări
- Design, Development of Formulation of Eperisone Hydrochrodide Floating Sustain Realease Tablet and Its EvaluationDocument22 paginiDesign, Development of Formulation of Eperisone Hydrochrodide Floating Sustain Realease Tablet and Its EvaluationabhitavÎncă nu există evaluări
- Sajp2 (4) 315 318Document4 paginiSajp2 (4) 315 318Habibur RahmanÎncă nu există evaluări
- 4.kalpana ArticleDocument5 pagini4.kalpana ArticleBaru Chandrasekhar RaoÎncă nu există evaluări
- Data 1Document7 paginiData 1Citra MalasariÎncă nu există evaluări
- Effect of Alcohols and Enhancers On Permeation Enhancement of KetorolacDocument6 paginiEffect of Alcohols and Enhancers On Permeation Enhancement of KetorolacDiana RalucaÎncă nu există evaluări
- 1214 Full PDFDocument6 pagini1214 Full PDFFeslyAnugerahAriestaPayungÎncă nu există evaluări
- Formulation Development and Evaluation of Transdermal Patches of LosartanDocument8 paginiFormulation Development and Evaluation of Transdermal Patches of LosartanYvd SinghÎncă nu există evaluări
- Development and Characterization of Prednisolone Liposomal Gel For The Treatment of Rheumatoid ArthritisDocument5 paginiDevelopment and Characterization of Prednisolone Liposomal Gel For The Treatment of Rheumatoid Arthritismazahir razaÎncă nu există evaluări
- Formulation and Evaluation of Sustained Release Sodium Alginate Microbeads of CarvedilolDocument8 paginiFormulation and Evaluation of Sustained Release Sodium Alginate Microbeads of CarvedilolDelfina HuangÎncă nu există evaluări
- Formulation Study of Topically Applied LotionDocument14 paginiFormulation Study of Topically Applied LotionEkky Husnie HilmansyahÎncă nu există evaluări
- th62 PDFDocument7 paginith62 PDFSnoAbuAlSamedÎncă nu există evaluări
- 8 CF 3Document10 pagini8 CF 3nelisaÎncă nu există evaluări
- Formulation and in Vitro/in Vivo Evaluation of Sustained Release Diltiazem Matrix TabletsDocument6 paginiFormulation and in Vitro/in Vivo Evaluation of Sustained Release Diltiazem Matrix TabletsKikhan Kiki KhandeaÎncă nu există evaluări
- Starch Microspheres With EPCLDocument9 paginiStarch Microspheres With EPCLancutauliniuc@yahoo.comÎncă nu există evaluări
- Design, Optimization, and Evaluation of Capecitabine-Loaded Chitosan Microspheres For Colon TargetingDocument11 paginiDesign, Optimization, and Evaluation of Capecitabine-Loaded Chitosan Microspheres For Colon TargetingNerita PuputhÎncă nu există evaluări
- Formulation and In-Vitro Evaluation of Glibenclamide Dry Emulsion in Vegetarian CapsulesDocument5 paginiFormulation and In-Vitro Evaluation of Glibenclamide Dry Emulsion in Vegetarian CapsulesBaru Chandrasekhar RaoÎncă nu există evaluări
- John 2013Document5 paginiJohn 2013Fhyrdha Slaluw ZetiaaÎncă nu există evaluări
- Formulation and Evaluation of Diclofenac Transdermal Gel PDFDocument12 paginiFormulation and Evaluation of Diclofenac Transdermal Gel PDFmariatikÎncă nu există evaluări
- TransdermalDocument7 paginiTransdermaldrugdrugÎncă nu există evaluări
- The Curcuminoids Extract of Curcuma Xanthorrhiza RoxB. Loaded Solid Lipid Nanoparticles.Document5 paginiThe Curcuminoids Extract of Curcuma Xanthorrhiza RoxB. Loaded Solid Lipid Nanoparticles.Gregory KalonaÎncă nu există evaluări
- Development and Evaluation of Transdermal Patches With Cissus Quadrangularis Plant ExtractDocument6 paginiDevelopment and Evaluation of Transdermal Patches With Cissus Quadrangularis Plant ExtractMeirianaÎncă nu există evaluări
- GlibenclamideDocument13 paginiGlibenclamiderotuaserevinaÎncă nu există evaluări
- Formulación Carbopol y HPMC - Estabilidad, Viscodias Pruebas en RataDocument6 paginiFormulación Carbopol y HPMC - Estabilidad, Viscodias Pruebas en RataLuz ArriagaÎncă nu există evaluări
- Formulation and Evaluation of Montelukast Sodium and Levocetirizine Dihydrochloride Sublingual TabletsDocument5 paginiFormulation and Evaluation of Montelukast Sodium and Levocetirizine Dihydrochloride Sublingual TabletsNeerajÎncă nu există evaluări
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocument8 paginiFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyÎncă nu există evaluări
- Beta-Cyclodextrin Solid DispersionDocument30 paginiBeta-Cyclodextrin Solid Dispersiondarkarva84100% (1)
- Pjps 25 2 2012 365 PDFDocument5 paginiPjps 25 2 2012 365 PDFdanielguerinÎncă nu există evaluări
- Fix 1Document7 paginiFix 1ジェラールフェルナンデスÎncă nu există evaluări
- Anisree G s12Document4 paginiAnisree G s12Iin Eirkha LembayungÎncă nu există evaluări
- Formulation and Evaluation of Tramadol Hydrochloride Loaded Transferosomal Gel by Thin Film Hydration TechniqueDocument8 paginiFormulation and Evaluation of Tramadol Hydrochloride Loaded Transferosomal Gel by Thin Film Hydration TechniqueIJAR JOURNALÎncă nu există evaluări
- Jurnal First Pass MetabolismDocument11 paginiJurnal First Pass MetabolismLelyta Ayu DewankgaÎncă nu există evaluări
- Permeation EnhancerDocument20 paginiPermeation EnhancerOmerMahdiÎncă nu există evaluări
- Jurnal Transdermal IbuprofenDocument12 paginiJurnal Transdermal IbuprofenRatissa Eka NingtiyasÎncă nu există evaluări
- Formulation Development and Evaluation of Medicated Jelly With Cuminum Cyminum Extract and Its Comparative Study Using Different Jelling AgentsDocument7 paginiFormulation Development and Evaluation of Medicated Jelly With Cuminum Cyminum Extract and Its Comparative Study Using Different Jelling AgentsBaru Chandrasekhar RaoÎncă nu există evaluări
- Formulation and Evaluation of Miconazole NiosomesDocument4 paginiFormulation and Evaluation of Miconazole NiosomesNovitra DewiÎncă nu există evaluări
- RTC Pharma07CatalogWebDocument168 paginiRTC Pharma07CatalogWebnophadonÎncă nu există evaluări
- Raw Milk FinalDocument32 paginiRaw Milk FinalnophadonÎncă nu există evaluări
- Site Validation Master Plan: Releasing Its Full PotentialDocument32 paginiSite Validation Master Plan: Releasing Its Full PotentialnophadonÎncă nu există evaluări
- Foodec Application MilkDocument6 paginiFoodec Application MilknophadonÎncă nu există evaluări
- Gerson Therapy HandbookDocument149 paginiGerson Therapy HandbookSonya Edwards100% (9)
- Chapter 4 Occupational Safety Hazards in Food Service OperationsDocument14 paginiChapter 4 Occupational Safety Hazards in Food Service OperationsStraichea Mae TabanaoÎncă nu există evaluări
- Foldable HelmetDocument16 paginiFoldable Helmetharsha kotewarÎncă nu există evaluări
- Chapter 5, Abdominal TraumaDocument41 paginiChapter 5, Abdominal TraumaRandy HarrisÎncă nu există evaluări
- Smith KJ Student Mathematics Handbook and Integral Table ForDocument328 paginiSmith KJ Student Mathematics Handbook and Integral Table ForStrahinja DonicÎncă nu există evaluări
- Bomber JacketDocument3 paginiBomber JacketLaura Carrascosa FusterÎncă nu există evaluări
- International Travel Insurance Policy: PreambleDocument20 paginiInternational Travel Insurance Policy: Preamblethakurankit212Încă nu există evaluări
- BiPAP ST Clinical ManualDocument37 paginiBiPAP ST Clinical ManualEng. Edelson Martins100% (2)
- DEAD STARS by Paz Marquez BenitezDocument17 paginiDEAD STARS by Paz Marquez BenitezArmiethazen Khea Page PalarcaÎncă nu există evaluări
- An Evaluation of The Strength of Slender Pillars G. S. Esterhuizen, NIOSH, Pittsburgh, PADocument7 paginiAn Evaluation of The Strength of Slender Pillars G. S. Esterhuizen, NIOSH, Pittsburgh, PAvttrlcÎncă nu există evaluări
- Worksheet - Labeling Waves: NameDocument2 paginiWorksheet - Labeling Waves: NameNubar MammadovaÎncă nu există evaluări
- Motor Starting: Why Do The Calculation?Document13 paginiMotor Starting: Why Do The Calculation?carlos_eqnÎncă nu există evaluări
- 4th Semester Electrical Engg.Document19 pagini4th Semester Electrical Engg.Bhojpuri entertainmentÎncă nu există evaluări
- Chapter 5 TEstDocument18 paginiChapter 5 TEstJeanneau StadegaardÎncă nu există evaluări
- Pediatric Gynecology BaruDocument79 paginiPediatric Gynecology BaruJosephine Irena100% (2)
- Osce05ans 110918053819 Phpapp01Document20 paginiOsce05ans 110918053819 Phpapp01masood alamÎncă nu există evaluări
- Circle Theorem 1Document3 paginiCircle Theorem 1yaw197Încă nu există evaluări
- Battery Installation ProcedureDocument5 paginiBattery Installation ProceduresantoshkumarÎncă nu există evaluări
- Onitsuka Tiger PDFDocument67 paginiOnitsuka Tiger PDFAhmad Bilal MawardiÎncă nu există evaluări
- IMCI UpdatedDocument5 paginiIMCI UpdatedMalak RagehÎncă nu există evaluări
- Nissan 720 L4-2.0-Z20 1983-86 Manual PDFDocument641 paginiNissan 720 L4-2.0-Z20 1983-86 Manual PDFEduardo Ariel JuarezÎncă nu există evaluări
- Foundation Design LectureDocument59 paginiFoundation Design LectureJamaica MarambaÎncă nu există evaluări
- Soccer Training DiaryDocument1 paginăSoccer Training DiaryMark DeaconÎncă nu există evaluări
- Certificate of No Damages in EarthquakeDocument5 paginiCertificate of No Damages in EarthquakeLemlem BardoquilloÎncă nu există evaluări
- DSR Codes - 1Document108 paginiDSR Codes - 1lakkireddy seshireddyÎncă nu există evaluări
- SVR Neuro Quote 2 PROvidoDocument3 paginiSVR Neuro Quote 2 PROvidoChejarla Naveen KumarÎncă nu există evaluări
- Operating Manual CSDPR-V2-200-NDocument19 paginiOperating Manual CSDPR-V2-200-NJohnTPÎncă nu există evaluări
- Editor: Lalsangliana Jt. Ed.: H.Document4 paginiEditor: Lalsangliana Jt. Ed.: H.bawihpuiapaÎncă nu există evaluări
- Initiation in Pre-Tantrasamuccaya Kerala Tantric Literature PDFDocument24 paginiInitiation in Pre-Tantrasamuccaya Kerala Tantric Literature PDFVenkateswaran NarayananÎncă nu există evaluări
- Classical Feedback Control With MATLAB - Boris J. Lurie and Paul J. EnrightDocument477 paginiClassical Feedback Control With MATLAB - Boris J. Lurie and Paul J. Enrightffranquiz100% (2)
- Process Plant Equipment: Operation, Control, and ReliabilityDe la EverandProcess Plant Equipment: Operation, Control, and ReliabilityEvaluare: 5 din 5 stele5/5 (1)
- Sodium Bicarbonate: Nature's Unique First Aid RemedyDe la EverandSodium Bicarbonate: Nature's Unique First Aid RemedyEvaluare: 5 din 5 stele5/5 (21)
- Process Steam Systems: A Practical Guide for Operators, Maintainers, and DesignersDe la EverandProcess Steam Systems: A Practical Guide for Operators, Maintainers, and DesignersÎncă nu există evaluări
- An Introduction to the Periodic Table of Elements : Chemistry Textbook Grade 8 | Children's Chemistry BooksDe la EverandAn Introduction to the Periodic Table of Elements : Chemistry Textbook Grade 8 | Children's Chemistry BooksEvaluare: 5 din 5 stele5/5 (1)
- Structural Analysis and Design of Process EquipmentDe la EverandStructural Analysis and Design of Process EquipmentÎncă nu există evaluări
- Piping Engineering Leadership for Process Plant ProjectsDe la EverandPiping Engineering Leadership for Process Plant ProjectsEvaluare: 5 din 5 stele5/5 (1)
- Well Control for Completions and InterventionsDe la EverandWell Control for Completions and InterventionsEvaluare: 4 din 5 stele4/5 (10)
- The Perfumed Pages of History: A Textbook on Fragrance CreationDe la EverandThe Perfumed Pages of History: A Textbook on Fragrance CreationEvaluare: 4 din 5 stele4/5 (1)
- An Applied Guide to Water and Effluent Treatment Plant DesignDe la EverandAn Applied Guide to Water and Effluent Treatment Plant DesignEvaluare: 5 din 5 stele5/5 (4)
- Lees' Process Safety Essentials: Hazard Identification, Assessment and ControlDe la EverandLees' Process Safety Essentials: Hazard Identification, Assessment and ControlEvaluare: 4 din 5 stele4/5 (4)
- Understanding Distillation Using Column Profile MapsDe la EverandUnderstanding Distillation Using Column Profile MapsÎncă nu există evaluări
- Functional Safety from Scratch: A Practical Guide to Process Industry ApplicationsDe la EverandFunctional Safety from Scratch: A Practical Guide to Process Industry ApplicationsÎncă nu există evaluări
- Troubleshooting Vacuum Systems: Steam Turbine Surface Condensers and Refinery Vacuum TowersDe la EverandTroubleshooting Vacuum Systems: Steam Turbine Surface Condensers and Refinery Vacuum TowersEvaluare: 4.5 din 5 stele4.5/5 (2)
- Coupled CFD-DEM Modeling: Formulation, Implementation and Application to Multiphase FlowsDe la EverandCoupled CFD-DEM Modeling: Formulation, Implementation and Application to Multiphase FlowsÎncă nu există evaluări
- Troubleshooting Process Plant Control: A Practical Guide to Avoiding and Correcting MistakesDe la EverandTroubleshooting Process Plant Control: A Practical Guide to Avoiding and Correcting MistakesEvaluare: 1 din 5 stele1/5 (2)
- A New Approach to HAZOP of Complex Chemical ProcessesDe la EverandA New Approach to HAZOP of Complex Chemical ProcessesÎncă nu există evaluări
- Guidelines for Chemical Process Quantitative Risk AnalysisDe la EverandGuidelines for Chemical Process Quantitative Risk AnalysisEvaluare: 5 din 5 stele5/5 (1)
- Handbook of Cosmetic Science: An Introduction to Principles and ApplicationsDe la EverandHandbook of Cosmetic Science: An Introduction to Principles and ApplicationsH. W. HibbottEvaluare: 4 din 5 stele4/5 (6)
- Pulp and Paper Industry: Emerging Waste Water Treatment TechnologiesDe la EverandPulp and Paper Industry: Emerging Waste Water Treatment TechnologiesEvaluare: 5 din 5 stele5/5 (1)
- The Periodic Table of Elements - Halogens, Noble Gases and Lanthanides and Actinides | Children's Chemistry BookDe la EverandThe Periodic Table of Elements - Halogens, Noble Gases and Lanthanides and Actinides | Children's Chemistry BookÎncă nu există evaluări
- Guidelines for the Management of Change for Process SafetyDe la EverandGuidelines for the Management of Change for Process SafetyÎncă nu există evaluări
- Fun Facts about Carbon : Chemistry for Kids The Element Series | Children's Chemistry BooksDe la EverandFun Facts about Carbon : Chemistry for Kids The Element Series | Children's Chemistry BooksÎncă nu există evaluări