Documente Academic
Documente Profesional
Documente Cultură
Managing Mental Illness in Patients From CALD Backgrounds: Psychiatry
Încărcat de
1234chocoTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Managing Mental Illness in Patients From CALD Backgrounds: Psychiatry
Încărcat de
1234chocoDrepturi de autor:
Formate disponibile
Psychiatry CLINICAL PRACTICE
Managing mental illness
in patients from CALD
backgrounds
Litza A Kiropoulos, BEd-Sc, BSc (Hons) Psych, MClinPsych, PhD (Psych), is a Research Fellow,
Department of General Practice, Monash University, Victoria. litza.kiropoulos@med.monash.edu.au
Grant Blashki, MD, FRACGP, is Senior Research Fellow, Department of General Practice, Monash University, Victoria,
and Honorary Senior Lecturer, Health Services Research Department, Institute of Psychiatry, Kings College London.
Steven Klimidis, BSc (Hons) Psych, PhD (ClinPsych), is Associate Professor and Research Co-ordinator, Centre for
International Mental Health, University of Melbourne and Victorian Transcultural Psychiatry Unit, Victoria.
BACKGROUND
Australian general practitioners are often the first point of call for people seeking
mental health care including those from culturally and linguistically diverse (CALD)
backgrounds, some of whom may be more at risk of having a mental illness but are
failing to access the appropriate mental health care.
OBJECTIVE
This article is intended to assist GPs in the recognition, diagnosis and management
of mental illness in patients from CALD backgrounds by providing current research
evidence and presenting some practical recommendations. More attention is paid to the
larger CALD populations such as the southern European and Asian communities, and
does not deal with indigenous Australians.
DISCUSSION
There is an increasing call for GPs to have a key role in the detection, diagnosis and
management of mental illness, including for patients from CALD backgrounds. Effective
care requires that GPs are aware of, and understand how culture may influence
recognition, diagnosis and management of mental illness in this group of patients.
significant proportion of Australias
population consists of people from culturally
and linguistically diverse (CALD) backgrounds.
According to the Australian 2001 Census,
28% of the Australian population were born
overseas; 15% in a non-English speaking
country (Table 1). 1 Notably, older persons
from CALD are becoming a substantial
subgroup among the Australian population;
by 2026 it is projected that one in four
people aged 70 years and over will be from
a CALD background.2 These figures will have
significant implications for general practice
as general practitioners are often the first
point of contact for people requiring mental
health care. However, even though census
data has indicated that 15% of the Australian
population is from a CALD background, only
7% of encounters with GPs were recorded
for CALD people in a national survey of GP-
patient encounters. 3 These consultations
were less likely to involve a psychological
or social problem than patients from an
English speaking background.3 Research also
suggests that people from CALD backgrounds
often prefer to consult with GPs who are of
the same ethnic background or who speak
the same primary language as themselves.4
Research regarding differences in rates of
mental illness in CALD populations compared
with their Australian born counterparts has
been equivocal. The National Health and
Wellbeing Survey found little difference
in rates of affective and anxiety disorders
between people from CALD backgrounds
and Anglo-Australians 5 (although the study
excluded those who could not speak English
sufficiently well to complete the interviews).
However, more recent Australian studies
employing culturally sensitive research
methodology (ie. interview in participant's
own language) have shown that people from
CALD backgrounds have higher levels of
depression and anxiety than their AngloAustralian counterparts. 4,6 The discrepancy
between the low level of GP consultations
involving social and psychological problems
found in CALD populations, and higher
rates of mental illness noted in some
Reprinted from Australian Family Physician Vol. 34, No. 4, April 2005 4 259
Clinical practice: Managing mental illness in patients from CALD backgrounds
CALD populations, have been attributed
to a number of factors related to the
presentation of illness by the patient and
the underdetection, misdiagnosis and
management of mental illness by GPs.
What is culture?
Culture has been defined as a shared
learned behavior transmitted from one
generation to another for purposes of
individual and societal growth, adjustment
and adaptation.7 It is represented externally
as artefacts, roles, and institutions, and
internally as values, beliefs, attitudes and
biological functioning. 7 The term 'culture'
also refers to the shared heritage and social
distinctiveness of the multiplicity of the
ethnic components within a community.
However, it is important to note that it is
impossible to generalise characteristics of
a particular culture to all members of that
group, as not all members subscribe to the
values, beliefs or behaviours common to that
group and members have different levels of
acculturation to mainstream culture.8
Presentation, detection and
diagnosis of mental illness
The influence of culture
Mental illness in different cultures constitutes
different forms of social reality 9 and
needs to be understood within the cultural
context. Cultural factors shape mental illness
including how it is understood and explained,
its experience and manifestation, and its
course and epidemiology.10,11 Some factors
influenced by culture affecting the GP-patient
interaction include: somatisation, explanatory
models, perception of the GP by the
patient, the patients social context, stigma
associated with mental illness, language
difficulties, the GP setting, the role of family
and other social networks and expectations
of medication and religious beliefs.
Somatisation
Cultural variations have been noted in the
expression and presentation of mental
illness in general practice.12 Patients from
some CALD backgrounds who have a mental
illness may present more often to their
GP with somatic rather than psychological
symptoms. 1315 This has been termed
somatisation and can be understood as
a culturally appropriate way of expressing
discomfort in many cultures. 13,16,17 For
example, CALD patients might complain to a
GP of somatic symptoms such as insomnia,
headaches, lethargy, abdominal, muscular,
back and joint pains, rather than low mood
or negative thoughts.15,18
Explanatory models
Detection of mental illness in general
p r a c t i c e c a n b e i n f l u e n c e d by t h e
patients conceptualisation of the illness
experience or their explanatory model.19 An
explanatory model relates to the meaning
of illness, specifically, what constitutes
the views of causes, important symptoms,
course, consequences, and treatments or
remedies.20 All aspects of the explanatory
model are influenced and shaped by culture
and social factors such as socioeconomic
status and education, 21 and can influence
help seeking, compliance with treatment
and patient satisfaction.22
Cultural variation in explanatory models is
particularly relevant to causal attributions of
mental illness. For example, psychosomatic
causation is widely accepted by southern
Europeans for anxiety or depression. 23
Indeed, in much of Italian and Greek culture
nerves or nervous breakdowns are not
highly stigmatised but are viewed instead as
common, often minor, afflictions.23 The typical
treatment of nerves may include prayer,
efforts to adopt a better attitude or seek a
change in the social or physical environment.23
Additionally, causal beliefs about mental
illness in older people of southern European
cultures have included witchcraft, demonic
forces and supernatural explanations,
especially in females of low socioeconomic
status and low educational levels, and those
that migrated from rural areas.24 Therefore,
GP consultations with patients from CALD
backgrounds may require a negotiation of
explanatory models where differences in
belief systems are acknowledged and
260 3Reprinted from Australian Family Physician Vol. 34, No. 4, April 2005
Table 1. Australian 2001 census data:
birthplace by country for NESB*
Country
% NESB
population
Italy
1.15
Vietnam
0.82
China
0.70
Greece
0.61
Germany
0.57
Philippines
0.55
India
0.50
Netherlands
0.44
Malaysia
0.41
Lebanon
0.38
Poland
0.30
Yugoslavia
0.29
Sri Lanka
0.28
Croatia
0.27
Indonesia
0.25
Malta
0.24
Fiji
0.23
FYROM**
0.23
Republic of South Korea
0.20
Singapore
0.18
Egypt
0.17
Turkey
0.16
France
0.09
Born elsewhere overseas*** 3.70
* non-English speaking background
** Former Yugoslav Republic of Macedonia
*** born elsewhere overseas (includes
inadequately described, at sea, not elsewhere
classified)
respected. Questions around the patients
view of mental illness will elicit information
about their explanatory model. Table 2
provides questions that can be used by GPs
to elicit CALD patients explanatory models
based on Kleinmans20 original concepts of
health and sickness and the Short Explanatory
Model Interview (SEMI).25
Perception of the GP
Patients from CALD backgrounds may have
different expectations, concerns, meanings
and values about GPs, and may view the GP as
the expert on physical illness. They may think
their role as patient is to present and describe
their physical illness; in part this may explain
the high rate of somatic presentations to GPs.
Clinical practice: Managing mental illness in patients from CALD backgrounds
It may also explain why emotional, social and
psychological difficulties are less often reported
to a GP, as the problem may not be considered
relevant or appropriate to report to a GP.20,26
Some studies suggest that different
communication styles in patients from
CALD backgrounds may be characterised
by a less direct and assertive manner. 27
This may explain why patients sometimes
readily agree with the treatment plan (in
order to please the physician) but do not
comply. Other studies suggest that patients
from CALD backgrounds may expect a
more authoritarian GP in the patient-doctor
relationship, often resulting in passive
acceptance of treatment and low demand
for education about medication.28
Patients social context
Mental illness may be strongly influenced
by adverse social circumstances and may
alert the GP to the possibility of a mental
illness.29,30 For example, factors affecting the
clinical presentation may include the political
context of arrival, reasons for migration (eg.
refugee, economic), level of contact with the
Table 2. Eliciting explanatory models of illness in CALD patients
Nature and causes of the problem
When did you first notice that there was a problem?
Why do you think that the problem began when it did?
What do you call this problem? What is its name?
How long ago did you first notice these problems?
What do you think caused this problem?
Do you think that this problem is an illness?
Australian majority group, level of exposure to
high risk industries, and lower postmigration
employment status relative to education.
Recent adverse life events (>1 in the past
year) could be seen as a reliable indicator of
mental illness in CALD patients, in addition
to multiple visits to the GP (>10 visits per
year). Therefore, those patients from CALD
backgrounds who have had recent adverse
life events or who attend the GP frequently,
warrant particular attention regarding their
psychological wellbeing.
Patients from CALD backgrounds are also
more likely to present to the GP at a later stage
of their mental illness, tolerating a great deal
of emotional and psychological distress before
seeking professional assistance.13 Patients may
consult a GP after having consulted a number
of other culturally appropriate healers, or may
be using other culturally sanctioned remedies
and rituals for their mental health.13
Stigma
Important symptoms of the problem
What do you think are the most troublesome aspects of this problem?
Which symptoms trouble you most?
Development and course of problem
How did the problem develop with time up to now?
How do you think this problem may develop and progress over time in the future?
Do you think the condition would become worse, improve or stay the same, or come
and go over time?
Severity and consequences of the problem
How serious do you think this problem is?
What are the most and least troublesome aspects of the problem?
What are the main difficulties your problem has caused you? How does the problem
affect your relationships, work/study, family role and responsibilities, attending to
your daily needs?
Treatment and help seeking for problem
Is there a particular way that people in your culture/ethnic group deal with this type
of problem? What is usually done?
Is this relevant to do in your case?
What do you think will be effective to help with this problem in your case?
What do you think you can do to help with this problem?
How do you think I can help with this problem?
(If medicine is asked for) Do you think the medicine will cure the problem or just help
control it? How quickly do you expect the medicine to do this?
The stigma associated with having a mental
illness may be particularly strong in some
CALD populations and this affects symptom
disclosure and help seeking behaviour. This may
be one of the explanations for presentation with
somatic symptoms as these may be viewed
as more socially benign than a psychological
problem.31,32 Depressive symptoms may be
seen as socially disadvantageous, and in some
cultures may interfere with marriage prospects,
diminish social status, and compromise the
self esteem required to perform effectively in
society.31,32
Language difficulties
Language preferences affect selection of GPs
by people from CALD backgrounds with
recent surveys showing that 39.5% of nonEnglish speaking patient consultations were
where the GP consulted in a language other
than English,3 and 78% of CALD patients
with poor English proficiency attended
bilingual GPs.4 For nonbilingual GPs, a trained
interpreter should be used to ensure a
meaning orientated translation. Interpreters
are available through the Translating and
Interpreting Service (www.immi.gov.au/tis/) or
Reprinted from Australian Family Physician Vol. 34, No. 4, April 2005 4 261
Clinical practice: Managing mental illness in patients from CALD backgrounds
VITS (www.vits.com.au/services/interpreting.
htm). Using an interpreter will help avoid
mistranslations of biomedical concepts and
errors of omission. An interpreter is preferred
over a family member as the patient may
not want to disclose information in front of
family and/or the family member may add
their own interpretations.
General practice setting
Underdetection of mental illness in general
practice is a complex issue that may be
exacerbated by difficulties in eliciting a
psychiatric history from CALD patients.33 For
example, GPs have been shown to diagnose
CALD patients using more limited indicators of
depression (ie. depressed appearance, sleep
disturbance, weight and appetite changes)
and are more likely to detect more severe
mental illness in general practice.33 Therefore
GPs need to be alert to the early signs of
emotional difficulties in CALD patients.
Role of family and friends
In many cultures, family members and close
friends play a key role in the patients health
care and often accompany the patient,
especially if they have limited English skills.
The GP needs to make sure that the patient
has explicitly given permission for any
discussions that might violate the patients
confidentiality. Where strong collectivistic
values typify the culture, the GP should be
aware that they may be negotiating treatment
with the entire family even if they are not
present. Acknowledging the importance of
other family members and accommodating
their views of the treatment is often essential
to adherence to the treatment plan.
Pharmacological management
N o n c o m p l i a n c e w i t h p s y ch o t r o p i c
medications appears to be more problematic
and prevalent in some nonwestern
cultures. 34 In recent years, research has
found significant differences among ethnic
groups in their response and propensity
to side effects of medications related to
genotypic variations in drug metabolising
isoenzymes. 3537 These differences lead to
variability in pharmacokinetics (ie. absorption,
distribution, metabolism and excretion) and
pharmacodynamics (ie. drug response to
psychotropic agents).38 Metabolism is regarded
as the most significant factor in determining
inter-individual and inter-ethnic differences.39,40
While a detailed description of these
differences is beyond the scope of this article,
GPs should consider variable metabolism
between ethnic groups before prescribing
psychotropics such as antidepressants,
benzodiazepines or antipsychotic medications.
Expectations of medications
Expectations of drug effects are strongly
influenced by a patients cultural origin. For
example, in some studies, patients from a
CALD background are more likely to have
negative attitudes toward medications and to
have poorer medication adherence.34 In some
studies, Chinese patients commonly perceived
that western medicines were more potent and
had greater adverse side effects than herbal
or traditional therapies.41 In another study
examining the side effects of lithium in Chinese
patients, although the actual side effect profile
was similar to caucasians, Chinese patients
showed more concern about fatigue and
drowsiness and were less concerned about
polydipsia and polyuria as such side effects
were regarded as a way of removing toxins
from the body.28 A further study found that
even though Chinese patients expected
western medicines to act quickly, they did not
expect them to treat the underlying condition.42
Religious beliefs
Religious beliefs may also affect compliance
with medication in people from CALD
backgrounds. For example, changes in intake
time and dosing of medication by some Muslim
patients during Ramadan have been found,
often without seeking GP advice.43 As efficacy
and toxicity of psychotropic medications can
vary depending on the time of administration
and their interaction with food intake, GPs
must consider religious beliefs when advising
patients. This is even more relevant for drugs
with a narrow therapeutic index as the risk of
toxicity or side effects are higher.43
262 3Reprinted from Australian Family Physician Vol. 34, No. 4, April 2005
Referral
General practitioners are the most common
referral source to specialist mental health
services for people experiencing a mental
illness and studies suggest that people from
CALD backgrounds are accessing specialist
mental health services at a lower rate compared
to the Australian born population.4 General
practitioners should familiarise themselves with
bilingual mental health professionals and ethnospecific services where they can refer CALD
patients or receive specific advice regarding
assessment and treatment.
Conclusion
General practitioners play a key role in the
detection, diagnosis and management of
CALD patients with mental illness, although
more research is clearly needed. Effective
care requires understanding and awareness
of how culture may affect the patient, GP, and
setting factors. The complex task of managing
mental illness in CALD populations can be
made easier by better understanding of the
patients culture, social and family context,
their explanatory models, their perception of
the GP, and the stigma associated with mental
illness. Additionally, GPs need to be aware of
factors contributing to the variable metabolism
of medications across CALD groups.
Summary of important points
Negotiate explanatory models with
your patient.
Be aware of the stigma that mental
illness may carry in some cultures.
Use interpreters to facilitate the GPpatient interaction.
Involvement of family and friends may
facilitate the GP-patient consultation
and treatment compliance.
Pharmacological effects may differ in
patients from CALD backgrounds.
Conflict of interest: none declared.
References
1.
2.
National Census of Population and Housing Data 2001.
Basic community profile, Australia. Canberra: Australian
Bureau of Statistics, 2001. (ABS Catalogue No. 2001.0).
Gibson D, Braun P, Benham C, Mason F. Projections of
older immigrants: people from culturally and linguistically
diverse backgrounds, 19962026. Canberra: Australian
Clinical practice: Managing mental illness in patients from CALD backgrounds
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
Institute of Health and Welfare, 2001.
Knox SA, Britt H. A comparison of general practice
encounters with patients from English speaking and
non-English speaking backgrounds. Med J Aust
2002;177:98101.
Stuart GW, Klimidis S, Minas IH. The treated prevalence of mental disorder amongst immigrants and the
Australian born: community and primary care rates. Int J
Soc Psychiatry 1998;44:2234.
McLennan W. Mental health and wellbeing: profile of
adults, Australia, 1997. Canberra: Australian Bureau of
Statistics, 1998. (ABS Catalogue No: 4326.0).
Kiropoulos LA, Klimidis S, Minas IH. Depression and
anxiety: a comparison of older aged Greek born immigrants and Anglo Australians in Melbourne. Aust NZ J
Psychiatry 2004;38:71424.
Marsella AJ. Cross-cultural research on severe mental
disorders: issues and findings. Acta Psychiatr Scand
1988;78:722.
Rosenthal D, Ranieri N, Klimidis S. Vietnamese adolescents in Australia: relationships between perceptions of
self and parental values, intergenerational conflict, and
gender dissatisfaction. Int J Psychology 1996;31:8191.
Good B, Kleinman A. Culture and depression: studies in
the anthropology and cross-cultural psychiatry of affect
and disorder. Berkeley: University of California Press,
1985.
Kirmayer LJ. Cultural variations in the clinical presentation of depression and anxiety: implications for diagnosis
and treatment. J Clin Psychiatry 2001;62:228.
Marsella AJ, Kaplan A, Suarez E. Cultural considerations
for understanding, assessing and treating depressive experience and disorder. In: Reinecke MA, Davison MR,
editors. Comparative treatments of depression. New York,
NY: Springer, 2000.
Bhui K, Bhugra D, Goldberg D. Causal explanations of
distress and general practitioners assessments of common
mental disorders among Punjabi and English attendees.
Soc Psychiatry Psychiatr Epidemiol 2002;37:3845.
Chan B, Parker G. Some recommendations to assess
depression in Chinese people in Australasia. Aust NZ J
Psychiatry 2004;38:1417.
Gater R, De Almeida e Sousa B, Barrientos G, et al.
The pathways to psychiatric care: a cross-cultural study.
Psychol Med 1991;21:76174.
Husain N, Creed F, Tomenson B. Adverse social circumstances and depression in people of Pakistani origin in the
UK. Br J Psychiatry 1997;171:4348.
Gureje O, Simon GE, Ustun TB, Goldberg DP.
Somatisation in cross-cultural perspective: a world health
organisation study in primary care. Am J Psychiatry
1997;154:98995.
Comino EJ, Silove D, Manicavasagar V, Harris E, Harris
MF. Agreement in symptoms of anxiety and depression
between patients and the GPs: the influence of ethnicity.
Fam Pract 2001;18:717.
Phan T, Silove D. The influence of culture on psychiatric assessment: the Vietnamese refugee. Psychiatr Serv
1997;48:8690.
Bhui K, Bhugra D. Explanatory models for mental distress: implications for clinical practice and research. Br J
Psychiatry 2002;181:67.
Kleinman A. Patients and healers in the context of culture.
Berkeley: University of California Press, 1980.
Carillo JEA, Green AR, Betancourt JR. Cross-cultural
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
primary care: a patient based approach. Ann Intern Med
1999;30:82934.
Jacob KS, Bhugra D, Lloyd KR. Common mental disorders, explanatory models and consultation behaviour
among Indian women living in the UK. J R Soc Med
1998;91:6671.
Kirmayer LJ, Young A, Robbins JM. Symptom attribution
in cultural perspective. Can J Psychiatry 1994;39:58495.
Meiser B, Gurr R. Non-English speaking persons perceptions of mental illness and associated needs: an explanatory
study of Arabic-, Greek- and Italian-speaking communities in New South Wales. Health Promotion Journal of
Australia 1996;6:449.
Lloyd KR, Jacob KS, Patel V, St Louis L, Bhugra D,
Mann AH. The development of the Short Explanatory
Model Interview (SEMI) and its use among primary care
attenders with common mental disorders. Psychol Med
1998;28:12317.
Parker G, Gladstone G, Chee KT. Depression in the
planets largest ethnic group: the Chinese. Am J Psychiatry
2001;158:85764.
Gao G, Ting-Toomey S, Gudykunst WB. Chinese
communication processes. In: Bond MH, editor. The
handbook of Chinese psychology. Hong Kong: Oxford
University Press, 1996;28093.
Lee S. Side effects of chronic lithium therapy in Hong
Kong Chinese: an ethnopsychiatric perspective. Cult Med
Psychiatry 1993;17:30120.
Odell SM, Surtees PG, Wainwright NWJ, Commander
MJ, Sashidharan SP. Determinants of general practitioner
recognition of psychological problems on a multi-ethnic
inner-city health district. Br J Psychiatry 1997;171:537
41.
Maginn S, Boardman AP, Craig TKJ, Hadad M, Heath
G, Stott J. The detection of psychological problems by
general practitioners: influence of ethnicity and other
demographic variables. Soc Psychiatry Psychiatr Epidemiol
2004;39:46471.
Bakshi L, Rooney R, ONeill K. Working transculturally
to reduce the stigma surrounding mental illness amongst
non-English speaking background communities: a guide.
Melbourne: Australian Transcultural Mental Health
Network, 1999.
Raguram R, Weiss MG, Channabasavanna SM, Devins
GM. Stigma, depression and somatization in South India.
Am J Psychiatry 1996;153:10439.
Mihalopoulos C, Pirkis J, Naccarella L, Dunt D. The role
of general practitioners and other primary care agencies in
transcultural mental health care. Melbourne: Australian
Transcultural Mental Health Network, 1999.
Li KM, Poland RE, Nakasaki G. Psychopharmacology
and psychobiology of ethnicity. Washington, DC:
American Psychiatric Press, 1993.
Ng C-H, Schweitzer I, Norman T, Easteal S. The emerging role of pharmacogenetics: implications for clinical
psychiatry. Aust NZ J Psychiatry 2004;38:4839.
Matthews HW. Racial, ethnic and gender differences
in response to medicines. Drug Metabol Drug Interact
1995;12:7791.
Pi EH, Gray GE. A cross-cultural perspective on psychopharmacology. Essential Psychopharmacol
1998;2:23359.
Lin K-M. Biological differences in depression and
anxiety across races and ethnic groups. J Clin Psychiatry
2001;62:1319.
39. Sjoqvist F, Borga O, Dahl M-L, Orme MLE.
Fundamentals of clinical pharmacology. In: Speight TM,
Holford NHG, editors. Averys Drug Treatment. 4th ed.
Auckland: Adis International, 1997;173.
40. Poolsup N, Li Wan Po A, Knight TL. Pharmacogenetics
and psychopharmacotherapy. J Clin Phar Ther
2000;25:197220.
41. Lee RP. Perceptions and uses of Chinese medicine
among the Chinese in Hong Kong. Cult Med Psychiatry
1980;4:34575.
42. Owan TC. Southeast Asian mental health: Treatment,
prevention, services, training, and research. Rockville,
MD: National Institute of Mental Health, 1985.
43. Aadil N, Houti IE, Moussamih S. Drug intake during
Ramadan. BMJ 2004;329:77882.
AFP
Correspondence
Email: afp@racgp.org.au
Reprinted from Australian Family Physician Vol. 34, No. 4, April 2005 4 263
S-ar putea să vă placă și
- Mental Health, Intellectual and Developmental Disabilities and the Ageing ProcessDe la EverandMental Health, Intellectual and Developmental Disabilities and the Ageing ProcessÎncă nu există evaluări
- 0408PP TrujilloDocument15 pagini0408PP TrujillojaverianaÎncă nu există evaluări
- Research Paper Topics On Mental IllnessDocument6 paginiResearch Paper Topics On Mental Illnesszufehil0l0s2100% (3)
- Cultural Competency in Health PDFDocument6 paginiCultural Competency in Health PDFMikaela HomukÎncă nu există evaluări
- Social Aspects of The Quality of Life of Persons Suffering From SchizophreniaDocument11 paginiSocial Aspects of The Quality of Life of Persons Suffering From SchizophreniaFathur RÎncă nu există evaluări
- Kleinman Culture and DepressionDocument3 paginiKleinman Culture and DepressionАлександра Курленкова100% (1)
- Outsmart Your Brain The Insider's Guide to Life-Long MemoryDe la EverandOutsmart Your Brain The Insider's Guide to Life-Long MemoryÎncă nu există evaluări
- A Framework for the Holistic Management of SchizophreniaDe la EverandA Framework for the Holistic Management of SchizophreniaÎncă nu există evaluări
- Understanding Psychological AbnormalityDocument21 paginiUnderstanding Psychological AbnormalityTitikshaÎncă nu există evaluări
- Psychology Assessment - I - M1Document42 paginiPsychology Assessment - I - M1Brinda ChughÎncă nu există evaluări
- The Health Improvement Profile: A manual to promote physical wellbeing in people with severe mental illnessDe la EverandThe Health Improvement Profile: A manual to promote physical wellbeing in people with severe mental illnessÎncă nu există evaluări
- Research Paper Mental HealthDocument5 paginiResearch Paper Mental Healthc9s9h7r7100% (1)
- Depression - Let's TalkDocument9 paginiDepression - Let's TalkThavam RatnaÎncă nu există evaluări
- Living with Bipolar: A Guide to Understanding and Managing the DisorderDe la EverandLiving with Bipolar: A Guide to Understanding and Managing the DisorderEvaluare: 2 din 5 stele2/5 (1)
- STUDENTS STRUGGLING WITH ANXIETY AND DEPRESSIONDocument10 paginiSTUDENTS STRUGGLING WITH ANXIETY AND DEPRESSIONAmie TabiÎncă nu există evaluări
- Psychology and Aging: PsychologistsDocument8 paginiPsychology and Aging: PsychologistsThamer SamhaÎncă nu există evaluări
- ECT FOR SCHIZOPHRENIADocument17 paginiECT FOR SCHIZOPHRENIAnurisÎncă nu există evaluări
- Epidemiology for Canadian Students: Principles, Methods and Critical AppraisalDe la EverandEpidemiology for Canadian Students: Principles, Methods and Critical AppraisalEvaluare: 1 din 5 stele1/5 (1)
- A Short Guide To Psychiatric DiagnosisDocument4 paginiA Short Guide To Psychiatric DiagnosisNaceiraÎncă nu există evaluări
- DSM V Def - Pink-1Document22 paginiDSM V Def - Pink-1Aarzoo MakhaniÎncă nu există evaluări
- Vacarolis Chapter OutlinesDocument181 paginiVacarolis Chapter Outlinesamashriqi100% (1)
- Eugenics as a Factor in the Prevention of Mental DiseaseDe la EverandEugenics as a Factor in the Prevention of Mental DiseaseÎncă nu există evaluări
- The Health Improvement Profile: A manual to promote physical wellbeing in people with severe mental illnessDe la EverandThe Health Improvement Profile: A manual to promote physical wellbeing in people with severe mental illnessÎncă nu există evaluări
- Neurodevelopmental Psychiatry - An Introduction For Medical StudentsDocument68 paginiNeurodevelopmental Psychiatry - An Introduction For Medical StudentsNiranjana MahalingamÎncă nu există evaluări
- Breaking the Silence: Shining a Light on Schizoid Personality DisorderDe la EverandBreaking the Silence: Shining a Light on Schizoid Personality DisorderÎncă nu există evaluări
- Is Substance Abuse Culturally Bound? Historical, Biological & Psychodiagnostic FactorsDocument19 paginiIs Substance Abuse Culturally Bound? Historical, Biological & Psychodiagnostic FactorsPriyansh JindalÎncă nu există evaluări
- Affective Disorders in Cultural Context: Laurence Kirmayer, and Danielle Groleau, PHDDocument14 paginiAffective Disorders in Cultural Context: Laurence Kirmayer, and Danielle Groleau, PHDvarhanÎncă nu există evaluări
- WHO report highlights global mental health burdenDocument29 paginiWHO report highlights global mental health burdenTet Velchez100% (1)
- Corresponding Author: Joel Adeleke AfolayanDocument29 paginiCorresponding Author: Joel Adeleke AfolayanAjoy BiswasÎncă nu există evaluări
- Mental health guidelines promote oral careDocument21 paginiMental health guidelines promote oral careKathrinaRodriguezÎncă nu există evaluări
- Bipolar Disorder Bipolar DisorderDocument3 paginiBipolar Disorder Bipolar DisorderJorgeÎncă nu există evaluări
- How cultural diversity improves healthcare outcomesDocument5 paginiHow cultural diversity improves healthcare outcomesCindy Mae CamohoyÎncă nu există evaluări
- Clinician's Guide to Chronic Disease Management of Long Term Conditions, TheDe la EverandClinician's Guide to Chronic Disease Management of Long Term Conditions, TheÎncă nu există evaluări
- UnconsciousnessDocument6 paginiUnconsciousnessSeema RahulÎncă nu există evaluări
- Definition of Disease and the Social Construction of IllnessDocument11 paginiDefinition of Disease and the Social Construction of Illnessbtailor17Încă nu există evaluări
- Introduction to Palliative Care Principles and HistoryDocument26 paginiIntroduction to Palliative Care Principles and HistoryAbdullah SakhiÎncă nu există evaluări
- Mental HealthDocument3 paginiMental Healthapi-293693569Încă nu există evaluări
- Download Wisdom Mind Mindfulness For Cognitively Healthy Older Adults And Those With Subjective Cognitive Decline Facilitator Guide Colette M Smart all chapterDocument68 paginiDownload Wisdom Mind Mindfulness For Cognitively Healthy Older Adults And Those With Subjective Cognitive Decline Facilitator Guide Colette M Smart all chapterjohn.eusebio964100% (11)
- Nourishing Minds: The Interplay of Eating and Mental HealthDe la EverandNourishing Minds: The Interplay of Eating and Mental HealthÎncă nu există evaluări
- Who PhsycogeriatriDocument6 paginiWho PhsycogeriatriWilson WilliamÎncă nu există evaluări
- Trans CulturalDocument6 paginiTrans CulturalAlyssa Santos JavierÎncă nu există evaluări
- Healing Across Cultures: Pathways to Indigenius Health EquityDe la EverandHealing Across Cultures: Pathways to Indigenius Health EquityÎncă nu există evaluări
- Research Papers On Depression in The ElderlyDocument7 paginiResearch Papers On Depression in The Elderlyojfhsiukg100% (1)
- Fatigue and Dysautonomia: Chronic or Persistent, What's the Difference?De la EverandFatigue and Dysautonomia: Chronic or Persistent, What's the Difference?Încă nu există evaluări
- Sample Research Paper On Mental IllnessDocument9 paginiSample Research Paper On Mental Illnessebvjkbaod100% (1)
- Counseling From Within: The Microbiome Mental Health ConnectionDe la EverandCounseling From Within: The Microbiome Mental Health ConnectionÎncă nu există evaluări
- Killer Diseases, Modern-Day Epidemics: Keys to Stopping Heart Disease, Diabetes, Cancer, and Obesity in Their TracksDe la EverandKiller Diseases, Modern-Day Epidemics: Keys to Stopping Heart Disease, Diabetes, Cancer, and Obesity in Their TracksÎncă nu există evaluări
- Oppositional Defiant Disorder and Conduct Disorder in ChildrenDe la EverandOppositional Defiant Disorder and Conduct Disorder in ChildrenÎncă nu există evaluări
- Mental Health Guide: For students, teachers, school psychologists, nurses, social workers, counselors and parents.De la EverandMental Health Guide: For students, teachers, school psychologists, nurses, social workers, counselors and parents.Încă nu există evaluări
- Saludamay Nursing JournalDocument76 paginiSaludamay Nursing JournalcrisjavaÎncă nu există evaluări
- FigmentDocument4 paginiFigmentanaella delacruzÎncă nu există evaluări
- Unit 1 Psychology: Mental Illness Across The LifespanDocument35 paginiUnit 1 Psychology: Mental Illness Across The Lifespanapi-116304916100% (1)
- Pokemon Theme Song 22Document4 paginiPokemon Theme Song 221234chocoÎncă nu există evaluări
- Code Geass - StoriesDocument5 paginiCode Geass - Stories1234chocoÎncă nu există evaluări
- Blue Veins Sub Theme TVBDocument4 paginiBlue Veins Sub Theme TVB1234chocoÎncă nu există evaluări
- Doctor Talk: Communication Practice Role PlaysDocument6 paginiDoctor Talk: Communication Practice Role Plays1234chocoÎncă nu există evaluări
- Fairy Tail - Main ThemeDocument3 paginiFairy Tail - Main Theme1234chocoÎncă nu există evaluări
- Osteo Infographic FinalDocument1 paginăOsteo Infographic Final1234chocoÎncă nu există evaluări
- Blue BirdDocument7 paginiBlue Bird1234chocoÎncă nu există evaluări
- QLD Rail Traim PDFDocument1 paginăQLD Rail Traim PDF1234chocoÎncă nu există evaluări
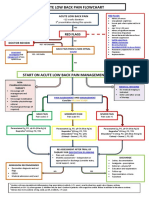
- Acute Low Back Pain Flowchart January 2017Document1 paginăAcute Low Back Pain Flowchart January 20171234chocoÎncă nu există evaluări
- Mbs Quick Guide: JULY 2020Document2 paginiMbs Quick Guide: JULY 20201234chocoÎncă nu există evaluări
- Getting the Hospital Job: A Step-by-Step Guide to Applying for Your First PositionDocument41 paginiGetting the Hospital Job: A Step-by-Step Guide to Applying for Your First Position1234chocoÎncă nu există evaluări
- Taking a Social and Cultural History: A Biopsychosocial ApproachDocument3 paginiTaking a Social and Cultural History: A Biopsychosocial Approach1234chocoÎncă nu există evaluări
- VTE GuidelinesDocument11 paginiVTE Guidelines1234chocoÎncă nu există evaluări
- Topical Steroids (Sep 19) PDFDocument7 paginiTopical Steroids (Sep 19) PDF1234chocoÎncă nu există evaluări
- Topical Steroids (Sep 19) PDFDocument7 paginiTopical Steroids (Sep 19) PDF1234chocoÎncă nu există evaluări
- USMLE Flashcards: Anatomy - Side by SideDocument190 paginiUSMLE Flashcards: Anatomy - Side by SideMedSchoolStuff100% (3)
- # 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in EDDocument7 pagini# 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in ED1234chocoÎncă nu există evaluări
- PBM Module1 MTP Template 0Document2 paginiPBM Module1 MTP Template 01234chocoÎncă nu există evaluări
- 2016 Applicant Guide Web V2Document83 pagini2016 Applicant Guide Web V21234chocoÎncă nu există evaluări
- Metro South Intern Training Form (Logan)Document3 paginiMetro South Intern Training Form (Logan)1234chocoÎncă nu există evaluări
- ImprovingMedAdherenceOlderAdultslyer Final 508CDocument2 paginiImprovingMedAdherenceOlderAdultslyer Final 508CKumar PatilÎncă nu există evaluări
- Language of PreventionDocument9 paginiLanguage of Prevention1234chocoÎncă nu există evaluări
- FLOWCHART - ARC Adult Cardiorespiratory ArrestDocument1 paginăFLOWCHART - ARC Adult Cardiorespiratory Arrest1234chocoÎncă nu există evaluări
- Fluids ElectrolytesDocument2 paginiFluids Electrolytes1234chocoÎncă nu există evaluări
- Herd Immunity'' A Rough Guide PDFDocument6 paginiHerd Immunity'' A Rough Guide PDF1234chocoÎncă nu există evaluări
- Defining and Assessing Risks To Health PDFDocument20 paginiDefining and Assessing Risks To Health PDF1234chocoÎncă nu există evaluări
- Clinical Contributions To Addressing The Social Determinants of HealthDocument5 paginiClinical Contributions To Addressing The Social Determinants of Health1234chocoÎncă nu există evaluări
- A Conceptual Framework For HealthDocument1 paginăA Conceptual Framework For Health1234chocoÎncă nu există evaluări
- The Effects of Social Networks On Disability in Older AustraliansDocument22 paginiThe Effects of Social Networks On Disability in Older Australians1234chocoÎncă nu există evaluări
- Riga Participants List FINALDocument9 paginiRiga Participants List FINALFredie IsaguaÎncă nu există evaluări
- 2 CGMPDocument78 pagini2 CGMPRICHELLE JIELEN QUEBECÎncă nu există evaluări
- Genetic Counselling Seminar for NursesDocument22 paginiGenetic Counselling Seminar for NursesGopika SÎncă nu există evaluări
- Four Handed DentistryDocument114 paginiFour Handed DentistryLie FelixÎncă nu există evaluări
- OSCE AcneDocument4 paginiOSCE AcneAliceLouisaÎncă nu există evaluări
- Potency and Dose PDF SEMINARDocument62 paginiPotency and Dose PDF SEMINARMd. Mahabub Alam100% (1)
- Interpretation MRCPCH 2009 Site: For Part 2 Exam For Part 2 ExamDocument35 paginiInterpretation MRCPCH 2009 Site: For Part 2 Exam For Part 2 Examyassine100% (1)
- 3M 9105 Wear It Right Poster PDFDocument2 pagini3M 9105 Wear It Right Poster PDFScott KramerÎncă nu există evaluări
- AURELIO-Issues, Trends and Challenges On The Care of Older Persons in The Different SettingsDocument14 paginiAURELIO-Issues, Trends and Challenges On The Care of Older Persons in The Different Settings3D - AURELIO, Lyca Mae M.0% (1)
- Welcome - Embrace QuoteEngineDocument3 paginiWelcome - Embrace QuoteEnginegabyÎncă nu există evaluări
- DLL - Pe11 - Q1 - Week 4Document5 paginiDLL - Pe11 - Q1 - Week 4Ysah Castillo Ü100% (1)
- A3 Process - A Pragmatic Problem-Solving Technique For Process Improvement in Health CareDocument11 paginiA3 Process - A Pragmatic Problem-Solving Technique For Process Improvement in Health CareNoé HumbertoÎncă nu există evaluări
- Review of Literature on School Canteen Food QualityDocument8 paginiReview of Literature on School Canteen Food QualityRich BarriosÎncă nu există evaluări
- Role of HRM in improving healthcare servicesDocument8 paginiRole of HRM in improving healthcare servicesZovana 2020Încă nu există evaluări
- Provide Care and Support To People With Special NeedsDocument13 paginiProvide Care and Support To People With Special NeedsJoshua S. Ce�idozaÎncă nu există evaluări
- Nursing ProcessDocument20 paginiNursing Processwideyatma100% (2)
- Journal of Psychiatric ResearchDocument8 paginiJournal of Psychiatric ResearchMaria CamposÎncă nu există evaluări
- CBDRP-Reporting-Forms TemplateDocument21 paginiCBDRP-Reporting-Forms TemplateKarl Anne Domingo100% (1)
- Borderline Personality Disorder in Clinical Practice: Carolyn Zittel Conklin, Ph.D. Drew Westen, PH.DDocument9 paginiBorderline Personality Disorder in Clinical Practice: Carolyn Zittel Conklin, Ph.D. Drew Westen, PH.DMarjorie AlineÎncă nu există evaluări
- International General Certificate Assessor's Marking Sheet (2011 Specification) Igc3 - The Health and Safety Practical ApplicationDocument11 paginiInternational General Certificate Assessor's Marking Sheet (2011 Specification) Igc3 - The Health and Safety Practical ApplicationVigneshwaraÎncă nu există evaluări
- Field Visit Gorai CemetryDocument4 paginiField Visit Gorai CemetryYogesh KharchanÎncă nu există evaluări
- NeuroDocument317 paginiNeuroNela Popa100% (2)
- Homeopathic First Aid For Infants and Children PDFDocument3 paginiHomeopathic First Aid For Infants and Children PDFRamesh Shah100% (1)
- Soal Kuis 7 Ppu - Bahasa Inggris: Text 1Document3 paginiSoal Kuis 7 Ppu - Bahasa Inggris: Text 1rayhan taufikÎncă nu există evaluări
- Air Force Body Composition Policy MemoDocument3 paginiAir Force Body Composition Policy MemoRichard PollinaÎncă nu există evaluări
- Effects of High Intensity Interval Training On Increasing Explosive Power, Speed, and AgilityDocument6 paginiEffects of High Intensity Interval Training On Increasing Explosive Power, Speed, and AgilityGytis GarbačiauskasÎncă nu există evaluări
- Achilles Tendon Injury Rehab Exercises GuideDocument6 paginiAchilles Tendon Injury Rehab Exercises GuideKEVIN NGUYENÎncă nu există evaluări
- Post-Partum Haemorrhage: Causes and Risk FactorsDocument12 paginiPost-Partum Haemorrhage: Causes and Risk FactorsLindha GraÎncă nu există evaluări
- Putnam Voice - 1/11/12Document10 paginiPutnam Voice - 1/11/12The Lima NewsÎncă nu există evaluări
- Cloze-Exam Practice With Key (August)Document10 paginiCloze-Exam Practice With Key (August)Mar CuervaÎncă nu există evaluări