Documente Academic
Documente Profesional
Documente Cultură
Jurnal RAS
Încărcat de
Linde RendDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Jurnal RAS
Încărcat de
Linde RendDrepturi de autor:
Formate disponibile
American Journal of OtolaryngologyHead and Neck Medicine and Surgery 27 (2006) 229 232
www.elsevier.com/locate/amjoto
Recurrent aphthous stomatitis: investigation of possible etiologic factors
Serap Koybasi, MDa,4, Ali Haydar Parlak, MDb, Erdinc Serin, MDc,
Fahrettin Yilmaz, MDa, Didem Serin, MDd
a
Department of Otolaryngology, Abant Izzet Baysal University, Izzet Baysal Faculty of Medicine, Bolu, Turkey
b
Department of Dermatology, Abant Izzet Baysal University, Izzet Baysal Faculty of Medicine, Bolu, Turkey
c
Department of Biochemistry, Abant Izzet Baysal University, Izzet Baysal Faculty of Medicine, Bolu, Turkey
d
Department of Ophthalmology, Abant Izzet Baysal University, Izzet Baysal Faculty of Medicine, Bolu, Turkey
Received 17 August 2005
Abstract
Objective: To investigate the association of serum vitamin B12, folic acid, iron, calcium, magnesium,
and phosphorus levels as well as family history and cigarette smoking with recurrent aphthous
stomatitis (RAS).
Methods: Thirty-four patients with RAS and 32 control subjects were included in this controlled
prospective screening study. Both groups received a questionnaire, and serum screening tests were
performed. The collected data were analyzed using v 2 test and binary logistic regression analysis.
Results: Family history was found to be the most significant predisposing factor for RAS among the
investigated ones. Regarding the serum tests, only vitamin B12 was found to have significant
correlation with RAS. Patients with vitamin B12 deficiency, positive family history, and nonsmoking
status have been found to have the highest risk for having RAS.
Conclusions: RAS is a multifactorial disease. Positive family history, vitamin B12 deficiency, and
nonsmoking status are among the important predisposing factors.
D 2006 Elsevier Inc. All rights reserved.
1. Introduction
Recurrent aphthous stomatitis (RAS) is one of the most
common oral diseases worldwide. The prevalence ranges
from 2% to 66% in different populations [1,2]. RAS is a
disease characterized by recurring ulcers in the oral mucosa
without any sign of other diseases. Aphthous ulcers are
painful and shallow ulcers, usually covered with a grayish
white pseudomembrane that is surrounded by an erythematous margin. Recurrent aphthous ulcers arise on nonkeratinized oral mucosa such as lateral margins of the tongue and
buccal and labial mucosa.
RAS is classified according to clinical characteristics
of the ulcers as minor ulcers, major ulcers, and herpetiform ulcers. The most common type is RAS with minor
ulcers and comprises approximately 80% of the cases. In
4 Corresponding author. Department of Otolaryngology, Abant Izzet
Baysal University, Izzet Baysal Faculty of Medicine, Bolu 14280, Turkey.
Tel.: +90 374 253 4656; fax: +90 374 253 4615.
E-mail address: serapkoybasi@yahoo.com (S. Koybasi).
0196-0709/$ see front matter D 2006 Elsevier Inc. All rights reserved.
doi:10.1016/j.amjoto.2005.09.022
this type, the ulcers are less than 1 cm in diameter,
round, clearly defined, and painful ulcers and heal within
10 to 14 days without scarring. In major RAS (Sutton
disease), painful lesions are more than 1 cm in diameter,
may last for weeks, and usually heal with scar formation.
The herpetiform aphthous stomatitis, the least common
type, presents itself as multiple clusters of pinpoint lesions
that may give rise to large irregular ulcers lasting 7 to
10 days [3].
Although there are many factors accused in the etiology
of RAS, we still need to seek for more accurate and strong
statements regarding the etiology because of the contradictory literature and for patients benefit.
In this prospective study, we aimed to investigate
possible roles of predisposing factors for RAS. These
included family history, cigarette smoking, and serum tests.
Serum tests included vitamin B12, folic acid, iron (Fe++),
Fe++ saturation levels, total iron-binding capacity (TIBC),
ferritin, calcium (Ca++), magnesium (Mg++), and phosphorus (P) levels. Complete blood count with hemoglobin and
hematocrit levels was also performed.
230
S. Koybasi et al. / American Journal of OtolaryngologyHead and Neck Medicine and Surgery 27 (2006) 229 232
2. Materials and methods
Thirty-four patients with a diagnosis of RAS with
recurrent minor ulcers were included in this study.
The control group was composed of 32 healthy volunteers
without oral aphthae history and undergoing preoperative
blood tests for septoplasty operation with a diagnosis of
nasal septal deviation. After obtaining an informed consent
(according to principles outlined in the Declaration of
Helsinki), both groups were given a questionnaire about
the disease. Questionnaire included age, sex, smoking status,
family history, and systemic disorders. Both groups were
acknowledged about the disease and asked if any of
their family members had the symptoms. In addition, the
patient group was asked about the frequency and duration of the disease and the ulcers. Family history was
accepted positive in case of the presence of the disease in at
least one first-degree relative. Patients who smoked more
than 1 cigarette on regular daily basis were accepted as
active smokers.
In addition to otolaryngological examination, dermatologic and ophthalmologic examinations were made for
exclusion purposes. Pathergy test and antinuclear antibody
tests were performed to rule out possible coexisting systemic disease; patients with Behcet disease or gastrointestinal symptoms were not included in the study.
Complete blood count and the levels of vitamin B12, folic
acid, Ca++, Mg++, P, Fe++, Fe++ saturation level, TIBC, and
ferritin were investigated. The tests were performed in
serum collected after an overnight fast.
The results were evaluated using v 2 test and binary
logistic regression analysis.
3. Results
Patient group was composed of 34 patients with 17 men
and 17 women, and the control group was composed of
32 individuals with 13 men and 19 women. Age ranged
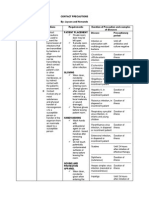
Fig. 1. Summary of the effect of studied predisposing factors for RAS in
relation with vitamin B12. As clearly seen, patients with low vitamin B12
level, positive family history, and nonsmoking status had the highest risk
for having RAS.
Table 1
Among the serum tests performed, only vitamin B12 was found to have a
statistically significant correlation with RAS ( P = .028).
Serum tests
Group
Mean
SD
Vitamin B12
Disease
Control
Disease
Control
Disease
Control
Disease
Control
Disease
Control
Disease
Control
Disease
Control
Disease
Control
Disease
Control
Disease
Control
Disease
Control
245.5
294.0
8.756
8.658
67.82
71.16
21.97
22.88
359.21
333.6
68.5
53.51
13.532
13.419
40.06
38.37
9.4412
9.6031
2.1765
2.0844
3.203
3.2719
97.9
80.0
4.422
3.172
33.41
31.98
10.50
13.53
50.18
66.0
61
49.48
2.046
1.543
6.36
7.31
0.3775
0.4748
0.2090
0.2142
0.696
0.5607
.028
Folic acid
Fe++
Fe++ saturation
TIBC
Ferritin
Hemoglobin
Hematocrit
Ca++
Mg++
P
.916
.675
.757
.074
.267
.797
.303
.122
.074
.654
between 10 and 66 years with a mean of 36.7 years in the
patient group and between 11 and 74 years in the control
group with a mean of 34.3 years. We did not show any
significant influence of age or sex on RAS (binary logistic
regression analysis, P N .05).
The most striking result was the influence of family
history on RAS. The rates of positive family history in
patient and control group were 54.2% and 9%, respectively.
In the presence of family history, we found a statistically
significant risk for having RAS (v 2 = 16.8, P b .001).
According to our laboratorys normal range (200835 pg/mL), we found 12 (35.2%) of 34 patients to be
deficient in vitamin B12, whereas in the control group, none
of the patients had vitamin B12 deficiency. Binary logistic
regression analysis revealed a significant relationship
between vitamin B12 and RAS probability ( P = .028).
As far as smoking was considered, 8 (20%) of 34 patients
were smokers in the patient group compared with 14 smokers
(43.7%) in the control group; v 2 test revealed a borderline
significance level (v 2 = 3.73, P = .052) concerning RAS and
smoking status.
When considered together, the influence of family
history, vitamin B12 deficiency, and cigarette smoking on
RAS probability was calculated to be statistically significant using binary logistic regression analysis ( P b
.001). This finding was summarized in Fig. 1. The nonsmoking patients with positive family history and vitamin
B12 deficiency were found to have the grater risk for
having RAS.
Folic acid, Ca++, Mg++, P, Fe++, Fe++ saturation level,
TIBC, ferritin, hemoglobin, and hematocrit levels were
found to have some degree of correlation with RAS, which
S. Koybasi et al. / American Journal of OtolaryngologyHead and Neck Medicine and Surgery 27 (2006) 229 232
were not statistically significant (binary logistic regression
analysis, P N .05). Results of these evaluations were
summarized in Table 1.
We studied the frequency and duration of the aphthous
lesions and whether they were related to family history,
vitamin B12 deficiency, or cigarette smoking. We could not
show any significant relation between these parameters and
RAS (binary logistic regression analysis P N .05).
4. Discussion
Morbidity is quite high in RAS; quality of life of RAS
patients is affected in that the recurrent and painful intraoral
mucosal lesions and increased salivation give discomfort
while eating, drinking, and speaking. Because the exact
etiology of RAS is still unknown, most patients with RAS are
usually given some medications to relieve their pain only,
instead of an etiologic screening and curative treatment.
RAS may be associated with several diseases such as
Behcet disease, gluten-sensitive enteropathy, pernicious
anemia, cyclic neutropenia, inflammatory bowel disease,
and FAPA (periodic fever, aphthous stomatitis, pharyngitis,
and adenitis). Despite extensive investigations, studies have
failed to find the exact etiology and pathophysiology of
RAS. Heredity, hemanitic deficiencies, immune dysregulation, some foods, drugs, stress, local trauma, hormonal
disturbances, infections, smoking habits, and poor oral
hygiene are proposed factors [4-8].
A high incidence of aphthous stomatitis was reported by
Miller et al [8] in identical twins compared with nonidentical twins (90% vs b 60%). Miller et al [9], in their study,
indicated an increased susceptibility to RAS among children
of RAS-positive parents. Shohat-Zabarski [10] reported that
more than 42% of RAS patients had first-degree relatives
with RAS. In our series, we found positive family history
in 54.2% of the patients. Whether this high degree of
association is because of a direct genetic influence or similar
social status, traditions, or habits of the family members is
not known yet. Among the predisposing factors we could
study, we found family history to have the strongest
correlation with RAS ( P b .001).
Serum vitamin status is another proposed predisposing
factor for RAS, and it has been shown that up to 20% of RAS
patients may have at least one hemanitic deficiency [5,11-13].
In our study, we found 12 (35.2%) of 34 patients to be
deficient in vitamin B12 according to our laboratorys normal
range comparing with none in the control group ( P b .05).
Palopoli and Waxman [12] proposed that the diseases
commonly associated with RAS do this through diminishing
intestinal absorption of vitamin B12, resulting in vitamin B12
deficiency. The question is how vitamin B12 deficiency
causes RAS. So far, this issue remained unclear, but the
dramatic response to vitamin B12 replacement therapy and
higher incidence of RAS in cases that have vitamin B12
deficiency suggest a direct role of this vitamin on the
pathogenesis of RAS [6,11,14,15].
231
Cigarette smoking is known to have a protective effect
on RAS. This protective effect of smoking may be related to
the increased keratinization of the oral mucosa in smokers.
Keratin layer may possibly act as a mechanical and chemical
barrier of the oral mucosa against minor traumas or
microbial agents [16]. Recurrent ulcerations were prevented
with the use of 8-mg 7-day Nicorette tablets [17]. In our
study, we found 20% active smokers (7 patients) in the RAS
group versus 43.7% (14 patients) in the control group
( P = .052). This finding, although not statistically
significant enough, is concurrent with the literature
[16,18]. The data about the protective effect of tobacco
are limited and need further studies.
Iron deficiency is another proposed predisposing factor
for RAS [5]. Porter et al [19], in their study, have shown a
significantly lower serum ferritin level (11.6%) in RAS
patients compared with control group (4.9%). However,
Wray et al [15] reported Fe++ deficiency to be very rare
among patients with recurrent ulcerations. They also
claimed that RAS patients with Fe++ deficiency respond in
a longer period to replacement therapy with Fe++, compared
with replacement with vitamin B12 and folic acid which they
attributed to the difficulty in reconstituting body stores of
Fe++. Others failed to demonstrate an association of Fe++
deficiency with RAS [6,20]. Results of our study did not
show a direct association of the disease neither with serum
Fe++, Fe++ saturation level, ferritin, nor hemoglobin and
hematocrit levels, but with TIBC, although statistically not
significant ( P = .074).
The association of RAS with the predisposing factors
found to be significant was summarized in Fig. 1. The
highest occurrence of RAS was found to be in nonsmoking
patients with a positive family history and vitamin B12
deficiency. Obviously, among these 3 factors, only vitamin
B12 deficiency might be overcome by replacement therapy
as we could not change the family history or encourage
patients to smoke.
Previous studies proposed possible etiologic roles of folic
acid and minerals [5,15]. However, there are studies that
deny such a relationship between RAS and folic acid [20].
Our attempts to find such an association between serum
folic acid, Ca++, Mg++, or P levels with RAS have failed.
This may be attributed to regional differences of our
patients, but we think that this issue should be studied
further with a larger multicenter series.
Taking all these findings into consideration, we can
clearly state that RAS is a multifactorial disease, and we can
conclude that positive family history, vitamin B12 deficiency, and smoking status are among the studied possible
etiologic factors.
References
[1] Axell T, Henricson V. The occurrence of recurrent aphthous stomatitis
in adult Swedish population. Acta Odontol Scand 1985;43:121 - 5.
[2] Ship II. Epidemiological aspects of recurrent aphthous ulcerations.
Oral Surg 1972;33:400 - 6.
232
S. Koybasi et al. / American Journal of OtolaryngologyHead and Neck Medicine and Surgery 27 (2006) 229 232
[3] Ship JA. Recurrent aphthous stomatitis. An update. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 1996;81:141 - 7.
[4] Ogura M, Yamamoto T, Morita M, et al. A case control study on food
intake of patients with recurrent aphthous stomatitis. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 2001;91:45 - 9.
[5] Nolan A, Lamey P-J, Milligan KA, et al. Recurrent aphthous
stomatitis and food sensitivity. J Oral Pathol Med 1991;20:473 - 5.
[6] Piskin S, Syan C, Durukan N, et al. Serum iron, ferritin, folic acid and
vitamin B12 levels in recurrent aphthous stomatitis. J Eur Acad
Dermatol Venereol 2002;16:66 - 7.
[7] Scully C, Gorsky M, Lozada-Nur F. Aphthous ulcerations. Dermatol
Ther 2002;15:185 - 205.
[8] Miller MF, Garfunkel AA, Ram C, et al. Inheritance patterns in
recurrent aphthous ulcers: twin and pedigree data. Oral Surg Oral Med
Oral Pathol 1977;43:886 - 91.
[9] Miller MF, Garfunkel AA, Ram CA, et al. The inheritance of recurrent
aphthous stomatitis. Observations on susceptibility. Oral Surg 1980;
94:18 - 23.
[10] Shohat-Zabarski R, Kalderon S, Klein T, et al. Close association of
HLA-B51 in persons with recurrent aphthous stomatitis. Oral Surg
Oral Med Oral Pathol 1992;74:463 - 5.
[11] Weusten BLAM, Wiel AV. Aphthous ulcers and vit B12 deficiency.
Neth J Med 1998;53:172 - 5.
[12] Palopoli J, Waxman J. Recurrent aphthous stomatitis and vitamin B12
deficiency. South Med J 1990;83:475 - 7.
[13] Wray D, Ferguson MM, Hutcheon AW, et al. Nutritional deficiencies
in recurrent aphthae. J Oral Pathol 1978;7:418 - 23.
[14] Nolan A, McIntosh WB, Allam BF, et al. Recurrent aphthous
ulceration: vitamin B1, B2 and B6 status and response to replacement
therapy. J Oral Pathol Med 1991;20:389 - 91.
[15] Wray D, Ferguson MM, Mason DK, et al. Recurrent aphthae:
treatment with vitamin B12, folic acid, and iron. Br Med J 1975;2:
490 - 3.
[16] Shapiro S, Olson DL, Chellimi SJ. The association between smoking and aphthous ulcers. Oral Surg Oral Med Oral Pathol 1970;30:
624 - 30.
[17] Bittoun R. Recurrent aphthous ulcers and nicotine. Med J Aust
1991;154:471 - 2.
[18] Tuzun B, Wolf R, Tuzun Y, et al. Recurrent aphthous stomatitis and
smoking. Int J Dermatol 2000;39:358 - 60.
[19] Porter SR, Scully C, Flint S. Hematologic status in recurrent aphthous
stomatitis compared with other oral diseases. Oral Surg Oral Med Oral
Pathol 1988;66:41 - 4.
[20] Olson JA, Feinberg I, Silverman S, et al. Serum vitamin B12 folate
and iron levels in recurrent aphthous ulceration. Oral Surg 1982;54:
517 - 20.
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
S-ar putea să vă placă și
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- 7 Health Benefits of CoffeeDocument9 pagini7 Health Benefits of CoffeeMaru PabloÎncă nu există evaluări
- APPROACH TO MANAGING JOINT PAINDocument44 paginiAPPROACH TO MANAGING JOINT PAINKavya Anoop100% (1)
- Congenital Hip DislocationDocument6 paginiCongenital Hip DislocationPaola CamainÎncă nu există evaluări
- Obg MCQSDocument11 paginiObg MCQSShriyansh ChaharÎncă nu există evaluări
- Mosbys Child Health Nursing 1Document62 paginiMosbys Child Health Nursing 1Darren VargasÎncă nu există evaluări
- MECONIUM Aspiration SyndromeDocument37 paginiMECONIUM Aspiration SyndromekamalaÎncă nu există evaluări
- Tension PneumothoraxDocument4 paginiTension PneumothoraxMichael MikuruÎncă nu există evaluări
- Appi Ajp 2008 08020272Document6 paginiAppi Ajp 2008 08020272andrei crisnicÎncă nu există evaluări
- Dis Mumps Color OfficeDocument2 paginiDis Mumps Color OfficeLinde RendÎncă nu există evaluări
- Jurnl Inrt 6 PDFDocument18 paginiJurnl Inrt 6 PDFNurhayati Al AzharÎncă nu există evaluări
- PTSD Combat VeteranDocument7 paginiPTSD Combat VeteranLinde RendÎncă nu există evaluări
- ProQuestDocuments 2015-09-11Document10 paginiProQuestDocuments 2015-09-11Linde RendÎncă nu există evaluări
- Global Immunization DataDocument4 paginiGlobal Immunization DataLinde RendÎncă nu există evaluări
- Aspirin in Patient Non Cardiac SurgeryDocument10 paginiAspirin in Patient Non Cardiac SurgeryagisagitaÎncă nu există evaluări
- Dis Mumps Color OfficeDocument2 paginiDis Mumps Color OfficeLinde RendÎncă nu există evaluări
- Infark Miokard Dengan Elevasi STDocument34 paginiInfark Miokard Dengan Elevasi STLinde RendÎncă nu există evaluări
- Tugas Jurding Radiologi (Debbiecindew)Document40 paginiTugas Jurding Radiologi (Debbiecindew)Linde RendÎncă nu există evaluări
- Tugas Jurding Anestesi (Debbiecindew)Document34 paginiTugas Jurding Anestesi (Debbiecindew)Linde RendÎncă nu există evaluări
- Tugas Jurding Anestesi (Debbiecindew)Document34 paginiTugas Jurding Anestesi (Debbiecindew)Linde RendÎncă nu există evaluări
- Power Point RASDocument16 paginiPower Point RASLinde RendÎncă nu există evaluări
- Hernia in AdultDocument81 paginiHernia in AdultLinde RendÎncă nu există evaluări
- Tugas Jurding Radiologi (Debbiecindew)Document40 paginiTugas Jurding Radiologi (Debbiecindew)Linde RendÎncă nu există evaluări
- Hernia 131122002435 Phpapp01Document72 paginiHernia 131122002435 Phpapp01Linde RendÎncă nu există evaluări
- Herniaruby 121013110825 Phpapp01Document41 paginiHerniaruby 121013110825 Phpapp01Linde RendÎncă nu există evaluări
- Titipan FilmDocument2 paginiTitipan FilmLinde RendÎncă nu există evaluări
- Film, F, L, I, MDocument1 paginăFilm, F, L, I, MLinde RendÎncă nu există evaluări
- COVID-19 Isolation Effects on Mental Health and EconomyDocument10 paginiCOVID-19 Isolation Effects on Mental Health and EconomyRimsHa ShAbbirÎncă nu există evaluări
- ModuleIV RespiratoryEmergencies CHF COPD AsthmaDocument96 paginiModuleIV RespiratoryEmergencies CHF COPD AsthmaSaiKiranÎncă nu există evaluări
- Contact PrecautionsDocument2 paginiContact PrecautionsCristina L. JaysonÎncă nu există evaluări
- 2021 - Viral Vector-Based Gene Therapies in The ClinicDocument20 pagini2021 - Viral Vector-Based Gene Therapies in The ClinicMaykol Hernán Rojas SánchezÎncă nu există evaluări
- First Announcement JSOF 5 Tahun - Revisi 3Document12 paginiFirst Announcement JSOF 5 Tahun - Revisi 3Wasisto YudisaputroÎncă nu există evaluări
- Activity IntoleranceDocument4 paginiActivity IntoleranceDianne MacaraigÎncă nu există evaluări
- NCM101j Quiz 2Document11 paginiNCM101j Quiz 2writingstuffforyou9Încă nu există evaluări
- Rheumatic Fever and Rheumatic Heart Disease in ChildrenDocument7 paginiRheumatic Fever and Rheumatic Heart Disease in ChildrenSurya MahardikaÎncă nu există evaluări
- Psych EnhancementDocument4 paginiPsych EnhancementRalph Elvin MacanlalayÎncă nu există evaluări
- Essay 5Document13 paginiEssay 5api-549025764Încă nu există evaluări
- Acute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFDocument9 paginiAcute Kidney Injury in Pregnancy and The Use of Non-Steroidal Anti-In Ammatory Drugs PDFSai Khin Aung TintÎncă nu există evaluări
- Oral Manifestations of Thyroid Disorders and Its MDocument4 paginiOral Manifestations of Thyroid Disorders and Its MNike WijayaÎncă nu există evaluări
- Emerging Re-Emerging Infectious Disease 2022Document57 paginiEmerging Re-Emerging Infectious Disease 2022marioÎncă nu există evaluări
- Endometrial CancerDocument192 paginiEndometrial CancerAbhishek VijayakumarÎncă nu există evaluări
- Group 1 Parkinsons Pre TestDocument4 paginiGroup 1 Parkinsons Pre TestAyman NabilÎncă nu există evaluări
- Guideline Karsinoma HepatoselulerDocument11 paginiGuideline Karsinoma HepatoselulerMohammad Ihsan RifasantoÎncă nu există evaluări
- Shan AsfDocument2 paginiShan AsfM.Fizan JavedÎncă nu există evaluări
- Crohn's Disease Case Study: Matt SimsDocument14 paginiCrohn's Disease Case Study: Matt SimsKipchirchir AbednegoÎncă nu există evaluări
- L01 Obs. - History - Dr.a.rahim 2021 2022Document5 paginiL01 Obs. - History - Dr.a.rahim 2021 2022salmaÎncă nu există evaluări
- Bacteria Isolated from Respiratory TractDocument5 paginiBacteria Isolated from Respiratory TractJihan novestaÎncă nu există evaluări
- Oral Pathology in Paediatric Patients-Mini-Systematic ReviewDocument7 paginiOral Pathology in Paediatric Patients-Mini-Systematic ReviewYuganya SriÎncă nu există evaluări
- FOP: Fibrodysplasia Ossificans ProgressivaDocument20 paginiFOP: Fibrodysplasia Ossificans ProgressivaAnnizaAgustinaÎncă nu există evaluări
- Jerome Cauthen V3 PCDocument4 paginiJerome Cauthen V3 PCSammy ChegeÎncă nu există evaluări
- Guidance Rapid Antibody COVID TestsDocument2 paginiGuidance Rapid Antibody COVID TestsRaghu NadhÎncă nu există evaluări