Documente Academic
Documente Profesional
Documente Cultură
Subacromial Impingement Syndrome and Rotator Cuff Tendinopathy: The Dilemma of Diagnosis
Încărcat de
TomBrambo0 evaluări0% au considerat acest document util (0 voturi)
82 vizualizări4 paginiPhysical therapy
Titlu original
Lewis_0913
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentPhysical therapy
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
82 vizualizări4 paginiSubacromial Impingement Syndrome and Rotator Cuff Tendinopathy: The Dilemma of Diagnosis
Încărcat de
TomBramboPhysical therapy
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 4
fag
KRONIKK
Subacromial impingement syndrome
and rotator cuff tendinopathy:
The dilemma of diagnosis
Dr Jeremy S
Lewis, PhD MSc
(Manipulative Physiotherapy) FCSP.
Consultant Physiotherapist, Sonographer. Research
and Innovation Lead,
Health at Stowe,
Central London
Community Healthcare NHS Trust.
Reader in Physiotherapy Research, University of Hertfordshire, Hertfordshire,
UK. Email:
jeremy.lewis@LondonShoulderClinic.com
Web: www.LondonShoulderClinic.com
Denne fagkronikken ble akseptert
06.03.2013. Fagkronikker vurderes av
fagredaktr.
Introduction
Musculoskeletal pathology involving the
shoulder is associated with substantial morbidity and loss of function that increases
with age (1-3). It is generally considered
that effective treatment is dependent upon
understanding the mechanism of onset together with identification of the structure(s)
involved with the symptoms and excluding
those not involved. Mechanisms may involve; trauma, inappropriate ergonomic setup, posture, repetitive and/or unaccustomed
loading, systemic illness, local disease, or be
idiopathic. Following routine clinical procedures that include; observation, assessment
of active and passive movements, palpation,
and resistance tests, a series of orthopaedic
tests are commonly applied to identify the
structure(s) responsible for the pain and
44
Fysioterapeuten 9/13
sub-optimal function (4). Orthopaedic
shoulder tests fall into a number of different categories. Tests have been proposed
to identify instability; such as the load and
shift, sulcus and provocation tests (5).The
Neer impingement sign (6), the Hawkins
test (7) and the internal rotation resistance
strength test (8) have been proposed to assess impingement. Clinicians identify labral
pathology utilising tests such as the; OBrien
active compression test (9) the Crank test
(10) and Kim test (11). Recommendations to identify rotator cuff and biceps
tendon pathology include; Speeds test (4),
Yergasons test (4) and Empty can test (12).
Clinical tests are devised by designing a clinical test to stretch, contract and/or compress a specific shoulder tissue. The diagnostic accuracy of the test is then determined by
comparing the clinical outcome with a gold
standard comparison, such as; radiography,
ultrasound scan, magnetic resonance imaging, computed tomography and direct observation such as during open or arthroscopic surgery. The gold standard tests involve
observation of structural pathology, and it
is this structural pathology which is considered to be the source of symptoms. In
the shoulder, structural pathology such as;
rotator cuff tendinopathy, bursal effusion,
partial and full thickness rotator cuff tears,
labral lesions and degenerative joint changes
are considered to generate symptoms and
the symptoms produced during the clinical
tests are compared against these changes.
For example weakness and pain during the
empty can test becomes diagnostic for supraspinatus pathology (tendinosis through
to full thickness tear) if an US or MRI scan
demonstrates structural failure. A true positive occurs when the gold standard test
is positive (ie observable rotator cuff tear)
and the clinical test is positive (ie pain and
weakness). A true negative is when the clinical test is negative (ie no pain and weakness)
and the gold standard test (ie MRI and US)
does not demonstrate any structural failure.
This process allows for the construction of
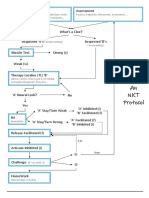
the classic 2x2 table used to determine diagnostic accuracy (Figure 1).
In this example if a patient presents with
a painful shoulder and a test for a labral tear
is positive and an MRI demonstrates a labral
tear this would be a true positive. If the
clinical test does not produce symptoms and
an MRI demonstrates no labral pathology,
then this is a true negative. Clinical tests that
produce only true positive and true negative
results provide clinicians with considerable
diagnostic confidence to enable clinical
reasoning, treatment planning and patient
education. However, situations occur
Figure 1 2x2 Table used to compare clinical findings and gold standard structural changes.
Reference test
positive +ve
Reference test
negative -ve
Clinical test
positive +ve
(a)
True positive
(b)
False positive
Clinical test
negative -ve
(c)
False negative
(d)
True negative
Some clinicians have recognised that making a
structural diagnosis is challenging and have moved towards a symptoms modification approach.
Mobilization If a single SSMP procedure totally alleviates symptoms, treatment is instigated to
reduce the kyphosis. This may be done by postural awareness exercises, strengthening exercise,
stretching, thoracic mobilizations and taping. Photo: Heidi Johnsen
when the clinical test is negative and the
diagnostic reference test is positive, and the
clinical test is positive and the diagnostic
reference test is negative. These results are
respectively known as false negatives and
false positives. For a clinical assessment
procedure to be of clinical value to identify
symptomatic pathology in only one
structure both the sensitivity of the test (true
positive/true positive and false negative),
and specificity of a test (true negative/true
negative and false positive), both must be
as close to 100% as possible (13). This
can only occur if the clinical test assesses
only one structure and the gold standard
reference tests only demonstrate structural
pathology when symptoms are present.
Reproduction of symptoms
If the sensitivity is high (ie close to 100%),
but the specificity is low, then the clinician
will be able to reproduce symptoms, but in
reality will not know which structure is causing the symptoms. Unfortunately this is the
case for the majority of tests designed to test
for impingement and rotator cuff pathology.
The clinical tests often reproduce the symptoms of pain and weakness, but frequently
the reference tests are negative, and equally
the clinical tests are negative and the reference tests are positive (14-17). Sometimes
the specificity of a test may only be 50% (16,
17) which would not allow the clinician to
develop an informed opinion as to where
the symptoms were coming from. Calis et
al (18) reported a sensitivity of 88.7% and
a specificity of 30.5% for the Neer impingement sign. Litaker et al (19) reported values
of 97.4% and 9.0% for the same test. Calis
et al (18) reported sensitivity and specificity
values of 92.1% and 25% for the Hawkins
test. These figures clearly question the ability
to arrive at a definitive diagnosis. Hegedus
et al (20) have recently published a comprehensive review investigating clinical shoulder tests. They concluded that the use of any
single shoulder orthopaedic tests to make a
conclusive diagnosis is questionable.
If diabetes is suspected, it is conceivable
that both clinicians and patients might be
reluctant to commence insulin therapy if a
blood test was only 50% accurate in detecting diabetes as the cause of the presenting
symptoms. However many patients are being referred for surgery (subacromial decompression and rotator cuff repair) on the
basis of clinical tests that cannot definitively
confirm a diagnosis and imaging tests that
might demonstrate structural pathology
but the structural changes may be entirely
asymptomatic (15, 21-26).
There are many reasons why the clinical
orthopaedic tests for the shoulder are incapable of isolating individual structures.
These include; (i) rotator cuff tendons that
are not individual units but attach to other
tendons and tissues such as ligaments and
capsules (27, 28), and (ii) the presence of
up to 12 bursae around the shoulder (29)
that are capable of generating pain (30).
These structures may be stretched and/or
compressed in all the shoulder orthopaedic
tests. In addition to this, weakness may not
be true weakness, but be due to pain inhibition (31, 32). It is not known why structural
change may not be symptomatic, but with
studies reporting that up to 50% or more of
people without symptoms may have structural change (21, 22, 24, 25), imaging cannot
inform a clinician conclusively where the
symptoms are emanating from. These issues
have recently been explored in detail (15,
26).
Currently it appears that the process of
making a diagnosis using a combination
of clinical tests supported by imaging findings will not allow a clinician to arrive at a
structural diagnosis with certainty (26). This
has been recognized by clinicians treating
other areas of the body (33, 34).
The Shoulder Symptom Modification
Procedure
With respect to the shoulder, some clinicians have recognized that making a structural diagnosis is challenging and have moved
towards a symptoms modification approach
(26, 35, 36). One such process is known as
the Shoulder Symptom Modification Procedure (SSMP) (26). The SSMP involves a sequential process that aims at immediately
Fysioterapeuten 9/13
45
FAG kronikk
identifying postures and techniques that
will reduce symptoms. Initially a number of
postures, movements and activities that reproduce shoulder symptoms are identified,
quantified and qualified. These are patient
determined and are associated with symptoms that if reduced or eliminated would
make a measureable improvement to the
quality of the patients life. Once identified,
the first procedure is to determine the immediate effect of altering the thoracic kyphosis on the symptoms. This is either done
actively or in the case of more challenging
functions, such as; swimming, throwing,
push ups or other complex upper limb function, tape is used to control the kyphosis
(26). If this single procedure totally alleviates
symptoms, treatment is instigated to reduce
the kyphosis. This may be done by postural
awareness exercises, strengthening exercise, stretching, thoracic mobilizations and
taping. The SSMP algorithm requires each
technique to be tested on 2 separate occasions to ensure the effect of any modification
procedure is consistent and mechanical. If
the thoracic procedure reduces symptoms
by 100% on two occasions, treatment is only
directed at treating this. If reducing the kyphosis makes no impact on symptoms then
the next part of the algorithm is assessed.
If reducing the kyphosis results in a partial
reduction in symptoms, the effect of this is
then added to the next part of the algorithm.
The next part of the algorithm involves assessing three planes of scapular position and
combinations of positions on symptoms.
This may be done during weight bearing and
non-weight bearing activities. The changes
to scapular position are minimal and are
not designed to restrict or facilitate scapular
movement. They only serve to alter the starting position of the scapula and the way the
scapular moves on the thorax and articulates
with the humeral head. Again if this procedure alone or in combination with the thoracic procedure results in 100% reduction in
symptoms on two occasions, the assessment
procedure is stopped and treatment commenced. If all symptoms are not resolved,
then the next part of the algorithm is assessed. The next component of the SSMP is to investigate the relationship between the glenoid fossa and humeral head. This component
assesses the glenohumeral relationship by
using up to 13 very quick procedures. Testing stops if one or a combination of techniques results in 100% reduction of symptoms
46
Fysioterapeuten 9/13
(on two occasions). As with the other parts
of the SSMP algorithm, techniques that are
used to assess and reduce symptoms are then
used to inform techniques that are used to
treat. As this is patient lead, it is hoped that
improved compliance results from the fact
it is the patient that has identified what is
helping to reduce their symptoms. The final
component of the Shoulder Symptom Modification procedure is determining the effect
of neuromodulation procedures on shoulder
symptoms. This involves, manual therapy,
taping and soft tissue based techniques. If all
the symptoms are eliminated by one part or
a combination of components of the SSMP,
then no further investigation is required. If
the SSMP fails to reduce any symptoms (as
will happen with frozen shoulder), another
care pathway is instigated. If the SSMP partially reduces symptoms, then a determination
of the reasons for the remaining symptoms is
made and appropriate treatment instigated.
Common reasons for this are a concomitant
rotator cuff and/or biceps tendinopathy. In
addition to using the componenets of the
SSMP that reduced symptoms, alternative
treatment is instigated respecting the stage
of the tendinopathy (37). It is essential that
prior to applying the SSMP other causes of
pain and symptoms such as sinister pathology/red flags are carefully and thoroughly
screened for (38). If the patient fails to respond, then an appropriate onward referral
is mandatory.
Conclusions
The SSMP has been advocated due to the
clinical dilemma of making a definitive
structural diagnosis. The reliability of the
procedure is currently being tested in intra- and inter-tester reliability studies, and
its ability to inform management will also
be subject to future research. In addition to
shoulder management approaches such as
the Shoulder Symptom Modification Procedure (26), effort is required to develop ways
to improve methods of making a structural
diagnosis through enhanced clinical and
imaging procedures.
References
1. Brox JI. Regional musculoskeletal conditions: shoulder pain.
Best Pract Res Clin Rheumatol. 2003;17(1):33-56.
2. van der Heijden GJ. Shoulder disorders: a state-of-the-art
review. Baillieres Clin Rheumatol. 1999;13(2):287-309.
3. Taylor W. Musculoskeletal pain in the adult New
Zealand population: prevalence and impact. N Z Med J.
2005;118(1221):U1629.
4. Magee D. Orthopedic Physical Assessment. 3rd ed. Philadel-
phia: WB Saunders Co; 1997.
5. Tzannes A, Paxinos A, Callanan M, Murrell GA. An assessment
of the interexaminer reliability of tests for shoulder instability.
Journal of shoulder and elbow surgery / American Shoulder and
Elbow Surgeons [et al]. 2004;13(1):18-23. Epub 2004/01/22.
6. Neer CS, 2nd. Impingement lesions. Clinical orthopaedics and
related research. 1983(173):70-7.
7. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes.
The American journal of sports medicine. 1980;8(3):151-8.
8. Zaslav KR. Internal rotation resistance strength test: a new
diagnostic test to differentiate intra-articular pathology from
outlet (Neer) impingement syndrome in the shoulder. Journal
of shoulder and elbow surgery / American Shoulder and Elbow
Surgeons [et al]. 2001;10(1):23-7.
9. OBrien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The
active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. The
American journal of sports medicine. 1998;26(5):610-3.
10. Liu SH, Henry MH, Nuccion SL. A prospective evaluation of
a new physical examination in predicting glenoid labral tears.
The American journal of sports medicine. 1996;24(6):721-5.
11. Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel
test for posteroinferior labral lesion of the shoulder--a comparison to the jerk test. The American journal of sports medicine.
2005;33(8):1188-92.
12. Jobe FW, Moynes DR. Delineation of diagnostic criteria and
a rehabilitation program for rotator cuff injuries. The American
journal of sports medicine. 1982;10(6):336-9.
13. Sackett D, Straus S, Richardson W, Rosenberg W, Haynes R.
Evidence-based medicine. How to teach and practice EBM. 2
ed. Edinburgh: Churchill Livingstone; 2000.
14. Lewis JS. Rotator cuff tendinopathy / subacromial impingement syndrome: Is it time for a new method of assessment?
British journal of sports medicine. 2008.
15. Lewis JS. Subacromial impingement syndrome: A musculoskeletal condition or a clinical illusion? Physical Therapy Review.
2011;16(5):388-98.
16. Lewis JS, Tennent TD. How effective are diagnostic tests
for the assessment of rotator cuff disease of the shoulder?
In: MacAuley D, Best TM, editors. Evidenced Based Sports
Medicine. 2nd ed. London: Blackwell Publishing; 2007.
17. Hegedus EJ, Goode A, Campbell S, Morin A, Tamaddoni
M, Moorman CT, 3rd, et al. Physical examination tests of the
shoulder: a systematic review with meta-analysis of individual
tests. British journal of sports medicine. 2008;42(2):80-92;
discussion
18. Calis M, Akgun K, Birtane M, Karacan I, Calis H, Tuzun F.
Diagnostic values of clinical diagnostic tests in subacromial
impingement syndrome. Annals of the rheumatic diseases.
2000;59(1):44-7.
19. Litaker D, Pioro M, El Bilbeisi H, Brems J. Returning to the
bedside: using the history and physical examination to identify
rotator cuff tears. J Am Geriatr Soc. 2000;48(12):1633-7.
20. Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer
DM, et al. Which physical examination tests provide clinicians
with the most value when examining the shoulder? Update
of a systematic review with meta-analysis of individual tests.
British journal of sports medicine. 2012;46(14):964-78. Epub
2012/07/10.
21. Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotatorcuff changes in asymptomatic adults. The effect of age, hand
dominance and gender. J Bone Joint Surg Br. 1995;77(2):296-8.
22. Frost P, Andersen JH, Lundorf E. Is supraspinatus pathology
as defined by magnetic resonance imaging associated with
clinical sign of shoulder impingement? Journal of shoulder and
elbow surgery / American Shoulder and Elbow Surgeons [et
al]. 1999;8(6):565-8.
23. Connor PM, Banks DM, Tyson AB, Coumas JS, DAlessandro
DF. Magnetic resonance imaging of the asymptomatic shoulder
of overhead athletes: a 5-year follow-up study. The American
journal of sports medicine. 2003;31(5):724-7.
24. Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic
shoulders. J Bone Joint Surg Am. 1995;77(1):10-5.
25. Miniaci A, Mascia AT, Salonen DC, Becker EJ. Magnetic resonance imaging of the shoulder in asymptomatic professional
Revmatiske leddsykdommer: Effekt av gruppebehandling
i oppvarmet basseng
Sammendrag av Bassengprosjektet.
Skrevet av Anne Christie, fysioterapeut,
Ph.d., Nasjonalt Kompetansesenter for
revmatologisk rehabilitering - NKRR, Diakonhjemmet Sykehus, Oslo.
Bakgrunn: Til tross for at gruppebehandling i oppvarmet basseng er hyt
verdsatt av personer med revmatisk leddsykdom er de helsemessige gevinstene av
slik behandling ikke tilstrekkelig vitenskapelig dokumentert. Hensikten med
prosjektet er underske effekt av gruppebehandling i oppvarmet basseng p
symptomer og fysisk aktivitetsniv hos
denne pasientgruppen.
Personer med inflammatorisk revmatisk leddsykdom kan oppleve store svingninger i symptomer, bde i lpet av en
dag og over tid. P grunn av sykdommens
svingende forlp kan det vre vanskelig
skille behandlingseffekt fra sykdommens
naturlige svingninger. Prosjektet benytter
derfor en metode med mange gjentatte
mlinger fr, under og etter bassengbehandlingen (interrupted time-series design = ITS). Tradisjonelt har pasientrapporterte data blitt samlet inn ved hjelp av
sprreskjema (gullstandard), men denne
metoden er lite egnet ved mange og hyppige mlinger.
Tekstmeldinger over mobiltelefon
baseball pitchers. The American journal of sports medicine.
2002;30(1):66-73.
26. Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment?
British journal of sports medicine. 2009;43(4):259-64.
27. Clark J, Sidles JA, Matsen FA. The relationship of the glenohumeral joint capsule to the rotator cuff. Clinical orthopaedics
and related research. 1990(254):29-34.
28. Clark JM, Harryman DT, 2nd. Tendons, ligaments, and
capsule of the rotator cuff. Gross and microscopic anatomy. J
Bone Joint Surg Am. 1992;74(5):713-25.
29. Codman E. The Shoulder: Rupture of the supraspinatus
tendon and other lesions in or about the subacromial bursa.
Boston: Thomas Todd Company; 1934.
30. Gotoh M, Hamada K, Yamakawa H, Inoue A, Fukuda H.
Increased substance P in subacromial bursa and shoulder pain
in rotator cuff diseases. J Orthop Res. 1998;16(5):618-21.
31. Steenbrink F, de Groot JH, Veeger HE, Meskers CG, van de
Sande MA, Rozing PM. Pathological muscle activation patterns
in patients with massive rotator cuff tears, with and without
subacromial anaesthetics. Manual therapy. 2006;11(3):231-7.
32. Wassinger CA, Sole G, Osborne H. The role of experimen-
(SMS) har vist seg egnet for dette designet,
i tillegg til at metoden gir mulighet for registrering av tid og dato for rapportering.
Pilotprosjekt: Metodeutprving: I
pilotprosjektet ble SMS (ny metode) sammenlignet med sprreskjema (gullstandarden). Hensikten med pilotprosjektet
var to-delt: 1)Teste metodens funksjonalitet og 2)Sammenligne tekstmelding (ny
metode) med sprreskjema (gullstandard).
Metode: Tjue-tte deltakere besvarte
daglig 4 sprsml (smerte, tretthet, stivhet
og evne til utfre daglige aktiviteter) p
en gradert numerisk skal (0 - 10, 10 = best)
over en periode p 28 pflgende dager.
Annenhver dag fikk deltakerne tilsendt
flgende SMS:
Fra 0-10, angi grad av smerte, tretthet,
stivhet og evne til utfre daglige aktiviteter n? 0 = ingen, 10 = verst tenkelig. Husk
punktum mellom tallene. TAKK!
Fullstendig tekst var gitt deltakerne p
plastbelagte kort i lommeformat.
Deltakerne skulle svare p SMS ved
taste inn det tallet de syntes passet best for
hvert sprsml og skille tallene med punktum, eks. 6.3.7.5. Annenhver dag skulle
deltakerne besvare de samme sprsmlene
p sprreskjema.
Data fra SMS ble lastet ned via en sikret
server, mens data fra sprreskjema mtte
tally-induced subacromial pain on shoulder strength and
throwing accuracy. Manual therapy. 2012;17(5):411-5. Epub
2012/04/17.
33. OSullivan P. Its time for change with the management of
non-specific chronic low back pain. British journal of sports
medicine. 2012;46(4):224-7. Epub 2011/08/09.
34. Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC.
Physical examination tests for assessing a torn meniscus in
the knee: a systematic review with meta-analysis. The Journal
of orthopaedic and sports physical therapy. 2007;37(9):54150. Epub 2007/10/18.
35. Mulligan BR. Manual Therapy Nags, Snags, MWMs
etc. 4th ed. New Zealand: Plane View Services; 1999.
36. McKenzie R, Watson G, Lindsay R. Treat your own shoulder.
New Zealand: Spinal Publications New Zealand Limited; 2009.
37. Lewis JS. Rotator cuff tendinopathy: a model for the continuum of pathology and related management. British journal of
sports medicine. 2010;44(13):918-23.
38. Greenhalgh S, Self J. Red flags: A guide to identifying
serious pathology of the spine. Edinburgh: Churchill Livingstone
Elsevie; 2006.
plottes manuelt.
Forelpige resultater fra pilotprosjektet viser (ikke publiserte data): Skrer
(gjennomsnitt) og variasjon (SD og range)
var sammenlignbare mellom de to formatene. SMS datasettene var mer komplette
enn datasettene fra sprreskjemaene. Deltakerne foretrakk SMS som metode.
Hovedprosjektet: Multisenterstudie
med deltakelse fra Haugesund Sanitetsforening Revmatismesykehus, Revmatismesykehuset i Lillehammer og Rehabiliteringssenteret Nord-Norges Kurbad i
Troms.
Intervensjon: Poliklinisk gruppebehandling i oppvarmet basseng (> 32 grader) en gang per uke 45 min over en 12
ukers periode. Behandlingen instrueres av
fysioterapeut og vektlegger trening av bevegelighet, styrke, utholdenhet og balanse.
Gruppene flges over fire perioder: To
perioder med bassengbehandling og to perioder uten bassengbehandling.
Metode: Datainnsamling med SMS 2
x per uke.
Status per 1. mars 2013: Annen omgang med intervensjon er i gang p alle
tre steder. Datainnsamlingen avsluttes i
tidsrommet 30. mai - 20. juni (avhengig av
sted).
Studien er enda ikke publisert.
Other relevant resources:
- Download copies of the Shoulder Symptom Modification
Procedure at www.LondonShoulderClinic.com
- Podcast: Prof Jeremy Lewis: Rotator cuff tendinopathies. BMJ
Group Podcasts
http://podcasts.bmj.com/bjsm/
- Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment?
British Journal of Sports Medicine. 2009;43(4):259-64.
http://bjsm.bmj.com/content/43/4/259.long
- Lewis JS. Rotator cuff tendinopathy: a model for the continuum of pathology and related management. British Journal of
Sports Medicine. 2010;44(13):918-23.
http://bjsm.bmj.com/content/44/13/918.full.pdf+html
- Lewis JS. Subacromial impingement syndrome: A musculoskeletal condition or a clinical illusion? Physical Therapy Review.
2011;16(5):388-98.
http://dx.doi.org/10.1179/1743288X11Y.0000000027.
Fysioterapeuten 9/13
47
S-ar putea să vă placă și
- Musculosketal Imaging in Physical TherapyDocument14 paginiMusculosketal Imaging in Physical TherapyWasemBhatÎncă nu există evaluări
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementDe la EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementÎncă nu există evaluări
- The Effects of Scapular Stabilization Based Exercise Therapy On PDFDocument15 paginiThe Effects of Scapular Stabilization Based Exercise Therapy On PDFElisabete SilvaÎncă nu există evaluări
- Balance and Vestibular Rehabilitation KitDocument9 paginiBalance and Vestibular Rehabilitation Kitmsnobody8Încă nu există evaluări
- Plug in GaitDocument70 paginiPlug in GaitJobin VargheseÎncă nu există evaluări
- Lab: Motor Pattern Assessment Screening & Diagnosis: Albert J Kozar DO, FAOASM, RMSKDocument72 paginiLab: Motor Pattern Assessment Screening & Diagnosis: Albert J Kozar DO, FAOASM, RMSKRukaphuongÎncă nu există evaluări
- PunctumFix Liebenson SundayLectureDocument17 paginiPunctumFix Liebenson SundayLecturepfi_jenÎncă nu există evaluări
- Mike ReinoldDocument20 paginiMike ReinoldVikas Kashnia0% (1)
- 6.motor AssessmentDocument32 pagini6.motor AssessmentSalman KhanÎncă nu există evaluări
- PRI Integration For Geriatrics - Complete FileDocument159 paginiPRI Integration For Geriatrics - Complete Filezhang yangÎncă nu există evaluări
- Kaltenborn Evjenth Concept of OMTDocument34 paginiKaltenborn Evjenth Concept of OMTJaan100% (1)
- 231a - Reconsidering The Way We Look at Movement-VCUDocument19 pagini231a - Reconsidering The Way We Look at Movement-VCUwolfgate0% (1)
- Module I - Lesson 3 - 4 - Metabolic - PPT NotesDocument14 paginiModule I - Lesson 3 - 4 - Metabolic - PPT NotesRobson ScozÎncă nu există evaluări
- Jurnal Frozen ShoulderDocument21 paginiJurnal Frozen ShoulderMega Mulya Dwi FitriyaniÎncă nu există evaluări
- Cervicovestibular Rehabilitation in Sport-Related Concussion - A Randomised Controlled TrialDocument7 paginiCervicovestibular Rehabilitation in Sport-Related Concussion - A Randomised Controlled TrialhilmikamelÎncă nu există evaluări
- Pre-Participation Screening: The Use of Fundamental Movements As An Assessment of Function - Part 2Document8 paginiPre-Participation Screening: The Use of Fundamental Movements As An Assessment of Function - Part 2gogo36Încă nu există evaluări
- Overhead Throwing: Biomechanics and PathologyDocument7 paginiOverhead Throwing: Biomechanics and Pathologyrapannika100% (1)
- A Kinetic Chain Approach For Shoulder RehabDocument9 paginiA Kinetic Chain Approach For Shoulder RehabRicardo QuezadaÎncă nu există evaluări
- Clinical Evaluation of Scapular DysfunctionDocument6 paginiClinical Evaluation of Scapular DysfunctionRudolfGerÎncă nu există evaluări
- Costa Rica GlucoseDocument91 paginiCosta Rica GlucoseAnthony HarderÎncă nu există evaluări
- Kinesiology by Carol OatisDocument2 paginiKinesiology by Carol OatisRakesh Kumar50% (2)
- NKT FlowChart - PDF Version 1 PDFDocument2 paginiNKT FlowChart - PDF Version 1 PDFJay SarkÎncă nu există evaluări
- Kinetic Chain Exercises - Open Versus ClosedDocument4 paginiKinetic Chain Exercises - Open Versus Closedamirreza jmÎncă nu există evaluări
- Measurement and EvaluationDocument21 paginiMeasurement and EvaluationIndah YulantariÎncă nu există evaluări
- PRI Integ For Pediatrics (Nov 2020) - Complete ManualDocument208 paginiPRI Integ For Pediatrics (Nov 2020) - Complete Manualzhang yangÎncă nu există evaluări
- Lumbopelvic Stability PresentationDocument64 paginiLumbopelvic Stability PresentationDeepi Gurung100% (1)
- Cohen 1992Document5 paginiCohen 1992Adriana Turdean VesaÎncă nu există evaluări
- The Shoulder: Theory & Practice: Jeremy LewisDocument3 paginiThe Shoulder: Theory & Practice: Jeremy Lewisparakram0% (1)
- How Could Periodization Help Enhance MuscleDocument9 paginiHow Could Periodization Help Enhance Musclemehrdad_44Încă nu există evaluări
- What Role Does Ethics Play in Sports - Resources - More - Focus Areas - Markkula Center For Applied Ethics - Santa Clara UniversityDocument4 paginiWhat Role Does Ethics Play in Sports - Resources - More - Focus Areas - Markkula Center For Applied Ethics - Santa Clara UniversityManish PrasadÎncă nu există evaluări
- Common Medical Terms, Abbreviations, and Acronyms Approved For Arizona WIC UseDocument7 paginiCommon Medical Terms, Abbreviations, and Acronyms Approved For Arizona WIC UseAsif Raza SoomroÎncă nu există evaluări
- The IFAST Assessment: Anterior Pelvic TiltDocument6 paginiThe IFAST Assessment: Anterior Pelvic Tiltjole000Încă nu există evaluări
- Phasic Activity of Intrinsic Muscles of The FootDocument14 paginiPhasic Activity of Intrinsic Muscles of The FootpetcudanielÎncă nu există evaluări
- The Effect of Stance On Muscle Activation in The SquatDocument5 paginiThe Effect of Stance On Muscle Activation in The Squatapi-320703111100% (1)
- 1 Reviews Evidences HandoutDocument25 pagini1 Reviews Evidences Handoutsefhilla putriÎncă nu există evaluări
- FUNHAB®: A Science-Based, Multimodal Approach For Musculoskeletal ConditionsDocument9 paginiFUNHAB®: A Science-Based, Multimodal Approach For Musculoskeletal ConditionsVizaÎncă nu există evaluări
- A Proposed Evidence-Based Shoulder Special Testing Examination Algorithm - Clinical Utility Based On A Systematic Review of The LiteratureDocument14 paginiA Proposed Evidence-Based Shoulder Special Testing Examination Algorithm - Clinical Utility Based On A Systematic Review of The LiteratureAfonso MacedoÎncă nu există evaluări
- Chapter 1: Basic Principles of Resistance Training andDocument12 paginiChapter 1: Basic Principles of Resistance Training andLuis Eduardo Barbosa Ortega100% (1)
- Access NPTE Review Lecture OutlineDocument12 paginiAccess NPTE Review Lecture OutlinecutlaborcostÎncă nu există evaluări
- Chondromalacia Patella RehabDocument1 paginăChondromalacia Patella Rehabjntownsend3404Încă nu există evaluări
- Ballistic StretchingDocument14 paginiBallistic Stretchingapi-351172625Încă nu există evaluări
- Transverse Rotation of The Segments of The Lower Extremity in LocomotionDocument15 paginiTransverse Rotation of The Segments of The Lower Extremity in Locomotionpetcudaniel100% (1)
- Motor Control The Heart of KinesiologyDocument13 paginiMotor Control The Heart of Kinesiologyferdinal dsakdskaÎncă nu există evaluări
- Reinold - Glenohumeral and Scapulothoracic RehabDocument45 paginiReinold - Glenohumeral and Scapulothoracic Rehabshivnair100% (2)
- Principles of Test SelectionDocument3 paginiPrinciples of Test SelectionALEX SNEHAÎncă nu există evaluări
- Whitley (2022) Periodisation of Eccentrically-Integrated Resistance Training During A National Rugby League Pre-SeasonDocument20 paginiWhitley (2022) Periodisation of Eccentrically-Integrated Resistance Training During A National Rugby League Pre-SeasonMiguel Lampre EzquerraÎncă nu există evaluări
- Effect of Exercise Training Intensity On Abdominal Visceral Fat andDocument19 paginiEffect of Exercise Training Intensity On Abdominal Visceral Fat andPepe EN LA LunaÎncă nu există evaluări
- Rehabilitation of Hamstring Strains: Phase I: Acute PhaseDocument3 paginiRehabilitation of Hamstring Strains: Phase I: Acute PhaseariyatiÎncă nu există evaluări
- Body PlanesDocument32 paginiBody PlanesStefanny Paramita EupenaÎncă nu există evaluări
- 52 Page PDF PF PPT Neurophysiological Effects of Spinal Manual Therapy in The Upper Extremity - ChuDocument52 pagini52 Page PDF PF PPT Neurophysiological Effects of Spinal Manual Therapy in The Upper Extremity - ChuDenise MathreÎncă nu există evaluări
- Kozar ScienceOfMotorControlLectureDocument114 paginiKozar ScienceOfMotorControlLectureMari PaoÎncă nu există evaluări
- A Framework For Exercise Prescription: DOI: 10.1097/TGR.0000000000000011Document23 paginiA Framework For Exercise Prescription: DOI: 10.1097/TGR.0000000000000011Lft Ediel PiñaÎncă nu există evaluări
- Kaltenborn 1993Document5 paginiKaltenborn 1993hari vijayÎncă nu există evaluări
- Pedia1 NewbornDocument300 paginiPedia1 NewbornNacel CelesteÎncă nu există evaluări
- Turocy StainCounterstrain LabPATS06ADocument53 paginiTurocy StainCounterstrain LabPATS06Awillone08Încă nu există evaluări
- PNFpresentationDocument32 paginiPNFpresentationNarkeesh ArumugamÎncă nu există evaluări
- Staged Approach For Rehabilitation ClassificationDocument10 paginiStaged Approach For Rehabilitation ClassificationCambriaChicoÎncă nu există evaluări
- Girls and Sport: Female Athlete Triad SimplifiedDe la EverandGirls and Sport: Female Athlete Triad SimplifiedÎncă nu există evaluări
- Original Article: Correspondence ToDocument9 paginiOriginal Article: Correspondence ToTomBramboÎncă nu există evaluări
- Overview of Blueberry Diseases: Dept. Plant, Soil, and Microbial Sciences Michigan State UniversityDocument51 paginiOverview of Blueberry Diseases: Dept. Plant, Soil, and Microbial Sciences Michigan State UniversityTomBramboÎncă nu există evaluări
- Chronic Pain ManagementDocument44 paginiChronic Pain ManagementTomBramboÎncă nu există evaluări
- Running and Osteoarthritis Does Recreational or Competitive Runn 2017Document1 paginăRunning and Osteoarthritis Does Recreational or Competitive Runn 2017TomBramboÎncă nu există evaluări
- Rotator Cuff Shoulder Pain DiagnosticDocument14 paginiRotator Cuff Shoulder Pain DiagnosticTomBramboÎncă nu există evaluări
- Posterior Shoulder Tightness: To Treat or Not To Treat?: ViewpointDocument4 paginiPosterior Shoulder Tightness: To Treat or Not To Treat?: ViewpointTomBramboÎncă nu există evaluări
- Basic Routine InfographicDocument1 paginăBasic Routine Infographicariraphiel100% (2)
- Growing Blueberries PDFDocument8 paginiGrowing Blueberries PDFOlivera PetrovicÎncă nu există evaluări
- Blueberry Varieties For MichiganDocument6 paginiBlueberry Varieties For MichiganTomBramboÎncă nu există evaluări
- Dominion Temne CasyDocument5 paginiDominion Temne CasyTomBramboÎncă nu există evaluări
- A Specific Exercise Program and Modification of Postural Alignment For Treating of CHDocument13 paginiA Specific Exercise Program and Modification of Postural Alignment For Treating of CHTomBramboÎncă nu există evaluări
- Influence of Scapular Position On Cervical ROMDocument6 paginiInfluence of Scapular Position On Cervical ROMTomBramboÎncă nu există evaluări
- Yellow Flags-Psychological IndicatorsDocument1 paginăYellow Flags-Psychological IndicatorsTomBramboÎncă nu există evaluări
- Effect of Manual Therapy and Neurodynamic Techniques VsDocument10 paginiEffect of Manual Therapy and Neurodynamic Techniques VsTomBramboÎncă nu există evaluări
- Treatment Manual and Therapy Map Greg Lehman Feb 2015Document26 paginiTreatment Manual and Therapy Map Greg Lehman Feb 2015TomBramboÎncă nu există evaluări
- Applying Modern Pain Neuroscience in Clinical - 2014Document12 paginiApplying Modern Pain Neuroscience in Clinical - 2014Juci FreitasÎncă nu există evaluări
- Effects of Isometric, Eccentric, or Heavy Slow Resistance Exercises On Pain and Function With PTDocument15 paginiEffects of Isometric, Eccentric, or Heavy Slow Resistance Exercises On Pain and Function With PTTomBramboÎncă nu există evaluări
- Specific Exercise Program For Impingement RMDocument2 paginiSpecific Exercise Program For Impingement RMTomBramboÎncă nu există evaluări
- Treatment Manual and Therapy Map Greg Lehman Feb 2015Document26 paginiTreatment Manual and Therapy Map Greg Lehman Feb 2015TomBramboÎncă nu există evaluări
- Influence of Scapular Position On Cervical ROMDocument6 paginiInfluence of Scapular Position On Cervical ROMTomBramboÎncă nu există evaluări
- Shoulder Derangement With An Underlying DysfunctionDocument28 paginiShoulder Derangement With An Underlying DysfunctionTomBramboÎncă nu există evaluări
- Evaluation The Patient Using MDTDocument34 paginiEvaluation The Patient Using MDTTomBramboÎncă nu există evaluări
- Postural Exercises On The Foam RollDocument3 paginiPostural Exercises On The Foam RollTomBrambo100% (1)
- Peripheral Mobilisation S With MovementDocument9 paginiPeripheral Mobilisation S With MovementTomBramboÎncă nu există evaluări
- Core Engaged Leg RaiseDocument1 paginăCore Engaged Leg RaiseTomBramboÎncă nu există evaluări
- Theoaknee MDTDocument67 paginiTheoaknee MDTTomBramboÎncă nu există evaluări
- Toe Touch ProgressionDocument1 paginăToe Touch ProgressionTomBramboÎncă nu există evaluări
- Straight Leg TDocument1 paginăStraight Leg TTomBramboÎncă nu există evaluări
- Toe Touch ProgressionDocument1 paginăToe Touch ProgressionTomBramboÎncă nu există evaluări
- Wall SitDocument1 paginăWall SitTomBramboÎncă nu există evaluări
- Lecture 4Document79 paginiLecture 4alaa emadÎncă nu există evaluări
- Cholera Outbreaks in Sub Saharan AfricaDocument7 paginiCholera Outbreaks in Sub Saharan AfricaMamadou CoulibalyÎncă nu există evaluări
- (Doi 10.1043 - 0003-3219 (2006) 076 (0388 - VOPRFM) 2.0.CO 2)Document6 pagini(Doi 10.1043 - 0003-3219 (2006) 076 (0388 - VOPRFM) 2.0.CO 2)Bulfendri DoniÎncă nu există evaluări
- Critical AppraisalDocument47 paginiCritical AppraisalNaman KhalidÎncă nu există evaluări
- 1b Static & Dynamic Characteristics&Loading Effect PDFDocument45 pagini1b Static & Dynamic Characteristics&Loading Effect PDFvishnuÎncă nu există evaluări
- Diagnostic Value of Gastric Shake Test For Hyaline Membrane Disease in Preterm InfantDocument6 paginiDiagnostic Value of Gastric Shake Test For Hyaline Membrane Disease in Preterm InfantNovia KurniantiÎncă nu există evaluări
- PSA Level and Gleason Score in Predicting The Stage of Newly Diagnosed Prostat CancerDocument6 paginiPSA Level and Gleason Score in Predicting The Stage of Newly Diagnosed Prostat CancergumÎncă nu există evaluări
- The Model and Empirical Research of Application Scoring Based On Data Mining MethodsDocument8 paginiThe Model and Empirical Research of Application Scoring Based On Data Mining MethodsGuilherme Miguel TavaresÎncă nu există evaluări
- Sensitivity and SpecificityDocument3 paginiSensitivity and SpecificityPrisia AnantamaÎncă nu există evaluări
- Chap 012Document84 paginiChap 012Noushin Khan0% (2)
- Salmo 6579Document7 paginiSalmo 6579DiegoÎncă nu există evaluări
- Saple Sze CCDocument14 paginiSaple Sze CCPeterÎncă nu există evaluări
- Applied Geochemistry: Mouigni Baraka Nafouanti, Junxia Li, Nasiru Abba Mustapha, Placide Uwamungu, Dalal AL-AlimiDocument8 paginiApplied Geochemistry: Mouigni Baraka Nafouanti, Junxia Li, Nasiru Abba Mustapha, Placide Uwamungu, Dalal AL-Alimik.ayushearth28Încă nu există evaluări
- Bio-Stats Step 3Document9 paginiBio-Stats Step 3S100% (4)
- Prosper 444 PDFDocument27 paginiProsper 444 PDFaliÎncă nu există evaluări
- 1 s2.0 S1368837518304299 MainDocument8 pagini1 s2.0 S1368837518304299 MainIgor VainerÎncă nu există evaluări
- New Scoring System APACHE HF For PredictDocument9 paginiNew Scoring System APACHE HF For PredictAdi PriyatnaÎncă nu există evaluări
- CHN QuestionsDocument13 paginiCHN QuestionsKristine CastilloÎncă nu există evaluări
- All Common ChecklistDocument66 paginiAll Common Checklistyousrazeidan1979Încă nu există evaluări
- Hemix: Technical SpecificationsDocument3 paginiHemix: Technical SpecificationsNia AmbarwatiÎncă nu există evaluări
- 2010 Article 1133Document15 pagini2010 Article 1133Asmaa ElarabyÎncă nu există evaluări
- Project Plagiarism Report (Before Removing)Document21 paginiProject Plagiarism Report (Before Removing)Shyam Raj SivakumarÎncă nu există evaluări
- International Journal of Scientific and Statistical Computing (IJSSC) Volume (1) IssueDocument18 paginiInternational Journal of Scientific and Statistical Computing (IJSSC) Volume (1) IssueAI Coordinator - CSC JournalsÎncă nu există evaluări
- (TNHS) : Summary and ExplanationDocument12 pagini(TNHS) : Summary and Explanationcass100% (2)
- Webster BioinstrumentationDocument394 paginiWebster BioinstrumentationMaria Jose GardeaÎncă nu există evaluări
- Lecture Notes - Logistic RegressionDocument11 paginiLecture Notes - Logistic RegressionPrathap BalachandraÎncă nu există evaluări
- Basic and Clinical Biostatistics, 5th EditionDocument368 paginiBasic and Clinical Biostatistics, 5th Editionmp4Încă nu există evaluări
- A Clinical Scoring System For Pediatric Hand - Foot-Mouth DiseaseDocument8 paginiA Clinical Scoring System For Pediatric Hand - Foot-Mouth DiseaseclaudyÎncă nu există evaluări
- TDX Oli DMR PS 4105Document3 paginiTDX Oli DMR PS 4105Ethan LynnÎncă nu există evaluări
- Seratec Hemdirect Hemoglobin Assay: Intended Use Description of The TestDocument2 paginiSeratec Hemdirect Hemoglobin Assay: Intended Use Description of The Testfabiola_magdalenoÎncă nu există evaluări