Documente Academic
Documente Profesional
Documente Cultură
2011 Gauge Amulree
Încărcat de
Agustina Anggraeni PurnomoDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
2011 Gauge Amulree
Încărcat de
Agustina Anggraeni PurnomoDrepturi de autor:
Formate disponibile
BGS Amulree Essay Prize
Long Term Post-Operative Cognitive
Dysfunction;
A 12 month longitudinal cohort study of elderly noncardiac patients.
Nathan Gauge1
Abstract
Post-operative cognitive dysfunction (POCD) in elderly non-cardiac patients has recently been
identified as a significant risk factor for increased mortality, welfare dependence and premature
withdrawal from work over a follow up of 8.5 years. The single most important risk factor for the
development of POCD is advancing age. In the UK population ageing, coupled with an increase in the
age of patients undergoing surgery will make POCD and increasingly important condition.
Despite the significant long term impact of POCD, previous studies in the elderly have failed to
identify significant levels of POCD at one year post operatively. This essay will present the first
longitudinal cohort study to demonstrate a significantly greater level of global cognitive impairment
in surgical patients compared to controls 1 year post-operatively. The discussion will identify why
previous trials have failed to show a significant level of POCD at 1 year post operatively and has
substantial implications for future research into reducing the impact of POCD.
Nathan Gauge is a KCL final year medical student
He was involved in all aspects of the study including design, data collection and was solely responsible for the
statistical analysis and authorship of this essay. This work has been submitted for the Amulree prize with the
permission of the other authors involved in the study.
BGS Amulree Essay Prize
Epidemiology of POCD
POCD has been identified in medical literature for over 50 years[4] when Bedford noted that "Hes
never been the same since his operation" is often heard in geriatric practice and conducted a
retrospective study identifying POCD for the first time. Despite this it took a further 40 years before
the landmark study into non-cardiac POCD was conducted by the ISPOCD study group - published in
1998 demonstrating that amongst major non-cardiac surgical patients greater than 60 years old POCD
was present in 25.8% of patients at one week and 9.9% at 3 months post operatively [31].
It is important to distinguish POCD from postoperative delirium which is a temporary change in
mental status characterized by a reduced awareness of the environment and a disturbance in attention
occurring shortly after surgery[13]. Post operative delirium is associated with delayed recovery and
increased mortality[30]. POCD in contrast is a more persistent condition identified by
neuropsychological testing which demonstrate a decline in cognitive function without an alteration in
mental status or awareness[13].
Estimates of the prevalence of POCD have varied widely from no reported change up to 71% of
patients showing POCD between one week and 6 months after surgery[34]. There are two principle
reasons for the wide range of incidence; firstly variation in type of surgery and anaesthesia and
secondly variation in the definition of POCD itself. The problem of defining POCD has been
addressed by several authors [28, 34, 40] and a consensus has yet to be reached. There are several
barriers to establishing a definition of POCD.
1. POCD is currently defined on the basis of a randomly assigned statistical cut off point.
Different authors have a variety of opinions on where this cut off point should be placed.
Important consideration needs to be given to previously established definitions of cognitive
decline in the elderly and both the clinical and personal impact of any given level of decline.
2. POCD is a binary definition of cognitive decline. It is plausible that POCD is present to a
greater or lesser extent in the majority of patients and therefore represents a continuum of
cognitive dysfunction. Reduction of the continuous data produced by neuropsychological tests
to binary data may therefore be inappropriate.
3. There is little data on whether different areas of cognition are preferentially affected in
POCD. Neuropsychological testing allows isolation of several areas of cognitive function.
Authors disagree on the number and type of tests as well as which cognitive aspects should be
focussed on.
The approach taken in this study is based on evidence that individual cognitive domains have different
effects on patients activities of daily living and capacity to function independently. Price et al.
demonstrated that POCD patients suffering from executive function deficits either alone or in
combination with memory deficits have the greatest functional impairment[36]. Previous studies have
demonstrated that deficits in attentional function have a particularly significant impact on patients
activities of daily living[8].
Computerised neuropsychometric testing and in particular the Cognitive Drug Research (CDR)
computerised assessment system has been shown to reduce the learning effect caused by repeated
assessments used in the study of POCD[47]. For these reasons we have employed a computerised test
2
BGS Amulree Essay Prize
Nathan Gauge
battery which focuses on attention and executive function. We have followed the ISPOCD study
group Z score method for calculating global cognitive decline as well as including analysis of
individual neuropsychometric tests.
BGS Amulree Essay Prize
Nathan Gauge
Impact of POCD
POCD has been shown to have severe long-term consequences for patients including increased
mortality in both the short term - between three months and one year post operatively [32] - and longterm with one study demonstrating an increased mortality over a median follow-up of 8.5 years post
operatively[44]. POCD has also been associated with increased duration of hospital stay[32],
premature withdrawal from the labour market and increased duration of welfare payments[44].
Following cardiac surgery Newman et al. have shown that cognitive decline is significantly associated
with significantly reduced quality of life and a less productive working status [33].
Despite the long-term implications of POCD both for the patient and the health service very few
studies have assessed POCD one year post operatively. A literature search of the Medline database2
identified only six papers that assessed POCD over six months post operatively and incorporated a
control group for comparison [1, 3, 5, 19, 20, 22]. The papers are summarised in table 3 in the
appendix. Only one paper found a significant difference in cognitive function between patients and
controls. Ancelin et al. identified a decline in cognitive function in visuo-spacial tests whilst also
noting a simultaneous improvement in patients compared to controls in the language tests[3]. This
study failed to control for the learning effect caused by repeated psychometric testing of patients and
did not include a measure of global decline.
The failure of previous trials to identify a significant difference in global cognitive decline between
patients and controls may represent either 1) evidence that POCD is a temporary impairment that
resolves completely within one year or 2) previous trials have failed to use a sufficiently sensitive
neuropsychological test battery to detect long-term changes in cognitive function without succumbing
to the difficulties of either the ceiling effect or the learning effect. The epidemiological evidence
demonstrating long-term health and welfare consequences to POCD suggest that there are lingering
cognitive deficits that have remained undetected.
Whilst POCD is believed to be a condition that is at least in some patients - reversible many authors
have considered a link between POCD and the development of dementia in later life. The difference
in definitions between POCD and measures of early dementia such as Mild Cognitive Impairment
(MCI) and Age Associated Cognitive Decline (AACG) is only the presence of a surgical history. MCI
and AACD have been used extensively throughout the psychiatric literature and are well documented
as predictors of future dementia including Alzheimers disease amongst elderly patients [27].
Xie and Tanzi [50] have argued that there is some experimental evidence to support a link between
general anaesthesia, surgery and permanent cognitive damage. They point to studies that show
ischemic brain injury is associated with the development of dementia, and - at least in experimental
2
The literature search was based on the systematic review by Newman et al.[34] Updated using the same search
terms to cover the period 2005 to 2010.
BGS Amulree Essay Prize
Nathan Gauge
models - exposure to anaesthetic substances including isoflurane and propofol has induced neuronal
cell death and altered the formation of A peptides associated with Alzheimers disease. However,
case-control studies linking Alzheimers disease with exposure to general anaesthetic, although
limited by design, have been inconclusive [6, 7]. Further research is clearly needed before a link can
be satisfactorily established.
BGS Amulree Essay Prize
Aetiology, Pathogenesis and Prevention
Several studies have identified risk factors associated with POCD. As with many diseases age is the
strongest predictor of POCD risk. In the ISPOCD1 study at three months POCD was found in 7% of
patients aged 60-69 and in 14% of patients over 69. In addition; duration of anaesthesia, respiratory
complications, infection and further operations were found to be independent risk factors for POCD
[31]. A connection has also been found between lower levels of education, depression and POCD [2].
It is suggested that these risk factors are explained by deficiencies in the test as individuals with high
level of intelligence are able to compensate for some levels of cognitive decline with their so called
cognitive reserve [16] and it is well recognised that depression can lead to a reduction in
neuropsychological test scores[42]. POCD has been associated with lower alcohol consumption in
middle aged patients thought to be a result of increased sensitivity to CNS active substances [25].
Conversely in male cardiac surgical patients a history of alcohol dependence has been associated with
increased cognitive decline [24].
A plethora of theories explaining the underlying pathogenesis of POCD have been put forward but
none have yet been satisfactorily proven. It is useful when considering an area where there are so
many possible mechanisms to construct a simple set of categories from which to explore potential
mechanisms. Assuming that POCD is genuine and is caused by part of the process of surgery there are
at least three major areas that should be considered:
Potential
Causes of
POCD
Surgical
Insult
Fat
microem boli
System ic
Inflammation
Blood loss
and anaem ia
General
Anaesthesia
Cerebral
Oxygen
Desaturation
Direct
Neurotoxicity
Cerebral and
System ic
Effects
Postoperative
Recovery
Medication
Infection
BGS Amulree Essay Prize
Nathan Gauge
Surgical Insult
The potential for microemboli to cause cognitive decline has been explored previously [15, 26]. Koch
et al. used transcranial Doppler to assess the number of microemboli in either of the middle cerebral
arteries during hip or knee replacements. Whilst microemboli were detected in both patients with and
without a venous-arterial shunt the authors were unable to correlate the number of emboli detected
with POCD. It is worth noting however that this study may have been underpowered to detect an
effect involving just 22 patients and size as well as number of emboli may play an important role.
The possibility of systemic inflammation causing POCD in cardiac surgery has been explored by
randomising the use of intra-venous ketamine during anaesthetic induction. The authors found a
significant improvement in the intervention arm in one specific cognitive domain and a significant
reduction in the levels of C-Reactive Protein postoperatively[23]. Experimentally the exposure of rats
to anaesthesia and splenectomy resulted in increased levels of CNS inflammation and cognitive
impairment [46] interestingly in rats exposed only to anaesthesia no cognitive deficit was found.
Cerebral oxygen de-saturation has been a significant area of study in cardiac and carotid artery
surgery and has been correlated with POCD[11, 43]. In non-cardiac surgery it is a more complex
picture. Significant cerebral oxygen desaturation only occurs in a minority of patients during noncardiac surgery [11], but amongst these individuals preliminary evidence indicates that monitoring to
enable intervention improves outcome [10]. Cerebral oxygen de-saturation has been shown to be
significantly correlated with blood loss in abdominal patients and a percentage fall in haemoglobin
[21]. Treatment of anaemia and vitamin B12 deficiency in patients with cognitive impairment has
been shown to significantly improve cognition [14] postoperative anaemia represents a plausible
cause of POCD.
General Anaesthetics on CNS
The possibility of General Anaesthetic (GA) agents causing long term cognitive impairment is a
controversial one and provokes strong responses amongst anaesthetists. Neurotoxicity of general
anaesthetics has been investigated both in the laboratory and the clinical context.
In a recent review article [35] considered the laboratory evidence for neurotoxicity of general
anaesthetics. In some animal models a paradoxical improvement in memory has been shown amongst
rats exposed to GA however refinement of the model showed a consistent impairment in learning
for 2-3 weeks following exposure [12]. Experiments on cells in vitro have exposed some potential
pathways for neurotoxicity of GA agents notably in the oligomerisation of A peptides linked with
Alzheimers disease [49]. The applicability of the laboratory work to clinical practice is not yet clear.
BGS Amulree Essay Prize
Nathan Gauge
Clinical assessment of the impact of GA on neurotoxicity has been addressed by studies comparing
regional anaesthesia (RA) with GA. A number of trials have looked at this with the majority finding
no significant difference between the two suggesting that GA plays only a small role in POCD,
however, methodological limitations complicates their results [38]. It is worth noting that the largest
study so far found when using per protocol analysis that there was a significant reduction in
POCD amongst patients with RA (12.7%) compared to patients receiving GA (21.2%) at one week
postoperatively [39]. Evidence from these trials is therefore still somewhat inconclusive.
An alternative assessment of the impact of GA can be achieved through the monitoring of the depth of
anaesthesia. However, this method is likely to pick up additional systemic effects of sedation as well
as any direct neurotoxicity from GA. Depth of anaesthesia monitoring using electroencephalography
has been attempted in four papers.
Three randomised control trials were reported [17, 18, 48]. Gaba et al. have not reported full analysis
of their data, however, they found no correlation between BiS values and postoperative delirium.
Wong et al randomised patients to either titration of isoflurane to Bispectral Index Scores (BiS) of 5060 or standard treatment. In the intervention group they showed a 30% reduction in use of isoflurane
(p <0.05), a reduction in time to orientation (p < 0.01) and no difference in POCD. However the
analysis of POCD was done without reference to baseline values and by repeating the
neuropsychological tests 7 times within the first 72 hours postoperatively[18]. Without a control
group for learning effect and conducting all psychometric tests within 3 days postoperatively these
results are more applicable to postoperative delirium than POCD.
Farag et al randomised patients to two different anaesthetic depths and found a significant reduction in
cognitive decline in the group randomised to deeper levels of anaesthesia (p = 0.006) in one of their
three neuropsychological tests the processing speed index at 4-6 weeks postoperatively.
Unfortunately the two anaesthetic depths were similar and both overlapped with the ideal level of
sedation (a BiS score of between 40-60 [37]). It has also been noted that there was poor compliance
with the target BiS values patients in the low BiS group were within or below the range only 54% of
the time and in the high BiS group were within or above the range for only 57% of the time[45].
Steinmetz et al. conducted an excellent correlation study using intraoperative cerebral state index
(CSI) a very similar measure to BiS - with POCD. They found no statistical difference in mean CSI,
deep hypnotic time (CSI<40) and light hypnotic time (CSI>60) between patients with POCD and
those without at 1 week postoperatively. They also found no significant correlation between the Z
scores for the 7 neuropsychological tests and mean CSI [45].
Given the mixed results found using depth of anaesthesia monitoring and issues with study design
further research is urgently needed. Any role for GA in the development of POCD is far from clear.
BGS Amulree Essay Prize
Nathan Gauge
Postoperative Recovery
A number of routine postoperative medications are known to have significant effects on patients
cognitive response especially in attention and reaction speed tasks. This effect has been monitored
only sporadically in POCD studies and has been found to be significant in some trials (see for
example opioid medication in [45]. However, a study addressing the effect of benzodiazepines in
elderly patients found no significant relationship between blood concentrations of the drug and POCD
[41]. Despite this finding the use of neurologically active drugs in studies of POCD is a potentially
important confounder. Postoperative complications including infection and respiratory difficulties
have been shown to be associated with increased risk of POCD [31]. Careful consideration of these
potential confounders is therefore essential.
Prevention
No modifiable cause of POCD in non cardiac surgery has yet been identified[38]. Several trials have
considered possible mechanisms (reviewed in (Newman et al., 2007). These include normotensive and
hypotensive anaesthesia, intravenous versus inhalation Anaesthesia, pulse oximetry monitoring,
hypocapnia and vitamin supplementation. None have found significant effects with respect to
POCD[34].
As identified previously, several trials in cardiac surgery have shown some promise in preventing
POCD[23, 43]. In non-cardiac surgery to date only one trial has shown a reduction in a sub test of
POCD[17]. This trial has been heavily criticised in the literature[45] and the results therefore need
cautious interpretation.
BGS Amulree Essay Prize
Nathan Gauge
Methods
The study protocol was approved by the local research ethics committees and all patients gave written
informed consent. Patients were taken from two UK regional teaching hospitals and were matched
based on age, gender and baseline mini mental state exam (MMSE) to control subjects taken from the
local regions. The full selection protocol for surgical patients has been published previously [29].
Patients were included if they were scheduled to undertake elective major abdominal or orthopaedic
surgery under general anaesthesia at either centre. Exclusion criteria included age under 60 years,
inability to complete or unwillingness to comply with any of the protocol or procedures and preexisting dementia (defined as a MMSE score of 23 or less).
Assessments
Patients were assessed using a combination of the MMSE and the standard computerised drug
research (CDR) battery. Assessments were carried out at baseline (preoperatively for surgical
patients) and as a minimum at 12 months following the baseline assessment.
In line with previous studies cognitive decline was classified at three levels; mild, moderate and
severe[36]. These levels correspond to measures commonly used to describe cognitive decline in
elderly subjects, specifically; age associated cognitive decline (AACD), mild cognitive impairment
(MCI) and post-operative cognitive dysfunction (POCD). The scores were calculated using the
ISPOCD Z score method described previously [31]. The change for individual subjects from baseline
was calculated and the control group was used to remove any learning effect and to provide the values
for standard deviation. The following seven cognitive tests were used; MMSE, simple reaction time,
digit vigilance accuracy, digit vigilance reaction time mean, choice reaction time accuracy, choice
reaction time mean and cognitive reaction time mean. The level of cognitive decline was defined as
follows;
Mild (AACD) = greater than 1 SD decline in at least one of the seven cognitive domains.
Moderate (MCI) = greater than 1.5 SD decline in at least one of the seven cognitive domains.
Severe (POCD) = greater than 1.96 SD decline in at least two of the seven cognitive domains.
Analysis
A sample size of 250 patients provides a 99% power to detect a difference of 25% between the two
groups with a 0.05 risk of type 1 error. Assuming a patient loss to follow up at one year of 25% this
requires an initial study population of 313. The 25% difference in proportions of decline was based on
the 3 month difference in mild cognitive decline reported previously from the London cohort i.
Analysis was conducted using SPSS software, version 17.0 (SPSS, Chicago, IL, USA). Significance
was determined as two-sided p values <005. No correction was made for multiple comparisons.
10
BGS Amulree Essay Prize
Nathan Gauge
Comparison of the baseline MMSE, age and gender of the control and surgical groups was made
using the 2 test, Students t test and MannWhitney U test as appropriate. The Kolmogorov-Smirnov
test was used to establish deviation from a normal distribution.
The primary outcome measure was predetermined as the difference in the prevalence of mild,
moderate and severe cognitive decline between surgical patients and controls assessed using the 2
test. Continuous analysis was also conducted on the individual cognitive domains using Students t
test, the MannWhitney U test as appropriate.
11
BGS Amulree Essay Prize
Nathan Gauge
Results
Cohort Analysis
Population Characteristics
330 subjects were assessed at baseline including 192 surgical patients and 138 controls. The baseline
characteristics are reported in table 1. There was no significant difference in Age (p = 0.498), baseline
MMSE (p= 0.252) or Gender (p = 0.563) between the two groups.
Age
MMSE
Male
Gender
Table 1
Group
Number
patient
control
patient
control
patient
control
192
138
192
138
192
138
Median (IQR) /
percentage
75 (9)
76 (7)
28 (2)
28 (2)
40%
37%
Test
Asymp. Sig. (2tailed)
M-W
0.498
M-W
0.252
0.563
A total of 256 (78%) subjects completed all of the 1 year assessments. There were no significant
differences with respect to Age (p = 0.910), baseline MMSE (p = 0.313) or Gender (p= 0.372)
between subjects who completed the 1 year assessment and those who did not.
Global Decline
At one year post operatively there was a significant difference between patients and controls in all
three levels of cognitive decline. Mild POCD was found in 76% of surgical patients compared to
50.4% of nonsurgical controls (Pearson 2 p = <0.001). Moderate POCD was found in 48% of
surgical patients compared to 27.5% of nonsurgical controls (Pearson 2 p = 0.001). Severe POCD
was identified in 11.2% of surgical patients compared to just 3.8% of nonsurgical controls (Pearson 2
p = 0.024). These results are displayed in figure 1.
Percentage of Subjects with POCD at 1 year
p = <0.001
p = <0.001
80.0%
70.0%
p = 0.001
60.0%
50.0%
surgical patient
40.0%
control
30.0%
p = 0.024
20.0%
10.0%
.0%
Mild
Moderate
Severe
Figure 1
12
BGS Amulree Essay Prize
Nathan Gauge
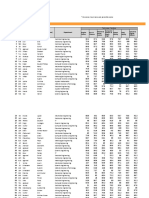
Individual Domains
Significant differences were found between surgical patients and controls with respect to simple
reaction times - median(IQR) 25.57(73.80) v 9.52(49.75) p = 0.025, cognitive reaction times median(IQR) -25.69(120.96) v -3.42(65.35)p = 0.006 and digit vigilance mean accuracy (median
(IQR) 0.00 (4.44) v 0.00 (0.00) p = 0.05). The full results of the continuous analysis are presented in
table 2.
Z
Asymp. Sig. (2tailed)
MMSE
-1.790
.073
Simple Reaction Time Mean
-2.243
.025
Digit Vigilance Mean
Accuracy
-1.940
.052
Digit Vigilance Reaction
Time Mean
-.504
.614
Choice Reaction Time Mean
Accuracy
-.896
.370
Choice Reaction Time Mean
-1.220
.223
Cognitive Reaction Time
Mean
-2.744
.006
Table 2
13
Surgical patient /
control
Median (IQR)
surgical
control
surgical
control
surgical
control
surgical
control
surgical
control
surgical
control
surgical
0.00 (2.00)
0.00 (2.00)
25.57 (73.80)
9.52 (49.75)
0.00 (4.44)
0.00 (0.00)
9.25 (59.26)
13.47 (29.80)
0.00 (3.34)
0.00 (3.33)
-5.81 (81.61)
-10.78 (57.70)
-25.69 (120.96)
control
-3.42 (65.35)
BGS Amulree Essay Prize
Nathan Gauge
Discussion
This is the first longitudinal cohort study of POCD to demonstrate a significant difference in the level
of global cognitive decline between surgical patients and controls at 12 months post operatively. It
identifies attentional and executive function as particularly sensitive neurocognitive domains in
POCD.
It is important to address the reasons why our trial has successfully identified significant differences
in the level of cognitive decline where previous trials have not. I have highlighted three possible
mechanisms for this:
The reduction of ceiling and learning effects using the CDR system
The use of multiple levels of POCD
The focus on attention and executive function
Our emphasis on computerised neuropsychometric analysis and reaction speeds substantially reduces
the learning effect observed with many other studies[47]. It is worth noting that the only other 12
month trial to demonstrate any difference between surgical patients and controls also employed a
computerised test battery[3]. Previous studies into POCD including the work of the ISPOCD study
group is substantially hampered by learning effect. Despite attempts to account for the effect using a
control group this analysis method exposes trials to 2 primary flaws.
Firstly the trial is not truly assessing cognitive decline but rather a failure to recall the
neuropsychometric tests and to demonstrate cognitive improvement. It has been previously noted that
memory function appears less significant in POCD than executive function and has a lower impact on
patients functional impairment[36].
Secondly the fixed and invariable nature of paper-based neuropsychometric tests exposes them to a
potential retest ceiling effect. This is distinct from an initial ceiling effect which will tend to
overestimate the levels of POCD[9]. Instead during repeated retesting over a short time period
subjects can achieve extremely high scores from which further improvement becomes exponentially
difficult. The normal subjects reach the test ceiling early and subsequent retesting provides impaired
subjects an opportunity to catch up. POCD
studies focusing on differences in the learning
effect will therefore tend to produce a gradual
convergence in test scores between impaired and
non-impaired subjects despite continued
cognitive deficits within the impaired group
demonstrated graphically in figure 2.
This pattern has been observed in previous
studies of POCD and has been presented as a
reduction in the level of cognitive dysfunction
with time [31]. The retest ceiling effect is
substantially reduced, though not completely
eliminated, with the CDR system employed in
our study as a result of the variability of the
Figure 2
14
BGS Amulree Essay Prize
Nathan Gauge
target, the emphasis on reaction times and the use of practice sessions prior to each test to standardise
familiarity with the tasks and equipment and has been demonstrated empirically[47].
Whilst our definition of three levels of POCD has been used previously[36] it is not widely employed
in POCD research. However, in our opinion it carries a number of advantages. Firstly it allows for the
detection of more subtle changes in cognitive function sacrificing specificity for increased
sensitivity to cognitive decline. Improving the sensitivity for decline has identified a greater
percentage difference between surgical and control populations, substantially increasing the statistical
power to detect a variation in the proportions of two populations. This method also allows for
comparison with the extensive literature on cognitive decline in the elderly with the definitions
corresponding to age associated cognitive decline and mild cognitive impairment. Finally we have
also included the classic definition of severe POCD allowing for comparison with previous literature
within this field.
Very few earlier papers assessing POCD over six months post operatively (table 4 appendix) have
incorporated measures of attention and executive function. Our emphasis on these two cognitive
domains was based on the evidence demonstrating their significance for functional impairment
associated with cognitive decline in the elderly [8, 36]. The results from this study demonstrate that
both attention and executive function are significantly affected in elderly surgical patients one year
post operatively. Given the significant impact on functional impairment caused by these specific
cognitive domains our findings may help to explain the substantial evidence demonstrating the
continued impact of POCD on patients mortality and their capacity to function within society well
beyond the 3 month cut off point previously identified[44].
As the first trial to identify significant levels of POCD a full twelve months post operatively our
findings represent an important step in bridging the gap that has emerged between the impact of
POCD on patients lives and our capacity to identify cognitive impairment beyond 3 months post
operatively. Given the recent evidence demonstrating the mortality and morbidity associated with
POCD as well as increased costs to the health service the identification of modifiable causes of POCD
is an important research challenge. This trial establishes the combination of computerised
neuropsychometric testing, a focus on attention and executive function and a multilevel approach to
scoring cognitive decline as a powerful new method for identifying the long term effects of POCD.
Our methods substantially reduce the experimental problems faced by previous trials and provide a
greater sensitivity for differences in cognitive decline with a longer duration of effect. It is our hope
that our findings will pave the way for future intervention trials.
15
BGS Amulree Essay Prize
Nathan Gauge
Appendix
Table 3
Lead
Author
Goldstein
Billig
Hall
Date
1998
1996
2005
Gilberstadt
1968
Abildstrom 2000
Ancelin
2010
follow
up
300
365
365
365 to
730
365 to
730
395
number Control
verbal
memory
of
for
and
and
attention and
subjects learning language learning concentration
108
N
x
104
N
x
122
N
63
336
270
x
x
16
visual
and
spatial
Visuomotor
numerical
executive
function
composite
screening
tools
x
x
x
Difference
None
None
None
None
x
x
None
language
visuospacial
BGS Amulree Essay Prize
Reference List
1. Abildstrom H, Rasmussen LS, Rentowl P, Hanning CD, Rasmussen H, Kristensen PA, Moller
JT. Cognitive dysfunction 1-2 years after non-cardiac surgery in the elderly. ISPOCD
group. International Study of Post-Operative Cognitive Dysfunction. Acta
Anaesthesiol Scand 2000; 44
2. Ancelin ML, de Roquefeuil G, Ledesert B, Bonnel F, Cheminal JC, Ritchie K. Exposure to
anaesthetic agents, cognitive functioning and depressive symptomatology in the
elderly. Br J Psychiatry 2001; 178
3. Ancelin ML, de RG, Scali J, Bonnel F, Adam JF, Cheminal JC, Cristol JP, Dupuy AM,
Carriere I, Ritchie K. Long-term post-operative cognitive decline in the elderly: the
effects of anesthesia type, apolipoprotein E genotype, and clinical antecedents.
J.Alzheimers.Dis. 2010; 22 Suppl 3:105-113
4. Bedford PD. Adverse cerebral effects of anaesthesia on old people. Lancet 1955; 269
5. Billig N, Stockton P, Cohen-Mansfield J. Cognitive and Affective Changes After Cataract
Surgery in an Elderly Population. American Journal of Geriatric Psych 1996; 4
6. Bohnen N, Warner MA, Kokmen E, Kurland LT. Early and midlife exposure to anesthesia
and age of onset of Alzheimer's disease. Int J Neurosci 1994; 77
7. Bohnen NI, Warner MA, Kokmen E, Beard CM, Kurland LT. Alzheimer's disease and
cumulative exposure to anesthesia: a case-control study. J Am Geriatr Soc 1994; 42
8. Bronnick K, Ehrt U, Emre M, De Deyn PP, Wesnes K, Tekin S, Aarsland D. Attentional
deficits affect activities of daily living in dementia-associated with Parkinson's
disease. J.Neurol.Neurosurg.Psychiatry 2006; 77:1136-1142
9. Browne SM, Halligan PW, Wade DT, Taggart DP. Cognitive performance after cardiac
operation: implications of regression toward the mean. J.Thorac.Cardiovasc.Surg.
1999; 117:481-485
10. Casati A, Fanelli G, Pietropaoli P, Proietti R, Tufano R, Danelli G, Fierro G, De Cosmo G,
Servillo G. Continuous monitoring of cerebral oxygen saturation in elderly patients
undergoing major abdominal surgery minimizes brain exposure to potential hypoxia.
Anesth Analg 2005; 101
11. Casati A, Spreafico E, Putzu M, Fanelli G. New technology for noninvasive brain monitoring:
continuous cerebral oximetry. Minerva Anestesiol 2006; 72
12. Culley DJ, Baxter MG, Crosby CA, Yukhananov R, Crosby G. Impaired acquisition of spatial
memory 2 weeks after isoflurane and isoflurane-nitrous oxide anesthesia in aged rats.
Anesth Analg 2004; 99
13. Deiner S, Silverstein JH. Postoperative delirium and cognitive dysfunction. Br J Anaesth
2009; 103 Suppl 1
14. Eastley R, Wilcock GK, Bucks RS. Vitamin B12 deficiency in dementia and cognitive
impairment: the effects of treatment on neuropsychological function. Int J Geriatr
Psychiatry 2000; 15
17
BGS Amulree Essay Prize
Nathan Gauge
15. Edmonds CR, Barbut D, Hager D, Sharrock NE. Intraoperative cerebral arterial embolization
during total hip arthroplasty. Anesthesiology 2000; 93
16. Elkins JS, Longstreth WT, Jr., Manolio TA, Newman AB, Bhadelia RA, Johnston SC.
Education and the cognitive decline associated with MRI-defined brain infarct.
Neurology 2006; 67
17. Farag E, Chelune GJ, Schubert A, Mascha EJ. Is depth of anesthesia, as assessed by the
Bispectral Index, related to postoperative cognitive dysfunction and recovery? Anesth
Analg 2006; 103
18. Gaba V. Correlation of the depth of anesthesia with POCD (postoperative cognitive
dysfunction). Anesth Analg 2007; 104
19. Gilberstadt H, Aberwald R, Crosbie S, Schuell H, Jimenez E. Effect of surgery on
psychological and social functioning in elderly patients. Arch.Intern.Med. 1968;
122:109-115
20. Goldstein MZ, Young BL, Fogel BS, Benedict RH. Occurrence and predictors of short-term
mental and functional changes in older adults undergoing elective surgery under
general anesthesia. Am.J.Geriatr.Psychiatry 1998; 6:42-52
21. Green DW. A retrospective study of changes in cerebral oxygenation using a cerebral
oximeter in older patients undergoing prolonged major abdominal surgery. Eur J
Anaesthesiol 2007; 24
22. Hall TA, McGwin G, Jr., Owsley C. Effect of cataract surgery on cognitive function in older
adults. J.Am.Geriatr.Soc. 2005; 53:2140-2144
23. Hudetz JA, Iqbal Z, Gandhi SD, Patterson KM, Byrne AJ, Hudetz AG, Pagel PS, Warltier
DC. Ketamine attenuates post-operative cognitive dysfunction after cardiac surgery.
Acta Anaesthesiol Scand 2009; 53
24. Hudetz JA, Patterson KM, Byrne AJ, Iqbal Z, Gandhi SD, Warltier DC, Pagel PS. A history
of alcohol dependence increases the incidence and severity of postoperative cognitive
dysfunction in cardiac surgical patients. Int J Environ Res Public Health 2009; 6
25. Johnson T, Monk T, Rasmussen LS, Abildstrom H, Houx P, Korttila K, Kuipers HM,
Hanning CD, Siersma VD, Kristensen D, Canet J, Ibanaz MT, Moller JT.
Postoperative cognitive dysfunction in middle-aged patients. Anesthesiology 2002;
96
26. Koch S, Forteza A, Lavernia C, Romano JG, Campo-Bustillo I, Campo N, Gold S. Cerebral
fat microembolism and cognitive decline after hip and knee replacement. Stroke
2007; 38
27. Levy R. Aging-associated cognitive decline. Working Party of the International
Psychogeriatric Association in collaboration with the World Health Organization. Int
Psychogeriatr 1994; 6
28. Lewis M, Maruff P, Silbert B. Statistical and conceptual issues in defining post-operative
cognitive dysfunction. Neurosci Biobehav Rev 2004; 28
18
BGS Amulree Essay Prize
Nathan Gauge
29. Lowery DP, Wesnes K, Ballard CG. Subtle attentional deficits in the absence of dementia are
associated with an increased risk of post-operative delirium. Dement Geriatr Cogn
Disord 2007; 23
30. Miller RD. Miller's anesthesia, Philadelphia, Pa. ; [Edinburgh]: Elsevier Churchill
Livingstone. 2005
31. Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, Rabbitt P, Jolles J,
Larsen K, Hanning CD, Langeron O, Johnson T, Lauven PM, Kristensen PA, Biedler
A, van Beem H, Fraidakis O, Silverstein JH, Beneken JE, Gravenstein JS. Long-term
postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD
investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet
1998; 351
32. Monk TG, Weldon BC, Garvan CW, Dede DE, van der Aa MT, Heilman KM, Gravenstein
JS. Predictors of cognitive dysfunction after major noncardiac surgery.
Anesthesiology 2008; 108
33. Newman MF, Grocott HP, Mathew JP, White WD, Landolfo K, Reves JG, Laskowitz DT,
Mark DB, Blumenthal JA. Report of the substudy assessing the impact of
neurocognitive function on quality of life 5 years after cardiac surgery. Stroke 2001;
32:2874-2881
34. Newman S, Stygall J, Hirani S, Shaefi S, Maze M. Postoperative cognitive dysfunction after
noncardiac surgery: a systematic review. Anesthesiology 2007; 106
35. Perouansky M, Hemmings HC, Jr. Neurotoxicity of general anesthetics: cause for concern?
Anesthesiology 2009; 111
36. Price CC, Garvan CW, Monk TG. Type and severity of cognitive decline in older adults after
noncardiac surgery. Anesthesiology 2008; 108:8-17
37. Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for
improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst
Rev 2007;
38. Rasmussen LS. Postoperative cognitive dysfunction: incidence and prevention. Best Pract Res
Clin Anaesthesiol 2006; 20
39. Rasmussen LS, Johnson T, Kuipers HM, Kristensen D, Siersma VD, Vila P, Jolles J,
Papaioannou A, Abildstrom H, Silverstein JH, Bonal JA, Raeder J, Nielsen IK,
Korttila K, Munoz L, Dodds C, Hanning CD, Moller JT. Does anaesthesia cause
postoperative cognitive dysfunction? A randomised study of regional versus general
anaesthesia in 438 elderly patients. Acta Anaesthesiol Scand 2003; 47
40. Rasmussen LS, Siersma VD. Postoperative cognitive dysfunction: true deterioration versus
random variation. Acta Anaesthesiol Scand 2004; 48
41. Rasmussen LS, Steentoft A, Rasmussen H, Kristensen PA, Moller JT. Benzodiazepines and
postoperative cognitive dysfunction in the elderly. ISPOCD Group. International
Study of Postoperative Cognitive Dysfunction. Br J Anaesth 1999; 83
42. Richardson MA, Satz PF, Myers HF, Miller EN, Bing EG, Fawzy FI, Maj M. Effects of
depressed mood versus clinical depression on neuropsychological test performance
19
BGS Amulree Essay Prize
Nathan Gauge
among African American men impacted by HIV/AIDS. J Clin Exp Neuropsychol
1999; 21
43. Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM3, Rodriguez AL, Magovern
CJ, Zaubler T, Freundlich K, Parr GV. Cerebral oxygen desaturation predicts
cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg
2009; 87
44. Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS. Long-term consequences of
postoperative cognitive dysfunction. Anesthesiology 2009; 110
45. Steinmetz J, Funder KS, Dahl BT, Rasmussen LS. Depth of anaesthesia and post-operative
cognitive dysfunction. Acta Anaesthesiol Scand 2009;
46. Wan Y, Xu J, Ma D, Zeng Y, Cibelli M, Maze M. Postoperative impairment of cognitive
function in rats: a possible role for cytokine-mediated inflammation in the
hippocampus. Anesthesiology 2007; 106
47. Wesnes KA. Assessing change in cognitive function in dementia: the relative utilities of the
Alzheimer's Disease Assessment Scale-Cognitive Subscale and the Cognitive Drug
Research system. Neurodegener.Dis. 2008; 5:261-263
48. Wong J, Song D, Blanshard H, Grady D, Chung F. Titration of isoflurane using BIS index
improves early recovery of elderly patients undergoing orthopedic surgeries. Can J
Anaesth 2002; 49
49. Xie Z, Dong Y, Maeda U, Moir RD, Xia W, Culley DJ, Crosby G, Tanzi RE. The inhalation
anesthetic isoflurane induces a vicious cycle of apoptosis and amyloid beta-protein
accumulation. J Neurosci 2007; 27
50. Xie Z, Tanzi RE. Alzheimer's disease and post-operative cognitive dysfunction. [Review]
[220 refs]. Experimental Gerontology 2006; 41:346-359
20
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Postoperative Cognitive Deficit After Cardiopulmonary Bypass With Preserved Cerebral Oxygenation: A Prospective Observational Pilot StudyDocument6 paginiPostoperative Cognitive Deficit After Cardiopulmonary Bypass With Preserved Cerebral Oxygenation: A Prospective Observational Pilot StudyAgustina Anggraeni PurnomoÎncă nu există evaluări
- Anesthesia & Analgesia Volume 114 Issue 2 2012 (Doi 10.1213/ane.0b013e31823b2602) Zhang, Bin Tian, Ming Zhen, Yu Yue, Yun Sherman, Janet Zhen - The Effects of Isoflurane and Desflurane On CognDocument6 paginiAnesthesia & Analgesia Volume 114 Issue 2 2012 (Doi 10.1213/ane.0b013e31823b2602) Zhang, Bin Tian, Ming Zhen, Yu Yue, Yun Sherman, Janet Zhen - The Effects of Isoflurane and Desflurane On CognAgustina Anggraeni PurnomoÎncă nu există evaluări
- 26854Document13 pagini26854Agustina Anggraeni PurnomoÎncă nu există evaluări
- Cognitive DisturbanceDocument4 paginiCognitive DisturbancedocbinÎncă nu există evaluări
- Post-Operative Cognitive Functions After General Anesthesia With Sevoflurane and Desflurane in South Asian ElderlyDocument6 paginiPost-Operative Cognitive Functions After General Anesthesia With Sevoflurane and Desflurane in South Asian ElderlyAgustina Anggraeni PurnomoÎncă nu există evaluări
- Tens Compared To Opioids in Postoperative Analgesic Therapy After Major Spinal Surgery With Regard To Cognitive FunctionDocument8 paginiTens Compared To Opioids in Postoperative Analgesic Therapy After Major Spinal Surgery With Regard To Cognitive FunctionAgustina Anggraeni PurnomoÎncă nu există evaluări
- 6Document5 pagini6Agustina Anggraeni PurnomoÎncă nu există evaluări
- Incidental Finding of Uterine Adenomyosis in A Bitch With Reproductive Disorders: A Case ReportDocument5 paginiIncidental Finding of Uterine Adenomyosis in A Bitch With Reproductive Disorders: A Case ReportAgustina Anggraeni PurnomoÎncă nu există evaluări
- JapanDocument9 paginiJapanAgustina Anggraeni PurnomoÎncă nu există evaluări
- Journal ObstetriDocument4 paginiJournal ObstetriDhiyah HarahapÎncă nu există evaluări
- 4Document11 pagini4Agustina Anggraeni PurnomoÎncă nu există evaluări
- Mrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningDocument2 paginiMrs. SH (52 YO) CC: Bleeding From The Nostril: Findings Assesment Therapy PlanningAgustina Anggraeni PurnomoÎncă nu există evaluări
- Interpreting Category II Fetal Heart Rate Tracings: Does Meconium Matter?Document8 paginiInterpreting Category II Fetal Heart Rate Tracings: Does Meconium Matter?Agustina Anggraeni PurnomoÎncă nu există evaluări
- Findings Assesment Therapy Planning: Abdominal PainDocument2 paginiFindings Assesment Therapy Planning: Abdominal PainAgustina Anggraeni PurnomoÎncă nu există evaluări
- Osteoporosis PowerpointDocument45 paginiOsteoporosis PowerpointAgustina Anggraeni Purnomo100% (1)
- Management of Stroke in Older PeopleDocument11 paginiManagement of Stroke in Older PeopleAgustina Anggraeni PurnomoÎncă nu există evaluări
- Morport 12 Juni 2014Document12 paginiMorport 12 Juni 2014Agustina Anggraeni PurnomoÎncă nu există evaluări
- Siriraj Stroke ScoreDocument2 paginiSiriraj Stroke ScoreUlil Fuad100% (4)
- Morport 8 Juni 2014Document5 paginiMorport 8 Juni 2014Agustina Anggraeni PurnomoÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Session 5 - Marketing ManagementDocument6 paginiSession 5 - Marketing ManagementJames MillsÎncă nu există evaluări
- Emergency Stop in PL E: SINUMERIK Safety IntegratedDocument10 paginiEmergency Stop in PL E: SINUMERIK Safety IntegratedVladimirAgeevÎncă nu există evaluări
- Taylor Linker ResumeDocument2 paginiTaylor Linker ResumeTaylor LinkerÎncă nu există evaluări
- Design of Power Converters For Renewable Energy Sources and Electric Vehicles ChargingDocument6 paginiDesign of Power Converters For Renewable Energy Sources and Electric Vehicles ChargingRay Aavanged IIÎncă nu există evaluări
- Welspun One Logistics Parks: Hazard Risk AssessmentDocument2 paginiWelspun One Logistics Parks: Hazard Risk AssessmentR. Ayyanuperumal AyyanuperumalÎncă nu există evaluări
- Barthes EiffelTower PDFDocument21 paginiBarthes EiffelTower PDFegr1971Încă nu există evaluări
- Chapter-12 Perf Appraisal & Career Strategy (I.m.s)Document4 paginiChapter-12 Perf Appraisal & Career Strategy (I.m.s)Waris KhanÎncă nu există evaluări
- CLOCKSDocument62 paginiCLOCKSdasarajubhavani05Încă nu există evaluări
- Types of WomanDocument16 paginiTypes of Womanveerendra75% (4)
- Project Execution PlanDocument69 paginiProject Execution PlanGraco Calle100% (6)
- Operating Temperature Considerations and Performance PDFDocument12 paginiOperating Temperature Considerations and Performance PDFccprado1Încă nu există evaluări
- Innoventure List of Short Listed CandidatesDocument69 paginiInnoventure List of Short Listed CandidatesgovindmalhotraÎncă nu există evaluări
- Unity FlowchartDocument1 paginăUnity Flowchartcippolippo123Încă nu există evaluări
- Chimney Design UnlineDocument9 paginiChimney Design Unlinemsn sastryÎncă nu există evaluări
- Curriculum VitaeDocument4 paginiCurriculum Vitaeapi-200104647Încă nu există evaluări
- Chapter I - Logic and Proofs: PropositionsDocument18 paginiChapter I - Logic and Proofs: PropositionsNênđặttênngắnTêndàiAimàmuốnđọcÎncă nu există evaluări
- Confidence Limits in StatisticsDocument30 paginiConfidence Limits in StatisticsaassmmrrÎncă nu există evaluări
- DonnetDocument12 paginiDonnetAsia SzmyłaÎncă nu există evaluări
- Upper Int U2 OnlineReviewsAndRecommendations PDFDocument2 paginiUpper Int U2 OnlineReviewsAndRecommendations PDFZsuzsa StefánÎncă nu există evaluări
- 3D CL Correction S1223RTLDocument7 pagini3D CL Correction S1223RTLakatsuki.exeÎncă nu există evaluări
- Labour WelfareDocument250 paginiLabour WelfareArundhathi AdarshÎncă nu există evaluări
- Community Service - Group 3 - Project 2Document24 paginiCommunity Service - Group 3 - Project 2rofiq wibawantoÎncă nu există evaluări
- AP HUG - Urban Developing ModelsDocument5 paginiAP HUG - Urban Developing ModelsMaria ThompsonÎncă nu există evaluări
- Finding The Right Place On The Map: Central and Eastern European Media Change in A Global PerspectiveDocument306 paginiFinding The Right Place On The Map: Central and Eastern European Media Change in A Global PerspectiveIntellect BooksÎncă nu există evaluări
- Advanced Java SlidesDocument134 paginiAdvanced Java SlidesDeepa SubramanyamÎncă nu există evaluări
- CP100 Module 2 - Getting Started With Google Cloud PlatformDocument33 paginiCP100 Module 2 - Getting Started With Google Cloud PlatformManjunath BheemappaÎncă nu există evaluări
- Organisational B.Document62 paginiOrganisational B.Viktoria MolnarÎncă nu există evaluări
- Bayan Ko Linis Ko ProgramDocument43 paginiBayan Ko Linis Ko ProgramCymagne Donna Aquino DelarosaÎncă nu există evaluări
- 2nd Announcement 13th InaSH Meeting 2019Document14 pagini2nd Announcement 13th InaSH Meeting 2019adinda permataÎncă nu există evaluări
- Flow Diagram: Equipment Identification Numbering SystemDocument24 paginiFlow Diagram: Equipment Identification Numbering Systemmkpq100% (1)