Documente Academic
Documente Profesional
Documente Cultură
Basic Renal Notes
Încărcat de
yannie.s.liDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Basic Renal Notes
Încărcat de
yannie.s.liDrepturi de autor:
Formate disponibile
Monday, May 4
Self-study: Homeostasis
Homeostasis maintenance of static or constant conditions
in the internal environment
Body fluid volume and composition are kept
relatively stable during steady state.
Fluid intake is highly variable. Thus, fluid output
must be carefully regulated to match it.
Total body water
~60% of body weight is water
Body water is distributed through body tissues:
o Muscle (43%), skeleton (16%), adipose
(10%), other organs (6%)
The distribution of water within tissues also varies
o Muscle/Organs (75%), skeleton (22%),
adipose (<10%)
There is an inverse relationship of body fat
percentage and total body water percentage
Body Fluid Balance
Intake should equal output
Intake consists of food and drink (~2000 mL/day)
and that generated from oxidative metabolism (~300
mL/day).
Output consists of urine (major), insensible water
loss (perspiration from skin/lung, more in burn
patients; sweat, more with exercise), and feces
(excessive in diarrhea).
The kidney is one of the most important regulatory
organs for fluid and metabolic waste balance.
Kidney Function
A. Basic function
1. Regulate water and inorganic ion balance
2. Remove metabolic waste products via urine
excretion (urea, uric acid, creatinine)
3. Remove foreign chemicals via urine (pesticides,
food additives)
B. Acid base balance
C. Secrete hormones
1. EPO (RBC production)
2. 1,25-dihydroxyvitamin D3 (Ca/Ph balance)
3. RAAS renin (Na balance)
D. Gluconeogenesis (fasting glucose maintenance)
Fluid compartments
A. Living things are open systems (in contact with
external environment; e.g. lung, kidney, GI, skin)
B. Two major fluid compartments
1. Intracellular fluid (ICF) in cells, 40% of BW
(~25L)
a. Composition is similar across all organisms
2. Extracellular fluid (ECF) 20% BW (15L)
a. Plasma fluid in blood vessels (1/4: 3 L)
b. Interstitial fluid (ISF) fluid outside
vessels (3/4: 12 L)
3. 60-40-20 rule
a. 60% total, 40% ICF, 20% ECF (15% ISF,
5% plasma)
C. Blood volume
1. 8% of BW (5 L)
a. 60% plasma, 40% RBC
D. Barriers
1. Capillaries separate plasma from ISF
a. Highly permeable, except to proteins; thus,
plasma is protein rich
2. Cell membrane separate ICF from ECF
a. Semi-permeable
Composition of Body fluids
A. Ionic composition of ECF (plasma and ISF) is
similar since capillary wall is highly permeable
1. Major cation: Na+
2. Major anions: Cl-, HCO33. Protein is impermeable across capillaries more
in plasma
a. Gibbs Donnan effect Na+ is 2% greater in
plasma (vs. ISF) due to negatively charged
proteins; Cl- is lower
B. Ionic composition of ICF
1. Major cations: K+, Mg2+
2. Major anions: proteins, inorganic phosphates
Measurement of body fluid compartments
A. Dilution principle
1. V=Adye/Cfinal
2. Subtract volume of dye injected
B. Measuring plasma volume
1. Probe that avidly binds plasma proteins (e.g.
131
I-albumiin, Evans blue dye)
2. Use same equation from dilution principle
(where V=plasma volume)
3. Blood Volume = PV/(1-Hct)
C. Measure ECF
1. Probe that cannot enter cell (stays in ICF/ECF)
(e.g. inulin, thiosulfate, mannitol, Na+)
2. Same equation (where V = ECF volume)
3. ISF = ECF- PV
4. Correct for urinary excretion of probe by
subtracting excreted probe amount from
injected amount
D. Measure Total Body Water
1. Probe that goes everywhere (e.g. 2H2O, 3H2O,
antipyrene)
2. Same equation, V = TBW
3. ICF = TBW ECF
Factors that determine fluid movement between
compartments
A. Between plasma and IF
1. Capillary filtration
a. Hydrostatic, oncotic pressures
B. Between ICF and ECF
1. Osmosis, based on permeability
a. Water, urea, sodium, glycerol
-Osmosis Net diffusion of water from region of high
water concentration to region of low water concentration
-Osmolarity based on number of particles after a mole of
something dissociates into L
A. Osmolarity of body fluids in different
compartments is the same (overall balance of solute
osmolarities)
B. Impermeable solutes: hypotonic causes RBC
swelling, hypertonic causes RBC shrinking
C. Permeable solutes (urea): things happen.
D. Slowly permeable solutes (glycerol): things happen.
-Osmolality based on number of particles after a mole of
something dissociates into kg
-Osmotic pressure pressure required to prevent the
osmosis; directly proportional to the concentration of
osmotically active particles, not their size
Dehydration
A. Decrease volume, increase osmolarity (normal is
290 mOsm)
Plasma Osmolarity
A. Plasma Osmolarity: (Glc/BUN can normally be
approximated by adding 10; the conversion factors
are for mg/dLmOsm/L)
2. Dehydration due to water deprivation only
water lost, NaCl retained:
a. Give isotonic glucose or hypotonic saline
with glucose
D. Osmolarity Gap difference between osmolarity
and osmolality: there is something making the
difference (EtOH, MeOh, etc.)
1. A gap of >10 is abnormal
2. Method: freezing point depression is preferred
Changes
A. Isosmotic volume expansion
1. Causes: isotonic saline infusion in clinic
2. Increase ECF volume, maintain Osm
3. No change in ICF volume or Osm
B. Hyposmotic volume expansion (gain of water)
1. Causes: SIADH, drinking water, nutritive
glucose soln. infusion
2. Volume increase in all compartments
3. Decrease Osm in all compartments
4. Hematocrit unchanged: RBC concentration
decreases, but cell volume increases
proportionally
C. Hyperosmostic volume expansion (Gain of salt)
1. Causes: dry NaCl consumption, hypernatremia
2. Water shifts from ICF to ECF, resulting in a
higher (but equal) osmolarity for both
3. Plasma protein concentration and hematocrit
both decrease due to increased ECF volume
B. How much to infuse?
1. Use original body weight, calculate TBW
2. Calculate current TBW
3. Find the difference, infuse
C. What to infuse?
1. Water? Saline? Isotonic glucose? Hypotonic
saline with glucose?
D. Hyposmotic volume contraction (Loss of NaCl)
1. Causes: adrenal insufficiency (aldosterone
deficiency, hyponatremia), drinking water after
profuse sweating
2. ECF osmolarity transiently decreases.
3. Water shifts from ECF to ICF.
4. Plasma protein concentration and hematocrit
both increase due to decreased ECF volume
(and increased RBC volume)
E. Infusion of isotonic urea
1. Increase volume of all compartments
2. No change in Osm
3. No change in RBC size
Algorithm for osmotic disturbances
1) Identify any changes occurring in ECF (solute added?
Water lost?)
2) Decide how ECF osmolarity is affected (incr, decr, none)
3) If there is a change, determine if water will shift into or
out of cells to reestablish equilibrium between ECF and ICF
osmolarity. (If no change in ECF osmolarity, a water shift
will not occur. And vice versa.)
Self-study: Renal Function Tests
Mass balance is key.
Total Body
A. Output = Intake + production metabolism
Kidney
B. Input (arterial) = Output (venous, lymph, urine)
Nephron
C. Excretion = Filtration Reabsorption + Secretion
Quantitative Analysis of Renal Function
A. GFR rate of filtration of plasma into Bowmans
capsule of the glomerulus; indicator of renal
function
1. Loss of glomeruli due to sclerosis and
destruction hinders GFR
2. Inulin as a model (not produced, metabolized,
secreted, or reabsorbed; just excreted in urine)
3. GFR = Vurine*Ci,urine/Ci,plasma = clearance (inulin)
B. Clearance rate at which a substance is cleared
from the plasma
C. Renal clearance - volume of plasma that is
completely cleared of a substance by kidneys per
unit time
D. Extraction Ratio percentage of substance removed
from plasma
1. X = [Ax-Vx]/Ax
E. Creatinine is the endogenous indicator of GFR
1. Produced by skeletal muscle metabolism
2. Shows a hyperbolic inverse relationship
S-ar putea să vă placă și
- Metabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentDe la EverandMetabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentCarole IchaiÎncă nu există evaluări
- Lec. 3 - Fluid and ElectrolyteDocument16 paginiLec. 3 - Fluid and Electrolyteمجيب سلطانÎncă nu există evaluări
- 3.14 Chapter 3 Water and Electrolytes Balance and ImblanceDocument140 pagini3.14 Chapter 3 Water and Electrolytes Balance and ImblanceShourav SarkarÎncă nu există evaluări
- Basic of Fluid Therapy ImaDocument69 paginiBasic of Fluid Therapy Imal Made ArtawanÎncă nu există evaluări
- Body FluidsDocument59 paginiBody FluidsAmmar SmadiÎncă nu există evaluări
- Regulation of Fluid and Electrolyte BalanceDocument43 paginiRegulation of Fluid and Electrolyte BalanceMsKizzyÎncă nu există evaluări
- Fluid Electrolyte and AcidBase BalanceDocument33 paginiFluid Electrolyte and AcidBase Balancemoncalshareen3Încă nu există evaluări
- Mabes Fluid and ElectrolytesDocument9 paginiMabes Fluid and ElectrolytesMabesÎncă nu există evaluări
- Kompartemen Cairan TubuhDocument27 paginiKompartemen Cairan Tubuhdalang leriÎncă nu există evaluări
- Water and Sodium 2024 PDFDocument61 paginiWater and Sodium 2024 PDFMpho MosehlaÎncă nu există evaluări
- Water and Electrolyte Balance: DR PreetiDocument116 paginiWater and Electrolyte Balance: DR PreetiSrishti GoenkaÎncă nu există evaluări
- Body Fluid: Presented BY DR (MRS) Okorie PDocument56 paginiBody Fluid: Presented BY DR (MRS) Okorie PKELECHI ELEJEÎncă nu există evaluări
- CH 25 of GuytonDocument7 paginiCH 25 of GuytonBea Samonte100% (2)
- Fluid and Electrolytes1Document7 paginiFluid and Electrolytes1Charl PabillonÎncă nu există evaluări
- Fluid, Electrolyte, Acid Base BalanceDocument42 paginiFluid, Electrolyte, Acid Base BalanceSutrisno YangÎncă nu există evaluări
- Fluids and ElectrolytesDocument9 paginiFluids and ElectrolytesaclumutÎncă nu există evaluări
- Lec 4Document32 paginiLec 4bosco kiuriaÎncă nu există evaluări
- S.No Table of Content Page NoDocument20 paginiS.No Table of Content Page NoTamilArasiÎncă nu există evaluări
- Fluids and Electrolytes Pathophysiology NursingDocument16 paginiFluids and Electrolytes Pathophysiology Nursinggrad_nurse_2015100% (3)
- Fluid N Electrolytes Balance - NDocument15 paginiFluid N Electrolytes Balance - NChandan SahÎncă nu există evaluări
- Fluid & Electrolyte Balance: Part 4: Regulation & MaintenanceDocument40 paginiFluid & Electrolyte Balance: Part 4: Regulation & MaintenanceMy MusicÎncă nu există evaluări
- 2012-Fluid and ElectrolytesDocument192 pagini2012-Fluid and Electrolyteskyuss2Încă nu există evaluări
- Total Body WaterDocument70 paginiTotal Body WaterZaara RashéidÎncă nu există evaluări
- Fluid and Electrolyte Balance: Presenter: Dr. Siyum Mathewos (Omfs-Ri) Modulator: Dr. Dereje (Omfs, Consultant)Document87 paginiFluid and Electrolyte Balance: Presenter: Dr. Siyum Mathewos (Omfs-Ri) Modulator: Dr. Dereje (Omfs, Consultant)Siyum MathewosÎncă nu există evaluări
- Fluids and Electrolytes FinalDocument50 paginiFluids and Electrolytes FinalOsego MokopotsaÎncă nu există evaluări
- Fluid & Electrolyte Imbalances FinalDocument142 paginiFluid & Electrolyte Imbalances FinalPriyanka T100% (3)
- 2022 Lecture 4 Body Fluids Compartments Na K 1 3Document49 pagini2022 Lecture 4 Body Fluids Compartments Na K 1 3Mariam ShenoudaÎncă nu există evaluări
- Liquidos y Electrolitos 2016Document5 paginiLiquidos y Electrolitos 2016MARIA JOSE MEDINA JAIMESÎncă nu există evaluări
- Body FluidDocument10 paginiBody FluidNwaoha Chibuzor AnthonyÎncă nu există evaluări
- F and 1Document51 paginiF and 1api-19641337Încă nu există evaluări
- Fluid and Electrolyte Imbalance PDFDocument21 paginiFluid and Electrolyte Imbalance PDFShafaq AlamÎncă nu există evaluări
- Fluid & ElectrolytesDocument85 paginiFluid & ElectrolytesAdarshBijapurÎncă nu există evaluări
- 1.1a Fluid Management 6th Seminar GRP AaDocument40 pagini1.1a Fluid Management 6th Seminar GRP AahalearnÎncă nu există evaluări
- Body Fluid 1Document55 paginiBody Fluid 1Anonymous z3afjyy1aÎncă nu există evaluări
- Fluid, Electrolyte, and Acid-Base BalanceDocument41 paginiFluid, Electrolyte, and Acid-Base BalanceRn nadeenÎncă nu există evaluări
- Body Fluida and Electrolytes PDFDocument31 paginiBody Fluida and Electrolytes PDFBeulah DasariÎncă nu există evaluări
- Fluid, Electrolyte, and Acid-Base BalanceDocument29 paginiFluid, Electrolyte, and Acid-Base BalancemeriiÎncă nu există evaluări
- Water and Electrolyte ImbalanceDocument17 paginiWater and Electrolyte Imbalancemhairat6043100% (1)
- Medical-Surgical Nursing 1Document28 paginiMedical-Surgical Nursing 1Maui Ting100% (1)
- F and e Imb .... Edu ..Document20 paginiF and e Imb .... Edu ..esakkiammalÎncă nu există evaluări
- Water LoseDocument29 paginiWater LoseJAKLIN EMPOLÎncă nu există evaluări
- Fluid and Electrolytes Lecture NotesDocument85 paginiFluid and Electrolytes Lecture NotesVince Peliño De MesaÎncă nu există evaluări
- 1a Introduction To SurgeryDocument109 pagini1a Introduction To SurgeryZllison Mae Teodoro MangabatÎncă nu există evaluări
- 02 - Body Fluids 2021Document33 pagini02 - Body Fluids 2021shabnam sajidaÎncă nu există evaluări
- 2012-Fluid and ElectrolytesDocument192 pagini2012-Fluid and ElectrolytesHarley Justiniani Dela CruzÎncă nu există evaluări
- Body Fluid, MML, 2021Document51 paginiBody Fluid, MML, 2021Boon AimanÎncă nu există evaluări
- WaterDocument16 paginiWaterAUBREY LISAYENÎncă nu există evaluări
- Body Fluids Hbc202-Lecture Notes-1Document9 paginiBody Fluids Hbc202-Lecture Notes-1Shreya AnandÎncă nu există evaluări
- Keseimbangan Cairan TubuhDocument60 paginiKeseimbangan Cairan TubuhoktavianyÎncă nu există evaluări
- 13) Body FluidsDocument20 pagini13) Body FluidsyohdeforemostÎncă nu există evaluări
- Fluid Volume BalanceDocument73 paginiFluid Volume BalanceSalman HabeebÎncă nu există evaluări
- Body FluidDocument15 paginiBody FluidrjÎncă nu există evaluări
- Body Fluids (Eng)Document27 paginiBody Fluids (Eng)Desmy FadillahÎncă nu există evaluări
- Fluids and ElectrolytesDocument7 paginiFluids and ElectrolytessetanpikulanÎncă nu există evaluări
- Fluid, Electrolyte, and Acid-Base Balance: Prepared by Janice Meeking, Mount Royal CollegeDocument96 paginiFluid, Electrolyte, and Acid-Base Balance: Prepared by Janice Meeking, Mount Royal CollegeRajesh KumarÎncă nu există evaluări
- Fluids and Electrolytes NCM 101Document142 paginiFluids and Electrolytes NCM 101France John Evangelista Torres100% (2)
- Fluid BalanceDocument50 paginiFluid Balancesiti sarahdeazÎncă nu există evaluări
- BODY Weight 100%: Balance/Imbalances & TherapyDocument11 paginiBODY Weight 100%: Balance/Imbalances & TherapyVictoria Castillo TamayoÎncă nu există evaluări
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDe la EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsÎncă nu există evaluări
- Engineering Project ListDocument25 paginiEngineering Project ListSyed ShaÎncă nu există evaluări
- Those With MoonDocument1 paginăThose With MoonRosee AldamaÎncă nu există evaluări
- Money Tree International Finance Corp. Checklist of Standard Loan RequirementsDocument2 paginiMoney Tree International Finance Corp. Checklist of Standard Loan RequirementsAgape LabuntogÎncă nu există evaluări
- Paper Specific Instructions:: GATE Chemical Engineering MSQ Paper - 1Document11 paginiPaper Specific Instructions:: GATE Chemical Engineering MSQ Paper - 1Mayank ShelarÎncă nu există evaluări
- Adenoid HypertrophyDocument56 paginiAdenoid HypertrophyWidi Yuli HariantoÎncă nu există evaluări
- Business Plan Example - Little LearnerDocument26 paginiBusiness Plan Example - Little LearnerCourtney mcintosh100% (1)
- 41 Assignment Worksheets For SchoolDocument26 pagini41 Assignment Worksheets For Schoolsoinarana456Încă nu există evaluări
- Offender TypologiesDocument8 paginiOffender TypologiesSahil AnsariÎncă nu există evaluări
- Laboratory Cold ChainDocument22 paginiLaboratory Cold ChainEmiÎncă nu există evaluări
- Starkville Dispatch Eedition 9-10-20Document12 paginiStarkville Dispatch Eedition 9-10-20The DispatchÎncă nu există evaluări
- Inlet Manifold Pressure - Test: Testing and AdjustingDocument2 paginiInlet Manifold Pressure - Test: Testing and AdjustingAbdoulaye Boua BERTHEÎncă nu există evaluări
- Kyocera Fleet Services White Paper: SecurityDocument20 paginiKyocera Fleet Services White Paper: SecurityHoratiu OanaÎncă nu există evaluări
- SPA - MichaelDocument1 paginăSPA - Michaelgilberthufana446877Încă nu există evaluări
- Recruitement Process - Siemens - Sneha Waman Kadam S200030047 PDFDocument7 paginiRecruitement Process - Siemens - Sneha Waman Kadam S200030047 PDFSneha KadamÎncă nu există evaluări
- API 510 Practise Question Nov 07 Rev1Document200 paginiAPI 510 Practise Question Nov 07 Rev1TRAN THONG SINH100% (3)
- DOWSIL™ 2-9034 Emulsion: Features & BenefitsDocument5 paginiDOWSIL™ 2-9034 Emulsion: Features & BenefitsLaban KantorÎncă nu există evaluări
- Conference Version of SB 1Document486 paginiConference Version of SB 1Paul MastersÎncă nu există evaluări
- Dungeon World ConversionDocument5 paginiDungeon World ConversionJosephLouisNadeauÎncă nu există evaluări
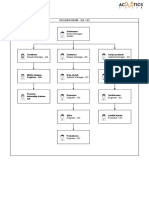
- Organogram - Qa / QC: Srinivasan SrinivasanDocument4 paginiOrganogram - Qa / QC: Srinivasan SrinivasanGowtham VenkatÎncă nu există evaluări
- Keratoconjunctivitis Sicca FinalDocument91 paginiKeratoconjunctivitis Sicca FinalJanki GajjarÎncă nu există evaluări
- Chapter Three Liquid Piping SystemDocument51 paginiChapter Three Liquid Piping SystemMelaku TamiratÎncă nu există evaluări
- Indian Standard (First Revision) : Method of Chemical Analysis of Hydraulic CementDocument44 paginiIndian Standard (First Revision) : Method of Chemical Analysis of Hydraulic CementArijit dasguptaÎncă nu există evaluări
- Jun Judging ClinicDocument1 paginăJun Judging Cliniccsponseller27Încă nu există evaluări
- ATI Respiratory PowerpointDocument90 paginiATI Respiratory PowerpointAnn KelseaÎncă nu există evaluări
- Care of Clients With Problems in OxygenationDocument5 paginiCare of Clients With Problems in OxygenationSkyla FiestaÎncă nu există evaluări
- Castle 1-3K E ManualDocument26 paginiCastle 1-3K E ManualShami MudunkotuwaÎncă nu există evaluări
- Lab Manual PDFDocument68 paginiLab Manual PDFSantino AwetÎncă nu există evaluări
- Chewable: Buy Pepcid AC Packages, Get Pepcid AC 18'sDocument2 paginiChewable: Buy Pepcid AC Packages, Get Pepcid AC 18'sMahemoud MoustafaÎncă nu există evaluări
- Blueprint Huynh My Ky Duyen 2022 McDonald'sDocument2 paginiBlueprint Huynh My Ky Duyen 2022 McDonald'sHuỳnh Mỹ Kỳ DuyênÎncă nu există evaluări
- Mil STD 792fDocument13 paginiMil STD 792fdoradoanÎncă nu există evaluări