Documente Academic
Documente Profesional
Documente Cultură
Efficacy and Safety Profile of Antibiotic Prophylaxis Usage in Clean and Clean-Contaminated Plastic and Reconstructive Surgery
Încărcat de
RmeMreErmDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Efficacy and Safety Profile of Antibiotic Prophylaxis Usage in Clean and Clean-Contaminated Plastic and Reconstructive Surgery
Încărcat de
RmeMreErmDrepturi de autor:
Formate disponibile
REVIEW ARTICLE
Efficacy and Safety Profile of Antibiotic Prophylaxis
Usage in Clean and Clean-Contaminated Plastic
and Reconstructive Surgery
A Meta-Analysis of Randomized Controlled Trials
Yi Zhang, MD, Jiasheng Dong, MD, Yufei Qiao, MD, Jinguang He, MD, Tao Wang, MD,
and Sunxiang Ma, MD
Background: There is no consensus with regard to antibiotic prophylaxis
usage in clean and clean-contaminated plastic and reconstructive surgery. This
meta-analysis sought to assess the efficacy and safety of antibiotic prophylaxis
and to determine appropriate duration of prophylaxis.
Methods: An English language literature search was conducted using PubMed
and the Cochrane Collaboration for randomized controlled trials (RCTs) that
evaluate the use of antibiotic prophylaxis to prevent postoperative surgical site
infection (SSI) in patients undergoing clean and clean-contaminated plastic and
reconstructive surgery. Data from intention-to-treat analyses were used where
available. For the dichotomous data, results for each study were odds ratio (OR)
with 95% confidence interval (CI) and combined for meta-analysis using the
Mantel-Haenszel method or the DerSimonian and Laird method. Study quality
was critically appraised by 2 reviewers using established criteria. STATA version
12 was used for meta-analyses.
Results: Twelve RCTs involving 2395 patients were included, of which 8 trials were considered to be of high methodological quality. Effect of antibiotic
prophylaxis in plastic and reconstructive surgery was found favorable over
placebo in SSI prevention (13 studies; 2449 participants; OR, 0.53; 95% CI,
0.4Y0.7; P G 0.01) and the other wound complication (OWC) prevention
(9 studies; 1843 participants; OR, 0.36; 95% CI, 0.15Y0.84; P G 0.02). Subgroup analysis performed according to surgical wound type or the duration of
prophylaxis did not modify the results except for the OWC with short-term
antibiotic treatment. Compared with short-term antibiotic prophylaxis, longterm administration showed no evidence of a difference in risk of SSI
(7 studies; 1012 participants; OR, 0.99; 95% CI, 0.63Y1.55; P G 0.95), OWC
(5 studies; 824 participants; OR, 0.92; 95% CI, 0.46Y1.86; P G 0.82), and
adverse event relative to antibiotic administration (3 studies; 653 participants;
OR, 0.23; 95% CI, 0.01Y4.92; P G 0.35).
Conclusions: This meta-analysis of RCTs provides evidence supporting that
antibiotic prophylaxis reduced postoperative SSI in clean plastic surgeries
with high-risk factors and clean-contaminated plastic surgeries. Besides, a
short-course administration regimen seemed to be of adequate efficacy and
safety. High-quality prospective trials on larger scale are needed to further
confirm these findings.
Key Words: antibiotic prophylaxis, surgical site infection, plastic surgery,
meta-analysis
(Ann Plast Surg 2014;72: 121Y130)
Received June 2, 2013, and accepted for publication, after revision, August 26, 2013.
From the Shanghai Ninth Peoples Hospital affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China.
Conflicts of interest and sources of funding: none declared
Reprints: Jiasheng Dong, MD, Department of Plastic and Reconstructive Surgery,
Shanghai Ninth Peoples Hospital affiliated to Shanghai Jiao Tong University
School of Medicine, No. 639 Zhizhaoju Rd, Shanghai 200011, China. E-mail:
dongjiasheng_9y@163.com.
Copyright * 2013 by Lippincott Williams & Wilkins
ISSN: 0148-7043/14/7201-0121
DOI: 10.1097/01.SAP.0000440955.93769.8c
Annals of Plastic Surgery
& Volume 72, Number 1, January 2014
ccording to classification of the National Nosocomial Infections
Surveillance System recommended by the American Society of
Health-System Pharmacist, most of elective plastic surgeries can
generally be defined as clean or clean-contaminated.1Y2 Despite
the low risk of incidence, postoperative surgical site infection (SSI)
was still the most frequent complication in plastic and reconstructive
surgeries, which could lead to delayed wound healing, extended
hospital stay, and a considerable financial burden for patients. The
reported incidence of SSI after plastic surgeries varies in literature
from 0% to 32.6%.3Y6
Antibiotic prophylaxis is the administration of antimicrobial
agents before bacterial contamination to prevent undesirable infectious complications by lowering the bacterial burden. In the past few
decades, prophylactic antibiotics have been widely prescribed by
most plastic and reconstructive surgeons with varying administration
route, regimen, and duration, most of which were generally based on
personal preference or institutional tradition for the absence of a
specific guideline supported by scientific evidence, and its efficacy
on the prevention of postoperative complication remains unclear and
controversial.5,7Y9
This meta-analysis was conducted with available published valid
randomized controlled trial (RCT) evidence to address whether a difference in the risk of SSI exists between cases with and without antibiotic prophylaxis, and between short-term and long-term prophylaxis
among patients undergoing clean and clean-contaminated plastic and
reconstructive surgeries. Risk of other surgical wound complication
(including wound bleeding, wound rapture, bleeding hematomas,
wound necrosis, and delayed wound healing) and adverse events relative to antibiotics (including nausea, vomiting, diarrhea, rashes, and
pruritus) were evaluated in the analysis as the second and the third
outcomes.
METHODS
Literature Search
Literature on the effectiveness of prophylactic antibiotics in
patients undergoing clean and clean-contaminated plastic and reconstructive surgery were identified and selected. PubMed and
the Cochrane Central Register of Controlled Trials in The Cochrane
Library were searched for all publications up to January 2013 using
the following medical subject headings terms: (plastic surgery or
reconstructive surgery or reconstruction) AND (antibiotics or
antimicrobial) OR (infection or SSI). Reference lists of relevant studies were searched for other potentially appropriate publications. Literature reviews, single-case reports, letters, comments,
animal studies, and publications in languages other than English were
excluded.
Inclusion Criteria
The eligibility criteria for a study to be included in the analysis
are delineated in Table 1.
www.annalsplasticsurgery.com
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
121
Annals of Plastic Surgery
Zhang et al
Data Extraction
Data extracted from each trial referred to the name of the first
author, year of publication, location of the study, intention-to-treat
population, sex distribution, mean age, wound types, antibiotic regimen (type, dosage, and duration), duration of follow-up, and data regarding the effectiveness and safety of compared treatments. In trials
with more than 1 intervention arm, each comparison of 2 arms was
considered a single study.
Assessment of Methodological Quality
Two independent authors assessed the methodological quality
of each study included in the present meta-analysis using the Jadad
scale by methods of random allocation (up to 2 points), blinding (up to
2 points), and patient withdrawals (up to 1 point).10 Points were added
from each component, and the total can range from weak (0) to strong
(5). High quality was defined as a Jadad score more than 3.11
Statistical Methods
The statistical analysis was performed using STATA version 12
software (Stata Corp, College Station, Tex). The heterogeneity was
tested with the W2-based Cochran statistic and the inconsistency index
(I2).12 Statistically significant heterogeneity was considered present
with Pheterogeneity G 0.05 or I2 9 50%.13 In the presence of substantial
heterogeneity, a random-effects model (REM) was adopted as the
pooling method as opposed to a fixed-effects model (FEM).14 Odds
ratios (ORs) were calculated separately for each main outcome with
either the Mantel-Haenszel test in FEM or the DerSimonian and Laird
test in REM. Statistical significance was indicated by P value of less
than 0.05. Forest plots were produced, from which the OR with 95%
confidence interval (CI) and P value were reported. Funnel plots, Egger
regression test, and Begg rank correlation test were used to assess
publication bias.15,16
Subgroup Analysis and Sensitivity Analysis
Subgroup analysis for antibiotic prophylaxis efficacy was
performed (when at least 2 studies included the considered outcome) according to the surgical wound classification (clean vs
clean-contaminated), and the duration of antibiotic administration
(long-term vs short-term). Sensitivity analyses were performed by excluding any trials of the included studies and the P value of the
rest studies was estimated.
RESULTS
A f lowchart of the selection process is shown in Figure 1.
From the total 1097 articles identified in the initial search, 262 articles
were found to be potentially relevant, out of which full texts of 56 articles were reviewed. Twelve RCTs met the inclusion criteria. Among
TABLE 1. Eligibility Criteria for the Inclusion in the
Meta-analysis
1. RCT
2. Reported at least 1 clinical end point
3. Compared prophylactic antibiotic treatment with treatment of longer or
shorter duration, or placebo treatment
4. Short-term treatment was defined as antibiotics administered intravenously
within 2 d or orally within 3 d
5. Long-term antibiotic treatment was at least 2 d longer than the
corresponding short-term treatment
6. The surgical procedure was limited to clean and clean-contaminated
122
www.annalsplasticsurgery.com
& Volume 72, Number 1, January 2014
these trials, four 3-arm RCTs evaluated antibiotic group (long-term
and short-term) versus placebo group, five 2-arm RCTs evaluated
short-term antibiotic group versus placebo group, and three 2-arm
RCTs compared the effect between long-term prophylaxis and
short-term prophylaxis. No publication bias was observed for the
outcomes using funnel plots (Supplemental Digital Content 1Y2,
http://links.lww.com/SPA/A83).
Characteristics and Quality Assessment of RCTs
The included RCTs were published between 1994 and 2012,
and comprised a total of 3495 patients in the pooled data, of whom
1882 received antibiotic prophylaxis (1389 long-term; 493 shortterm). Among them, 1100 patients from the study of Baran et al17
were not included in the analysis because they had undergone a
contaminated surgical procedure rather than a clean or cleancontaminated operation, or the surgical wound type was unknown.
The methodological features and outcomes measured in the included
studies were presented in Tables 2 and 3; 8 of 12 of the RCTs were
considered to be of high methodological quality according to the
Jadad score (Table 4).
Antibiotic Versus Placebo
Surgical Site Infection
The incidence of postoperative SSI was reported as the primary outcome in all selected trials. The heterogeneity analysis did
not reach statistical significance neither for the overall analysis nor
for the subgroup analysis, so a FEM was used. Pooled analysis of the
9 included RCTs showed a 47% decrease in the risk of developing
SSI after prophylactic administration of antibiotics compared with
placebo groups (13 studies; 2449 participants; OR, 0.53; 95% CI,
0.4Y0.7; P G 0.01) (Fig. 2). Favorable effect was still observed in both
short-term and long-term antibiotic subgroup analysis (short-term,
9 studies; 1724 participants; OR, 0.50; 95% CI, 0.35Y0.7; P G 0.01;
long-term, 4 studies; 587 participants; OR, 0.59; 95%CI, 0.37Y0.94;
P G 0.03) (Fig. 2), and both clean and clean-contaminated operations
(clean operations, 4 studies; 404 participants; OR, 0.35; 95% CI,
0.21Y0.61; P G 0.01; clean-contaminated operations, 5 studies; 1282
participants; OR, 0.63; 95% CI, 0.42Y0.94; P G 0.02) (Fig. 3). In the
sensitivity analysis, exclusion of any comparison did not change the
overall efficacy of antibiotic prophylaxis and the efficacy of shortterm antibiotic prophylaxis. However, the effect with long-term
antibiotic regimen failed to reach statistical significance with the
exclusion of studies by Lilja et al.18
Other Wound Complication
Rates of surgical wound complication other than SSI or
wound infection, documented as wound bleeding, wound rapture,
bleeding hematomas, wound necrosis, and delayed wound healing,
were determined and combined. The heterogeneity analysis reached
statistical significance for both the overall analysis and the subgroup
analysis, so a REM was used. Analysis of the data from 6 included
RCTs showed a 64% decrease in the risk of developing other wound
complication (OWC) with antibiotic prophylaxis compared with
placebo groups (9 studies; 1843 participants; OR, 0.36; 95% CI,
0.15Y0.84; P G 0.01) (Fig. 4). Subgroup analysis revealed significant
decrease in patients with long-term prophylaxis (3 studies; 587 participants; OR, 0.22; 95% CI, 0.05Y0.91; P G 0.04), but no significant
effect with short-term prophylaxis (6 studies; 1256 participants; OR,
0.44; 95% CI, 0.15Y1.28; P G 0.13) (Fig. 4). In the sensitivity analysis, the effect of overall antibiotic prophylaxis presented marginal
statistical significance (P G 0.06) with the exclusion of study by
Ahmadi et al.19 And the effect with long-term antibiotic regimen
* 2013 Lippincott Williams & Wilkins
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Annals of Plastic Surgery
& Volume 72, Number 1, January 2014
Meta-analysis of Antibiotic Prophylaxis for PRS
failed to reach statistical significance with the exclusion of studies by
Ahmadi et al19 and Whittaker et al.20
0.46Y1.86; P G 0.82) (Fig. 5). Exclusion of any of the comparisons
did not change the result.
Long-term versus Short-term
Adverse Event
Adverse events potentially associated with the antibiotic administration were assessed by 3 RCTs, but events took place only in 2
studies. Heterogeneity existed among included studies and analysis
with REM was performed. The estimation did not significantly favor
either of the 2 intervention arms (3 studies; 653 participants; OR,
0.23; 95% CI, 0.01Y4.92; P G 0.35) (Fig. 5). The sensitivity analysis
excluding the study by Ricci and DAscanio21 showed statistically
significant decrease with the patients with short-term regimen.
Surgical Site Infection
The incidence rate of SSI was reported by 7 studies. The
heterogeneity analysis did not reach statistical significance, and
analysis with FEM was performed. Pooled analysis of the 7 included
RCTs did not favor either of the 2 treatment groups in SSI (7 studies;
1012 participants; OR, 0.99; 95% CI, 0.63Y1.55; P G 0.95) (Fig. 5).
Exclusion of any of the comparisons did not change the result.
Other Wound Complication
The incidence rate of OWC was reported in 5 studies. The
heterogeneity analysis did not reach statistical significance, and
analysis with FEM was performed. No advantage of either treatment
group was shown (5 studies; 824 participants; OR, 0.92; 95% CI,
DISCUSSION
Patients undergo plastic and reconstructive surgeries for both
therapeutic and cosmetic reasons. Although the risk of postoperative
FIGURE 1. Flowchart of the selection process.
* 2013 Lippincott Williams & Wilkins
www.annalsplasticsurgery.com
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
123
124
Country
www.annalsplasticsurgery.com
Italy
UK
Ricci 2012
Whittaker 2005
NA
46/28
417/213
22
39
100
NA
61.6
33
36.6
41
69
NA
NA
NA
NA
37
32
Mean
Age, y
Cle-Con
Cle-Con
Cle-Con
Cle and Cle-Con
Cle-Con
Cle-Con
Cle and Cle-Con
Clean
Cle-Con
Cle-Con
Clean
Clean
Wound
Type
Cefotaxime sodium for 24 h
IV clindamycin, 900 mg q 8 h, 3 doses
IV amoxicillin-clavulanate, 2.2 g once
Cephalosporin
(allergy: vancomycin)
for 24Y48 h
PO azithromycin, 1 g
(adults/children over 45 kg)/800 mg
(children 36Y45 kg)/600 mg
(children 26Y35 kg)/400 mg
(children 15Y25 kg) once
IV sulbactam-ampicillin, 2 g once
IV cefuroxime, 1.5 g once
PO azithromycin, 500 mg qd, 3 d
IV flucloxacillin,
1.0 g once
IV cephalosporin,
1 g once preoperatively
(IV levofloxacin, 500 mg
once for cephalosporin allergy)
IV cefazolin, 1.0 g once
IV cefazolin,
1 g once preoperatively
(IV levofloxacin,
500 mg once for
cephalosporin allergy)
ShortYTerm Antibiotics
(Type, Dosage, Duration)
Cefotaxime sodium for 5 d
IV clindamycin, 900 mg q 8 h, 15 doses
IV amoxicillin-clavulanate, 2.2 g once followed
by oral amoxicillin-clavulanate, 1 g bid, 7 d
None
None
None
None
None
IV cefazolin, 1 g once preoperatively
followed by postoperative IV cefazolin,
1 g q 8 h, 2 doses; and then oral cephalexin,
500 mg qd, 3 d (IV levofloxacin, 500 mg
once preoperatively followed by
postoperative oral levofloxacin,
500 mg qd, 3 d, for cephalosporin allergy)
IV cephalosporin, 1 g once preoperatively
(IV levofloxacin, 500 mg once for
cephalosporin allergy) followed by
postoperative levofloxacin, 500 mg qd, 3 d
IV cefazolin, 1.0 g once followed
by oral amoxicillin, 1 g q 12 h, 7 d
IV flucloxacillin, 1.0 g once followed
by oral flucloxacillin, 1 g qd, 7 d
LongYTerm Antibiotics
(Type, Dosage, Duration)
NA
1 wk
4 wk
11Y12 d
4 wk
2 wk
4 wk
NA
4 wk
2 wk
6 wk
NA
Duration of
Follow-Up
Annals of Plastic Surgery
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Cle-Con indicates clean-contaminated; F, female; ITT, intention-to-treat; L, long-term; M, male; NA, data not available; P: placebo; S: short-term.
NA
148/40
18/12
168/171
168/171
129/28
417/213
129/28
None
None
None
None
46
181
69
Baran 1999
Turkey
150 150
Lilja 2011
Finland
100 100
Kuijpers 2006
Netherlands
14
16
Short-term antibiotics vs long-term antibiotics
Bhathena 1998
India
None
28
Carroll 2003
United States None
35
Rajan 2005
Australia
None 100
168
47
56
197
69
None
Norway
59
55
252
69
NA
Sex
(M/F)
171
Amland 1995
Placebo vs short-term antibiotics
Serletti 1994
United States
Turkey
Asuman 2007
Placebo vs short-term antibiotics vs long-term antibiotics
Ahmadi 2005
United States
17
17
16
First Author
and Year
ITT Population
TABLE 2. Details of the RCTs Included in the Meta-Analysis
Zhang et al
& Volume 72, Number 1, January 2014
* 2013 Lippincott Williams & Wilkins
Outcomes
P
S
SSIs
* 2013 Lippincott Williams & Wilkins
14/17
NA
6/69
4/36
NA
4/34
OWCs
Wound infection; death; flap
necrosis; other infection;
fistula; adverse effect
Wound infection; adverse effect
None
None
0/100
4/35
2/28
L indicates long-term; NA, data not available; P, placebo; S: short-term.
Rajan 2005
Carroll 2003
None
3/100
4/39
2/22
None
None
None
NA
NA
NA
NA
NA
NA
NA
NA
None
None
None
None
None
NA
NA
None
None
None
NA
3/46
NA
NA
NA
NA
1/181
NA
9/36
Conclusion
0/39
NA
None
None
None
None
None
There is no beneficial effect rom administration of antibiotics for more
than 24 h postoperatively in patients undergoing major flap
reconstruction for head and neck cancel.
Short-course clindamycin is as effective as long-course in SSI
prevention in free flap reconstruction of head and neck.
The use of prophylactic antibiotics in reduction mamoplastic is not
efficacious in reducing the rate of wound infection or delayed healing.
There is a significant reduction in postoperative complication and in
additional use of antibiotics postoperatively in prophylaxis group.
Antibiotic prophylaxis is not necessary for plastic surgeries.
A single dose of intravenous cefuroxime before septoplasty is
recommended in patients having crusts or purulent secretion in the
nasal cavities or if the operation is expected to be prolonged.
Systemic antibiotics with an accurate bacterial spectrum should be
advised in full-thickness skin graft reconstruction after surgery for
nonmelanoma skin cancer of the nose.
2/100 29/100 A single dose of antibiotics administered preoperatively is sufficient
for prophylaxis of postoperative infections in septorhinoplasty.
0/35
NA
NA
NA
0/100
4/168
NA
NA
No favorable effect of antibiotic prophylaxis was found in SSI
prevention in reduction mammaplasty.
NA
NA A single preoperative dose of intravenous antibiotics is sufficient
to prevent postoperative infections in abdominoplasty.
23/197 22/181 Septal surgery with early removal of nasal packing does not require
routine antibiotic prophylaxis because of the low infection risk.
NA
NA No significant difference exists among the 3 groups with clean incised
hand injures.
NA
Adverse Events
& Volume 72, Number 1, January 2014
Short-term antibiotics vs long-term antibiotics
Bhathena 1998 Wound infection
Wound infection; wound
35/252 23/197 19/181 1/252 0/197
bleeding; adverse effect
Whittaker 2005 All wound problems;
8/55
7/56
2/46 11/55
8/56
wound infection
Placebo group vs short-term antibiotics
Serletti 1994
Wound infection; delayed
4/59
4/47
None 19/59 12/47
wound healing
Amland 1995
Wound infection; hematomas;
32/168 8/171 None
8/168 3/171
wound rupture; adverse effect
Baran 1999
Wound infection
3/150 2/150 None
NA
NA
Lilja 2011
Wound infection; wound
8/100 2/100 None
1/100 4/100
bleeding; wound hematomas;
allergic reaction
Kuijpers 2006 Wound infection;
0/14
0/16
None
NA
NA
graft survive rate
Ricci 2012
Placebo group vs short-term antibiotics vs long-term antibiotics
Ahmadi 2005
Wound infection; delayed
5/17
3/34
wound healing
Asuman 2007 Wound infection
9/69
3/69
First Author
and Year
TABLE 3. Outcomes and Conclusion of the RCTs Included in the Meta-analysis
Annals of Plastic Surgery
Meta-analysis of Antibiotic Prophylaxis for PRS
www.annalsplasticsurgery.com
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
125
Annals of Plastic Surgery
Zhang et al
& Volume 72, Number 1, January 2014
TABLE 4. Jadad Score of the Included RCTs
First Author
and Year
Ahmadi 2005
Amland 1995
Asuman 2007
Baran 1999
Bhathena 1998
Carroll 2003
Ricci 2012
Lilja 2011
Kuijpers 2006
Rajan 2005
Serletti 1994
Whittaker 2005
Randomization
Randomization
Described
Double
Blind
Method of Blinding
Described
Description of
Withdrawal + Dropouts
JADAD
Score
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
0
0
1
1
1
0
1
0
1
0
1
0
0
0
1
1
1
0
1
0
1
0
1
0
0
0
1
0
1
0
0
0
1
1
1
1
1
0
0
0
1
0
1
1
1
3
5
3
2
1
4
3
5
1
4
2
5
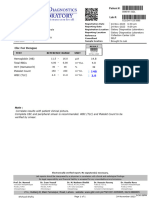
FIGURE 2. Pooled OR for the overall SSI incidence with prophylactic antibiotics (long-term and short-term) compared to placebo.
The diamond denotes the fixed-effects pooled OR and 95% CI. The dashed line is drawn at the overall pooled estimate.
*Comparison of short-term arm and placebo in trials with more than 1 intervention arm; **comparison of long-term arm and
placebo in trials with more than 1 intervention arm.
126
www.annalsplasticsurgery.com
* 2013 Lippincott Williams & Wilkins
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Annals of Plastic Surgery
& Volume 72, Number 1, January 2014
Meta-analysis of Antibiotic Prophylaxis for PRS
FIGURE 3. Pooled OR for SSI incidence after clean and clean-contaminated plastic and reconstructive surgeries with prophylactic
antibiotics compared to placebo. Size of the solid squares is inversely proportional to the variance of the study estimate. The
diamond denotes the fixed-effects pooled OR and 95% CI. Cle-Con indicates clean-contaminated.
infection is low, SSI will severely compromise therapeutic results,
facilitating OWCs, leading to significant discomfort and inconvenience for patients.22,23 On the other hand, inappropriate administration of prophylactic antibiotics will also cause iatrogenic
complications such as allergic reaction, thrombophlebitis, and the
risk of selecting resistant strains among hospital f lora.2 Therefore,
a better understanding of antibiotic prophylaxis will by all means
help plastic surgeons and benefit both aesthetic and functional
outcomes for patients.
In this meta-analysis, which identified as eligible for inclusion
only RCT performed in patients undergoing plastic surgeries, significant reduction of postoperative SSI as well as OWC rates were
shown with the prophylactic antibiotic treatment. In the subgroup
analysis, the most results still preferred the treatment group when
analyzed according to the duration of antibiotic administration (longterm vs short-term) and the surgical wound classification (clean vs
clean-contaminated).
The SSI incidence rate of plastic surgery varies according to
the operation performed and the presence of specific risk factors.3
Generally, clean-contaminated surgery is considered with higher risk
of infection and less debate on prophylactic antibiotic usage.18,24 In
the field of clean plastic surgery, antibiotic prophylaxis remains a
* 2013 Lippincott Williams & Wilkins
controversial subject and was not routinely recommended.9,25Y27 In
the present study, the total SSI rate of the clean plastic operations was
11.6%, much higher than was generally anticipated for clean surgery.2 The increased infection rate might be associated with the
spectrum of operations involved, most (85%) of which in our study
were characterized with large surgical incision and long procedure
duration such as breast reduction and abdominoplasty. Prolonged
procedure length (92 h), complicated anatomy of involved area, and
the surgical technique adopted had been identified as independent
risk factors magnifying SSI risk of clean operation, and should be
taken into consideration when antibiotic is administrated.3,28,29 Unfortunately, there were insufficient data available for these variables
to achieve a summated outcome in this analysis. Further high-quality
work of large scale with sufficient relative details documented is
expected.
Another subject of controversy is the optimal duration of antibiotic administration. Consistent with previous studies,30Y32
noninferiority of short-term prophylaxis was demonstrated compared
with long-term prophylaxis on postoperative SSI and OWCs in our
analysis. Ideally, short-term antibiotic prophylaxes are preferred to
longer-course regimen in reduction of hospitalization costs, drug
toxicity, and the emergence of resistant pathogens, especially in clean
www.annalsplasticsurgery.com
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
127
Annals of Plastic Surgery
Zhang et al
& Volume 72, Number 1, January 2014
FIGURE 4. Pooled OR for the overall incidence of wound complications except for SSI with prophylactic antibiotics (long-term
and short-term) compared to placebo. The diamond denotes the random-effects pooled OR and 95% CI. The dashed line is
drawn at the overall pooled estimate. *Comparison of short-term arm and placebo in trials with more than 1 intervention arm;
**comparison of long-term arm and placebo in trials with more than 1 intervention arm.
surgeries. Evidence of antibacterial activity with short-term regimen
had been reported by trials on clean operations of hernia, breast, and
varicose vein.33Y35 Gil-Ascencio et al36 advocated that a single-dose
intravenous first-generation cephalosporin was of adequate efficacy
to prevent SSI in clean-contaminated outpatient operations of short
duration. For inpatient surgeries, Thomas et al37 advocated that antibiotic prophylaxis could be achieved with long-acting antimicrobial
agents (like third-generation cephalosporins) even in a short-course
regimen. In terms of adverse events relative to antibiotics, no difference was found between long-term and short-term antibiotic regimens, which, however, should be interpreted with caution as they
might be due to the smaller number of studies (only 2) and lack of
power rather than a real lack of difference.
In conclusion, the results of this meta-analysis implied that antibiotic prophylaxis reduced postoperative SSI in clean plastic surgeries
with potential risk factors (prolonged procedure length, complicated
anatomy of involved area, and specific surgical technique adopted) and
clean-contaminated plastic surgeries. In addition, between long-term
and short-term prophylaxis, the analysis of the available data does not
show superiority of either regimen in prevention of SSI, OWC, or
128
www.annalsplasticsurgery.com
adverse events. Considering the hospitalization costs and adverse effects arising with antibiotic treatments, we recommend that a short-term
antibiotic regimen be of adequate efficacy and safety for clean plastic
surgeries and most clean-contaminated surgeries. The findings of this
study should not be interpreted without the consideration of potential
limitations. As previously documented, factors like patient-related risk,
operation type, surgical technique, surgical wound classification, antibiotic type, timing, and duration of antibiotic administration may
function as source of heterogeneity.38Y42 In this study, we only separately analyzed influence of surgical wound classification and duration
of antibiotics. Due to limitation of the number of studies and lack of
original data, we were not able to carry out subgroup analysis according
to the rest factors, and so the chance of possible performance bias might
be higher.43 Besides, although criteria for diagnosis of outcome events
were documented in most of the included RCTs, the definitions were
not standardized among studies because of the difference in operation
type and methodological quality, which might affect interpretation of the benefit of intervention. To overcome these limitations, we
recommend more high-quality RCTs of large scale to produce
conclusive results.
* 2013 Lippincott Williams & Wilkins
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Annals of Plastic Surgery
& Volume 72, Number 1, January 2014
Meta-analysis of Antibiotic Prophylaxis for PRS
FIGURE 5. Pooled OR for incidence of SSI, OWC, and AE relative to antibiotics with short-term prophylactic antibiotics
compared to long-term prophylactic antibiotics for plastic and reconstructive surgeries. The diamond denotes the fixed-effects
(SSI and OWC) or random-effects (AE) pooled OR and 95% CI. The dashed lines are drawn at the overall pooled estimate.
***Comparison of short-term and long-term arms in trials with more than 1 intervention arm; AE indicates adverse event.
* 2013 Lippincott Williams & Wilkins
www.annalsplasticsurgery.com
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
129
Annals of Plastic Surgery
Zhang et al
REFERENCES
1. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for
antimicrobial prophylaxis in surgery. Surg Infect (Larchmt). 2013;14:73Y156.
2. CDC NNIS System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2003, issued August
2003. Am J Infect Control. 2003;31:481Y498.
3. Gravante G, Caruso R, Araco A, et al. Infections after plastic procedures: incidences, etiologies, risk factors, and antibiotic prophylaxis. Aesthetic Plast
Surg. 2008;32:243Y251.
4. Kuijpers DI, Smeets NW, Lapiere K, et al. Do systemic antibiotics increase the
survival of a full thickness graft on the nose? J Eur Acad Dermatol Venereol.
2006;20:1296Y1301.
5. Landes G, Harris PG, Lemaine V, et al. Prevention of surgical site infection and
appropriateness of antibiotic prescribing habits in plastic surgery. J Plast
Reconstr Aesthet Surg. 2008;61:1347Y1356.
6. Mirzabeigi MN, Mericli AF, Ortlip T, et al. Evaluating the role of postoperative
prophylactic antibiotics in primary and secondary breast augmentation: a retrospective review. Aesthet Surg J. 2012;32:61Y68.
7. Krizek TJ, Koss N, Robson MC. The current use of prophylactic antibiotics in
plastic and reconstructive surgery. Plast Reconstr Surg. 1975;55:21Y32.
8. Rohrich RJ, Rios JL. The role of prophylactic antibiotics in plastic surgery:
whom are we treating? Plast Reconstr Surg. 2003;112:617Y618.
9. Perrotti JA, Castor SA, Perez PC, et al. Antibiotic use in aesthetic surgery: a
national survey and literature review. Plast Reconstr Surg. 2002;109:1685Y1693;
discussion 94Y5.
10. Jadad AR, McQuay HJ. Meta-analyses to evaluate analgesic interventions: a
systematic qualitative review of their methodology. J Clin Epidemiol.
1996;49:235Y243.
11. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1Y12.
12. Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in metaanalyses. BMJ. 2003;327:557Y560.
13. Deeks JJ. Systematic reviews in health care: systematic reviews of evaluations
of diagnostic and screening tests. BMJ. 2001;323:157Y162.
14. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials.
1986;7:177Y188.
15. Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by
a simple, graphical test. BMJ. 1997;315:629Y634.
16. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for
publication bias. Biometrics. 1994;50:1088Y1101.
17. Baran CN, Sensoz O, Ulusoy MG. Prophylactic antibiotics in plastic and reconstructive surgery. Plast Reconstr Surg. 1999;103:1561Y1566.
18. Lilja M, Makitie AA, Anttila VJ, et al. Cefuroxime as a prophylactic preoperative antibiotic in septoplasty. A double blind randomized placebo controlled
study. Rhinology. 2011;49:58Y63.
19. Ahmadi AH, Cohen BE, Shayani P. A prospective study of antibiotic efficacy
in preventing infection in reduction mammaplasty. Plast Reconstr Surg.
2005;116:126Y131.
20. Whittaker JP, Nancarrow JD, Sterne GD. The role of antibiotic prophylaxis in
clean incised hand injuries: a prospective randomized placebo controlled
double blind trial. J Hand Surg Br. 2005;30:162Y167.
21. Ricci G, DAscanio L. Antibiotics in septoplasty: evidence or habit? Am J
Rhinol Allergy. 2012;26:194Y196.
22. Krizek TJ, Gottlieb LJ, Koss N, et al. The use of prophylactic antibacterials in
plastic surgery: a 1980s update. Plast Reconstr Surg. 1985;76:953Y963.
130
www.annalsplasticsurgery.com
& Volume 72, Number 1, January 2014
23. Weichman KE, Levine SM, Wilson SC, et al. Antibiotic selection for the treatment
of infectious complications of implant-based breast reconstruction. Ann Plast
Surg.2013;71(2):140Y143.
24. Amland PF, Andenaes K, Samdal F, et al. A prospective, double-blind, placebocontrolled trial of a single dose of azithromycin on postoperative wound infections in plastic surgery. Plast Reconstr Surg. 1995;96:1378Y1383.
25. Phillips BT, Bishawi M, Dagum AB, et al. A systematic review of antibiotic use
and infection in breast reconstruction: what is the evidence? Plast Reconstr
Surg. 2013;131:1Y13.
26. Hauck RM, Nogan S. The use of prophylactic antibiotics in plastic surgery:
update in 2010. Ann Plast Surg. 2013;70:91Y97.
27. Tadiparthi S. Prophylactic antibiotics for clean, non-implant plastic surgery:
what is the evidence? J Wound Care. 2008;17:392Y394, 6Y8.
28. Kompatscher P, von Planta A, Spicher I, et al. Comparison of the incidence and
predicted risk of early surgical site infections after breast reduction. Aesthetic
Plast Surg. 2003;27:308Y314.
29. Bucher BT, Warner BW, Dillon PA. Antibiotic prophylaxis and the prevention
of surgical site infection. Curr Opin Pediatr. 2011;23:334Y338.
30. Mathur P, Trikha V, Farooque K, et al. Implementation of a short course of
prophylactic antibiotic treatment for prevention of postoperative infections in
clean orthopaedic surgeries. Indian J Med Res. 2013;137:111Y116.
31. Wang F, Chen XZ, Liu J, et al. Short-term versus long-term administration of single
prophylactic antibiotic in elective gastric tumor surgery. Hepatogastroenterology.
2012;59:1784Y1788.
32. Chang WC, Hung YC, Li TC, et al. Short course of prophylactic antibiotics in
laparoscopically assisted vaginal hysterectomy. J Reprod Med. 2005;50:524Y528.
33. Scher KS. Studies on the duration of antibiotic administration for surgical
prophylaxis. Am Surg. 1997;63:59Y62.
34. Esposito S, Leone S, Noviello S, et al. Antibiotic prophylaxis in hernia repair
and breast surgery: a prospective randomized study comparing piperacillin/
tazobactam versus placebo. J Chemother. 2006;18:278Y284.
35. Hopper AN, Lane IF. Randomized clinical trial of co-amoxiclav versus no
antibiotic prophylaxis in varicose vein surgery (Br J Surg 2010; 97: 29Y36).
Br J Surg. 2010;97:1148; author reply -9.
36. Gil-Ascencio M, Castillo-Gomez CJ, Palacios-Saucedo GD, et al. Antibiotic
prophylaxis in tonsillectomy and its relationship with postoperative morbidity.
Acta Otorrinolaringol Esp. 2013;64(4):273Y278.
37. Thomas R, Alvino P, Cortino GR, et al. Long-acting versus short-acting
cephalosporins for preoperative prophylaxis in breast surgery: a randomized
double-blind trial involving 1,766 patients. Chemotherapy. 1999;45:217Y223.
38. McHugh SM, Hill AD, Humphreys H. Intraoperative technique as a factor in
the prevention of surgical site infection. J Hosp Infect. 2011;78:1Y4.
39. Uckay I, Harbarth S, Peter R, et al. Preventing surgical site infections. Expert
Rev Anti Infect Ther. 2010;8:657Y670.
40. Gyssens IC. Preventing postoperative infections: current treatment recommendations. Drugs. 1999;57:175Y185.
41. Peled IJ, Dvir G, Berger J, et al. Prophylactic antibiotics in aesthetic and
reconstructive surgery. Aesthetic Plast Surg. 2000;24:299Y302.
42. Clayton JL, Bazakas A, Lee CN, et al. Once is not enough: withholding postoperative prophylactic antibiotics in prosthetic breast reconstruction is associated
with an increased risk of infection. Plast Reconstr Surg. 2012;130:495Y502.
43. Vale CL, Tierney JF, Burdett S. Can trial quality be reliably assessed from
published reports of cancer trials: evaluation of risk of bias assessments in
systematic reviews. BMJ. 2013;346:f1798.
* 2013 Lippincott Williams & Wilkins
Copyright 2013 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Syndrome of Inappropriate Antidiuretic Hormone Secretion SIADHDocument14 paginiSyndrome of Inappropriate Antidiuretic Hormone Secretion SIADHbhatubim100% (1)
- NormaltestreportDocument1 paginăNormaltestreportgalaxydiagnosticlabcclghÎncă nu există evaluări
- Health Sector of Arunanchal PradeshDocument14 paginiHealth Sector of Arunanchal PradeshJatin ChauhanÎncă nu există evaluări
- Complete Blood Picture: Test Name Value Units Reference Range 3.44 7.4 76 22 28.5Document107 paginiComplete Blood Picture: Test Name Value Units Reference Range 3.44 7.4 76 22 28.5anil tanankiÎncă nu există evaluări
- White FungusDocument279 paginiWhite FungusDjsjsbÎncă nu există evaluări
- Orahex Oral SolutionDocument1 paginăOrahex Oral SolutionconanmarcÎncă nu există evaluări
- Clinical Skills: Bed Making and Patient Positioning: Glynis Collis PellattDocument4 paginiClinical Skills: Bed Making and Patient Positioning: Glynis Collis PellattDenny MatulessyÎncă nu există evaluări
- Health CareDocument10 paginiHealth Caresonali mishraÎncă nu există evaluări
- Severe Sepsis Is Sepsis CausingDocument6 paginiSevere Sepsis Is Sepsis CausingHerryanto AgustriadiÎncă nu există evaluări
- Poison and Antidote ChartDocument5 paginiPoison and Antidote ChartSusanne Mae Gonzales50% (2)
- The Scoop On Brain Healt Dietary Supplement Products Containing Huperzine ADocument7 paginiThe Scoop On Brain Healt Dietary Supplement Products Containing Huperzine Avasilyi IvanenkoÎncă nu există evaluări
- Prof Norhayati RMC KPJUCDocument18 paginiProf Norhayati RMC KPJUCtheskywlkrÎncă nu există evaluări
- Keguguran Berulang - Kanadi SumaprajaDocument63 paginiKeguguran Berulang - Kanadi SumaprajaNetty HerawatiÎncă nu există evaluări
- Role of Histomorphology and Chronic Inflammation Score in Chronic DacryocystitisDocument3 paginiRole of Histomorphology and Chronic Inflammation Score in Chronic Dacryocystitissanchanaa anbalaganÎncă nu există evaluări
- Basic Measurements in EpidemiologyDocument58 paginiBasic Measurements in EpidemiologyRida AwwalÎncă nu există evaluări
- Ichroma II Test Panels 210331 104829Document2 paginiIchroma II Test Panels 210331 104829Sinergy DiagnosticÎncă nu există evaluări
- You Exec - KPIs - 169 - BlueDocument14 paginiYou Exec - KPIs - 169 - BlueEssa SmjÎncă nu există evaluări
- An Introduction To Corneal TransplantationDocument2 paginiAn Introduction To Corneal TransplantationNovii NoviiÎncă nu există evaluări
- Absorption of Drugs From Extravascular RoutesDocument11 paginiAbsorption of Drugs From Extravascular RoutesraviÎncă nu există evaluări
- A Review of Strategies To Decrease The Duration of Indwelling Urethral Catheters and Potentially Reduce The Incidence of Catheter-Associated Urinary Tract Infections - ProQuestDocument10 paginiA Review of Strategies To Decrease The Duration of Indwelling Urethral Catheters and Potentially Reduce The Incidence of Catheter-Associated Urinary Tract Infections - ProQuestHelmy HanafiÎncă nu există evaluări
- Closer The Client Is To The Origination of Risk, The Higher The Risk For Complications. Sometimes, The TimeDocument3 paginiCloser The Client Is To The Origination of Risk, The Higher The Risk For Complications. Sometimes, The Timeiamlx2100% (1)
- Health Care Law OutlineDocument17 paginiHealth Care Law OutlineMegan Lindsay Ruffin100% (1)
- Oral and Maxillofacial Manifestations in Patients With Drug AddictionDocument8 paginiOral and Maxillofacial Manifestations in Patients With Drug AddictionDiana Mihaela IlieÎncă nu există evaluări
- 5.respiratory Distress Dental LectureDocument40 pagini5.respiratory Distress Dental LecturehaneeneeÎncă nu există evaluări
- Breast Self Examination 1Document36 paginiBreast Self Examination 1zehan iraniÎncă nu există evaluări
- Cardio System 2Document1 paginăCardio System 2api-298312370Încă nu există evaluări
- Evaluation of The Pain Resource Nurse Role - A Resource For Improving Pediatric Pain ManagementDocument8 paginiEvaluation of The Pain Resource Nurse Role - A Resource For Improving Pediatric Pain ManagementWahyu WidiyantoÎncă nu există evaluări
- Phlebotomy - It's A Risky BusinessDocument41 paginiPhlebotomy - It's A Risky BusinessMahogony ScottÎncă nu există evaluări
- A Textbook of General Practice - 2nd EditionDocument336 paginiA Textbook of General Practice - 2nd Editionstrahiltodorov100% (2)
- Here's Your Coronavirus Insurance: You Have Made A Wise ChoiceDocument3 paginiHere's Your Coronavirus Insurance: You Have Made A Wise ChoiceAjay Kumar GumithiÎncă nu există evaluări