Documente Academic
Documente Profesional
Documente Cultură
3 Vol. 6 Issue 7 IJPSR 2015 RE 1557
Încărcat de
memeeeyyyTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
3 Vol. 6 Issue 7 IJPSR 2015 RE 1557
Încărcat de
memeeeyyyDrepturi de autor:
Formate disponibile
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
E-ISSN: 0975-8232; P-ISSN: 2320-5148
IJPSR (2015), Vol. 6, Issue 7
(Review Article)
Received on 05 October 2014; received in revised form, 08 February, 2015; accepted, 28 February, 2015; published 01 July, 2015
COLON TARGETED DRUG DELIVERY SYSTEM: A REVEIW ON PRIMARY AND NOVEL
APPROACHES
P. Ghugarkar*, P. Kulat, K. Swain and V. Suggala and D. Shaik
Department of Pharmaceutics, Padmashree Dr. Vithalrao Vikhe Patil Foundations College of Pharmacy,
Vilad Ghat, Ahmednagar-414111, Maharashtra, India.
Keywords:
Colon drug delivery system,
Primary approaches, newly
developed approaches, evaluation of
colon targeted drug delivery systems
Correspondence to Author:
P. Ghugarkar
Department of Pharmaceutics,
Padmashree Dr. Vithalrao Vikhe Patil
Foundations College of Pharmacy,
Vilad Ghat, Ahmednagar-414111,
Maharashtra, India.
E-mail: ghugarkarp@gmail.com
ABSTRACT: In the recent years there is new development in field of colon
specific drug delivery system. The colon is the terminal part of the GIT
which has gained as a potential site for delivery of various novel therapeutic
drugs. The colon is a site where both local and systemic delivery of drugs
can take place. Local delivery allows topical treatment of inflammatory
bowel disease, Crohns disease, ulcerative colitis, etc. However, treatment
can be made effective if the drugs can be targeted directly into the colon,
thereby reducing the systemic side effects. It also plays vital role in systemic
delivery of proteins, therapeutic peptides, anti-asthmatic drugs,
antihypertensive drugs and anti-diabetic agents. This review article discusses
introduction of colon, need and Primary approaches for CDDS (Colon
Specific Drug Delivery), which includes prodrugs, pH and time dependent
systems and microbially triggered drug delivery system. Newly developed
CDDS, which includes pressure controlled colonic delivery capsules
(PCDCS), CODE and osmotic controlled drug delivery and also focuses on
evaluations of Colon targeted drug delivery in general.
INTRODUCTION: Targeted drug delivery to the
colon is highly desirable for local treatment of a
variety of bowel diseases such as (ulcerative colitis,
crohns disease) amebiosis, colonic cancer, and for
local treatment of local colonic pathologies, and the
systemic delivery of protein and peptide drugs 1.
The colon specific drug delivery system (CDDS)
should be capable of protecting the drug en route to
colon i.e. drug release and absorption should not
occur in the stomach as well as the small intestine
and bioactive agent should not be degraded and to
allow drug release only in the colon 2.
QUICK RESPONSE CODE
DOI:
10.13040/IJPSR.0975-8232.6(7).2681-88
Article can be accessed online on:
www.ijpsr.com
The colon is believed to be a suitable absorption
site for peptides and protein drugs for the following
reasons; (i) less diversity, and intensity of digestive
Colon targeted drug delivery system increases the
absorption of poorly absorbable drug due to high
retention time of the colon.enzymes, (ii)
comparative proteolytic activity of colon mucosa is
much less than that observed in the small intestine,
thus CDDS protects peptide drugs from hydrolysis,
and enzymatic degradation in duodenum and
jejunum, and eventually releases the drug into
ileum or colon which leads to greater systemic
bioavailability.3 And finally, because the colon has
a long residence time which is up to 5 days and is
highly responsive to absorption enhancers.4
Advantages: 5
DOI link: http://dx.doi.org/10.13040/IJPSR.0975-8232.6(7).2681-88
International Journal of Pharmaceutical Sciences and Research
1. Used for the effective treatment of
inflammatory bowel diseases like ulcerative
colitis, crohns disease, etc.
2681
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
2. Decreases the side effects in the treatment
of colon diseases.
3. Prevents gastric irritation resulting due to
the administration of NSAIDs.
4. Minimizes first pass metabolism.
5. Provides suitable environment for proteins
and peptides that are sensitive to gastric
fluid and digestive enzymes.
6. Increased patient compliance.
7. Decreased frequency of administration.
Hence decreased cost of drugs.
8. High retention time thus increasing the
bioavailability of poorly absorbable drugs.
Limitations of colon target DDS:
Difficult to access colon:
1. Successful delivery requires the drug to be
in solution before it arrives in the colon, but
the fluid content in the colon is lower and
more viscous than in upper GIT, which is
the limiting factor for poorly soluble drugs.
2. Lower surface area and relative tightness of
the tight junctions in the colon can restrict
drug transport across the mucosa in to the
systemic circulation.6
Need for colon targeting drug delivery:
1. Targeted drug delivery to the colon to ensure
that direct treatment at the disease site (local
delivery), at lower dosing and fewer systemic
side effects 7.
E-ISSN: 0975-8232; P-ISSN: 2320-5148
2. Site-specific or targeted drug delivery system
would allow oral administration of peptide and
protein drugs, colon-specific formulation could
also be used to prolong the drug delivery 8.
3. Colon-specific drug delivery system is
considered to be beneficial in the treatment of
colon diseases 8.
4. The colon is a site where both local or
systemic drug delivery could be achieved,
topical treatment of inflammatory bowel
disease, e.g. ulcerative colitis or Crohns
disease. Such inflammatory conditions are
usually treated with glucocorticoids and
sulphasalazine 9.
5. A number of others serious diseases of the
colon, e.g. colorectal cancer, might also be
capable of being treated more effectively if
drugs were targeted to the colon 10.
6. Formulations for colonic delivery are also
suitable for delivery of drugs which are polar
and/or susceptible to chemical and enzymatic
degradation in the upper GI tract, highly
affected by hepatic metabolism, in particular,
therapeutic proteins and peptides 10.
Criteria for Selection of Drug for CDDS:
The best Candidates for CDDS are drugs which
show poor absorption from the stomach or intestine
including peptides. The drugs used in the treatment
of IBD (Inflammatory Bowel Disease), ulcerative
colitis, diarrhea, and colon cancer are ideal
candidates for local colon delivery 11. The criteria
for selection of drugs for CDDS is summarized in
Table 1.12 13
TABLE 1: CRITERIA FOR SELECTION OF DRUGS FOR CDDS
Criteria
Pharmacological Class
Non-peptide drugs
Drugs used for local
Anti-inflammatory drugs
Oxyprenolol,
effects in Colon
Metoprolol,
against GIT diseases
Nifedipine
Drugs poorly
Antihypertensive and
Ibuprofen,
absorbed from upper
Antianginal drugs
Isosorbides,
GIT
Theophylline
Drugs for colon
Antineoplastic drugs
Pseudoephedrin
cancer
Drugs that degrade
Peptides and proteins
Bromophenaramine,
in stomach and small
5-Flourouracil,
intestine
Doxorubicin
Drugs that undergo
Nitroglycerin and
Bleomycin, Nicotine
extensive first pass
corticosteroids
metabolism
International Journal of Pharmaceutical Sciences and Research
Peptide drugs
Amyline, Antisense,
Oligonucleotide
Cyclosporin,
Desmopressin
Epoetin,
Glucagon
Gonadoreline,
Insulin, Interferons
Protirelin Sermorelin,
Saloatonin
2682
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
E-ISSN: 0975-8232; P-ISSN: 2320-5148
Drug Carrier is another factor which influences
CDDS. The selection of carrier for particular drugs
depends on the physiochemical nature of the drug
as well as the disease for which the system is to be
used. Factors such as chemical nature, stability and
partition coefficient of the drug and type of
absorption enhancer chosen influence the carrier
selection. Moreover, the choice of drug carrier
depends on the functional groups of the drug
molecule 14. For example, aniline or nitro groups on
a drug may be used to link it to another benzene
group through an azo bond. The carriers, which
contain additives like polymers (may be used as
matrices and hydro gels or coating agents) may
influence the release properties and efficacy of the
systems 15.
dependent polymers is based on these differences
in pH levels. The polymers described as pH
dependent in colon specific drug delivery are
insoluble at low pH levels but become increasingly
soluble as pH rises.20
Approaches for colon targeted drug delivery: 16
1. Primary approaches for colon targeted drug
delivery:
b. Delayed or time controlled release drug
delivery system:
Time controlled drug delivery system 22 includes
sustained or delayed release systems. In this system
the delayed release or colon targeted drug delivery
is attained by prolonging the lag time. The transit
time varies in different parts of gastrointestinal
tract. This transit time is responsible for the
delayed release of drug. The main drawbacks of
this delivery system are that the transit time varies
from one person to other and amount of food
intake.
a) pH sensitive polymer coated drug delivery
system
b) Delayed release drug delivery system
c) Microbially triggered drug delivery
i. Prodrug approach
ii. Polysaccharide based system
Although a pH dependent polymer can protect a
formulation in the stomach, and proximal small
intestine, it may start to dissolve in the lower small
intestine, and the site-specificity of formulations
can be poor.21 The decline in pH from the end of
the small intestine to the colon can also result in
problems, lengthy lag times at the ileo-cecal
junction or rapid transit through the ascending
colon which can also result in poor site-specificity
of enteric-coated single-unit formulations.20
2. New approaches for colon targeted drug
delivery:
a. Pressure controlled drug delivery system
(PCDDDS)
b. CODE
c. Osmotic controlled drug delivery system
(OROS-CT)
1. Primary Approaches for CDDS:
a. pH sensitive polymer coated drug delivery
system:
In the stomach, pH ranges between 1 and 2 during
fasting but increases after eating.17 The pH is about
6.5 in the proximal small intestine, and about 7.5 in
the distal small intestine.18 From the ileum to the
colon, pH declines significantly. It is about 6.4 in
the cecum. However, pH values as low as 5.7 have
been measured in the ascending colon in healthy
volunteers.19 The pH in the transverse colon is 6.6
and 7.0 in the descending colon. Use of pH
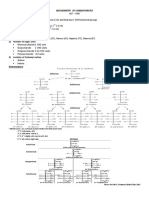
FIG.1: DESIGN OF ENTERIC COATED TIMED-RELEASE
PRESS COATED TABLET (ETP TABLET)
Enteric coated time-release press coated (ETP)
tablets, are composed of three components, a drug
containing core tablet (rapid release function), the
press coated swellable hydrophobic polymer layer
(Hydroxy propyl cellulose layer (HPC), time
release function) and an enteric coating layer (acid
resistance function). The tablet does not release the
drug in the stomach due to the acid resistance of the
outer enteric coating layer. After gastric emptying,
International Journal of Pharmaceutical Sciences and Research
2683
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
the enteric coating layer rapidly dissolves and the
intestinal fluid begins to slowly erode the press
coated polymer (HPC) layer.
c. Microbially triggered drug delivery system:
The microflora of colon is in the range of 1011 -1012
CFU/mL23, consisting mainly of anaerobic bacteria,
e.g. Bacteroides, Bifidobacteria, Eubacteria,
Clostridia, Enterococci, Enterobacteria and
Ruminococcus etc. This vast microflora fulfills its
energy needs by fermenting various types of
substrates that have been left undigested in the
small intestine, e.g. di- and tri- saccharides,
polysaccharides etc 24. For this fermentation, the
microflora produces a vast number of enzymes like
glucoronidase,
xylosidase,
arabinosidase,
galactosidase,
nitroreductase,
azareducatase,
deaminase, and urea dehydroxylase 25. Because of
the presence of the biodegradable enzymes only in
the colon, the use of biodegradable polymers for
colon-specific drug delivery seems to be a more
site-specific approach as compared to other
approaches 26.
These polymers shield the drug from the
environments of stomach and small intestine, and
are able to deliver the drug to the colon. On
reaching the colon, they undergo assimilation by
micro-organism, or degradation by enzyme or
break down of the polymer back bone leading to a
subsequent reduction in their molecular weight and
thereby loss of mechanical strength 27-31. They are
then unable to hold the drug entity any longer. 32
TABLE 2: EXAMPLES OF PRODRUG SYSTEM FOR
CDDS
Drug
Carrier
Linkage
hydrolysed
5-ASA
Azo
Azo linkage
conjugates
Dexamethasone
Saccharide
Glycosidic
carriers
linkage
Prednisolone,
Glucose,
Glycosidic
hydrocortisone,
galactose
linkage
fludrocortisone
Salicylic acid
Amino acid
Amide
conjugates,
linkage
glycine
Prodrug 33 is the main approach of microbial
triggered drug delivery system in which the drug
release from the formulation is triggered by the
microflora present in the gut. Prodrug is the
E-ISSN: 0975-8232; P-ISSN: 2320-5148
inactive form of an active parent drug that
undergoes enzymatic transformation to release the
active drug. The produrgs are prepared by linking
the active drug with hydrophobic moieties like
amino acids, glucoronic acids, glucose, galactose,
cellulose, etc. These prodrug molecules get
hydrolysed in the presence of the enzymes released
by the microflora.
The main drawback of this approach is that the
formulation depends on the functional groups
available on drug moiety for chemical linkage. The
prodrugs formed upon linkage results in the
formation of new chemical entities that need a lot
of evaluation before using them as carriers.
The most widely used prodrug approach is the
metabolism of azo compounds by intestinal
bacteria. Polysaccharide based delivery system is
the other form of microbial triggered drug delivery
system. Naturally occurring polysaccharides like
guar gum, xanthan gum, chitosan, alginates, etc. are
used in targeting the drug delivery. These are
broken down by the colonic microflora to simple
saccharides.
TABLE 3: DIFFERENT POLYMERS USED FOR CDDS
BASED ON MICROBIAL DRUG DELIVERY SYSTEM 33
Class
Disaccharides
Oligosaccharides
Examples
Lactose, Maltose
Cyclodextrins, Lactulose,
Raffinose,
Stachyose
Polysaccharides
Alginates, Amylose,
Cellulose, Chitosan,
Starch, Chondroitin
sulphate, pectin,
xanthan gum, etc
2. New approaches for colon targeted drug
delivery:
a. Pressure controlled drug delivery system:
Digestion mainly occurs due to the contractility of
the stomach and peristaltic movement of the
intestine. The contractility movement of stomach
leads to the digestion or breakdown of larger
particles to smaller ones which are then transferred
to intestine. The peristaltic movement of intestine is
responsible for the passage of bolus from one part
of GIT to the next part. The peristaltic movement
of ascending colon transfers the bolus to transverse
colon called as mass peristalsis. These peristaltic
International Journal of Pharmaceutical Sciences and Research
2684
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
movements occur in limited number i.e. three to
four times a day. These peristaltic movements of
intestine results in an increase in the luminal
pressure. This increase in luminal pressure is the
key point in the development of pressure controlled
drug delivery system.
The pressure controlled drug delivery system 34
consists of a capsule in which the drug is present.
These gelatin capsules are coated with water
insoluble polymer like ethyl cellulose on their inner
side. The drug is introduced into the capsule along
with suppository base. The thickness of ethyl
cellulose coating determines the disintegration
capacity of the capsule. After administration the
suppository base dissolves at body temperature.
The water from intestinal contents is absorbed
resulting in increased viscosity which leads to an
increase in the pressure in the capsule. The pressure
in the capsule expels the drug into the colon.
b. CODES:
CODES is a unique CDDS technology that was
designed to avoid the inherent problems associated
with pH-or time dependent systems 35, 36. CODES
is a combined approach of pH dependent and
microbially triggered CDDS. It has been developed
by utilizing a unique mechanism involving
lactulose, which acts as a trigger for site specific
drug release in the colon, (Fig. 2).
FIG. 2: SCHEMATICS OF THE CONCEPTUAL DESIGN OF
CODES
E-ISSN: 0975-8232; P-ISSN: 2320-5148
The system consists of a traditional tablet core
containing lactulose, which is over coated with and
acid soluble material, Eudragit E, and then
subsequently overcoated with an enteric material,
Eudragit L. The premise of the technology is that
the enteric coating protects the tablet while it is
located in the stomach and then dissolves quickly
following gastric emptying. The acid soluble
material coating then protects the preparation as it
passes through the alkaline pH of the small
intestine.37
Once the tablet arrives in the colon, the bacteria
enzymetically
degrade
the
polysaccharide
(lactulose) into organic acid. This lowers the pH
surrounding the system sufficient to effect the
dissolution of the acid soluble coating and
subsequent drug release.38
c. Osmotic controlled drug delivery system
(OROS-CT):
The OROS-CT (Alza corporation) can be used to
target the drug locally to the colon for the treatment
of disease or to achieve systemic absorption that is
otherwise unattainable.39 The OROS-CT system
can be a single osmotic unit or may incorporate as
many as 5-6 push-pull units, each 4mm in diameter,
encapsulated within a hard gelatin capsule, (Fig. 3).
40
Each bilayer push pull unit contains an osmotic
push layer and a drug layer, both surrounded by a
semipermeable membrane. An orifice is drilled
through the membrane next to the drug layer.
Immediately after the OROS-CT is swallowed, the
gelatin capsule containing the push-pull units
dissolves.
Because of its drug-impermeable enteric coating,
each push-pull unit is prevented from absorbing
water in the acidic aqueous environment of the
stomach, and hence no drug is delivered. As the
unit enters the small intestine, the coating dissolves
in this higher pH environment (pH >7), water
enters the unit, causing the osmotic push
compartment to swell, and concomitantly creates a
flowable gel in the drug compartment. Swelling of
the osmotic push compartment forces drug gel out
of the orifice at a rate precisely controlled by the
rate of water transport through the semipermeable
membrane. For treating ulcerative colitis, each push
pull unit is designed with a 3-4 h post gastric delay
International Journal of Pharmaceutical Sciences and Research
2685
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
to prevent drug delivery in the small intestine. Drug
release begins when the unit reaches the colon.
OROS-CT units can maintain a constant release
rate for up to 24 hours in the colon or can deliver
drug over a period as short as four hours. Recently,
new phase transited systems have come which
promise to be a good tool for targeting drugs to the
colon.[41-44] Various in vitro / in vivo evaluation
techniques have been developed and proposed to
test the performance and stability of CDDS.
E-ISSN: 0975-8232; P-ISSN: 2320-5148
buffers may be undertaken to characterize the
behavior of formulations at different pH levels.
Dissolution tests of a colon-specific formulation in
various media simulating pH conditions and times
likely to be encountered at various locations in the
gastrointestinal tract have been studied.46 The
media chosen were, for example, pH 1.2 to
simulate gastric fluid, pH 6.8 to simulate the jejunal
region of the small intestine, and pH 7.2 to simulate
the ileum segment. Enteric-coated capsules for
CDDS have been investigated in a gradient
dissolution study in three buffers. The capsules
were tested for two hours at pH 1.2, then one hour
at pH 6.8, and finally at pH 7.4.47
b) In vitro enzymatic test:
For this there are 2 tests:
a. Incubate carrier drug system in fermenter
containing suitable medium for bacteria
(Streptococcus faccium or B.ovatus) amount of
drug released at different time intervals
determined.
FIG.3: CROSS-SECTION OF THE OROS-CT COLON
TARGETED DRUG DELIVERY SYSTEM
For in vitro evaluation, not any standardized
evaluation technique is available for evaluation of
CDDS because an ideal in vitro model should
posses the in-vivo conditions of GIT such as pH,
volume, stirring, bacteria, enzymes, enzyme
activity, and other components of food. Generally,
these conditions are influenced by the diet, physical
stress, and these factors make it difficult to design a
slandered in-vitro model. In vitro models used for
CDDS are:
a) In vitro dissolution test:
Dissolution of controlled-release formulations used
for colon-specific drug delivery are usually
complex, and the dissolution methods described in
the USP cannot fully mimic in vivo conditions such
as those relating to pH, bacterial environment and
mixing forces.45 Dissolution tests relating to CDDS
may be carried out using the conventional basket
method. Parallel dissolution studies in different
b. Drug release study is done in buffer medium
containing enzymes (enzyme pectinase,
dextranase), or rat or guinea pig or rabbit cecal
contents. The amount of drug released in
particular time is determined, which is directly
proportional to the rate of degradation of
polymer carrier 48.
c) In vivo evaluation:
A number of animals such as dogs, guinea pigs,
rats, and pigs are used to evaluate the delivery of
drug to colon because they resemble the anatomic
and physiological conditions as well as the micro
flora of human GIT. While choosing a model for
testing a CDDS, relative model for the colonic
diseases should also be considered. Guinea pigs are
commonly used for experimental IBD model. The
distribution of azoreductase and glucouronidase
activity in the GIT of rat and rabbit is fairly
comparable to that in the human.49 For rapid
evaluation of CDDS, a novel model has been
proposed. In this model, the human fetal bowel is
transplanted into a subcutaneous tullel on the back
of thymic nude mice, which bascularizes within
four weeks, matures, and becomes capable of
developing of mucosal immune system from the
host.
International Journal of Pharmaceutical Sciences and Research
2686
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
E-ISSN: 0975-8232; P-ISSN: 2320-5148
Drug Delivery Index (DDI) and Clinical
Evaluation of Colon-Specific Drug Delivery
Systems:
DDI is a calculated pharmacokinetic parameter,
following single or multiple dose of oral colonic
prodrugs. DDI is the relative ratio of RCE (Relative
colonic tissue exposure to the drug) to RSC
(Relative amount of drug in blood i.e. that is
relative systemic exposal to the drug). High drug
DDI value indicates better colon drug delivery.
Absorption of drugs from the colon is monitored by
colonoscopy and intubation. Currently, gamma
scintigraphy and high frequency capsules are the
most preferred techniques employed to evaluate
colon drug delivery systems.50
6.
CONCLUSION: The colonic region of the GIT
has become an increasingly important site for drug
delivery and absorption. Colon targeted drug
delivery system offers benefits of both local as well
as systemic effects. Colon specificity is more likely
to be achieved with systems that utilize natural
materials that are degraded by colonic bacterial
enzymes. The main advantage of CDDS is that the
colon offers near neutral pH, a long transit time,
reduced enzymatic activity and increased
responsiveness to absorption enhancers. The novel
approaches are more specific compared to the
primary approaches. The biodegradable polymers
are used for the colon specific delivery of the drug.
For the in vitro evaluation of the system the current
dissolution techniques are not suitable. Research is
going on to develop suitable dissolution methods to
evaluate the colon targeted drug delivery systems.
13.
REFERENCES:
1.
2.
3.
4.
5.
Adkin DA, Davis SS, Sparrow RA, Wilding IR. Colonic
transit of different sized tablets in healthy subjects. Journal
of Controlled Release. 1993; 23: 147- 156.
Ahrabi SF, Madseh G, Dyrstad K, Sande SA, Graffner C.
Development of pectin matrix tablets for colonic delivery
of model drug ropivacanie. European Journal of
Pharmaceutical Sciences.2000; 10: 43-52.
Akala EO, Elekwachi O, Chase V, Johnson H, Lazarre M,
Scott K. Organic redox-initiated polymerization process
for the fabrication of hydrogels for colon-specific drug
delivery. Drug Dev Ind Pharm 2003. Apr;29(4):375-386
Chourasia MK, Jain SK. Pharmaceutical approaches to
colon targeted drug delivery systems. J Pharm Pharm
Sci 2003. Jan-Apr;6(1):33-66
Sonasaniya Balvir, Dr. M.R. Patel, Dr. K.R.Patel, Dr.
N.M. Patel. A Review on colon targeted drug delivery
system. International Journal of Universal Pharmacy and
Bio Sciences. 2013; 2(1):20-34.
International Journal of Pharmaceutical Sciences and Research
7.
8.
9.
10.
11.
12.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
Pramod Kumar Biswal, Anant Kumar and Anupam Singh
Bhadouriya. Design and evolution of colon specific drug
delivery system. IJPCBS. 2013; 3:1 150-167.\
Malik K, Goswami L, Kothiyal P, Mukhopadhyay S.A
Review on Colon targeting Drug Delivery System: Novel
Approaches, Anatomy and Evaluation. The Pharma
Innovation. 2012; 1(9):1-12.
Encyclopedia of controlled drug delivery, John wiley and
sons, Inc. Newyork, 2003, pp 698-726
Sarasija S, Hota A. Indian J Pharmaceutical Sci. 2000; 62:
1-8.
Reena Sharma, Nimrata Seth. Colon Targeted Drug
Delivery System: A review.2013: 4:4: 66-77.
Vyas SP, Khar RK. Gastroretentive systems. In: Vyas SP,
Khar RK, editors. Controlled drug delivery: concepts and
advances. New Delhi: Vallabh Prakashan, 2005; 218-253.
Antonin KH, Rak R, Bieck PR, Preiss R, Schenker U,
Hastewell J, et al. The absorption of human calcitonin
from
the
transverse
colon
of
man. Int
J
Pharm 1996;130(1):33-39 .10.1016/0378-5173(95)042482
Mackay M, Tomlinson E. Colonic delivery of therapeutic
peptides and proteins, In: Biek PR, editors. Colonic drug
absorption and metabolism. New York: Marcel Dekker,
1993; 159-176.
Friend DR, Chang GW. A colon-specific drug-delivery
system based on drug glycosides and the glycosidases of
colonic bacteria. J Med Chem 1984. Mar;27(3):261-266
10.1021/jm00369a005
Chavan MS , Sant VP, Nagarsenkar MS. Azo-containing
urethane analogus for colonic drug delivery system:
synthesis, charectarisation and in-vitro evaluation. Journal
of Pharmacy Pharmacology. 2001;53: 895-900
Vinay K Gupta, G. Gnanarajan, Preeti Kothiyal. A Review
Article on Colonic Targeted Drug Delivery System. 2012;
1(7): 14-24.
Rubinstein A. Approaches and opportunities in colonspecific drug delivery. Crit Rev Ther Drug Carrier Syst
1995;12(2-3):101-149
Evans DF, Pye G, Bramley R, Clark AG, Dyson TJ,
Hardcastle JD. Measurement of gastrointestinal pH
profiles in normal ambulant human subjects. Gut 1988.
Aug;29(8):1035-1041 10.1136/gut.29.8.1035
Bussemer T, Otto I, Bodmeier R. Pulsatile drug-delivery
systems. Crit Rev Ther Drug Carrier Syst 2001;18(5):433458
Ashord M, Fell JT, Attwood D, Sharma H, Woodhead P.
An evaluation of pectin as a carrier for drug targeting to
the colon. J Control Release 1993; 26: 213-220
.10.1016/0168-3659(93)90188-B
Fukui E, Miyamura N, Kobayashi M. An in vitro
investigation of the suitability of presscoated tablets with
hydroxypropylmethylcellulose
acetate
succinate
(HPMCAS) and hydrophobicn additives in the outer shell
for colon targeting. J Control Rel 200; 70:97-107.
Anil K. Philip. Colon Targeted Drug Delivery Systems: A
Review on Primary and Novel Approaches. OMJ. 2012;
70-78.
Cole E, Scott R, Connor A, Wilding I, Petereit HU,
Schminke C, Beckert T, Cade D. Enteric coated HPMC
capsules designed to achieve intestinal targeting.
International Journal of Pharmaceutics. 2002; 231: 83-95.
Cui N, Friend DR, Fedora RN. A budesonide prodrug
accelerates of colitis in rats. Gut. 1994; 35: 1439-1446
Scheline RR. Metabolism of foreign compounds by
gastrointestinal microorganisms. Pharmacol Rev 1973.
Dec;25(4):451-523
2687
Ghugarkar et al., IJPSR, 2015; Vol. 6(7): 2681-2688.
26. Basit A, Bloor J. Prespectives on colonic drug delivery,
Business briefing. Pharmtech 2003; 185-190.
27. Peters R, Kinget R. Film-forming polymers for colonic
drug deliver: Synthesis and physical and chemical
properties of methyl derivatives of Eudragit S. Int J Pharm
1993;94:125-134 .10.1016/0378-5173(93)90016-9
28. Huang SI, Bansleben DA, Knox JR. Biodegradable
polymers: Chymotrypsin degradation of low molecular
weight poly (ester-urea) containing phenylalanine. J Appl
Polym Sci 1979; 23: 429-437. 10.1002/app.1979.
070230212
29. Swift G. Biodegradable polymers in the environment: are
they really biodegradable. Proc ACS Div Poly Mat Sci
Eng 1992; 66:403-404.
30. Ratner BD, Gladhill KW, Horbett TA. Analysis of in vitro
enzymatic and oxidative degradation of polyurethanes. J
Biomed
Mater
Res
1988.
Jun;22(6):509-527
10.1002/jbm.820220607
31. Hergenrother RW, Wabewr HD, Cooper SL. The effect of
chain extenders and stabilizers on the in vivo stability of
polyurethanes.
J
Appl
Biomater
1992;3:17-22
.10.1002/jab.770030104
32. Park K, Shalaby WS, Park H, eds. Biodegradation In:
Biodegradable hydrogels for drug delivery, USA:
Technomic publishing company, 1993; 13-34
33. Ankita Patel, Dhruvita Patel, TruptiSolanki, Dr. P. D.
Bharadia, Mr. V.M. Pandya and Mr. D.A. Modi. Novel
Approaches for Colon Targeted Drug Delivery System.
IJPIs Journal of Pharmaceutics and Cosmetology. 2011;
1(5): 86-97.
34. Tarak Jayraj Mehta, A. D. Patel, Mukesh R. Patel, N. M.
Patel. Need of colon specific drug delivery: Review on
primary and novel approaches. Int. Journal of Pharma.
Research & Development. March 2011; 3(1): 134-153.
35. Watanabe S, Kawai H, Katsuma M, Fukui M. Colon
specific drug release system. U. S. Patent, 1998,
09/183339.
36. Takemura S, Watanabe S, Katsuma M, Fukui M. Human
gastrointestinal treatment study of a novel colon delivery
system (CODES) using scintography, Pro Int Sym Control
Rel Bioact Mat 2000, 27.
37. Katsuma M, Watanabe S, Takemura S, Sako K, Sawada T,
Masuda Y, et al. Scintigraphic evaluation of a novel colontargeted delivery system (CODES) in healthy volunteers. J
Pharm Sci 2004. May;93(5):1287-1299 10.1002/jps.20063
E-ISSN: 0975-8232; P-ISSN: 2320-5148
38. Yang L, Chu JS, Fix JA. Colon-specific drug delivery:
new approaches and in vitro/in vivo evaluation. Int J
Pharm
2002.
Mar;235(1-2):1-15
10.1016/S03785173(02)00004-2
39. Theeuwes F, Guittared G, Wong P. Delivery of drugs to
colon by oral dosage forms. U. S. Patent, 4904474
40. Swanson D, Barclay B, Wong P, Theeuwes F. Nifedipine
gastrointestinal therapeutics system. Am J Med
1987;8(6):3 .10.1016/0002-9343(87)90629-2
41. Philip AK, Pathak K. Osmotic flow through asymmetric
membrane: a means for controlled delivery of drugs with
varying solubility. AAPS PharmSciTech 2006;7(3):56
10.1208/pt070356
42. Philip AK, Pathak K. In situ-formed asymmetric
membrane capsule for osmotic release of poorly watersoluble drug. PDA J Pharm Sci Technol 2007. JanFeb;61(1):24-36
43. Philip AK, Pathak K, Shakya P. Asymmetric membrane in
membrane capsules: a means for achieving delayed and
osmotic flow of cefadroxil. Eur J Pharm Biopharm 2008.
Jun;69(2):658-666 10.1016/j.ejpb.2007.12.011
44. Philip AK, Pathak K. Wet process-induced phase-transited
drug delivery system: a means for achieving osmotic,
controlled, and level A IVIVC for poorly water-soluble
drug. Drug Dev Ind Pharm 2008. Jul;34(7):735-743
10.1080/03639040801911032
45. Yang L, Chu JS, Fix JA. Colon-specific drug delivery:
new approaches and in vitro/in vivo evaluation. Int J
Pharm 2002. Mar; 235(1-2):1-15 10.1016/S03785173(02)00004-2
46. Ahmed IS. Effect of simulated gastrointestinal conditions
on drug release from pectin/ethylcellulose as film coating
for drug delivery to the colon. Drug Dev Ind Pharm 2005.
May;31(4-5):465-470 10.1080/03639040500214704
47. Cole ET, Scott RA, Connor AL, Wilding IR, Petereit HU,
Schminke C, et al. Enteric coated HPMC capsules
designed to achieve intestinal targeting. Int J Pharm 2002.
Jan;231(1):83-95 10.1016/S0378-5173(01)00871-7
48. Hay DJ, Sharma H, Irving MH. Spread of steroid
containing foam after intrarectal administration. British
Medical Journal. 1979; 1: 1751-1753.
49. Mooter VG, Kinget R. Oral colon-specific drug delivery:
A review. Drug Deliv 1995;2:881-931
50. Hergenrother RW, Wabewr HD, Cooper SL. The effect of
chain extenders and stbilizers on the in vivo stability of
polyurethanes. Journal Appllied Biomat. 1992; 3: 17-22.
How to cite this article:
Ghugarkar P, Kulat P, Swain K and Suggala V and Shaik D: Colon Targeted Drug Delivery System: A Reveiw on Primary and Novel
Approaches. Int J Pharm Sci Res 2015; 6(7): 2681-88.doi: 10.13040/IJPSR.0975-8232.6(7).2681-88.
All 2013 are reserved by International Journal of Pharmaceutical Sciences and Research. This Journal licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License.
This article can be downloaded to ANDROID OS based mobile. Scan QR Code using Code/Bar Scanner from your mobile. (Scanners are available on Google
Playstore)
International Journal of Pharmaceutical Sciences and Research
2688
S-ar putea să vă placă și
- Bahan Analisis SalepDocument4 paginiBahan Analisis SalepmemeeeyyyÎncă nu există evaluări
- Caker EmulsiDocument2 paginiCaker EmulsimemeeeyyyÎncă nu există evaluări
- Bahan Analisis SalepDocument4 paginiBahan Analisis SalepmemeeeyyyÎncă nu există evaluări
- 2013 Article 835 Konsumsi TehDocument12 pagini2013 Article 835 Konsumsi TehmemeeeyyyÎncă nu există evaluări
- 2015 Article 1220Document9 pagini2015 Article 1220memeeeyyyÎncă nu există evaluări
- 2015 Article 37 Kontraasepsi OralDocument10 pagini2015 Article 37 Kontraasepsi OralmemeeeyyyÎncă nu există evaluări
- Lower XDDI risk with SOF vs SIM HCV therapyDocument12 paginiLower XDDI risk with SOF vs SIM HCV therapymemeeeyyyÎncă nu există evaluări
- Jurnal PubmedDocument23 paginiJurnal PubmedmemeeeyyyÎncă nu există evaluări
- Diary NG PangetDocument11 paginiDiary NG PangetmemeeeyyyÎncă nu există evaluări
- Form Penilaian PBL FARMAKOTERAPI 2 P 3Document10 paginiForm Penilaian PBL FARMAKOTERAPI 2 P 3memeeeyyyÎncă nu există evaluări
- Lower XDDI risk with SOF vs SIM HCV therapyDocument12 paginiLower XDDI risk with SOF vs SIM HCV therapymemeeeyyyÎncă nu există evaluări
- Stabilitas Obat AspirinDocument4 paginiStabilitas Obat AspirinIngrid DCÎncă nu există evaluări
- Daftar PustakaDocument3 paginiDaftar PustakamemeeeyyyÎncă nu există evaluări
- Print DressDocument1 paginăPrint DressmemeeeyyyÎncă nu există evaluări
- Kurva Berat Anak Timbangan Dan RPMDocument2 paginiKurva Berat Anak Timbangan Dan RPMmemeeeyyyÎncă nu există evaluări
- Kurva Berat Anak Timbangan Dan RPMDocument2 paginiKurva Berat Anak Timbangan Dan RPMmemeeeyyyÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Division of Davao del Norte Unified Test in Secondary Science Grade 10Document6 paginiDivision of Davao del Norte Unified Test in Secondary Science Grade 10Agustin L. IdausosÎncă nu există evaluări
- Worksheet Biological MoleculesDocument5 paginiWorksheet Biological MoleculesNabeeha RaheelÎncă nu există evaluări
- Main Functions of ProteinDocument3 paginiMain Functions of ProteinsweetwaffleÎncă nu există evaluări
- Lesson 2 - CarbohydratesDocument30 paginiLesson 2 - CarbohydratesWycliffe AsmanÎncă nu există evaluări
- Edexcel IAL Biology Unit 1 Topic 1 - Molecules, Transport and HealthDocument40 paginiEdexcel IAL Biology Unit 1 Topic 1 - Molecules, Transport and HealthEshalÎncă nu există evaluări
- SCIENCE-10 Q4 MOD3 Biomolecules-Carbohydrates-Lipids BookletDocument12 paginiSCIENCE-10 Q4 MOD3 Biomolecules-Carbohydrates-Lipids BookletRetep Aren100% (2)
- Module 2 - Biochemistry (2) - 10Document2 paginiModule 2 - Biochemistry (2) - 10Amrah RcmnÎncă nu există evaluări
- Carbs: Energy Storage, Structural Roles and MoreDocument75 paginiCarbs: Energy Storage, Structural Roles and MoreRahul SharmaÎncă nu există evaluări
- Fructans of Jerusalem ArtichokesDocument7 paginiFructans of Jerusalem ArtichokesAsmaa OtifyÎncă nu există evaluări
- Molecules of Life: Carbs, Lipids, Proteins & EnzymesDocument102 paginiMolecules of Life: Carbs, Lipids, Proteins & Enzymeskavya nandhiÎncă nu există evaluări
- Biotech Reviewer PDFDocument31 paginiBiotech Reviewer PDFGerald LimÎncă nu există evaluări
- Quizlet Chapter 5Document9 paginiQuizlet Chapter 5EUNAH LimÎncă nu există evaluări
- Bio 101 Study Guide Test 1Document8 paginiBio 101 Study Guide Test 1mattyg35Încă nu există evaluări
- BCH 202 Practical Note on General Biochemistry Laboratory GuidelinesDocument40 paginiBCH 202 Practical Note on General Biochemistry Laboratory GuidelinesEmmanuel LangatÎncă nu există evaluări
- Quiz 1 - MacromoleculesDocument2 paginiQuiz 1 - MacromoleculesRosielyn Fano CatubigÎncă nu există evaluări
- 2017JGLEPS119 19FirstAuthorNon Indexed PDFDocument12 pagini2017JGLEPS119 19FirstAuthorNon Indexed PDFSony GeorgeÎncă nu există evaluări
- 02 Carbohydrates BiochemDocument7 pagini02 Carbohydrates BiochemtabudlongyazminezekielleÎncă nu există evaluări
- Carbohydrates Handout PDFDocument15 paginiCarbohydrates Handout PDFAra AlibasaÎncă nu există evaluări
- Degumming Methods For Bast-FibersDocument16 paginiDegumming Methods For Bast-FibersNHÎncă nu există evaluări
- Exam 2Document4 paginiExam 2reyna alilingÎncă nu există evaluări
- Biochemistry of Carbohydrates PDFDocument7 paginiBiochemistry of Carbohydrates PDFAshley Beatriz Pascual100% (1)
- Instant Download Ebook PDF Biological Science 2nd Canadian Edition PDF ScribdDocument41 paginiInstant Download Ebook PDF Biological Science 2nd Canadian Edition PDF Scribdmatthew.weimar370100% (37)
- Biological MoleculesDocument6 paginiBiological MoleculessanaullahÎncă nu există evaluări
- Recent Developments in Polysaccharide-Based Materials Used As Adsorbents in Wastewater TreatmentDocument33 paginiRecent Developments in Polysaccharide-Based Materials Used As Adsorbents in Wastewater TreatmentThomas SantosaÎncă nu există evaluări
- Bio Topic 4 Notes PDFDocument11 paginiBio Topic 4 Notes PDFdgfhjÎncă nu există evaluări
- DAT Bootcamp High-Yield Biology NotesDocument135 paginiDAT Bootcamp High-Yield Biology NotesAliya RizviÎncă nu există evaluări
- Botnay Notes Class 11Document138 paginiBotnay Notes Class 11Suresh chand100% (1)
- CarbohydratesDocument44 paginiCarbohydratesApril Jean Cahoy100% (3)
- BIOL BCHM 111 BiomoleculesDocument49 paginiBIOL BCHM 111 BiomoleculeshavenÎncă nu există evaluări
- Unit 14 BiomoleculesDocument3 paginiUnit 14 BiomoleculesDeepesh kumarÎncă nu există evaluări