Documente Academic
Documente Profesional
Documente Cultură
Chossegros Retromdb Approach
Încărcat de
sevattapillaiDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Chossegros Retromdb Approach
Încărcat de
sevattapillaiDrepturi de autor:
Formate disponibile
Short retromandibular approach of subcondylar fractures
Clinical and radiologic long-term evaluation
Cyrille Chossegros, MD. DMD a Francois Cheynet. MD. DMD. a
Jean-Louis Blanc. MD. DMD, a and Znnbir Bourezak. b Marseille. France
TIMONE UNIVERSITY HOSPITAL CENTER
Objective. The classic technique for open reduction of subcondylar fracture is the submandibular approach, The aim of
this study was to evaluate long-term clinical and radiologic results of the short retromandibular approach to displaced
subcondylar fractures.
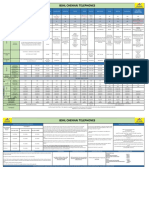
Material and methods. During a period of 66 months we performed a prospective study with a modified version of the
retromandibular approach in 38 patients with displaced subcondylar fractures. In this article we describe clinical and
radiologic results in 19 patients with follow-ups longer than 6 months Irange, 6 to 66 monthsl. Preoperatively all patients
had malocclusion and radiology demonstrated displacement.
Results. The retromandibular surgical approach was successful in all cases. Roughly 25 months after surgery, mouth
opening was 43 mm with symmetric laterotrusive movements. Permanent marginal nerve palsy was never observed.
Conclusions. Our findings indicate that the short retromandibular approach "s an easy and safe technique for displaced
subcondylar fractures.
(Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;82;248-52)
One third of all mandibular fractures involve the
condylar region. 1 There is a consensus that the
method of choice in cases without displacement is
conservative treatment by immobilization of the
mandible. Indications for surgical management in
adults are controversial. 2' 3 When surgery is indicated.
surgical methods include open reduction and osteosynthesis with a miniplate, wire, or lag-screw. 4-6 The
classic submandibular Ridson approach 7, * that we
used for several years achieves poor exposure of the
fracture and is associated with a high rate (30%) of
transitory facial nerve palsy. In an attempt to avoid
these problems we used a modified retromandibular
approach 8, 9 in a prospective series of 38 patients. The
aim of the present article was to describe clinical and
radiologic results in 19 patients with follow-ups
longer than 6 months.
PATIENTS A N D M E T H O D S
Between 1989 and 1994. 38 subcondylar fractures
with displacement but no dislocation were treated
surgically in the Department of Maxillofacial Surgery
at the Timone University Hospital Center in
Marseilles. At the time of writing 19 patients had follow-ups longer than 6 months and were included in
aOral and Maxillofacial Surgeon, Department of Oral and Maxillofacial Surgery.
bForeign resident.
Received for publication Nov. 9. 1995: returned for revision Dec.
14. 1995: accepted for publication Apr. 16. 1996.
Copyright 9 1996 by Mosby-Year Book, Inc.
1079-2104/96/55.00 + 0 7/12/74212
248
the study. The other patients had follow-ups that were
too short or were lost to follow-up. No early complication were observed or reported in any of the excluded patients.
Surgery via the retromandibular approach was performed as soon as possible. Surgical indications were
based either on clinical examination that found shortening of the ramus associated with ipsilateral molar
prematurity or edentulous posterior segment and radiologic findings that showed subcondylar fracture
with displacement (Figs. 1 and 2). The mean age ot
the 19 patients evaluated was 31 years: 68% were
men. Preoperative data such as pain, mouth opening,
and noise were not recorded. Mean duration ot
follow-up was 26 months. Follow-up consisted ol
clinical and radiologic evaluation. Clinical examination by an independent examiner included assessment
of the following factors: pain. mouth opening, laterotrusive movement, noise, facial nerve function, ear
sensitivity, intraocclusional relationship, and scar.
Radiologic examination included panoramic view
and facial and lateral teleradiographs.
Maxillomandibular fixation with elastics was
placed at the beginning of the procedure. Intubation
was done by the nasotracheal route, and the head was
not overly rotated. The incision is made in a natural
crease of the neck beginning from 1 cm under the
mastoid apex and running parallel to the anterior aspect of the sternocleidomastoid muscle (Fig. 3). The
length of the incision is between 3 and 4 cm. If the
fracture is located too high, the inferior part of the
parotid gland must be freed. After locating the angle
ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
Chossegros et aL
249
Volume 82, Number 3
Fig. 1. Part of panoramic view; right displaced subcondylar fracture.
Fig. 2. Panoramic view; postoperative view with miniplate fixation.
of the mandible the pterygomasseteric sling is released by making a 6 to 8 cm incision, and the masseter muscle is detached. The edge of the condylar
fragment is sharp and the surgeon must take care to
avoid self-injury. 1~ A towel clip is inserted in the
mandibular angle to facilitate fracture reduction after
placement of a periosteal elevator behind the condyle.
After positioning the miniplate (four holes with
bridge) and placing the upper two screws, the fracture
is then reduced with the towel clip before placement
of the lower two screws (Fig. 4). Placing the upper
screws before reduction provides a greater skin mobility. If the condyle has been displaced into the infratemporal fossa, the finger should be used to push
it from the deep portion of the ramus toward the glenoid fossa. The last step in the procedure is vacuum
drain placement with closure of the periosteum and
intradermal suture. In cases of single fractures, maxillomandibular fixation is removed after 1 week.
Normal food intake is not permitted until postoperative day 21. Physical exercise is prescribed only if
range of mouth opening is limited (4 of 19 cases or
21%).
Maximal mouth opening was greater than 35 m m in
all cases and greater than 40 m m in 13 (81%) of 16
patients with follow-ups longer than 10 months. Seventy-nine percent (15 of 19) presented sagittal opening movement. Laterotrusive movements ranged from
4 to 14 m m but were always symmetric. Constant
noise was reported on the contralateral side by one
patient (5%) and transient noise on the ipsilateral side
by six patients (32%). The interocclusional relationship was the same as before the procedure in 79% of
cases (15 of 19) and slightly different (deviation of the
incisors to the fractured side <1 ram) in 11% (2 of 19)
of cases. In two patients the interocclusional relationship was abnormal: angle class III in one patient
in whom subcondylar fracture was associated with
fracture of the body of the mandible and angle class
II (edge-to-edge occlusion) in o n e p a t i e n t in whom
subcondylar fracture was associated with four mandibular fractures and partial preoperative edentulism.
A prefracture interocclusional relationship was not
known in either o f these two patients. Chewing was
normal in 89% of cases (17 of 19) and unilateral in
the remaining two patients with occlusional abnormalities. Temporary facial palsy occurred in two
cases (2 of 19); it lasted for 3 weeks in one patient and
6 weeks in the other. Two patients had transitory auricular hypoesthesia for 2 to 3 weeks. Scar widening
(about 2 m m large) was noted in one case and slight
transient inflammation without infection in another.
RESULTS
All patients reported Satisfaction with the outcome
of the procedure. None complained of fatigue or pain
on chewing. Two patients complained of facial tenderness associated with chan~es in the weather.
250
Chossegros et al.
ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
September 1996
Fig. 3. Drawing (A) and photograph (B) of retromandibular approach show skin incision (arrow). Note incision is rather short (3 to 4 cm). (A, angle of mandible; M, mastoid apex)
In the remaining 17 cases (89%) healing was considered as excellent. Radiologic examination revealed
normal condyles in 15 patients, insufficient reduction
in 1 (5%), slight ipsilateral upper condylar flattening
(as a result of resorption (1 mm) of the anterosuperiot part of the condyle) in 2 (11%), and slight contralateral upper condylar flattening in 1 (5%).
DISCUSSION
Various techniques have been proposed for surgical treatment of displaced condylar fractures including the submandibular approach, 8 the preauricular
approach, 8 the rhytidectomy approach, 8, 11 or the intraoral approach. 12 For subcondylar fractures, the
submandibular approach is too low and the preauricular approach is too high. For this reason we chose the
retromandibular approach in most cases. Our technique is slightly different from the one proposed by
Ellis8; the approach is more posterior, the parotid
gland is not entered, the nerve branches are not
encountered, and the scar is slightly more conspicuous.
In all cases the retromandibular approach allowed
direct visual alignment of the fragments. Condylar
removal, 13 which seems to us to be a source of iatrogenic complications, 14, 15 is not needed. Reduction
was good in 95% of patients. Postoperative mouth
opening was over 40 m m in 81% of patients, but these
results cannot be compared with those of McArthm
et al. 7 with dislocated condyles (43% >35 mm). Neurologic complications in our series were minimal (i.e.,
11% of transient palsy). This is low in comparison
with previous reports: 48% (14 of 29) for Ellis and
Dean s with the retromandibular approach, 37% foi
Tasanen 16 with the Ridson approach, and 13% foi
Eckelt 6 with the lag-screw. The rate of 11% was perhaps due to the fact that we do not enter the parotid
gland. Long-term condylar resorption observed i~
five cases in our series (ipsilateral in two cases and
contralateral in three) underlines the fragility of the
condyle even in nondeviated fractures. Contralatera]
bone resorption without fracture observed in one patient (case 5) was due either to a microfracture oi
secondary osteonecrosis. Bone resorption is usual in
dislocated condyle 7' 14 but has not been frequently
reported in nondislocated condylar fracturesJ 7
Because the disk cannot be visualized with the retromandibular approach, preoperative magnetic resonance imaging is mandatory in patients with dislocated fractures 18 because of the remote possibility ot
separation of the disk from the condyle. If separatio~
is detected the disk must be sutured to the periosteunn
ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
Volume 82, Number 3
Chossegros et al.
251
Fig. 4. Operative view. Upper two screws are placed before reduction. With this technique the whole
miniplate cannot be seen through the incision at the same time. Note that the incision is short and that the
view is quite good.
of the posterior border of the c o n d y l e with a preauricular approach, a double approach (preauricular and
retromandibular), or a large cutaneous rhytidectomy
incision. After recovery we do not r e c o m m e n d the
r e m o v a l of c o n d y l a r miniplates because of the risk of
nerve and salivary gland injury associated with the
forces required o n the fibrous tissues for miniplate
removal. However, it should be m e n t i o n e d that successful r e m o v a l was performed in one patient who
c o m p l a i n e d of tenderness associated with changes in
the weather.
CONCLUSION
T r e a t m e n t of displaced s u b c o n d y l a r fractures
should be as n o n a g g r e s s i v e as possible. W h e n open
reduction and osteosynthesis are required, the retrom a n d i b u l a r approach is an effective and safe technique, especially for displaced s u b c o n d y l a r fractures
without deviation. Further study is needed to c o n f i r m
that the retromandibular approach is safer and easier
than s u b m a n d i b u l a r approach.
We thank Mr. A. Corsini and Dr. J. Conrath for their
translation and review of the manuscript.
REFERENCES
1. Blanc JL, Lagier JP, Gras R, Bremond D, Belloni D. Les sequelles des fractures condyliennes ~i travers l'experience du
service et l'expertise medicale. (Condylar fractures sequelae
through our clinical experience and medical expertise). Rev
Stomatol Chir Maxillofac 1985;86:29-31.
2. Hidding J, Wolf R, Pingel D. Surgical versus nonsurgical
treatment of the articular process of the mandible. J Craniomaxillofac Surg 1992;20:345-7.
3. Lachard J, Zattara H, Romette JM, Vitton J. Indications des
ost6osynth~ses dans les fractures s0us condyliennes basses.
(Osteosyuthesis indications in subcondylar fractures) Rev
Stomatol 1971;72:201-4.
4. Fernandez JA, Mathog RH. Open treatment of condylar fractures with biphase technique. Arch Otolaryngol Head Neck
Surg 1987;113:262-5.
5. Koberg WR, Momma W. Treatment of fractures of the man-
252
6.
7.
8.
9.
10.
11.
12.
13.
Chossegros e t al.
dibular process by functional stable osteosynthesis using
miniaturized dynamic compression plates. Int J Oral Surg
1978;7:256-62.
Eckelt U, Rasse M. Clinical radiographic and axiographic
control after traction screw osteosynthesis of fractures of the
mandibular condyle region. Rev Stomatol Chir Maxillofac
1995;96:158-65.
McArthur C, Donald P, Knowles J, Moore C. Open reductionfixation of mandibular subcondylar fractures. Arch Otolaryngol Head Neck Surg 1993;119:403-6.
Ellis E, Dean J. Rigid fixation of mandibular condyle
fractures. Oral Surg Oral Med Oral Pathol 1993;76:6-15.
Hinds EC, Girotti WJ. Vertical subcondylar osteotomy: a reappraisal. Oral Surg Oral Med Oral Pathol 1967;24:164-70.
Cheynet F, Gere E, Chossegros C, Tagliana P, Lemaire P,
Blanc JL. Faux an6vrysmes traumatiques associ6s anx fractures ferm6s de la mandibule. (False-aneurysm associated to
mandibular fractures) Rev Stomotal Chir Maxillofac
1992;93:6-12.
Zide MF, Kent JN. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg 1983;41:89-93.
Lachner J, Clanton JT, Waiter PD. Open reduction and internal rigid fixation of the subcondylar fractures via an intraoral
approach. Oral Surg Oral Med Oral Pathol 1991;71:257-61.
Ellis E, Reynolds ST, Park HS. A method to rigidly fix high
ORAL SURGERY ORAL MEDICINE ORAL PATHOLOGY
September 1996
14.
15.
16.
17.
18.
condylar fractures. Oral Surg Oral Med Oral Pathol 1989;
68:369-74.
Iizuka T, Lindqvist C, Hallikainen D, Mikkonen P, Pankku P.
Severe bone resorption and osteoarthrosis after miniplates
fixation of high condylar fractures. Oral Surg Oral Med Oral
Pathol 1991;72:400-7.
Zhang X, Obeid G. A comparative study of the treatment of
unilateral fractured and dislocated mandibular condyles in the
rabbit. J Oral Maxillofac Surg 1991;49:1181-90.
Tasanen A, Lamberg MA. Transosseous wiring in the treatment of condylar fractures of the mandible. J Oral Maxillofac
Surg 1976;4:200-11.
Dahlstr6m L, Kahnberg KE, Lindhahl L. Fifteen year follow-up on condylar fractures. Int J Oral Maxillofac Surg
1989;18:18-23.
Chuong R, Piper MA. Open reduction of condylar fractures
of the mandible in conjunction with repair of discal injury: a
preliminary report. J Oral Maxillofac Surg 1988;46:257-62.
Reprint requests:
Dr Cyrille Chossegros
Service du Pr Blanc
CHU Timone
13385 Marseille cedex 5
France
BOUND VOLUMES AVAILABLE TO SUBSCRIBERS
Bound volumes of Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics
are available to subscribers (only) for the 1996 issues from the Publisher, at a cost of $69.00 for domestic, $86.67 for Canadian, and $81.00 for international, for Vol. 81 (January-June) and Vol. 82
(July-December). Shipping charges are included. Each bound volume contains a subject and author index and all advertising is removed. Copies are shipped within 60 days after publication of the last issue
in the volume. The binding is durable buckram with the journal name, volume number, and year
stamped in gold on the spine. Payment must accompany all orders. Contact Mosby-Year Book, Subscription Services, 11830 Westline Industrial Drive, St. Louis, MO 63146-3318, USA; phone
(800)453-4351, or (314)453-4351. Subscriptions must be in force to qualify. B o u n d volumes are
not available in place of a regular journal subscription.
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Profession Tax Procedure OnlineDocument1 paginăProfession Tax Procedure Onlinehemanvshah892Încă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Life and Work of Shri Hans Ji MaharajDocument75 paginiLife and Work of Shri Hans Ji Maharajsevattapillai100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Retromolar Canal Infiltration Reduces Pain of Mandibular Molar RCTDocument6 paginiRetromolar Canal Infiltration Reduces Pain of Mandibular Molar RCTSetu KatyalÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Plan Vouchers 12092019Document2 paginiPlan Vouchers 12092019sevattapillaiÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Life of Gajanan Vijay Granthi UneditedDocument63 paginiLife of Gajanan Vijay Granthi UneditedsevattapillaiÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Antibiotics in Oral & Maxillofacial SurgeryDocument50 paginiAntibiotics in Oral & Maxillofacial SurgerysevattapillaiÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Penjelasan Consort Utk Artikel KlinisDocument28 paginiPenjelasan Consort Utk Artikel KlinisWitri Septia NingrumÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Praveena Clinic Visiting CardDocument1 paginăPraveena Clinic Visiting CardsevattapillaiÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Closed Reduction Nasal Fracture Post Op InstructionsDocument2 paginiClosed Reduction Nasal Fracture Post Op InstructionssevattapillaiÎncă nu există evaluări
- Nerve InjuriesDocument39 paginiNerve InjuriessevattapillaiÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- SBV Dissertation Template 2017Document22 paginiSBV Dissertation Template 2017sevattapillaiÎncă nu există evaluări
- Jackie ChanDocument1 paginăJackie ChansevattapillaiÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Sterilization of ArmamentariumDocument41 paginiSterilization of ArmamentariumsevattapillaiÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Best Practices OMFS DEPTDocument2 paginiBest Practices OMFS DEPTsevattapillaiÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- Sterilization and AsepsisDocument48 paginiSterilization and AsepsissevattapillaiÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Basic Preprosthetic SurgeryDocument27 paginiBasic Preprosthetic SurgerysevattapillaiÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Lymphangioma of The TongueDocument3 paginiLymphangioma of The TonguesevattapillaiÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- DNA Probes and Primers in Dental PracticeDocument6 paginiDNA Probes and Primers in Dental PracticesevattapillaiÎncă nu există evaluări
- Oral Lesions in NeonatesDocument8 paginiOral Lesions in NeonatessevattapillaiÎncă nu există evaluări
- Congenital Sublingual CystDocument5 paginiCongenital Sublingual CystsevattapillaiÎncă nu există evaluări
- Oral Lesions in Neonates PDFDocument8 paginiOral Lesions in Neonates PDFsevattapillaiÎncă nu există evaluări
- Lymphangioma of The Tongue PDFDocument3 paginiLymphangioma of The Tongue PDFsevattapillaiÎncă nu există evaluări
- Oral LymphangiomaDocument8 paginiOral LymphangiomasevattapillaiÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Congenital Ranula in A Newborn A Rare PresentationDocument3 paginiCongenital Ranula in A Newborn A Rare PresentationsevattapillaiÎncă nu există evaluări
- Post-Extraction Complication Course PDFDocument11 paginiPost-Extraction Complication Course PDFsevattapillai100% (1)
- The Effects of Using Hyaluronic Acid On The Extraction SocketsDocument5 paginiThe Effects of Using Hyaluronic Acid On The Extraction SocketssevattapillaiÎncă nu există evaluări
- A Retrospective Study On The Use of A Dental Dressing To Reduce Dry Socket Incidence in SmokersDocument5 paginiA Retrospective Study On The Use of A Dental Dressing To Reduce Dry Socket Incidence in SmokerssevattapillaiÎncă nu există evaluări
- Nonsurgical Management of Periapical LesionsDocument11 paginiNonsurgical Management of Periapical LesionssevattapillaiÎncă nu există evaluări
- Periapical Lesions - A Review of Clinical, Radiographic, and Histopathologic Features PDFDocument7 paginiPeriapical Lesions - A Review of Clinical, Radiographic, and Histopathologic Features PDFsevattapillaiÎncă nu există evaluări
- CANINE Impaction Oral SurgeryDocument46 paginiCANINE Impaction Oral SurgeryFourthMolar.com100% (5)
- ASMOPS 2016 - International Invitation PHILIPPINEDocument4 paginiASMOPS 2016 - International Invitation PHILIPPINEMl Phil0% (3)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Manual Analizador Fluoruro HachDocument92 paginiManual Analizador Fluoruro HachAitor de IsusiÎncă nu există evaluări
- Math5 Q4 Mod10 DescribingAndComparingPropertiesOfRegularAndIrregularPolygons v1Document19 paginiMath5 Q4 Mod10 DescribingAndComparingPropertiesOfRegularAndIrregularPolygons v1ronaldÎncă nu există evaluări
- Fernandez ArmestoDocument10 paginiFernandez Armestosrodriguezlorenzo3288Încă nu există evaluări
- Mercedes BenzDocument56 paginiMercedes BenzRoland Joldis100% (1)
- Oracle Learning ManagementDocument168 paginiOracle Learning ManagementAbhishek Singh TomarÎncă nu există evaluări
- Algorithms For Image Processing and Computer Vision: J.R. ParkerDocument8 paginiAlgorithms For Image Processing and Computer Vision: J.R. ParkerJiaqian NingÎncă nu există evaluări
- FSRH Ukmec Summary September 2019Document11 paginiFSRH Ukmec Summary September 2019Kiran JayaprakashÎncă nu există evaluări
- Towards A Human Resource Development Ontology Combining Competence Management and Technology-Enhanced Workplace LearningDocument21 paginiTowards A Human Resource Development Ontology Combining Competence Management and Technology-Enhanced Workplace LearningTommy SiddiqÎncă nu există evaluări
- CR Vs MarubeniDocument15 paginiCR Vs MarubeniSudan TambiacÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Portfolio Artifact Entry Form - Ostp Standard 3Document1 paginăPortfolio Artifact Entry Form - Ostp Standard 3api-253007574Încă nu există evaluări
- Merchandising Calender: By: Harsha Siddham Sanghamitra Kalita Sayantani SahaDocument29 paginiMerchandising Calender: By: Harsha Siddham Sanghamitra Kalita Sayantani SahaSanghamitra KalitaÎncă nu există evaluări
- Theory of Linear Programming: Standard Form and HistoryDocument42 paginiTheory of Linear Programming: Standard Form and HistoryJayakumarÎncă nu există evaluări
- PointerDocument26 paginiPointerpravin2mÎncă nu există evaluări
- TDS Sibelite M3000 M4000 M6000 PDFDocument2 paginiTDS Sibelite M3000 M4000 M6000 PDFLe PhongÎncă nu există evaluări
- Sarvali On DigbalaDocument14 paginiSarvali On DigbalapiyushÎncă nu există evaluări
- 8.1 Interaction Diagrams: Interaction Diagrams Are Used To Model The Dynamic Aspects of A Software SystemDocument13 pagini8.1 Interaction Diagrams: Interaction Diagrams Are Used To Model The Dynamic Aspects of A Software SystemSatish JadhaoÎncă nu există evaluări
- Ancient Greek Divination by Birthmarks and MolesDocument8 paginiAncient Greek Divination by Birthmarks and MolessheaniÎncă nu există evaluări
- The European Journal of Applied Economics - Vol. 16 #2Document180 paginiThe European Journal of Applied Economics - Vol. 16 #2Aleksandar MihajlovićÎncă nu există evaluări
- Onan Service Manual MDJA MDJB MDJC MDJE MDJF Marine Diesel Genset Engines 974-0750Document92 paginiOnan Service Manual MDJA MDJB MDJC MDJE MDJF Marine Diesel Genset Engines 974-0750GreenMountainGenerators80% (10)
- Modified Syllabus of Control SystemDocument2 paginiModified Syllabus of Control SystemDigambar PatilÎncă nu există evaluări
- Sri S T Kalairaj, Chairman: Income Tax TaxesDocument3 paginiSri S T Kalairaj, Chairman: Income Tax TaxesvikramkkÎncă nu există evaluări
- 2023-Physics-Informed Radial Basis Network (PIRBN) A LocalDocument41 pagini2023-Physics-Informed Radial Basis Network (PIRBN) A LocalmaycvcÎncă nu există evaluări
- Hindustan Motors Case StudyDocument50 paginiHindustan Motors Case Studyashitshekhar100% (4)
- Additional Help With OSCOLA Style GuidelinesDocument26 paginiAdditional Help With OSCOLA Style GuidelinesThabooÎncă nu există evaluări
- M8-2 - Train The Estimation ModelDocument10 paginiM8-2 - Train The Estimation ModelJuan MolinaÎncă nu există evaluări
- Case Study Hotel The OrchidDocument5 paginiCase Study Hotel The Orchidkkarankapoor100% (4)
- Oxford Digital Marketing Programme ProspectusDocument12 paginiOxford Digital Marketing Programme ProspectusLeonard AbellaÎncă nu există evaluări
- Multiple Choice: CH142 Sample Exam 2 QuestionsDocument12 paginiMultiple Choice: CH142 Sample Exam 2 QuestionsRiky GunawanÎncă nu există evaluări
- Social Media Exposure and Its Perceived Impact On Students' Home-Based Tasks ProductivityDocument9 paginiSocial Media Exposure and Its Perceived Impact On Students' Home-Based Tasks ProductivityJewel PascuaÎncă nu există evaluări
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (13)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipDe la EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipEvaluare: 4.5 din 5 stele4.5/5 (1135)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÎncă nu există evaluări