Documente Academic
Documente Profesional
Documente Cultură
Jurnal PDCA
Încărcat de
Juwita Verawati SiahaanTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Jurnal PDCA
Încărcat de
Juwita Verawati SiahaanDrepturi de autor:
Formate disponibile
Scientific Research and Essays Vol. 6(2), pp.
463-468, 18 January, 2011
Available online at http://www.academicjournals.org/SRE
DOI: 10.5897/SRE10.1061
ISSN 1992-2248 2011 Academic Journals
Full Length Research Paper
Reducing the charging errors in an hospital emergency
department: A PDCA approach
Frank, F. C. Pan1* and Shu-Jyuan Chou2
1
Healthcare Business Administration, Tajen University, Pingtung, Taiwan.
Graduate Institute of Leisure Business Management, Tajen University, Pingtung, Taiwan.
Accepted 30 December, 2010
Modern hospitals are highly computerized in managing the routine and operational documentary
procedures. One of the best practices in managing with a computerized system was the materials used
in a hospital. One of the benefits the computer system may provide to the hospital was to save labor
force. Some problems occurred in the emergency department because the healthcare staff failed to
communicate with the system properly. This have had adverse effects on the efficiency and
effectiveness of the hospitals operation due to incorrect information the computer produced. This
project is designed to solve the problem by reducing the charging errors by adopting a PDCA cycle.
The project had achieved both tangible and intangible improvements. We have discussed the research
findings and compared this with previous studies. Several recommendations were provided for the
hospital management and the public policy decision makers.
Key words: Hospital, charging error, emergency department, PDCA, revenue leakage.
INTRODUCTION
Hospitals adopted computer in several ways to reduce
waste and error, to upgrade service quality, to facilitate a
seamless
cross-department
communication
and
cooperation, and ultimately to improve the hospitals
operational efficiency. Although some benefits were
gained, waste and errors remained. Looking into the
entire computer-aided managerial system, the labor
force remains the main mediating factor for the system.
A computer-aided managerial system requires correct
input of sufficient data, the GIGO (garbage in garbage
out) occurs when data feed into the system were wrong
in quantity and quality (Chang and Henry, 1999). The
emergency department (ED) of a hospital is typically
characterized with highly restricted time and thus
requires speedy treatment, timely decision, and seamless cooperation among healthcare professionals. Life
first is certainly the rule number one in this particular
context. It is not uncommon to find incorrect data,
particularly the material used, under this rush and
*Corresponding author. E-mail: frankpan@mail.tajen.edu.tw,
pan@msa.hinet.net. Tel: (886) 8-7624002 ext. 3120.
sometimes jammed environment. As a result, the
complexity in the current emergency treatment process
have created various opportunities for revenue leakage,
of which may result from personal ignorance to the
charging procedure. This called for keen insights into the
current operation procedure. Root cause analysis was
generally viewed as a capable approach in identifying
causes of problems, particularly in the problems that
may lead to financial leakage (Racidemann and Sandhu,
2007). Waste and errors in inventory occurs, and then
becomes an extra cost to the hospital (Sears, 2006).
This project is designed to solve the problem by first
identifying the causes step by step by a team from the
emergency department (Seid et al., 2007).
The purpose of the project is to correctly charge all
kinds of medicine, healthcare materials along with
medical treatments, to correctly reflect the costs of each
treatment and avoid waste. Accordingly, this in turn
increases the hospitals revenue (Sears, 2006).
The members of the team comprise physicians and
nurses on duty to the emergency department. Measures
to perform were categorized into two directions, one for
physicians and the other for nurses to improvement. The
former aims to input carefully with correct data, and the
464
Sci. Res. Essays
later aims to double-checking for the correctness of the
outcomes.
The project follows the PDCA cycles in the period of
June to October 2010. The process includes the
following steps in sequential order such as;
Establishing the theme, project planning, defining
current problem, targeting, analyzing, alternative evaluating, decisions, results measuring, and standardizing
the operation (Pines et al., 2002; Carter and Chochinov,
2007).
PDCA
PDCA refers to a Plan-Do-Check-Act cycle. This famous
quality improvement model was generally recognized as
one of greatest thoughts of Edward Deming. The concept of PDCA was based on the scientific method that
follow the process of "hypothesis" "experiment"
"evaluation", or plan do check (Deming, 1986;
Walton, 1986).
Initiated in the 1950s in Japan after the World War II,
the PDCA cycle was later adopted by the top Japanese
engineers and helped the Japanese industries grow
rapidly. It is also known as the Deming circle, Shewhart
cycle, Deming cycle, Deming wheel, Control circle or
cycle, or Plandostudyact (PDSA, Deming prefers to
replace check with study to emphasize the need of
control).
Some scholars pay respect to the contribution of
PDCA to the quality improvement for both manufacturing
and service process, and termed it as the Demings
Management Method (DMM) (Walton, 1986) to make the
PDCA more a theoretical approach. The DMM and the
associated fourteen points of management perspectives
were thought can serve as guidelines for quality
management by performing proper organizational
behavior and practice (Anderson, 1994). In general, the
core to the power of Deming's management method lies
in its apparent simplicity (Walton, 1986).
Other than the well-known quality process of PDCA,
there are many others that were frequently used as an
improvement model. For example, the Six-Sigma is
another commonly used improvement model in health
care (Hall et al., 2008). This typically adopts a five-phase
methodology of Define Measure Analyze Improve
- Control (DMAIC) for improving an existing process, or
another distinctive yet related sub-model of DMADV
(Define Measure Analyze Design - Verify) for designing a new process. The HFMEA (Healthcare Failure
Mode Effects Analysis) is one of the famous one that
was used in the healthcare process. Based on the failure
mode analysis in the air plane accidents, the HFMEA
has been adopted by health care industries to analyze a
new process or product to detect potential weakness or
failure prior to an actual implementation, and later on the
patient safety.
Although the recent development of Six-Sigma has
been proven to be able to result in the same purpose for
quality improvement, PDCA is a simpler, easy understanding and user-friendly approach. This is also true to
the underlying DMAIC. As to the DMADV and HFMEA,
they were mainly for checking the potential pitfalls of a
new process, and may not be appropriate for the use of
the current project (Johnson and Raterink, 2009).
MATERIALS AND METHODS
Materials used in this project are order-related information (Dean,
1996; Srivastava, 2005) in the emergency department of the
National Taitung Hospital in Taiwan for a period of June 1st to July
9th in the year 2010. This included all transactional documents
related to the physicians orders that are specifically for the
individual patients case during this period.
Methods taken in the procedure followed the FOCUS-PDCA.
These processes are finding a process to improve, organizing a
team, clarifying the current knowledge, understanding causes, and
selecting the process to improve (FOCUS) as the preparation
stage of the project. And then in the program stage followed by
planning the improvement, doing data collection and analysis jobs,
checking the improvement and customer outcomes, and acting to
hold and continue the improvement (PDCA) (Redick, 1999).
Charging procedure
The process began with a triage and ends with the patient leave
for IPD or discharge. The physician gave orders and supervised
treatments, and then performed computer key-in for prescriptions.
Nurses hand over the certified documents to the patients. As the
current process indicated, errors may occur in any steps of the
area to be improved, as shown in Figure 1, in which the physician
can fail to charge correct data with the computer and the nurse
may fail to correctly double-check the printout.
Materials
Errors found in the department were used as the material to be
investigated. Data before launching the project were collected
during the period of June 21st and July 9th, 2010 for further
analysis. A total of 342 records were collected, among which 59
errors were found, as shown in Table 1. These errors were brought
to the team meeting for further analysis. The errors that occurred
in the ED could be categorized into several aspects, as the Find
activities in the FOCUS.
Target
The target is established by including several criteria into
consideration, and a team was organized to include direct
members of ED operation, such as emergency physicians, ED
nurses, pharmacists, and medical technicians, as the Organizing
of FOCUS proposed. The target is then established as shown in
the following equation. The project team attempted to improve the
current level from 17.23% of errors to a level of 5.85% by including
the estimation of the members current capability and knowledge at
a level of 75% (that is, some capabilities needed for improvement
may exceed members current abilities) (DOH, 2006), as what the
Clarify of FOCUS required.
Current level Weight
Capability=Improvement
of
improvement
Expected
Pan and Chou
465
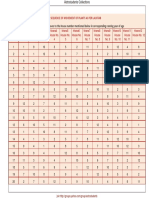
Table 1. Errors to be improved.
Descriptions
Fail to key-in treatment code
Fail to double-check the prescription
Treatment before charge
Patient discharge against physician order
Ignored a chargeable treatment
Sum
Errors
42
10
4
2
1
59
% / total
12.28
2.92
1.16
0.58
0.29
17.23
%
71.19
16.95
6.78
3.39
1.69
100.00
% accuracy
71.19
88.14
94.92
98.31
100.00
100.00
Note: 59 errors with 346 cases.
Alternatives evaluation
Triage
Area to be
improved
Medical treatment
PhysicianProduce physician orders
including prescription, documents for Xrays, examinations.
Nurse: Passes relevant documents and
offers proper health education to the
patient.
Payment / Pharmacy
Discharge/ Transfer/ IPD
Figure 1. Current procedure for ED charging.
(17.23% 88.14% x 75%11.38%)
Current level Improvement levelTargeted improvement
(17.23%11.38%5.85%)
Several alternatives were then raised, discussed, and then
evaluated by the team members, as the understanding of FOCUS
assumed. Members discussed and evaluated each alternative by
giving one (poor) to five (excellent) points on criteria of feasibility,
economy, and effectiveness.
The alternatives that received 96 points were implemented with
PDCA, as the selection action in the FOCUS, shown in Table 2. The
team then decided to take the quality improvement (QI) processes,
mainly the root-cause analysis (RCA). Other tools included in this
project by the members include flowcharts, check sheets, Pareto
diagrams, cause and effect diagrams, histograms, scatter diagrams,
and control charts (Hughes, 2008; Langley et al., 1996) to solve this
problem, as the Plan in the PDCA.
RESULTS AND ANALYSES
The team member adopted the plan in the cases of the
emergency department in the period between July 15th
and August 20th, 2010 with substantial supervisions of
nursing group leaders, as the Do action in PDCA. Major
difficulties in this stage were found in the inter-personal
communication in passing the orders. This problem had
come back to the team meeting again, and then a
modified procedure was established. In the Check
process of PDCA, the project achieved several improvements. Materially, the project sharply reduced the errors
from 17.23% for a 29 day period to the fractional 3.9% of
a 54 day period. This result is far better than the expected
target, at 5.85%. This improvement had brought visible
and tangible benefits to the hospital in terms of revenue
increasing and cost reduction, as shown in Table 3 and
Figure 2, as the Check process of PDCA.
Noteworthy, the factor of fail to key-in treatment code
gained a notably improvement, from 12.28% to a very low
level at 2.34%, as shown in Table 3. This is particularly
important to a hospital management since errors of this
kind were conventionally occurred with an emergency
physician, and were always one of the major barriers to a
hospital improvement project.
One of the most important challenges to the PDCA
management process was to hold or maintain the results
as a standard, and to encourage the members on a
continuous improvement. In the Act stage of PDCA, the
team established several guidelines for the standardized
charging process in the forms of wall posters (point by
466
Sci. Res. Essays
Table 2. Alternatives evaluations.
Problem
Evaluations
Feasibility Economy
8
10
34
18
Causes
Alternatives
Under- staffed nursing labor
Fail to double-checking prescription
Add nursing labors
Double-checking before approval
Fail to key-in treatment code
Physician established a common code for
checking purpose
40
32
30
102
Code unknown
Posters: (Around computer desk)
1. Frequent used code
2. Mis-charging reminder
38
24
24
96
Code absent
Filing frequent used codes
36
24
36
96
ED Mis-charging
Effective
28
32
Points
Decisions
46
84
Notes: Actions to be taken are those scored 96 points or more; marked with an
Table 3. Improvement summaries.
Items
Fail to key-in treatment code
Fail to double-check the prescription
Treatment before charge
Patient discharge against physician order
Ignored a chargeable treatment
Sum
point) and pamphlet. A concise process of the
standard process is also illustrated in a simple
chart, and to be added as a notice in shiftrotating
checklist. This action helps keeping the charging
errors low.
Before
(06/21- 07/09)
n
%
42
12.28
10
2.92
4
1.16
2
0.58
1
0.29
59
17.23
Process
(08/09-08/20)
n
%
30
8.77
6
1.75
1
2.92
2
5.84
0
0.00
39
19.28
DISCUSSION
This project involved several physicians and
nurses that were assigned to the emergency
department for a mis-charging problem. This
After
(08/30-09/10)
n
%
8
2.34
3
0.87
1
0.29
1
0.29
0
0.00
13
3.79
project was successful by not only substantially
reducing the charging errors from 17.28 to 3.79%,
and accordingly reflected true operational costs
and increase revenue, but also provided a
communication opportunity for team members to
Pan and Chou
14.00
12.28
12.00
10.00
8.77
Before
8.00
Process
6.00
After
4.00
2.34
2.00
0.00
Before
Process
After
Figure 2. Substantial improvements (fail to key-in).
gain consensus on the process of charging procedure.
Important of note is the cooperative manner provided by
the medical department, which was hardly expected in
normal cases. Compared to the improvement level
suggested by DOH (DOH, 2006) that to count the
members capability at 75% and to reduce the rate to
5.85%, this project had achieved a better performance
than the suggested standard by reducing this rate to
3.79%. As a matter of fact, the major component of the
project achievement was contributed by the emergency
physicians. Other than the top management support, one
of the major reasons behind a full cooperation from the
medicine department may originate from the simplicity
and easy understanding of a PDCA cycle. This further
provides evidence on the applicability and the usefulness
of PDCA cycle due to its simplicity (Walton, 1986).
Take this project as an example, hospitals must provide
a consistent, easy-to-use and simplistic interface for
correct information exchange in order to enable the
visibility of a process. A combination of order-to-invoice
quality and collections automation technologies may be
worthy to adopt to fill up possible sources of profit leaking
(Srivastava, 2005).Members of the team then received
varied forms of awards and incentives. However, the
more important implication to the success of this project
was to deliver a clear message that a possibility of
improvement was always there for the team to identify
and gain further advancement (Judith, 1997). There were
plenty of blind spots that were ignored by inertia. This
team has decided to exploit this experience to improve
the correctness of patient identification.
Barriers to the success of an improvement pro-gram
may stem from both structure and process (Johnson and
Raterink, 2009). Whilst the process problem could be
overcome by close supervision and quality control
training, the former was typically out of the control of a
467
project team, thus require a support of the management
of an organi-zation. To gain and hold the success
constant of any improvement, support from the organization is essential (Seid et al., 2007; Sadeghian, 2010).
Project initiated by the emergency department has gained
multiple supports from the hospital management. The
director of the hospital clearly declared full support by
announcing the project with spiritual speech in the
hospital-wide meeting, and offered incentive promises to
the team. This acts as an important moderator for the
success of the project, which was consistent with the
studies of Parker et al. (1999); Seid et al. (2007) and
Sadeghian (2010).
Since maintaining a healthy status is part of the primary
rights of a human being, the hospital industry shall align
its operation policy with the nationals health concern.
This means the healthcare industry, including hospital,
and it does not matter if was private- or state-owned,
shall be viewed as part of a public service. A quality
improvement gained in a hospital department will not be
of benefit to the hospital by reducing cost or waste, but
also increasing the service quality (Deming, 1986). It is
recommended that the government shall establish an
accessible incentive program to encourage hospital
industry continuously conducting the quality improvement
projects, among which the PDCA would be one of the
best alternative approaches for its simplicity.
Conclusions
A simple yet effective approach to solve problems in a
hospital emergency department is possible. A strategy
that integrates team members effort to create a
consensus toward a well-defined problem is the critical
success factor (Stone, 1998).
This charging error reduction project had gained good
results and will benefit multiple parties without additional
costs or safety sacrifice. Correct recording in the process
of emergency treatment avoids wastes in healthcare
material and time. It accordingly creates more room for
healthcare professionals to care for the patients (Carter
and Chochinov, 2007), which in turn will increase family
satisfaction (Zimmermann et al., 2008). The hospital
gained additional revenue by filling the leakage, polished
its managerial system with correct and timely information;
the patients are charged with users expenses under a
correct record that would be used as important information for future diagnosis; the team was cheered with
the performance (material and psychological) from the
project. Team member realized the existence of a
personal blind spot, and gained confidence from the
project activities (Stone, 1998; Sears, 2006). It is a winwin outcome.
REFERENCES
Anderson JC (1994). A theory of quality management underlying the
468
Sci. Res. Essays
Deming management method. Aca. Manage. Rev., 19(3): 472-509.
Carter AJ, Chochinov AH (2007). A systematic review of the impact of
nurse practitioners on cost, quality of care, satisfaction and wait times
in the emergency department. CJEM., 9: 286-95.
Chang WY, Henry BM (1999). Methodologic principles of cost analysis
in the nursing, medical, and health service literature, 1990-1996.
Nurs. Res.,48(2): 94-104.
Deming WE (1986). Out of the Crisis. MA: MIT Center for Advanced
Engineering Study.
Department of Health (DOH) (2006). Treatment of disposal operations
reduce the amount of leakage account. Taiwan Joint Commission on
Hospital Accreditation. The 6th Medical Quality Award Competition.
(In Chinese).
Hall LW, Moore SM, Barnsteiner JH (2008). Quality and nursing: moving
from a concept to a core competency. Urologic Nurs.,28(6):417- 425.
Hughes R (2008). Tools and strategies for quality improvement and
patient safety. In Patient safety and quality: An evidence-based
handbook for nurses. Chapter 44. AHRQ Publication No. 08- 0043.
Rockville, MD: Agency for Healthcare Research and Quality.
Johnson P, Raterink G (2009). Implementation of a diabetes clinic-in-aclinic project in a family practice setting: using the plan, do, study, act
model. J. Clinic. Nurs., 18(14): 2096-2103.
Judith S (1997). How nursing contributes towards quality and costeffective health care. Int. Nurs. Rev., 44: 79-84.
Langley GJ, Nolan KM, Nolan TW, Norman CL, Provost LP (1996). The
Improvement
Guide:
A
Practical
Approachto
Enhancing
Organizational Performance. San Francisco: Jossey-Bass.
Parker VA, Wubbernhost WH, Young GJ, Desai KR, Charns MP (1999).
Implementing quality improvement in hospitals: the roles of
leadership and culture. Am. J. Med. Qual., 14: 64-69.
Pines JM, Fager SS, Milzman DP (2002). A review of costing
methodologies in critical care studies. J. Crit. Care, 17: 181-186.
Racidemann B, Sandhu R (2007). Root cause analysis to improve payer
profiling. Healthcare Fin. Manage., 61(8): 97-98.
Redick EL (1999). Applying FOCUS-PDCA to solve clinical problems.
Dimens. Critic. Care Nurs., 18(6): 30-34.
Sadeghian MR (2010). A Study of the Significance of Organisational
Culture for the Successful Implementation and Operation of Total
Quality Management (TQM): A Comparative Study between Iran and
the UK. Doctoral dissertation, University of Huddersfield, West
Yorkshire, UK.
Sears NJ (2006). Deriving cost savings while enhancing quality of care
through effective case management in the acute care facility.
Lippincotts Case Manage., 11: 59-60.
Seid M, Lotstein D, Williams VL, Nelson C, Leuschner KJ, Diamant A,
Stern S, Wasserman J, Lurie N (2007). Quality improvement in
public health emergency preparedness. Annu. Rev. Public Heal., 28:
19-31.
Srivastava S (2005). Using technology to trim revenue and receivables
leakage. Fin. Exe., 21 (7): 64-65.
Stone PW (1998). Methods for conducting and reporting costeffectiveness analysis in nursing. J. Nurs. Scholar., 30: 229-234.
Walton M (1986). The Deming Management Method. NY: Penguin
Group.
Zimmermann C, Riechelmann R. Krzyzanowska M, Rodin G, Tannock I
(2008). Effectiveness of specialized palliative care: a systematic
review. JAMA, 299: 1698-1709.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Cba2 PDFDocument9 paginiCba2 PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Jurnal Pdca 2 PDFDocument5 paginiJurnal Pdca 2 PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Jurnal MutuDocument18 paginiJurnal MutuJuwita Verawati SiahaanÎncă nu există evaluări
- Publikasi 06.12.1476Document20 paginiPublikasi 06.12.1476Hachiko Dhe-dheÎncă nu există evaluări
- Jurnal MutuDocument18 paginiJurnal MutuJuwita Verawati SiahaanÎncă nu există evaluări
- Jurnal Mutu KeperawatanDocument7 paginiJurnal Mutu KeperawatanJuwita Verawati SiahaanÎncă nu există evaluări
- Formula Tenaga Perawat PDFDocument12 paginiFormula Tenaga Perawat PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Formula Tenaga Perawat PDFDocument12 paginiFormula Tenaga Perawat PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Formula Tenaga Perawat PDFDocument12 paginiFormula Tenaga Perawat PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Formula Tenaga Perawat PDFDocument12 paginiFormula Tenaga Perawat PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Formula Tenaga Perawat PDFDocument12 paginiFormula Tenaga Perawat PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Formula Tenaga Perawat PDFDocument12 paginiFormula Tenaga Perawat PDFJuwita Verawati SiahaanÎncă nu există evaluări
- Formula Tenaga Perawat PDFDocument12 paginiFormula Tenaga Perawat PDFJuwita Verawati SiahaanÎncă nu există evaluări
- LicenseDocument3 paginiLicenseDidi IrawanÎncă nu există evaluări
- Frequency Polygons pdf3Document7 paginiFrequency Polygons pdf3Nevine El shendidyÎncă nu există evaluări
- RV900S - IB - Series 3Document28 paginiRV900S - IB - Series 3GA LewisÎncă nu există evaluări
- Integration Plan Grade 9 Mapeh SeptemberDocument3 paginiIntegration Plan Grade 9 Mapeh Septemberbernie evaristo bacsaÎncă nu există evaluări
- INSTRUCTIONAL SUPERVISORY PLAN 1st Quarter of SY 2023 2024 Quezon ISDocument7 paginiINSTRUCTIONAL SUPERVISORY PLAN 1st Quarter of SY 2023 2024 Quezon ISayongaogracelyflorÎncă nu există evaluări
- Bug Life Cycle in Software TestingDocument2 paginiBug Life Cycle in Software TestingDhirajÎncă nu există evaluări
- Daily Lesson Log (English)Document8 paginiDaily Lesson Log (English)Julius Baldivino88% (8)
- FmatterDocument12 paginiFmatterNabilAlshawish0% (2)
- Jarir IT Flyer Qatar1Document4 paginiJarir IT Flyer Qatar1sebincherianÎncă nu există evaluări
- USB-to - Serial RS-232 Hub USB-to - Serial RS-422/485 Hub: UC2322/UC2324/UC4852/UC4854Document1 paginăUSB-to - Serial RS-232 Hub USB-to - Serial RS-422/485 Hub: UC2322/UC2324/UC4852/UC4854sitrakiniavoÎncă nu există evaluări
- Lalkitab Varshphal Chart PDFDocument6 paginiLalkitab Varshphal Chart PDFcalvinklein_22ukÎncă nu există evaluări
- Non-Emulsifying Agent W54Document12 paginiNon-Emulsifying Agent W54Pranav DubeyÎncă nu există evaluări
- Report Painter GR55Document17 paginiReport Painter GR55Islam EldeebÎncă nu există evaluări
- Sta404 07Document71 paginiSta404 07Ibnu Iyar0% (1)
- Electric PotentialDocument26 paginiElectric PotentialGlitchÎncă nu există evaluări
- 3.15.E.V25 Pneumatic Control Valves DN125-150-EnDocument3 pagini3.15.E.V25 Pneumatic Control Valves DN125-150-EnlesonspkÎncă nu există evaluări
- Sap EwmDocument2 paginiSap EwmsirivirishiÎncă nu există evaluări
- DJF 41032 Manufacturing Workshop Practice 3 Plastic Lab: Mini Project (Transfer Moulding)Document7 paginiDJF 41032 Manufacturing Workshop Practice 3 Plastic Lab: Mini Project (Transfer Moulding)Lokhman HakimÎncă nu există evaluări
- Changing Historical Perspectives On The Nazi DictatorshipDocument9 paginiChanging Historical Perspectives On The Nazi Dictatorshipuploadimage666Încă nu există evaluări
- ZH210LC 5BDocument24 paginiZH210LC 5BPHÁT NGUYỄN THẾ0% (1)
- Science, Technology and Society Module #1Document13 paginiScience, Technology and Society Module #1Brent Alfred Yongco67% (6)
- Feasibility and Optimization of Dissimilar Laser Welding ComponentsDocument366 paginiFeasibility and Optimization of Dissimilar Laser Welding Componentskaliappan45490Încă nu există evaluări
- Distillation Column DesignDocument42 paginiDistillation Column DesignAakanksha Raul100% (1)
- DAB Submersible PumpsDocument24 paginiDAB Submersible PumpsMohamed MamdouhÎncă nu există evaluări
- Question BankDocument3 paginiQuestion BankHimanshu SharmaÎncă nu există evaluări
- Formula Renault20 Mod00Document68 paginiFormula Renault20 Mod00Scuderia MalatestaÎncă nu există evaluări
- 01 IntroductionDocument15 pagini01 IntroductionAli FarhatÎncă nu există evaluări
- Using Impact IX49 and 61 With Nektar DAW Integration 1.1Document21 paginiUsing Impact IX49 and 61 With Nektar DAW Integration 1.1Eko SeynÎncă nu există evaluări
- ARCASIA Students Design Competition TORDocument4 paginiARCASIA Students Design Competition TORDeena McgeeÎncă nu există evaluări
- ER288 090714 5082 CV OKP (089) Method Statement For Plate Baring TestDocument3 paginiER288 090714 5082 CV OKP (089) Method Statement For Plate Baring TestWr ArÎncă nu există evaluări
- BS7430 Earthing CalculationDocument14 paginiBS7430 Earthing CalculationgyanÎncă nu există evaluări