Documente Academic
Documente Profesional
Documente Cultură
Blood Banking Lec (Part 1)
Încărcat de
Scott Tabuena GonzalesDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Blood Banking Lec (Part 1)
Încărcat de
Scott Tabuena GonzalesDrepturi de autor:
Formate disponibile
What is immunohematology?
Serologic, genetic, biochemical, and
molecular study of antigens associated with
membrane structures on the cellular
constituents of blood, as well as the
immunologic properties and reactions of
blood component
(Henry, 2011)
Study of blood related antigens and
antibodies as applied to situations in blood
bank and the transfusion service (Whitlock,
2010)
Historical Timeline
1492
Pope Innocent VII
First recorded blood transfusion in
history
1667
Jean Baptiste Denis: first recorded
animal-to-human blood transfusion (calf
blood)
Richard Lower: sheeps blood
1795
Philip Syng Physick: unconfirmed first
human-to-human transfusion
1816
John Henry Leacock: On the
Transfusion of Blood in Extreme Cases
of Hemorrhage
James Blundell: took inspiration from
Leacock in performing transfusions for
women suffering from postpartum
hemorrhages
Late 1800s
Emil Ponfick: RBC lysis in a blood of a
woman who died after sheep blood
transfusion
Leonard Landois: Human RBCs lyse
when mixed in vitro with sera of other
animals
1869
Braxton Hicks: NaPO4 as an
anticoagulant
20th Century
1901: Karl Landsteiner ABO Blood
Group System
1902: Anthony Decastello and Adriano
Sturli AB blood group
20th Century
Edward E. Lindemann: vein-to-vein
transfusion
Unger: syringe-valve apparatus, more
practical
1907
Richard Weil: 1st to perform ABO typing
and began compatibility testing, 1st to
suggest ABO inheritance
Refrigeration of citrated blood prior to
use
1913
Reuben Ottenberg: stressed importance
of compatibility testing
1914
Albert Hustin: sodium citrate as an
anticoagulant solution
1915
Richard Lewisohn: minimum amount of
citrate needed for anticoagulation
1916
Rous and Turner: introduction of citrate
dextrose solution for RBC preservation
1924
Felix Bernstein: proof of inheritance of
blood groups
Issues in race distribution
1927
American Association of Immunologists:
adopted the current ABO terminology
proposed by Landsteiner
1939-1940
Philip Levine (together with Stetson,
Landsteiner and Alex Wiener): 1st
discovery of Rh blood groups
1941
Charles Drew: developing techniques in
blood transfusion and blood
preservation during WWII
1943
Loutit and Mollison: acid-citrate dextrose
formula
1945
Robin Coombs, Rob Race and Arthur
Mourant: (re)discovery of anti-human
globulin (AHG) sera and antiglobulin test
which was first described by Carlo
Moreschi in 1908
1947
Rh immune Globulin for prevention of
Hemolytic Disease of the Fetus and
Newborn
1951
Edwin Cohn: development of cell
separator, paved the way for component
therapy
Carl Walter: blood collection using a
collapsible bag of polyvinyl resin
1957
Gibson: introduction of citratephosphate-dextrose (CPD)
1965
Judith Pool: concentrated factor VIII
found in the cryoprecipitate portion of
plasma
1968
Brinkhous and Shanbrom: pooling of
plasma units to produce factor VIII
concentration
Adverse effects of Transfusion
1970s
Transition to an all-volunteer blood
supply
Availability of commercial testing for
HBV
1980s
The first serologic test to detect HIV was
implemented by blood banks to protect
the blood supply
Opened the possibility of transmission of
blood-borne pathogens other than HBV,
HCV, and HIV through blood transfusion
Non-infectious effects of Transfusion
Transfused leukocytes were found to have a number
of undesirable effects
Graw and colleagues GVHD
prevention by blood component
irradiation
Greenwalt and colleagues first
generation leukocyte filter in the
prevention of febrile transfusion
reactions
Blood Banking in the Modern World
Discovery of West Nile Virus in 2002 as
a new transfusion-transmitted pathogen
Regulation of bacterial contamination on
blood components
Blood substitutes or blood alternatives
Areas of RBC Biology
1. Normal chemical composition and structure
of RBC membrane
2. Hemoglobin structure and function
3. RBC metabolism
RBC Membrane
A semipermeable lipid bilayer supported by a protein
meshlike cytoskeleton structure
1. Phospholipids arranged in bilayer structure
(40%)
2. Proteins integral and peripheral (52%)
3. Carbohydrates 8%
Deformability Factors affecting RBC deformability
1. Loss of ATP levels = decrease in spectrin
phosphorylation
2. Calcium accumulation or increase in
deposition
Permeability
RBC membrane is permeable to water and
anions (Cl- and HCO3-) but impermeable to
cations (Na+ and K+)
To maintain RBC volume and water
homeostasis, intracellular concentrations of
Na+ and K+ are controlled by utilizing ATP
RBC Metabolism
Mainly ANAEROBIC
Glycolysis breakdown of glucose to
generate energy for RBCs
1.
2.
3.
4.
Glycolytic (Embden-Meyerhof) Pathway
Pentose Phosphate Pathway
Methemoglobin Reductase Pathway
Leubering-Rapaport Pathway
Hemoglobin Structure and Function
Hemoglobin Synthesis
1. Adequate iron delivery and supply
2. Adequate synthesis of protoporphyrins
3. Adequate globin synthesis
Types in normal adults
1. HbA (two alpha, two beta chains; 92-95%)
2. HbA2 (two alpha, two delta chains; 2-3%)
3. HbF (two alpha, two gamma chains; 1-2%)
Three functions
1. Transport of O2 from the lungs to tissues
2. Transport of CO2 from tissues to the lungs
3. Buffering of blood
Hemoglobin function
Oxygen delivery to tissues
- 2-3 DPG
- Tense form lower High affinity to
oxygen
- Relaxed form higher High affinity
to oxygen
Loss of RBC viability associated with
various biochemical changes
Decrease in pH, decrease in glucose
consumption, decrease ATP levels,
buildup of lactic acid, loss of RBC
function
Anticoagulant Preservative Solutions
Name
Storage time
Acid-citrate-dextrose (ACD)
21 days
Citrate-phosphate-dextrose (CPD) 21 days
Citrate-phosphate-double dextrose 21 days
Citrate-phosphate-dextrose
-adenine (CPDA-I)
35 days
Hemoglobin-oxygen dissociation curve
Importance: It permits a considerable
amount of oxygen to be delivered to the
tissues with a small drop in oxygen
tension
Additive Solutions
Preserving solutions that are added to
the RBCs after removal of plasma
with/without platelets
Beutler development
Lovric and Hogman implementation
a. Lovric CP2D and additive solution
(saline, adenine, glucose, trisodium
citrate, citric acid, sodium
phosphate)
b. Hogman CPD and additive
solution (saline, adenine, glucose
(SAG), and later with mannitol
(SAGM)
Ligands
1. H+ ions
2. CO2
3. Organic phosphates (2,3 DPG)
Shift to the right
- Increased 2,3 DPG = decrease High
affinity to oxygen = increase oxygen
delivery to tissues
RBC Preservation
RBC viability
Measure of in-vivo RBC survival
following transfusion
75% of cells transfused should remain
viable for 24 hours
Liquid state at 1-6 degrees Celsius for a
specific number of days
RBC freezing
- For autologous units and storage of
rare blood types
- -65 C, 10 years
- Glycerol
Storage lesion
RBC Rejuvenation
Restoration of ATP and 2,3 DPG levels
PIGPA
PIPA
Rejuvesol used to salvage liquidstored RBCs that have reached outdate
S-ar putea să vă placă și
- BloodtransfusieDocument79 paginiBloodtransfusieGod RaÎncă nu există evaluări
- Chapter 1 - Blood BankDocument18 paginiChapter 1 - Blood Bankmaria clara RizalÎncă nu există evaluări
- Blood ProductDocument89 paginiBlood ProductSam0% (1)
- Chapter 1 - History of BBDocument21 paginiChapter 1 - History of BBGheri Anne OnayanÎncă nu există evaluări
- Introduction To BBDocument58 paginiIntroduction To BBRich Darlene Dela CruzÎncă nu există evaluări
- Old Blood, New Blood or Better Stored Blood?: Giancarlo Maria Liumbruno, James P. AubuchonDocument3 paginiOld Blood, New Blood or Better Stored Blood?: Giancarlo Maria Liumbruno, James P. AubuchonKatona imreÎncă nu există evaluări
- BloodbankingDocument7 paginiBloodbankingJae TÎncă nu există evaluări
- The Composition of BloodDocument40 paginiThe Composition of BloodBringle C DasÎncă nu există evaluări
- Immghy1 Prelims Notes 2Document43 paginiImmghy1 Prelims Notes 2lorraineannganuelasÎncă nu există evaluări
- RBC FunctionDocument25 paginiRBC FunctionGabriela SolanoÎncă nu există evaluări
- 2-Transfusion of Blood and Blood ProductsDocument47 pagini2-Transfusion of Blood and Blood ProductsAiden JosephatÎncă nu există evaluări
- ImmunohematologyDocument26 paginiImmunohematologyHanna MaraeÎncă nu există evaluări
- History of Blood BankingDocument4 paginiHistory of Blood BankingShaira AlcantaraÎncă nu există evaluări
- Blood Functions: Presented by Dr. Khaled Ezam PHD PhysiologyDocument34 paginiBlood Functions: Presented by Dr. Khaled Ezam PHD PhysiologyShrouk EldakroryÎncă nu există evaluări
- Microanalysis of Cardiolipin in Small Biopsies IncDocument9 paginiMicroanalysis of Cardiolipin in Small Biopsies IncSam SoeteÎncă nu există evaluări
- Blood: Jeff Tjong, PHDDocument59 paginiBlood: Jeff Tjong, PHDyat yat szeÎncă nu există evaluări
- Wilson Disease (MedScape)Document9 paginiWilson Disease (MedScape)Moileon2011Încă nu există evaluări
- Development of Recombinant Hemoglobin-Based Oxygen Carriers: Orum Eview RticleDocument15 paginiDevelopment of Recombinant Hemoglobin-Based Oxygen Carriers: Orum Eview RticleJakeusÎncă nu există evaluări
- Priming SolutionDocument38 paginiPriming SolutionShagufta IrfanÎncă nu există evaluări
- Erythrocyte Preservation: Red Blood Cell StorageDocument15 paginiErythrocyte Preservation: Red Blood Cell StorageMariela GonzalezÎncă nu există evaluări
- LSM3212 - Lecture 2-4 BloodDocument59 paginiLSM3212 - Lecture 2-4 BloodAbraham KangÎncă nu există evaluări
- MLS 306 Blood Bank Anticoagulants and Preservatives: AKINBO D.B. Lecture SeriesDocument27 paginiMLS 306 Blood Bank Anticoagulants and Preservatives: AKINBO D.B. Lecture SeriesFredÎncă nu există evaluări
- Ih M1.1 Chapt1 RevDocument16 paginiIh M1.1 Chapt1 Revさあ ああさÎncă nu există evaluări
- Components JLVDocument175 paginiComponents JLVHarry PatriceÎncă nu există evaluări
- Chapter 4 Blood Coagulation and Coagulation DisordersDocument27 paginiChapter 4 Blood Coagulation and Coagulation DisordersdaisysintszwaiÎncă nu există evaluări
- Milligan Blood SubstitutesDocument34 paginiMilligan Blood Substitutesneha100% (1)
- Artificial Blood and Blood SubstitiuteDocument34 paginiArtificial Blood and Blood SubstitiuteASHISH RANJANÎncă nu există evaluări
- Components JLVDocument176 paginiComponents JLVMayank TiwariÎncă nu există evaluări
- Blood Groups: 1 PhysiologyDocument36 paginiBlood Groups: 1 PhysiologyAkash JaatÎncă nu există evaluări
- Effects of Aged Stored Autologous Red Blood Cells On Human Plasma MetabolomeDocument13 paginiEffects of Aged Stored Autologous Red Blood Cells On Human Plasma MetabolomeRaul Rios RitterÎncă nu există evaluări
- jlrM062752 PDFDocument13 paginijlrM062752 PDFTheodora TeddyÎncă nu există evaluări
- Historical Background: William Harvey CirculationDocument9 paginiHistorical Background: William Harvey Circulationmeku mekuÎncă nu există evaluări
- Hypo Kale MiaDocument12 paginiHypo Kale MiadonloteÎncă nu există evaluări
- Lactato RevisaoDocument29 paginiLactato Revisaolucas cadeteÎncă nu există evaluări
- Chapter-6 Circulatory System: Body FluidsDocument6 paginiChapter-6 Circulatory System: Body Fluidskavitaruby1980Încă nu există evaluări
- Neutrophil Activation by Heme: Implications For Inflammatory ProcessesDocument7 paginiNeutrophil Activation by Heme: Implications For Inflammatory ProcessesraysellaÎncă nu există evaluări
- Ahuja, Motiani - 2004 - Current and Evolving Issues in Transfusion PracticeDocument8 paginiAhuja, Motiani - 2004 - Current and Evolving Issues in Transfusion Practicesushmakumari009Încă nu există evaluări
- NotesDocument24 paginiNotesSapna JainÎncă nu există evaluări
- Detection of Reactive Oxygen Species by Flow Cytometry: Alexander Christov, Ladan Hamdheydari, and Paula GrammasDocument10 paginiDetection of Reactive Oxygen Species by Flow Cytometry: Alexander Christov, Ladan Hamdheydari, and Paula GrammasTim WongÎncă nu există evaluări
- Immunohematology ASCPi Review Booklet (Part 1)Document22 paginiImmunohematology ASCPi Review Booklet (Part 1)Mark Justin OcampoÎncă nu există evaluări
- Effects of The Resuscitation Fluid and The Hemoglobin Based Oxygen Carrier (HBOC) Excipient On The Toxicity of The HBOC: Ringer's - Lactate, Ringer's Lactate, and Ringer's Ketone SolutionsDocument7 paginiEffects of The Resuscitation Fluid and The Hemoglobin Based Oxygen Carrier (HBOC) Excipient On The Toxicity of The HBOC: Ringer's - Lactate, Ringer's Lactate, and Ringer's Ketone SolutionsIstván PortörőÎncă nu există evaluări
- Blood Composition and Functions: Indian Institute of Technology PatnaDocument41 paginiBlood Composition and Functions: Indian Institute of Technology PatnaHritik KumarÎncă nu există evaluări
- Blood - Physiology Short SummaryDocument39 paginiBlood - Physiology Short SummaryParth ChaudharyÎncă nu există evaluări
- Artif Cells 23002404Document17 paginiArtif Cells 23002404István PortörőÎncă nu există evaluări
- Blood Group SerologyDocument89 paginiBlood Group SerologynelsonlaizerÎncă nu există evaluări
- Lecture 1 Cardiovascular SystemDocument70 paginiLecture 1 Cardiovascular SystemJerilee SoCute WattsÎncă nu există evaluări
- The Red Cell Storage Lesion andDocument12 paginiThe Red Cell Storage Lesion andhasanahÎncă nu există evaluări
- Histology of Blood Histology of Blood VesselsDocument6 paginiHistology of Blood Histology of Blood VesselsgerginÎncă nu există evaluări
- Physiology of The BloodDocument16 paginiPhysiology of The BlooddiytÎncă nu există evaluări
- Hess 2010Document9 paginiHess 2010Sumptuous SoulÎncă nu există evaluări
- Blood Group SerologyDocument19 paginiBlood Group Serologydr.azimikitiÎncă nu există evaluări
- Historical Perspectives: FatalDocument6 paginiHistorical Perspectives: FatalMaryÎncă nu există evaluări
- Blood Banking: By: Anie Jan K. SegoviaDocument19 paginiBlood Banking: By: Anie Jan K. SegoviaArshie08Încă nu există evaluări
- Anticoagulants Used in Blood BankDocument27 paginiAnticoagulants Used in Blood Banklovi bahunÎncă nu există evaluări
- Rheology For CliniciansDocument8 paginiRheology For CliniciansRaluca LÎncă nu există evaluări
- Ajrccm LactatemiaDocument8 paginiAjrccm LactatemiaGuamata GuamataÎncă nu există evaluări
- Hematology: AbbreviationsDocument5 paginiHematology: AbbreviationsReyven Niña DyÎncă nu există evaluări
- Leytin 2003Document7 paginiLeytin 2003francisca.torres.tmÎncă nu există evaluări
- Official Boston Celtics Bandwagon Transferral FormDocument1 paginăOfficial Boston Celtics Bandwagon Transferral FormScott Tabuena GonzalesÎncă nu există evaluări
- Gelo Man (Midterm)Document2 paginiGelo Man (Midterm)Scott Tabuena GonzalesÎncă nu există evaluări
- Official Boston Celtics Bandwagon Transferral FormDocument1 paginăOfficial Boston Celtics Bandwagon Transferral FormScott Tabuena GonzalesÎncă nu există evaluări
- RBC Indices or Wintrobe Indices: Prepared By: Francis Gerald Scott T. Gonzales, RMTDocument14 paginiRBC Indices or Wintrobe Indices: Prepared By: Francis Gerald Scott T. Gonzales, RMTScott Tabuena GonzalesÎncă nu există evaluări
- Appendix B Availability of Concentrations of Antimicrobial Agents Needed To Implement Revised CLSI Breakpoints On Commercial AST PanelsDocument1 paginăAppendix B Availability of Concentrations of Antimicrobial Agents Needed To Implement Revised CLSI Breakpoints On Commercial AST PanelsScott Tabuena GonzalesÎncă nu există evaluări
- Appendix A Brief Validation Protocol FINALDocument1 paginăAppendix A Brief Validation Protocol FINALScott Tabuena GonzalesÎncă nu există evaluări
- ChristineDocument2 paginiChristineScott Tabuena GonzalesÎncă nu există evaluări
- Circular Books Trading: Isbn Title PriceDocument1 paginăCircular Books Trading: Isbn Title PriceScott Tabuena GonzalesÎncă nu există evaluări
- "Just Stop Trying, You're Embarrassing Yourself.": Victory Is A Thousand Times Sweeter When You're The UnderdogDocument1 pagină"Just Stop Trying, You're Embarrassing Yourself.": Victory Is A Thousand Times Sweeter When You're The UnderdogScott Tabuena GonzalesÎncă nu există evaluări
- Group 4, DonatismDocument14 paginiGroup 4, DonatismScott Tabuena GonzalesÎncă nu există evaluări
- Asia Pacific Cosmetics PhilsDocument1 paginăAsia Pacific Cosmetics PhilsScott Tabuena GonzalesÎncă nu există evaluări
- GONZALES, Coxsackie VirusDocument3 paginiGONZALES, Coxsackie VirusScott Tabuena GonzalesÎncă nu există evaluări
- Uric Acid SynthesisDocument1 paginăUric Acid SynthesisScott Tabuena GonzalesÎncă nu există evaluări
- Osteoarthritis DissertationDocument8 paginiOsteoarthritis DissertationPaperHelpJackson100% (1)
- Types of Business OwnershipDocument2 paginiTypes of Business Ownershipprelovedseller bnÎncă nu există evaluări
- Compositional Changes of Crude Oil SARA Fractions Due To Biodegradation and Adsorption Supported On Colloidal Support Such As Clay Susing IatroscanDocument13 paginiCompositional Changes of Crude Oil SARA Fractions Due To Biodegradation and Adsorption Supported On Colloidal Support Such As Clay Susing IatroscanNatalia KovalovaÎncă nu există evaluări
- Steen Kamp 2021Document16 paginiSteen Kamp 2021LARANSA SOLUNA GOGO SIMATUPANGÎncă nu există evaluări
- The Modern Fire Attack - Phil Jose and Dennis LegearDocument7 paginiThe Modern Fire Attack - Phil Jose and Dennis LegearTomÎncă nu există evaluări
- Shloka Seminar: - DR Vikas SarochDocument15 paginiShloka Seminar: - DR Vikas SarochDrVikas100% (3)
- Cwts ThesisDocument7 paginiCwts Thesisbufukegojaf2100% (2)
- Technical Reference For Water Conservation in Cooling TowersDocument41 paginiTechnical Reference For Water Conservation in Cooling TowersDorn GalamarÎncă nu există evaluări
- School Administration and Supervision MAED 605Document24 paginiSchool Administration and Supervision MAED 605Jaynie Ann TapdasanÎncă nu există evaluări
- From Crème Fraîche To Sour Cream: What's The Difference?Document14 paginiFrom Crème Fraîche To Sour Cream: What's The Difference?Maricel BautistaÎncă nu există evaluări
- A Novel Procedure For Transient CFD Modeling of Basin Solar Stills, Coupling of Species and Energy EquationsDocument16 paginiA Novel Procedure For Transient CFD Modeling of Basin Solar Stills, Coupling of Species and Energy EquationsAverroesÎncă nu există evaluări
- Cen-Tech 63759Document8 paginiCen-Tech 63759GregÎncă nu există evaluări
- Critique PaperDocument1 paginăCritique PapernicolealerÎncă nu există evaluări
- Shelf Life ControlDocument7 paginiShelf Life ControlRushikesh Deshpande100% (1)
- Fan Adta-En-50hz-March-2018 - 20180315Document52 paginiFan Adta-En-50hz-March-2018 - 20180315Andi JatmikoÎncă nu există evaluări
- Atomic Structure Worksheet: Name PeriodDocument4 paginiAtomic Structure Worksheet: Name Periodapi-496534295100% (1)
- Manual GISDocument36 paginiManual GISDanil Pangestu ChandraÎncă nu există evaluări
- JAMB Biology Past Questions 1983 - 2004Document55 paginiJAMB Biology Past Questions 1983 - 2004Keith MooreÎncă nu există evaluări
- Absenteeism in Public Sector: Presented byDocument25 paginiAbsenteeism in Public Sector: Presented byPravin Rathod50% (2)
- 50-Article Text-116-1-10-20191113Document6 pagini50-Article Text-116-1-10-20191113Annisa FauziahÎncă nu există evaluări
- Lithium Battery Handling RegulationDocument11 paginiLithium Battery Handling RegulationFan Man ChungÎncă nu există evaluări
- People v. Jerry BugnaDocument1 paginăPeople v. Jerry BugnaRey Malvin SG PallominaÎncă nu există evaluări
- ChartDocument27 paginiChartFlorijan ŠafarÎncă nu există evaluări
- Trophic Levels - 10% RuleDocument5 paginiTrophic Levels - 10% RulerebbiegÎncă nu există evaluări
- Peoria County Booking Sheet 03/01/15Document8 paginiPeoria County Booking Sheet 03/01/15Journal Star police documentsÎncă nu există evaluări
- iGCSE Biology Section 1 Lesson 1Document44 paginiiGCSE Biology Section 1 Lesson 1aastha dograÎncă nu există evaluări
- Vendor Security ChecklistDocument11 paginiVendor Security ChecklistHarisÎncă nu există evaluări
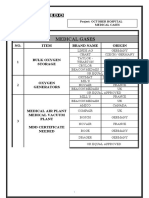
- Medical Gases: NO. Item Brand Name OriginDocument4 paginiMedical Gases: NO. Item Brand Name OriginMahmoud AnwerÎncă nu există evaluări
- Publication PDFDocument152 paginiPublication PDFAlicia Mary PicconeÎncă nu există evaluări
- Testing of Semifinished Products of Thermoplastics Bases - Indications Directive DVS 2201-1Document4 paginiTesting of Semifinished Products of Thermoplastics Bases - Indications Directive DVS 2201-1OscarÎncă nu există evaluări