Documente Academic
Documente Profesional
Documente Cultură
2011 Bacterial Impact Position 1.5
Încărcat de
Jason MarshallDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
2011 Bacterial Impact Position 1.5
Încărcat de
Jason MarshallDrepturi de autor:
Formate disponibile
Australian Wound Management Association Inc.
Bacterial impact on wound healing:
From contamination to infection
POSITION
PAPER
www.awma.com.au
Version 1.5
October 2011
Position Document of the Australian Wound Management Association (AWMA)
Bacterial impact on wound healing: From contamination to infection
Foreword
Health professionals face many challenges in their practice but for those tasked with healing wounds
there seems to be an abundance of situations where diagnosis and choice of appropriate therapies is not
always straightforward. The interactions between microbes and wounds create some of the more difficult
dilemmas is the delayed healing due to bacteria, do I need to swab the wound, how do I respond to the
bacteria the lab has cultured, do I use topical antiseptics or systemic antibiotics, what dressings best
handle topical infection? These are just a sample of the issues the clinician often needs to resolve. Sue
Templeton and her committee have produced this Australian Wound Management Association (AWMA)
position document to provide the clinician with the latest knowledge on the complex interactions between
bacteria and wounds, and assist them in their role as wound healer. It is not a clinical practice guideline,
as that requires a much longer and more extensive appraisal of the literature, but AWMA feel that this
document will be extremely useful. It is clear, concise and well presented- and I have no doubt it will be
widely referred to and utilised. There will be many people with wounds, currently and in the future, who
will suffer less and regain quality of life as a result of this work, and that is what we are all striving for.
Associate Professor Michael Woodward
President, Australian Wound Management Association.
Summary of recommendations:
1
2
3
4
5
6
7
8
9
10
11
12
13
14
Service providers should consider mechanisms to collect data on wound infections including
prevalence, organisms cultured and bacterial resistance in all healthcare settings. More advanced
data collection to evaluate the outcomes of wound infection such as treatment and patient
response may be considered where appropriate.
Local health authorities, service providers and practitioners should use the Australian framework
as outlined above for defining and collecting data related to surgical site infection (SSI).
Service providers and practitioners should adopt a consistent consensus framework for defining
the level of bacterial impairment of wound healing based on assessment of the patient and their
wound.
A wound management regimen should include strategies to minimise infection risk. These
strategies should be embedded in service provider protocols and practices.
All wounds should be assessed regularly for the indicators of infection and outcomes of the
assessment documented.
A wound should be considered infected if the clinical signs of local infection are present (even if
wound swab results do not indicate infection).
A wound swab should generally be taken to guide appropriate antibiotic therapy but should not be
regarded as binding.
Agents for treatment of wound infection should be tailored to the extent of infection and based on
recommended treatment guidelines.
For complex, unresponsive, recalcitrant or recurrent infections consultation with a microbiologist or
infectious disease specialist is recommended.
The length of treatment with topical and/or systemic agents should be determined by the response
of the wound and the patient.
Topical antiseptic solutions should generally be used for treatment of topical contamination or
minor skin infections and their use avoided on clean, healing wounds.
Topical antibiotics are rarely recommended for use on wounds due to the risk of resistance
developing.
Topical antimicrobials should be used judiciously for appropriate clinical indications and their use
evaluated regularly.
Regular wound assessment and documentation includes:
Identification of factors that might indicate infection and, if present those signs are acted upon.
Evaluation of the response of the patient and wound to any treatment for wound infection.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 1 of 16
Australian Wound Management Association
Preface
Bacteria are an essential component of life and are found in all corners of the planet. The human body
relies on bacteria for normal physiological functioning. Indeed, the cellular organelle the mitochondria
was probably once a bacteria that has become essential to cellular function. However, bacteria can also
cause disease, injury and death.
A delicate balance exists in maintaining the bacteria humans need and preventing the
opportunistic invasion of bacteria that will result in infection.
The wound offers bacteria an attractive environment in which they can potentially flourish and, if left
unchecked, cause significant damage. With the potential for damaging infection and the surge in multiresistant bacteria, practitioners have become increasingly challenged to find solutions to wound
infection. There is considerable research and development focused on new technologies and
innovations to identify and manage wound infection. It is hoped that using a global, collaborative
approach new solutions will be found to reduce the burden of wound infection.
Scope of this document
Surgical
site
infection
(SSI)
is
well
defined
and
monitored
(http://www.health.gov.au/internet/safety/publishing.nsf). Therefore, this document will only briefly
address this. However, infection in wounds healing via secondary intention lacks definition and
management can be variable so the majority of this document will address infections in these wounds.
Introduction and background
It is well recognised that bacteria can impair wound healing. This document outlines the position of the
Australian Wound Management Association (AWMA) regarding definitions, diagnosis, investigation and
management of the bacterial impairment of wound healing. Whilst it is acknowledged other microbes,
such as viruses, parasites and fungi can impair wound healing, management of these infections is not
within the scope of this document.
This document should be considered in conjunction with local influences including
service provider characteristics and protocols, and professional and legal
requirements.
Scope of the problem
The true extent of bacterial impairment of wound healing is unknown.
Many hospitals monitor their inpatient infection rates and these are reported through coding
mechanisms. Studies have demonstrated that surgical site infections result in increased hospital length
of stay and increased costs. However, for patients post hospital discharge and those who develop
wound infections in the community, reporting mechanisms are often poor or non-existent. Infection in any
setting can result in increased costs (e.g. diagnostic studies, antibiotics), increased resource use due to
delayed wound healing, lost productivity and pain.
Severe infection leading to sepsis has the potential to result in significant patient
morbidity or even death.
Recommendation 1
Service providers should consider mechanisms to collect data on wound infections including
prevalence, organisms cultured and bacterial resistance in all healthcare settings.
More advanced data collection to evaluate the outcomes of wound infection such as treatment
and patient response may be considered where appropriate.
Surgical site infections
Significant work has been undertaken by some health jurisdictions and service providers to define,
detect, collect data on and manage surgical site infections (SSI).
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 2 of 16
Australian Wound Management Association
Many service providers require that any infection that might be related to a surgical
procedure must be reported as a clinical indicator.
Usually, recording of the rates for SSI are surgical procedure specific as identified by the ICD-10-AM
coding system used to group like procedures. In 2004 the Australian Safety and Quality Council and the
Australian Infection Control Association developed definitions and general reporting instructions for SSI.
These were approved by the Healthcare Associated Infections Advisory Committee. Whilst the
Australian Safety and Quality Council ceased its activities on 31 December 2005, the Australian
Commission for Safety and Quality in Healthcare has assumed responsibility for the Councils
documents and initiatives - including those related to Surgical Site Infection.
Please consult the relevant source (listed below) for a full description of diagnostic indicators and
reporting recommendations.
http://www.health.gov.au/internet/safety/publishing.nsf
Table 1 Definitions for SSI
Superficial incisional
Infection involves only skin or subcutaneous tissue of the incision and occurs
SSI
within 30 days after the operative procedure.
Deep incisional/organ
space SSI
Infection involves deep soft tissues (e.g. fascial and muscle layers) AND/OR
organs/spaces opened or manipulated during an operation and occurs within
30 days after the operative procedure if implant not present or within one
year if implant insitu.
Recommendation 2
Local health authorities, service providers and practitioners should use the Australian
framework as outlined above for defining and collecting data related to SSI.
Wounds healing by secondary intention
With over 270,000 Australians living with chronic wounds, the burden of infection is unknown, but likely
to be considerable.
AWMA encourages policy makers, health jurisdictions and service providers to
consider methodologies for monitoring and reporting chronic wound infection rates
and evaluation of management strategies.
With collaborative analysis and commitment to evidence based practice, optimal outcomes for the
patient and the health system can be achieved. This document is a guide to be used in conjunction with
clinical judgement and consideration of individual patient and service delivery parameters to identify and
manage bacterial impairment of wound healing. This guide does not replace the advice of an
appropriately trained and skilled health care practitioner.
The bacterial impact continuum
There are several classification systems and many definitions used to categorise the impact of bacteria
on a wound and the patient. Some practitioners continue to use the concept that >10 5 microorganisms
per gram of tissue constitutes infection. Whilst this might remain true in some circumstances, this does
not account for factors that might compromise the patients immune response or for bacteria that are
particularly virulent. The effect of bacteria on wound healing can best be conceptualised by the following
relationship:
Number of bacteria x virulence
Patient resistance
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 3 of 16
Australian Wound Management Association
For some practitioners and in certain care settings quantitatively determining the numbers and types of
bacteria accurately through wound swabbing or biopsy may not be possible.
Reliance on clinical signs is paramount in establishing where on a bacterial impact
continuum a particular wound and patient is at any given time.
Table 2 outlines a classification system that can be used to assist practitioners determine how bacteria
might be impacting on the wound healing process in wounds healing via secondary intention. This
classification system considers the effect of the bacteria on the wound and patient. It is not necessarily
related to increasing numbers of bacteria, but in many instances increasing numbers of bacteria and an
increasing variety of bacteria will result in greater impairment to wound healing and possibly local and/or
systemic effects.
Wound infection can be defined as multiplication of bacteria that overwhelm host
defences, resulting in disruption of healing and damage to the wound.
Wound infection can result in local and systemic host responses.
A wound can move in either direction along the bacterial impact continuum.
In clinical practice the boundaries between levels of bacterial impairment of wound
healing are often difficult to distinguish and data can be misleading or may not
support the expected results.
For example, clinically a wound can exhibit signs of local infection but a wound swab shows no growth.
Therefore, it is important for practitioners to remain vigilant and flexible in their practice and use all
available tools and evaluation methods.
Table 2 Bacterial impact on wound healing by secondary intention (Also refer to appendix 1)
Level of bacterial Bacterial activity
Degree of impairment to wound
impairment
healing & clinical signs
Contamination
Bacteria are on the wound surface. No
No impairment to healing.
division is occurring.
No obvious clinical signs of infection.
Colonisation
Bacteria are dividing.
No impairment to healing.
No obvious clinical signs of infection.
(Clinical wound appearance does not
usually differ from contamination)
Topical infection
Bacteria are dividing. Bacteria and/or their Impairment to healing.
(Critical
products have invaded the wound
Clinical signs of infection may not be
colonisation)
surface. There might be an increasing
obvious or are subtle.
variety of bacteria present. Biofilm may be (Refer to table 3)
present.
Local infection
Bacteria and/or their products have
Impairment to healing.
invaded the local tissues.
Usually obvious clinical signs of
infection localised to wound
environment and immediate periwound tissue. (Refer to table 3
Regional /
Bacteria and/or their products have
Impairment to healing.
Spreading
invaded surrounding tissues.
Usually obvious clinical signs of
infection / Cellulitis
infection. May have systemic signs.
Sepsis
Bacteria and/or their products have
Impairment to healing.
entered the bloodstream and may spread Usually obvious systemic clinical
to distant sites or organs.
signs: patient usually acutely unwell.
Damage to organs may occur.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 4 of 16
Australian Wound Management Association
There is controversy about the use of the term Critical Colonisation. Whilst the term is widely used and
accepted in current literature, the term implies a level of colonisation and colonisation is not associated
with impaired healing. As the clinical significance of infection is bacterial impairment of wound healing,
the term topical infection might be a more accurate descriptor than critical colonisation.
Topical infection implies that there is impairment to wound healing at a wound bed
level and accounts for the improvement often seen when topical antimicrobials (which
may include topical antiseptic washes) are used. The term implies that infection has
not invaded the deeper tissues.
Whatever term is used, many practitioners believe they can identify a level of bacteria delaying wound
healing; however, the clinical signs are often not consistent with those commonly recognised as features
of infection.
Recommendation 3
Service providers and practitioners should adopt a consistent consensus framework for
defining the level of bacterial impairment of wound healing based on assessment of the patient
and their wound.
Effects of bacteria on the wound environment
Bacteria can impair wound healing through the following mechanisms:
Formation of biofilm and the effects of the biofilm including an overall increase in pathogenic
effect due to the interactions of bacteria within the biofilm
Production of toxins and destructive enzymes
Release of free radicals
Degradation of growth factors
Secretion of immune-evasive factors and down-regulation of the immune response
Consumption of local oxygen
Localised thrombosis and release of vasoconstricting metabolites
Interference with collagen formation
Production of overexuberant small vessel angiogenesis
Production of metabolic products
This can lead to a chronic inflammatory state and promote increased exudate that can have a range of
toxic effects including degrading growth factors and matrix metalloproteinases
Biofilms
It is recognised that healing of many chronic wounds is impaired by formation of biofilms. A biofilm forms
when bacteria (often several species) attach to a wound and encase themselves in an exopolymeric
substance. These bacteria vary in morphology and physiology to planktonic, single cell bacteria. The
bacteria living in a biofilm are likely to have increased metabolic efficiency, substrate accessibility,
improved resistance to environmental stress and substances, and increased ability to cause local tissue
damage and infection. A biofilm is very difficult to directly eradicate. Penetration of a biofilm by antibiotics
and topical antimicrobials is very limited.
Wound swabbing techniques are less likely to collect bacteria within a biofilm as swabs
generally only collect free, planktonic bacteria.
This can result in misleading findings, which in turn can lead to ineffective therapies being implemented.
Aggressive debridement techniques are usually required to remove a biofilm. Managing all systemic and
local conditions impacting on wound healing will assist in the bodys ability to deal with a biofilm.
However, if the underlying conditions that led to a biofilm - both at a systemic and local level - are not
treated, the biofilm is likely to recur.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 5 of 16
Australian Wound Management Association
Minimising infection risk
Infection risk should be minimised for all patients with a wound through the following strategies:
Optimisation of patient immune response through good nutrition, adequate rest, avoidance of
smoking and control of other health conditions (e.g. diabetes, reduction of stress).
Removal of non-viable wound tissue (unless contra-indicated).
Adherence to strict infection control principles, including hand hygiene.
Adequate wound cleansing to remove foreign bodies, debris and remnants of dressing products.
Control of excess exudate including removal by cleansing and appropriate choice of dressing.
Use of dressings that minimize potential for entry of bacteria where possible.
Education of patients and practitioners.
Recommendation 4
A wound management regimen should include strategies to minimise infection risk. These
strategies should be embedded in service provider protocols and practices.
Indicators of infection
There are several broad indicator categories available to assess for bacterial impairment of wound
healing. These categories include clinical, microbiological, haematological and radiological. Some or all
indicators can be used to determine infection, its severity and management.
Table 3 Clinical indicators of infection
Level of bacterial impairment Clinical indicators of bacterial impairment to wound healing
Topical infection /
Dull wound tissue absence of vibrant granulation tissue
Critical colonisation
Slough
Failure of wound to decrease in size or increase in wound size
Increased exudate
Hypergranulation / friable tissue
Demarcated and/or rolled and/or raised wound margins
Local infection
Wound breakdown / increase in wound size
Erythema usually localised to peri-wound tissue
Increased pain or unexplained pain
Oedema usually localised to peri-wound tissue
Purulent or discoloured, viscous exudate
Malodour
Bridging and/or pocketing within the tissue
Increased temperature of peri-wound tissue
Regional/Spreading infection Spreading erythema more than 2cm from wound margin
Cellulitis
Induration of regional tissues
Fever
Oedema of regional tissues
Malaise and/or general feeling of unwellness
Sepsis
High fever or hypothermia
Lymphangitis and regional lymphadenopathy
Delirium
Organ compromise or failure
Circulatory shock hypotention, tachypnoea, tachycardia
Some or all of the above signs might be present. Bacterial impairment of wound healing is a continuum;
therefore worsening infection may or may not include some or all of the factors in the preceding
categories.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 6 of 16
Australian Wound Management Association
It should be noted that:
In some persons the traditional clinical signs of inflammation (erythema,
oedema, pain, heat) may not be present due to a dampening of the immune
response as a result of ischaemia, neuropathy or immunosuppression
(which can result from age, poor nutrition, other co-morbidities and medications).
The traditional clinical signs of inflammation can also be seen in conditions not associated with
bacteria, including: Charcots arthropathy, pressure-related injury or recurrent tissue injury. In
addition, some wounds are themselves part of an inflammatory but non- infection condition, such
as vasculitis.
Darkly pigmented skin or changes such as lipodermatosclerosis can make assessment of the
peri-wound tissue difficult.
Some wound aetiologies may present with a relatively specific range of signs that indicate
infection.
Other indicators of infection:
Microbiological:
A wound swab should be performed, according to service provider protocol:
When the signs of infection are present, in an attempt to determine the causative bacteria and
most appropriate antibiotic treatment.
When a wound has not responded to antibiotic therapy.
The Levine technique is recommended for collecting a wound swab.
Table 4: Levine Technique for Taking a Wound Swab
Procedure
Precautions
Remove dressing and discard
Do not swab old dressing
If necessary, remove/debride non
viable tissue
Cleanse wound with saline or
water
Avoid swabbing non viable tissue
Do not cleanse wound with
antiseptics
Do not swab pooled, stale
exudate
Wait 2-5 minutes
If wound is fairly dry, moisten
swab with sterile normal saline
(available in boot stock), if wound
is moist swab can be used dry.
Using moderate pressure depress
and rotate the swab against a
1cm2 area of viable wound tissue
Place swab in transport medium
and seal container.
Transport to pathology laboratory
for processing as soon as
possible
Avoid wound margins
Rationale
May not collect causative
organsims
May not collect causative
organisms
May kill or inhibit causative
organisms
May not collect causative
organisms
Allows fresh exudate to rise to
wound surface
Maximises uptake of exudate by
swab to enhance a higher
recovery rate of bacteria and
therefore more precise data for
sampling
Assists in collection of fresh
exudate
Avoid over-heating of sample.
A tissue biopsy might be useful for identifying causative bacteria in recalcitrant or unusual infections.
It should be noted that a wound swab may not provide an accurate representation of the bacteria
impairing healing for several reasons including:
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 7 of 16
Australian Wound Management Association
Poor wound swabbing technique
Failure to collect the causative bacteria or collection of non pathogenic bacteria
Inability of regular swabs to collect anaerobic bacteria specific swabs are required
Presence of a biofilm
Use of antiseptics prior to wound swabbing
Use of antibiotic therapy at the time of wound swabbing
Blood cultures should be performed if sepsis is suspected.
Haematological:
Increased white cell counts, erythrocyte sedimentation rates (ESR) and/or C-reactive protein (CRP) can
assist in detecting a physiological response to bacteria.
Radiological:
MRI, plain x-ray, bone scan, labelled leucocyte scan or bone biopsy can be useful for determining the
presence of osteomyelitis. MRI is the recommended investigation for osteomyelitis. However, not all
service providers have access to MRI and therefore alternative investigations may be necessary.
It should be noted that:
Biopsy, haematological and radiological indicators are usually undertaken by specialist
practitioners. However, lack of ready access to these services should not be a barrier to
diagnosing infection.
Wound swabs results should not over-rule clinical judgement. If a swab result seems inconsistent
with the clinical features, antimicrobial therapy may need to be guided by clinical judgement. For
instance, a bright green exudate is highly suggestive of Pseudomonas infection and appropriate
antibiotics could be used even if the swab fails to culture Pseudomonas. Bright red beefy tissue
may be indicative of Streptococci infection.
Recommendation 5
All wounds should be assessed regularly for the indicators of infection and outcomes of the
assessment documented.
Recommendation 6
A wound should be considered infected if the clinical signs of local infection are present (even
if wound swab results do not indicate infection).
Recommendation 7
A wound swab should generally be taken to guide appropriate antibiotic therapy but should not
be regarded as binding.
Management of infection
Management of wound infection will depend on: the severity of infection; available resources; and patient
factors (i.e. preferences, allergies).
Management of infection involves:
Treatment of the local wound environment - including regular debridement of non viable tissue
(unless contraindicated).
Support of the patients immune system- e.g. reviewing immunosuppressant therapy and
optimising nutritional status
Control of other health factors and illnesses that might impair healing
e.g. malnutrition, micronutrient deficiency, diabetes, smoking.
Patient education and participation.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 8 of 16
Australian Wound Management Association
Appropriate management of wound infection involves treating the right bacteria with
the right agent/s, delivered in the right manner for the right length of time.
Table 4: Management of wound infection
Level of bacterial impairment Management
Topical infection
Primary agents topical antimicrobials and washes with topical
(Critical colonisation)
antiseptic solution. (Antibiotics are not required.)
Local infection
Primary agent systemic enteral antibiotics
Adjunct agent topical antimicrobials
Regional/Spreading infection Primary agent systemic enteral or parenteral antibiotics
Cellulitis
Adjunct agent topical antimicrobials
Sepsis
Primary agent systemic parenteral antibiotics
Primary management agents are those recommended as first-line treatment. Adjunct agents are
recommended as secondary agents that might assist in controlling topical bioburden but will not be
adequate to treat deeper infection. Adjunct agents might or might not be used depending on service
provider, wound and patient factors.
In determining the most appropriate systemic antibiotic agents, authoritative texts
can be used as a guide.
The Australian Therapeutic Guidelines for Antibiotic therapy include recommended treatment regimens
for various skin and soft tissue infections and this is a valuable resource to guide practice. The Australian
Medicines Handbook includes comprehensive information regarding use of systemic antibiotics. Referral
for specialist services provided by microbiologists and infectious diseases practitioners should be
considered for complex, unresponsive, recalcitrant or recurrent infections that do not respond to
standard, recommended antibiotic therapy.
Empiric, systemic antibiotics should be commenced immediately when signs of clinical
infection are present.
Review of the appropriateness of the antibiotic occurs when wound biopsy or wound swab or blood
culture results are received. For most wound infections a defined course of systemic antibiotics is
satisfactory treatment. However, occasionally prolonged treatment with systemic antibiotics might be
indicated where cessation of antibiotics results in rapid deterioration of the wound, cessation of healing
or wound recurrence.
Recommendation 8
Agents for treatment of wound infection should be tailored to the extent of infection and based
on recommended treatment guidelines.
Recommendation 9
For complex, recurrent, recalcitrant or unresponsive infections consultation with a
microbiologist or infectious disease specialist is recommended.
Recommendation 10
The length of treatment with topical and/or systemic agents should be determined by the
response of the wound and the patient.
Topical antiseptics
Topical antiseptic solutions can be of benefit in wound management if they are used for the correct
indications.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 9 of 16
Australian Wound Management Association
Antiseptics have generally remained free from the resistance problems experienced by antibiotics, as
antiseptic agents act against bacteria and microbes in several ways, rather than the single mechanism of
action antibiotics employ. Topical antiseptic solutions can be very useful for decontamination following
wounding, particularly where the wound is likely to have been grossly contaminated. For example, a skin
tear sustained in the garden or a laceration with a dirty knife. Topical antiseptic solutions can also be of
benefit for some patients with minor skin-related infections.
Topical antiseptic solutions are not indicated for use on clean, healing wounds as they
can impair healing.
The most efficacious topical antiseptic solutions are povidone iodine and chlorhexidine.
However, occasionally other solutions may be appropriate for use in wound management (e.g. acetic
acid or potassium permanganate). Most topical antiseptic solutions are rapidly inactivated in a wound
environment, therefore their efficacy is usually short lived. When using topical antiseptic solutions it is
recommended that they are not mixed with other topical applications as this can reduce their efficacy
and potentially promote resistance. It is recommended that the solution is applied liberally, left it in
contact with the skin and/or wound for 3-5 minutes, and then rinsed off with saline or potable water.
Often, management with topical antiseptic solutions is only required for a limited time period. Once the
problem is rectified, wound cleansing with saline or potable water is recommended.
Topical antiseptic solutions can cause sensitivity and irritation in some patients. If this occurs, their use
should be discontinued.
Recommendation 11
Topical antiseptic solutions should generally be used for treatment of topical contamination or
minor skin infections and their use avoided on clean, healing wounds.
Topical antimicrobials
Antimicrobial is a broad term used to describe a variety of agents that kill or inhibit the growth or
replication of bacteria and other microbes.
However:
Topical antimicrobials should be used judiciously for appropriate clinical indications. Topical
antimicrobials are not indicated for use in clean, healing wounds. The most commonly used topical
antimicrobials include (but are not limited to) products containing silver, therapeutic honey, hypertonic
salt, iodine, chlorhexidine, metronidazole, murpirocin or polyhexamethylene biguanide (PHMB).
Topical antimicrobials can be divided in several ways:
Antiseptic and antibiotic
Mild and powerful
An antiseptic is an agent that non-selectively inhibits the growth of bacteria and micro-organisms.
Most agents promoted as topical antimicrobial have antiseptic effects.
A mild topical antimicrobial is generally an agent that:
Is only held within the product and not released, or
Is released in only very small quantities, and/or
Does not have a sustained mechanism of action
A powerful topical antimicrobial is generally an agent that:
Is released from the product into the wound environment, and
Is released in moderate to high quantities, and
Has a sustained mechanism of action
An antibiotic is an agent that can selectively inhibit or kill bacteria.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 10 of 16
Australian Wound Management Association
Due to the risk of resistance and sensitisation, topical antibiotics are rarely
appropriate for wound management.
Generally powerful topical antimicrobials are indicated where the practitioner
believes that:
Bacteria (or other microbes) are impairing wound healing and a topical agent
will be of benefit, and/or
The wound is at significant risk of infection and if infection occurred
catastrophic consequences could result
(e.g. patients with major burns or a neuro-ischaemic foot wound).
Topical antimicrobials are sometimes indicated for highly exuding or malodorous wounds as these
clinical signs are often due to the actions of bacteria.
The effectiveness of topical antimicrobials should be evaluated regularly. Patient and wound
management should be reviewed if topical antimicrobials fail to result in wound improvement.
If a wound has failed to improve after four weeks use of topical antimicrobials:
Other factors impairing healing should be considered as these may be the cause
of failure to heal, or
Consider the need for treatment with a more powerful agent (topical
antimicrobial or systemic antibiotic).
Recommendation 12
Topical antibiotics are rarely recommended for use on wounds due to the risk of resistance
developing.
Recommendation 13
Topical antimicrobials should be used judiciously for appropriate clinical indications and their
use evaluated regularly.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 11 of 16
Australian Wound Management Association
Local wound management
Good local wound management utilising the principles of wound bed preparation will assist in managing
bacterial impairment of wound healing and preventing recurrence of infection. The concept of TIME
(refer to table 5) can be used to guide local wound management.
Table 5: Local wound management for infected wounds
Element
Aim
Practice application
T
Remove non viable
Debride
wound
as
necessary
(unless
tissue viability
tissue
contraindicated).
(unless contraRegular, repeated debridement of chronic wounds
indicated)
may be necessary.
Cleanse wound at each dressing change.
I
infection and
inflammation control
Treat infection and
chronic inflammation
and prevent recurrence
Use antimicrobial agents and antibiotics as indicated
and regularly evaluate patient and wound response.
Use good infection control practices including hand
hygiene.
Use dressings that minimise environment contact
wherever possible.
Seek specialist advice for management of chronic
inflammation.
M
moisture balance
Maintain optimal wound
moisture, temperature
and pH
Use dressings that regulate the wound moisture
level to maintain a moist wound environment (unless
contra-indicated).
Avoid changing dressings too frequently.
Minimise wound exposure.
Avoid using hot or cold solutions.
E
edge of wound and
evaluation
Monitor wound progress
to determine if
management is
effective
Assess the wound systematically and regularly.
Document wound size and progress regularly.
Reassessment treatment if the wound fails to
progress and this is the expectation.
Recommendation 14
Regular wound assessment and documentation includes:
Identification of factors that might indicate infection and, if present those signs are acted
upon.
Evaluation of the response of the patient and wound to any treatment for wound infection.
Refer to appendix 2 for an overview of the prevention, classification, diagnosis and management
of infection
Conclusion
Bacterial impairment of wound healing is a significant burden on patients, service providers and the
health system. A systematic approach to preventing, identifying and managing wound infection can
reduce this burden and improve the lives of persons with a wound. Policy makers, service providers and
practitioners are encouraged to adapt these recommendations to their local care setting. It is only
through coordinated, consistent and persistent efforts that the impact of bacteria on wound healing can
be minimised.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 12 of 16
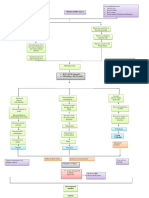
Appendix 1: The infection continuum
Contamination
Colonisation Topical infection
No overt signs of infection
Wound healing progresses
May be local
subtle signs of
infection
Local infection
Usually overt
local signs of
infection
Wound healing impaired
Host/Patient defences prevail
Topical infection
Regional infection Sepsis
Usually overt
regional signs of
infection
Usually overt
systemic signs
of infection
Patient health impaired
Bacteria prevail
Local infection
Regional infection (cellulitis)
Photos published with kind permission RDNS SA Inc.
Document Information Version 1.5
Title:
Position Document of the Australian Wound Management Association
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc.
Date:
October 2011
Source: www.awma.com.au
Page 13 of 16
Appendix 2: Prevention, classification, diagnosis and management of infection
Increasing severity of clinical response to bacteria
Level of bacterial
impairment
Local wound
management focus
Contamination
Colonisation
Basic infection
control and
Debris removal
Basic infection
control and
Wound cleansing
Debride non
viable tissue
Moisture balance
Clinical assessment
No treatment
Investigations
Primary treatment
Secondary/adjunct
treatment
No treatment
Short term topical
antiseptics for
acute
contamination
Topical infection
Local infection
Regional infection
Systemic infection
Debride non
viable tissue and
Moisture balance
Debride non
viable tissue and
Moisture balance
Debride non
viable tissue and
Moisture balance
Clinical assessment
Clinical assessment
Wound swab
Clinical assessment
Wound swab OR
Tissue biopsy
Clinical assessment
Blood cultures
Powerful topical
antimicrobials
Oral antibiotics
Oral antibiotics
OR Intravenous
antibiotics
Intravenous
antibiotics
Powerful topical
antimicrobials
Powerful topical
antimicrobials
Review
antibiotics
against swab
results
Review antibiotics
against swab/
biopsy results
Review antibiotics
against blood
culture results
Review
management
against patient
response
Review
management
against patient
response
Review
management
against patient
response
Mild topical
antimicrobials
only if high risk
of infection
Treatment review
Patient review
Review
management
against patient
response
Review
management
against patient
response
Review
management
against patient
response
Aim: to reduce the patient and wound response to bacteria
Document Information Version 1.5
Title:
Position Document of the Australian Wound Management Association: Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc.
Date:
October 2011
Source: www.awma.com.au
Page 14 of 16
Australian Wound Management Association
Glossary
Antimicrobial
Healing by secondary intention
Patient
Peri-wound
Potable
Practitioner
Service provider
Wound infection
A broad term used to describe a variety of agents that kill or inhibit the
growth or replication of bacteria and other microbes.
Wounds that heal by granulation and contraction.
The person with a wound. Can also be known as a client, resident,
consumer or customer.
The area of integument immediately surrounding the wound.
Water suitable for human consumption.
An individual health care provider/clinician.
Any person, organisation or institution providing wound management
services.
Multiplication of bacteria that overwhelm host defences, resulting in
disruption of healing and damage to the wound. Wound infection can
result in local and systemic host responses.
Bibliography
AAWC (Association for the Advancement of Wound Care) 2008 Advancing your practice: Understanding
wound infection and the role of biofilms, Malvern, PA.
Australian Commission on Safety and Quality in Healthcare 2004.
www.health.gov.au/internet/safety/publishing.nsf Accessed 1/6/08
Australian Wound Management Association (AWMA) 2010 Standards for wound management 2nd
Edition, www.awma.com.au
Cutting, K.F. & White, R. 2004, Defined and refined: criteria for identifying wound infection revisited,
British Journal of Community Nursing, Vol 9, No 3, Supp, pp S6-S15.
EWMA (European Wound Management Association) 2004, EWMA Position Document: Wound bed
preparation in practice, Medical Education Partnership, London.
EWMA (European Wound Management Association) 2005, EWMA Position Document: Identifying
criteria for wound infection, Medical Education Partnership, London.
EWMA (European Wound Management Association) 2005, EWMA Position Document: Management of
wound infection, Medical Education Partnership, London.
MacLellan, D.G. (ed) 2007, woundGLOSSARY: Terminology for wound practitioners, Health Education
and Management Innovations.
Schultz, G.S. Barillo, D.J. Mozingo, D.W. & Chin, G. A. 2004, Wound bed preparation and a brief history
of TIME, International Wound Journal, Vol 1, No 1, pp 19-32.
Sibbald, R.G. Orsted, H. Schultz, G.S. Coutts, P. & Keast, D. 2003. Preparing the wound bed 2003:
focus on infection and inflammation, OstomyWound Management, Vol 49, No 11, pp 24-51.
Templeton, S. 2005. Management of chronic wounds: The role of silver-containing dressings, Primary
Intention, Vol 13, No 4 pp 170-9.
WUWHS (World Union of Wound Healing Societies), 2008, Wound infection in clinical practice: An
international consensus, International Wound Journal, Vol 5, Suppl 3, pp 1-11.
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 15 of 16
Australian Wound Management Association
Disclaimer: This information presented in this document is intended as a general guide only. Application of this
information should be guided by the circumstances of each individuals or service providerss circumstances. No
responsibility is taken by AWMA for any harm to person or property arising from the information presented in this
document. No responsibility is accepted by AWMA for the consequence of inaccuracy or omission of information
presented in this document. Provision of information in this document is intended as a guide and does not
constitute endorsement of any product or organisation.
Version:
1.5
First published:
July 2009
Updated:
October 2011
Due for Revision:
July 2012
Document Information Version 1.5
Title: Position Document of the Australian Wound Management Association:
Bacterial impact on wound healing: From contamination to infection
Author: Australian Wound Management Association Inc
Date:
October 2011
Source: www.awma.com.au
Page 16 of 16
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- DM Foot CareDocument27 paginiDM Foot CareKatrina KattÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- 21718682Document6 pagini21718682Jason MarshallÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Amjpathol00018-0050Document8 paginiAmjpathol00018-0050Jason MarshallÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- Research Article: Effects of Three Types of Japanese Honey On Full-Thickness Wound in MiceDocument11 paginiResearch Article: Effects of Three Types of Japanese Honey On Full-Thickness Wound in MiceJason MarshallÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- 21718682Document6 pagini21718682Jason MarshallÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- GoodDocument14 paginiGoodJason MarshallÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- ShearDocument14 paginiShearJason MarshallÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- SXP035 M Butcher Bacterial Management in Modern Wound CADocument7 paginiSXP035 M Butcher Bacterial Management in Modern Wound CAJason MarshallÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Yun Li and Jing Zheng: Taylor & Francis Inc. ISSN: 1062-3329 Print/1029-2373 Online DOI: 10.1080/10623320590933743Document20 paginiYun Li and Jing Zheng: Taylor & Francis Inc. ISSN: 1062-3329 Print/1029-2373 Online DOI: 10.1080/10623320590933743Jason MarshallÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- ShearDocument14 paginiShearJason MarshallÎncă nu există evaluări
- NIH Public Access: Author ManuscriptDocument20 paginiNIH Public Access: Author ManuscriptJason MarshallÎncă nu există evaluări
- NIH Public Access: Author ManuscriptDocument20 paginiNIH Public Access: Author ManuscriptJason MarshallÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- 9Document7 pagini9Jason MarshallÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- 10.1007 - s00125 008 0940 0Document9 pagini10.1007 - s00125 008 0940 0leykelateÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Nurse Practitioner Clinical Protocol: Management of CellulitisDocument11 paginiNurse Practitioner Clinical Protocol: Management of CellulitisJason MarshallÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Diagnosing and Managing Lower Limb Cellulitis: A Guide for NursesDocument4 paginiDiagnosing and Managing Lower Limb Cellulitis: A Guide for NursesJason MarshallÎncă nu există evaluări
- Cellulitis Guidelines, CREST, 05 PDFDocument31 paginiCellulitis Guidelines, CREST, 05 PDFanathasia_christineÎncă nu există evaluări
- Cellulitis and Wound Management: Joanne Martin, RN, BSN, CWOCN Deaconess Home Health Care, Savannah, TNDocument1 paginăCellulitis and Wound Management: Joanne Martin, RN, BSN, CWOCN Deaconess Home Health Care, Savannah, TNJason MarshallÎncă nu există evaluări
- Diagnosing and Managing Lower Limb Cellulitis: A Guide for NursesDocument4 paginiDiagnosing and Managing Lower Limb Cellulitis: A Guide for NursesJason MarshallÎncă nu există evaluări
- Report Documentation Page: Headquarters Information Please Do Return Your To The Above AddressDocument6 paginiReport Documentation Page: Headquarters Information Please Do Return Your To The Above AddressJason MarshallÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- E 4 7iii openSurgicalWoundDocument23 paginiE 4 7iii openSurgicalWoundJason MarshallÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- Advances in Wound CareDocument8 paginiAdvances in Wound CareJason MarshallÎncă nu există evaluări
- Prevention and Management of Wound InfectionDocument3 paginiPrevention and Management of Wound InfectionagabattiÎncă nu există evaluări
- Ankle Brachial Index 3Document9 paginiAnkle Brachial Index 3Jason MarshallÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Bagus Wound DehisenceDocument8 paginiBagus Wound DehisenceJason MarshallÎncă nu există evaluări
- Fibrin Cuff Lysis in Chronic Venous Ulcfrs TreatedDocument4 paginiFibrin Cuff Lysis in Chronic Venous Ulcfrs TreatedJason MarshallÎncă nu există evaluări
- Ankle Brachial Index:: Best Practice For CliniciansDocument8 paginiAnkle Brachial Index:: Best Practice For Clinicianszaky soewandiÎncă nu există evaluări
- 1471 244X 8 41Document12 pagini1471 244X 8 41Yoan Love AnindyaÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Self-Regulation & CHronic IllnessDocument12 paginiSelf-Regulation & CHronic IllnessJason MarshallÎncă nu există evaluări
- About UsDocument3 paginiAbout UsKrishna SinghÎncă nu există evaluări
- How To Write A Systematic ReviewDocument8 paginiHow To Write A Systematic ReviewNader Alaizari100% (1)
- Immunology & Oncology Review 2Document99 paginiImmunology & Oncology Review 2Melchor Felipe SalvosaÎncă nu există evaluări
- A Review of The Use of The Health Belief Model For Weight ManagementDocument1 paginăA Review of The Use of The Health Belief Model For Weight ManagementpatresyaÎncă nu există evaluări
- Javma-Javma 21 04 0213Document5 paginiJavma-Javma 21 04 0213Black manÎncă nu există evaluări
- Tom's Fourth Year Guide (2011-12)Document709 paginiTom's Fourth Year Guide (2011-12)jangyÎncă nu există evaluări
- Nutrition FactsDocument232 paginiNutrition FactsAriana Sălăjan100% (2)
- Susan M. Pollak, Thomas Pedulla, Ronald D. Siegel - Sitting Together - Essential Skills For Mindfulness-Based Psychotherapy-The Guilford Press (2014)Document258 paginiSusan M. Pollak, Thomas Pedulla, Ronald D. Siegel - Sitting Together - Essential Skills For Mindfulness-Based Psychotherapy-The Guilford Press (2014)duasherazi55Încă nu există evaluări
- Heiland ResumeDocument2 paginiHeiland Resumeapi-297797784Încă nu există evaluări
- The many benefits of music. Listening to and creating music helps children learn numeracy, literacy and emotional skillsDocument5 paginiThe many benefits of music. Listening to and creating music helps children learn numeracy, literacy and emotional skillsHarold JimenezÎncă nu există evaluări
- Practice Guidelines For The Diagnosis and Management of Aspergilosis 2016 Update by AmericaDocument60 paginiPractice Guidelines For The Diagnosis and Management of Aspergilosis 2016 Update by AmericaNur Prasetyo Nugroho100% (1)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Wound AssessmentDocument19 paginiWound Assessmentdrsonuchawla100% (1)
- Test 1 XIEDocument2 paginiTest 1 XIESimona IrimiaÎncă nu există evaluări
- Exam Procedures: Steps for Completing a Biochemistry ExamDocument19 paginiExam Procedures: Steps for Completing a Biochemistry Exampmp123456Încă nu există evaluări
- February 4, 2015Document12 paginiFebruary 4, 2015The Delphos HeraldÎncă nu există evaluări
- High Yield Step 2ckDocument4 paginiHigh Yield Step 2ckCesar_Palana_3832Încă nu există evaluări
- Concept Map MarwahDocument5 paginiConcept Map MarwahAsniah Hadjiadatu AbdullahÎncă nu există evaluări
- Migraine and Cluster HeadacheDocument24 paginiMigraine and Cluster HeadachekhemamettaÎncă nu există evaluări
- Bastidas 2021Document13 paginiBastidas 2021ruben dario meza bertelÎncă nu există evaluări
- Liceo de Cagayan University: Acute AppendicitisDocument2 paginiLiceo de Cagayan University: Acute AppendicitisKylie AstrudÎncă nu există evaluări
- Sketchy Pharm RuntimesDocument5 paginiSketchy Pharm RuntimesAmin ValenciaÎncă nu există evaluări
- Managing Disease and Avoiding Complications Through Diet Diversification - PPTX 31.10.14Document134 paginiManaging Disease and Avoiding Complications Through Diet Diversification - PPTX 31.10.14iqraÎncă nu există evaluări
- Ethics in GeriatricDocument22 paginiEthics in GeriatricCessie GutzÎncă nu există evaluări
- Antidepressants For The Treatment of Depression in People With Cáncer 2018Document78 paginiAntidepressants For The Treatment of Depression in People With Cáncer 2018José Luis Rivera Z.Încă nu există evaluări
- COE WorksheetDocument16 paginiCOE WorksheetiloveraynaÎncă nu există evaluări
- Classification of Veneer PreparationsDocument11 paginiClassification of Veneer PreparationsVinisha Vipin SharmaÎncă nu există evaluări
- Shiatsu Helps Treat AsthmaDocument9 paginiShiatsu Helps Treat Asthmaडा. सत्यदेव त्यागी आर्यÎncă nu există evaluări
- Analgezia Si Anestezia in Obstetrica. Analgezia IN Travaliu: IndicatiiDocument31 paginiAnalgezia Si Anestezia in Obstetrica. Analgezia IN Travaliu: IndicatiiAlex GrigoreÎncă nu există evaluări
- Negative Affect Erasing MethodDocument2 paginiNegative Affect Erasing MethodmirkjhaelÎncă nu există evaluări
- Protection of Human Rights of Women PrisonersDocument5 paginiProtection of Human Rights of Women PrisonersBrajakanta NameirakpamÎncă nu există evaluări
- Uncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicDe la EverandUncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicÎncă nu există evaluări
- Deaths of Despair and the Future of CapitalismDe la EverandDeaths of Despair and the Future of CapitalismEvaluare: 4.5 din 5 stele4.5/5 (30)
- The Atlas of Disease: Mapping Deadly Epidemics and Contagion from the Plague to the CoronavirusDe la EverandThe Atlas of Disease: Mapping Deadly Epidemics and Contagion from the Plague to the CoronavirusEvaluare: 4.5 din 5 stele4.5/5 (10)
- Epic Measures: One Doctor. Seven Billion Patients.De la EverandEpic Measures: One Doctor. Seven Billion Patients.Evaluare: 4 din 5 stele4/5 (13)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisDe la EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (9)
- Do You Believe in Magic?: The Sense and Nonsense of Alternative MedicineDe la EverandDo You Believe in Magic?: The Sense and Nonsense of Alternative MedicineÎncă nu există evaluări
- The Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsDe la EverandThe Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsEvaluare: 4.5 din 5 stele4.5/5 (5)