Documente Academic
Documente Profesional
Documente Cultură
JR Faiz
Încărcat de
rizkyfatirTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
JR Faiz
Încărcat de
rizkyfatirDrepturi de autor:
Formate disponibile
Ann Dermatol Vol. 23, No.
3, 2011
DOI: 10.5021/ad.2011.23.3.386
CASE REPORT
Childhood Granulomatous Periorificial Dermatitis
Yoon Jee Kim, M.D., Jung Woong Shin, M.D., Jong Suk Lee, M.D., Young-Lip Park, M.D., Kyu-Uang
Whang, M.D., Sung Yul Lee, M.D.
Department of Dermatology, College of Medicine, Soonchunhyang University, Cheonan, Korea
Childhood granulomatous periorificial dermatitis (CGPD),
also known as facial Afro-Caribbean childhood eruption
(FACE), is a distinctive granulomatous form of perioral
dermatitis. It is a condition of unknown etiology, characterized by monomorphous, small, papular eruptions around
the mouth, nose and eyes that histopathologically show a
granulomatous pattern. It affects prepubescent children of
both sexes and typically persists for several months but
resolved without scarring. We report a 9 year-old girl with
multiple, discrete, monomorphic, papular eruptions of
2-months duration on the perioral and periocular areas.
Histopathological examination demonstrated upper dermal
and perifollicular granulomatous infiltrate. (Ann Dermatol
23(3) 386388, 2011)
-KeywordChildhood granulomatous periorificial dermatitis
INTRODUCTION
Childhood granulomatous periorificial dermatitis (CGPD)
is a benign eruption of the face previously reported in
prepubertal, Afro-Caribbean children. It was first described
in 1970 in French published by Gianotti et al.1. It occurs
most commonly in prepubertal children as an asymptomatic, discrete, 13 mm dome-shaped papule that is
Received January 25, 2010, Revised July 26, 2010, Accepted for
publication July 26, 2010
Corresponding author: Sung Yul Lee, M.D., Department of Dermatology, College of Medicine, Soonchunhyang University, 8 Soonchunhyang
2-gil, Dongnam-gu, Cheonan 330-721, Korea. Tel: 82-41-570-2272,
Fax: 82-41-578-2270, E-mail: dermsung@schmc.ac.kr
This is an Open Access article distributed under the terms of the
Creative Commons Attribution Non-Commercial License (http://
creativecommons.org/licenses/by-nc/3.0) which permits unrestricted
non-commercial use, distribution, and reproduction in any medium,
provided the original work is properly cited.
386 Ann Dermatol
red or yellow-brown around the mouth, nose and eyes.
Typically, the disease is benign and self-limited, therefore
treatment is unnecessary. Differential diagnoses of CGPD
include perioral dermatitis (PD), granulomatous-rosacea,
sarcoidosis, and lupus miliaris disseminatus faciei (LMDF).
Herein, we report a case of CGPD with a review of the
literature.
CASE REPORT
A 9 year-old girl first presented to our department with a
two-month history of non-pruritic papular eruption on her
face. She had no personal or family history of skin
disorders, including acne, atopy, contact allergies, or oily
skin. She was not on oral medication and denied the use
of topical steroids/irritants on her face. Physical examination revealed numerous monomorphic, small red-toyellow-colored papules ranging from 1 to 3 mm in
diameter, primarily located in the perioral area (Fig. 1A). A
few papules were noted around the nose and both lower
eyelids (Fig. 1B). Several dome-shaped papules on the
lower eyelids were suspected to be syringoma or LMDF.
Laboratory evaluation, including complete blood cell
count, chemistry panel, calcium level, erythrocyte
sedimentation rate (ESR), and serum levels of anti-nuclear
antibody, showed no abnormalities.
Biopsy was taken from a papule on the face. Granulomatous infiltrates were located around the hair follicles in
the superficial dermis, comprised of epitheloid histiocytes
and lymphocytes (Fig. 2). A small nodular granulomatous
infiltrate containing many lymphocytes and a few epithelioid cells could also be seen in the mid to deep dermis.
There was no caseation necrosis. Special stains for fungi
and acid-fast bacilli revealed no microorganisms. These
clinicopathological features were consistent with the
diagnosis of CGPD. The patient did not receive treatment,
but the papular eruptions resolved spontaneously over
several months without therapy.
Childhood Granulomatous Periorificial Dermatitis
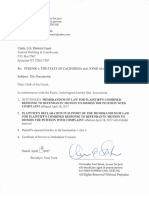
Fig. 1. (A) A close up view of the papular lesions around the mouth. Numerous firm papules seen on the erythematous base in
a perioral distribution. (B) A close-up view of the papular lesions around the eyes. Several yellow-brown dome-shaped papules can
seen in the lower eyelid.
Fig. 2. Skin biopsy from the perioral area shows upper and perifollicular granuloma with adjacent lymphocytes. A granuloma is
comprised of epithelioid cells and lymphocytes (H&E, 200).
DISCUSSION
CGPD was first reported in 1970 in the French literature
by Gianotti et al.1. He described five Italian children
ranging in age from 2.5 to 7 years with distinctive eruption of the skin around the mouth. In 1974, Marten et al.2
reported 22 black children with papular eruption limited
to the face. This eruption was described as flesh-colored
papules grouped primarily on the central face. In 1989,
Frieden et al.3 termed the disease as granulomatous PD in
4
children. In 1990, Williams et al. reported 5 patients very
similar to those of Marten et al. and Frieden et al.. He
coined the term facial Afro-Caribbean childhood eruption
(FACE) to reflect that all their cases occurred in
Afro-Caribbean children. Finally, in 1996, Knautz and
5
Lesher used the term CGPD to differentiate the eruption
from traditional PD and to avoid the term FACE which
limits the diagnosis to Afro- Caribbeans subjects.
CGPD is thought to be an uncommon variant of perioral
dermatitis. It typically affects prepubertal children and is
more common in boys than girls6,7. In the Korean
dermatologic literature, 3 cases in boys and 1 case in a
girl were reported and the affected age of CGPD was
known to be commonly between 3 and 126-9. According
to the literature, CGPD is seen more commonly in darkskinned patients, but several cases involving fair-skinned
children have been reported10. Typical lesions have been
described as flesh-colored, yellow-brown papules, not
pustules or paulovesicles. The lack of pustules and the
presence of discrete yellow-brown papules, less prominent erythema and scaling, and perifollicular granulomatous infiltrate on examination of a biopsy specimen can
differentiate CGPD from perioral dermatitis5.
The etiology of this condition remains unknown. In some
cases the eruption was related to allergens or irritants3.
Other reports have implicated reactions to bubble gum,
formaldehyde, cosmetic preparations, and antiseptic solutions11,12. Long-term use of topical steroids may induce or
3,13
14
exacerbate CGPD . In 2002, Urbatsch et al. reported a
case of GPD as an unusual reaction to varicella vaccination.
Histopathologically, upper dermal and perifollicular granulomatous infiltrates are seen. Granulomatous infiltrates
consist of epithelioid macrophages, lymphocytes, and
giant cells. In some biopsy specimens, the infiltrate has
been more diffuse, in others, well formed non-caseating
Vol. 23, No. 3, 2011
387
YJ Kim, et al
granuloma are surrounded by lymphocytes. CGPD may
also show epidermal change with mild to moderate spongiosis. The results of special stains and cultures are always
negative for mycobacteria and fungus.
CGPD should be differentiated from sarcoidosis, granulomatous rosaea, and LMDF. Sarcoidosis differs clinically
and histologically. Clinically, sarcoidosis is very rare in
children and almost always associated with systemic
involvement and symptoms such as fatigue, fever, cough,
and dyspnea15. Histologically, sarcoidosis is characterized
by naked granulomas, without the inflammatory cells
around and within the granulomas. Granulomatous
rosacea usually involves the central third of the face and is
characterized by erythema, telangiectasia, pustules, flushing, and edema16. It is most common in 30 to 50 year-old
women17. LMDF is clinically characterized by chronic
papular eruption occurring primarily in the central face.
The lesions are usually red or yellow-brown dome-shaped
papules with a predilection for the eyelid and are seen
more commonly in the adult population. Histologic examination demonstrates well-formed granuloma with central
caseation necrosis, but some exceptions have been
reported, that in early LMDF lesions, they may not have
central caseation18. However, LMDF is distinguished from
CGPD by epithelioid cell granuloma with central caseation necrosis; the clinical course of LMDF resolves spontaneously with scarring.
The first step in therapeutic management should be discontinuation of all topical corticosteroids. Although CGPD
is considered a self-limiting condition, treatment with
tetracyclines, metronidazole, and erythromycin may be
efficacious in CGPD. Most importantly, patients and
parents should be reassured that CGPD is a benign, selflimited condition.
REFERENCES
1. Gianotti F, Ermacora E, Bennelli MG, Caputo R. Particuliere
dermatite peri-orale infantile. Observations sur 5 cas. Bull
Soc Fr Dermatol Syphiligr 1970;77:341.
388 Ann Dermatol
2. Marten RH, Presbury DG, Adamson JE, Cardell BS. An
unusual papular and acneiform facial eruption in the negro
child. Br J Dermatol 1974;91:435-438.
3. Frieden IJ, Prose NS, Fletcher V, Turner ML. Granulomatous
perioral dermatitis in children. Arch Dermatol 1989;125:
369-373.
4. Williams HC, Ashworth J, Pembroke AC, Breathnach SM.
FACE-facial Afro-Caribbean childhood eruption. Clin Exp
Dermatol 1990;15:163-166.
5. Knautz MA, Lesher JL Jr. Childhood granulomatous periorificial dermatitis. Pediatr Dermatol 1996;13:131-134.
6. Kim MS, Kim BS, Koh WS, Cho JJ, Chun DK. A case of
childhood granulomatous perioral dermatitis. Korean J Dermatol 2000;38:526-529.
7. Lee WJ, Yang JH, Lee MW, Choi JH, Moon KC, Koh JK. A
case of childhood granulomatous periorificial dermatitis.
Korean J Dermatol 2008;46:1570-1572.
8. Kim JY, Park SY, Kim CW, Lee KS. A case of childhood
granulomatous periorificial dermatitis. Korean J Dermatol
2004;42:1333-1336.
9. Choi JC, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. A
case of childhood granulomatous perioral dermatitis. Ann
Dermatol 2001;13:113-115.
10. Urbatsch AJ, Frieden I, Williams ML, Elewski BE, Mancini
AJ, Paller AS. Extrafacial and generalized granulomatous
periorificial dermatitis. Arch Dermatol 2002;138:1354-1358.
11. Georgouras K, Kocsard E. Micropapular sarcoidal facial
eruption in a child: Gianotti-type perioral dermatitis. Acta
Derm Venereol 1978;58:433-436.
12. Hafeez ZH. Perioral dermatitis: an update. Int J Dermatol
2003;42:514-517.
13. Fisher AA. Sarcoid-like periocular dermatitis due to strong
topical corticosteroids: prompt response to treatment with
tetracycline. Cutis 1987;40:95-96.
14. Urbatsch AJ, Frieden I, Williams ML, Elewski BE, Mancini
AJ, Paller AS. Extrafacial and generalized granulomatous
periorificial dermatitis. Arch Dermatol 2002;138:1354-1358.
15. English JC 3rd, Patel PJ, Greer KE. Sarcoidosis. J Am Acad
Dermatol 2001;44:725-743.
16. Wilkin JK. Rosacea. Int J Dermatol 1983;22:393-400.
17. Drolet B, Paller AS. Childhood rosacea. Pediatr Dermatol
1992;9:22-26.
18. el Darouti M, Zaher H. Lupus miliaris disseminatus faciei-pathologic study of early, fully developed, and late lesions.
Int J Dermatol 1993;32:508-511.
S-ar putea să vă placă și
- Plant Vs Filter by Diana WalstadDocument6 paginiPlant Vs Filter by Diana WalstadaachuÎncă nu există evaluări
- Rubin Skin Review Q's&a'sDocument7 paginiRubin Skin Review Q's&a'sJUSASBÎncă nu există evaluări
- Harper's Textbook of Pediatric DermatologyDe la EverandHarper's Textbook of Pediatric DermatologyProf. Dr. Alan D. IrvineÎncă nu există evaluări
- Pics MCQSDocument22 paginiPics MCQStania100% (1)
- RELATION AND FUNCTION - ModuleDocument5 paginiRELATION AND FUNCTION - ModuleAna Marie ValenzuelaÎncă nu există evaluări
- Hom M, Demodex - Clinical Cases & Diagnostic Protocol. OVS 2013Document8 paginiHom M, Demodex - Clinical Cases & Diagnostic Protocol. OVS 2013cassie_kuldaÎncă nu există evaluări
- Dermatology MCQ With AnswersDocument27 paginiDermatology MCQ With Answershesham0% (1)
- Childhood Granulomatous Periorificial DermatitisDocument4 paginiChildhood Granulomatous Periorificial DermatitisNiaUlfaAngreiniTambunanÎncă nu există evaluări
- CGPD 2 PDFDocument3 paginiCGPD 2 PDFNiaUlfaAngreiniTambunanÎncă nu există evaluări
- UC Davis: Dermatology Online JournalDocument6 paginiUC Davis: Dermatology Online JournalmirzaÎncă nu există evaluări
- 1 s2.0 S1578219020300792 MainDocument2 pagini1 s2.0 S1578219020300792 MainFeyzullah TokgözÎncă nu există evaluări
- Perioral DermatitisDocument5 paginiPerioral Dermatitissusanti michellinaÎncă nu există evaluări
- Pityriasis AlbaDocument7 paginiPityriasis AlbaAri Kurniawan100% (1)
- Perioral Dermatitis JurnalDocument15 paginiPerioral Dermatitis JurnalElokÎncă nu există evaluări
- 13.autoimmune Basement AbreuVelezAMDocument16 pagini13.autoimmune Basement AbreuVelezAMJulie Payne-KingÎncă nu există evaluări
- Erupsi AkneiformisDocument11 paginiErupsi AkneiformisBagus Putra KurniawanÎncă nu există evaluări
- Perioral DermatitisDocument5 paginiPerioral DermatitisAstriana IndrawatiÎncă nu există evaluări
- Clinical Heterogeneity and Differential Diagnosis of Atopic DermatitisDocument5 paginiClinical Heterogeneity and Differential Diagnosis of Atopic DermatitisAlina BoiangiuÎncă nu există evaluări
- American Journal of Clinical DermatologyDocument13 paginiAmerican Journal of Clinical DermatologyJoel ChocaÎncă nu există evaluări
- Diagnosis and Management of Atopic Dermatitis For Primary Care ProvidersDocument10 paginiDiagnosis and Management of Atopic Dermatitis For Primary Care ProvidersMira GÎncă nu există evaluări
- Antimonium Crudum in Pediatric Skin ConditionsDocument9 paginiAntimonium Crudum in Pediatric Skin ConditionsJohn LangeÎncă nu există evaluări
- Subcutaneous Granuloma Annulare (Pseudorheumatoid Nodule) - , F 38, Ankles.Document13 paginiSubcutaneous Granuloma Annulare (Pseudorheumatoid Nodule) - , F 38, Ankles.Deba P SarmaÎncă nu există evaluări
- Bullous PemphigoidDocument13 paginiBullous PemphigoidSharifah HanimÎncă nu există evaluări
- Jadotte Pityriasis AlbaDocument8 paginiJadotte Pityriasis Albapene asoyÎncă nu există evaluări
- Case Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureDocument6 paginiCase Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureIrsalinaHusnaAzwirÎncă nu există evaluări
- Perioral Dermatitis PDFDocument6 paginiPerioral Dermatitis PDFanissa fitriÎncă nu există evaluări
- Aiims SkinDocument85 paginiAiims SkinSagar MukherjeeÎncă nu există evaluări
- Seminar: Enno Schmidt, Detlef ZillikensDocument13 paginiSeminar: Enno Schmidt, Detlef ZillikensUssiy RachmanÎncă nu există evaluări
- Diagnosisandclinical Featuresofpemphigus Vulgaris: Supriya S. Venugopal,, Dédée F. MurrellDocument1 paginăDiagnosisandclinical Featuresofpemphigus Vulgaris: Supriya S. Venugopal,, Dédée F. MurrellDwiKamaswariÎncă nu există evaluări
- Jurnal 3Document6 paginiJurnal 3Putri AmeliaÎncă nu există evaluări
- Pyoderma Gangrenosum: Etiology and PathogenesisDocument13 paginiPyoderma Gangrenosum: Etiology and PathogenesisIga Nurwani RidwanÎncă nu există evaluări
- Skin in Clinical DiagnosisDocument64 paginiSkin in Clinical Diagnosisadamu mohammad0% (1)
- Pityriasis AlbaDocument6 paginiPityriasis AlbaLee Eng SiangÎncă nu există evaluări
- Pemphigus: by Demetris Ioannides, MD Associate Professor of DermatologyDocument43 paginiPemphigus: by Demetris Ioannides, MD Associate Professor of DermatologyYulita PurbaÎncă nu există evaluări
- Demodex JurnalDocument9 paginiDemodex JurnalRisky PerdanaÎncă nu există evaluări
- Chromoblastomycosis: Differential DiagnosesDocument4 paginiChromoblastomycosis: Differential DiagnosesPranab ChatterjeeÎncă nu există evaluări
- Perioral DermatitisDocument6 paginiPerioral DermatitisYeni OktaviaÎncă nu există evaluări
- Atopic DermatitisDocument8 paginiAtopic DermatitiskoesantoÎncă nu există evaluări
- UntitledDocument10 paginiUntitledMarande LisaÎncă nu există evaluări
- Bullous Fixed Drug Eruption Induced by Paracetamol: Report of A Pediatric CaseDocument4 paginiBullous Fixed Drug Eruption Induced by Paracetamol: Report of A Pediatric CaseRirin AgustinÎncă nu există evaluări
- Atopicdermatitisisabarrier Issue, Notanallergyissue: Monica T. Kraft,, Benjamin T. PrinceDocument13 paginiAtopicdermatitisisabarrier Issue, Notanallergyissue: Monica T. Kraft,, Benjamin T. PrinceJesus MoralesÎncă nu există evaluări
- Refen 3 PDFDocument8 paginiRefen 3 PDFSiti Aulia Rahma SyamÎncă nu există evaluări
- Etiology of Proptosis in Children Sindhu 1998Document3 paginiEtiology of Proptosis in Children Sindhu 1998Putri Wulan SukmawatiÎncă nu există evaluări
- Ashka Kodnani Et Al.Document4 paginiAshka Kodnani Et Al.International Journal of Clinical and Biomedical Research (IJCBR)Încă nu există evaluări
- Perioral Dermatitis: Acta Dermatovenerologica Croatica: ADC / Hrvatsko Dermatolosko Drustvo February 2008Document6 paginiPerioral Dermatitis: Acta Dermatovenerologica Croatica: ADC / Hrvatsko Dermatolosko Drustvo February 2008Firdani MutiaraÎncă nu există evaluări
- Pityriasis Alba: A Condition With Possibly Multiple EtiologiesDocument2 paginiPityriasis Alba: A Condition With Possibly Multiple EtiologiesAndana Haris R.Încă nu există evaluări
- Nicotine-Induced Bullous Fixed Drug EruptionDocument3 paginiNicotine-Induced Bullous Fixed Drug Eruptionamal amanahÎncă nu există evaluări
- Content ServerDocument3 paginiContent ServerAngela Maria SanchezÎncă nu există evaluări
- 1476 ArticleText 6472 1 10 20100118 PDFDocument6 pagini1476 ArticleText 6472 1 10 20100118 PDFJayantiÎncă nu există evaluări
- (Serbian Journal of Dermatology and Venereology) National Guidelines For The Treatment of Atopic DermatitisDocument25 pagini(Serbian Journal of Dermatology and Venereology) National Guidelines For The Treatment of Atopic DermatitisFebtri IRnawitaÎncă nu există evaluări
- PD Art 22401Document5 paginiPD Art 22401Haris TanÎncă nu există evaluări
- 0610 - Peds Acne FeaDocument9 pagini0610 - Peds Acne FeaReginaÎncă nu există evaluări
- B. Diseases With Subepidermal Blistering (Pemphigoid Group) : 9. Fogo Selvagem, Brazilian Pemphigus FoliaceusDocument7 paginiB. Diseases With Subepidermal Blistering (Pemphigoid Group) : 9. Fogo Selvagem, Brazilian Pemphigus FoliaceusLukman GhozaliÎncă nu există evaluări
- Childhood Erythrodermic Lichen Planus Pemphigoides After Nonavalent Human Papillomavirus VaccinationDocument3 paginiChildhood Erythrodermic Lichen Planus Pemphigoides After Nonavalent Human Papillomavirus Vaccinationnurul hidayatiÎncă nu există evaluări
- Perioral DermatitisDocument12 paginiPerioral Dermatitissanti dwi rahmawatiÎncă nu există evaluări
- Bullous Pemphigoid: PathogenesisDocument5 paginiBullous Pemphigoid: PathogenesisLukman GhozaliÎncă nu există evaluări
- Yang 2019Document11 paginiYang 2019RaissaÎncă nu există evaluări
- Pemphigus Vulgaris Confined To The Gingiva: A Case ReportDocument16 paginiPemphigus Vulgaris Confined To The Gingiva: A Case ReportAlmasulah Al-akmaliyahÎncă nu există evaluări
- Enfermedades InmunologicasDocument14 paginiEnfermedades InmunologicasKarina OjedaÎncă nu există evaluări
- Propp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeDocument10 paginiPropp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeRohith KumarÎncă nu există evaluări
- Portfolio Write-UpDocument4 paginiPortfolio Write-UpJonFromingsÎncă nu există evaluări
- STRUNK V THE STATE OF CALIFORNIA Etal. NYND 16-cv-1496 (BKS / DJS) OSC WITH TRO Filed 12-15-2016 For 3 Judge Court Electoral College ChallengeDocument1.683 paginiSTRUNK V THE STATE OF CALIFORNIA Etal. NYND 16-cv-1496 (BKS / DJS) OSC WITH TRO Filed 12-15-2016 For 3 Judge Court Electoral College ChallengeChristopher Earl Strunk100% (1)
- Research Paper On Marketing PlanDocument4 paginiResearch Paper On Marketing Planfvhacvjd100% (1)
- Bankers ChoiceDocument18 paginiBankers ChoiceArchana ThirunagariÎncă nu există evaluări
- 2017-04-27 St. Mary's County TimesDocument32 pagini2017-04-27 St. Mary's County TimesSouthern Maryland OnlineÎncă nu există evaluări
- Hot Rolled Coils Plates & SheetsDocument40 paginiHot Rolled Coils Plates & Sheetssreekanth6959646Încă nu există evaluări
- Introduction To Pharmacology by ZebDocument31 paginiIntroduction To Pharmacology by ZebSanam MalikÎncă nu există evaluări
- Corregidor Title DefenseDocument16 paginiCorregidor Title DefenseJaydee ColadillaÎncă nu există evaluări
- License Fee PaidDocument1 paginăLicense Fee Paidmy nÎncă nu există evaluări
- Pell (2017) - Trends in Real-Time Traffic SimulationDocument8 paginiPell (2017) - Trends in Real-Time Traffic SimulationJorge OchoaÎncă nu există evaluări
- Whitepaper ITES Industry PotentialDocument6 paginiWhitepaper ITES Industry PotentialsamuraiharryÎncă nu există evaluări
- Pepcoding - Coding ContestDocument2 paginiPepcoding - Coding ContestAjay YadavÎncă nu există evaluări
- Forensic My Cology Mcgraw HillDocument8 paginiForensic My Cology Mcgraw HillJayanti RaufÎncă nu există evaluări
- 2 Year Spares List For InstrumentationDocument2 pagini2 Year Spares List For Instrumentationgudapati9Încă nu există evaluări
- Korea Times - Korean-EnglishDocument313 paginiKorea Times - Korean-EnglishgyeryongÎncă nu există evaluări
- Line Integrals in The Plane: 4. 4A. Plane Vector FieldsDocument7 paginiLine Integrals in The Plane: 4. 4A. Plane Vector FieldsShaip DautiÎncă nu există evaluări
- Portfolio AdityaDocument26 paginiPortfolio AdityaAditya DisÎncă nu există evaluări
- Reservoir Bag Physics J PhilipDocument44 paginiReservoir Bag Physics J PhilipJashim JumliÎncă nu există evaluări
- Altura Architect & Interior Design BriefDocument56 paginiAltura Architect & Interior Design BriefDave WongÎncă nu există evaluări
- The Global Entrepreneurship and Development Index 2014 For Web1 PDFDocument249 paginiThe Global Entrepreneurship and Development Index 2014 For Web1 PDFAlex Yuri Rodriguez100% (1)
- Wire Rope TesterDocument4 paginiWire Rope TesterclzagaÎncă nu există evaluări
- Zkp8006 Posperu Inc SacDocument2 paginiZkp8006 Posperu Inc SacANDREA BRUNO SOLANOÎncă nu există evaluări
- E9 Đề khảo sát Trưng Vương 2022 ex No 1Document4 paginiE9 Đề khảo sát Trưng Vương 2022 ex No 1Minh TiếnÎncă nu există evaluări
- D15 Hybrid P1 QPDocument6 paginiD15 Hybrid P1 QPShaameswary AnnadoraiÎncă nu există evaluări
- ERBS UPDATE John Doe ProceedingDocument3 paginiERBS UPDATE John Doe ProceedingtpeppermanÎncă nu există evaluări
- Prediction of Mechanical Properties of Steel Using Artificial Neural NetworkDocument7 paginiPrediction of Mechanical Properties of Steel Using Artificial Neural NetworkInternational Association of Scientific Innovations and Research (IASIR)Încă nu există evaluări
- Sco 8th Class Paper - B Jee-Main Wtm-15 Key&Solutions Exam DT 17-12-2022Document4 paginiSco 8th Class Paper - B Jee-Main Wtm-15 Key&Solutions Exam DT 17-12-2022Udaya PrathimaÎncă nu există evaluări