Documente Academic
Documente Profesional
Documente Cultură
Premedication With Intramuscular Midazolam A.8
Încărcat de
Riski DohartuaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Premedication With Intramuscular Midazolam A.8
Încărcat de
Riski DohartuaDrepturi de autor:
Formate disponibile
ANESTH ANALG
1982;61:933-7
Premedication with Intramuscular Midazolam:
A Prospective Randomized Double-Blind
Controlled Study
H. Ronald Vinik, MD,* J. G. Reves, MD,P and Debra Wright, RN$
VINIK, H. R., REVES,J. G., AND WRIGHT, D.:Premedication with intramuscular midazolam: a prospective randomized
double-blind controlled study. Anesth Analg 1982;61:933-7.
One hundred A.S.A. physical status I and II surgical patients were randomized to receive midazolam, 0.07 mg/kg
(group M, 31 patients), hydroxyzine, 1 .O mg/kg (group H, 34 patients), or midazolam diluent as a placebo (group P,
35 patients). Drugs were administered in the vastus lateralis muscle 60 to 90 minutes before anesthesia induction.
Anesthesia was induced with thiopental, 3.0 mg/kg, followed by 1.O-mg/kg increments if required. An entry criterion
was that patients score 250% on a subjective Anxiety Visual Analog Test (AVAT). Anxiety was also objectively rated
on a six-point scale by a trained observer. Patients and observer were unaware of type of premedication used.
Midazolam and hydroxyzine produced significantly ( p c 0.05) greater reduction of anxiety than placebo on both the
AVAT and objective anxiety evaluations. Peak onset appeared between 30 and 60 minutes after drug administration.
Hemodynamic changes were similar in all groups, and no untoward reactions were encountered before anesthesia.
The injection site 24 and 48 hours after administration showed evidence of mild tissue irritation in 68% of patients in
group H, 26% of patients in group M, and none of the patients in group P. Midazolam is an efficacious, safe
premedicant in relatively healthy patients. It has a prompt onset of action with only minimal tissue irritation.
Key Words: PREMEDICATION: midazolam; HYPNOTICS: benzodiazepines, rnidazolam.
IDAZOLAM is an imidazobenzodiazepine the
pharmacology of which has been shown in
animals to be similar to other 1-4-benzodiazepines
(1).It has been used clinically for intravenous induction of anesthesia (2-6). It has hypnotic, anxiolytic,
and amnestic properties that make it suitable for
preanesthetic medication. Intravenous midazolam
produces satisfactory premedication (3). The purpose
of this investigation was to determine the safety and
efficacy of intramuscular midazolam used for preoperative sedation. To accomplish this purpose, midazoiam was compared with an active compound, hydroxyzine, and placebo using a double-blind randomized experimental design.
* Associate Professor of Anesthesiology.
t Professor
of Anesthesiology and Director of Anesthesia Research.
$ Research Assistant.
Received from the Departments of Anesthesiology and Anesthesia Research, The University of Alabama Medical Center, Birmingham, Alabama. Accepted for publication June 7, 1982.
Reprint requests to Dr. H. R. Vinik, Department of Anesthesiology, The University of Alabama Medical Center, Birmingham,
AL 35294.
Methods
Patients in A.S.A. physical status I or I1 scheduled
for elective surgery composed the study population.
One hundred patients were randomly assigned to one
of three premedication groups (Table 1).Patients with
a subjective anxiety score of 250% on an Anxiety
Visual Analog Test (AVAT) were eligible for participation in the investigation. The AVAT is a visual
analogue quantitative measure of anxiety (Figure). To
determine the AVAT score, patients are given a sheet
of paper with a 100-mm length line and asked to rate
their anxiety along the line (from 0 to 100 mm). Of
233 patients screened, 133 (57%) were excluded because their AVAT score was less than 50. Also excluded were patients who had a history of drug abuse
and/or chronic hypnotic, tranquilizer, and narcotic
therapy. All patients gave informed consent, and the
investigation was approved by the Institutional Review Board of the University of Alabama in Birmingham.
Test drugs were administered 60 to 90 minutes
before anesthesia. All medications were given with a
4-cm, 22-gauge needle in the vastus lateralis muscle.
ANESTHESIA AND ANALGESIA
Vol61, No 1 1 , November 1982
933
INTRAMUSCULAR MIDAZOLAM PREMEDICATION
Patients in group M received 0.07 mg/kg of midazolam hydrochloride (5 mg/ml), those in group H received hydroxyzine 1.0 mg/kg (50 mg/ml), and those
in group P midazolam diluent in a volume equal to
TABLE 1
Three Premedication Experimental Groups
Group
Midazolam
(n = 31)
Hydroxyzine
(n = 34)
Placebo
(n = 35)
Age
yr
31 ? 1 . 7
Sex
(M/F)
Weight
5/26
kg
75 ? 4.2
Drug dose
0.07 mg/kg IM
30 f 1.8
3/31
70 f 3.3
1 .O mg/kg IM
36 f 1.8
9/26
71 i 2.4
Midazolam
vehicle?
* Values are means f SD.
t Volume of injection equal to that of midazolam group.
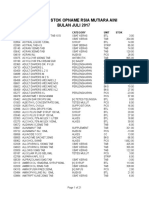
ANXIETY RATING SCALE
INSTRUCTIONS
WE WOULD L I K E TO ESTIMATE YOUR PRESENT LEVEL OF ANXIETY
REGAROING YOUR UPCOMING OPERATION
THE B O n O U
OF THE L I N E REPRESENTS
NO ANXIETY A T A L L A N D THE TOP OF THE LINE THE HIGHEST A N X I E T Y V O U CAN I M A G l N E
PLELJE MAUE A MARK A T THE LEVEL Y O U PRESENTLV FEEL RiGnT NOW
YES. V E R Y
uuw so
I
NO NOT A T ALL
FIGURE.Anxiety Visual Analog Test (AVAT) used to quantitate
subjective anxiety. Line is 100 mm in length. Patients are told to
mark line at point at which they feel their anxiety level rests.
Instructions for marking anxiety level are orinted above line.
that given to patients in group M. Anesthesia in all
patients was induced with thiopental, 3.0 mg/kg IV
(25 mg/ml), followed by I.o-mg/kg incremental doses
if the first and subsequent doses did not induce
anesthesia. Criteria for anesthesia induction were all
of the following: loss of response to verbal commands,
loss of eyelid reflex, and loss of voluntary movement.
Patients were observed before drug administration,
15, 30, 45, and 60 minutes after drug administration,
during anesthetic induction, during emergence from
anesthesia, and 24 and 48 hours after surgery. The
double-blind study design consisted of a floor nurse
administering a known drug to patients who were
unaware of which drug was administered, combined
with observations that were made by a different
trained nurse observer who was unaware of the medication administered. Measurements in the preoperative period included systolic, diastolic, and mean
blood pressures, heart rate, and objective evaluation
of sedation. The objective assessment of sedation
consisted of classification of patients into one of six
groups: hyperactive, awake/alert, awake but drowsy,
asleep but easily arousable, asleep and difficult to
arouse, and asleep and not arousable by verbal commands. These six categories were assigned a numerical value from 1 (asleep/no response) to 6 (hyperactive). AVAT was performed the night before surgery,
just prior to premedication, 60 minutes before premedication and/or just before the patient was transferred to the operating room. The observation made
before transfer to the operating room was defined as
the last observation. The time required for anesthesia
induction and amount of thiopental needed were
recorded. Postoperative nausea and vomiting were
noted and the injection site was evaluated 24 and 48
hours after premedication.
Statistical analysis included computation of mean
values for variables in each group. Analysis of variance or covariance was used to compare groups and
TABLE 2
Blood Pressure (BP) and Heart Rate (HR) after Premedication.
Group M
n
Before medication
15 mint
30 min
45 min
60 min
30
30
29
30
25
f 2.3
f 2.0
f 1.8
f 1.9
t 2.8
f 1.8
f 1.8
2 1.8
t 2.6
80 +. 2.6
33
33
32
33
30
79
78
75
87
Values are means & SD;n = number of patients
Minutes after administration of drug or placebo.
934
ANESTHESIA AND ANALGESIA
Voi 61. No 1 1, November 1982
Group P
__
HR
BP
92
88
88
93
90
Group H
.-
BP
91
92
91
95
89
t 2.4
? 2.0
f 2.3
t 2.3
+. 1.9
HR
77 -+ 2.1
76 f 1.9
73 f 2.0
81 f 1.8
78 k 2.3
34
34
32
34
28
BP
89
88
90
95
92
f 1.9
f 1.8
k 1.7
f 1.9
f 2.5
HR
76
76
75
82
82
f 2.2
f 1.9
f 2.0
f 2.4
* 2.3
VINIK, REVES, AND WRIGHT
determine statistically significant ( p < 0.05) differences. A one-sided test was used for the placebo
comparison and two-sided tests were used for active
drug comparisons. Fischer's exact test was used for
comparison among groups of the incidence of apnea,
nausea, vomiting, and quality of sedation.
Results
The three groups were similar with regard to age,
sex, weight (Table I), and race. Blood pressure and
heart rate values were the same in each group at each
observation period (Table 2). There was no confusion,
restlessness, tremor, nausea, or apnea in any patient
from the time of premedication until the time of
induction. There were differences among the groups
in terms of objective degree of sedation (Table 3). The
mean base line values were similar in all groups, but
midazolam produced significantly ( p < 0.01)better
sedation than placebo. Midazolam also produced significantly (p 5 0.02) lower scores (better sedation)
than hydroxyzine at the 15, 30, and 60-minute observation periods. The results of AVAT are shown in
Table 4. The base line values were similar in all
groups, but midazolarn produced significantly ( p <
0.01) better scores than placebo at the last observation
and at the 60-minute period. Midazolam was also
significantly ( p = 0.04) superior to hydroxyzine at the
60-minute observation period, but not different at the
last observation. Both drugs were superior to placebo
at the last observation period. In groups M and H
satisfactory sedation scores were significantly ( p <
0.01)different from group P. The time for anesthesia
induction was significantly ( p < 0.02) shorter in
groups M (54 f 36.2 seconds) and H (45 & 26.7
seconds) than group P (73 f 45.1 seconds). The
induction dosage of thiopental was also significantly
( p < 0.05) less in groups M (3.2 & .54 rng/kg) and H
(3.1 f 0.58 mg/kg) than in group P (3.6 2 0.89 mg/
kg). Although not significantly different ( p = 0.20),
TABLE 4
Subjective Degree of Sedation after Prernedication: Anxiety
Visual Analog*
Midazolam
Hydroxyzine
Placebo
66 t 23.5
(31 1
52 i 28.3
(32)
35 f 21.4t
(28)
44 f 28.7t
51 f 27.7
29 f 20.ltS
46 f 30.1
(21)
Control (96)
61 t 22.8
Last observation
(28)
(96)
+60 min (%)
(1 5)
* Where %
(311
= percent anxiety. Values are means f
(32)
49 f 24.9
(22)
SD. Number of
patients is shown in parentheses.
t p < 0.01 versus placebo.
$ p < 0.02 versus hydroxyzine.
TABLE 3
Objective Degree of Sedation after Prernedication
Degree of Sedation *
Interval
Mean f SD
No. of
patients
2
5
15
0
0
0
4
8
5
6
1
1
30
30
29
27
16
Midazolam
Base line
15 min
30 min
45 rnin
60 min
5.0 f 0.37
4.6f 0.73t3
3.9 f 0.70t$
3.9 f 0.70t
3.5 f 0.63tS
2
0
0
0
0
26
21
6
3
0
Hydroxyzine
Base line
15 min
30 min
45 min
60 min
5.0 f 0.17
5.0 f 0.30
4.4 f 0.501.
3.9 f 0.60t
3.9 f 0.58t
0
1
0
0
0
32
30
13
4
3
1
2
18
20
16
0
0
0
7
5
0
0
0
0
0
0
0
0
0
0
33
33
31
31
24
Placebo
Base line
15 min
30 min
45 rnin
60 min
4.9 f 0.45
4.9 & 0.38
4.9 f 0.43
4.9 f 0.56
4.9k 0.60
1
0
0
29
32
28
27
18
2
1
2
2
1
1
2
1
0
0
0
0
0
0
34
34
31
31
23
18
0
0
* Numerical designations are: 6, hyperactive; 5, awake and alert; 4, awake and drowsy; 3, asleep/easily responds to verbal
command; 2,asleep/difficult to respond to verbal command; I , asleep/no response to verbal command.
t p < 0 01 versus placebo.
$ p < 0.02versus hydroxyzine.
ANESTHESIA AND ANALGESIA
Vol61, No 1 1 , November 1982
935
INTRAMUSCULAR MIDAZOLAM PREMEDICATION
TABLE 5
Evidence (YO)
of Tissue Irritation at Injection Site after 24
and 48 hours
Midazolam
~~
Pain
Erythema
Induration
Swelling
* p
< 0.01
Hydroxyzine
Placebo
26 *
0
0
68t
0
0
0
0
versus hydroxyzine and placebo.
+ p < 0.01 versus placebo
there was a trend toward more frequent apnea during
anesthesia induction in group M (52%) and group H
(50%)than in group I' (33%).
After surgery, patients in group H (2670)had a
significantly ( p < 0.05) lower incidence of nausea
than patients in group M (54%). The incidence of
nausea in patients in group P was 44%. The incidence
of vomiting was similar in all three groups of patients
(group M 2170, group H 1070,and group P 20%).
Evaluations of injection sites 24 and 48 hours after
drug administration are shown in Table 5 . The incidence of pain at the injection site, the same at 24 and
48 hours after injection, was greatest in group H
(68%), absent in group P, and 26% in group M. The
incidence of pain was significantly ( p < 0.01)greater
in group H than in group M. There was a 6%incidence
of erythema and induration in patients given hydroxyzine and an incidence of swelling of 9% in that
group.
Discussion
I'remedication traditionally has several goals: reduction of anxiety, pain, and secretions, and provision
of basal or background sedation. Of these, the primary purpose of prescribing drugs in the immediate
preoperative period is to allay patient anxiety. Midazolam is a hypnotic with anxiolytic properties which
has been used intravenously for preoperative medication (3). Our study was designed so that both the
patient and observer were unaware of the medication
(double-blind). Randomization produced groups with
similar demographic characteristics and all patients
received the same visits, tests, and treatments.
The results demonstrate that midazolam may be
safely given intramuscularly to produce satisfactory
premedication. Intravenous midazolam can produce
respiratory depression (7-lo),but our study did not
use tests sensitive enough to detect this potential
adverse effect. The degree of respiratory depression
from intramuscular midazolam has not been deter-
936
ANESTHESIA AND ANALGESIA
Vol 61, No 1 1 , November 1982
mined, but presumably it should be similar to the
respiratory depression associated with intravenous
midazolam as similar blood levels may be attained
(11).Also, it is important to realize that the present
investigation included relatively young, healthy patients and the safety of midazolam in older, more ill
patients has not been demonstrated.
Midazolam and hydroxyzine proved to be effective
anxiolytic drugs. Patients had high preoperative anxiety levels (>SO% AVAT scores), and both compounds
were clearly superior to placebo in reducing preoperative anxiety. Midazolam proved to be slightly superior to hydroxyzine in terms of subjective (AVAT)
(Table 4) and objective scoring (Table 3) of sedation.
Fragen and co-workers (12) have reported preliminary
data also demonstrating efficacy of midazolam for
intramuscular premedication. In that study, using
slightly higher doses of midazolam (0.075 mg/kg) and
hydroxyzine (1.5 mg/kg) in smaller groups of patients, midazolam and hydroxyzine were superior to
placebo in anxiolytic effects. Additionally, in the same
study, Fragen et a1 (12) demonstrated that intramuscular midazolam caused significantly greater lack of
recall than either hydroxyzine or placebo 30 minutes
after premedication. We did not investigate the
amnestic properties of the drugs in this study.
The preoperative interview itself is known to have
a calming effect (13). Indeed, some anesthesiologists
subscribe to a pharmacologic nihilism, feeling that
proper preanesthetic interview, examination, and consultation obviate the need for preoperative anxiolytic
drug therapy. The present findings demonstrate
clearly that despite identical preoperative visits, the
active compounds, midazolam and hydroxyzine,
proved significantly superior to placebo in reducing
patient anxiety. In our experimental setting, the effect
on anxiety of the preoperative interview per se was
not examined.
Of particular interest was the rapidity of onset of
sedative action associated with midazolam. Fifteen
minutes after premedication, midazolam had significantly reduced the objective ratings of anxiety from
a score of 5.0 to 4.5 with the peak effect measured at
60 minutes. With both active drugs a time-response
effect pattern emerged, both drugs producing progressive effect as time elapsed, whereas the anxiety
remained constant in patients given placebo injections
(Table 3). The pharmacodynamic measures of drug
activity (anxiety levels) are consistent with the pharmacokinetic studies. Amrein and co-workers (14), for
example, demonstrated in six subjects rapid absorption of midazolam folIowing intramuscular adminis-
VINIK, REVES, A N D WRIGHT
tration with peak blood levels after 30 minutes. The
rapid absorption of intramuscular midazolam contrasts to the more variable absorption of another 1-4benzodiazepine, diazepam (15-17), when given intramuscularly. The vastus lateralis muscle, the site of
administration in the present study, is known to
influence favorably the absorption of intramuscular
benzodiazepines (16).
The postoperative evaluation of the injection site
revealed minimal tissue reaction to midazolam (group
M) and midazolam vehicle (group P). This is not
surprising as laboratory evidence reveals that midazolam produces little tissue reaction (18), and this
confirms the findings of Fragen et al, who also administered midazolam intramuscularly (0.075 mg/kg)
(12). Water solubility of midazolam occurs only at a
pH <4.0 (I), but the acid vehicle is nonirritating to
the muscle.
Postoperative nausea was more prevalent in patients given placebo injections and in patients given
midazolam than in patients receiving hydroxyzine.
This probably reflects the known antiemetic effect of
hydroxyzine (19),as all patients received similar anesthetic drugs and postoperative analgesics. The incidence of nausea was similar after placebo and midazolam, which indicates that midazolam has no antiemetic action. There was no nausea or vomiting before
anesthesia in any group.
In summary, patients premedicated with intramuscular midazolam and hydroxyzine are better sedated
than are patients given placebo injections. The sedation results in lower anesthesia induction requirements. There are no untoward side effects associated
with midazolam and hydroxyzine except for a tendency toward more apnea during induction. Midazolam is a safe and effective premedicant when given
intramuscularly in relatively young, healthy patients.
ACKNOWLEDGMENTS
The authors appreciate the clerical assistance and excellence of
Rae Kerutis and the cooperation of Jay Miller of Hoffman-La Roche
who helped with the statistical evaluation of the data.
REFERENCES
1. Pieri L, Schaffner R, Scherschlicht R, et al. Pharmacology of
midazolam. Arzneim Forsch 1981;31:2180-2201.
2. Brown CR, Sarnquist FH, Canup CA, Pedley TA. Clinical,
electroencephalographic, and pharmacokinetic studies of a water-soluble benzodiazepine, midazolam maleate. Anesthesiology 1979;50:467-70.
3. Conner JT, Katz RL, Pagano RR, Graham CW. RO 21-3981 for
intravenous surgical prernedication and induction of anesthesia. Anesth Analg 1978;57:1-5.
4. Dundee JW, Samuel 10, Wilson DB, Toner W, Howard PJ.
Midazolam maleate: a water-soluble benzodiazepine; preliminary results. Br J Clin Pharmacol 1980;9:305.
5 Fragen RJ, Gahl F, Caldwell N. A water-soluble benzodiazepine,
RO 21-3981, for induction of anesthesia. Anesthesiology
1978;49:41-3.
6 Reves JG, Corssen G, Holcomb C. Comparison of two benzodiazepines for anaesthesia induction: midazolam and diazepam.
Can Anaesth SOCJ 1978;25:211-4.
7 Carel WD, Zebrowski ME, Gardner S, Smith TC. Ventilatory
depression following midazolam induction. Anesthesiology
1980;53:5408.
8. Forster A, Gardaz JP, Suter IM, Gemperle M. Respiratory
depression by midazolam and diazepam. Anesthesiology
1980;53:494-7.
9. Gross JB, Smith TC. Ventilation after midazolam and thiopental
in subjects with COPD. Anesthesiology 1981;55:A384.
10. Southorn P, Rehder K, Didier EF. Midazolam sedation and
respiratory mechanics in man. Anesthesiology 1981;55:A367.
11. Crevoisier PC, Eckert M, Heizmann P, Thurneysen DJ, Ziegler
WH. Relation entre Ieffect clinique et al pharmacocinetique
du midazolam apres administration i.v. et i.m. Arzneim Forsch
1981;31:2211-5.
12. Fragen RJ, Funk DI, Avrarn MJ, Costello C, DeBruine K.
Midazolam versus hydroxyzine as intramuscular premedicants.
Anesthesiology 1981;55A278.
13. Egbert LD, Battit GE, Turndorf H, Beecher HK. The value of
the preoperative visit by an anesthetist. JAMA 1963;185:553-5.
14. Amrein VR, Cano JP, Eckert M. Coassolo P. Pharmakokinetik
von Midazolam nach intravenoser Verabreichung. Arzneim
Forsch 1981;31:2202-5.
15. Hillestad L, Hansen T, Melsom H. Diazepam metabolism in
normal man. I. Serum concentrations and clinical effects after
intravenous, intramuscular, and oral administration. Clin Pharmacol Ther 1974;16:479-84.
16. Korttila K, Linnoila M. Absorption and sedative effects of
diazepam after oral administration and intramuscular administration into the vastus lateralis muscle and the deltoid muscle.
Br J Anaesth 1975;47:857-62.
17. Mandelli M, Tognoni G, Garattini S. Clinical pharmacokinetics
of diazepam. Clin Pharmacokinet 1978;3:72-91.
18. Pagano RR, Graham CW, Galligan M, Conner JT, Katz RL.
Histopathology of veins after intravenous lorazepam and R O
21-3981. Can Anaesth SOCJ 1978;25:50-2.
19. McKenzie R, Wadhwa RK, Uy NTL, et al. Antiemetic effectiveness of intramuscular hydroxyzine compared with intramuscular droperidol. Anesth Analg 1981;60:783-8.
ANESTHESIA AND ANALGESIA
Vol 61, No 1 1 . November 1982
937
S-ar putea să vă placă și
- CampurDocument19 paginiCampurRiski DohartuaÎncă nu există evaluări
- MidazolamDocument22 paginiMidazolamRiski Dohartua100% (1)
- Versed (Midazolam) Dosing, Indications, Interactions, Adverse Effects, and MoreDocument2 paginiVersed (Midazolam) Dosing, Indications, Interactions, Adverse Effects, and MoreRiski DohartuaÎncă nu există evaluări
- ISTC 3rdedDocument92 paginiISTC 3rdedmichaelqurtisÎncă nu există evaluări
- Immunology NotesDocument27 paginiImmunology Notescomputerlois88% (8)
- COPDWhat Has Happened To The Airway System - DR Amira 031211 RESPINADocument38 paginiCOPDWhat Has Happened To The Airway System - DR Amira 031211 RESPINARiski DohartuaÎncă nu există evaluări
- Unlock-01 Paggiaro AsmaDocument51 paginiUnlock-01 Paggiaro AsmaRiski DohartuaÎncă nu există evaluări
- 163089Document7 pagini163089Riski DohartuaÎncă nu există evaluări
- Sensitization and Irritant-Induced Occupational Asthma With Latency Are Clinically IndistinguishableDocument6 paginiSensitization and Irritant-Induced Occupational Asthma With Latency Are Clinically IndistinguishableRiski DohartuaÎncă nu există evaluări
- Booker 2011 Sepsis in ED ReviewDocument24 paginiBooker 2011 Sepsis in ED ReviewRiski DohartuaÎncă nu există evaluări
- Booker 2011 Sepsis in ED ReviewDocument24 paginiBooker 2011 Sepsis in ED ReviewRiski DohartuaÎncă nu există evaluări
- Endobronchial TBDocument10 paginiEndobronchial TBRiski Kawa RamadaniÎncă nu există evaluări
- Copd With Chf2Document9 paginiCopd With Chf2Riski DohartuaÎncă nu există evaluări
- 1 24 13 MosierDocument59 pagini1 24 13 MosierRiski DohartuaÎncă nu există evaluări
- Spirometric Findings As Predictors of Survival: Peter LangeDocument3 paginiSpirometric Findings As Predictors of Survival: Peter LangeRiski DohartuaÎncă nu există evaluări
- A Randomized Prospective Trial of The Utility of of Transbronchial Needle Aspirate SpecimensDocument18 paginiA Randomized Prospective Trial of The Utility of of Transbronchial Needle Aspirate SpecimensRiski DohartuaÎncă nu există evaluări
- A Randomized Prospective Trial of The Utility of of Transbronchial Needle Aspirate SpecimensDocument18 paginiA Randomized Prospective Trial of The Utility of of Transbronchial Needle Aspirate SpecimensRiski DohartuaÎncă nu există evaluări
- Emd166 Slide Pulmonary Emergency MedicineDocument93 paginiEmd166 Slide Pulmonary Emergency MedicineRiski DohartuaÎncă nu există evaluări
- Molecular Biology of Lung CancerDocument124 paginiMolecular Biology of Lung CancerRiski DohartuaÎncă nu există evaluări
- City Newsletter: What's Right With Washington Terrace City?Document4 paginiCity Newsletter: What's Right With Washington Terrace City?Riski DohartuaÎncă nu există evaluări
- Thorax 2012 Lewis 26 34Document11 paginiThorax 2012 Lewis 26 34Riski DohartuaÎncă nu există evaluări
- Thorax 2012 Lewis 26 34Document11 paginiThorax 2012 Lewis 26 34Riski DohartuaÎncă nu există evaluări
- Isolated Mediastnal TuberculosisDocument2 paginiIsolated Mediastnal TuberculosisRiski DohartuaÎncă nu există evaluări
- Small CEL CarcinomaDocument24 paginiSmall CEL CarcinomaRiski DohartuaÎncă nu există evaluări
- Indian Pneumonia Guidelines: EditorialDocument2 paginiIndian Pneumonia Guidelines: EditorialRiski DohartuaÎncă nu există evaluări
- Unlock LungIndia29627 5427929 - 150439Document36 paginiUnlock LungIndia29627 5427929 - 150439Riski DohartuaÎncă nu există evaluări
- Broncho S Copy Background ErDocument2 paginiBroncho S Copy Background ErRiski DohartuaÎncă nu există evaluări
- Ventilator Associated PneumoniaDocument37 paginiVentilator Associated PneumoniaRiski DohartuaÎncă nu există evaluări
- Recommendations For Treatment of Hospital - Acquired and Ventilator-Associated Pneumonia Review of Recent International GuidelinesDocument6 paginiRecommendations For Treatment of Hospital - Acquired and Ventilator-Associated Pneumonia Review of Recent International GuidelinesRiski DohartuaÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Drugs Used in PregnancyDocument39 paginiDrugs Used in PregnancySneha BencyÎncă nu există evaluări
- Endoscopy and ColonosDocument17 paginiEndoscopy and ColonosKim RamosÎncă nu există evaluări
- Integrated Application Form (XLSX Format)Document42 paginiIntegrated Application Form (XLSX Format)edna hilarioÎncă nu există evaluări
- Alcain Peritoneal-DialysisDocument4 paginiAlcain Peritoneal-DialysisErika Trina AlcainÎncă nu există evaluări
- Journal Club - EichlerDocument4 paginiJournal Club - Eichlerapi-648595816Încă nu există evaluări
- CHAPTER 17 - Clinical PharmacyDocument20 paginiCHAPTER 17 - Clinical PharmacyShubhanjay KumarÎncă nu există evaluări
- Kasus AsmaDocument5 paginiKasus AsmaHananun Zharfa0% (3)
- Drug Study Nicardipine AlacazarDocument1 paginăDrug Study Nicardipine AlacazarDanica Pauline RamosÎncă nu există evaluări
- Comparative DissolutionDocument34 paginiComparative DissolutionVeena Reddy SingamÎncă nu există evaluări
- 1344 PDFDocument3 pagini1344 PDFMithÎncă nu există evaluări
- Dem Tickler NotesDocument1 paginăDem Tickler NotesSeff CausapinÎncă nu există evaluări
- 1st Panel Inventory September 2021mdsDocument199 pagini1st Panel Inventory September 2021mds김에렌Încă nu există evaluări
- Data ObatDocument21 paginiData ObatHalimatun SyadyahÎncă nu există evaluări
- FDA's Current Practice and Challenges in The Use of Dissolution Similarity Testing For Demonstration of Bioequivalence - Case StudiesDocument19 paginiFDA's Current Practice and Challenges in The Use of Dissolution Similarity Testing For Demonstration of Bioequivalence - Case StudiesSrinivas Reddy MaramÎncă nu există evaluări
- AnestheticsDocument11 paginiAnestheticsKalidasan KrishnaÎncă nu există evaluări
- Label Kotak Obat BaruDocument25 paginiLabel Kotak Obat BaruOrin Tri WulanÎncă nu există evaluări
- Unit 7. Sympathomimetics and SympatholyticsDocument44 paginiUnit 7. Sympathomimetics and SympatholyticsApril Mergelle Lapuz100% (2)
- Dexlansoprazole Vs Esomeprazole ERGEDocument12 paginiDexlansoprazole Vs Esomeprazole ERGELuis Felipe Gomez AndradeÎncă nu există evaluări
- DisolusiDocument47 paginiDisolusiNoonaNuzha Lestary NuzhaAyuÎncă nu există evaluări
- Emergency Care Procedures: Cardiopulmonary ResuscitationDocument13 paginiEmergency Care Procedures: Cardiopulmonary ResuscitationKim BadillesÎncă nu există evaluări
- Pharmacology Assignment - Medicines and MealsDocument15 paginiPharmacology Assignment - Medicines and MealsFarhat JahanÎncă nu există evaluări
- Cito 27Document58 paginiCito 27dewakusumaÎncă nu există evaluări
- Nama Obat/Barang Satuan No. ID Jenis Barang Keluar Jan 2022 Keluar Jan 2023Document27 paginiNama Obat/Barang Satuan No. ID Jenis Barang Keluar Jan 2022 Keluar Jan 2023CitrahsnÎncă nu există evaluări
- Coldex CapsuleDocument3 paginiColdex Capsulehk_scribdÎncă nu există evaluări
- Phage Therapy - PresentationDocument16 paginiPhage Therapy - PresentationImen Brz100% (1)
- 1 s2.0 S0196070923000819 MainDocument6 pagini1 s2.0 S0196070923000819 MainRALF KEVIN PIANOÎncă nu există evaluări
- Calabar Bean (Physostigma Venenosum) : Origin Family Geographical Source The Part Uses Chemical TestsDocument1 paginăCalabar Bean (Physostigma Venenosum) : Origin Family Geographical Source The Part Uses Chemical Testscyper zoonÎncă nu există evaluări
- Dialysis in AkiDocument66 paginiDialysis in Akiwael abodiabÎncă nu există evaluări
- Ect Consent FormDocument2 paginiEct Consent FormChalla Krishna VasanÎncă nu există evaluări
- CHEMOTHERAPYDocument28 paginiCHEMOTHERAPYDwi CahyaÎncă nu există evaluări