Documente Academic
Documente Profesional
Documente Cultură
Syed-Iqbal 2005 Evaluation ELISA HIV Detection
Încărcat de
Maya RustamDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Syed-Iqbal 2005 Evaluation ELISA HIV Detection
Încărcat de
Maya RustamDrepturi de autor:
Formate disponibile
CLINICAL AND DIAGNOSTIC LABORATORY IMMUNOLOGY, Dec. 2005, p.
14251428
1071-412X/05/$08.000 doi:10.1128/CDLI.12.12.14251428.2005
Copyright 2005, American Society for Microbiology. All Rights Reserved.
Vol. 12, No. 12
Evaluation and Diagnostic Usefulness of Domestic and Imported
Enzyme-Linked Immunosorbent Assays for Detection of Human
Immunodeficiency Virus Type 1 Antibody in India
H. Syed Iqbal, Suniti Solomon, K. G. Murugavel, Sunil Suhas Solomon, and P. Balakrishnan*
VHS-YRG CARE Infectious Diseases Laboratory, Centre for AIDS Research and Education,
Voluntary Health Services Hospital Campus, Taramani, Chennai, India
Received 28 July 2005/Returned for modification 12 August 2005/Accepted 3 October 2005
Diagnosis of human immunodeficiency virus (HIV) infection is important for patient management and
prevention of new infections. The number of test kits available for the detection of HIV antibodies is unprecedented. In order to identify appropriate test kits, we evaluated a variety of commercial kits manufactured
abroad as well as in India. The plasma and serum specimens (n 264) were collected from individuals
attending the Voluntary Counseling and Testing Centre at the YRG Centre for AIDS and Education. The
specimens were used to evaluate six commercially available HIV test kits: Enzaids HIV 12, HIV-CheX, Murex
HIV-1.2.0, Genscreen HIV 1/2 version 2, Vironostika HIV Uni-Form II Ag/Ab, and CombAids RS Advantage.
High sensitivities and specificities (>99%) were observed for the Enzaids, Murex, Vironostika, and CombAids
assays. HIV-CheX showed the highest number of false-positive and false-negative results. The Genscreen test
also gave many false positives. The study indicated that the Enzaids, Murex, and Vironostika enzyme-linked
immunosorbent assay kits and the CombAids RS Advantage rapid assay could be used to achieve acceptable
results for the detection of HIV antibodies. A combination of two tests is recommended to optimize the
efficiency of HIV antibody testing algorithms, especially when evaluation with an HIV Western blot confirmatory test is not possible.
available diagnostic ELISA kits, and also a rapid test kit, for
their performance in diagnosing HIV infection.
Infection with human immunodeficiency virus (HIV) has
become pandemic since its first documentation in 1981 and is
a major public health concern (11). HIV antibody testing is
critical for the diagnosis and counseling of HIV-infected persons, the monitoring of trends in HIV prevalence, and the
evaluation of the effectiveness of HIV prevention programs (5,
12). An unprecedented number of tests for the detection of
HIV antibodies are available. In some kits, improved sensitivity is frequently accompanied by a decreased specificity. This
has been of particular concern with the introduction of test kits
that detect all isotypes of antibodies, such as those based on
antibody capture by antigens on a solid phase with labeled
antigens as the detecting reagents (4, 8).
In resource-poor developing countries, the surveillance and
diagnosis of HIV infection are major challenges (15). The
conventional algorithm for HIV diagnostic testing consists of
screening with enzyme immunoassays followed by confirmation with a Western blot test. Moreover, a double enzymelinked immunosorbent assay (ELISA) without Western blotting has been accepted as the customary screening assay for
HIV infection (18). Because of the high cost of the Western
blot test, it has not been affordable in a number of laboratories
in developing countries (1). Rapid screening for HIV infection
performed on-site with tests that do not require expensive
laboratory infrastructure or highly skilled personnel helps with
the diagnoses of patients in emergencies (13). The present
study has been designed to evaluate five different commercially
MATERIALS AND METHODS
This study was carried out at the Y. R. Gaitonde Centre for AIDS Research
and Education (YRG CARE) in Chennai, India; it is a referral center for
voluntary counseling and testing (VCT) in South India. A total of 264 specimens
(plasma and serum) collected from VCT clients were tested using various commercial HIV ELISA kits, and the positive specimens were confirmed by Western
blot analysis (Genetic Systems HIV-1 Western blot; Bio-Rad Laboratories, Redmond, WA). The following commercially available ELISA kits were employed in
this study: Enzaids HIV 12 (Span Diagnostics Ltd., Surat, India), HIV-CheX
(Xcyton Diagnostics Ltd., Bangalore, India), Murex HIV-1.2.0 (Murex Biotech
Limited, Dartford, United Kingdom), Genscreen HIV 1/2 version 2 (Bio-Rad
Laboratories, France), and Vironostika HIV Uni-Form II Ag/Ab (BioMerieux,
The Netherlands). Along with these, a rapid test kit, CombAids RS Advantage
(Span Diagnostics Ltd., Surat, India), was also evaluated. A double-blind format
was adopted in order to conceal patient information from the testing personnel.
One staff member generated duplicate numbers for specimens at the specimen
processing section; a second staff member generated plate maps and performed
the tests. Finally, the results were analyzed by both personnel. The kits were
stored under cold conditions at all times, and all of the tests were performed
according to the manufacturers instructions. An optical density higher than the
cutoff value, obtained per the manufacturers instructions, was considered a
positive result, and an optical density lower than the cutoff value was considered
a negative result. Sensitivity, specificity, predictive values, and efficiency were
calculated using the Western blot results as the standard. A Western blot was
considered positive for HIV type 1 (HIV-1) if any two of the following viral
proteins were present: p24, gp41, and gp120/160 (per the manufacturers instructions). We have calculated the performance characteristics of all the kits using
formulae given elsewhere (17).
The kits were also evaluated with the following known specimens: 100 Western
blot-confirmed HIV-positive specimens (Genetic Systems HIV-1; Bio-Rad Laboratories), 100 HIV-negative specimens (U.S. FDA-approved ELISA; Genetic
Systems HIV-1/2 PLUS O), 4 HIV-II-positive specimens (confirmed by NEW
LAV BLOT II; Bio-Rad Laboratories, France), and 9 in-house seroconversion
specimens. Six specimens from Boston Biomedica, Inc. (BBI panel), Boston,
Mass., were tested with only two kits (Enzaids and Murex) due to insufficient
* Corresponding author. Mailing address: YRG Centre for AIDS Research and Education, Voluntary Health Services Campus, Taramani,
Chennai 600 113, India. Phone: 91-44-22542929. Fax: 91-44-22542939.
E-mail: bala@yrgcare.org.
1425
1426
IQBAL ET AL.
CLIN. DIAGN. LAB. IMMUNOL.
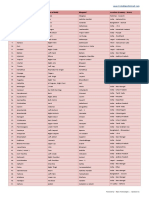
TABLE 1. Performance of kits with known specimens
No. of specimens identified correctly by:
Specimen (total no.)
Enzaids Murex Genscreen
Western blot confirmed,
HIV-I positive (n 100)
HIV-I negative, in FDAapproved ELISA (n 100)
HIV- Comb
CheX Aids
100
100
100
89
100
100
100
100
100
100
BBI panel (n 6)
4a
ND b
ND
ND
NEW LAV BLOT II
confirmed, HIV-II positive
(n 4)
In-house seroconversion
panel (n 9)
a
b
The two initial specimens, from 0 and 9 days, were not detected.
ND, not done.
specimen volume. Of the six BBI panel specimens, four were 0, 9, 11, and 20 days
old, and the others were known positive specimens for HIV-2 and HIV-1 group
O, respectively. We were unable to include the Vironostika kit due to the
unavailability of funding.
RESULTS
As far as the known specimens are concerned (Table 1), all
of the specimens which contained antibodies to HIV-1 were
correctly identified by all of the kits except HIV-CheX, which
was unable to detect 11 HIV Western blot-positive specimens,
thus resulting in reduced sensitivity. All of the kits correctly
identified negative specimens. All of the nine in-house sero-
conversion specimens were identified as positive by all of the
kits except HIV-CheX, which recorded two specimens as negative. All of the in-house specimens of HIV-2 were identified
as positive by all of the kits. From the BBI seroconversion
panel, Murex detected all six specimens, while Enzaids did not
detect the two initial specimens (i.e., 0 and 9 days). Both kits
showed positive results for the HIV-2 and HIV-1 group O
specimens from the BBI panel.
The results of the 264 VCT specimens used for the evaluation of commercially available kits for the diagnosis of HIV
infection are summarized in Table 2. It is clearly evident that
the Enzaids, Murex, Vironostika, and CombAids test kits gave
uniform results with good sensitivity and specificity. All four of
these kits exhibited one false positive (Table 3). The results of
the HIV-CheX and Genscreen tests were not satisfactory due
to their poor performance characteristics. Of the 264 specimens tested by Western blotting, one was indeterminate in
exhibiting the p24 band, positive in the Murex kit, and negative
in all of the other kits, and this specimen was removed from the
analysis due to the unavailability of PCR results. A total of 19
specimens were found to be discordant with the Western blot
results, which can be considered an inherent limitation of the
respective test kits (Table 3). Many false positives and false
negatives were observed in the Genscreen and HIV-CheX
tests, respectively.
DISCUSSION
In the present study, we have evaluated the performance of
two domestic and three imported HIV ELISA kits. We have
also included a domestic rapid HIV kit with the ELISA kits.
TABLE 2. Performance characteristic of six HIV antibody tests used for comparative evaluation
Antibody test
and result
Western blot
results a
POS
NEG
Enzaids HIV 12
Positive
Negative
127
0
1
135
Murex HIV-1.2.0
Positive
Negative
127
0
1
135
HIV-CheX
Positive
Negative
123
4
5
131
Vironostika
Positive
Negative
127
0
1
135
Genscreen HIV 1/2
Positive
Negative
127
0
7
129
CombAids
Positive
Negative
127
0
1
135
Performance characteristic result (%)b
Sensitivity (95% CI)
Specificity (95% CI)
PPV
NPV
Efficiency
100 (100100)
99.3 (97.8100)
99.2
100
99.6
100 (100100)
99.3 (97.8100)
99.2
100
99.6
96.3 (93.199.6)
96.1
97
96.5
100 (100100)
99.3 (97.8100)
99.2
100
99.6
100 (100100)
94.9 (91.098.7)
94.8
100
97.3
100 (100100)
99.3 (97.8100)
99.2
100
99.6
96.9 (93.999.8)
a
Total number of samples, 264 (one sample was removed from the analysis; see text for the details). POS, positive; NEG, negative. Values shown are numbers of
samples with indicated result.
b
CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value.
VOL. 12, 2005
EVALUATION OF HIV ELISA KIT
1427
TABLE 3. Samples found to be discordant with Western blot results
Results with a:
Sample
Western blot
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
a
b
TN
TP
TP
TN
TN
TP
TN
TN
TN
TP
TN
TN
TN
TN
TN
TN
TN
TN
Enzaids
Murex
Genscreen
HIV-CheX
CombAids
Vironostika
TN
TN
TP
TP
TN
TN
TP
TN
TN
TN
TP
TN
TN
TN
FP
TN
TN
TN
TN
NK
TN
TP
TP
TN
TN
TP
TN
TN
TN
TP
FP
TN
TN
TN
TN
TN
TN
TN
TN
FP
TP
TP
TN
TN
TP
TN
TN
FP
TP
TN
TN
FP
FP
FP
FP
FP
TN
TN
TN
FN
FN
FP
FP
FN
FP
FP
FP
FN
TN
TN
TN
TN
TN
TN
TN
TN
TN
TN
TP
TP
TN
TN
TP
TN
TN
TN
TP
TN
TN
TN
TN
TN
TN
TN
FP
TN
TN
TP
TP
TN
TN
TP
TN
TN
TN
TP
TN
FP
TN
TN
TN
TN
TN
TN
TP, true positive; FP, false positive; FN, false negative; TN, true negative; NK, status unknown.
Sample was indeterminate with p24 and was removed due to the unavailability of PCR results.
Poor performance was seen with the Genscreen and HIVCheX kits. The Murex test detected antibodies in all of the
specimens in the BBI panel, and this result coincided with
those of other studies (2, 7). Concordant results were obtained
with the in-house seroconversion specimens with all of the kits
except HIV-CheX. In other studies, the Genscreen kit demonstrated worse performance characteristics than other kits, as
it could not detect either HIV-1 group M, subtypes A and B, or
HIV-1 group O antigens in the range tested (10 to 125 pg/ml)
(7, 19, 20). This result matches the poor performance shown in
our study, as many false positives were detected.
Even though Western blot analysis is a confirmatory test (3,
9), the combination of two or more antibody screening assays,
which use different antigenic bases, may be more sensitive and
specific than Western blotting (3, 810, 16, 18). According to
our study, for double ELISA combinations, the recommended
kits are the Enzaids, Murex, and Vironostika kits. Using the
HIV-CheX or Genscreen kit with any other kit would be an
ineffective combination. One notable issue here is the discordance between the results of two assays (6, 8, 14), which can be
resolved if better kits are used. Hence, this kind of evaluation
gains importance for determining a better choice of kits. It is
also noted that the sera of up to 40% of uninfected persons
gave indeterminate Western blot results (3, 8, 9).
As far as patients are concerned, discordant results may have
the consequence of inducing psychological stress while the
patient is waiting for confirmatory testing and may also result
in additional expenses. False-positive results could cause considerable unnecessary anxiety and mental trauma for the patients. This outcome may also lead to the unnecessary waste of
valuable blood in blood banks. In this evaluation, we found a
large number of false positives with the Genscreen kit. The
damage caused by false-negative test results is also a serious
problem, as a person who is falsely tested to be negative may
continue the transmission of the virus. The possibility of transfusing blood after such a false-negative test also underlines the
need for high-quality, sensitive ELISAs. In this evaluation, we
found false-negative results with the HIV-CheX kit, leaving
the population under the threat of silent HIV transmission.
Even though this study did not concentrate on a rapid HIV
detection assay, we included the CombAids rapid assay in
order to evaluate its comparative performance. The performance of this rapid assay was found to be comparable to that
of ELISA in terms of sensitivity and specificity. Therefore, the
CombAids assay can be a useful tool for the prompt screening
of patient specimens at point-of-care facilities, reference laboratories (15), prenatal clinics, and emergency rooms located
in regions where laboratorial infrastructure is either not
present or not well outfitted. We do not have the clinical
characteristics of the patients, such as concomitant infections
or use of chemotherapeutic or recreational drugs, to compare
with our results. Due to insufficient quantities of specimens, we
used the seroconversion panel only for the Murex and Enzaids
tests. One test specimen, found to be positive by only the
Murex HIV-1.2.0 test, was indeterminate by Western blotting
with the p24 band. Due to the lack of availability of PCR
assay and/or follow-up specimen results for this individual,
we were unable to resolve the conflicting serology for this
specimen; hence, it was removed from the analysis. Also due
to unavailability of funds, we did not use the Vironostika kit
to test known specimens. These are some of the limitations
of this study.
To conclude, as demonstrated by the data presented in this
report, the domestic Enzaids kit exhibits a high level of performance that equals that of the imported Murex and Vironostika kits. The same performance was also observed with the
domestic CombAids rapid assay, while poor performance was
observed with the domestic HIV-CheX kit and the imported
Genscreen kit. The other advantages of the Enzaids kit are a
short run time, comparative cost-effectiveness, and incubation
of samples at room temperature. Hence, the domestically developed Enzaids kit is sufficiently accurate to screen for HIV-1
1428
IQBAL ET AL.
CLIN. DIAGN. LAB. IMMUNOL.
infection and can be widely used in India where people cannot
afford to test with imported kits.
10.
ACKNOWLEDGMENTS
11.
We thank Edward Livant, QA/QC Coordinator, for reviewing the
manuscript and for suggestions and the laboratory staff of YRG CARE
for their assistance.
12.
REFERENCES
1. Asihene, P. J., R. L. Kline, M. W. Moss, A. V. Carella, and T. C. Quinn. 1994.
Evaluation of rapid test for detection of antibody to human immunodeficiency virus type 1 and type 2. J. Clin. Microbiol. 32:13411342.
2. Bu
rgisser, P., F. Simon, M. Wernli, T. Wu
st, M.-F. Beya, and P. C. Frei.
1996. Multicenter evaluation of new double-antigen sandwich enzyme immunoassay for measurement of anti-human immunodeficiency virus type 1
and type 2 antibodies. J. Clin. Microbiol. 34:634637.
3. Genesca, J., J. W. K. Shih, B. W. Jett, I. K. Hewlett, J. S. Epstein, and H. J.
Alter. 1989. What do Western blot indeterminate patterns for human immunodeficiency virus mean in EIA-negative blood donors? Lancet ii:1023
1025.
4. Gonzalez, L., R. W. Boyle, M. Zhang, J. Castillo, S. Whittier, P. Della-Latta,
L. M. Clarke, J. R. George, X. Fang, J. G. Wang, B. Hosein, and C. Y. Wang.
1997. Synthetic-peptide-based enzyme-linked immunosorbent assay for
screening human serum or plasma for antibodies to human immunodeficiency virus type 1 and type 2. Clin. Diagn. Lab. Immunol. 4:598603.
5. Kannangai, R., S. Ramalingam, S. Pradeepkumar, K. Damodharan, and G.
Sridharan. 2000. Hospital-based evaluation of two rapid human immunodeficiency virus antibody screening tests. J. Clin. Microbiol. 38:34453447.
6. Lin, H. J., L. E. Myers, B. Yen-Lieberman, F. B. Hollinger, D. Henrard, C. J.
Hooper, R. Kokka, S. Kwok, S. Rasheed, M. Vahey, M. A. Winters, L. J.
McQuay, P. L. Nara, P. Reichelderfer, R. W. Coombs, and J. B. Jackson.
1994. Multicenter evaluation of quantification methods for plasma human
immunodeficiency virus type 1 RNA. J. Infect. Dis. 170:553562.
7. Ly, T. D., L. Martin, D. Daghefal, A. Sandridge, D. West, R. Bristow, L.
Chalouas, X. Qiu, S. C. Lou, J. C. Hunt, G. Schochetman, and S. G. Devare.
2001. Seven human immunodeficiency virus (HIV) antigen-antibody combination assays: evaluation of HIV seroconversion sensitivity and subtype
detection. J. Clin. Microbiol. 39:31223128.
8. Matter, L., and D. Germann. 1995. Detection of human immunodeficiency
virus (HIV) type 1 antibodies by new automated microparticle enzyme immunoassay for HIV types 1 and 2. J. Clin. Microbiol. 33:23382341.
9. Midthun, K., L. Garrison, M. L. Clements, H. Farzadegan, B. Fernie, T.
Quinn, and the NIAID AIDS Vaccine Clinical Trials Network. 1990. Fre-
13.
14.
15.
16.
17.
18.
19.
20.
quency of indeterminate Western blot tests in healthy adults at low risk for
human immunodeficiency virus infection. J. Infect. Dis. 162:13791382.
Mortimer, P. P. 1991. The fallibility of HIV Western blot. Lancet 337:286
287.
National AIDS Control Organization. 2004. An overview of the spread and
prevalence of HIV/AIDS in India. NACO, Ministry of Health and Family
Welfare, Government of India. [Online.] http://www.nacoonline.org/facts
_overview.htm.
Nkengasong, J. N., C. Maurice, S. Koblavi, M. Kalou, D. Yavo, M. Maran,
C. Bile, K. Nguessan, J. Kouadio, S. Bony, S. Z. Wiktor, and A. E. Greenberg. 1999. Evaluation of HIV serial and parallel serologic testing algorithms
in Abidjan, Co
te dIvoire. AIDS 13:109117.
Palmer, C. J., J. M. Dubon, E. Koenig, E. Perez, A. Ager, D. Jayaweera, R. R.
Cuadrado, A. Rivera, A. Rubido, and D. A. Palmer. 1999. Field evaluation of
the Determine rapid human immunodeficiency virus diagnostic test in Honduras and the Dominican Republic. J. Clin. Microbiol. 37:36983700.
Pyra, H., J. Boni, and J. Schupbach. 1994. Ultrasensitive retrovirus detection
by a reverse transcriptase assay based on product enhancement. Proc. Natl.
Acad. Sci. USA 91:15441548.
Ribeiro-Rodrigues, R., L. F. da Silva Pinto Neto, C. B. Cunha, V. P. Cabral,
and R. Dietze. 2003. Performance characteristics of a rapid new immunochromatographic test for detection of antibodies to human immunodeficiency virus. Clin. Diagn. Lab. Immunol. 10:303307.
Sato, P. A., W. J. Maskill, H. Tamashiro, and D. L. Heymann. 1994. Strategies for laboratory HIV testing: an examination of alternative approaches
not requiring Western blot. Bull. WHO 72:129134.
Schochetman, G., and J. R. George. 1992. Serodiagnosis of HIV infection,
p. 6667. In G. Schochetman and J. R. George (ed.), AIDS testing: methodology and management issues. Springer-Verlag, New York, N.Y.
UNAIDS/WHO Working Group on Global HIV/AIDS/STI Surveillance. 2001.
Guidelines for using HIV testing technologies in surveillance: selection, evaluation, and implementation. UNAIDS and WHO HIV testing strategies. Strategy II. WHO/CDS/CSR/EDC/2001.16 UNAIDS/01.22E:23 [Online.] http://www
.who.int/hiv/pub/surveillance/en/guidelinesforUsingHIVTestingTechs_E.pdf.
Weber, B., A. Berger, H. Rabenau, and H. W. Doerr. 2002. Evaluation of a
new combined antigen and antibody human immunodeficiency virus screening assay, VIDAS HIV DUO Ultra. J. Clin. Microbiol. 40:14201426.
Weber, B., L. Gu
rtler, R. Thorstensson, U. Michl, A. Mu
hlbacher, P. Bu
rgisser, R. Villaescusa, A. Eiras, C. Gabriel, H. Stekel, S. Tanprasert, S. Oota,
M.-J. Silvestre, C. Marques, M. Ladeira, H. Rabenau, A. Berger, U. Schmitt,
and W. Melchior. 2002. Multicenter evaluation of a new automated fourthgeneration human immunodeficiency virus screening assay with a sensitive
antigen detection module and high specificity. J. Clin. Microbiol. 40:1938
1946.
S-ar putea să vă placă și
- SARS-CoV-2 Viral Outbreak Investigation: Laboratory Perspective: Clinical Updates in COVID-19De la EverandSARS-CoV-2 Viral Outbreak Investigation: Laboratory Perspective: Clinical Updates in COVID-19Evaluare: 3 din 5 stele3/5 (1)
- UK NHS Improvement in HIV AssaysDocument13 paginiUK NHS Improvement in HIV AssaysChris ThomasÎncă nu există evaluări
- Rapid On-site Evaluation (ROSE): A Practical GuideDe la EverandRapid On-site Evaluation (ROSE): A Practical GuideGuoping CaiÎncă nu există evaluări
- HIV Diagnostic Testing 30 Years of EvolutionDocument5 paginiHIV Diagnostic Testing 30 Years of EvolutionYashinta SetyandaÎncă nu există evaluări
- Molecular and Antibody Point-Of-Care Tests To Support The Screening, Diagnosis and Monitoring of COVID-19Document12 paginiMolecular and Antibody Point-Of-Care Tests To Support The Screening, Diagnosis and Monitoring of COVID-19vicndubÎncă nu există evaluări
- Jurnal Kulkel HemDocument5 paginiJurnal Kulkel HemAnonymous PrskyT0co6Încă nu există evaluări
- JCM 43 8 4194-4196 2005Document3 paginiJCM 43 8 4194-4196 2005Sumesh ShresthaÎncă nu există evaluări
- Field Evaluation of Four Rapid Tests For Diagnosis of HIV Infection in PanamaDocument3 paginiField Evaluation of Four Rapid Tests For Diagnosis of HIV Infection in PanamaYashinta SetyandaÎncă nu există evaluări
- ID - HIV 1 1 WesternBlotBrief - 62015Document4 paginiID - HIV 1 1 WesternBlotBrief - 62015Eleanor LouanaÎncă nu există evaluări
- SARS-CoV-2 VLPS Specifically Detect Humoral Immune ReactionsDocument10 paginiSARS-CoV-2 VLPS Specifically Detect Humoral Immune ReactionsAnna Carolyne VidalÎncă nu există evaluări
- Jurnal 1Document7 paginiJurnal 1Nur Alifah Dina SÎncă nu există evaluări
- Infant HIV TestsDocument5 paginiInfant HIV TestsProf Rakesh SharmaÎncă nu există evaluări
- Increase in False-Positive Fourth-Generation Human Immunodeficiency Virus Tests in Patients With Coronavirus Disease 2019Document5 paginiIncrease in False-Positive Fourth-Generation Human Immunodeficiency Virus Tests in Patients With Coronavirus Disease 2019emmanuel AndemÎncă nu există evaluări
- Molecular Approaches To Diagnosing and Managing Infectious Diseases: Practicality and CostsDocument7 paginiMolecular Approaches To Diagnosing and Managing Infectious Diseases: Practicality and CostsIsrar NasirÎncă nu există evaluări
- Understanding Antigen Tests and Results ENG FinalDocument4 paginiUnderstanding Antigen Tests and Results ENG FinalAna CatarinaÎncă nu există evaluări
- Manuscript 4Document4 paginiManuscript 4maryÎncă nu există evaluări
- ASM Web Protocol Serology 062220 FINALDocument11 paginiASM Web Protocol Serology 062220 FINALChristian Saldaña DonayreÎncă nu există evaluări
- Diagnosis Brucella TurkeyDocument5 paginiDiagnosis Brucella TurkeyJoshua SmithÎncă nu există evaluări
- Pak J Med Res 2012 51 3 72 76Document5 paginiPak J Med Res 2012 51 3 72 76uzairÎncă nu există evaluări
- Accuracy Evaluation of Hiv Rapid Tests RDocument14 paginiAccuracy Evaluation of Hiv Rapid Tests RĐạt Trần TiếnÎncă nu există evaluări
- Seminar 22nd AugDocument27 paginiSeminar 22nd AugjohndemoÎncă nu există evaluări
- Comparison of The HIV 1 Specific Immunoglobulin GDocument5 paginiComparison of The HIV 1 Specific Immunoglobulin GAlex MorwabeÎncă nu există evaluări
- Appendix 14 YZR-011CG25 YZR-011CG25 Clinical Validation ReportDocument23 paginiAppendix 14 YZR-011CG25 YZR-011CG25 Clinical Validation ReportMedical LepuÎncă nu există evaluări
- Performance Verification of Anti-Sars-Cov-2-Specific Antibody Detection by Using Four Chemiluminescence Immunoassay SystemsDocument6 paginiPerformance Verification of Anti-Sars-Cov-2-Specific Antibody Detection by Using Four Chemiluminescence Immunoassay SystemsadnanÎncă nu există evaluări
- Assessingthesensitivityandspecificityoffirstresponse HIVtestkitDocument9 paginiAssessingthesensitivityandspecificityoffirstresponse HIVtestkitNurhasan Agung PrabowoÎncă nu există evaluări
- Potential For False Positive HIV Test Results With The Serial Rapid HIV Testing AlgorithmDocument4 paginiPotential For False Positive HIV Test Results With The Serial Rapid HIV Testing AlgorithmNeway GetahunÎncă nu există evaluări
- Retrospective Audit of The Widal Test For Diagnosis of Typhoid Fever in Pediatric Patients in An Endemic RegionDocument4 paginiRetrospective Audit of The Widal Test For Diagnosis of Typhoid Fever in Pediatric Patients in An Endemic RegionKiagus Mahendra EffendyÎncă nu există evaluări
- Serologic Diagnosis of Tuberculosis Using A Simple Commercial Multiantigen AssayDocument6 paginiSerologic Diagnosis of Tuberculosis Using A Simple Commercial Multiantigen AssayTanveerÎncă nu există evaluări
- Advances of Basic Sciences - Diagnostic & Prognostic ApplicationDocument38 paginiAdvances of Basic Sciences - Diagnostic & Prognostic ApplicationKamini WaliaÎncă nu există evaluări
- Gueudin2016 PDFDocument21 paginiGueudin2016 PDFibnuÎncă nu există evaluări
- 1 Clinical Evaluation of BioPlex 2200 HIV AgAb, An Automated Screening Method Providing Discrete Detection of HIV1 p24 Antigen, HIV1 Antibody, and HIV2 Antibody.Document5 pagini1 Clinical Evaluation of BioPlex 2200 HIV AgAb, An Automated Screening Method Providing Discrete Detection of HIV1 p24 Antigen, HIV1 Antibody, and HIV2 Antibody.Adrilupiss ArroyoÎncă nu există evaluări
- Out Comes of Improved TechniquesDocument6 paginiOut Comes of Improved Techniquesnydiacastillom2268Încă nu există evaluări
- Enhanced Virome Sequencing Using Targeted Sequence Capture: Wylie - T@kids - Wustl.eduDocument34 paginiEnhanced Virome Sequencing Using Targeted Sequence Capture: Wylie - T@kids - Wustl.eduAnh H NguyenÎncă nu există evaluări
- 2 Comparacion BD Phoenix Vitek MicroscanDocument10 pagini2 Comparacion BD Phoenix Vitek MicroscanBenjamin MendozaÎncă nu există evaluări
- Bulletin of The World Health OrganizationDocument11 paginiBulletin of The World Health OrganizationJohn LewandowskiÎncă nu există evaluări
- Rapid Diagnostic Tests Versus RT-PCR For Ebola Virus Infections: Systematic Review and Meta-AnalysisDocument24 paginiRapid Diagnostic Tests Versus RT-PCR For Ebola Virus Infections: Systematic Review and Meta-Analysissri wahyuniÎncă nu există evaluări
- Dried Tube Specimens A Simple and Cost-Effective MDocument7 paginiDried Tube Specimens A Simple and Cost-Effective MFrank JoneÎncă nu există evaluări
- Theoretical Model Basis of Clinical Guidelines For Ebola Viral Infection Containment in Lagos NigeriaDocument27 paginiTheoretical Model Basis of Clinical Guidelines For Ebola Viral Infection Containment in Lagos NigeriaRiya CassendraÎncă nu există evaluări
- Tubex TestDocument9 paginiTubex TestdnnivÎncă nu există evaluări
- Laboratory Diagnosis of HIV Infection: Kamal KishoreDocument7 paginiLaboratory Diagnosis of HIV Infection: Kamal KishoreanastasialantangÎncă nu există evaluări
- Clinical Microbiology Newsletter: Genexpert Testing: Applications For Clinical Microbiology, Part IDocument5 paginiClinical Microbiology Newsletter: Genexpert Testing: Applications For Clinical Microbiology, Part ImagicianchemistÎncă nu există evaluări
- Anti HafDocument7 paginiAnti Hafzenita avisenaÎncă nu există evaluări
- ArchitechDocument5 paginiArchitechERIE YUWITA SARIÎncă nu există evaluări
- Jurnal HibridisasiDocument12 paginiJurnal HibridisasiNurfanida Natasya mÎncă nu există evaluări
- Can A Rapid Test Justify As A Screening Test For Syphilis in Hard-To-Reach Population? Its EvaluationDocument3 paginiCan A Rapid Test Justify As A Screening Test For Syphilis in Hard-To-Reach Population? Its EvaluationInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Caracterizacion NigeriaDocument9 paginiCaracterizacion NigeriaAndrea LunaÎncă nu există evaluări
- Comparison Between Elisa and Ict Techniques For The Detection of AntiDocument6 paginiComparison Between Elisa and Ict Techniques For The Detection of Antimariam zameerÎncă nu există evaluări
- Basic Problems of Serological Laboratory DiagnosisDocument37 paginiBasic Problems of Serological Laboratory DiagnosisSuzan MatarÎncă nu există evaluări
- 4th Generation HIV TestingDocument31 pagini4th Generation HIV TestingSC SCÎncă nu există evaluări
- Serological Testing of HIVDocument4 paginiSerological Testing of HIVhamody662002Încă nu există evaluări
- Annex 5.3 PICO 1 - How To Test (HBV) Diagnostic Accuracy of Tests To Detect Hepatitis B Surface Antigen: A Meta-Analysis and Review of The LiteratureDocument78 paginiAnnex 5.3 PICO 1 - How To Test (HBV) Diagnostic Accuracy of Tests To Detect Hepatitis B Surface Antigen: A Meta-Analysis and Review of The LiteratureWini LugasÎncă nu există evaluări
- SARS CoV 2 Testing TypesDocument4 paginiSARS CoV 2 Testing TypesFree PeepÎncă nu există evaluări
- tmp4886 TMPDocument5 paginitmp4886 TMPFrontiersÎncă nu există evaluări
- PlebaniDocument2 paginiPlebaniGrescia Ramos VegaÎncă nu există evaluări
- A Systematic Review and Meta-Analysis Ofdiagnostic Accuracy of Serum 1,3s On CutofDocument11 paginiA Systematic Review and Meta-Analysis Ofdiagnostic Accuracy of Serum 1,3s On CutofTatiana BedoyaÎncă nu există evaluări
- 2023.01.21 Diagnostic Test Accuracy of Gram Stain in Formalin Fixed Tissue SectionsDocument10 pagini2023.01.21 Diagnostic Test Accuracy of Gram Stain in Formalin Fixed Tissue SectionsErwin Foster-SmithÎncă nu există evaluări
- Molecular, Serological, and Biochemical Diagnosis and Monitoring of COVID-19: IFCC Taskforce Evaluation of The Latest EvidenceDocument16 paginiMolecular, Serological, and Biochemical Diagnosis and Monitoring of COVID-19: IFCC Taskforce Evaluation of The Latest Evidenceabekhti abdelkaderÎncă nu există evaluări
- Molecular Diagnostics in Virology - PMCDocument14 paginiMolecular Diagnostics in Virology - PMCAISHAÎncă nu există evaluări
- Test Bank For Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics 7th Edition by BurtisDocument35 paginiTest Bank For Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics 7th Edition by Burtiscereus.kailc39cf97% (38)
- D M P S: Ecision Aking and Roblem OlvingDocument6 paginiD M P S: Ecision Aking and Roblem OlvingMaya RustamÎncă nu există evaluări
- Amylase UrinDocument3 paginiAmylase UrinMaya RustamÎncă nu există evaluări
- Rates of Positive Cardiac Troponin I and Creatine Kinase MB Mass Among Patients Hospitalized For Suspected Acute Coronary SyndromesDocument6 paginiRates of Positive Cardiac Troponin I and Creatine Kinase MB Mass Among Patients Hospitalized For Suspected Acute Coronary SyndromesMaya RustamÎncă nu există evaluări
- 01-2009 EASD C-Peptide Poster 580Document1 pagină01-2009 EASD C-Peptide Poster 580Maya RustamÎncă nu există evaluări
- Neumaier 1998 Fundamentals Quality Assessment Molecular Ampli MethodDocument15 paginiNeumaier 1998 Fundamentals Quality Assessment Molecular Ampli MethodMaya RustamÎncă nu există evaluări
- Jurnal Malaria TesDocument5 paginiJurnal Malaria TesMaya RustamÎncă nu există evaluări
- Adiponektin 1Document8 paginiAdiponektin 1Maya RustamÎncă nu există evaluări
- Homocysteine and Markers of Coagulation and Endothelial Cell ActivationDocument7 paginiHomocysteine and Markers of Coagulation and Endothelial Cell ActivationMaya RustamÎncă nu există evaluări
- Amylase - Urine: Medlineplus TopicsDocument3 paginiAmylase - Urine: Medlineplus TopicsMaya RustamÎncă nu există evaluări
- Homosistein AMIDocument7 paginiHomosistein AMIMaya RustamÎncă nu există evaluări
- Changes in Plasma Fibrinogen, Homocysteine and Lipid Profile in Coronary Artery Disease Patients of North Indian (Punjab) Popu-LationDocument4 paginiChanges in Plasma Fibrinogen, Homocysteine and Lipid Profile in Coronary Artery Disease Patients of North Indian (Punjab) Popu-LationMaya RustamÎncă nu există evaluări
- Carey 2005 CD4 Quantitation HIV + Child Antiretroviral TXDocument4 paginiCarey 2005 CD4 Quantitation HIV + Child Antiretroviral TXMaya RustamÎncă nu există evaluări
- Lipase: Related ArticlesDocument4 paginiLipase: Related ArticlesMaya RustamÎncă nu există evaluări
- Hema Sysmex CSDocument8 paginiHema Sysmex CSMaya RustamÎncă nu există evaluări
- Hema Stago DLLDocument9 paginiHema Stago DLLMaya RustamÎncă nu există evaluări
- Peethas ListDocument1 paginăPeethas ListChetan PrajapatiÎncă nu există evaluări
- Excess Fluid VolumeDocument27 paginiExcess Fluid VolumeAdrian Ardamil100% (1)
- Troublesshooting Manual 3b6 PDFDocument50 paginiTroublesshooting Manual 3b6 PDFAgnieszka Wawrzyniak Rybka100% (1)
- Details of Placed Students in Academic Session 2022-23Document10 paginiDetails of Placed Students in Academic Session 2022-23Rahul MishraÎncă nu există evaluări
- TCNHS - Diagnostic-test-G8-cookery 7&8Document2 paginiTCNHS - Diagnostic-test-G8-cookery 7&8Elna Grace Dicon-Ybañez100% (4)
- TMJDocument38 paginiTMJAnonymous 6kAmeZzIÎncă nu există evaluări
- Bushing TestingDocument8 paginiBushing TestingjoseÎncă nu există evaluări
- Fire AlarmDocument18 paginiFire AlarmgauriÎncă nu există evaluări
- Lenskart Solutions PVT LTD Company ProfileDocument13 paginiLenskart Solutions PVT LTD Company ProfileAnujaÎncă nu există evaluări
- CHEM333 Syllabus 2020 2021Document4 paginiCHEM333 Syllabus 2020 2021lina kwikÎncă nu există evaluări
- Calibrating Images TutorialDocument14 paginiCalibrating Images TutorialtrujillomadrigalÎncă nu există evaluări
- Vertical HabitatDocument6 paginiVertical HabitatAbdul SakurÎncă nu există evaluări
- A Guide To Maintenance Metrics-ProgramDocument5 paginiA Guide To Maintenance Metrics-ProgramLy QuanÎncă nu există evaluări
- The Poet of NatureDocument31 paginiThe Poet of NaturejulyÎncă nu există evaluări
- Crimin Q and A Set 1Document6 paginiCrimin Q and A Set 1Marc angelo RegnerÎncă nu există evaluări
- 3 RVDocument8 pagini3 RVDivaruzÎncă nu există evaluări
- Advanced Automatic ControlDocument26 paginiAdvanced Automatic Controlabdullah 3mar abou reashaÎncă nu există evaluări
- Required Obstacle ClearanceDocument14 paginiRequired Obstacle ClearancePero PericÎncă nu există evaluări
- Advance Probability and Statistics - 2014 - 2da Edición - Ottman PDFDocument383 paginiAdvance Probability and Statistics - 2014 - 2da Edición - Ottman PDFAdan Graus RiosÎncă nu există evaluări
- Winter Solstice, CGW 2011Document38 paginiWinter Solstice, CGW 2011Lady HekateShadowMoonfire0% (1)
- Catalog Prince Hydraulic Cylinders Valves Pump Motors Accessories PDFDocument123 paginiCatalog Prince Hydraulic Cylinders Valves Pump Motors Accessories PDFBruno CecattoÎncă nu există evaluări
- Pathoftherosesyllabus2015 1 PDFDocument12 paginiPathoftherosesyllabus2015 1 PDFsperm100% (7)
- A Very Old MachineDocument20 paginiA Very Old MachineSwathi G. SalemÎncă nu există evaluări
- C-81-9903-17-82 Halal 100g 2024-06-08Document1 paginăC-81-9903-17-82 Halal 100g 2024-06-08NURUL FAUZANY BINTI MOHD BASARUDDINÎncă nu există evaluări
- Hemodynamic Monitoring in ICUDocument111 paginiHemodynamic Monitoring in ICUManjunath Gemini100% (2)
- The Foods of Italy BookDocument92 paginiThe Foods of Italy BookmanupopÎncă nu există evaluări
- CEPF640/CEBF640 CEFF640: N-Channel Enhancement Mode Field Effect Transistor FeaturesDocument4 paginiCEPF640/CEBF640 CEFF640: N-Channel Enhancement Mode Field Effect Transistor FeaturesAngel FaneitezÎncă nu există evaluări
- BKC 80Document2 paginiBKC 80jawaidchemicalsÎncă nu există evaluări
- Essentials of o Ste 00 DaveDocument112 paginiEssentials of o Ste 00 DaveGeki Iovan100% (1)
- STAN Statistika 12 PDFDocument25 paginiSTAN Statistika 12 PDFPembelajaran Jarak JauhÎncă nu există evaluări
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceDe la EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceEvaluare: 4.5 din 5 stele4.5/5 (517)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (5)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsDe la EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsEvaluare: 4.5 din 5 stele4.5/5 (6)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (393)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)De la EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Evaluare: 4 din 5 stele4/5 (411)
- Alex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessDe la EverandAlex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessÎncă nu există evaluări
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesDe la EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesEvaluare: 4.5 din 5 stele4.5/5 (397)
- Dark Matter and the Dinosaurs: The Astounding Interconnectedness of the UniverseDe la EverandDark Matter and the Dinosaurs: The Astounding Interconnectedness of the UniverseEvaluare: 3.5 din 5 stele3.5/5 (69)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincDe la EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincEvaluare: 3.5 din 5 stele3.5/5 (137)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessDe la Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessEvaluare: 4 din 5 stele4/5 (33)
- Tales from Both Sides of the Brain: A Life in NeuroscienceDe la EverandTales from Both Sides of the Brain: A Life in NeuroscienceEvaluare: 3 din 5 stele3/5 (18)
- Masterminds: Genius, DNA, and the Quest to Rewrite LifeDe la EverandMasterminds: Genius, DNA, and the Quest to Rewrite LifeÎncă nu există evaluări
- Water: The Epic Struggle for Wealth, Power, and CivilizationDe la EverandWater: The Epic Struggle for Wealth, Power, and CivilizationEvaluare: 3.5 din 5 stele3.5/5 (37)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedDe la EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedEvaluare: 4 din 5 stele4/5 (11)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionDe la EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionEvaluare: 4 din 5 stele4/5 (812)
- Return of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseDe la EverandReturn of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseEvaluare: 4.5 din 5 stele4.5/5 (52)
- Good Without God: What a Billion Nonreligious People Do BelieveDe la EverandGood Without God: What a Billion Nonreligious People Do BelieveEvaluare: 4 din 5 stele4/5 (66)
- Moral Tribes: Emotion, Reason, and the Gap Between Us and ThemDe la EverandMoral Tribes: Emotion, Reason, and the Gap Between Us and ThemEvaluare: 4.5 din 5 stele4.5/5 (115)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomDe la EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomEvaluare: 4 din 5 stele4/5 (216)
- Fast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperDe la EverandFast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperEvaluare: 4.5 din 5 stele4.5/5 (15)
- Seven and a Half Lessons About the BrainDe la EverandSeven and a Half Lessons About the BrainEvaluare: 4 din 5 stele4/5 (110)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorDe la EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorÎncă nu există evaluări