Documente Academic
Documente Profesional
Documente Cultură
Flail Chest
Încărcat de
Rora LusianaDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Flail Chest
Încărcat de
Rora LusianaDrepturi de autor:
Formate disponibile
ORIGINAL ARTICLE
Flail chest injuries: A review of outcomes and treatment practices
from the National Trauma Data Bank
Niloofar Dehghan, MD, Charles de Mestral, MD, PhD, Michael D. McKee, MD, Emil H. Schemitsch, MD,
and Avery Nathens, MD, MS, PhD, MPH, Toronto, Ontario, Canada
Flail chest injuries are associated with severe pulmonary restriction, a requirement for intubation and mechanical ventilation,
and high rates of morbidity and mortality. Our goals were to investigate the prevalence, current treatment practices, and
outcomes of ail chest injuries in polytrauma patients.
METHODS:
The National Trauma Data Bank was used for a retrospective analysis of the injury patterns, management, and clinical
outcomes associated with ail chest injuries. Patients with a ail chest injury admitted from 2007 to 2009 were included in the
analysis. Outcomes included the number of days on mechanical ventilation, days in the intensive care unit (ICU), days in the
hospital, and rates of pneumonia, sepsis, tracheostomy, chest tube placement, and death.
RESULTS:
Flail chest injury was identied in 3,467 patients; the mean age was 52.5 years, and 77% of the patients were male. Signicant
head injury was present in 15%, while 54% had lung contusions. Treatment practices included epidural catheters in 8% and
surgical xation of the chest wall in 0.7% of the patients. Mechanical ventilation was required in 59%, for a mean of 12.1 days.
ICU admission was required in 82%, for a mean of 11.7 days. Chest tubes were used in 44%, and 21% required a tracheostomy.
Complications included pneumonia in 21%, adult respiratory distress syndrome in 14%, sepsis in 7%, and death in 16%. Patients
with concurrent severe head injury had higher rates of ventilatory support and ICU stay and had worse outcomes in every category
compared with those without a head injury.
CONCLUSION:
Patients who have sustained a ail chest have signicant morbidity and mortality. More than 99% of these patients were treated
nonoperatively, and only a small proportion (8%) received aggressive pain management with epidural catheters. Given the high
rates of morbidity and mortality in patients with a ail chest injury, alternate methods of treatment including more consistent
use of epidural catheters for pain or surgical xation need to be investigated with large randomized controlled trials. (J Trauma
Acute Care Surg. 2014;76: 462Y468. Copyright * 2014 by Lippincott Williams & Wilkins)
LEVEL OF EVIDENCE: Epidemiologic/prognostic study, level IV.
KEY WORDS:
Flail chest; rib fracture; thoracic trauma; chest wall fixation.
BACKGROUND:
ib fractures are common injuries and occur in up to 39% of
patients with blunt chest trauma.1 These fractures are
routinely treated nonoperatively, and most heal without major
complications. However, a number of these injuries can result
in a mechanically unstable chest wall or ail chest, which is
associated with high rates of short-term mortality and longterm morbidity.1,2
A ail chest is dened as three or more consecutive rib
fractures, in two or more locations, creating a ail segment.3
This denition also applies to three or more bilateral consecutive rib fractures, and three or more rib fractures associated
with a sternal fracture because both of these also lead to the
creation of a mechanically unstable ail segment.4 A ail chest
can lead to chest wall instability, asynchronous movement of
the ail segment, and paradoxical chest motion. It also leads to
Submitted: July 7, 2013, Revised: November 10, 2013, Accepted: October 14, 2013.
From the Division of Orthopaedics (N.D., M.D.M., E.H.S.), Department of Surgery,
St. Michaels Hospital; Division of General Surgery (C.D.M.), Department of
Surgery, and Department of Surgery (A.N.), Sunnybrook Health Sciences
Centre, University of Toronto, Ontario, Canada.
This study was presented at the Canadian Orthopaedic Association Annual Conference 2013.
Address for reprints: Niloofar Dehghan, MD, 55 Queen St East, Suite 800, Toronto,
Ontario, Canada, M5C 1R6; email: Niloofar.Dehghan@Mail.UToronto.ca.
DOI: 10.1097/TA.0000000000000086
462
deformity of the chest wall and loss of thoracic volume.4 These
in turn lead to decreased lung volume, atelectasis, chest
tightness, dyspnea, and chronic pain.1,2,4,5
The current treatment of ail chest injuries consists of
nonsurgical management via intubation and intermittent positive pressure ventilation (internal pneumatic splint), analgesia,
pulmonary toilet, and chest physiotherapy.1,4,6 However, even
with aggressive nonoperative management, patients with severe
chest wall injuries remain at risk for many complications. A ail
chest injury causes compromised respiratory function with poor
pulmonary toilet or inability to clear secretions, which typically
requires mechanical ventilatory support. Prolonged mechanical
ventilation can in turn result in barotrauma and increases the
risk for pneumonia, sepsis, extended time in the intensive care
unit (ICU), and death.1,2,4,5,7,8 Even in the presence of extrathoracic injuries in these polytrauma patients, pneumonia and
the resultant sepsis remain two of the most common causes of
death in patients with ail chest injuries.4
A better understanding of the present-day burden of ail
chest injuries will provide useful information on the potential utility of different treatment strategies. A contemporary
description of practice patterns and in-hospital outcomes of
patients with ail chest injuries is currently lacking in the literature. This is relevant, given the increased interest in surgical
xation of selected cases. The purposes of this study were to
J Trauma Acute Care Surg
Volume 76, Number 2
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
J Trauma Acute Care Surg
Volume 76, Number 2
determine the prevalence of ail chest injuries in the trauma
patient population and to describe current treatment practices,
both nonsurgical and surgical, as well as the morbidity and
mortality of patients with these injuries.
PATIENTS AND METHODS
Study Design
We designed a retrospective cohort study of patients with
ail chest injuries identied in the National Trauma Data Bank
(NTDB), to characterize the prevalence of this injury as well
as injury patterns, current management, and in-hospital morbidity and mortality. Certain patient subgroups were compared.
The subgroups were dened based on the presence of severe
head injury or the presence of lung contusions because these
have been reported in the literature to require longer duration
of ventilatory support and have worse outcomes compared
with patients without such injuries.1,2,4,9
Data Source and Setting
The NTDB is the largest aggregation of US/Canadian
trauma registry data and was used in this study. Data from
NTDB version 10.1, years 2007 to 2009, were used.
Dehghan et al.
coding listed earlier (450264.4: ail injury with lung contusion); however, there was no denition or grading system with
regard to the extent of contusion present.
Management, Morbidity, and Mortality
We examined the duration of mechanical ventilation,
ICU stay, and total hospital stay. We also calculated the proportion of patients who received a chest tube, tracheostomy, or
epidural catheter. Procedures were captured based on ICD-9
procedure codes. The frequency of complications and mortality
were also calculated. The selected complications were obtained
from the complications eld of the NTDB and included pneumonia, adult respiratory distress syndrome (ARDS), and sepsis.
Statistical Analysis
Management and in-hospital morbidity and mortality
were compared across subgroups and dened based on the
presence or absence of severe head injury and the presence or
absence of lung contusion. W2 or Fishers exact test was used
for categorical variables, and t test or Kruskal-Wallis test was
used for continuous variables. A two-tailed > G 0.05 was
considered statistically signicant.
Cohort
The cohort included adults (Q16 years of age) sustaining
a ail chest injury following blunt trauma, treated at a Level 1
or 2 trauma center. Flail injury was identied based on the
following Abbreviated Injury Scale (AIS) diagnosis codes:
450260.3 (ail injuryVunilateral or not further specied),
450262.3 (ail injury without lung contusion), 450264.4 (ail
injury with lung contusion), and 450266.5 (bilateral ail injury).
At the patient level, patients who were dead on arrival or
died in the emergency department were excluded owing to
limited opportunity for injury ascertainment or intervention.
At the center level, facilities with the following criteria were
included for analysis: trauma center Level 1 or 2, facilities with
90% or more of patients having at least one AIS code, facilities
coding for a minimum of 100 patients, those that code complications, and facilities that code at least one exploratory
laparotomy. We wished to exclude centers that did not consistently code procedures. We therefore identied and excluded
centers where no patient underwent either of the two most
commonly coded operative procedures in NTDB, namely, open
reduction and internal xation of the femur and open reduction
and internal xation of the tibia (ICD-9 procedure codes 79.35
and 79.36). To derive more valid estimates of in-hospital complications, we also excluded centers unlikely to accurately code
complications. In doing so, we excluded centers that did not
code at least one pneumonia or urinary tract infection during the
3-year study period.
Patient Characteristics
The patient characteristics examined included age, sex,
the presence of an associated severe head injury, and the
presence of a lung contusion. A severe head injury was dened
as a head injury with AIS score of 3 or greater and a motor
Glasgow Coma Scale (GCS) score of 4 or less. The presence of
a lung contusion was identied based on the AIS diagnosis
RESULTS
We identied 354,945 patients with an Injury Severity
Score (ISS) of 9 or greater following blunt trauma treated
at 199 Level 1 and 2 trauma centers (representing 980% of
trauma centers for that period). Of these patients, 3,467 (1%)
experienced a documented ail chest injury. The following
data pertain to the 3,467 patients identied with a ail chest
diagnosis.
Entire Cohort
The average age at the time of injury was 52.5 years,
with 77% male and 23% female patients. The mean ISS was
30.4, and the most common mechanism of injury was motor
vehicle collision (79%). Other causes included fall (16%) and
other blunt injury (5%). A severe head injury was present in
15% of patients, while 54% had documented lung contusions.
Overall, intubation and mechanical ventilation were required in 59% (1762/2984, data unavailable for 483 patients),
for a mean of 7.2 days overall (SD 11, median 1, interquartile
range (IQR) 0Y12). The mean duration of mechanical ventilation was 12.1 days for the 59% who required intubation and
mechanical ventilation (SD 12, median 9, IQR 3Y18). ICU
admission was required in 82% of patients (2767/3377, data
unavailable for 90 patients), for a mean of 9.6 days overall
(median 5, SD 12, IQR 1Y15). The mean length of ICU stay
was 11.7 days for the 82% who required ICU admission (SD
12, median 8, IQR 3Y17). Mean length of hospital stay overall
was 16.6 days (SD 16, median 12, IQR 6Y22) (Figs. 1, 2).
Chest tubes were used in 44% (1,542 of 3,467), and 21%
(714 of 3,467) of the patients required a tracheostomy. Inhospital complications included pneumonia in 21% (713 of
3,467), ARDS in 14% (480 of 3,467), sepsis in 7% (255
of 3,467), and death in 16% (544 of 3,467) of the population
(Fig. 1). Epidural catheters were used in 8% (263 of 3,467) of
* 2013 Lippincott Williams & Wilkins
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
463
J Trauma Acute Care Surg
Volume 76, Number 2
Dehghan et al.
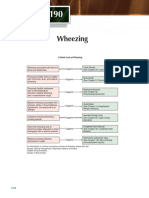
Figure 1. Outcomes, morbidity and mortality for 3,467 patients identied with ail chest injury.
the patients, and surgical xation of the chest wall was performed in only 0.7% (24 of 3,467) of the patients.
Patients With Severe Head Injury
Severe head injury (dened as head AIS score Q 3 and a
motor GCS score e 4) was present in 15% (523 of 3,467) of
the patients. When comparing the outcomes of patients with
severe head injury with those without a documented severe
head injury, there were statistically signicant higher rates of
complications and poor outcomes in all categories.
Compared with those without a severe head injury, patients with a severe head injury had statistically signicant
increase in rates of need for mechanical ventilation (88% vs.
54%, p G 0.00001) and ICU stay (89% vs. 81%, p G 0.00001).
They also had more days on a mechanical ventilator (11.2 vs.
6.5, p G 0.001), more days in the ICU (13.4 vs. 8.9, p G 0.001),
and more days in the hospital (21.4 vs. 15.8, p G 0.0005).
(Fig. 2, Tables 1 and 2)
With regard to other outcomes, patients with a severe
head injury compared with those without severe head injury also
had higher rates of chest tube use (51% vs. 43%, p G 0.001),
tracheostomy (34% vs. 18%, p G 0.0001), pneumonia (31% vs.
19%, p G 0.0001), ARDS (17% vs. 13%, p G 0.016), sepsis (11% vs.
7%, p G 0.001), and death (40% vs. 11%, p G 0.0001) (Fig. 3).
These patients were also less likely to receive an epidural
catheter for pain management (1% vs. 9%, p G 0.0001), while
there was no difference between rates of surgical xation between the two groups (Fig. 3, Table 1).
Figure 2. Number of days on mechanical ventilation, ICU stay, total hospital stayVbased on injury pattern.
464
* 2013 Lippincott Williams & Wilkins
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
J Trauma Acute Care Surg
Volume 76, Number 2
Dehghan et al.
TABLE 1. Complications and Outcomes for Patients with Flail Chest Injury - Based on Injury Pattern
No Severe
Head Injury
All patients
With Severe
Head Injury
No Pulmonary
Contusion
With Pulmonary
Contusion
Outcomes
Percentage
Percentage
Percentage
Percentage
Percentage
No. patients
Mechanical ventilation
ICU admission
Chest tube
Tracheostomy
Pneumonia
ARDS
Sepsis
Death
Epidural use
Open reduction and
internal xation
chest wall
100
59
82
44.5
20.6
20.6
13.8
7.4
15.7
7.6
0.7
3,467
1,762
2,767
1,542
714
713
480
255
544
263
24
85
54
81
43.3
18.2
18.8
13.2
6.7
11.4
8.7
0.6
2,944
1,369
2,306
1,276
535
553
390
198
337
257
18
15
88
89
50.9
34.2
30.6
17.2
10.9
39.6
1.1
1.1
523
393
461
266
179
160
90
57
207
6
6
0.00001*
0.00001*
0.0014*
0.0001*
0.0001*
0.0156*
0.0008*
0.0001*
0.0001*
0.17
46
56
80
41.8
20.9
18.7
13.1
6.8
16.1
6.7
0.4
1,587
778
1,229
663
332
297
208
108
255
107
7
54
61
84
46.8
20.3
22.1
14.5
7.8
15.4
8.3
0.9
1,880
984
1,538
879
382
416
272
147
289
156
17
0.005*
0.003*
0.003*
0.66
0.013*
0.25
0.25
0.57
0.08
0.10
*Statistical signicance, p G 0.05
Patients With Pulmonary Contusion
Of the 3,467 patients, 54% (1,880 of 3,467) had a documented lung contusion. When comparing patients with pulmonary contusion with those without contusion, there was a
statistically signicant increase in the rate of mechanical
ventilation (61% vs. 56%, p G 0.005), time on the ventilator
(7.3 days vs. 7.0 days, p G 0.016), need for ICU admission
(84% vs. 80%, p G 0.003), days spent in the ICU (9.9 days vs.
9.2 days, p G 0.0032), and total days in the hospital (17.1 days vs.
16.1 days, p G 0.018). Patients with pulmonary contusions
also had higher rates of chest tube placement (47% vs. 42%,
p G 0.003) and pneumonia (22% vs. 19%, p G 0.013). While
these were statistically signicant, the magnitude of the difference was not as great as when comparing patients with presence
or absence of severe head injury. There were no differences with
regard to the rate of tracheostomy, ARDS, sepsis, or death. There
were also no differences between the two groups with regard
to use of epidural catheters for pain or surgical xation of the
chest wall (Tables 1 and 2).
Treatment ModalitiesVEpidural Catheters,
Surgical Fixation of the Chest Wall
Epidural catheters were used in 8% (283 of 3,467), and
only 24 of the 3,467 patients underwent surgical xation of
their ail chest (0.7%).
DISCUSSION
The current treatment of severe chest wall injuries consists of nonsurgical management via intubation and intermittent positive pressure ventilation (internal pneumatic splint),
analgesia, pulmonary toilet, and chest physiotherapy.1,4,6 Patients with severe chest wall injuries have been reported to have
high rates of morbidity and mortality, and studies have shown
that only 43% of such patients return to their previous full-time
employment.10 Many patients complain of chronic pain, subjective dyspnea, chest tightness, and chest wall deformity10,11
and have low scores on the SF-36.12
TABLE 2. Days on Mechanical Ventilation, ICU Stay, Total Hospital StayVBased on Injury Pattern
All Patients
Outcomes
Day on mechanical ventilation
Ventilated patients only
All patients
Days in ICU
Patients admitted to ICU only
All patients
Days in hospital
No Severe
Head Injury
With Severe
Head Injury
No Pulmonary
Contusion
With
Pulmonary
Contusion
Mean
SD
Mean
SD
Mean
SD
Mean
SD
Mean
SD
12.1
7.2
11.0
12.0
12.0
6.5
11.9
10.6
12.7
11.2
12.1
12.1
0.60
0.001*
12.4
7.0
12.1
11.0
11.9
7.3
11.9
11.0
0.91
0.016*
11.7
9.6
16.6
11.8
12.0
16.0
11.0
8.9
15.8
11.6
11.3
14.6
15.0
13.4
21.4
13.4
13.5
21.7
0.0001*
0.001*
0.0005*
11.5
9.2
16.1
11.9
11.6
15.6
11.8
9.9
17.1
12.1
11.9
16.3
0.242
0.0032*
0.018*
*Statistical signicance, p G 0.05
* 2013 Lippincott Williams & Wilkins
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
465
J Trauma Acute Care Surg
Volume 76, Number 2
Dehghan et al.
Figure 3. Outcome for patients with ail chest, based on head injury.
This study of 3,467 patients with a ail chest injury
demonstrated high rates of morbidity and mortality. More
than 80% of patients required ICU admission, for a mean of
11.7 days. Mechanical ventilation was used in a large proportion (59%) of patients, and those on a mechanical ventilator
had a mean of 12.1 ventilation days. Long-term mechanical
ventilation has many complications. Prolonged mechanical
ventilation in patients with chest trauma has been reported
to result in high rates of pneumonia, barotrauma, sepsis, ICU
stay, and death.1,2,4,5,7,8 Decreasing the number of days on
mechanical ventilation may result in decreased morbidity
and mortality and may dramatically decrease medical costs.
The average hospital cost of mechanical ventilation/ICU stay
for trauma patients in the United States is approximately
$3,500 per day;13 decreasing the length of stay by even a few
days can produce dramatic savings in health care expenses.
There have been a number of studies demonstrating
the benet of surgical xation of severe chest wall injuries,2,5,7,8,14
including fewer days on mechanical ventilation,5,7Y9 decreased
length of ICU stay,2,5,7,8 fewer chest infections,5,7,8 and less
chronic pain,2 while improving long-term respiratory function15,16 and promoting earlier return to work.8 There are three
previously published randomized controlled trials on this topic.5,8,17 Tanaka et al.8 demonstrated that patients with surgical
xation were extubated a mean of 2.5 days postoperatively,
compared with 18.3 days in the nonoperative group. Granetzky
et al.5 reported 2 days of mechanical ventilation in the surgical
group, compared with 12 days in the nonsurgical group. However, these randomized controlled trials have been criticized
for small sample size, outdated methods of surgical xation
(K-wires, Judet struts, absorbable plates), and vague inclusion/
exclusion criteria. We believe there is a need for a large, multicenter, well-designed, randomized controlled trial in this area,
to better assess the benets of surgical xation versus nonoperative care for trauma patients with ail chest injuries.
Given the increased interest in surgical xation in recent
years,18,19 we sought to determine if this translated into more
466
patients being treated with surgical intervention. Contrary
to our expectations, a very small proportion of patients were
treated with surgical xation (24 of 3,467, or 0.7%). This could
be caused by the fact that the data were collected from 2007
to 2009, and it is possible that xation rates have increased
since that time. It could also mean that despite numerous recent published series of surgical xation of ail chest injuries,
nonoperative treatment is still the overwhelming choice of
treatment.
The optimal nonoperative treatment of patients with
ail chest includes adequate pain management, via use of
epidural catheters, intercostal nerve blocks, or patient-centered
analgesia.6 The use of epidural catheters seems to be the most
preferred method, with improved outcomes and lower complications compared with other methods.6,20Y22 Compared with
intravenous narcotic use, epidural catheters allow for improved
subjective pain perception, pulmonary functions tests, lower
rate of pneumonia, as well as decreased length of time on a
mechanical ventilator or ICU stay.6,20,21 They also have lower
rate of complications such as respiratory depression, somnolence, and gastrointestinal symptoms.6 Epidural catheters have
also been compared with intrapleural catheters in a previous
randomized controlled trial and have shown to decrease pain
and improve tidal volume and negative inspiratory pressures.22
While we were unable to assess the number of patients treated
with intercostal nerve blocks or patient-centered analgesia, we
were able to examine the use of epidural catheters for patients
with ail chest injuries, and we were able to determine that
these were seldom used (8%). While coding validity remains
unknown, such a low number raises the possibility of underuse.
The literature supports the suspicion that patients with
ail chest injury, with concurrent severe head injury or pulmonary contusion, have poor outcomes. In addition, the literature on surgical xation of such injuries consistently reports
severe head injury and pulmonary contusion as exclusion
criteria for surgical xation. The reason suggested is that the
primary early benet of surgical xation is decreased time on
* 2013 Lippincott Williams & Wilkins
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
J Trauma Acute Care Surg
Volume 76, Number 2
Dehghan et al.
mechanical ventilation; however, patients with head injury
and pulmonary contusion may require long-term mechanical
ventilation and do not attain the benets of early extubation.
Based on the results of this study, we can conrm that patients
with a ail chest and severe head injury have poor outcomes
in all categories compared with patients without severe head
injury. These patients had an increased rate of need for mechanical ventilation and time on a ventilator and had higher
rates of chest tube placement, pneumonia, ARDS, and sepsis.
Tracheostomy was performed almost twice as often, and the
death rate was more than 3.5 times higher than patients without
a severe head injury. Further research in this area is warranted
to help improve outcomes of this subset of patients with ail
chest injuries.
With respect to the impact of pulmonary contusion, there
were statistically signicant differences, of a much smaller
magnitude compared with the effect of head injury. This may
be caused by variability in coding this injury and a lack of a
clear denition for pulmonary contusion. Whether these were
diagnosed based on radiologist reports of imaging or more
objective tests such as bronchoalveolar lavage is unknown.
Many patients with blunt chest injuries have pulmonary contusions, but the severity of this entity may determine outcome.
Patients with extensive pulmonary contusion may have worse
outcomes compared with those without. However, including
all patients with contusions, whether small or extensive, and
using less than optimal criteria result in difculty in the interpretation of results. There is currently no widely used classication of pulmonary contusions, and there is a need for a
more consistent method of diagnosis and classication of these
injuries.
The limitations of this study are its retrospective nature;
there were missing data for some of the outcomes, and the validity of coding remains unknown. Given the heterogeneity of
head injuries and coding uncertainty around pulmonary contusions, multivariable analyses of these conditions were not performed. The strengths are that we have attempted to restrict our
analysis to centers that code accurately and have been able to
identify one of the largest populations of patients with ail chest
injuries in the literature to date.
CONCLUSION
Patients who have sustained a ail chest have signicant
morbidity (ICU admission, 82%; mechanical ventilation, 59%;
need for chest tube, 44%; tracheostomy, 21%; ARDS, 14%;
sepsis, 7%) and a high rate of mortality (16%). Patients with
concurrent severe head injury have signicantly worse outcomes compared with those without a severe head injury on all
parameters studied. Patients with concurrent pulmonary contusion also had poor outcomes, although the magnitude of this
difference was less than that seen with the presence of severe
head injury.
More than 99% of patients with ail chest injuries were
treated without surgical intervention, and only a small proportion (8%) received aggressive pain management with epidural
catheters. Given the high rates of morbidity and mortality in
patients with ail chest injuries, alternate methods of treatment
need to be investigated, such as more consistent use of epidural
catheters for pain or surgical xation. Previous small randomized trials have suggested improvements with surgical xation of
these injuries, although this practice is neither widely accepted
nor practiced in North America, with only 0.7% of ail chests
being surgically treated. More research in this area is warranted
to help improve patient outcomes. A large multicenter randomized controlled trial comparing modern surgical techniques
versus nonoperative care for trauma patients with ail chest
injuries is required.
AUTHORSHIP
N.D. and A.N. performed the literature search. N.D., C.D.M., and
M.D.M. designed this study. C.D.M. collected the data. N.D. and
C.D.M. analyzed and interpreted the data. All authors participated in
writing and critically revision.
DISCLOSURE
The authors declare no conicts of interest.
REFERENCES
1. Lafferty PM, Anavian J, Will RE, Cole PA. Operative treatment of chest
wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am.
2011;93(1):97Y110.
2. Engel C, Krieg JC, Madey SM, Long WB, Bottlang M. Operative chest
wall xation with osteosynthesis plates. J Trauma. 2005;58(1):181Y186.
3. Kaiser LRSS. Thoracic Trauma. Surgical Foundations, Essentials of
Thoracic Surgery. Philadelphia, PA: Elvisor; 2004:109.
4. Nirula R, Diaz JJ Jr, Trunkey DD, Mayberry JC. Rib fracture repair: indications, technical issues, and future directions. World J Surg. 2009;33(1):
14Y22.
5. Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical
versus conservative treatment of ail chest. Evaluation of the pulmonary
status. Interact Cardiovasc Thorac Surg. 2005;4(6):583Y587.
6. Simon B, Ebert J, Bokhari F, Capella J, Emhoff T, Hayward T 3rd, et al.
Management of pulmonary contusion and ail chest: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma
Acute Care Surg. 2012;73(5 Suppl 4):S351YS361.
7. Ahmed Z, Mohyuddin Z. Management of ail chest injury: internal xation versus endotracheal intubation and ventilation. J Thorac Cardiovasc
Surg. 1995;110:1676Y1680.
8. Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, et al.
Surgical stabilization of internal pneumatic stabilization? A prospective
randomized study of management of severe ail chest patients. J Trauma.
2002;52(4):727Y732; discussion 732.
9. Voggenreiter G, Neudeck F, Aufmkolk M, Obertacke U, Schmit-Neuerburg
KP. Operative chest wall stabilization in ail chestVoutcomes of patients
with or without pulmonary contusion. J Am Coll Surg. 1998;187(2):130Y138.
10. Landercasper J, Cogbill TH, Lindesmith LA. Long-term disability after
ail chest injury. J Trauma. 1984;24:410Y414.
11. Beal SL, Oreskovich MR. Long-term disability associated with ail chest
injury. Am J Surg. 1985;150:324Y326.
12. Kerr-Valentic MA, Arthur M, Mullins RJ, Pearson TE, Mayberry JC. Rib
fracture pain and disability: can we do better? J Trauma. 2003;54(6):1058Y1063;
discussion 1063Y1064.
13. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive
care unit day: the contribution of mechanical ventilation. Crit Care Med.
2005;33(6):1266Y1271.
14. Nirula R, Allen B, Layman R, Falimirski ME, Somberg LB. Rib fracture
stabilization in patients sustaining blunt chest injury. Am Surg. 2006;72(4):
307Y309.
* 2013 Lippincott Williams & Wilkins
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
467
J Trauma Acute Care Surg
Volume 76, Number 2
Dehghan et al.
15. Lardinois D, Krueger T, Dusmet M, Ghisletta N, Gugger M, Ris HB.
Pulmonary function testing after operative stabilisation of the chest wall for
ail chest. Eur J Cardiothorac Surg. 2001;20(3):496Y501.
16. Mayberry JC, Kroeker AD, Ham LB, Mullins RJ, Trunkey DD. Long-term
morbidity, pain, and disability after repair of severe chest wall injuries. Am
Surg. 2009;75(5):389Y394.
17. Marasco SF, Davies AR, Cooper J, Varma D, Bennett V, Nevill R, et al.
Prospective randomized controlled trial of operative rib xation in traumatic ail chest. J Am Coll Surg. 2013;216(5):924Y932.
18. Althausen PL, Shannon S, Watts C, Thomas K, Bain MA, Coll D, et al. Early
surgical stabilization of ail chest with locked plate xation. J Orthop
Trauma. 2011;25(11):641Y647.
468
19. Bottlang M, Long WB, Phelan D, Fielder D, Madey SM. Surgical stabilization of ail chest injuries with MatrixRIB implants: a prospective
observational study. Injury. 2013;44:232Y238.
20. Simon BJ, Cushman J, Barraco R, Lane V, Luchette FA, Miglietta M, et al.
Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;
59(5):1256Y1267.
21. Bulger EM, Edwards T, Klotz P, Jurkovich GJ. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136(2):
426Y430.
22. Luchette FA, Radafshar SM, Kaiser R, Flynn W, Hassett JM. Prospective
evaluation of epidural versus intrapleural catheters for analgesia in chest
wall trauma. J Trauma. 1994;36(6):865Y869; discussion 869Y870.
* 2013 Lippincott Williams & Wilkins
Copyright 2014 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Acute Respiratory FailureDocument13 paginiAcute Respiratory FailureKartikaÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Critical Care Therapy and Respiratory Care Section: 1.0 DescriptionDocument7 paginiCritical Care Therapy and Respiratory Care Section: 1.0 DescriptionStefano Ignacio Valenzano FigueroaÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Lecture Notes On Respiratory Medicine (Wiley, 2003) PDFDocument213 paginiLecture Notes On Respiratory Medicine (Wiley, 2003) PDFNavin ShawnÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- A Guide To Using Inhalers For COPD & Asthma: Smarter. Medication. ManagementDocument28 paginiA Guide To Using Inhalers For COPD & Asthma: Smarter. Medication. ManagementGUSWAN FERDIANSYAHÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Acute Exacerbation of Copd by DR Irappa MadabhaviDocument39 paginiAcute Exacerbation of Copd by DR Irappa MadabhaviIrappa MadabhaviÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Chapter 190: A Quick Guide to Wheezing CausesDocument1 paginăChapter 190: A Quick Guide to Wheezing CausespelinÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Effectiveness and Pharmacoeconomic Analysis of The Treatment of Severe Asthma With Omalizumab in Clinical PracticeDocument9 paginiEffectiveness and Pharmacoeconomic Analysis of The Treatment of Severe Asthma With Omalizumab in Clinical PracticePetrus Kabul TogarmaÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Test Biology 10th Class Ch#10 Gaseous ExchangeDocument1 paginăTest Biology 10th Class Ch#10 Gaseous ExchangeASAD73% (11)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Decrease in Paco2 With Prone Position Is Predictive of Improved Outcome in Acute Respiratory Distress SyndromeDocument7 paginiDecrease in Paco2 With Prone Position Is Predictive of Improved Outcome in Acute Respiratory Distress SyndromedarwigÎncă nu există evaluări
- 380 Case Study CDocument11 pagini380 Case Study Capi-639359658Încă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Efficacy of Retraining Diaphragm by Proprioceptive Neuromuscular Facilitation Versus Diaphragmatic Breathing Exercises in Reducing Dyspnoea in The Copd PatientsDocument4 paginiEfficacy of Retraining Diaphragm by Proprioceptive Neuromuscular Facilitation Versus Diaphragmatic Breathing Exercises in Reducing Dyspnoea in The Copd PatientsInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Announcement BIRCDocument8 paginiAnnouncement BIRCHendarsyah SuryadinataÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Respiratory Distress SyndromeDocument3 paginiRespiratory Distress SyndromeJamaica Louise Quetua MacalinoÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Weaning An Adult Patient From Invasive Mechanical VentilationDocument22 paginiWeaning An Adult Patient From Invasive Mechanical VentilationYuanda ArztÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- Spirometry Interpretation: Lung VolumesDocument4 paginiSpirometry Interpretation: Lung VolumesBobet ReñaÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Asma 1Document14 paginiAsma 1Dwi Yuli YantiÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Lower Respiratory Tract InfectionDocument8 paginiLower Respiratory Tract InfectionRarasRachmandiarÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- Jurnal Internasional BaruDocument4 paginiJurnal Internasional BaruCahaya YusmaniÎncă nu există evaluări
- Physical Exam For PneumoniaDocument3 paginiPhysical Exam For PneumoniaAnna SłońskaÎncă nu există evaluări
- Dupilumab COPD NEJMDocument10 paginiDupilumab COPD NEJM5fqkqkcdhtÎncă nu există evaluări
- Techniques in Cardiopulmonary PhysiotherapyDocument180 paginiTechniques in Cardiopulmonary PhysiotherapyAaliyah ShaikhÎncă nu există evaluări
- Practical Physiology RRS ResDocument9 paginiPractical Physiology RRS Resmina mounirÎncă nu există evaluări
- TuberculosisDocument475 paginiTuberculosisMaría De Los Ángeles Costta Michuy75% (4)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Bronchial AsthmaDocument59 paginiBronchial Asthmashefalika mandremÎncă nu există evaluări
- Chest and LungsDocument49 paginiChest and LungsChala KeneÎncă nu există evaluări
- Deep Breathing ExerciseDocument7 paginiDeep Breathing ExerciseRuchika Kaushal100% (5)
- Use of Expired CO Monitoring in The ICU: Dennis Bing, RRTDocument24 paginiUse of Expired CO Monitoring in The ICU: Dennis Bing, RRTasyi-2Încă nu există evaluări
- Dapus Ensefalitis 2Document4 paginiDapus Ensefalitis 2lamidahfazaÎncă nu există evaluări
- Awake Versus Deep ExtubationDocument22 paginiAwake Versus Deep Extubationtipanan_earnÎncă nu există evaluări
- G1 Health Teaching PlanDocument4 paginiG1 Health Teaching Planbernadil01Încă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)