Documente Academic
Documente Profesional
Documente Cultură
Minimal Invasive Hallux Valgus Surgery
Încărcat de
Juniper PublishersDrepturi de autor
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Minimal Invasive Hallux Valgus Surgery
Încărcat de
Juniper PublishersDrepturi de autor:
Review Article
Volume 1 Issue 1 - August 2015
Orthop Rheumatol Open Access J
Copyright All rights are reserved by Thinesh VS
Minimal Invasive Hallux Valgus Surgery:
Myth or Magic. A Systematic Review
Gopinath Mathavan1,2,3, Lynne Gaskell1, Anand Pillai2, Thinesh VS3* and Pravin DC3
1
University of Salford, United Kingdom
University Hospital of South Manchester, United Kingdom
Hospital Port Dickson, Malaysia
Submission: September 03, 2015; Published: September 10, 2015
*Corresponding author: Thinesh VS, Registrar, Orthopedic Department, Hospital Port Dickson, Negeri Sembilan, Malaysia, Lot 474, Jalan Terisu,
Batu 49, Kuala Terla, 39010 Cameron Highlands, Pahang, Malaysia, Tel: 6012-5884656; Email:
Abstract
A Better understanding of foot biomechanics coupled with technological advancement and governance to improve patient outcomes
have facilitated newer innovations in Hallux Valgus (HV) surgery. Minimally Invasive Surgery (MIS) is one of the greatest advances in modern
medicine and an emerging trend in foot and ankle surgeries. The needs to provide a quicker post- operative recovery, reduce operative time
and minimize complications have led to development of various MIS techniques in HV correction over the past decades. This systematic
review aims to establish the efficacy and safety of MIS for HV correction. A systematic search of Cumulative Index to Nursing and Allied
Health Literature (CINAHL), Embase, Medline, Science Direct and Cochrane Central Registry of Controlled Trials from inception of database
till 28th February 2014 was conducted. A total of 27 English language articles published in peer reviewed journals with available clinical and
radiological outcome measures were deemed appropriate and were critically analyzed to determine the efficacy and safety of minimally
invasive HV surgery (MIHVS). These studies included a total of 1485 patients with 1952 surgical procedures using MIHVS. The clinical and
radiological outcomes achieved with MIHVS along the complications reported were comparable with the conventional open techniques.
The MIHVS within this review consisted of case series that differed in terms of procedure, patient selection, techniques, instrumentation,
rehabilitation protocol, use of fluoroscopy and reporting outcome measures. The complication rates were significantly lower in centers
specializing with MIHVS. Higher levels of evidence with large population studies are required to recommend MIHVS which have shorter
operating time, quicker recovery and reduced hospital stay compare to open surgery.
Level of clinical evidence: 4
Keywords: Percutaneous; Minimum Incision; Hallux Valgus; Arthroscopy; Osteotomy; Metatarsal
Abbreviations: AOFAS: American Orthopedic Foot and Ankle Society; CMS: Coleman Methodology Score; DLMO: Distal Linear Metatarsal
Osteotomy; DMAA: Distal Metatarsal Articular Angle; DSTR: Distal Soft Tissue Release; FAOS: Foot and Ankle Outcome Score; HV: Hallux
Valgus; HVA: Hallux Valgus Angle; IMA: Inter-Metatarsal Angle; K-Wire: Kirschner-Wire; MICA: Minimally Invasive Chevron and Akin;
MIDMO: Minimally Invasive Distal Metatarsal Osteotomy; MIHVS: Minimally Invasive HV Surgery; MIS: Minimally Invasive Surgery; MOXFQ:
Manchester-Oxford Foot Questionnaire; MP-IP: Metatarsophalangeal-Interphalangeal; MTPJ: Metatarsophalangeal Joint; NHS: National
Health Service; OA: Osteoarthritis; PDMO: Percutaneous Distal Metatarsal Osteotomy; PDO: Percutaneous Distal Osteotomy; RA: Rheumatoid
Arthritis; ROM: Range of Movement; SERI: Simple Effective Rapid Inexpensive: CONSORT: Consolidated Standards of Reporting Trials;
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Introduction
Foot surgery has greatly developed over the past two
decades. Continuous effort in understanding the anatomy and
biomechanics of foot with technological advancement and
growing social needs has facilitated newer innovations. Digital
deformities are the commonest forefoot presentation to the
foot and ankle clinic [1]. Among the common digital deformities,
Hallux Valgus (HV) has long been an area of interest to the foot
and ankle surgeons. The complex multifactorial nature and
biomechanical dysfunction have resulted in numerous surgical
Orthop Rheumatol Open Access J 1(1): OROAJ.MS.ID.555552 (2015)
correction techniques [2-4].
Minimal invasive HV surgery is one of the greatest advances
in operating field of orthopedic. Advantages like short operating
time, quicker recovery, reduced hospital stay and fewer
complications compare to traditional open surgeries contributed
to diversity. Invention of new techniques and modification of
existing techniques have changed the operating principle of HV
surgery. Despite all of the available minimal invasive techniques
on correction of HV, scientific validation of the safety and efficacy
of these techniques is still inconclusive. Previously published
001
Orthopedics and Rheumatology Open Access Journal
systematic reviews by Maffulli et al. [5], Roukis [1] National
Institute for Clinical Excellence (NICE) guidelines and Trnka [1,57] have well identified the limitations of the available evidence to
determine clear recommendations for MIS in HV correction [1,57]. The renewed interest in the recent past has seen emerging
trends of newer techniques such as the Minimally Invasive
Chevron and Akin (MICA) and Endolog that aim to improve
clinical outcomes [8,9]. However, the topic remains highly
controversial due to limited evidence.
This systematic review aims to establish the efficacy and
safety of minimally invasive surgery for HV correction and to
provide patients and medics with evidence in determining their
choice of surgery. Furthermore, if the procedure is safe and
efficacious, does it offer cost effective management.
Materials and Methods
A systematic search of the following databases CINAHL,
Embase, Medline, Science Direct and Cochrane Central Regristry
of Controlled Trials from inception of database till 28th February
2014 was conducted. Combinations of words used to locate
appropriate studies were Percutaneous, Minimally invasive, HV,
Bunion, SERI (simple effective, rapid, inexpensive), Riverdin,
Riverdin-isham Osteotomy, Endolog system, less invasive,
minimal incision and MICA. Full text English articles were
obtained based on search strategy and keywords. Only articles
found in peer-reviewed journals are considered. Each article
is reviewed and information gathered regarding study details
including name and type of the study, number of patients
involved, year of publication and procedure or technique used.
Selected articles show minimal invasive Hallux Valgus surgery
with clinical or radiological assessment score to determine the
efficacy of the procedure. Safety of the procedure was based
on specific complications analysis reported by individual
publications. Conference abstracts were not included due to
limitation to appraise study methodology.
Quality assessment of the included studies was done
by two independent assessors using the modified Coleman
Methodology Scale (CMS) which are based on the subsections
of the Consolidated Standards of Reporting Trials (CONSORT)
statement [5,10]. The obtained values were based on the average
obtained from both the assessors. The reporting of this systematic
review was also done in accordance with the Preferred Reporting
Items for Systematic Reviews and Meta-Analyses (PRISMA)
statement [11]. The authors used Review manager (Version 5.1)
to evaluate the magnitude of intervention assessed if pooling of
data was possible. However, based on the evidence level of the
available literature and between study heterogeneity, narrative
synthesis of the study findings were undertaken.
Results
Electronic searches of the database resulted in retrieval of 71
relevant articles and a further 33 articles were identified from
the review of the references. Only 27 articles were selected based
on this reviews inclusion and exclusion criteria. These articles
002
included a total of 1485 patients with 1952 various techniques
of MIHVS.
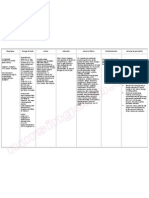
The evidence reviewed included 24 retrospective case series
with level IV evidence, 3 retrospective comparative studies with
level III evidence and 1 prospective comparative study with level
II evidence. Various techniques of MIS were used and summarized
in (Table 1).
CMS assesses the methodology of the study by using 10
criteria with a total score of 0 to 100. Chance, various biases
and confounding factors are absent if the study has a total score
of 100. Average CMS values for all of the 27 articles agreed by
two assessors were calculated and shown in (Table 2). Highest
score was 60 and lowest was 31. Most of the studies had
methodological drawbacks such as poor study sample and short
follow up time with average score of 40.6.13 studies used the
American Orthopedic Foot and Ankle Society (AOFAS) score to
assess the clinical outcome. AOFAS score ranges from 0 to 100
with high scores indicate better outcome clinically. Average
preoperative scores were 48.5 and average postoperative
scores were 87.5. Radiological measurements of hallux valgus
angle (HVA) preoperative and postoperative are 31.7 and 14.2.
Intermetatarsal angle (IMA) showed preoperative average
value of 13.9 and postoperative average value of 7.7. List of
complications associated with minimally invasive hallux valgus
surgery are summarized in (Table 3).
Discussion
The increasing trend towards MIHVS aims to reduce surgical
complications, reduce operative times and provide patients
with quicker recovery time [1,36,37,38]. However, the technical
maturity and advancement achieved are not proportionate to
the quality of available publications. The present systematic
review reinforces the issue that most of the available evidence
is observational in nature which consists of case series. Only one
prospective and 3 retrospective comparative case control studies
were available in this systematic review [4,14,24,29].
The lack of homogeneity among studies reviewed is the major
limiting factor towards generalizing the available evidence. The
broad term of HV surgery consists of a wide variety of procedures
including percutaneous distal metatarsal osteotomy with
percutaneous lateral release and proximal phalanx osteotomy,
percutaneous distal metatarsal osteotomy without soft tissue
procedure, minimally invasive distal metatarsal osteotomy,
modified minimal incision distal metatarsal osteotomy, minimal
incision distal oblique osteotomy using the Endolog system,
percutaneous double metatarsal osteotomy,percutaneous distal
soft tissue release with Akin procedure and the arthroscopic
assisted HV correction [8,9,20,24,26,28,31]. No techniques have
shown superiority to others due to lack of randomized control
trials and insufficient comparative case control studies.
Metatarsal osteotomy plays an important role in determining
the outcome of the procedure. Most authors practicing the
MIHVS correction have always used the conventional distal
How to cite this article: Mathavan G, Gaskell L, Pillai A, Thinesh VS, Pravin DC. Minimal Invasive Hallux Valgus Surgery: Myth or Magic. A Systematic
Review. Orthop Rheumatol Open Access J. 2015;1(1): 555551.
Orthopedics and Rheumatology Open Access Journal
Table 1: Details of the studies included.
No
1
2
Study (year of Publications)
Type of Study (Level of Evidence)
Angthong et al. (2013)[12]
Retrospective Case series (IV)
Bauer et al.(2010)[8]
Procedure/Technique
Number of
Patients
(Feet)
*CMS
30(36)
35
MIDLMO
Retrospective Case series (IV)
Reverdin-Isham Osteotomy
82(104)
Chiang et al.(2012)[14]
Retrospective Comparative Study (III)
Modified Bosch Technique
30(32)
53
Gadek & Liszka(2013)[16]
Retrospective Case series (IV)
Minimal Incision Mitchell-Kramer
54(54)
33
Giannini et al.(2013)[4]
Prospective Comparative Study(II)
SERI
10
Huang et al.(2011)[18]
Retrospective Case series (IV)
12
Lavigne et al.(2011)[20]
Bsch et al.(2000)[13]
Enan, Abo-Hegy & Seif(2010)[15]
Giannini & Ceccarelli(2003)[17]
Giorgio et al.(2013)[9]
11
Kadakia et al.(2007)[21]
15
Lui et al.(2008)[23]
16
17
18
19
Maffulli et al.(2009)[24]
Maffulli et al.(2005)[25]
26
27
24(36)
Retrospective Case series (IV)
Minimal Incision-ENDOLOG
Retrospective Case series (IV)
Bosch Technique(MIDMO)
37(54)
Retrospective Comparative Study (III)
Retrospective Case series (IV)
42
72(85)
47
6(6)
32
13(13)
35
MIDMO
31(47)
32
MIDMO
36(36)
60
Arthroscopic Assisted Percutaneous
Screw Fixation
83(94)
MIDMO
Retrospective Case series (IV)
37
82(125)
MIDMO
Retrospective Case series (IV)
59
25(33)
Percutaneous Double Metatarsal
Osteotomy
Retrospective Case series (IV)
42
20(20)
PDMO
Retrospective Case series (IV)
35
36
15(21)
PDMO
33
82(118)
44
Bosch technique(PDMO)
Radwan & Mansor (2012)[29]
Retrospective Comparative Study (III)
PDMO
24(29)
51
Scala & Vendettuoli (2013)[31]
Retrospective Case series (IV)
Modified MIDMO
126(146)
45
Tong & Ho( 2012)[33]
Retrospective Case series (IV)
Bosch Technique(PDMO)
20(23)
Retrospective Case series (IV)
PDMO
Sanna & Ruiu(2005)[30]
25
Bosch Technique (PDMO)
42
Retrospective Case series (IV)
22
24
64(98)
SERI
Retrospective Case series (IV)
Magnan et al.(2005)[26]
Bosch Technique (PDMO)
Markowski et al.(1991)[27]
Martinez-Nova et al.(2011)[28]
23
Retrospective Case series (IV)
Lin et al.(2009)[22]
20
21
Retrospective Case series (IV)
Iann et al.(2013)[19]
13
14
Retrospective Case series (IV)
51
Retrospective Case series (IV)
CMS was used with permission from Maffulli N [24].
38
83(90)
MIDMO
Retrospective Case series (IV)
31
79(79)
PDLMO
Retrospective Case series (IV)
Valles- Figueroa et al. (2010)[34]
Weinberger et al. (1991)[35]
DSTR-Akin Procedure
Retrospective Case series (IV)
Sun et al.(2010)[32]
44(64)
38
79(150)
Bosch Technique(PDMO)
49
31
40(58)
33
204(301)
33
Table 2: Clinical and radiological outcome measure from available studies.
No
Study
(year of Publications)
Angthong et al. (2013)[12]
Bsch et al. (2000)[13]
87.5 (67-93.5)
Chiang et al. (2012)[14]
44.3 14.9
84.5 6.2
Gadek & Liszka (2013)[16]
37.0
Giannini & Ceccarelli(2003)[17]
Giorgio et al. (2013)[9]
10
003
95 6.4
49 (44-52)
Enan, Abo-Hegy & Seif (2010)[15]
70.2 11.3
Bauer et al.(2010)[8]
5
6
AOFAS
HVA
IMA
Preoperative Postoperative Preoperative Postoperative Preoperative Postoperative
Giannini et al. (2013)[4]
Huang et al. (2011)[18]
NA
NA
NA
32.3 8.2
15 (11-18)
14 (12-15)
35.1 4.2
11.3 7.1
14.9 2.2
33.9
14.2
14.8
36 (14-54)
91.1 6.8
27.7 3.8
90.7
14.2 4.0
30 (25-32)
NA
81.0
10.3 7.5
NA
19 (7-40)
14.6 5.8
NA
7.1 8.0
11(9-13)
13 (6-18)
10(3-18)
11.2 1.8
5.8 2.4
NA
6.6 2.9
9.7
NA
51 10
81.2 15.1
38.5 3.5
21.8 4.1
16.1 3.9
6.8 4.3
NA
NA
26.7(15-43.8)
15.5(3-32.4)
11.9(7.2-15.4)
7.2(2-12.7)
22.1 11.1
88.2 6.2
36.6 8.1
22.7 6.7
16.0 1.9
6.1 2.9
How to cite this article: Mathavan G, Gaskell L, Pillai A, Thinesh VS, Pravin DC. Minimal Invasive Hallux Valgus Surgery: Myth or Magic. A Systematic
Review. Orthop Rheumatol Open Access J. 2015;1(1): 555551.
Orthopedics and Rheumatology Open Access Journal
11
Iann et al. (2013)[19]
47.6 13.3
87.3 11.5
13
Kadakia et al. (2007)[21]
34
84
15
Lui et al. (2008)[23]
12
14
Lavigne et al.(2011)[20]
NA
34.7 8.2
14.8 7.8
14.7 4
6.6 3.6
NA
25 (16-33)
12 (1-24)
10.3 (7-14)
6.4 (2-10)
26 4.9
14.2 6.7
11.6 1.6
5.3 2.3
43
16
22
11
Lin et al. (2009)[22]
NA
92.7 6.2
Maffulli et al. (2009)[24]
54 10
85 11
Magnan et al. (2005)[26]
NA
88.2 12.9
31.5 10.2
13.7 6.7
12.3 3
7.3 2.7
20
Martinez-Nova et al. (2011)[28]
68.5 10.6
86.6 8.5
24.1 3.7
11 1.7
11.8 0.5
9.4 0.5
22
Sanna & Ruiu (2005)[30]
NA
NA
32 (14-55)
12.5
15 (10-23)
9.1
84.2 4.3
33.28 9.59
12.31 4.64
11.75 2.89
6.80 1.95
91.1
NA
13.1 5.6
NA
7.5 2.1
16
17
18
19
21
23
24
25
26
27
Maffulli et al. (2005)[25]
Markowski et al.
(1991)[27]
NA
NA
NA
Radwan & Mansor,(2012)[29]
44.6 16.8
Scala & Vendettuoli (2013)[31]
54.6
Sun et al.(2010)[32]
Tong & Ho ( 2012) [33]
Valles- Figueroa et al.(2010)[34]
Weinberger et al.(1991)[35]
NA
93 8
NA
NA
90.2 6.8
85.3
53
91.8 7.9
NA
NA
NA
linear metatarsal osteotomy and frequently associated with
postoperative complications like nonunion, delayed union and
loss of correction. However, Sun et al. operated on 150 feet using
oblique technique for metatarsal osteotomy and there was no
reported nonunion, delayed union, avascular necrosis, infection
and recurrence. Oblique osteotomy which provides a larger
surface area for bony contact and union may have resulted in
lesser incidence of postoperative nonunion [32].
Stabilization techniques in HV surgery differ and need to be
highlighted due to its importance [39,40]. Bosch started with
the use of a single extra articular Kirschner-wire (K-wire) as a
stabilization technique of the osteotomy site [13]. Several other
authors have used a similar pattern of stabilization using a
single k-wire [4,25,26] while others have modified the available
techniques to use two k-wires to provide greater stability [24].
Sun et al. and Martinez et al. [28,32] have described sole use
of postoperative bandaging without hardware placement for
stabilization of metatarsal osteotomy [28,32]. Newer innovations
led to the emergence of Endolog system and percutaneous screws
for stabilization [9,20].
The varying use of intraoperative fluoroscopy is another
technical aspect that differs among the studies reviewed. Several
studies have advocated the use of fluoroscopy as part of MIHVS
[15,19,26,33]. However, some studies have excluded the use of
intraoperative fluoroscopy aimed at reducing intraoperative
radiation exposure [4,24,32]. Several experienced authors
have stressed the importance of radiological control to avoid
complications arising from decreased visualization of the
surgical field and improve the accuracy of positioning the
surgical instrumentation [41]. Although fluoroscopy provides
reassurance towards the correction achieved, but efficacy and
cost effectiveness of this procedure may be affected significantly
due to its influence on increasing operative time, radiation
exposure and manpower requirements.
004
33 7
27 6
32 12
36 (24-61)
27.9 4.4
32.3
31.3 5.3
26 8.3
14 5
17 4
14.1 4.7
19(5-40)
13.1 2.8
4.5
15.7 7.7
7.5 6.3
14 3
15 6
11.5 4
13
12.6 1.9
14.4
16.7 2.8
NA
92
83
7.5 3
8
7.8 1.3
4.8
7.7 3.8
NA
The feasibility of applying a surgical treatment modality to
the general population very much relies on patient selection. This
review highlights an important setback to the current available
evidence in deciding the efficacy and reproducibility of this
procedure. Most studies have correctly excluded patients with
inflammatory arthritis, adjacent joint degeneration, peripheral
vascular disease and systematic conditions such as diabetes
mellitus [4,24,29]. However several studies lacked appropriate
exclusion of patients and have a potential to influence
interpretation of the available evidence. The studies that have
included patients with underlying systemic comorbidities have
failed to relate their association with complications reported [31].
HV in rheumatoid arthritis is a complex interaction of both soft
tissue and osseous elements [42]. When procedure like minimally
invasive distal metatarsal osteotomy (MIDMO) is used to correct
this complex HV deformity purely relying on bony component,
neglecting the soft tissue correction may lead to recurrence of
the deformity. This once again reinforces that patient selection
within the studies reviewed may have potential of skewing the
available evidence due to poorly specified exclusion criteria.
The outcome measures used are of fundamental importance
when evaluating the success of surgical procedure. In HV
surgery the post-surgical assessment is commonly based
on clinical and radiological assessment. AOFAS score is the
commonest clinical outcome that has been utilized in the current
review. Unfortunately, the AOFAS score has not been validated
[43,44,45,46]. It is known to be a surgeon designed outcome
scale, lacks quality of life assessment and patient based outcome
assessment [47].
Soo Hoo et al. [43] evaluated the validity of the AOFAS clinical
rating system in 2003. Pearson correlation coefficient for patients
with forefoot disorders ranged from -0.05 -0.25 when AOFAS score
is compared to Medical Outcome Study Short Form-36(SF-36)
that has been well validated. The relatively low correlation
How to cite this article: Mathavan G, Gaskell L, Pillai A, Thinesh VS, Pravin DC. Minimal Invasive Hallux Valgus Surgery: Myth or Magic. A Systematic
Review. Orthop Rheumatol Open Access J. 2015;1(1): 555551.
005
Valles- Figueroa et
al. [34]
Weinberger et al.
[35]
Tong & Ho [33]
Sun et al. [32]
Scala & Vendettuoli
[31]
Sanna & Ruiu [30]
Martinez-Nova et
al. [28]
Radwan & Mansor,
[29]
Markowski et al. [27]
Magnan et al. [26]
Maffulli et al. [25]
Maffulli et al. [24]
Lui et al. [23]
Lin et al. [22]
Lavigne et al. [21]
Kadakia et al. [20]
Iann et al. [19]
Huang et al. [18]
Giorgio et al. [9]
Giannini et al. [4]
Giannini & Ceccarelli
[17]
Gadek & Liszka [16]
Enan, Abo-Hegy &
Seif [15]
Chiang et al. [14]
8.3 (2-39)
22
11
7.5 years
12
11
2)
30.5 (25-46)
12
28.1
16 (8-32)
25 3.2
35.9 10.9
2.5
years(2.1-3.2
years)
30.5(24-74)
24
23.7 weeks
(16-68 weeks)
73.3 38.1
130 days(50207)
18.3(9-38)
18.2(12-36)
84
36 (22-52)
18
21
24
105
24(12-40)
Bsch et al. [13]
Bauer et al. [8]
10
Angthong et al. [12]
Study
Superficial inMean follow
fection/
up (months)
skin irritation
Table 3: Complications seen in minimally invasive hallux valgus surgery.
16
29
9
-
--
24
2(
Deep
NonMalDeep
Bro- DMMA
infec- HalDis- union/
De- Transfer Osteo- union/ M1/P1 MTP1 MTPJ
vein
ken hyper- Recurtion/
lux
CRPS placed Pseudolayed Metatar- necrosis angu- Fracstiff- arthri- Numbnes
thromhard- correc- rence
Dehiss- Varus
K-wire arthrounion
salgia
N(%)
lation ture
ness
tis
bosis
ware
tion
cence
sis
N(%)
Orthopedics and Rheumatology Open Access Journal
How to cite this article: Mathavan G, Gaskell L, Pillai A, Thinesh VS, Pravin DC. Minimal Invasive Hallux Valgus Surgery: Myth or Magic. A Systematic
Review. Orthop Rheumatol Open Access J. 2015;1(1): 555551.
Orthopedics and Rheumatology Open Access Journal
reflects poor validity and reliability of AOFAS to assess functional
outcome in forefoot disorders. The current review deals with
majority of case series that have used retrospective collection of
preoperative data that may have potential to overestimate the
improvement achieved using the AOFAS scale [48]. Maffulli et al.
[24] in 2009 was the only study in our review that had utilized
the validated Foot and Ankle Outcome Score (FAOS) [24]. The
FAOS and MOFQ have been validated and are a reliable patient
orientated assessment although their usage remains limited in
our review [49,50]. The dependence on a non- validated scale to
define the efficacy of a procedure reflects the poor reliability of
the available evidence.
The outcome analysis that relates radiological assessment
needs to be reviewed with caution. This review includes HVA
and IMA but excludes DMMA due to its poor inter and intraobserver reliability [51,52,53]. Radiological outcome may not
be a true reflection of the clinical outcome. Angthong et al. [12]
reviewed 36 feet with predominant moderate HV treated with
DLMO at mean follow up of 10 months in 2013 [12]. The mean
AOFAS scores improved from 70.2 11.3 to 95 6.4. At final
follow up, they observed nine feet (25%) with recurrence of
deformity (HVA>15, significant sagittal malunion in twenty-four
feet (66.7%) and significant sesamoid lateralization observed
(p<0.05). These radiological abnormalities did not correlate
with reported clinical outcomes including the postoperative
AOFAS score (p>0.05). It is therefore important to bear in mind
that radiological assessment may not represent the measure of
clinical and functional efficacy.
The review of complications encountered following MIHVS
revealed contrasting reports. While some authors [4,9] have
revealed no major complications with the procedure, others [19]
have described significant complications that include recurrence
of deformity in 18.8%, stiffness of first MTPJ in 8.8%, hallux
varus in 9.4%. Dorsal malunions in 15.6% and infection rates
ranging from 3.5-8.9%. Comparative case control studies using
MIS revealed equal or less complication rates in comparison to
conventional open techniques such as scarf osteotomy, Ludloff
and Chevron osteotomy. Maffulli et al. [24] in 2009 reported
higher rates of intraoperative fractures (8.3%) and hardware
intolerance (13.9%) with conventional scarf osteotomy as
compared to the MIDMO technique [24]. Gianini et al. [4] in 2013
compared the scarf technique with SERI technique in 20 patients
with bilateral HV [4]. Each patient was subjected to a separate
procedure on either foot. They reported higher incidence of
hardware intolerance (10%) in patients with scarf osteotomy.
One possible explanation to this is the low rates experienced
using the minimally invasive technique is that the reporting done
by the centers with extensive experience and expertise dealing
with MIHVS.
Conclusion
MIHVS have several advantages such as shorter operating
time, quicker recovery and return to work or sports, reduced
hospital stay and fewer complications compare to open surgery.
But, the MIHVS studies available at present differ in terms of
procedure, patient selection, techniques, instrumentation and
006
rehabilitation protocol, use of fluoroscopy and outcome measure.
. These factors may have a significant influence on study outcomes
and limit the generalizability of this procedure. Future research
involving MIHVS should include adequately sized randomized
control trials, standardization of treatment protocols, use of
validated tools for measurement of clinical outcome and future
reporting by non-specialized centers to accept overwhelming
evidence and theoretical advantage of MIHVS compare to open
surgeries.
Acknowledgement
A special thanks to Professor Nicola Maffulli and Professor
Hans-Joerg Trnka for their support, guidance and encouragement.
References
1. Roukis TS (2009) Percutaneous and minimum incision metatarsal
osteotomies: a systematic review. J Foot Ankle Surg 48(3): 380-387.
2. Saro C, Andren B, Wildemyr Z , Fellander-Tsai L (2007) Outcome
after distal metatarsal osteotomy for hallux valgus: a prospective
randomized controlled trial of two methods. Foot Ankle Int 28(7):
778-787.
3. Oh IS, Kim MK, Lim KY, Bae JH (2007) Modified technique of distal
metatarsal osteotomy for hallux valgus. Foot Ankle Int 28(4): 527528.
4. Giannini S, Cavallo M, Faldini C, Luciani D, Vannini F (2013) The SERI
distal metatarsal osteotomy and Scarf osteotomy provide similar
correction of hallux valgus. Clin. Orthop Relat Res 471(7): 2305-2311.
5. Maffulli N, Longo UG, Marinozzi A , Denaro V (2011) Hallux valgus:
effectiveness and safety of minimally invasive surgery. A systematic
review. Br Med Bull 97: 149-167.
6. NICE (2010) National Institute for Health and Clinical Excellence.
Interventional Procedure Overview of Surgical Correction of Hallux
Valgus Using Minimal Access Techniques. Interventional Procedure
Guidance.
7. Trnka HJ, Krenn S, Schuh R (2013) Minimally Invasive hallux valgus
surgery: a critical review of the evidence. Int Orthop 37(9): 17311375.
8. Bauer T, Biau D, Lortat-Jacob A, Hardy P (2010) Percutaneous hallux
valgus correction using the Riverdin-Isham osteotomy. Orthop
Traumatol Surg Res 96(4): 407-416.
9. Di Giorgio L, Touloupakis G, Simone S, Imparato L, Sodano L, et al.
(2013) The Endolog system for moderate to severe hallux valgus. J
Orthop Surg 21(1): 47-50.
10. Altman DG, Schulz KF, Moher D, Egger M, Davidoff F (2001) The revised
CONSORT statement for reporting randomized trials: explanation and
elaboration. Ann Intern Med 134(8): 663-694.
11. Moher D, Liberati A, Tetzlaff , Altman DG (2010) Preferred reporting
items for systematic reviews and meta-analyses: the PRISMA
statement. Int J Surg 8(5): 336-341.
12. Angthong C, Yoshimura I, Kanazawa K, Hagio T, Ida T, et al. (2013)
Minimally invasive distal linear metatarsal osteotomy for correction
of hallux valgus: a preliminary study of clinical outcome and analytical
radiographic results via a mapping system. Arch Orthop Trauma Surg
133(3): 321-331.
13. Bsch P, Wanke S, Legenstein R (2000) Hallux valgus correction by the
method of Bsch: a new technique with a seven to ten year follows up.
Foot Ankle Clin 5(3): 485-498.
How to cite this article: Mathavan G, Gaskell L, Pillai A, Thinesh VS, Pravin DC. Minimal Invasive Hallux Valgus Surgery: Myth or Magic. A Systematic
Review. Orthop Rheumatol Open Access J. 2015;1(1): 555551.
Orthopedics and Rheumatology Open Access Journal
14. Chiang CC, Lin CF, Tzeng YH, Huang CK, Chen WM, et al. (2012) Distal
linear osteotomy compared to oblique diaphyseal osteotomy in
moderate to severe hallux valgus. Foot Ankle Int 33(6): 479-486.
15. Enan A, Abo-Hegy M, Sheif H (2010) Early results of distal metatarsal
osteotomy through minimally invasive approach for mild to moderate
hallux valgus. Acta Orthop Belg 76(4): 526-535.
16. Gadek A, Liszka H (2013) Mini invasive Mitchell-Kramer method in
the operative treatment of hallux valgus deformity. Foot Ankle Int
34(6): 865-869.
17. Giannini S, Ceccarelli F (2003) Hallux valgus surgery: the minimally
invasive bunion correction (SERI). Tech Foot Ankle Surg 2(1): 11-20.
18. Huang PJ, Lin YC, Fu YC, Yang YH, Cheng YM (2011) Radiographic
evaluation of minimally invasive distal metatarsal osteotomy for
hallux valgus. Foot Ankle Int 32(5): 503-507.
19. Iann B, Familiari F, De Gori M, Galasso O, Ranuccio F, (2013) Midterm
results and complications after minimally invasive distal metatarsal
osteotomy for treatment of hallux valgus. Foot Ankle Int 34(7): 969977.
20. De Lavigne CD, Rasmont Q, Hoang B (2011) Percutaneous double
metatarsal osteotomy for correction of severe hallux valgus deformity.
Acta Orthop Belg 77(4): 516-521.
21. Kadakia A, Smerek J, Myerson M (2007) Radiographic results after
percutaneous distal metatarsal osteotomy for correction of hallux
valgus deformity. Foot Ankle Int 28(3): 355-360.
22. Lin YC, Cheng YM, Chang JK, Chen CH, Huang PJ (2009) Minimally
invasive distal metatarsal osteotomy for mild to moderate hallux
valgus deformity. Kaohsiung J Med Sci 25(8): 431-437.
23. Lui TH, Chan KB, Chow HT, Ma CM, Chan PK, et al. (2008) Arthroscopyassisted correction of hallux valgus deformity. Arthroscopy 24(8):
875-880.
24. Maffulli N, Longo UG, Oliva F, Denaro V, Coppola C (2009) Bosch
osteotomy and scarf osteotomy for hallux valgus correction. Orthop
Clin North Am 40(4): 515-524.
25. Maffulli N, Oliva F, Coppola C, Miller D (2005) Minimally invasive
hallux valgus correction: a technical note and a feasibility study. J Surg
Orthop Adv 14(4): 193-198.
26. Magnan B, Pezz L, Rossi N, Bartolozzi P (2005) Percutaneous distal
metatarsal osteotomy for correction of hallux valgus. J Bone Joint Surg
Am 87(6): 1191-1199.
27. Markowski HP, Bosch P, Rannicher V (1992) Surgical technique and
preliminary results of a percutaneous neck osteotomy of the first
metatarsal for hallux valgus. Foot 2(2): 93-98.
28. Martnez-Nova A, Snchez-Rodrguez R, Leal-Muro A, PedreraZamorano JD (2011) Dynamic plantar pressure analysis and midterm
outcomes in percutaneous correction for mild hallux valgus. J Orthop
Res 29(11): 1700-1706.
29. Radwan YA, Mansour AM (2012) Percutaneous distal metatarsal
osteotomy versus distal chevron osteotomy for correction of mild to
moderate hallux valgus deformity. Arch Orthop Trauma Surg 132(11):
1539-1546.
30. Sanna P, Ruiu GA (2005) Percutaneous distal osteotomy of the first
metatarsal (PDO) for the surgical treatment of hallux valgus. Chir
Organi Mov 90(4): 365-369.
31. Scala A, Vendettuoli D (2013) Modified minimal incision subcapital
osteotomy for hallux valgus correction. Foot Ankle Spec 6(1): 65-72.
32. Sun WD, Wen JM, Hu HW, Sun YS, Sang ZC, et al. (2010) Long term
007
efficacy of minimal incision osteotomy for hallux abducto valgus.
Orthop Surg 2(3): 223-228.
33. Tong CK, Ho YF (2012) Use of minimally invasive distal metatarsal
osteotomy for correction of hallux valgus. J Orthop Trauma Rehabili
16(1): 16-21.
34. Valles- Figueroa JFJ, Rodrquez-Resndiz F, Caleti-del Mazo E,
Malacara-Becerra M, Surez-Ahedo CE (2010) Percutaneous distal
metatarsal osteotomy for the correction of hallux valgus. Acta Ortop
Mex 24(6): 384-388.
35. Weinberger BH, Fulp JM, Falstrom P, Anavian RR, Gore Al, Bazak I
(1991) Retrospective evaluation of percutaneous bunionectomies
and distal osteotomies without internal fixation. Clin Podiatr Med
Surg 8(1): 111-136.
36. Van Enoo RE, Cane EM (1986) Minimal incision surgery. A plastic
technique or a cover up? Clin Podiatr Med Surg 3(2): 321-335.
37. C De Lavigne, S Guillo, O Laffentre, M De Prado (2007) The treatment
of hallux valgus with the mini-invasive technique. Interac Surg 2(1):
31-37.
38. Lpez J, Rodrguez S, Mndez L (2005) Functional, esthetic and
radiographic results of treatment of hallux valgus with minimally
invasive surgery. Acta Ortop Mex 19(1): 41-46.
39. Trnka HJ, Zembsch A, Easley ME (2000) The Chevron Osteotomy for
correction of Hallux Valgus. J Bone Joint Surg 82(10): 1373-1378.
40. Banks A, Downey M, Martin DE (1992) McGlamrys Comprehensive
Textbook of Foot & Ankle Surgery (2nd edn), Lipincott Williams &
Wilkins, Philadelphia PA, USA.
41. De Prado M (2013) Complications in minimally invasive foot surgery.
Fu & Sprung gelenk 11(2): 83-94.
42. Louwerens JW, Schrier JC (2013) Rheumatoid forefoot deformity:
pathophysiology, evaluation and operative treatment options. Int
Orthop 37(9): 1719-1729.
43. SooHoo NF, Shuler M, Fleming LL (2003) Evaluation of the validity
of the AOFAS clinical rating systems by correlation to the SF-36. Foot
Ankle Int 24(1): 50-55.
44. Baumhauer JF, Nawoszenski DA, DiGiovanni BF, Wilding GE (2006)
Reliability and validity of the American Orthopaedic Foot and Ankle
Society Clinical Rating Scale: a pilot study for the hallux and lesser
toes. Foot Ankle Int 27(12): 1014-1019.
45. Pinsker E, Daniels TR (2011) AOFAS position statement regarding the
future of the AOFAS clinical rating systems. Foot Ankle Int 32(9): 841842.
46. Button G, Pinney S (2004) A meta-analysis of outcome rating scales
in foot and ankle surgery: is there a valid, reliable and responsive
system? Foot Ankle Int 25(8): 521-525.
47. Parker J, Nester CJ, Long AF, Barrie J (2003) The problem with
measuring patient perceptions of outcome with existing outcome
measures in foot and ankle surgery. Foot Ankle Int 24(1): 56-60.
48. Easley ME, Trnka HJ (2007) Current concepts review: hallux valgus
part I. Pathomechanics, clinical assessment and non-operative
management. Foot Ankle Int 28(5): 654-659.
49. Chen L, Lyman S, Do H, Karlsson J, Adam SP, et al. (2012) Validation
of foot and ankle outcome scores for hallux valgus. Foot Ankle Int
33(12): 1145-1155.
50. Morley D, Jenkinson C, Doll H, Lavis G, Sharp R, et al. (2013) The
Manchester- Oxford Foot Questionnaire (MOXFQ): Development and
validation of a summary index score. Bone Joint Res 2(4): 66-69.
How to cite this article: Mathavan G, Gaskell L, Pillai A, Thinesh VS, Pravin DC. Minimal Invasive Hallux Valgus Surgery: Myth or Magic. A Systematic
Review. Orthop Rheumatol Open Access J. 2015;1(1): 555551.
Orthopedics and Rheumatology Open Access Journal
51. Srivastava S, Chockalingam N, El FAkhri T (2010) Radiographic
measurements of hallux angles: a review of current techniques. Foot
(Edinb) 20(1): 27-31.
52. Chi TD, Davitt J, Younger A, Holt S, Sangeorzan BJ (2002) Intra- and
inter-observer reliability of the distal metatarsal articular angle in
008
adult hallux valgus. Foot Ankle Int 23(8): 722-726.
53. Vittetoe DA, Saltzman CL, Krieg JC, Brown TD (1994) Validity and
reliability of the first distal metatarsal articular angle. Foot Ankle Int
15(10): 541-547.
How to cite this article: Mathavan G, Gaskell L, Pillai A, Thinesh VS, Pravin DC. Minimal Invasive Hallux Valgus Surgery: Myth or Magic. A Systematic
Review. Orthop Rheumatol Open Access J. 2015;1(1): 555551.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Lifestyle and DiabesityDocument1 paginăLifestyle and DiabesityJuniper PublishersÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- In The Era of Budgetary Constraints, Cost-Effective Management of Metabolic Syndrome, Type 2 Diabetes, and Obesity Is EssentialDocument6 paginiIn The Era of Budgetary Constraints, Cost-Effective Management of Metabolic Syndrome, Type 2 Diabetes, and Obesity Is EssentialJuniper PublishersÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- DiabesityDocument1 paginăDiabesityJuniper PublishersÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Critical Limb Ischemia Treatment Strategies in Diabetics: Present Deeds and Future ChallengesDocument5 paginiCritical Limb Ischemia Treatment Strategies in Diabetics: Present Deeds and Future ChallengesJuniper PublishersÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Value of Urocortin As A Marker For Preterm LaborDocument7 paginiValue of Urocortin As A Marker For Preterm LaborJuniper Publishers100% (1)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hidden EctopicDocument2 paginiThe Hidden EctopicJuniper PublishersÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Type 2 Diabetic Patients On Insulin Can Reduce or Eliminate Insulin With Lifestyle Change and Carbohydrate RestrictionDocument5 paginiType 2 Diabetic Patients On Insulin Can Reduce or Eliminate Insulin With Lifestyle Change and Carbohydrate RestrictionJuniper PublishersÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Diagnostic Performance of Magnetic Resonance Imaging in The Pretreatment Evaluation of Invasive Cervical CarcinomaDocument7 paginiDiagnostic Performance of Magnetic Resonance Imaging in The Pretreatment Evaluation of Invasive Cervical CarcinomaJuniper PublishersÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Unusual Clinical Presentation of Congenital Malaria: Cholestasis in NewbornDocument3 paginiUnusual Clinical Presentation of Congenital Malaria: Cholestasis in NewbornJuniper PublishersÎncă nu există evaluări
- Infertility Awareness Among UK University StudentsDocument9 paginiInfertility Awareness Among UK University StudentsJuniper PublishersÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Use of Semen Quality To Predict Pregnancy in Couples Undergoing ICSIDocument4 paginiUse of Semen Quality To Predict Pregnancy in Couples Undergoing ICSIJuniper PublishersÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Experience and Knowledge of Female Genital Mutilation Amongst London Obstetrics and Gynaecology TraineesDocument4 paginiExperience and Knowledge of Female Genital Mutilation Amongst London Obstetrics and Gynaecology TraineesJuniper PublishersÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Endometrial Cancer Treatment: New Insights Into The Role of Erbb ReceptorsDocument3 paginiEndometrial Cancer Treatment: New Insights Into The Role of Erbb ReceptorsJuniper PublishersÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Safety and Efficacy of Yoga and Naturopathy Based Lifestyle in Patients Suffering From Rheumatoid ArthritisDocument5 paginiSafety and Efficacy of Yoga and Naturopathy Based Lifestyle in Patients Suffering From Rheumatoid ArthritisJuniper PublishersÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Rural Composting For Improvement of Soil Health and Sustainable AgricultureDocument8 paginiRural Composting For Improvement of Soil Health and Sustainable AgricultureJuniper PublishersÎncă nu există evaluări
- Arsenic Pollution in Agriculture: Its Uptake and Metabolism in Plant SystemDocument5 paginiArsenic Pollution in Agriculture: Its Uptake and Metabolism in Plant SystemJuniper PublishersÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Six Million Ways of Science CommunicationDocument2 paginiSix Million Ways of Science CommunicationJuniper PublishersÎncă nu există evaluări
- Energy Balance in Modern Agroecosystems Why and How?Document4 paginiEnergy Balance in Modern Agroecosystems Why and How?Juniper PublishersÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Serum Serotonin As A Novel Marker For Hepatocellular CarcinomaDocument7 paginiSerum Serotonin As A Novel Marker For Hepatocellular CarcinomaJuniper PublishersÎncă nu există evaluări
- Effect of Quercus Cortex Extract With Alum For Bacterial Metritis and Vaginitis Treatment in Different Ages in CowsDocument5 paginiEffect of Quercus Cortex Extract With Alum For Bacterial Metritis and Vaginitis Treatment in Different Ages in CowsJuniper PublishersÎncă nu există evaluări
- Quantifying The Trade Effects of Sanitary and Phytosanitary Regulations of The Eu On Sudan's Groundnuts ExportsDocument9 paginiQuantifying The Trade Effects of Sanitary and Phytosanitary Regulations of The Eu On Sudan's Groundnuts ExportsJuniper PublishersÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Ogilvie's Syndrome Complicating A Hemorrhagic Stroke of BrainstemDocument3 paginiOgilvie's Syndrome Complicating A Hemorrhagic Stroke of BrainstemJuniper PublishersÎncă nu există evaluări
- Hepatic Artery Thrombosis After Orthotopic Liver TransplantationDocument4 paginiHepatic Artery Thrombosis After Orthotopic Liver TransplantationJuniper PublishersÎncă nu există evaluări
- Quality and Complications of Colonoscopy in Ahvaz Jundishapur UniversityDocument4 paginiQuality and Complications of Colonoscopy in Ahvaz Jundishapur UniversityJuniper PublishersÎncă nu există evaluări
- Evaluation of Human Epidermal Growth Factor As A Tumor Marker in Patients With Hepatocellular Carcinoma Related To Hepatitis C VirusDocument5 paginiEvaluation of Human Epidermal Growth Factor As A Tumor Marker in Patients With Hepatocellular Carcinoma Related To Hepatitis C VirusJuniper PublishersÎncă nu există evaluări
- Transient Elastography is superior to the FIB 4 Index, Aspartate Platelet Ratio Index, Aspartate Alanine Aminotransferase Ratio, Age Platelet Index and Fibrosis Index in Diagnosing Fibrosis in Chronic Hepatitis B PatientsDocument17 paginiTransient Elastography is superior to the FIB 4 Index, Aspartate Platelet Ratio Index, Aspartate Alanine Aminotransferase Ratio, Age Platelet Index and Fibrosis Index in Diagnosing Fibrosis in Chronic Hepatitis B PatientsJuniper PublishersÎncă nu există evaluări
- Portal Venous Gas in A Patient With End-Stage Renal DiseaseDocument4 paginiPortal Venous Gas in A Patient With End-Stage Renal DiseaseJuniper PublishersÎncă nu există evaluări
- Robotic by Pass Made SimpleDocument1 paginăRobotic by Pass Made SimpleJuniper PublishersÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- A Randomized Comparative Study of Efficacy of Lamivudine and Adefovir Combination Versus Tenofovir Versus Entecavir in Decompensated Cirrhotic Patients of Hepatitis BDocument5 paginiA Randomized Comparative Study of Efficacy of Lamivudine and Adefovir Combination Versus Tenofovir Versus Entecavir in Decompensated Cirrhotic Patients of Hepatitis BJuniper PublishersÎncă nu există evaluări
- Student Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument2 paginiStudent Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationVen Belista86% (14)
- Health History GuidelinesDocument12 paginiHealth History GuidelinesRosechelle Baggao Siupan-Elarco100% (1)
- Infeksi NosokomialDocument29 paginiInfeksi NosokomialAlunaficha Melody KiraniaÎncă nu există evaluări
- Mastoidectomy and EpitympanectomyDocument18 paginiMastoidectomy and EpitympanectomyAsiya ZaidiÎncă nu există evaluări
- San Ma&no,: John Frush, and Roland FisherDocument11 paginiSan Ma&no,: John Frush, and Roland FisherAbhishek SharmaÎncă nu există evaluări
- Ebp Cauti Research PaperDocument11 paginiEbp Cauti Research Paperapi-598708595Încă nu există evaluări
- Siberia Medical TrainDocument1 paginăSiberia Medical TrainSantiago CarreñoÎncă nu există evaluări
- Perio Orto KokishDocument10 paginiPerio Orto KokishKARLA IBARRAÎncă nu există evaluări
- Pressure Ulcers - Prevention and Management of Pressure Ulcers StrategyDocument38 paginiPressure Ulcers - Prevention and Management of Pressure Ulcers StrategyAlex Alexandra AlexÎncă nu există evaluări
- Augmentation Mammoplasty:MastopexyDocument12 paginiAugmentation Mammoplasty:MastopexyfumblefumbleÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Diabetes Mellitus Prevention and Control Program I. RationaleDocument11 paginiDiabetes Mellitus Prevention and Control Program I. RationaleDayCee Ditz Gulane Orbeta50% (2)
- Daftar Pustaka: Universitas Sumatera UtaraDocument4 paginiDaftar Pustaka: Universitas Sumatera UtaraDwita Setya FitrantiÎncă nu există evaluări
- Diatermi Tonsilektomi PDFDocument6 paginiDiatermi Tonsilektomi PDFalitÎncă nu există evaluări
- 01 - Activity 01Document2 pagini01 - Activity 01Denice VicenteÎncă nu există evaluări
- Ratio - Assessment Exam Np1Document29 paginiRatio - Assessment Exam Np1Ian Mizzel A. DulfinaÎncă nu există evaluări
- Clonidine HydrochlorideDocument1 paginăClonidine HydrochlorideLovelyn Joy Abubo CortezÎncă nu există evaluări
- Regulatory Requirements For Clinical Trials in IndiDocument8 paginiRegulatory Requirements For Clinical Trials in IndiMahendran NÎncă nu există evaluări
- Incivility and Bullying PDFDocument10 paginiIncivility and Bullying PDFAndre GunawanÎncă nu există evaluări
- Clinical Trial Protocol TemplateDocument33 paginiClinical Trial Protocol TemplateNasilÎncă nu există evaluări
- The Diagnostic and Statistical Manual (Of Mental Disorder) and An Evaluation of The DSMDocument1 paginăThe Diagnostic and Statistical Manual (Of Mental Disorder) and An Evaluation of The DSMmsoonÎncă nu există evaluări
- Rights and Obligations of PatientsDocument10 paginiRights and Obligations of PatientsRey BenítezÎncă nu există evaluări
- Ethics in Abnormal PregnanciesDocument123 paginiEthics in Abnormal PregnanciesspicylaingÎncă nu există evaluări
- Medicine CasesDocument58 paginiMedicine CasesKaren McCarthyÎncă nu există evaluări
- American Bar AssociationDocument6 paginiAmerican Bar AssociationMarkWarner100% (1)
- Joanna Serat ResumeDocument2 paginiJoanna Serat Resumeapi-592283512Încă nu există evaluări
- Infection ControlDocument6 paginiInfection ControlhiyahninjaÎncă nu există evaluări
- CBT - Confidentiality and Data Protection EditedDocument5 paginiCBT - Confidentiality and Data Protection EditedChristiana OnyinyeÎncă nu există evaluări
- BrochureDocument6 paginiBrochureMargos MosgarÎncă nu există evaluări
- Reviewer - CardioDocument3 paginiReviewer - CardioLizzy WayÎncă nu există evaluări
- 03 BIRADS Mammography FAQsDocument5 pagini03 BIRADS Mammography FAQsginga tiberiuÎncă nu există evaluări
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (2)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (170)