Documente Academic
Documente Profesional
Documente Cultură
6 07.Pdfs 3 Faculty Files
Încărcat de
Ella GolikDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
6 07.Pdfs 3 Faculty Files
Încărcat de
Ella GolikDrepturi de autor:
Formate disponibile
The PCSO Bulletin is proud to introduce a new column, edited by
UCSF Clinical Professor, Ib Leth Nielsen, DDS. His initial article reminds
us of some of the values of headfilm analysis and some of the pitfalls.
For future columns, he will invite articles from others who are faculty in
the PCSO orthodontic programs, both in the U.S. and Canada.
FAC U LT Y
Files
WHAT YOU MAY HAVE FORGOTTEN
ABOUT CEPHALOMETRIC ANALYSIS
BY IB LETH NIELSEN, DDS
hen Hofrath in Germany and Broadbent in the
USA introduced the radiographic headfilm technique to orthodontists in 1931, it initiated a new
era in orthodontic diagnosis and treatment planning. Around
the turn of the 20th century, Angle and his followers could
only plan treatment based on the patients facial profile
and the malocclusion of the teeth. With the introduction
of radiographic headfilm technique, orthodontists could
plan their treatment using radiographic information about
the patients facial skeleton. Many possibilities opened up
for orthodontists that to this day have proven an invaluable
help in treatment planning, analysis of growth and treatment and prediction of possible treatment outcomes. In
the following we shall discuss the technique and application of cephalometric analysis in several areas where this
technique is used today:
a) Cephalometric morphological analysis of
individual headfilms
b) Growth and treatment analysis
c) Growth and treatment prediction or simulation
In this first Faculty Files article, we will focus on the
morphological analysis. In later articles we will describe
the growth and treatment analysis and the prediction or
simulation of growth and treatment.
MORPHOLOGICAL ANALYSIS
The main area of application of cephalometrics today is in
the description of a patients facial profile, in a so-called
morphological analysis. A main purpose of a cephalometric
analysis is to determine departures from the average in
skeletal and dento-alveolar morphology. The information
gathered from such a single headfilm is limited and represents information about the face in profile at one time point
and says very little about future growth and development of
the face. With the information gathered from many of the
numerous analyses available today, it is possible, however,
to determine whether the malocclusion is related to skeletal or dento-alveolar deviations, which is very valuable
to the orthodontist in the treatment planning phase. Some
analyses also enable the clinician to determine if there is
dento-alveolar compensation or dysplastic development
in a patient with a skeletal discrepancy and where this
change is located.
S U M M E R 2 0 0 7 P C S O B U L L ET I N
Figure 1
This type of analysis basically describes the facial makeup of an individual, so to speak, and is somewhat limited
in its clinical values. It should therefore be reduced to
parameters that are meaningful and informative.
Today there are many morphological analyses available to
the clinician. Most are based on individual preferences and
frequently lack sufficient data base to support the use on
larger groups of individuals. In this area of facial analysis
more numbers are not necessarily better, and often serve
only to confuse the clinician. As a result, the analysis becomes an exercise in futility and does not provide much
help with treatment decisions.
Most orthodontists are aware that averages or mean values
should not be applied to the individual case. The mean
values are only a guide to help determine an individuals
facial make-up and the standard deviations indicate the
extent of the variation from the mean. Nevertheless, these
mean values are sometimes used as treatment goals with the
interpretation that if the individual does not fit the mean,
something is wrong. This concept of means, or norms,
is misleading and erroneous as it can make the orthodontist think he or she should treat patients to a given mean
value. The fact of the matter is that all the mean values we
routinely use are associated with large standard deviations,
which demonstrate the great variability within the normal
population. We also should remember that in the U.S. there
are many different ethnic groups. The esthetic goals from
one population may be very different for another.
13
FAC U LT Y
F IL ES
A misunderstanding that we frequently encounter is the
incorrect use of the concept of the standard deviation. The
fact that a measurement of a skeletal discrepancy is within
one standard deviation does not mean that it is almost
normal and therefore insignificant. There are in most cases
several components involved such as the protrusion of the
maxilla, the prognathism of the mandible and the shape of
the cranial base. Each of these parameters can be within
one standard deviation, but if they go in opposite direction,
amount to a pronounced discrepancy.
Conversely, an acute cranial base angle is associated with
bimaxillary prognathism.
SKELETAL AND DENTO-ALVEOLAR MALOCCLUSIONS
The association between malocclusion and the dento-alveolar
and skeletal components present can be illustrated in case of
excessive overjet, as seen in Figure 3. The possible combinations of dental, alveolar and skeletal deviations that can cause
an excessive overjet are illustrated as seen below.
In a cephalometric analysis, it is preferable to use angular
rather than linear measurements, as angular measurements
vary little due to size and age differences between individuals.
The use of linear parameters should always be accompanied
by a respect for the wide individual variability.
The cephalometric values in general must be used with
caution and only as guides to what area or structure an occlusal problem may be related and the numbers serve only
as guides not as a target. Most cephalometric analysis are
so-called component analysis that provide information
as to relationships between facial and dental components
in the horizontal, vertical and transverse dimension.
Figure 3 (From Bjrk, 1974)
Figure 2 (From Solow, 1980)
As seen in Fig. 2, the facial components consist of the
cranial base, the maxilla and the mandible. In addition,
there is an upper and a lower dento-alveolar component.
The facial components are highly correlated to each other
and changes in their sagittal and vertical position influence
the dento-alveolar relationships and thereby the occlusion
of the teeth. One example is the cranial base which depending on its shape, can affect the position of the jaws. If,
for instance, the median cranial base, as measured by the
(N-S-Ba) angle, is increased or more obtuse than normal,
it frequently is associated with bimaxillary retrognathism.
14
Illustration (1-2) shows the alveolar changes that can result
in an overjet; maxillary alveolar protrusion, mandibular
alveolar retrusion or a combination of the two; (3-4) shows
the possible variations in maxillary or mandibular incisor
inclination; and (5) the skeletal relationships where maxillary protrusion, mandibular retrognathism or a combination
thereof can result in an excessive overjet. In other words,
variations in overjet can be expressed through five factors
that each can be increased, reduced or remain unchanged
during the development. This yields a total of 35=243 possible combinations for variations in the development of the
overjet. It should remind us of the importance of developing
a differential diagnosis for each patient in order to correctly
address the problems at hand.
DENTO-ALVEOLAR COMPENSATION
Another biological phenomenon that is critical to a successful treatment outcome is to recognize and understand
the role of dento-alveolar compensation. In patients with
sagittal, vertical or transverse skeletal discrepancies, there
is often a considerable amount of dento-alveolar compensation. This biological mechanism often masks the actual
skeletal deviations and must be considered during treatment planning. In most patients, it is necessary to reduce
or remove the compensation in order to achieve a skeletal
P C S O B U L L ET I N S U M M E R 2 0 0 7
FAC U LT Y
correction, especially in growing patients and adults who
are planned for orthognathic surgical correction. In other
patients, it may be desirable to maintain the compensatory
changes or even accentuate them to achieve an acceptable
treatment result.
FIL ES
A further step towards incorporating compensation in
treatment planning has been put forward by Ricketts
(1957), who set up treatment goals in his visual treatment
plan incorporating compensation for variations in the jaw
relationship. He used a line from point A to Pog as a socalled compensation line, and related the incisal edge of
the lower incisor to this line. By relating the incisal edge
to this line, he automatically introduced a certain amount
of dental compensation. Then different positions would be
developed relative to the individual facial growth type.
The approach to analyzing a headfilm should, first of all,
concentrate on determining the jaw relationship and then on
to what extent departures from the normal jaw relationship
have been compensated in the dento-alveolar structures.
The goal for treatment will then depend on whether the
skeletal problem is best corrected by growth modification,
tooth movements or surgical correction.
PREDICTIVE POWER OF THE LATERAL HEADFILM
Figure 4
In the example seen in Figure 4, the patient has a Class II,
Div. 1 malocclusion due to a retrognathic mandible. The
lower incisors show compensatory proclination as the
natural biological attempt to mask the skeletal problem
(Solow, 1980). No compensation is seen in the maxilla
where the teeth are dysplastically proclined, possibly due
to a lip habit. In this patient, surgical correction through
mandibular advancement was planned so the orthodontic
treatment was directed towards reducing the compensation
to maximize the mandibular advancement. The concept of
dento-alveolar compensation has been incorporated not
only in the Bjrk (1961) analysis, but in other analysis as
well on a more or less intuitive basis. For example, Steiner
(1959) developed a series of acceptable compromises for
variations in the sagittal jaw relationship. As seen in Fig.
5, varying jaw relationships, according to Steiner, require
different changes in upper and lower incisor inclination for
an acceptable occlusion of the anterior teeth.
Figure 5 (From Steiner, 1959)
S U M M E R 2 0 0 7 P C S O B U L L ET I N
As to the predictive value of individual headfilms, it is
possible to some degree to predict the quality of future
facial growth and in particular of mandibular growth.
Bjrk (1966), in his facial growth studies of the mandible,
demonstrated that certain stable structures in the mandible
could consistently be relied upon as indicators of future
growth rotation of this jaw. He also emphasized that these
structural signs were only indicators and had the greatest
predictive value in the more pronounced cases of mandibular growth rotations.
After many years of continued research into area of
mandibular growth, Bjrk and Skieller (1972) concluded
that by using additional signs such as inter-molar angle,
shape of the lower border of the mandible, and inclination
of the mandibular symphysis, it was possible to improve
the predictability of growth rotation of the mandible. In
this context it should be emphasized that the majority of
untreated patients demonstrate some degree of anterior
or forward growth rotation of the mandible. Orthodontic
treatment, however, influences the rotation of the mandible
depending upon maxillary growth changes and the extent
of upper and lower molar eruption during treatment.
Posterior or backward rotation is seen only in a small
percentage of patients and is in the more pronounced cases
predictable with a great degree of certainty. The importance
of forward growth rotation of the mandible is that it is
associated with a favorable anterior displacement of the
chin and the potential for improvement in a deficient jaw
relationship. Posterior or backward mandibular growth
rotation, on the other hand, is associated with no forward
15
FAC U LT Y
F I LES
mandibular displacement and in some instances may make the
facial balance worse. There are several other positive implications of this rotational change that relate to the actual treatment,
the treatment mechanics and the post treatment stability, which
is outside the scope of this description of the application of
cephalometric analysis.
Bjrk, A. and Skieller, V. Facial development and tooth eruption. Am.
J. Orthod. 62; 339-383, 1972
WHAT DOES IT ALL MEAN?
Solow, B. The dento-alveolar compensatory mechanism: Background
and clinical implications. Brit. J. Orthod. 7:145-161, 1980
The initial analysis of the lateral headfilm is an important part of
the work up of the patient. The information gathered should be
an integral part of the diagnosis and guide the clinician towards
the right treatment plan. Differentiating between skeletal or
primarily dento-alveolar malocclusions is important, as it tells
the clinician what problems he or she is dealing with. It is just
as important in this case to determine if dysplastic changes have
taken place, as it is in cases with skeletal problems to discern
if dento-alveolar compensations are present. Then it must be
decided to what extent this compensation needs to be removed
in order to achieve an ideal result. In cases where there are the
so-called dysplastic changes, it is frequently an indication that
some form of soft tissue problem such as a lip habit, tongue
thrust or airway problem is present that needs to be taken into
consideration. A careful cephalometric analysis is therefore not
only a great help in locating the problems, but often points to
what needs to be corrected and should not be ignored as an integral part of the treatment planning. It is important to remember
that meaningful data can be obtained from the headfilm and if
the information is carefully applied, it can guide the clinician
towards the correct treatment plan for the patient.
REFERENCES
Bjrk, A. The face in profile. An anthropological X-ray investigation
on Swedish children and conscripts. Swedish Tandlkare-Tidskrift.
Suppl. 40: 1947
Bjrk, A. The relationship of the jaws to the cranium. In Lundstrm,
A. (Ed.) Introduction to Orthodontics. pp. 104-140, London:
McGraw-Hill, 1961
Ricketts, R. M. Planning treatment on the basis of the facial pattern
and an estimate of growth. Angle Orthod. 27: 14-37, 1957
Steiner, C. C. Cephalometrics in clinical practice. Angle Orthodonticst.
29: 8-29, 1959
CALAOMS 2007 Fall Meeting
November 10 & 11, 2007
Estancia Resort and Spa
La Jolla, CA
Speakers:
Dale Bloomquist, DDS, MS
Emeritus Associate Professor
Department of OMS
University of Washington
&
Don Joondeph, DDS, MS
Emeritus Associate Professor
Department of Orthodontics
Bjrk, A. Variations in the growth pattern of the human mandible:
Longitudinal radiographic study by the implant method. J. Dent.
Res.. 42: 400-411, 1963
Topic:
Orthognathic Surgery Made Practical:
The Orthodontic and Surgical Approaches
Bjrk, A. Prediction of mandibular growth rotation. Am. J. Orthod.
55: 55; 585-599, 1969
A course for the Surgical Orthodontic team
This seminar is open to all Orthodontists,
Dentists, Physicians and
Oral & Maxillofacial Surgeons
visit our website at www.calaoms.org/events
16
P C S O B U L L ET I N S U M M E R 2 0 0 7
S-ar putea să vă placă și
- Facial Keys To Orthodontic Diagnosis and Treatment Planning. Part I. G. William Arnett, DDS and Robert T. Bergman, DDS, MSDocument14 paginiFacial Keys To Orthodontic Diagnosis and Treatment Planning. Part I. G. William Arnett, DDS and Robert T. Bergman, DDS, MSdrimtiyaz123100% (1)
- Orthodontic and Peadiatric Dentistry - COLOUR GUIDE 2000Document172 paginiOrthodontic and Peadiatric Dentistry - COLOUR GUIDE 2000api-3806407100% (7)
- Vto Seminar No.2Document115 paginiVto Seminar No.2Dr Shivam Verma100% (1)
- Facial Keys To Orthodontic Diagnosis and Treatment, Part IIDocument15 paginiFacial Keys To Orthodontic Diagnosis and Treatment, Part IIAlvaro Chacón100% (1)
- Cranial Strains and MalocclusionDocument5 paginiCranial Strains and MalocclusionRyan Dobbeck100% (1)
- Management of Perio Prostho Situations in DentistryDocument18 paginiManagement of Perio Prostho Situations in DentistryHarsha ReddyÎncă nu există evaluări
- Facial Analysis. A Chomprensyve Approach To Treatment Planning in Ahesthetic DentistryDocument8 paginiFacial Analysis. A Chomprensyve Approach To Treatment Planning in Ahesthetic DentistryOmanakuttan KrÎncă nu există evaluări
- Pharmacology Made Insanely Easy PowerPointDocument42 paginiPharmacology Made Insanely Easy PowerPointBetsy Brown Byersmith82% (22)
- Orthognathic Surgery RonalDocument56 paginiOrthognathic Surgery Ronaldrghempik100% (2)
- A Countdown To Orthognathic SurgeryDocument5 paginiA Countdown To Orthognathic SurgeryhaneefmdfÎncă nu există evaluări
- Facial Aesthetics 2Document9 paginiFacial Aesthetics 2Putri Morteza100% (1)
- Orthodontic Treatment PlanningDocument22 paginiOrthodontic Treatment PlanningRian Al-Murtadha50% (2)
- Multidisciplinary Approach to Esthetic DentistryDocument19 paginiMultidisciplinary Approach to Esthetic DentistryAya Ibrahim Yassin100% (1)
- Hip Disorders in Children: Postgraduate Orthopaedics SeriesDe la EverandHip Disorders in Children: Postgraduate Orthopaedics SeriesEvaluare: 3 din 5 stele3/5 (2)
- Open Bite, A Review of Etiology and Manageme PDFDocument8 paginiOpen Bite, A Review of Etiology and Manageme PDFVieussens JoffreyÎncă nu există evaluări
- The Osseous Genioplasty: Clinicsin Plastic SurgeryDocument16 paginiThe Osseous Genioplasty: Clinicsin Plastic SurgeryRajan KarmakarÎncă nu există evaluări
- Critical Incident Stress Debriefing GuideDocument11 paginiCritical Incident Stress Debriefing GuideMae Goñez100% (2)
- Lyons Et Al-2017-Periodontology 2000Document4 paginiLyons Et Al-2017-Periodontology 2000Julio César PlataÎncă nu există evaluări
- Orthognathic Surgery & Lefort 1 OsteotomiesDocument71 paginiOrthognathic Surgery & Lefort 1 OsteotomiesNikhilAsokÎncă nu există evaluări
- Orthodontic Aspects of Orthognathic Surgery - Shiva ShankarDocument57 paginiOrthodontic Aspects of Orthognathic Surgery - Shiva Shankarnevin santhosh100% (1)
- El Exprime Hombres 2Document11 paginiEl Exprime Hombres 2Carlos GonzalezÎncă nu există evaluări
- 10.2 Major Surgical ProceduresDocument22 pagini10.2 Major Surgical ProceduresishtiiiÎncă nu există evaluări
- Meaw TechniqueDocument11 paginiMeaw TechniqueElla Golik100% (4)
- Context and Counseling BasicsDocument49 paginiContext and Counseling BasicsJohn Paul BrionesÎncă nu există evaluări
- Smile Design Dental PhotographyDocument3 paginiSmile Design Dental Photographydranilshinde100% (2)
- Computers in Orthodontics PDFDocument239 paginiComputers in Orthodontics PDFElla GolikÎncă nu există evaluări
- 7.principles of Dentofacial Orthopedics PDFDocument10 pagini7.principles of Dentofacial Orthopedics PDFMafer VazquezÎncă nu există evaluări
- Orthodontics andDocument9 paginiOrthodontics andSimona DobreÎncă nu există evaluări
- chin implantDocument6 paginichin implantAnkita GuravÎncă nu există evaluări
- Orthodontically Assisted Restorative Dentistry: Donald F. Reikie, DDS, MSDocument5 paginiOrthodontically Assisted Restorative Dentistry: Donald F. Reikie, DDS, MSAdityaÎncă nu există evaluări
- Bio-Progressive Therapy2C Part 53A Orthopedics in Bio-Progressive Therapy - JCO-ONLINE - COM - Journal of Clinical OrthodonticsDocument15 paginiBio-Progressive Therapy2C Part 53A Orthopedics in Bio-Progressive Therapy - JCO-ONLINE - COM - Journal of Clinical OrthodonticsKanchit SuwanswadÎncă nu există evaluări
- Registration: Stage II - Intermaxillary Relations: ProstheticsDocument6 paginiRegistration: Stage II - Intermaxillary Relations: ProstheticsOmar RamadanÎncă nu există evaluări
- 1. 1-s2.0-S0278239119305518-mainDocument15 pagini1. 1-s2.0-S0278239119305518-mainALEJANDRA INÉS NIETO ARIASÎncă nu există evaluări
- CirugiaDocument27 paginiCirugiaalexmtzgÎncă nu există evaluări
- Video Cephalometric Diagnosis (VCD) : A New Concept in Treatment Planning?Document17 paginiVideo Cephalometric Diagnosis (VCD) : A New Concept in Treatment Planning?Ismail BenameurÎncă nu există evaluări
- Applying New Knowledge To The CorrectionDocument27 paginiApplying New Knowledge To The Correctionandres belloÎncă nu există evaluări
- Deep Overbite Malocclusion: Analysis of The Underlying ComponentsDocument8 paginiDeep Overbite Malocclusion: Analysis of The Underlying ComponentsJorge Antonio Llaxacondor LlaxacondorÎncă nu există evaluări
- Open Bite: A Review of Etiology and Management: Peter Ngan, DMD Henry W. Fields, DDS, MS, MSDDocument8 paginiOpen Bite: A Review of Etiology and Management: Peter Ngan, DMD Henry W. Fields, DDS, MS, MSDAzi Pertiwi HussainÎncă nu există evaluări
- Calamia JR, Et Al. Smile Design and Treatment Planning With The Help of A Comprehensive Esthetic Evaluation Form. Dent Clin North Am. 2011Document24 paginiCalamia JR, Et Al. Smile Design and Treatment Planning With The Help of A Comprehensive Esthetic Evaluation Form. Dent Clin North Am. 2011justin4leÎncă nu există evaluări
- Alhammadi 2019Document9 paginiAlhammadi 2019Dela MedinaÎncă nu există evaluări
- Lecrure 7 Clinical Diagnosis 4th StageDocument16 paginiLecrure 7 Clinical Diagnosis 4th StageIbrahim HysamÎncă nu există evaluări
- Content ServerDocument10 paginiContent ServerJose Antonio Figuroa AbadoÎncă nu există evaluări
- Jurnal KennedyDocument5 paginiJurnal KennedydrgozanÎncă nu există evaluări
- Diagnosis and Treatment Planning: Nigel HarradineDocument22 paginiDiagnosis and Treatment Planning: Nigel HarradineLabassy RymeÎncă nu există evaluări
- Diagnosing and Treating Dentofacial AsymmetriesDocument4 paginiDiagnosing and Treating Dentofacial Asymmetriesblogger bloggerÎncă nu există evaluări
- Mi Sympheal DODocument10 paginiMi Sympheal DOChhavi SinghalÎncă nu există evaluări
- Orthognathic Surgery For Patients With Maxillofacial DeformitiesDocument25 paginiOrthognathic Surgery For Patients With Maxillofacial DeformitiesahmedatefÎncă nu există evaluări
- Diagnostic Limitations of Cephalometrics in OrthodonticsDocument6 paginiDiagnostic Limitations of Cephalometrics in OrthodonticsDevata RaviÎncă nu există evaluări
- Comlicaciones Osteotomia Saguital de RamaDocument4 paginiComlicaciones Osteotomia Saguital de RamaLeonardCarreraDiazÎncă nu există evaluări
- Occlusion, Orthodontics and Posture: Are There Evidences? The Example of ScoliosisDocument10 paginiOcclusion, Orthodontics and Posture: Are There Evidences? The Example of ScoliosisAndreaVanoyMartinÎncă nu există evaluări
- Clinical Considerations For Increasing Occlusal Vertical DimensionDocument9 paginiClinical Considerations For Increasing Occlusal Vertical DimensionAmar BhochhibhoyaÎncă nu există evaluări
- Journal of The World Federation of Orthodontists: Nasser Alqahtani, Brian Preston, Guoqiang GuanDocument5 paginiJournal of The World Federation of Orthodontists: Nasser Alqahtani, Brian Preston, Guoqiang GuanPaulanermÎncă nu există evaluări
- Retention and Relapse 3Document13 paginiRetention and Relapse 3Tara TeraÎncă nu există evaluări
- The Single-Tooth Dental Implant: Practical Guidelines For Hard Tissue AugmentationDocument16 paginiThe Single-Tooth Dental Implant: Practical Guidelines For Hard Tissue Augmentation歐亦焜100% (1)
- 10.2478_aoj-1980-0007Document10 pagini10.2478_aoj-1980-0007Naliana LupascuÎncă nu există evaluări
- Surgically Assisted Rapid Palatal Expansion: A Literature ReviewDocument13 paginiSurgically Assisted Rapid Palatal Expansion: A Literature ReviewRahulLife'sÎncă nu există evaluări
- Rationale of Total Arch Intrusion For Gummy Smile CorrectionDocument16 paginiRationale of Total Arch Intrusion For Gummy Smile CorrectionJair OliveiraÎncă nu există evaluări
- Evidence-Based Orthodontics For The 21st Century: Cover StoryDocument6 paginiEvidence-Based Orthodontics For The 21st Century: Cover StoryDeep GargÎncă nu există evaluări
- Centric Relation Critically Revisited - What Are The Clinical ImplicationDocument6 paginiCentric Relation Critically Revisited - What Are The Clinical ImplicationAlejandro RuizÎncă nu există evaluări
- Bioprogressive Simplified2C Part 13A Diagnosis and Treatment Planning - JCO-ONLINE - COM - Journal of Clinical OrthodonticsDocument9 paginiBioprogressive Simplified2C Part 13A Diagnosis and Treatment Planning - JCO-ONLINE - COM - Journal of Clinical OrthodonticsKanchit SuwanswadÎncă nu există evaluări
- Wolford 1994 - Occlusal Plane Alteration in Orthognathic Surgery, EstheticsDocument13 paginiWolford 1994 - Occlusal Plane Alteration in Orthognathic Surgery, EstheticsBillÎncă nu există evaluări
- Buccal Smile CorridorsDocument2 paginiBuccal Smile CorridorsTiến TrịnhÎncă nu există evaluări
- 1960 - Ricketts - Stating Objectves and Planning With Ceph TracingsDocument27 pagini1960 - Ricketts - Stating Objectves and Planning With Ceph Tracingsccy234196Încă nu există evaluări
- Therapeutic Alternatives For Addressing Pink Esthetic Complications in Single-Tooth Implants: A Proposal For A Clinical Decision TreeDocument12 paginiTherapeutic Alternatives For Addressing Pink Esthetic Complications in Single-Tooth Implants: A Proposal For A Clinical Decision TreeFrancisco VargasÎncă nu există evaluări
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementDe la EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementÎncă nu există evaluări
- Orthodontics in Obstructive Sleep Apnea Patients: A Guide to Diagnosis, Treatment Planning, and InterventionsDe la EverandOrthodontics in Obstructive Sleep Apnea Patients: A Guide to Diagnosis, Treatment Planning, and InterventionsSu-Jung KimÎncă nu există evaluări
- The Effectiveness of Locally Injected Platelet-Rich Plasma On Orthodontic Tooth Movement Acceleration: A Systematic Review of Animal StudiesDocument8 paginiThe Effectiveness of Locally Injected Platelet-Rich Plasma On Orthodontic Tooth Movement Acceleration: A Systematic Review of Animal StudiesElla GolikÎncă nu există evaluări
- Three-Dimensional Alteration of Constricted Alveolar Ridge Affected by Root Thrusting With and Without Open-Flap DecorticationDocument8 paginiThree-Dimensional Alteration of Constricted Alveolar Ridge Affected by Root Thrusting With and Without Open-Flap DecorticationElla GolikÎncă nu există evaluări
- Long Face Syndrome: A Literature Review: Journal of Dental Health, Oral Disorders & TherapyDocument6 paginiLong Face Syndrome: A Literature Review: Journal of Dental Health, Oral Disorders & TherapyElla GolikÎncă nu există evaluări
- PDFDocument12 paginiPDFElla GolikÎncă nu există evaluări
- Comparison of Anterior and Posterior Mini-Implant-Assisted Maxillary Incisor Intrusion: Root Resorption and Treatment EfficiencyDocument7 paginiComparison of Anterior and Posterior Mini-Implant-Assisted Maxillary Incisor Intrusion: Root Resorption and Treatment EfficiencyElla GolikÎncă nu există evaluări
- Interaction Between Deglutition, Tongue Posture, and MalocclusionDocument8 paginiInteraction Between Deglutition, Tongue Posture, and MalocclusionElla GolikÎncă nu există evaluări
- Effects of Palatal Crib and Bonded Spurs in Early Treatment of Anterior Open BiteDocument6 paginiEffects of Palatal Crib and Bonded Spurs in Early Treatment of Anterior Open BiteflorinÎncă nu există evaluări
- Short - and Long-Term Evaluation of Mandibular Dental Arch Dimensional ChangesDocument8 paginiShort - and Long-Term Evaluation of Mandibular Dental Arch Dimensional ChangesElla GolikÎncă nu există evaluări
- A Randomized Clinical Trial Comparing Mandibular Incisor Proclination Produced by Fixed Labial Appliances and Clear AlignersDocument9 paginiA Randomized Clinical Trial Comparing Mandibular Incisor Proclination Produced by Fixed Labial Appliances and Clear AlignersElla GolikÎncă nu există evaluări
- Relationship Between Dental Crowding and Mandibular Incisor ProclinationDocument7 paginiRelationship Between Dental Crowding and Mandibular Incisor ProclinationElla GolikÎncă nu există evaluări
- The Effect of Mechanical Vibration On Orthodontically Induced Root ResorptionDocument6 paginiThe Effect of Mechanical Vibration On Orthodontically Induced Root ResorptionElla GolikÎncă nu există evaluări
- Another Way of Looking at Treatment StabilityDocument6 paginiAnother Way of Looking at Treatment StabilityElla GolikÎncă nu există evaluări
- Evaluation of Posttreatment Stability After Orthodontic Treatment in The Mixed and Permanent DentitionsDocument9 paginiEvaluation of Posttreatment Stability After Orthodontic Treatment in The Mixed and Permanent DentitionsElla GolikÎncă nu există evaluări
- Do Prenatal and Postnatal Hypothyroidism Affect The Craniofacial Structure?: An Experimental StudyDocument8 paginiDo Prenatal and Postnatal Hypothyroidism Affect The Craniofacial Structure?: An Experimental StudyElla GolikÎncă nu există evaluări
- 011216-33 1Document7 pagini011216-33 1Ella GolikÎncă nu există evaluări
- Quantitative Light-Induced Fluorescence-Digital As An Oral Hygiene Evaluation Tool To Assess Plaque Accumulation and Enamel Demineralization in OrthodonticsDocument7 paginiQuantitative Light-Induced Fluorescence-Digital As An Oral Hygiene Evaluation Tool To Assess Plaque Accumulation and Enamel Demineralization in OrthodonticsElla GolikÎncă nu există evaluări
- Changes in Salivary Periodontal Pathogens After Orthodontic Treatment: An in Vivo Prospective StudyDocument6 paginiChanges in Salivary Periodontal Pathogens After Orthodontic Treatment: An in Vivo Prospective StudyElla GolikÎncă nu există evaluări
- Evaluation of Mandibular VolumeDocument6 paginiEvaluation of Mandibular VolumeElla GolikÎncă nu există evaluări
- Dynamic Smile Evaluation in Different Skeletal PatternsDocument7 paginiDynamic Smile Evaluation in Different Skeletal PatternsElla GolikÎncă nu există evaluări
- Reproducibility and Reliability of Three-Dimensional Soft Tissue Landmark Identification Using Three-Dimensional StereophotogrammetryDocument6 paginiReproducibility and Reliability of Three-Dimensional Soft Tissue Landmark Identification Using Three-Dimensional StereophotogrammetryElla GolikÎncă nu există evaluări
- Evaluation of Posttreatment Stability After Orthodontic Treatment in The Mixed and Permanent DentitionsDocument9 paginiEvaluation of Posttreatment Stability After Orthodontic Treatment in The Mixed and Permanent DentitionsElla GolikÎncă nu există evaluări
- Dynamic Smile Evaluation in Different Skeletal PatternsDocument7 paginiDynamic Smile Evaluation in Different Skeletal PatternsElla GolikÎncă nu există evaluări
- Effects of Miniplate Anchored and Conventional Forsus Fatigue Resistant DevicesDocument7 paginiEffects of Miniplate Anchored and Conventional Forsus Fatigue Resistant DevicesElla GolikÎncă nu există evaluări
- The Use of SPHARM-PDM and Mean Latitude Axis To Evaluate Airway ChangesDocument6 paginiThe Use of SPHARM-PDM and Mean Latitude Axis To Evaluate Airway ChangesElla GolikÎncă nu există evaluări
- Facial Soft-Tissue Changes After Rapid Maxillary ExpansionDocument9 paginiFacial Soft-Tissue Changes After Rapid Maxillary ExpansionElla GolikÎncă nu există evaluări
- Next Door Solutions To Domestic Violence: Facts & FiguresDocument20 paginiNext Door Solutions To Domestic Violence: Facts & FiguresecopperÎncă nu există evaluări
- Braverman Personality Type Assessment - Online TestDocument16 paginiBraverman Personality Type Assessment - Online TestKomkor GuyÎncă nu există evaluări
- Centering Before SessionDocument9 paginiCentering Before SessionJuanaÎncă nu există evaluări
- Policies Reporting Notifiable DiseasesDocument4 paginiPolicies Reporting Notifiable DiseasesJanPaolo TorresÎncă nu există evaluări
- The Prediction of Preeclampsia The Way Forward 20Document14 paginiThe Prediction of Preeclampsia The Way Forward 20Ecaterina Sorto de ArgeñalÎncă nu există evaluări
- BS BuzzDocument8 paginiBS BuzzBS Central, Inc. "The Buzz"Încă nu există evaluări
- FluconazoleDocument4 paginiFluconazoleeucaÎncă nu există evaluări
- Enf Tiroidea y Embarazo Lancet 2018Document12 paginiEnf Tiroidea y Embarazo Lancet 2018Jair Alexander Quintero PanucoÎncă nu există evaluări
- Everything Can Cause Stress: Big Events, Daily Hassles & Life ChangesDocument4 paginiEverything Can Cause Stress: Big Events, Daily Hassles & Life ChangesOkello StevenÎncă nu există evaluări
- Parcare Assessment MaxillofacialDocument22 paginiParcare Assessment Maxillofacialqta omerÎncă nu există evaluări
- SHENAAZ Surgical Chronicles - Final VersionDocument6 paginiSHENAAZ Surgical Chronicles - Final VersionSumayyah EbrahimÎncă nu există evaluări
- Plant and Equipment Risk Assessment Fgoc - NewDocument12 paginiPlant and Equipment Risk Assessment Fgoc - Newmajid khanÎncă nu există evaluări
- Final Draft - Sleep EssayDocument11 paginiFinal Draft - Sleep Essayapi-609533757Încă nu există evaluări
- JSA Erection of Steel StructureDocument9 paginiJSA Erection of Steel StructureOvais FarooqÎncă nu există evaluări
- Spiritual Health Teaching for Mrs. JDocument2 paginiSpiritual Health Teaching for Mrs. Jcayla mae carlosÎncă nu există evaluări
- Section E - Problems Facing The Aged PDFDocument6 paginiSection E - Problems Facing The Aged PDFMoses OntitaÎncă nu există evaluări
- AM-Clad DATA SHEET PVC Ceilings Jan 2021Document4 paginiAM-Clad DATA SHEET PVC Ceilings Jan 2021Job AÎncă nu există evaluări
- Paper Grommet THT KntdeDocument15 paginiPaper Grommet THT KntdeSunu Bintan GifariÎncă nu există evaluări
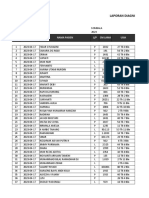
- Laporan Diagnosa Pasien Harian: Puskesmas: TanggalDocument9 paginiLaporan Diagnosa Pasien Harian: Puskesmas: TanggalRamlawatiÎncă nu există evaluări
- Decort AmpDocument7 paginiDecort AmpDr.2020Încă nu există evaluări
- Model Edukasi Postnatal Melalui Pendekatan FamilyDocument19 paginiModel Edukasi Postnatal Melalui Pendekatan FamilyAgustina VivoÎncă nu există evaluări
- Zesthomas Zapanta VUCA ActivityDocument1 paginăZesthomas Zapanta VUCA ActivityNederysiad ManuelÎncă nu există evaluări
- Graph Data Analysis AEUK ExampleDocument8 paginiGraph Data Analysis AEUK ExampleHuỳnh Xuân NhiÎncă nu există evaluări
- Riphah University PhysiosDocument3 paginiRiphah University PhysiosSalman KhanÎncă nu există evaluări
- Evidence Map of Cupping Therapy: Clinical MedicineDocument13 paginiEvidence Map of Cupping Therapy: Clinical MedicineBence KlusóczkiÎncă nu există evaluări
- Parents Evaluation of Aural Performance of Children (PEACH) v.4Document2 paginiParents Evaluation of Aural Performance of Children (PEACH) v.4Gwyneth PañaÎncă nu există evaluări