Documente Academic
Documente Profesional
Documente Cultură
Nano
Încărcat de
Haroon RahimDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Nano
Încărcat de
Haroon RahimDrepturi de autor:
Formate disponibile
See
discussions, stats, and author profiles for this publication at: http://www.researchgate.net/publication/265852284
Investigation of various practical techniques to
enhance dissolution of ezetimibe from oral
tablets: A comparative study
ARTICLE in JOURNAL OF YOUNG PHARMACISTS MAY 2014
DOI: 10.5530/jyp.2014.1.2
DOWNLOADS
VIEWS
85
69
4 AUTHORS, INCLUDING:
Jithan Aukunuru
Mother Teresa College of Pharmacy, Ghatksar
30 PUBLICATIONS 176 CITATIONS
SEE PROFILE
Available from: Jithan Aukunuru
Retrieved on: 15 July 2015
Original Article
Investigation of various practical techniques to enhance
dissolution of ezetimibe from oral tablets: A comparative study
Prema Kumari Nanam1, Kiran Thadkala1, Chinta Sailu2, Jithan Aukunuru1*
Mother Teresa College of Pharmacy, Osmania University, 2University College of Technology,
Osmania University, Hyderabad, Andhra Pradesh, India
ABSTRACT
Objective: The aim of this work was to investigate and compare various practical techniques to enhance dissolution
of ezetimibe, a Class II Biopharmaceutics Classification System compound. Ezetimibe is a poorly soluble compound
with variable oral bioavailability. Nanosuspensions, hydroxypropyl-beta-cyclodextrin (HPCD) complexes as well
as combination of surfactant were techniques investigated. Materials and Methods: Nanosuspension of ezetimibe
was prepared using solvent-antisolvent precipitation technique. The nanosuspensions were characterized by powder
X-ray diffractometry and scanning electron microscopy. HPCD inclusion complexes were prepared using physical
mixture, co-evaporation, and kneading methods. These complexes were characterized using Fourier transform
infrared spectroscopy (FTIR) and differential scanning calorimetry (DSC). Ezetimibe tablet formulations containing
drug nanosuspensions, HPCD complexes as well as sodium lauryl sulfate (SLS) enrichment were prepared and
evaluated for dissolution. Results and Discussion: Nanosuspensions of ezetimibe with a mean particle size of 900 nm
were successfully prepared using solvent-antisolvent precipitation. FTIR and DSC studies confirmed the formation of
ezetimibe inclusion complexes. Tablets prepared using pure drug showed very poor dissolution. In contrast, tablets of
nanosuspensions, HPCD inclusion complexes and SLS mixtures showed enhanced dissolution. The tablets prepared
using nanosuspensions demonstrated enhanced dissolution rate when compared to the formulations prepared using
HPCD complexes and SLS enrichment. All the techniques investigated can be used to enhance the dissolution of
ezetimibe and thus can enhance the oral bioavailability and also reduce the fluctuations in the oral bioavailability.
Conclusion: The techniques that were employed in this present work, nanosuspensions seem to be better when
compared to cyclodextrin inclusion complexes and SLS enrichment in enhancing solubility and dissolution rate of
ezetimibe.
Key words: Drug-sodium lauryl sulphate tablets, ezetimibe, hydroxypropyl-beta-cyclodextrin complexes,
nanosuspension, nanosuspension tablets, sodium lauryl sulphate
Access this article online
Journal Sponsor
Website:
www.jyoungpharm.org
DOI:
10.5530/jyp.2014.1.2
INTRODUCTION
Oral drug delivery is the most common method for
administration of drugs.1 For the assessment of new drug
entities, researchers and industry invariably use oral route
in the exploratory stages. In the current situation, a large
number of drugs reaching the hands of formulators are
*Address for correspondence:
Mr. Jithan Aukunuru, Mother Teresa College of Pharmacy, Osmania University, Hyderabad, Andhra Pradesh,
India. E-mail: aukunjv@gmail.com
8
Journal of Young Pharmacists
Vol 6 Issue 1 Jan-Mar 2014
Nanam, et al.: Enhancement of dissolution of ezetamibe
poorly water soluble and thus their oral pharmacokinetics
are compromised with the oral bioavailability and
absorption across the gastrointestinal tract (GIT) is either
low or variable.2 Different techniques have been successfully
investigated to improve the solubility. These techniques
modify the physicochemical properties of the drug or add
novel functionality to the molecular structure of the drug
or develop newer formulations. Such techniques include
microparticles, nanoparticles, liposomes, nanosuspension,
cyclodextrin inclusion complexes, surfactant-enrichment,
salts, pH modification, prodrugs, nanoemulsions and redispersable emulsion powders.3,4 Of these many techniques,
practical and clinical reality has been achieved with
nanosuspensions, cyclodextrin inclusion complexes and
surfactant enrichment. The enhancement in dissolution
rate of a drug enhances the oral bioavailability as well as
reduces the fluctuations in the bioavailability of poorly
soluble compounds.
Ezetimibe is a lipid-lowering compound that selectively
inhibits the absorption of cholesterol and related
phytosterols from the intestine.5 It is a Biopharmaceutics
Classification System Class II drug with low solubility
and high permeability. Water solubility of ezetimibe is
8.46e-03 g/l. It is a weakly basic compound and thus
contains ionizable groups. Its log P = 4.5. Its strongest acidic
pKa and strongest basic pKa are 9.48 and 3, respectively.
As it is poorly soluble in water, its oral absorption is less,
and it was found that it also has the problem of variable
pharmacokinetics after oral administration.6 This could be
mainly attributed to poor solubility and poor dissolution
rate. Its absolute bioavailability cannot be determined as it
has very low solubility that an intravenous injection cannot
be prepared. Even though ezetimibe contain ionizable
groups, it shows essential pH independent solubility
characteristics across GIT pH range.7 Thus, pH-based
strategies to improve solubility/dissolution characteristics
(e.g. salts, addition of pH modifiers) were not the first
line strategy. The other strategies can be attempted with
success, but their manufacture is not practical. In this
regard, nanosuspensions, cyclodextrin complexes and
addition of surfactants may be the practical approaches.
Thus, the objective of this study was to enhance the
dissolution rate of ezetimibe so as to solve its poor and
variable bioavailability problems using selected techniques,
which include nanosuspensions, hydroxypropyl-betacyclodextrin (HPCD) complexes and sodium lauryl sulfate
(SLS) enrichment and compare each of these techniques.
The techniques selected are practical and the formulations
prepared using these techniques can be conveniently
commercialized.
Journal of Young Pharmacists
Vol 6 Issue 1 Jan-Mar 2014
MATERIALS AND METHODS
Ezetimibe and HPCD were obtained as a gift sample from
Suven Nishtaa Ltd., Hyderabad, India. Ethanol, Tween 80
and SLS were obtained from SD fine chemicals limited.
Magnesium stearate, lactose, croscarmellose sodium and
povidone K 30 were obtained from Lab tech. All the other
ingredients were used of analytical grade. All the equipment
used in the study is routinely calibrated using procedures
described by the manufacturers.
Preparation and characterization of ezetimibe
nanosuspensions
Ezetimibe is a lipid lowering agent. PUMchem indicates its
molecular formula as C24H21F2NO3 and molecular weight
as 409.42. Ezetimibe nanosuspensions were prepared by a
modification of solvent-antisolvent precipitation method
as previously described for other drugs.8 Ethanol was used
as solvent and water was used as antisolvent. Tween 80
was used as surfactant to stabilize the nanosuspension.
The drug ezetimibe (100 mg) was dissolved in solvent
ethanol (4 ml). A 0.2 ml of tween 80 was dissolved in
distilled water (20 ml). Ethanolic solution was injected drop
wise into tween 80 solution with a constant stirring on a
magnetic stirrer. Ethanol was evaporated under vaccum to
precipitate the nanosuspension. The product was recovered
by centrifugation at 7000 rpm for 10 min using a Remi
high speed centrifuge, washed twice with water and then
freeze dried. The freeze dryer used was Delvac Mini Lyodel,
Chennai, India. Freeze dried nanosuspension was then used
for further studies. The yield of the formulation from one
batch was determined using an assay method developed
using ultra violet-vis. spectrophotometer. Briefly, 10 mg
of ezetimibe nanosuspensions were dissolved in 10 ml of
methanol, the aliquot was centrifuged and the supernatant
was taken for the drug assay. The max used for the assay
was 232 nm. The percentage yield was calculated using
the formula:
% Yield =
Amount of the drug in nanususpensions
100
he drug taken for preparation
Amount of th
The mean particle size was determined using an optical
microscope. In order to examine the particle surface
morphology and shape, scanning electron microscopy (SEM)
was used. A concentrated aqueous suspension was spread over
a slab and dried under vacuum. The sample was shadowed in a
cathodic evaporator with gold layer 20 nm thick. Photographs
were taken using a JSM-5200 SEM (Tokyo, Japan) operated at
20 kV. The crystallinity of the drug was evaluated using X-ray
powder diffraction (XRPD). X-ray spectra were recorded with
9
Nanam, et al.: Enhancement of dissolution of ezetamibe
XPert-PRO multipurpose X-ray diffractometer (PANalytical,
Tokyo, Japan) using Ni-filtered, Cu Ka radiation, a voltage of
45 kV, and a current of 40 mA with a scintillation counter. The
instrument was operated in the continuous scanning speed of
10/min over a 2 range of 10 to 80.
Preparation and characterization of
hydroxypropyl-beta-cyclodextrin inclusion
complexes of ezetimibe
Ezetimibe HPCD inclusion complexes were prepared
using three methods as described earlier. 9,10 These
methods are physical mixing, kneading method, and
co-evaporation method. Preliminary phase solubility
experiments were conducted to determine drug: HPCD
ratio for optimum binding. Based on the results, 1:1 weight
ratio was considered optimum and we used this ratio
in all the studies. In physical mixing method, ezetimibe
and HPCD were accurately weighed in equal ratios of
1:1 and were prepared by simply mixing powders with a
spatula for 15 min and then sieved through 120# to obtain
final desired inclusion complex. In case of kneading
method, 1:1 ratio of drug and HPCD were weighed.
HPCD and distilled water mixed together in a mortar
so as to obtain a homogenous paste. Drug was added
slowly; while mixing, a small quantity of methanol was
added to assist the dissolution of drug. Mixtures were
then blended for 2 h using an appropriate quantity of
water to maintain suitable consistency. The paste was
dried in oven at 45-50C for 24 h. The dried complex
was pulverized and then sieved through 120# to obtain
final desired inclusion complex. In co-evaporation, drug
and HPCD were accurately weighed in the equal ratios
of 1:1 and dissolved in the same quantities (5 ml) of
methanol and water respectively. Both the solutions were
mixed and solvents were evaporated by controlled heating
at 45-50C. The resulting solid was pulverized and then
sieved through 120# to obtain final desired particle size
of inclusion complex. It was made sure that the entire
methanol was removed from the complex at the end of
its preparation.
E z e t i m i b e H P C D i n c l u s i o n c o m p l e xe s we r e
characterized by Fourier transform infrared spectroscopy
(FTIR) and DSC. T he FTIR spectra of dr ug,
cyclodextrin, physical mixture, kneading method, and
co-evaporation method were obtained. About 5 mg of
sample was mixed thoroughly with 100 mg potassium
bromide IR powder and compacted under vacuum a
pressure of about 12 Psi for 3 min. The resulting disc
was mounted in a suitable holder in Perkin Elmer IR
10
spectrophotometer, and the IR spectrum was recorded
from 4000/cm to 625/cm in a scan time of 12 min.
Thermal properties of the powder samples were
investigated with a differential scanning calorimetry
(DSC). DSC measurements were taken by the Perkin
Elmers PYRIS Diamond DSC. The temperature was
calibrated with pure indium. All measurements were
performed under a high-purity nitrogen atmosphere to
minimize degradation. Approximately, 10 mg of sample
was analyzed in an open aluminum pan, and heated at
scanning rate of 10C/min between 0C and 400C.
Magnesia was used as the standard reference material.
Preparation of ezetimibe sodium lauryl sulfate
powder complex
The ezetimibe SLS complex were prepared by addition of
SLS in different amounts (0.1%, 0.2%, and 1%) to the drug.
The powder mixture was thoroughly blended and sieved
to obtain powder of desired size. This technique is called
surfactant enrichment, is commonly used in industry and
has been previously described.11
Preparation and evaluation of ezetimibe tablets
using nanosuspensions, cyclodextrin complexes
and sodium lauryl sulfate mixtures
Tablets containing pure drug, nanosuspensions, cyclodextrin
inclusion complexes, and SLS enrichment were prepared
using conventional wet granulation technique. Compressed
tablets each containing 10 mg of ezetimibe were prepared
by wet granulation method employing pure ezetimibe,
nanosuspensions, cyclodextin complexes, surfactantenriched drug. Lactose was used as diluent to adjust the
weight of the tablet to 200 mg, acacia (2%), talc (2%) and
magnesium stearate (2%) were incorporated respectively
as a binder and lubricants. The tablet granules were
compressed into tablets on a Cadmach 16-station rotary
tablet punching machine (M/s Cadmach Engineering Co.
Pvt. Ltd., Mumbai, India) using 9 mm concave punches.
All the tablets prepared were evaluated for content of
active ingredients, hardness, friability, disintegration time
and dissolution rate as per official (IP) methods. Bulk
density apparatus (Cintex industrial corporation, Mumbai,
India), hardness tester (Monsanto), dissolution apparatus
USP (Electrolab, TDT-08 L) were used. In-vitro dissolution
studies of tablet formulations were carried out using USP
apparatus II paddle method. Accurately, weighed tablets
were added to 900 ml of buffer media (acetate buffer
pH 4.5) at 37C 0.5C and stirred at 50 rpm. An aliquot
of 10 ml was withdrawn at different time intervals. An
Journal of Young Pharmacists
Vol 6 Issue 1 Jan-Mar 2014
Nanam, et al.: Enhancement of dissolution of ezetamibe
equal volume of fresh dissolution medium was immediately
replaced. The samples were assayed spectrophotometrically
at 232 nm.
Statistical analysis
Results are expressed as mean standard error of the
mean of six samples per treatment group. Data were
analyzed using a one-way analysis of variance followed by
Dunnett test. Differences were considered as significant
at P 0.05.
RESULTS AND DISCUSSION
In this study, various practical techniques of enhancement
of solubility of a poorly soluble compound ezetimibe were
investigated and compared. The novel technique that was
investigated to enhance the dissolution rate of a poorly
soluble compound is nanosuspensions. Poor solubility,
incomplete dissolution, and insufficient efficacy are the
major problems of oral drug administration. Due to smaller
particle size and much larger surface to volume ratio, oral
nanosuspensions or nanocrystals are specially used to solve
these problems. In case of azithromycin nanosuspensions,
more than 65% drug was found to be dissolved in 5 h as
compared with 20% of micronized drugs.12 By using the
standard manufacturing techniques, drug nanosuspensions
can be simply incorporated into various dosage forms.13
The other techniques that were investigated to enhance
the solubility and dissolution rate of ezetimibe are use of
cyclodextrins and surfactant enrichment, which are popular
in pharmaceutical formulation development.10,11
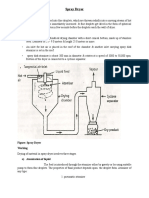
Nanosuspension of ezetimibe was successfully prepared
using the technique employed in this investigation. Particles
were spherical and had an average size of 0.9 m with a
yield of 80% (Figure 1). XRPD was used to investigate the
physical nature of the drug in the nanosuspensions. From
the XRPD graphs, it was observed that the crystallanity of
the drug was changed in the nanosuspensions (Figure 2).
The peaks obtained for pure drug was very clear and
sharp and the intensity of the peaks was very high when
compared with peaks of ezetimibe nanosuspensions.
Reduction in the peak intensity indicates the change
in crystal structure. From this, we can conclude that
there was reduction in the crystallanity and change into
amorphous structures upon fabricating into ezetimibe
nanosuspensions. Nanosuspensions of ezetimibe were not
previously investigated.
Inclusion complexes of ezetimibe with HPCD were
prepared successfully by physical mixture, co-evaporation
Journal of Young Pharmacists
Vol 6 Issue 1 Jan-Mar 2014
and kneading method in a weight ratio of 1:1. This was
confirmed by FTIR and DSC studies. The chemical
interaction between the drug and the carrier can be
observed by changes in the infrared (IR) profile of
complexes and can be interpreted by careful study of
the spectrum. Representative FTIR spectra are shown
in Figure 3. The FTIR spectras of the complexes were
compared with spectrum of pure HPCD and pure
drug. When compared to pure drug, it has been observed
that there is reduction in peak intensities of several
functional groups in the complexes. Change in peak
intensity indicates the complex formation. Therefore, it
has been confirmed that inclusion complex of ezetimibe
is formed by complexation with HPCD. This was further
corroborated by DSC studies. DSC is used to detect all
processes in which energy is required or produced. The
ezetimibe showed a melting peak at 184C (Figure 4). Peak
of ezetimibe at 184C was present at the same position in
all the samples with a reduction of intensity. Reduction in
intensity is interpreted as formation of the complex. FTIR
and DSC results suggest the trapping of drug in HPCD
Figure 1: Scanning electron microscope pictures of nanosuspension
Figure 2: Powder X-ray diffraction of pure drug and nanosuspension
11
Nanam, et al.: Enhancement of dissolution of ezetamibe
c
Figure 3: Fourier transform infrared spectroscopy graphs of cyclodextrin complexes. (a) Pure drug; (b) cyclodextrin; (c) cyclodextrin complexes
prepared using co-evaporation
Figure 5: Cumulative % drug release from ezetimibe tablets prepared
using pure drug and nanosuspensions
Figure 4: Cumulative differential scanning calorimetry graph of drugcyclodextrin complexes
in all the techniques. Such an interpretation was previously
made in the literature.14 The enhancement of dissolution
of ezetimibe with HPCD was previously investigated
by Taupitz et al.7 However, in their study, the aim was to
improve the solubility of ezetimibe along with simvastatin
in fixed dose combination formulations. HPCD enhanced
the dissolution rate of ezetimibe. We proved the results for
ezetimibe tablets and not in combination with other drugs.
Ezetimibe tablets were prepared with the nanosuspensions,
cyclodextrin inclusion complexes and surfactants using wet
granulation technique. The prepared tablets were evaluated
for the following parameters: weight variation, friability,
hardness, disintegration time, assay, content uniformity,
dissolution studies, and the results were compared. Tablet
parameters indicated that good quality of tablets was
12
Table 1: Evaluation of ezetimibe tablets prepared using various
approaches
Evaluation
Nanosuspension Cyclodextrin
Tablets
parameters
tablets
complex
containing
tablets
surfactant
Weight variation (%)
1002
1002
1002
2.5
2.7
3.0
Hardness (kg/cm2)
Friability (%)
1.8
1.9
1.4
Disintegration (s)
10
15
15
Content
1000.5
1000.5
1000.5
uniformity (%)
prepared (Table 1). The results of dissolution studies
demonstrated interesting results. The onset of dissolution
of tablets prepared using unprocessed pure ezetimibe was
very low (20.56% in 1 h) when compared with the tablets
prepared using nanosuspensions (Figure 5). It was observed
that there was an increase in % drug release (82.4% in 1 h)
with tablets prepared using ezetimibe nanosuspensions.
Journal of Young Pharmacists
Vol 6 Issue 1 Jan-Mar 2014
Nanam, et al.: Enhancement of dissolution of ezetamibe
It clearly indicates that nanosuspension formulation has
been a successful technique to improve the dissolution
rate thereby could enhance oral bioavailability and reduce
fluctuations in oral bioavailability. Cyclodextrin complexes
also resulted in enhancement of dissolution rate (Figure 6).
Complexes prepared using co-evaporation and physical
mixing significantly enhanced dissolution rates within 1 h
compared with pure drug and complexes prepared using
kneading technique. Inclusion complexes prepared using
co-evaporation and physical mixing significantly enhanced
dissolution rate of ezetimibe (59.2%, 32.75% within 1 h).
Even dissolution rate of complexes prepared using kneading
method also increased (28.71% within 1 h). The use of
surfactants to improve the dissolution performance of poorly
soluble drug products has also been successfully employed.
There was an increase in dissolution as the concentration of
surfactant increased (Figure 7). A 53.21% of the drug was
released in 1 h in the dissolution studies with the addition of
1% SLS. All the results demonstrated statistical significance.
Cumulative Percentage Drug Release
Although oral bioavailability of ezetimibe was not
measurable because of intravenous for mulation
developmental problems, the studies from administering
oral formulations in humans indicated that the drug
exhibited moderate intersubject variability with coefficient
of variation ranging from 34-43% to 32-37% for Cmax
and AUC, respectively.15 Several formulation approaches
have been addressed to reduce this variability 16-21
Such successful formulations include nanoemulsions,
nanocrystals, self-nanoemulsifying granules, solid
dispersions, etc. If these studies are carefully reviewed,
it could indicate that nanotechnology can solve this
problem of variable bioavailability of ezetimibe in a
better way.16-20 Cyclodextrin inclusion complexes were
also investigated to enhance the solubility and dissolution
70
of ezetimibe and probably may reduce the fluctuations in
its gastro-intestinal tract absorption.7 Since earlier studies
have given us leads that nanotechnology can solve the
problem to a better extent and since nanosuspensions of
ezetimibe were not investigated, we set to investigate this
approach in our study. From dissolution profiles from
the tablets containing ezetimibe prepared using various
techniques, nanosuspensions are found to enhance the
dissolution rate to a greater extent compared with the
other techniques. In this study, three different practical
approaches for reduction in the variability of gastrointestingal tract absorption of ezetimibe have been
investigated, which include nanosuspensions, cyclodextrin
inclusion complexes and sodium lauryl sulfate enriched
formulations. All the techniques demonstrated an increase
in dissolution of the drug and could therefore reduce
the fluctuations in the oral bioavailability of ezetimibe.
The technology can be commercialized to obtain better
ezetimibe formulations.
CONCLUSIONS
Taken together, results of this work indicate that
all the practical techniques employed here led to an
improvement in dissolution of ezetimibe and results
are comparable to similar studies conducted earlier
with other techniques. Within the techniques that were
employed in this research work, nanosuspensions seem
to be better when compared to cyclodextrin inclusion
complexes and SLS enrichment in enhancing solubility
and dissolution rate of ezetimibe.
AUTHOR CONTRIBUTION
This work is a part of M. Pharm project of Prema Kumari
Nannam and a part of Ph.D. project of Kiran Thadkala.
Prema Kumari and Kiran have conducted the experiments.
60
50
pure drug
40
DC (CE)
30
DC (PM)
20
DC (K)
10
0
20
40
60
Time (min)
Figure 6: Cumulative % drug release from ezetimibe tablets prepared
using various drug-cyclodextrin complexes (DC) (PM: Physical mixture;
CE: Coevaporation; K: Kneading)
Journal of Young Pharmacists
Vol 6 Issue 1 Jan-Mar 2014
Figure 7: Cumulative % drug release from ezetimibe tablets prepared
using various amounts of sodium lauryl sulphate
13
Nanam, et al.: Enhancement of dissolution of ezetamibe
The experiments were designed by both Dr. Chinta Sailu
and Dr. Jithan Aukunuru. The manuscript was written by
Dr. Jithan Aukunuru and for this editorial assistance was
provided by Prema Kumari and Kiran.
REFERENCES
Aukunuru J. Oral Drug Delivery Technology. 2nd ed. Hyderabad, India:
Pharma Book Syndicate; 2012.
2. Stegemann S, Leveiller F, Franchi D, de Jong H, Lindn H. When poor
solubility becomes an issue: from early stage to proof of concept. Eur J
Pharm Sci 2007;31:249-61.
3. Savjani KT, Gajjar AK, Savjani JK. Drug solubility: importance and
enhancement techniques. ISRN Pharm 2012;2012:195727.
4. Kotta S, Khan AW, Pramod K, Ansari SH, Sharma RK, Ali J. Exploring
oral nanoemulsions for bioavailability enhancement of poorly water-soluble
drugs. Expert Opin Drug Deliv 2012;9:585-98.
5. Croom K. Ezetimibe for the treatment of primary hypercholesterolaemia.
Drug Context 2008;4:153-72.
6. Kiekens F, Eelen S, Verheyden L, Daems T, Martens J, Van Den Mooter
G. Use of ordered mesoporous silica to enhance the oral bioavailability of
ezetimibe in dogs. J Pharm Sci 2012;101:1136-44.
7. Taupitz T, Dressman JB, Klein S. New formulation approaches to improve
solubility and drug release from fixed dose combinations: case examples
pioglitazone/glimepiride and ezetimibe/simvastatin. Eur J Pharm Biopharm
2013;84:208-18.
8. Mansouri M, Pouretedal HR, Vosoughi V. Preparation and characterization
of ibuprofen nanoparticles by using solvent/antisolvent precipitation. Open
Conf Proc J 2011;2:88-94.
9. George S, Vasudevan D. Studies on the preparation, characterization, and
solubility of 2-HP--cyclodextrin-meclizine HCl inclusion complexes.
J Young Pharm 2012;4:220-7.
10. Nicolescu C, Arama C, Monciu C. Preparation and characterization
11.
12.
13.
1.
14
14.
15.
16.
17.
18.
19.
20.
21.
of inclusion complexes between repaglinide and -cyclodextrin,
2-hydroxypropyl--cyclodextrin and randomly methylated -cyclodextrin.
Farmacia 2010;58:78-83.
Ghorab MM, Babiker ME. Formulation and in vitro evaluation of isotritinoin
tablets. J Chem Pharm Res 2012;4:2817-31.
Zhang D, Tan T, Gao L, Zhao W, Wang P. Preparation of azithromycin
nanosuspensions by high pressure homogenization and its physicochemical
characteristics studies. Drug Dev Ind Pharm 2007;33:569-75.
Kesisoglou F, Panmai S, Wu Y. Nanosizing oral formulation
development and biopharmaceutical evaluation. Adv Drug Deliv Rev
2007;59:631-44.
Bandi N, Wei W, Roberts CB, Kotra LP, Kompella UB. Preparation of
budesonide- and indomethacin-hydroxypropyl-beta-cyclodextrin (HPBCD)
complexes using a single-step, organic-solvent-free supercritical fluid
process. Eur J Pharm Sci 2004;23:159-68.
Kosoglou T, Statkevich P, Johnson-Levonas AO, Paolini JF, Bergman AJ,
Alton KB. Ezetimibe: a review of its metabolism, pharmacokinetics and
drug interactions. Clin Pharmacokinet 2005;44:467-94.
Bali V, Ali M, Ali J. Nanocarrier for the enhanced bioavailability of a
cardiovascular agent: in vitro, pharmacodynamic, pharmacokinetic and
stability assessment. Int J Pharm 2011;403:46-5.
Bali V, Ali M, Ali J. Study of surfactant combinations and development of a
novel nanoemulsion for minimising variations in bioavailability of ezetimibe.
Colloids Surf B Biointerfaces 2010;76:410-20.
Dixit RP, Nagarsenker MS. Self-nanoemulsifying granules of ezetimibe:
design, optimization and evaluation. Eur J Pharm Sci 2008;35:183-92.
Bandyopadhyay S, Katare OP, Singh B. Optimized self nano-emulsifying
systems of ezetimibe with enhanced bioavailability potential using long
chain and medium chain triglycerides. Colloids Surf B Biointerfaces
2012;100:50-61.
Gulsun T, Gursoy RN, Oner L. Design and characterization of
nanocrystal formulations containing ezetimibe. Chem Pharm Bull (Tokyo)
2011;59:41-5.
Parmar KR, Shah SR, Sheth NR. Studies in dissolution enhancement of
ezetimibe by solid dispersions in combination with a surfactant adsorbent.
Dissolution Technol 2011;55-61.
Journal of Young Pharmacists
Vol 6 Issue 1 Jan-Mar 2014
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Cod Liver Oil EmulsionDocument2 paginiCod Liver Oil EmulsionHaroon Rahim75% (4)
- Regulatory AffairsDocument14 paginiRegulatory AffairsSiddarth Reddy100% (2)
- ACI 523.1 (1992) Guide For Cast-In-Place Low-Density ConcreteDocument8 paginiACI 523.1 (1992) Guide For Cast-In-Place Low-Density Concretephilipyap0% (1)
- High Frontier 3rd Card ListDocument14 paginiHigh Frontier 3rd Card ListfireheartÎncă nu există evaluări
- Thermal Insulation Hot ServiceDocument19 paginiThermal Insulation Hot Serviceசரத்குமார் தமிழ்செல்வம்100% (1)
- ACECLOFENAC TabletsDocument6 paginiACECLOFENAC TabletsHaroon RahimÎncă nu există evaluări
- Milling PDFDocument5 paginiMilling PDFHaroon RahimÎncă nu există evaluări
- 5580 D 298 C 81 A 9Document6 pagini5580 D 298 C 81 A 9MuhammadAmdadulHoqueÎncă nu există evaluări
- GLIMEPIRIDE in DogsDocument10 paginiGLIMEPIRIDE in DogsHaroon RahimÎncă nu există evaluări
- Lecture DryersDocument20 paginiLecture DryersHaroon RahimÎncă nu există evaluări
- Pharmaceutical ChemistryDocument1 paginăPharmaceutical ChemistryHaroon RahimÎncă nu există evaluări
- Drying 1Document5 paginiDrying 1Haroon RahimÎncă nu există evaluări
- Drying 1Document5 paginiDrying 1Haroon RahimÎncă nu există evaluări
- GMP and CGMP Considerations PDFDocument9 paginiGMP and CGMP Considerations PDFHaroon RahimÎncă nu există evaluări
- GMP and CGMP Considerations PDFDocument9 paginiGMP and CGMP Considerations PDFHaroon RahimÎncă nu există evaluări
- GMP and CGMP Considerations PDFDocument9 paginiGMP and CGMP Considerations PDFHaroon RahimÎncă nu există evaluări
- Pharmaceutical Biochemistry ContentsDocument1 paginăPharmaceutical Biochemistry ContentsHaroon Rahim100% (1)
- Lecture On Heat Transfer and Conduction in Industrial PharmacyDocument17 paginiLecture On Heat Transfer and Conduction in Industrial PharmacyHaroon Rahim100% (2)
- Sterile ProductsDocument24 paginiSterile ProductsHaroon Rahim100% (1)
- Dryers in Word FileDocument5 paginiDryers in Word FileHaroon RahimÎncă nu există evaluări
- Spray Dryer & Freeze DryerDocument20 paginiSpray Dryer & Freeze DryerHaroon RahimÎncă nu există evaluări
- Environmental MonitoringDocument19 paginiEnvironmental MonitoringHaroon RahimÎncă nu există evaluări
- Milling PDFDocument5 paginiMilling PDFHaroon RahimÎncă nu există evaluări
- Spray Dryer & Freeze DryerDocument20 paginiSpray Dryer & Freeze DryerHaroon RahimÎncă nu există evaluări
- Flurbiprofen ArticleDocument8 paginiFlurbiprofen ArticleHaroon RahimÎncă nu există evaluări
- Eights Easures I-The Metric System:: Z Z Z Z Z ZDocument27 paginiEights Easures I-The Metric System:: Z Z Z Z Z ZHaroon RahimÎncă nu există evaluări
- Weights Measures FinalDocument2 paginiWeights Measures FinalHaroon RahimÎncă nu există evaluări
- RCF To RPMDocument1 paginăRCF To RPMHaroon RahimÎncă nu există evaluări
- Aceclofenac NanouspensionDocument4 paginiAceclofenac NanouspensionHaroon RahimÎncă nu există evaluări
- Classification of DrugsDocument2 paginiClassification of DrugsHaroon RahimÎncă nu există evaluări
- Review NanoDocument7 paginiReview NanoHaroon RahimÎncă nu există evaluări
- RCF To RPMDocument1 paginăRCF To RPMHaroon RahimÎncă nu există evaluări
- GB PR May 2012 Featured ArticleDocument16 paginiGB PR May 2012 Featured ArticleRia DeviÎncă nu există evaluări
- Industrial Practicals ManualDocument26 paginiIndustrial Practicals ManualHaroon Rahim40% (5)
- Equipo 6Document7 paginiEquipo 6Iris CsmÎncă nu există evaluări
- Geotechnical ENGGDocument10 paginiGeotechnical ENGGUjjwal GuptaÎncă nu există evaluări
- Electrochemistry Part 1Document19 paginiElectrochemistry Part 1Jenny ArutaÎncă nu există evaluări
- Mitsubishi AcDocument28 paginiMitsubishi AcZeeshanÎncă nu există evaluări
- High Temprature and High Pressure 2Document16 paginiHigh Temprature and High Pressure 2Sushmita SatiÎncă nu există evaluări
- Microbial Identification in The Pharmaceutica IndustryDocument11 paginiMicrobial Identification in The Pharmaceutica IndustrySurendar KesavanÎncă nu există evaluări
- Paints Coatings Novel Teta Free Polyamides 2k Epoxy SystemsDocument10 paginiPaints Coatings Novel Teta Free Polyamides 2k Epoxy SystemsHugo WizenbergÎncă nu există evaluări
- Characterization of Iron Oxide Thin Film Prepared by The Sol-Gel MethodDocument2 paginiCharacterization of Iron Oxide Thin Film Prepared by The Sol-Gel MethodBryan Anders AguilarÎncă nu există evaluări
- Celuloza MicrocristalinaDocument5 paginiCeluloza MicrocristalinaAna VicoveanuÎncă nu există evaluări
- Target Iit-Jee: DATE: 12-12-2014Document8 paginiTarget Iit-Jee: DATE: 12-12-2014asuhassÎncă nu există evaluări
- Bond Work IndexDocument7 paginiBond Work IndexJaime Alberto Sanchez CardonaÎncă nu există evaluări
- 120:360 - Biochemistry Fall 2015 Sample Questions For Exam 1Document5 pagini120:360 - Biochemistry Fall 2015 Sample Questions For Exam 1BluedevÎncă nu există evaluări
- Front Page To Chapter 5Document28 paginiFront Page To Chapter 5Alex DGÎncă nu există evaluări
- Lesson Plan CHE430/ CHE495 Organic Chemistry/ Hydrocarbon Chemistry Faculty of Chemical Engineering Universiti Teknologi MaraDocument9 paginiLesson Plan CHE430/ CHE495 Organic Chemistry/ Hydrocarbon Chemistry Faculty of Chemical Engineering Universiti Teknologi MaraMalik HamzaÎncă nu există evaluări
- TilesDocument84 paginiTilesgagan raoÎncă nu există evaluări
- BS Chemical EngineeringDocument110 paginiBS Chemical EngineeringhorasiusÎncă nu există evaluări
- Materials For Bridge Deck Waterproofing Membrane SystemsDocument2 paginiMaterials For Bridge Deck Waterproofing Membrane SystemstenÎncă nu există evaluări
- Catnic LintelsDocument68 paginiCatnic LintelsAlisa BendasÎncă nu există evaluări
- Zeon Productguide 20150717Document16 paginiZeon Productguide 20150717khushboo.mamtani2932Încă nu există evaluări
- Nano Coating Application For Corrosion Reduction in Oil and Gas Transmission Pipe: A Case Study in South of IranDocument7 paginiNano Coating Application For Corrosion Reduction in Oil and Gas Transmission Pipe: A Case Study in South of IranInternational Journal of Science and Engineering InvestigationsÎncă nu există evaluări
- Science of The Total Environment: M. Andersson, T.E. Finne, L.K. Jensen, O.A. EggenDocument13 paginiScience of The Total Environment: M. Andersson, T.E. Finne, L.K. Jensen, O.A. EggenSyahrul RamadhanÎncă nu există evaluări
- CALIBER PAINTBALL MARKER ManualDocument2 paginiCALIBER PAINTBALL MARKER Manualnick18Încă nu există evaluări
- Engineering Materials: Mechanism in MetalsDocument38 paginiEngineering Materials: Mechanism in Metalssamurai7_77Încă nu există evaluări
- FloPro SFDocument4 paginiFloPro SFLoganBohannonÎncă nu există evaluări
- (Courseware) ICSE: Mendeleev's Periodic TableDocument39 pagini(Courseware) ICSE: Mendeleev's Periodic Tableorigami ninjaÎncă nu există evaluări
- Dioscorea HispidaDocument9 paginiDioscorea HispidaHorcruxesÎncă nu există evaluări