Documente Academic
Documente Profesional
Documente Cultură
Cardiology Prescription
Încărcat de
Marta HalimDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Cardiology Prescription
Încărcat de
Marta HalimDrepturi de autor:
Formate disponibile
Common Drug interactions in
cardiology prescription
4 : 10
Sunip Banerjee, Kolkata
Introduction
Drugs predominantly act through cellular pathways and there is every chance of interaction with each
other if both drugs share same pathways for either their action or metabolism. Both the cases will
interfere the bioavailability and action of the one or both the drugs.
It is essential to determine the pharmacokinetics and pharmacodynamics of various cardiac drugs in
order to minimize the interaction of prescribed drugs. A good knowledge of cardiac drug interaction
will help physician to take decision during critical care to stop a certain drug over another to get
desired result, at the same time polymorphism in patients gene should also be accounted for such
variability in drug action.
Drugs commonly used in cardiology practice:
There are certain drugs which are predominantly used in cardiac medicine are:
1. Antihypertensive: ARB (angiotensin receptor blocker), CCB (calcium channel blocker), ACEi
(angiotensin-converting enzyme inhibitors), diuretics.
2. Anti-dyslipidemia: Statin, nicotinic acid.
3. Anti-platelet drug: Aspirin, GP IIb/IIIa antagonist.
4. Anti-coagulants: coumadins, heparin.
5. Anti-arrhythmic: amiodarone.
6. Anti-Heart failure: Beta blocker, ACEi.
Causes of Common Drug Interaction:
1. Pharmacodynamic ( what drug does to your body)
2. Pharmacokinetics ( what body does to drug)
3. Effect of genetic polymorphism for variable pharmacokinetics of drug.
Common pharmacodynamic drug interaction:
1. Concurrent use of anticoagulant and antiplatelet drug is a classic example of pharmacodynamic
drug interaction. Using heparin or warfarin with aspirin or clopidogrel mutually enhance (OR,
1.53; 95% CI, 1.05 to 2.22) the bleeding complication (Shireman et al. 2004).
2. Non-hydropyridine CCB (Verapamil) when concomitantly used with beta-blocker (Carvedilol)
may induce bradycardia.
3. Concomitant use of Sildenafil with nitrate (vasodilator) may result in severe hypotension even
sudden cardiac death.
4. Co administration of ACEi with potassium-sparing diuretics causes hyperkalemia, more so in
diabetic patients.
223
Medicine Update 2012 Vol. 22
Fig. 1: Interaction of ACE inhibitor (ACEi) and Aspirin which results in possible loss of function of ACEi. Cox1: cyclo-oxygenase
1, TxA2: Thromboxane A2.
Drug interaction between antihypertensive and antiplatelet aggregator:
Aspirin with ACE inhibitor (ACEi):
Aspirin is frequently prescribed with ACE inhibitor.
Prostaglandin activity is the point of confliction between
these two drugs where aspirin severely inhibit the activity
of prostaglandin while ACE inhibitor needs the activity of
prostaglandin for its optimal response (Fig 1).
Effect of inhibition of prostaglandin is not so pronounced
in normotensive and euvolemic subjects. In hypertensive
subjects, inhibition of prostaglandin hampers the effect of
nearly every antihypertensive drug including ACE inhibitor.
As ACE inhibitor is immensely effective in controlling
remodeling of heart and thus reduce the heart failure,
concurrent use of aspirin and ACE inhibitor in moderate to
high degree of heart failure patient will reduce the effect of
ACE inhibitor (Hall et al.2000), though it was countered by
Latini et al. 2000.
Reports from the Cooperative New Scandinavian Enalapril
Survival Study II (CONSENSUS II) (Nguyen et al. 1997) and
Studies of Left Ventricular Dysfunction (SOLVD) (Rand et
al. 1998) suggested the attenuation of ACE inhibitor response
when aspirin was used concomitantly.
Peterson & Laurer (2011) recommended the low dose and
non-long term aspirin therapy in concomitant with ACEi or
using alternate anti-platelet therapy like clopidogrel (if patient
is nonresponsive to low dose aspirin with ischemic event) and
restriction in use of NSAID with ACEi for the same reason.
Reduced activity of aspirin in concomitant use with other NSAID
Use of Non-steroidal anti-inflammatory such as ibuprofen
will eliminate the protective effect of aspirin and physician
should be careful to determine which analgesic best suitable
in patient with heart failure.
Fig 2: Possible route of statin metabolism and adverse effect.
CYP= Cytochrome P450.
The possible cause of this interaction
Arachidonic acid binds to COX-1 (Cyclooxygenase-1) and
converted to TXA2 (Thromboxane A2) to stimulate the platelet
for aggregation. Aspirin blocks the access of arachidonic acid
and inhibits the production of TXA2 and thus prevent the
platelet aggregation. If ibuprofen (NSAID) is administered
concurrently with aspirin, Prior reversible occupancy of
ibuprofen inhibits aspirin from permanently binding to COX1. However, aspirin differs by irreversibly acetylating a serine
residue at position 530 within the channel, blocking access
of arachidonic acid to its catalytic site, while other NSAIDs
are reversible inhibitors of the catalytic site. The mechanism
proposed is that ibuprofen inhibits the access of aspirin to the
COX-1 acetylation site in platelets resulting in antagonizing
irreversible platelet inhibition.
Reduced bioactivity of statin due to
drug interaction and gene mutation in
its transport system:
Statin is common cholesterol lowering drug by affecting the
HMG-Co-A reductase enzyme responsible for cholesterol
formation.
Possible causes of diminished statin activity:
1. Statins are transported to Liver via an enzyme OATP1B1
(organic anion-transporter B1) which is encoded by SLCO1B1 (Solute carrier organic anion transporter family,
member 1B1) gene. If statins are not successfully metabolized, their level in blood will be increased which
may result in rhabdomyolysis or myopathy. Common
SNP (single nucleotide polymorphism) in SLCO1B1
gene (SLCO1B1*5, c.521T>C, protein p.V174A,
rs4149056) can cause impairment of statin transportation to Liver leads to high level of statin in circulation
(Niemi et al.2011).
2. Statins are predominantly metabolized through CYP
(Cytochrome P) isozymes in the Liver. Most of the
statins ( Simvastatin, Atorvastatin, Lovastatin, Mevastatin )are metabolized through CYP3A4.Some statin
including rosuvastatin and Fluvastatin use CYP2C19
224
Common Drug Interactions in Cardiology Prescription
Table 1: Different CYP3A4 inhibitor drug stratified according
to their potency.
High
Moderate
Antibiotics
Clarithromycin, Telithromyocin,
Chloramphenicol
Antifungal
Azole
Antidepressant
Nefazodone
CCB
Verapamil, diltiazem
Antibiotics
Erythromycin
Herbal therapy
Grape fruit juice
Unspecified potency Amiodarone
Fig. 3 : Variable pharmacodynamic responses of Clopidogrel under
different interactions (modified after Tantry et al. JACC, 2011).
Ciprofloxacin
Norfloxacin
Dithiocarbamate
Table 2: Profile of Reports of Rhabdomyolysis Associated
With selected statins (modified after Omar et al. 2002)
2. If CYP3A4 inhibitor is necessary, then either statin therapy should be stopped or use rosuvastatin or pravastatin.
(Simvastatin & atorvastatin to be avoided).
Statin
Drug interaction of Clopidogrel:
Simvastatin
Cerivastatin
Lovastatin
Frequency of
Reports/Unique
Cases
321/215
231/192
51/40
No. of Cases Associated With Potentially Interacting Drugs* (n)
Fusidic acid (1)
Azole antifungals
(4)
Fibrates (33)
Chlorzoxazone (2)
Cyclosporine (31)
Nefazodone (2)
Warfarin (12)
Niacin (2)
Macrolide antibiotics (10)
Tacrolimus (1)
Digoxin (9)
Fibrates (22)
Digoxin (7)
Warfarin (6)
Macrolide antibiotics (2)
Cyclosporine (1)
Cyclosporine (12)
Digoxin (2)
Macrolide antibiotics (11)
Nefazodone (2)
Azole antifungals
(6)
Niacin (1)
Fibrates (5)
Warfarin (1)
Fig 3 demonstrates that only 10% of total infused Clopidogrel
is absorbed in system and then uses several P450 group of
enzymes, i.e. 2C19, 1A2, 2B6, 3A4 to be metabolized into
active form.
Several chemical hypotheses are there which predict the
worsening of pharmacokinetic response of Clopidogrel:
1. Polymorphism in 2C19 enzyme may result into poor metabolism of Clopidogrel which is accepted in epidemiological study. A SNP CYP2C19(*)2 (or 681 G > A) can
cause an increased risk of major adverse cardiovascular
events in the follow-up (RR: 1.96 (1.14-3.37); P = 0.02).
When studies evaluating stent thrombosis (n = 4) for a
total of 4975 patients were considered, the presence of
the variant allele was associated with an increased risk
of stent thrombosis (RR: 3.82 (2.23-6.54); P = 0.0001).
(Sofi et al. 2011).
& CYP2C9 for their metabolism, though pravastatin is
metabolized through non-CYP pathway (Fig 2). Concomitant therapy of CYP3A4 inhibitor (Table 1) with
simvastatin results in rhabdomyolysis (Rowan et al.,
2010).Though no such data is available for other statins
using same CYP3A4 pathway (Atorvastatin, Lovastatin,
Mevastatin), but similar result should be assumed for
them for such concomitant therapy (Table 2).
Possible alternate regime:
1. Genetic test rarely required to rule out statin toxicity.
2. Statin and CCB has competitive utilization of CYP3A4
enzyme with Clopidogrel for metabolism which may reduce the activity of both the drugs (Clarke et al, 2003,
Jolanta et al. 2008). But epidemiological study shows
that there is no competitive interaction of statin and
clopidogrel (Saw et al. 2007, Mukherjee et al. 2005,
Schmidt et al, 2011).
3. Most striking interaction is happened between smoking and activity of clopidogrel. Smoking induces the
activity of CYP1A2 and thus enhances the metabolism
and in turn efficacy of clopidogrel. Some epidemiological studies corroborate this hypothesis (Jae Kean Ryu,
2010; Berger et al. 2009) which is contradicted by recent
study (Sibbald et al 2010).
4. An interaction between PPI (proton pump inhibitor) and
clopidogrel is possible when the both agents are taken
with Grapefruit juice. PPI use CYP 3A4 while Clopi-
225
Medicine Update 2012 Vol. 22
in a high concentration. As amiodarone crosses the placenta and secreted in breast milk also.
Table 3: Important Amiodarone Drug Interactions
Drug
Result of interaction
Digoxin
Elevated digoxin plasma concentration
Warfarin
Elevated prothrombin time
Simvastatin
Increased incidence of myopathy when simvastatin dosage is higher than 20 mg per day
Sildenafil
Increased sildenafil plasma concentration
Cyclosporine
Increased cyclosporine plasma concentration
Drug interaction of beta blocker:
Antiarrhythmic drugs
Additive effects: possible elevated plasma concentrations of quinidine, disopyramide, flecainide,
propafenone and dofetilide.
-adrenergic receptor blocker has both pharmacokinetic and
pharmacodynamic interaction with other drugs.
Quinolones
Additive QT effect: possible increased risk of
proarrhythmia
Antidepressants
Increased plasma concentration of drugs metabolized in liver: possible increased risk of proarrhythmia
4. Desethylamiodarone (DEA) is active metabolite of amiodarone to have anti-arrhythmic property.
5. Due its slow release from lipid rich tissue its half-life is
generally high (mean 58 days).
Pharmacodynamic interaction:
dogrel use CYP 2C19 which has no impact to each other.
As grapefruit juice use the CYP3A4 which shunted the
PPI metabolism through 2C19 may diminish the clopidogrel response.
5. St Johns wort is a potent inducer of both CY3A4 and
2C19 pathways and simultaneous administration this
with clopidogrel and any of the PPIs may lead to significant drug interactions.
Possible alternate regime:
1. Grapefruit juice or St Johns wort should not be taken
with PPI and Clopidogrel medication.
2. Though trial data is still to draw any conclusion about
interaction between statin and clopidogrel, care should
be taken in high risk patients. Either nonCYP statin
(Pravastatin) should be used or statin should be used in
low dose to avert the interaction with clopidogrel, else
alternate antiplatelet therapy (prasugrel) should be introduced if statin is essential for patient.
3. In case of concomitant use of CCB and clopidogrel, response of both the agents should be closely monitored to
avoid any interaction.
Interaction of amiodarone with other
drugs:
Amiodarone is widely used anti-arrhythmic drug particularly
in life threatening ventricular arrhythmia.
1. Non-hydropyridine CCB (Verapamil or diltiazem) when
concomitantly used with beta-blocker may induce sinus
bradycardia and AV block of various types. But such
combination is useful in patients with AF and FVR, particularly in patient with MS and FVR and symptomatic
CV dysfunction.
Pharmacokinetic interaction:
1. Beta blockers (specially propranolol and metoprolol)
are generally metabolized in Liver and have high first
pass clearance. Many enzyme inducing drugs increase
the clearance of metabolized beta blocker and in turn
reduce their bio-availability.
2. Cimetidine is reported to have role in clearance of propranolol and metoprolol by enhancing the peak plasma
level by 70% & 95% in concomitant therapy with cimetidine (Kirch et al. 1981).
3. First pass clearance is also dependent on hepatic flow.
Hydralazine in this way reduces the first pass clearance
of propranolol and metoprolol which increases the plasma concentration of the beta blocker.
Cardiac drug interaction with alternate medicine or herb:
1. Findings suggest that Ginkgo biloba extract reduces the
therapeutic potency of the Calcium channel blocker,
nicardipine (Shinozuka et al. 2002).
2. Ginger reinforces warfarin action by heterogeneous
mechanisms. It should thus not be used in patients on
oral anticoagulant and/or antiplatelet therapy (Argento
et al.2000).
Pharmacokinetics:
3. Clove may increase the risk of bleeding or potentiate the
effects of warfarin therapy (Heck et al. 2000).
1. Possess very high content of iodine which may be a
cause of its interaction with thyroid gland.
4. Garlic with warfarin or aspirin causes bleeding complication (Vaes and Chyka, 2000).
2. Bioavailability is generally poor (22-94%) and well absorbed when taking with food
5. Guggul is an ayurvedic anti-dyslipidemic drug. Concomitant oral administration with propranolol or diltiazem
can reduce their bioavailability and might reduce their
therapeutic effects. Because of its action on the thyroid
3. Amiodarone is lipid soluble and stored in fat and muscle
226
Common Drug Interactions in Cardiology Prescription
Table 4: Interaction of common cardiac medicines with food &
chemical: (Pronsky, Z. M., 2006).
Drug
Beta Blockers (Antihypertensive)
Atenolol, Carvedilol ,Metoprolol
Chlorothiazide ,Furosemide,
Hydro-chlorothiazide,
Possible interaction with food
Avoid natural licorice. Take
2 hours before or 6 hours after calcium supplements and/
or orange juice. Calcium salts
may decrease absorption.
Avoid alcohol, grapefruit juice
and related citrus. Do not take
some with high doses of niacin. Separate fiber, pectin and
oat bran from drug by several
hours.
Vasodilators, also known as nitrates
(Antihypertensive)
Isosorbide dinitrate, Nesiritide, Hydralazine, Nitrates and Minoxidil
Limit alcohol. Decreased sodium and calcium intake may
be recommended. Avoid natural licorice.
Anticoagulants
Warfarin ,Enoxaparin ,Heparin
Interacts with vitamin K;
keep levels in diet consistent,
caution with vitamin E and
alcohol intake. Avoid or limit
garlic, ginger, ginkgo, ginseng,
green tea and avocado.
Barbiturates & phenytoin accelerates warfarin degradation
in liver, reducing its efficacy.
Metronidazole & Co-trimoxazole, Cimetidine decrease warfarin degradation increasing its
efficacy.
Amiodarone,
Allopurinol,
cephalosporins inhibit generation of vitamin K, accentuating
warfarin potency.
Conclusion
Polypharmacy is often prescribed during management of
cardiac patients who are mostly sick. When options of other
drugs are not available it is desirable to keep a close vigil on
patients vitals with help of ECG and INR. Patients need to
be counseled about the complexity of situation.
Increases excretion of electrolytes (potassium, magnesium and calcium). May need
to supplement losses. Avoid
natural licorice. Caution with
calcium &/or vitamin D supplement.
Statins, HMG-CoA Reductase In-
hibitors (Antihyperlipidemic)
Simvastatin,
Rosuvastatin,
Atorvastatin
7. Grapefruit juice is a CYP3A4 inhibitor. So, statins, CCB
or clopidogrel which use CYP3A4 for their metabolism,
will be reduced in bioavailability or activity if taken
with grapefruit juice (Tachjian et al. 2010).
References
1.
Al-Khadra AS, Salem DN, Rand WM, et al. Antiplatelet agents
and survival: a cohort analysis from the Studies of Left Ventricular
Dysfunction (SOLVD) trial. J Am Coll Cardiol 1998; 31:419-425.
2.
Argento A, Tiraferri E, Marzaloni M. Oral anticoagulants and medicinal plants. An emerging interaction. Ann Ital Med Int 2000;
15:139-43.
3.
Ara Tachjian, Viqar Maria, and Arshad Jahangir. Use of Herbal
Products and Potential Interactions in Patients with Cardiovascular Diseases. J Am Coll Cardiol 2010; 55;515-525.
4.
Christopher Rowan B.S, Allen D. Brinker M.D, Parivash Nourjah,
Jennie Chang, Andrew Mosholder , Jeffrey S. Barrett , Mark Avigan. Rhabdomyolysis reports show interaction between simvastatin and CYP3A4 inhibitors. Pharmacoepidemiology and Drug
Safety 2009;18: 301309.
5. DeWitt CR, Waksman JC. Pharmacology, pathophysiology and
management of calcium channel blocker and beta-blocker toxicity. Toxicol Rev 2004; 23:223-38.
6.
Donald Hall. The AspirinAngiotensin-Converting EnzymeInhibitor Tradeoff: To Halve and Halve Not. JACC 2000; 35:180812.
7.
Dalvi SS, Nayak VK, Pohujani SM, Desai NK, Kshirsagar NA,
Gupta KC. Effect of gugulipid on bioavailability of diltiazem and
propranolol. J Assoc Physicians India 1994; 42:454-5.
8.
Heck AM, DeWitt BA, Lukes AL. Potential interactions between
alternative therapies and warfarin. Am J Health Syst Pharm 2000;
57:1221-7.
Jeffrey S. Berger, Deepak L. Bhatt, Steven R. Steinhubl, Mingyuan Shao, P. Gabriel Steg, Gilles Montalescot, Werner Hacke, Keith
A. Fox, A. Michael Lincoff, Eric J. Topol, Peter B. Berger. Circulation 2009; 120: 2337-2344.
Antiplatelet Agents
Aspirin, Ticlopidine, Clopidogrel,
Dipyridamole
Avoid natural licorice. Take 2
hours before or 6 hours after
calcium supplements.
9.
Angiotensin Converting Enzyme
(ACE) Inhibitors (Antihypertensive)
Avoid salt substitutes. Caution
with potassium (K) and magnesium (Mg) supplements.
Limit alcohol. Decreased sodium (Na) and calcium may be
recommended.
10. Jae Kean Ryu. Smoking Interaction with Clopidogrel; another
Smokers Paradox? Korean Circ J 2010; 40: 112113.
Diuretics
11. Jolanta M. Siller-Matula, Irene Lang, Guenter Christ and Bernd
Jilma. Calcium-Channel Blockers Reduce the Antiplatelet Effect
of Clopidogrel. J Am Coll Cardiol 2008; 52:1557-1563.
Probenecid & lithium inhibit
tubular excretion of thiazide
diuretics.
(guggulsterone has thyroid-stimulating activity) caution
should be used when administering with thyroid drugs
(Dalvi et al. 1994).
6. Ginseng can inhibit the warfarin activity (Vaes and Chyka, 2000).
12. Matthew Sibbald, Andrew T. Yan, Wei Huang, Keith A.A. Fox,
Joel M. Gore, Gabriel Steg, Kim A. Eagle, David Brieger, Gilles
Montalescot, Shaun G. Goodman. Association between Smoking,
Outcomes, and Early Clopidogrel Use in Patients with Acute Coronary Syndrome: Insights from the Global Registry of Acute Coronary Events. American Heart Journal2010; 160:85-861.
13. Mukherjee D, Kline-Rogers E, Fang J, Munir K, Eagle KA. Lack
227
Medicine Update 2012 Vol. 22
of clopidogrel-CYP3A4 statin interaction in patients with acute
coronary syndrome. Heart 2005;91:23-6.
14. Nguyen KN, Aursnes I, Kjekshus J. Interaction between enalapril
and aspirin on mortality after acute myocardial infarction: subgroup analysis of the Cooperative New Scandinavian Enalapril
Survival Study II (CONSENSUS II). Am J Cardiol 1997; 79:115119.
15. Niemi M, Pasanen MK, Neuvonen PJ.Organic anion transporting
polypeptide 1B1: a genetically polymorphic transporter of major
importance for hepatic drug uptake. Pharmacol Rev 2011; 63:15781.
16. Peterson J, Lauer M. Using aspirin and ACE inhibitor in combination: Why the hullabaloo? Cleaveland Clinic Journal of Medicine
2011; 68:569-574.
17. Pronsky, Z. M. (2006). Food-Medication Interactions, 14th Edition. Birchrunville, PA: Food-Medication Interactions. Cardiac
Medications At-A-Glance. 2009, September 21. Retrieved from
http://www.americanheart.org/presenter.jhtml?identifier=303884
6#diuretics
18. Schmidt M, Johansen MB, Robertson DJ, Maeng M, Kaltoft A,
Jensen LO, Tilsted HH, Btker HE, Srensen HT, Baron JA.
Use of clopidogrel and calcium channel blockers and risk of major adverse cardiovascular events. Eur J Clin Invest 2011;doi:
10.1111/j.1365-2362.2011.02579.x. [Epub ahead of print]
19. Shinozuka K, Umegaki K, Kubota Y, Tanaka N, Mizuno H,
Yamauchi J, Nakamura K, Kunitomo M. Feeding of Ginkgo biloba extract (GBE) enhances gene expression of hepatic cytochrome
P-450 and attenuates the hypotensive effect of nicardipine in rats.
Life Sci 2002;70:2783-92.
20. Sofi F, Giusti B, Marcucci R, Gori AM, Abbate R, Gensini GF.
Cytochrome P450 2C19*2 polymorphism and cardiovascular recurrences in patients taking clopidogrel: a meta-analysis. Pharmacogenomics J 2011; 11:199-206.
21. Theresa I. Shireman, Patricia A. Howard, Timothy F. Kresowik,
Edward F. Ellerbeck. Combined AnticoagulantAntiplatelet Use
and Major Bleeding Events in Elderly Atrial Fibrillation Patients.
Stroke 2004; 35: 2362-2367.
22. Thomas A. Clarke and Lucy A. Waskell. The Metabolism of Clopidogrel Is Catalyzed by Human Cytochrome P450 3A and Is Inhibited by Atorvastatin. DMD 2003 ; 31(1):53-59.
23. Omar MA, Wilson JP. FDA adverse event reports on statin-associated rhabdomyolysis. Ann Pharmacother 2002; 36:288295.
24. Udaya S. Tantry, Dean J. Kereiakes, Paul A. Gurbel. Clopidogrel
and Proton Pump Inhibitors:Influence of Pharmacological Interactions on Clinical Outcomes and Mechanistic Explanations. J Am
Coll Cardiol Intv 2011; 4:365-380.
228
S-ar putea să vă placă și
- Sediment Exercise Manual Lymphatic Drainage Massage PDFDocument5 paginiSediment Exercise Manual Lymphatic Drainage Massage PDF1712013Încă nu există evaluări
- Six Steps To The Perfect LipDocument9 paginiSix Steps To The Perfect LipTatiana Araujo100% (1)
- The List - Eric Falstrault - Strength SenseiDocument11 paginiThe List - Eric Falstrault - Strength SenseiJon shieldÎncă nu există evaluări
- Action Plan For Rejuvenation of River Tunga 1Document11 paginiAction Plan For Rejuvenation of River Tunga 1anitha_mathanÎncă nu există evaluări
- Practice HPIDocument3 paginiPractice HPImedicalmatins100% (1)
- Cardiovascular PharmacologyDocument61 paginiCardiovascular PharmacologyTeeOne920% (1)
- Haad Exam 7Document22 paginiHaad Exam 7MallikarjunÎncă nu există evaluări
- Ace InhibitoriDocument12 paginiAce InhibitoriMedical StudentÎncă nu există evaluări
- Dialysis Products Catalog PDFDocument52 paginiDialysis Products Catalog PDFAFRIANSYAHÎncă nu există evaluări
- Head InjuryDocument22 paginiHead InjuryNguyễn Ly100% (1)
- Diabetes: Oxidative Stress and Dietary AntioxidantsDe la EverandDiabetes: Oxidative Stress and Dietary AntioxidantsÎncă nu există evaluări
- Letter of RecomendationDocument2 paginiLetter of RecomendationJorge Luis Sánchez Alarcón100% (1)
- Clopidogrel-Drug Interactions: Eric R. Bates, MD, Wei C. Lau, MD, Dominick J. Angiolillo, MD, P DDocument13 paginiClopidogrel-Drug Interactions: Eric R. Bates, MD, Wei C. Lau, MD, Dominick J. Angiolillo, MD, P DAyu ApriliantiÎncă nu există evaluări
- DR - Hussam Lec 3 Drugs Affecting Blood 2023 4Document13 paginiDR - Hussam Lec 3 Drugs Affecting Blood 2023 4ManWol JangÎncă nu există evaluări
- Review: Graeme J Hankey, John W EikelboomDocument12 paginiReview: Graeme J Hankey, John W EikelboomFilip IlievskiÎncă nu există evaluări
- Aspirin Resistance in Cardiovascular Disease A ReviewDocument10 paginiAspirin Resistance in Cardiovascular Disease A ReviewVioleta GrigorasÎncă nu există evaluări
- ACE IsDocument37 paginiACE IsPriyanshi ShahÎncă nu există evaluări
- Drug InteracttionDocument8 paginiDrug InteracttionMuh. AnugrawanÎncă nu există evaluări
- Meyer 2010Document24 paginiMeyer 2010deltanueveÎncă nu există evaluări
- Clinical Pharmacokinetics of Angiotensin II (AT) Receptor Blockers in HypertensionDocument14 paginiClinical Pharmacokinetics of Angiotensin II (AT) Receptor Blockers in HypertensionShreya SinhaÎncă nu există evaluări
- Anticoagulacion 2Document9 paginiAnticoagulacion 2Annette ChavezÎncă nu există evaluări
- Nephrotoxic DrugsDocument8 paginiNephrotoxic DrugsJelina MagsuciÎncă nu există evaluări
- Article Wjpps 1454142274Document17 paginiArticle Wjpps 1454142274Arshad Iqbal 383-FLL/BSURDU/S18Încă nu există evaluări
- Antiplatelet Therapy in Older Adults With Non-ST-Segment Elevation Acute Coronary Syndrome: Considering Risks and BenefitsDocument6 paginiAntiplatelet Therapy in Older Adults With Non-ST-Segment Elevation Acute Coronary Syndrome: Considering Risks and BenefitsJicko Street HooligansÎncă nu există evaluări
- Anticoagulation Module 2Document13 paginiAnticoagulation Module 2angelmedurÎncă nu există evaluări
- Angiotensin II Receptor Blockers An OverviewDocument7 paginiAngiotensin II Receptor Blockers An OverviewAmit KhairnarÎncă nu există evaluări
- Antiplatelet Treatment in Stable Coronary Artery DiseaseDocument6 paginiAntiplatelet Treatment in Stable Coronary Artery DiseaserambutsapukusayangÎncă nu există evaluări
- Nteraksi Obat Dalam Praktek Edokteran Igi: Drg. Yayun Siti Rochmah SPBMDocument29 paginiNteraksi Obat Dalam Praktek Edokteran Igi: Drg. Yayun Siti Rochmah SPBMtristiarinaÎncă nu există evaluări
- Antihypertensive Drug InteractionsDocument8 paginiAntihypertensive Drug InteractionsNur AzimahÎncă nu există evaluări
- Paracetamol Overdose and Management IIIDocument10 paginiParacetamol Overdose and Management IIIعلي حسين عودة العلياويÎncă nu există evaluări
- Anti-Diabetic DrugsDocument14 paginiAnti-Diabetic DrugsHossam Elden Helmy HaridyÎncă nu există evaluări
- Neuro-Oncology PracticeDocument16 paginiNeuro-Oncology Practice6ydn87w6gpÎncă nu există evaluări
- Angiotensin Receptor BlockersDocument6 paginiAngiotensin Receptor BlockersMohammad Arafat SiddiquiÎncă nu există evaluări
- Name: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of SubmissionDocument10 paginiName: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of SubmissionAnoosha FarooquiÎncă nu există evaluări
- The Effect of ARB in Diabetic NephropathyDocument6 paginiThe Effect of ARB in Diabetic NephropathyYosefina CindyÎncă nu există evaluări
- مقاله انگیسی پایان نامهDocument17 paginiمقاله انگیسی پایان نامهmilad latifiÎncă nu există evaluări
- Parasympathetic Nervous System: Uptake of CholineDocument16 paginiParasympathetic Nervous System: Uptake of Cholinegksah711Încă nu există evaluări
- Contraindications To Thrombolytic Therapy: Aminocaproic AcidDocument3 paginiContraindications To Thrombolytic Therapy: Aminocaproic AcidTia Siti RoilaÎncă nu există evaluări
- Drugs: 1-The Mechanism of Action of ASADocument11 paginiDrugs: 1-The Mechanism of Action of ASAVgdgÎncă nu există evaluări
- Principles of An-Tiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyDocument36 paginiPrinciples of An-Tiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyAbby LiewÎncă nu există evaluări
- 2010-Case Report Severe Hepatic Encephalopathy in A Patient With PDFDocument4 pagini2010-Case Report Severe Hepatic Encephalopathy in A Patient With PDFAnugrah ElfaÎncă nu există evaluări
- And Prevention of Thrombosis, 9th Ed: Antiplatelet Drugs: Antithrombotic TherapyDocument33 paginiAnd Prevention of Thrombosis, 9th Ed: Antiplatelet Drugs: Antithrombotic TherapyNube AzulÎncă nu există evaluări
- Diabetic Kidney DiseaseDocument13 paginiDiabetic Kidney DiseaseyulibudhyÎncă nu există evaluări
- AEDand LiverdiseaseDocument22 paginiAEDand LiverdiseaseEmir SmailbegovićÎncă nu există evaluări
- Lipideologia StatinasDocument8 paginiLipideologia StatinasErick HernandezÎncă nu există evaluări
- Farmakoterapi II - HypertensionDocument52 paginiFarmakoterapi II - Hypertensionfebi TaqwaÎncă nu există evaluări
- COLOGYDocument8 paginiCOLOGYYATIN GULSHANÎncă nu există evaluări
- 4 5999270362695600886Document20 pagini4 5999270362695600886123Încă nu există evaluări
- sTUDI KASUS LIPIDDocument3 paginisTUDI KASUS LIPIDAccung BuccuÎncă nu există evaluări
- Angiotensin Receptor Blockers (ARBs) PDFDocument3 paginiAngiotensin Receptor Blockers (ARBs) PDFpriya singhÎncă nu există evaluări
- 2.5. Drugs Interaction (Dr. Kinanti)Document135 pagini2.5. Drugs Interaction (Dr. Kinanti)dikri pangersaÎncă nu există evaluări
- Ranolazine: A Novel Antianginal Compound: Ua'Ica 'Document1 paginăRanolazine: A Novel Antianginal Compound: Ua'Ica 'belaginaÎncă nu există evaluări
- Azilsartan Medoxomil (Edarbi)Document15 paginiAzilsartan Medoxomil (Edarbi)nicasioaquinoÎncă nu există evaluări
- Advpub 1109130415Document11 paginiAdvpub 1109130415Zahid MahmoodÎncă nu există evaluări
- Antihypertensive Drugs: Re Jackson BSC MB CHB Frca and MC Bellamy MB BS MA FRCA FRCP (Edin) FficmDocument15 paginiAntihypertensive Drugs: Re Jackson BSC MB CHB Frca and MC Bellamy MB BS MA FRCA FRCP (Edin) FficmAndreas SmfÎncă nu există evaluări
- Interaction Between Statins and Clopidogrel Is TheDocument12 paginiInteraction Between Statins and Clopidogrel Is TheAnisa ArmadaniÎncă nu există evaluări
- Atorvastatin RaDocument2 paginiAtorvastatin RaNejra JonuzÎncă nu există evaluări
- 15-Medscape J Med. 2008 10 (Supp) S4. ©2008 MedscapeDocument12 pagini15-Medscape J Med. 2008 10 (Supp) S4. ©2008 MedscapeMohammad ElghazalyÎncă nu există evaluări
- Drug StudyDocument2 paginiDrug StudymatthewchadÎncă nu există evaluări
- Antinauseants and Antiemetic AgentsDocument4 paginiAntinauseants and Antiemetic Agentsmuhammad ilmanÎncă nu există evaluări
- ACE Inhibitors & Angiotensin II Antagonists: October 1997Document4 paginiACE Inhibitors & Angiotensin II Antagonists: October 1997indee533Încă nu există evaluări
- aurUS 2017 Aurobindo Pharma (DailyMed)Document19 paginiaurUS 2017 Aurobindo Pharma (DailyMed)JohnnyÎncă nu există evaluări
- Vorapaxar: General InformationDocument21 paginiVorapaxar: General InformationIoana GhirvuÎncă nu există evaluări
- VorapaxarDocument21 paginiVorapaxarIoana GhirvuÎncă nu există evaluări
- MS Levy-Moura Avec ThrombosedDocument47 paginiMS Levy-Moura Avec Thrombosedswaleh breik misfirÎncă nu există evaluări
- Patient CharacteristicsDocument7 paginiPatient CharacteristicsHazem AlmasryÎncă nu există evaluări
- Novel-Antiplatelet Therapies For Atherothrombotic Diseases: K.malleswari, D.Rama Bramha Reddy, A.Karthikeya SharmaDocument8 paginiNovel-Antiplatelet Therapies For Atherothrombotic Diseases: K.malleswari, D.Rama Bramha Reddy, A.Karthikeya Sharma9493.karthikÎncă nu există evaluări
- Analgesic Agents: Maya Ganda Ratna Department of Pharmacology and Pharmacy Faculty of Medicine - Lampung UniversityDocument46 paginiAnalgesic Agents: Maya Ganda Ratna Department of Pharmacology and Pharmacy Faculty of Medicine - Lampung UniversityMuhammad GilangÎncă nu există evaluări
- Drug Interaction Profesi New (PRT)Document72 paginiDrug Interaction Profesi New (PRT)auliaÎncă nu există evaluări
- Nutraceuticals and Human Blood Platelet Function: Applications in Cardiovascular HealthDe la EverandNutraceuticals and Human Blood Platelet Function: Applications in Cardiovascular HealthÎncă nu există evaluări
- The Blood Harvest - Reader ViewDocument6 paginiThe Blood Harvest - Reader ViewMarta HalimÎncă nu există evaluări
- 4 Types of Chemical Bonds - DummiesDocument2 pagini4 Types of Chemical Bonds - DummiesMarta HalimÎncă nu există evaluări
- Vanilin Ekstrak PDFDocument9 paginiVanilin Ekstrak PDFMarta HalimÎncă nu există evaluări
- Cara Matematika SederhanaDocument92 paginiCara Matematika SederhanaMarta HalimÎncă nu există evaluări
- Manufacturing of Tablets by Direct Compression Method - Reader ViewDocument1 paginăManufacturing of Tablets by Direct Compression Method - Reader ViewMarta HalimÎncă nu există evaluări
- Format Label Tom Jerry (MS Word)Document3 paginiFormat Label Tom Jerry (MS Word)Marta HalimÎncă nu există evaluări
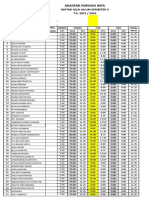
- Nilai Anfisman 2015 2016 MartaDocument20 paginiNilai Anfisman 2015 2016 MartaMarta HalimÎncă nu există evaluări
- Galaxys7edge 3Document1 paginăGalaxys7edge 3Marta HalimÎncă nu există evaluări
- Galaxys7edge 3Document1 paginăGalaxys7edge 3Marta HalimÎncă nu există evaluări
- AspirinDocument61 paginiAspirinMarta Halim100% (1)
- Setup LGFlashTool 1.8.1.1023.zip at StockROMsDocument2 paginiSetup LGFlashTool 1.8.1.1023.zip at StockROMsMarta HalimÎncă nu există evaluări
- Limulus Amebocyte LysateDocument44 paginiLimulus Amebocyte LysateMarta HalimÎncă nu există evaluări
- Health Literacy Toolkit Tool #9 Pharmacist Consultation - Tool9Document2 paginiHealth Literacy Toolkit Tool #9 Pharmacist Consultation - Tool9Marta HalimÎncă nu există evaluări
- Motivasi PajakDocument18 paginiMotivasi PajakMarta HalimÎncă nu există evaluări
- Elementary School Diploma: This Diploma Is Proudly Presented ToDocument1 paginăElementary School Diploma: This Diploma Is Proudly Presented ToMarta HalimÎncă nu există evaluări
- Kitchen Chemistry: A Scoping Review of The Diversionary Use of Pharmaceuticals For Non-Medicinal Use and Home Production of Drug SolutionsDocument10 paginiKitchen Chemistry: A Scoping Review of The Diversionary Use of Pharmaceuticals For Non-Medicinal Use and Home Production of Drug SolutionsAntonioÎncă nu există evaluări
- Diastolic CHF DiagnosisDocument3 paginiDiastolic CHF DiagnosissamÎncă nu există evaluări
- TB of The TestesDocument2 paginiTB of The Testesntambik21Încă nu există evaluări
- Bio Medical Waste Management PPT 25-06-2019Document47 paginiBio Medical Waste Management PPT 25-06-2019Dark InvaderÎncă nu există evaluări
- Infection: Dr. Mehrunnisa Umar Assistant Professor Department of MedicineDocument57 paginiInfection: Dr. Mehrunnisa Umar Assistant Professor Department of MedicinedrusmanjamilhcmdÎncă nu există evaluări
- CL12Document598 paginiCL12preeti dÎncă nu există evaluări
- 1. Đề ôn tập GHK1 - Môn Anh 10 - Đề số 1Document14 pagini1. Đề ôn tập GHK1 - Môn Anh 10 - Đề số 1Nguyễn Đ.KhangÎncă nu există evaluări
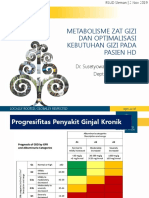
- Seminar HD-RSUD Sleman 2019Document36 paginiSeminar HD-RSUD Sleman 2019herkamaya100% (1)
- Study Guide - SAPCDocument7 paginiStudy Guide - SAPCSudhakar KuppireddyÎncă nu există evaluări
- Dream Abstracts PDFDocument61 paginiDream Abstracts PDFAlice Gina100% (1)
- Operation Maintenance of EtpDocument1 paginăOperation Maintenance of Etpaminur rahamanÎncă nu există evaluări
- Sterilisation-Chemical Methods: Submitted By, C.Gopika Dileep 1 MSC BiotechnologyDocument12 paginiSterilisation-Chemical Methods: Submitted By, C.Gopika Dileep 1 MSC BiotechnologyKarthika Gokulan0% (1)
- The Good and Bad Effects of TV On ChildrenDocument4 paginiThe Good and Bad Effects of TV On Childrenapi-206219067100% (1)
- Daftar PustakaDocument3 paginiDaftar PustakaEKAÎncă nu există evaluări
- Mucocele 9Document5 paginiMucocele 9Devi AlfianiÎncă nu există evaluări
- NCP Micu Hascvd Cad - RioDocument5 paginiNCP Micu Hascvd Cad - RioRio BonifacioÎncă nu există evaluări
- Dengue (Break Bone Fever) - FAQ, DPH-TAMIL NADU, IndiaDocument3 paginiDengue (Break Bone Fever) - FAQ, DPH-TAMIL NADU, IndiaDr.SagindarÎncă nu există evaluări
- Chapter 4 A1 Poster Example 2Document3 paginiChapter 4 A1 Poster Example 2Krisna PamungkasÎncă nu există evaluări
- Chapter 8Document30 paginiChapter 8ankitmanash0% (1)
- Comp ReDocument15 paginiComp ReROBERT C. REÑA, BSN, RN, MAN (ue)Încă nu există evaluări