Documente Academic
Documente Profesional
Documente Cultură
1 s2.0 S0278239105003472 Main
Încărcat de
bortho10Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
1 s2.0 S0278239105003472 Main
Încărcat de
bortho10Drepturi de autor:
Formate disponibile
TECHNICAL NOTES
J Oral Maxillofac Surg
63:1048-1051, 2005
Methylmethacrylate as a Space
Maintainer in Mandibular
Reconstruction
N. M. Goodger, FRCS, FDS, DLORCS,*
J. Wang, DMD, MD, MPH, G. W. Smagalski, DDS, FACD,
and Bradford Hepworth, DDS, MD, MS
The use of alloplastic materials in oral and maxillofacial surgery is an accepted practice with the frequent utilization of bone substitutes, titanium plates,
mesh, and various onlay grafts. Methylmethacrylate
cement is an inert and well-tolerated material that has
been used for decades in orthopedic and neurosurgical procedures. Because it is moldable prior to
curing and easily trimmed, it is of particular use in
the reconstruction of awkwardly shaped defects,
such as those created by craniectomy. However, its
use has rarely been reported in the facial bones. We
have found methylmethacrylate to be a convenient
and practical material for the temporary space
maintenance of mandibular continuity defects following resection or for osseous defects secondary
to osteomyelitis. The material provides functional
stability, allows the intraoral soft tissue defects to
heal with minimal distortion from scarring, and
creates a soft tissue envelope into which bone
grafts can later be placed. The most significant
advantage to the patient is the maintenance of facial
*Consultant Oral and Maxillofacial Surgeon, Kent and Canterbury
Hospital, Canterbury, United Kingdom.
Formerly, Resident, Department of Oral and Maxillofacial Surgery, University of California, San Francisco, San Francisco, CA;
Currently, Private Practice, Sunnyvale, CA.
Formerly, Deputy Chief of Service, Department of Oral and
Maxillofacial Surgery, San Francisco General Hospital, San Francisco, and Assistant Clinical Professor, University of California, San
Francisco, San Francisco, CA.
Formerly, Resident, Department of Oral and Maxillofacial Surgery, University of California, San Francisco, San Francisco, CA;
Currently, Private Practice, Bainbridge Island, WA.
Address correspondence and reprint requests to Dr Wang: Silicon Valley Oral and Maxillofacial Surgery, 877 W. Fremont Ave, E-1,
Sunnyvale, CA 94087; e-mail: drkvj@earthlink.net
2005 American Association of Oral and Maxillofacial Surgeons
0278-2391/05/6307-0029$30.00/0
doi:10.1016/j.joms.2005.03.024
esthetics, with little extraoral evidence of soft tissue contraction.
Report of Cases
CASE 1
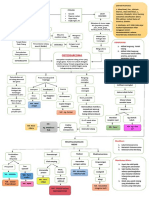
A 22-year-old man sustained a fracture of the mandibular
symphysis, failed to seek immediate treatment, and eventually developed osteomyelitis with a draining intraoral sinus
tract. Debridement of the mandibular fracture site was required, leaving a symphyseal trapezoidal defect 4 cm in
width inferiorly and 2 cm superiorly. A reconstruction plate
was applied to the mandible, a methylmethacrylate space
maintainer impregnated with 600 mg of clindamycin was
inserted into the defect region, and titanium screws were
placed to stabilize the acrylic. Postoperatively, the intraoral
communication healed without incident. Three months after the initial procedure, the patient was readmitted and the
mandible was approached through the previous submental
incision. A fibrous capsule was found encompassing the
methylmethacrylate space maintainer and the bone margins
were found to be well vascularized, after removal of a minor
amount of granulation tissue (Figs 1, 2). A corticocancellous
iliac crest bone graft was shaped, placed into the defect,
and retained with titanium screws. The surgical site was
reapproximated, and the patient healed without complication or esthetic compromise.
CASE 2
A 52-year-old man was referred to the Oral and Maxillofacial Surgery Service with a history of inadequate open
reduction and rigid fixation of bilateral body fractures of an
edentulous mandible. An actively draining orocutaneous
fistula was present in the right submandibular region and
had been present for 6 months. The left and right mandibular fracture sites were grossly mobile. The fractures were
debrided, hardware was removed, and the bilateral sites
were reconstructed with rib grafts fixed to a reconstruction
plate. Following this procedure, the patient developed adult
respiratory distress syndrome and was confined to the intensive care unit for 2 weeks. The bone graft on the right
side of the mandible became exposed intraorally and infection ensued. Four weeks after the initial procedure, the
patient was taken back to the operating room, and the
right-side bone graft was removed, the region was debrided,
and the intraoral wound was closed (Fig 3). A methylmethacrylate space maintainer impregnated with clindamy-
1048
1049
GOODGER ET AL
FIGURE 1. Case 1: Intraoperative picture of acrylic space maintainer
prior to bone graft.
Goodger et al. Methylmethacrylate as a Space Maintainer. J Oral
Maxillofac Surg 2005.
FIGURE 3. Case 2: Intraoperative appearance of defect after debridement of infected rib graft.
Goodger et al. Methylmethacrylate as a Space Maintainer. J Oral
Maxillofac Surg 2005.
CASE 3
cin and vancomycin was fabricated and secured to the
reconstruction plate (Fig 4). The extraoral wound was
closed in multiple layers. The patient made an excellent
postoperative recovery with no evidence of persisting infection or wound breakdown and then was referred for a
course of hyperbaric oxygen. Four months after placement
of the acrylic space maintainer, he was readmitted and the
methylmethacrylate was removed via an extraoral approach. A fibrous capsule was found to encompass the
acrylic, and after curetting a minor amount of granulation
tissue to expose well-vascularized bone ends, an iliac crest
corticocancellous bone graft was placed into the defect and
fixed to the reconstruction plate with titanium screws. The
decision was made to augment the contralateral bone graft
site with additional iliac crest bone at the same operative
procedure. The patient had an excellent postoperative recovery (Fig 5).
This patient is a 26-year-old, otherwise healthy man, who
originally presented to the Oral and Maxillofacial Surgery
Service with an expansile lesion of the mandible from the
right canine extending posteriorly to the condylar neck.
The lesion underwent biopsy and was found to be consistent with a cementifying fibroma. After thorough deliberation considering the extent of the lesion, the treatment
elected was a partial mandibular resection. The patient was
taken to the operating room for a resection of the right
mandible from the symphysis to within 2 cm of the condylar head. A reconstruction plate was placed from the condylar neck to the symphyseal region and then was removed
to facilitate the resection. The reconstruction plate was
then reapplied to the remaining mandibular sections, and
an alginate impression of the resected mandibular segment
FIGURE 2. Case 1: Intraoperative appearance of defect after removal of space maintainer.
FIGURE 4. Case 2: Intraoperative picture of placement of acrylic
space maintainer.
Goodger et al. Methylmethacrylate as a Space Maintainer. J Oral
Maxillofac Surg 2005.
Goodger et al. Methylmethacrylate as a Space Maintainer. J Oral
Maxillofac Surg 2005.
1050
FIGURE 5. Case 2: Panoramic radiograph showing bone graft 1
month postsurgery.
Goodger et al. Methylmethacrylate as a Space Maintainer. J Oral
Maxillofac Surg 2005.
was obtained. Methylmethacrylate was then mixed, incorporating 600 mg of clindamycin, and was poured into the
negative alginate impression. The fabricated acrylic mandibular segment was inserted into the original resection site
and was affixed to the reconstruction plate with titanium
screws. The tissues were reapproximated, and the incision
was closed in multiple layers.
The patient healed without complication and was followed for 4 months. The esthetics were excellent, with
preservation of optimal facial contours. Secondary surgical
intervention was undertaken using iliac crest bone to reconstruct the mandibular defect. The surgical site was approached through the original submandibular scar to the
level of the reconstruction plate. An incision was made
along the lateral side of the plate, and the soft tissues were
reflected, revealing a well-encapsulated acrylic space maintainer. The acrylic was easily removed, leaving a well-defined pocket for the bone graft. No additional dissection
was required, although a minor amount of granulation tissue was noted at the bone resection ends. After curettage,
the bone ends were noted to be well vascularized, were
bleeding, and had the appearance of a fresh resection. Using
the methylmethacrylate space maintainer as a template, the
corticocancellous bone graft was shaped and contoured to
fit the defect and the plate. The fibrous capsule was scored
to encourage revascularization, and the bone graft was
inserted and fixed to the reconstruction plate with titanium
screws. The incision was reapproximated in the usual multilayer fashion. The patient had a benign postoperative
course. He was followed for 14 months (Fig 6) and then
referred for placement of dental implants to facilitate crown
and bridge reconstruction. He continues to have a good
occlusion and an excellent cosmetic result with minimal
evidence of surgical intervention.
METHYLMETHACRYLATE AS A SPACE MAINTAINER
air spaces.3 The material is easily molded prior to
polymerization and has excellent structural integrity.
It is now commonly used for temporary and permanent cranioplasty and as bone cement for alloplastic
joint replacement in orthopedic surgery.4 There are
several reports in the literature of methylmethacrylate
having been used in vertebral reconstruction and for
cosmetic alloplastic procedures.59 Govila10 reported
2 cases of mandibular reconstruction, and a larger
series of combined metal and acrylic implants was
published by Benoist11 with implants being fabricated
preoperatively.
Methylmethacrylate is reported to be well tolerated
by bone and soft tissues, and this has been confirmed
in our experience.4 16 The stabilized methylmethacrylate blocks allow the overlying oral mucosa and skin
to heal without delay or wound breakdown. A fibrous
capsule formed around the implant in each of the
patients reported here, but there was no significant
bone resorption and minimal evidence of granulation
tissue. During its exothermic reaction stage, it is important to irrigate the setting methylmethacrylate
with water or saline, or to remove it from bone
contact to avoid damage to the adjacent osseous
cells.17
The incidence of toxicity of methylmethacrylate is
low. There are reports of allergy to the monomer and
occasional reports of hypotension and cardiac arrest
following its use in joint surgery. However, there is a
possible correlation to these complications when
large amounts of unbound monomer are applied to a
large bone surface area or a plunger effect results in
fat embolism.7,18,19 Also, methylmethacrylate has
been reported to be detectable in both plasma and in
breast milk following joint surgery.20,21 Considering
Discussion
Heat-cured methylmethacrylate was originally used
in the early 1940s for facial prosthetics,1 and coldcured methylmethacrylate was reported to be initially
used in cranial reconstruction in 1941.2 The structure
of hardened methylmethacrylate cement is a composite of previously polymerized granules bound by recently polymerized monomer resulting in integrated
FIGURE 6. Case 3: Section from panoramic radiograph showing
integration of bone graft 1 year postsurgery.
Goodger et al. Methylmethacrylate as a Space Maintainer. J Oral
Maxillofac Surg 2005.
GOODGER ET AL
its widespread use, methylmethacrylate has a low
incidence of associated complication.
The primary problem reported with methylmethacrylate implants in regions other than the facial bones
is infection,11,22,23 with rates near 20% at 1 to 2 years
postimplantation. These findings are supported by
Govila,10 but Benoist11 reports an infection rate of up
to 25% of cases in his series. In these situations,
nonvascularized bone grafts inevitably failed, yet
small defects may not warrant free vascularized bone
grafts such as fibula, scapula, or iliac crest with their
attendant morbidity. As the length of time of implantation increases, so does the incidence of infection.
No conclusive studies have reported short-term infection rates,16,22,23 but the risk can be limited in these
cases by the incorporation of antibiotics into the cement. It has been our experience that the implants
have not become infected even when placed in contaminated sites with associated intraoral fistula and
have permitted healing of the fistula (see patients 1
and 2). The first part of the technique described for
patients 1 and 2 has similarities to that of using antibiotic-impregnated polymethylmethacrylate beads in
the treatment of chronic osteomyelitis.24 27 In the
latter method, the mandible is usually approached by
an extraoral incision and the necrotic bone is debrided or resected. Mandibular form may be maintained with a reconstruction plate, and antibioticimpregnated methylmethacrylate beads are implanted
into the surgical site. The beads are removed 10 days
to 3 months later, and good results are reported.
However, our technique has the advantages of preservation of mandibular shape and facial soft tissue
contour, while creating an envelope into which a
bone graft can be placed when the implant is removed. This is performed 2 to 4 months after placement, minimizing the long-term infection risk and
allowing definitive bone grafting at the same procedure.
References
1. Munson FT, Heron DF: Facial reconstruction with acrylic resin.
Am J Surg 53:291, 1941
2. Kleinschmidt O: Plexiglas zur decking von schadellucken.
Chirurg 13:273, 1941
3. Cameron HU, Mills RH, Jackson RW, et al: The structure of
polymethylmethacrylate cement. Clin Orthop Rel Res 100:287,
1974
4. Robinson AC, ODwyer TP, Gullane PJ, et al: Anterior skull
defect reconstruction with methylmethacrylate. J Otolarygol
18:241, 1989
1051
5. Whitehill R, Cicoria AD, Hooper WE, et al: Posterior cervical
reconstruction with methyl methacrylate cement and wire: A
clinical review. J Neurosurg 68:576, 1988
6. Branch CL, Kelly DL, Davis CH Jr, et al: Fixation of fractures of
the lower cervical spine using methylmethacrylate and wire:
Technique and results in 99 patients. Neurosurgery 25:503,
1989
7. Rubin LR: Bone cement implantation, in Rubin LR (Ed):
Biomaterials in Reconstructive Surgery. St Louis, MO, CV
Mosby, 1983, p 452
8. Cheung LK, Samman N, Tideman H: The use of moldable
acrylic for restoration of the temporalis flap donor site. J Craniomaxillofac Surg 22:335, 1994
9. Schwartz AB, Kaufman P, Gluck M: Intraoral implantation of
methyl methacrylate for the restoration of facial contour in old
fractures of the malar complex. J Oral Surg 31:763, 1973
10. Govila A: Use of methyl methacrylate in bone reconstruction.
Br J Plast Surg 43:210, 1990
11. Benoist M: Experience with 220 cases of mandibular reconstruction. J Maxillofac Surg 6:40, 1978
12. van Mullem PJ, de Wijn JR: Bone and soft connective tissue
response to porous acrylic implants. J Craniomaxillofac Surg
16:99, 1988
13. Wellisz T, Lawrence M, Jazayeri MA, et al: The effects of
alloplastic implant onlays on bone in the rabbit mandible. Plast
Reconstr Surg 96:957, 1995
14. Worley RD: The experimental use of polymethyl methacrylate
implants in mandibular defects. J Oral Surg 31:170, 1973
15. Al-Sibahi A, Shanoon A: The use of soft polymethylmethacrylate
in the closure of oro-antral fistula. J Oral Maxillofac Surg 40:
165, 1982
16. Cabanela ME, Coventry MB, Maccarty CS, et al: The fate of
patients with methylmethacrylate cranioplasty. J Bone Joint
Surg 54:278, 1972
17. Wykman AGM: Acetabular cement temperature in arthroplasty.
Acta Orthop Scand 63:543, 1992
18. Peebles DJ, Ellis RH, Stride SDK, et al: Cardiovascular effects of
methylmethacrylate cement. Br Med J 1:349, 1972
19. Milne IS: Hazards of acrylic bone cement. Anaesthesia 28:538,
1973
20. Gentil B, Paugam C, Wolf C, et al: Methylmethacrylate plasma
levels during total hip arthroplasty. Clin Orthop Rel Res 287:
112, 1993
21. Hersh J, Bono JV, Padgett DE et al: Methyl methacrylate levels
in breast milk of a patient after total hip arthroplasty. J Arthroplasty 10:91, 1995
22. Benzel EC, Thammavaram K, Kesterson L: The diagnosis of
infections associated with acrylic cranioplasties. Neuroradiology 32:151, 1990
23. Blum KS, Schneider SJ, Rosenthal AD: Methylmethacrylate cranioplasty in children: Long-term results. Pediatr Neurosurg
26:33, 1997
24. Merholtz ET, Haneke A: Gentamycin-PMMA kugeln als topische
therapie, in Wunderer S: Der Kieferchirurgie. Septische MundKiefer-Gesichtschirurgie, Vol 29. Stuttgart, Germany, Thieme,
1984, p 69
25. Grime PD, Bowerman JE, Weller PJ: Gentamicin impregnated
polymethylmethacrylate (PMMA) beads in the treatment of
primary chronic osteomyelitis of the mandible. Br J Oral Maxillofac Surg 28:367, 1990
26. Dierks EJ, Potter BE: Treatment of an infected mandibular graft
using tobramycin-impregnated methylmethacrylate beads: Report of a case. J Oral Maxillofac Surg 50:1243, 1992
27. Chisholm BB, Lew D, Sadasivan K: The use of tobramycinimpregnated polymethylmethacrylate beads in the treatment of
osteomyelitis of the mandible: Report of three cases. J Oral
Maxillofac Surg 51:444, 1993
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- CABGDocument14 paginiCABGClaudette CayetanoÎncă nu există evaluări
- Orahex Oral SolutionDocument1 paginăOrahex Oral SolutionconanmarcÎncă nu există evaluări
- Contemporary Chinese Pulse Diagnosis A Modern InteDocument8 paginiContemporary Chinese Pulse Diagnosis A Modern InteAnkit JainÎncă nu există evaluări
- Total Gastrectomy ConsentDocument18 paginiTotal Gastrectomy ConsentTanyaNganÎncă nu există evaluări
- Prof Norhayati RMC KPJUCDocument18 paginiProf Norhayati RMC KPJUCtheskywlkrÎncă nu există evaluări
- Conjoined Twins: Bioethics, Medicine and The Law: ViewpointDocument2 paginiConjoined Twins: Bioethics, Medicine and The Law: ViewpointSulistyawati WrimunÎncă nu există evaluări
- Historical Development of Psychiatric Social Work and Role of Psychiatric Social Worker in SocietyDocument9 paginiHistorical Development of Psychiatric Social Work and Role of Psychiatric Social Worker in SocietyZubair Latif100% (7)
- Communicable Disease SurveillanceDocument60 paginiCommunicable Disease SurveillanceAmeer MuhammadÎncă nu există evaluări
- Here's Your Coronavirus Insurance: You Have Made A Wise ChoiceDocument3 paginiHere's Your Coronavirus Insurance: You Have Made A Wise ChoiceAjay Kumar GumithiÎncă nu există evaluări
- Woc Osteosarcoma WidyaDocument1 paginăWoc Osteosarcoma WidyaWidya Agustiani0% (1)
- Decreased Urine Out PutDocument11 paginiDecreased Urine Out PutHila AmaliaÎncă nu există evaluări
- Barba D, Et Al, 2021Document103 paginiBarba D, Et Al, 2021Andrea QuillupanguiÎncă nu există evaluări
- Hipaa FillableDocument2 paginiHipaa FillableRameezNatrajanÎncă nu există evaluări
- Essential Intra Natal Care 11aiDocument78 paginiEssential Intra Natal Care 11aiDr Ankush VermaÎncă nu există evaluări
- Nursing Care Plan CholecystectomyDocument2 paginiNursing Care Plan Cholecystectomyderic87% (23)
- GDMDocument30 paginiGDMCharlz ZipaganÎncă nu există evaluări
- Amputation and RehabilitationDocument4 paginiAmputation and RehabilitationimherestudyingÎncă nu există evaluări
- PhysioEx Exercise 7 Activity 1 Damagel)Document3 paginiPhysioEx Exercise 7 Activity 1 Damagel)CLAUDIA ELISABET BECERRA GONZALESÎncă nu există evaluări
- Inseparable - Prospectus With 2021 BudgetDocument9 paginiInseparable - Prospectus With 2021 BudgetAralee HenighanÎncă nu există evaluări
- Self-Monitoring of Blood Glucose in Type 2 Diabetes Recent StudiesDocument11 paginiSelf-Monitoring of Blood Glucose in Type 2 Diabetes Recent StudiesSelaÎncă nu există evaluări
- Motion To DismissDocument16 paginiMotion To DismissBasseemÎncă nu există evaluări
- Infection Control Management Plan: PurposeDocument6 paginiInfection Control Management Plan: PurposeRekhaÎncă nu există evaluări
- The Most CommonsDocument80 paginiThe Most CommonsJmee8Încă nu există evaluări
- Case Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeDocument5 paginiCase Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeSuci Triana PutriÎncă nu există evaluări
- NCMA113 FUNDA SKILL 1 Performing Medical HandwashingDocument3 paginiNCMA113 FUNDA SKILL 1 Performing Medical HandwashingJessoliver GalvezÎncă nu există evaluări
- Journal ReadingDocument3 paginiJournal ReadingRachelle Anne LetranÎncă nu există evaluări
- A Brief Sample Content of The " PACING THE PACES Tips For Passing MRCP and Final MBBS"Document24 paginiA Brief Sample Content of The " PACING THE PACES Tips For Passing MRCP and Final MBBS"Woan Torng100% (2)
- You Exec - KPIs - 169 - BlueDocument14 paginiYou Exec - KPIs - 169 - BlueEssa SmjÎncă nu există evaluări
- 2020 Mcqs Endondontic EmergencyDocument17 pagini2020 Mcqs Endondontic Emergencyareej alblowi100% (4)
- Genetic Disorders PDFDocument38 paginiGenetic Disorders PDFEllen Mae PrincipeÎncă nu există evaluări