Documente Academic
Documente Profesional
Documente Cultură
Evaluation of Preoperative Pulmonary Risk
Încărcat de
CharlieBrown_QBDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Evaluation of Preoperative Pulmonary Risk
Încărcat de
CharlieBrown_QBDrepturi de autor:
Formate disponibile
14/1/2016
Evaluation of preoperative pulmonary risk
Official reprint from UpToDate
www.uptodate.com 2016 UpToDate
Evaluation of preoperative pulmonary risk
Author
Gerald W Smetana, MD
Section Editors
Talmadge E King, Jr, MD
Andrew D Auerbach, MD, MPH
Natalie F Holt, MD, MPH
Deputy Editor
Lee Park, MD, MPH
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Dec 2015. | This topic last updated: Jan 16, 2015.
INTRODUCTION Postoperative pulmonary complications contribute significantly to overall perioperative
morbidity and mortality. In a study of patients undergoing elective abdominal surgery, as an example, pulmonary
complications occurred significantly more often than cardiac complications and were associated with
significantly longer hospital stays [1]. The National Surgical Quality Improvement Program (NSQIP) also found
that postoperative pulmonary complications were the most costly of major postoperative medical complications
(including cardiac, thromboembolic, and infectious) and resulted in the longest length of stay [2].
The field of preoperative pulmonary evaluation is increasingly driven by evidence-based medicine, rather than
expert opinion. As the impact of pulmonary complications following surgery has become increasingly apparent,
estimation of their risk should be a standard element of all preoperative medical evaluations.
The definition of postoperative pulmonary complications, pertinent anesthetic physiology, identification of patient
and procedure-related risk factors, and the role of preoperative pulmonary function testing and pulmonary risk
indices will be reviewed here. Strategies for reducing postoperative pulmonary complications and the evaluation
of candidates for lung resection surgery are discussed separately. (See "Strategies to reduce postoperative
pulmonary complications" and "Preoperative evaluation for lung resection".)
DEFINITION OF POSTOPERATIVE PULMONARY COMPLICATIONS The reported frequency of
postoperative pulmonary complications in the literature varies from 2 to 70 percent. This wide range is due in
part to patient selection and procedure-related risk factors, although differing definitions for postoperative
complications account for much of the variability and make comparison of reported incidences across different
studies difficult.
One broad definition of postoperative pulmonary complications includes all patients with fever and either
pulmonary signs, symptoms (eg, productive cough, rhonchi, or diminished breath sounds), or changes on chest
x-ray (eg, atelectasis, consolidation, or incomplete expansion) [3,4]. However, many such liberally defined
postoperative complications are of no clinical relevance.
Another proposed definition is a pulmonary abnormality that produces identifiable disease or dysfunction that is
clinically significant and adversely affects the clinical course [5]. This would include several major categories of
clinically significant complications, including [6,7]:
Atelectasis
Infection, including bronchitis and pneumonia
Prolonged mechanical ventilation and respiratory failure
Exacerbation of underlying chronic lung disease
Bronchospasm
The rate of postoperative pulmonary complications across all types of surgery was 6.8 percent in a systematic
review of studies that provided explicit outcome definitions [8].
PERIOPERATIVE PULMONARY PHYSIOLOGY Postoperative pulmonary complications follow logically as
an extension of normal perioperative pulmonary physiology. Reduced lung volume after surgery is a major factor
contributing to the development of postoperative pulmonary complications.
Thoracic and upper-abdominal surgery are associated with a reduction in lung volumes in a restrictive pattern as
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
1/19
14/1/2016
Evaluation of preoperative pulmonary risk
follows [9,10]:
Vital capacity (VC) is reduced by 50 to 60 percent and may remain decreased for up to one week.
Functional residual capacity (FRC) is reduced by about 30 percent.
Diaphragmatic dysfunction appears to play the most important role in these changes; postoperative pain and
splinting are also factors [11]. Reduction of the FRC below closing volumes contributes to the risk of
atelectasis, pneumonia, and ventilation/perfusion (V/Q) mismatching. Microatelectasis results in areas of the
lung that are perfused but not ventilated, leading to impaired gas exchange with consequent postoperative
hypoxemia [12].
A decrease in tidal volume, loss of sighing breaths, and increase in respiratory rate occur after abdominal and
thoracic surgery and contribute to the risk of complications. In addition, residual effects of anesthetic agents
and postoperative opioids both depress the respiratory drive. Inhibition of cough and impairment of mucociliary
clearance of respiratory secretions are factors that contribute to the risk of postoperative infection [13].
Lower abdominal surgery is associated with similar changes but to a lesser degree. Reductions in lung volumes
are not seen with surgery on the extremities [14].
PATIENT-RELATED RISK FACTORS Risk factors for pulmonary complications can be grouped into patientrelated and procedure-related risks. The potential patient-related factors that have been studied include the
following:
Age
Chronic obstructive pulmonary disease
Asthma
Smoking
General health status
Obesity
Obstructive sleep apnea
Pulmonary hypertension
Heart failure
Upper-respiratory infection
Metabolic factors
Age The influence of age as an independent predictor of postoperative pulmonary complications has been
questioned. Early studies suggested an increased risk of pulmonary complications with advanced age [15].
These studies, however, were not adjusted for overall health status or the presence of known pulmonary
disease, and subsequent studies did not reliably demonstrate age as a predictor of postoperative complications
[16,17]. The risk of surgical mortality was similar across age groups when stratified by American Society of
Anesthesiologists (ASA) class (table 1) [18].
A systematic review prepared for the American College of Physicians estimated the impact of age on
postoperative pulmonary complications among studies that used multivariable analysis to adjust for age-related
comorbidities [8]. This review made the novel observation that age >50 years was an important independent
predictor of risk. When compared to patients <50 years old, patients aged 50 to 59 years, 60 to 69 years, 70 to
79 years, and 80 years had odds ratios (OR) of 1.50 (CI 1.31-1.71), 2.28 (CI 1.86-2.80), 3.90 (CI 2.70-5.65),
and 5.63 (CI 4.63-6.85), respectively of developing pulmonary complications. Therefore, even healthy older
patients carry a substantial risk of pulmonary complications after surgery. This is in sharp contrast to
perioperative cardiac risk. (See "Evaluation of cardiac risk prior to noncardiac surgery".)
Chronic obstructive pulmonary disease (COPD) Known COPD is an important patient-related risk factor
for postoperative pulmonary complications. Unadjusted relative risks of postoperative pulmonary complications
have ranged from 2.7 to 6.0 [19].
In a retrospective cohort study, compared with patients who did not have COPD, those with severe COPD were
six times more likely to have major postoperative pulmonary complications after abdominal or thoracic surgery
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
2/19
14/1/2016
Evaluation of preoperative pulmonary risk
[20]. In another case control study, increased postoperative complications were associated with physical
findings of decreased breath sounds, prolonged expiration, rales, wheezes, or rhonchi [21]. In a multivariate
regression model, important predictors of complications were age 65 or greater (OR 1.8), smoking 40 packyears or more (OR 1.9), and maximum laryngeal height of 4 cm or less (distance from the top of the thyroid
cartilage to the suprasternal notch at end expiration, known to be an accurate sign of COPD) [22].
A systematic review found that among studies that used multivariable analysis to adjust for patient-related
confounders, the odds ratio for postoperative pulmonary complications attributable to COPD was 2.36 (CI 1.902.93) [8]. In a subsequent observational study using the National Surgical Quality Improvement Program
(NSQIP) database including over 450,000 patients, after adjusting for confounders, the presence of COPD was
an independent predictor for postoperative pneumonia (OR 1.71, 95% CI 1.59-1.83), reintubation (OR 1.54, 95%
CI 1.42-1.66), failure to wean from the ventilator (OR 1.45, 95% CI 1.35-1.56), in addition to non-pulmonary
adverse outcomes [23].
Despite the increased risk of postoperative pulmonary complications in patients with obstructive lung disease,
there appears to be no prohibitive level of pulmonary function below which surgery is absolutely contraindicated.
This was illustrated in a study of 12 very high-risk patients as defined by older criteria of inoperability (FEV1 <1
liter) in which only 3 of 15 surgeries were associated with postoperative complications and no deaths occurred
[24]. In another report of surgery in patients with severe COPD (FEV1 <50 percent predicted), mortality was 5.6
percent (primarily related to a high mortality rate after cardiac surgery) and severe postoperative pulmonary
complications occurred in 6.5 percent [17]. The benefit of surgery must be weighed against the known risks;
even very high-risk patients may proceed to surgery if the indication is sufficiently compelling. (See "Strategies
to reduce postoperative pulmonary complications", section on 'Chronic obstructive lung disease'.)
Asthma Despite early reports indicating that patients with asthma had higher than expected rates of
postoperative pulmonary complications, more recent studies have found no link for patients with well-controlled
asthma. (See "Anesthesia for adult patients with asthma", section on 'Preoperative evaluation'.)
Smoking Current cigarette smokers have an increased risk for postoperative pulmonary complications;
smoking cessation at least four weeks prior to surgery reduces the risk of postoperative complications, and
longer periods of smoking cessation may be even more effective [3]. (See "Strategies to reduce postoperative
pulmonary complications", section on 'Smoking cessation'.)
In a 2014 meta-analysis of 107 cohort and case-control studies, preoperative smoking was associated with an
increased risk of postoperative complications, including pulmonary complications (RR 1.73, 95% CI 1.35-2.23)
[25]. Smokers with a greater than 20 pack-year smoking history have a higher incidence of postoperative
pulmonary complications than those with a lesser pack-year history [26].
Obesity Physiologic changes that accompany morbid obesity include reduction in lung volumes,
ventilation/perfusion mismatch, and relative hypoxemia [27]. These findings might be expected to accentuate
similar changes seen with anesthesia and increase the risk of pulmonary complications.
However, obesity has not consistently been shown to be a risk factor for postoperative pulmonary
complications. A review of 10 series of obese gastric bypass patients, as an example, showed a 3.9 percent
incidence of pneumonia and atelectasis, a rate similar to that seen in the general population [27]. Similarly, in a
second prospective study of 117 patients undergoing thoracic surgery, there was no difference in the rate of
pulmonary complications when patients were stratified by body mass index (BMI) [28].
In contrast, a prospective report of 1000 patients undergoing laparotomy found obesity, as defined by BMI >25
kg/m2, to be an independent risk factor for postoperative pulmonary complications [6]. In addition, a prospective
study of 400 patients undergoing abdominal surgery found obesity (BMI >27 kg/m2) to be one of six
independent risk factors for pulmonary complications [29].
The discrepancy between these reports may arise in part because many studies do not adequately distinguish
between obesity itself and comorbid conditions. A prospective study of 272 patients referred for medical
evaluation before nonthoracic surgery that used explicit criteria for postoperative pulmonary complications found
an odds ratio of 4.1 for pulmonary complications in patients with a BMI 30 kg/m2, but in a multivariate model
this ceased to be a significant factor [30]. A systematic review found that, among eight studies using
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
3/19
14/1/2016
Evaluation of preoperative pulmonary risk
multivariate analysis, only one study identified obesity as an independent predictor [8].
Obesity is not a significant risk factor for postoperative pulmonary complications and should not affect patient
selection for otherwise high-risk procedures.
Obstructive sleep apnea Obstructive sleep apnea (OSA) is a risk factor for pulmonary (and other)
complications after surgery. This is discussed in detail elsewhere. (See "Surgical risk and the preoperative
evaluation and management of adults with obstructive sleep apnea", section on 'Perioperative risks' and
"Overview of obstructive sleep apnea in adults".)
Many patients who are preparing for surgery have undiagnosed OSA. Screening for OSA prior to surgery is
discussed in detail elsewhere. (See "Surgical risk and the preoperative evaluation and management of adults
with obstructive sleep apnea", section on 'Initial assessment'.)
Pulmonary hypertension Pulmonary hypertension increases complication rates after surgery, including in
patients with mild to moderate pulmonary hypertension [31]. This appears to be true regardless of the underlying
etiology of the pulmonary hypertension. As an illustration, authors studied 145 surgical patients with pulmonary
hypertension, excluding those where the condition was due to left heart disease [32]. Complications included
respiratory failure (n = 41), cardiac dysrhythmias (n = 17), congestive heart failure (n = 16), renal insufficiency (n
= 10), and sepsis (n = 10). Risk predictors included a history of pulmonary embolus, NYHA functional class 2,
intermediate or high risk surgery, and duration of anesthesia >3 hours.
A subsequent study compared 62 patients with pulmonary hypertension of any etiology to matched controls
[33]. Mortality (10 percent versus 0) and major morbidity (24 versus 3 percent) were both significantly higher
among patients with pulmonary hypertension. The increased risk warrants careful consideration of indications for
surgery and discussion of potential risks with patients with pulmonary hypertension.
In one administrative database, there was a marked increase in perioperative mortality for orthopedic patients
with pulmonary hypertension (n = 3543), compared to matched controls (OR 3.72, 95% CI 2.13-6.39 for hip
replacement, OR 4.55, 95% CI 2.16-9.39 for knee replacement) [34]. A limitation was the use of ICD-9 coding
for comorbidities which underestimates the prevalence of pulmonary hypertension.
Heart failure The risk of pulmonary complications may be higher in patients with heart failure than in those
with chronic obstructive pulmonary disease. This is suggested by data from the systematic review that formed
the basis of the American College of Physicians guideline, in which the pooled adjusted odds ratio for
pulmonary complications was 2.93 (95% CI 1.02-8.43) for heart failure patients and 2.36 (1.90-2.93) for patients
with chronic obstructive pulmonary disease [8].
The original Goldman cardiac risk index has been shown to predict postoperative pulmonary as well as cardiac
complications [21]. Although the Revised Cardiac Risk Index is now more commonly used to estimate risk for
cardiovascular complications, validation studies of the revised index in predicting pulmonary complications have
not been done. (See "Evaluation of cardiac risk prior to noncardiac surgery".)
General health status Overall health status is an important determinant of pulmonary risk. Functional
dependence and impaired sensorium each increase postoperative pulmonary risk [8].
The commonly used American Society of Anesthesiologists (ASA) classification correlates well with pulmonary
risk (table 1) [6,16,17]. The criteria for assigning ASA class include the presence of a systemic disease that
affects activity or is a threat to life. Thus, patients with significant preexisting lung disease would be classified in
a higher ASA class. ASA class >2 confers a 4.87 fold increase in risk (95% CI 3.34-7/10) [8].
ASA 1: Healthy.
ASA 2: Mild systemic disease (eg, well-controlled hypertension, stable, asthma, diabetes mellitus).
ASA 3: Severe systemic disease (eg, history of angina, COPD, poorly controlled hypertension, morbid
obesity).
ASA 4: Severe systemic disease with a constant threat to life (eg, history of unstable angina, uncontrolled
diabetes or hypertension, advanced renal, pulmonary, or hepatic dysfunction).
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
4/19
14/1/2016
Evaluation of preoperative pulmonary risk
ASA 5: Moribund patient not expected to survive without operation (eg, ruptured aortic aneurysm).
ASA 6: A declared brain-dead patient whose organs are being removed for donor purposes.
Upper respiratory infection Data regarding the risk of pulmonary complications among adults undergoing
high-risk surgical procedures with current or recent upper respiratory infection are limited. Most of the data
regarding the impact of URIs on perioperative morbidity are for children undergoing surgery. Children with active
URIs have more minor postoperative respiratory events such as oxygen desaturation, but no apparent increase
in major morbidity or long-term sequelae [35]. Whether the same applies to surgical outcomes in adults is
unknown. However, it would seem wise to defer elective surgery in this setting.
Metabolic factors A multifactorial risk index for postoperative respiratory failure identified two metabolic risk
factors [36]. Albumin less than 3 g/dL and blood urea nitrogen (BUN) greater than 30 mg/dL each predicted risk;
odds ratios were 2.53 and 2.29, respectively. A systematic review found that the magnitude of risk associated
with a low serum albumin was similar to the degree of the most important patient-related risk factors and a
stronger predictor of risk than an elevated BUN [8].
PROCEDURE-RELATED RISK FACTORS Surgical factors that may potentially affect pulmonary risk include
the following:
Surgical site
Duration of surgery
Type of anesthesia
Type of neuromuscular blockade
Additionally, emergency surgery increases the risk for pulmonary complications [37].
Surgical site Surgical site is the single most important factor in predicting the overall risk of postoperative
pulmonary complications; the incidence of complications is inversely related to the distance of the surgical
incision from the diaphragm. Thus, the complication rate is significantly higher for thoracic and upper abdominal
surgery than for lower abdominal and all other procedures [7,16,29]. In a systematic review of 83 univariate
studies, complication rates for upper abdominal surgery, lower abdominal surgery, and esophagectomy were
19.7, 7.7, and 18.9 percent, respectively [8]. The higher rates of complications in upper versus lower abdominal
surgery relate to the effect upon respiratory muscles and diaphragmatic function. Abdominal aortic aneurysm
repair is also associated with a high risk of postoperative pulmonary complications [36]. Other high risk
procedures include head and neck surgery and neurosurgery [38,39].
Laparoscopic cholecystectomy is associated with shorter recovery times, less postoperative pain, and less
reduction in postoperative lung volumes [8]. Its impact on pulmonary complication rates is less well established.
While the decrease in postoperative pain might be expected to translate into lower pulmonary complication
rates, few studies have evaluated clinically important pulmonary complications as an endpoint. In a pooled
analysis of 12 studies of laparoscopic versus open colon cancer surgery, there was a nonsignificant trend
towards reduced pulmonary complications (OR 0.65, CI 0.28-1.49) [8].
Duration of surgery Surgical procedures lasting more than three to four hours are associated with a higher
risk of pulmonary complications [29,30,40,41]. As an example, a study of risk factors for postoperative
pneumonia in 520 patients found an incidence of 8 percent for surgeries lasting less than two hours versus 40
percent for procedures lasting more than four hours [16]. This observation suggests that, when available, a less
ambitious, briefer procedure should be considered in a very high risk patient.
Type of anesthesia There are conflicting data with regard to the pulmonary risk of spinal or epidural
anesthesia when compared with general anesthesia [42]. One study, as an example, found no difference in the
rate of pulmonary complications between patients undergoing transurethral prostate surgery with spinal
anesthesia and those undergoing general surgery with general anesthesia [7]. These findings were confirmed in
a second report of patients undergoing abdominal surgery [40].
In contrast, an early retrospective study of 475 men with chronic lung disease undergoing general surgery
revealed a 9 percent incidence of death in the general anesthesia group compared with no deaths in the spinal
anesthesia group [43]. These findings have been subsequently supported by others [41], including a review of
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
5/19
14/1/2016
Evaluation of preoperative pulmonary risk
high-risk patients that found that the rate of respiratory failure was significantly higher with general anesthesia
than with epidural analgesia and light anesthesia [44].
Subsequently, investigators conducted the largest systematic review of this literature to date [45]. The review
evaluated the results of 141 trials that included 9559 patients. They reported a reduction in risk of pulmonary
complications among patients receiving neuraxial blockade (either epidural or spinal anesthesia) with or without
general anesthesia, when compared to those receiving general anesthesia alone. Patients receiving neuraxial
blockade had an overall 39 percent reduction in the risk of pneumonia and a 59 percent decrease in the risk of
respiratory depression. Potential limitations of the review include study heterogeneity and small sample size.
Based upon this comprehensive review, it appears likely that general anesthesia leads to a higher risk of
clinically important pulmonary complications than does epidural or spinal anesthesia, although further studies
are required to confirm this observation.
Regional nerve block is associated with lower risk and should be considered when possible for high risk patients
[14]. As an example, an axillary block with conscious sedation could be used for an upper extremity procedure.
Type of neuromuscular blockade Residual neuromuscular blockade can cause diaphragmatic
dysfunction, impaired mucociliary clearance, and ultimately contribute to postoperative pulmonary
complications. Pancuronium, a long-acting neuromuscular blocker, leads to a higher incidence of postoperative
residual neuromuscular blockade compared to shorter acting agents [46]. Residual neuromuscular blockade is
also an important risk factor for critical respiratory events in the immediate postoperative period [47]. (See
"Strategies to reduce postoperative pulmonary complications".)
PREOPERATIVE RISK ASSESSMENT A complete history and physical examination are the most important
elements of preoperative risk assessment [21,29]. Significant risk factors, as defined above, should be
identified. Any history suggesting unrecognized chronic lung disease or heart failure, such as exercise
intolerance, unexplained dyspnea, or cough, requires further consideration. It is unknown whether screening for
sleep apnea will affect surgical complication rates, but it is reasonable to question obese patients about
symptoms that may suggest obstructive sleep apnea prior to major surgery, in particular, the four question
STOP questionnaire [48]. (See "Surgical risk and the preoperative evaluation and management of adults with
obstructive sleep apnea", section on 'Screening for OSA'.)
Physical examination should be directed toward evidence for obstructive lung disease, especially noting
decreased breath sounds, wheezes, rhonchi, or prolonged expiratory phase [29]. In addition, measurement of
oxygen saturation by oximetry helps to stratify risk and is useful before high-risk surgeries [49].
All candidates for lung resection should have preoperative pulmonary function tests performed (see "Preoperative
evaluation for lung resection"). For all other procedures, laboratory tests serve as adjuncts to the clinical
evaluation and should be obtained only in selected patients. Potential preoperative laboratory tests include the
following:
Pulmonary function tests (PFTs)
Arterial blood gas analysis
Chest radiographs
Exercise testing
Pulmonary function testing There is considerable debate regarding the role of preoperative pulmonary
function testing for risk stratification [50]. These tests simply confirm the clinical impression of disease severity
in most cases, adding little to the clinical estimation of risk. There has also been concern that preoperative
PFTs are overused and a source of wasted health care dollars [51].
A number of measures of pulmonary function have been evaluated. Bedside spirometry is widely available, and
measures of the forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) have been
frequently reported. Early reviews suggested criteria for increased risk that included the following [52]:
FEV1 <70 percent predicted
FVC <70 percent predicted
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
6/19
14/1/2016
Evaluation of preoperative pulmonary risk
FEV1/FVC ratio <65 percent
Two reasonable goals that could potentially justify the use of preoperative PFTs:
Identification of a group of patients for whom the risk of the proposed surgery is not justified by the benefit.
Identification of a subset of patients at higher risk for whom aggressive perioperative management is
warranted.
There is little support from the literature that either of these goals is routinely met other than for lung resection
surgery. As an example, in a study of patients with severe COPD (FEV1 <50 percent predicted), preoperative
PFTs did not predict the risk of pulmonary complications, whereas length of surgery, ASA class, and type of
procedure were all significant predictors [29]. Similarly, in a case control study of 164 patients undergoing
abdominal surgery, no component of spirometry predicted pulmonary complications [29].
A critical review of preoperative pulmonary function testing evaluated 14 studies that met strict methodologic
criteria [8]. Spirometric values were significant risk predictors in three of four studies that used multivariable
analysis. However, other factors conferred higher odds ratios for pulmonary complications than did abnormal
spirometry in two of these studies: ASA class >3 [53] and chronic mucous hypersecretion [54].
Two well designed case-control studies have evaluated the benefit of PFTs as risk predictors. In a study of
patients undergoing abdominal surgery, there was no difference in FEV1, FVC, or FEV1/FVC between patients
who had a pulmonary complication and those who did not [29]. In contrast, factors from the physical
examination did predict risk. In a second report, investigators matched smokers with severe airflow obstruction
and an FEV1 of less than 40 percent of predicted to smokers with a normal FEV1 [55]. Only bronchospasm
was more common among those patients with abnormal spirometry. The incidence of postoperative pneumonia,
prolonged intubation, prolonged intensive care unit stay, and death were not significantly different between the
two groups.
Few studies have compared the incremental value obtained by spirometry with the risk estimate based on
clinical evaluation. Most patients with abnormal spirometry would be identified based on history and physical
examination.
Recommendations Based on a systematic review, a 2006 American College of Physicians guideline
recommends that clinicians not use preoperative spirometry routinely for predicting the risk of postoperative
pulmonary complications [37].
A reasonable approach to patient selection for preoperative pulmonary function testing follows:
Obtain PFTs for patients with COPD or asthma if clinical evaluation cannot determine if the patient is at
their best baseline and that airflow obstruction is optimally reduced. In this case, PFTs may identify
patients who will benefit from more aggressive preoperative management.
Obtain PFTs for patients with dyspnea or exercise intolerance that remains unexplained after clinical
evaluation. In this case, the differential diagnosis may include cardiac disease or deconditioning. The
results of PFTs may change preoperative management.
PFTs should not be used as the primary factor to deny surgery
PFTs should not be ordered routinely prior to abdominal surgery or other high risk surgeries
Arterial blood gas analysis No data suggest that the finding of hypercapnia identifies high-risk patients who
would not have otherwise been identified based upon established clinical risk factors. Several small case series
have suggested a high risk of postoperative pulmonary complications among patients with a PaCO2 >45 mmHg,
a finding usually seen only in patients with severe chronic obstructive lung disease [14,24]. The risk associated
with this degree of PaCO2 elevation is not necessarily prohibitive, although it should lead to a reassessment of
the indication for the proposed procedure and aggressive preoperative preparation.
One study reported an association between preoperative hypoxemia and postoperative pulmonary complications
among 102 patients undergoing surgery for gastric or esophageal cancer [56]. However, hypoxemia has
generally not been identified as a significant independent predictor of complications after adjustment for potential
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
7/19
14/1/2016
Evaluation of preoperative pulmonary risk
confounders.
Current data do not support the use of preoperative arterial blood gas analyses to stratify risk for postoperative
pulmonary complications.
Chest radiographs Abnormal chest x-rays are seen with increasing frequency with age. However, chest xrays add little to the clinical evaluation in identifying healthy patients at risk for perioperative complications. As
an example, one study screened 905 surgical admissions for the presence of clinical factors that were thought
to be risk factors for an abnormal preoperative chest x-ray [57]. These risk factors were age over 60 years or
clinical findings consistent with cardiac or pulmonary disease. No risk factors were evident in 368 patients; of
these, only one (0.3 percent) had an abnormal chest x-ray, which did not affect the surgery. On the other hand,
504 patients had identifiable risk factors; of these, 114 (22 percent) had significant abnormalities on preoperative
chest x-ray. (See "Preoperative medical evaluation of the healthy patient".)
A meta-analysis of studies of routine preoperative chest x-rays demonstrated a low yield for abnormalities that
actually change preoperative management [58]. Of 14,390 preoperative x-rays, there were only 140 unexpected
abnormalities and only 14 cases where the chest x-ray was abnormal and influenced management.
The prevalence of abnormal preoperative chest radiographs increases with age. As an example, in a review of
studies published between 1976 and 1999, 21.1 percent of all preoperative chest radiographs were abnormal,
but the prevalence of abnormal studies for patients under age 50 years old was only 4.9 percent.
The available literature does not allow an evidence-based determination of which patients will benefit from a
preoperative chest x-ray. In the opinion of the author, it is reasonable to obtain a preoperative chest x-ray in
patients with known cardiopulmonary disease and in those over age 50 years undergoing high risk surgical
procedures, including upper abdominal, aortic, esophageal, and thoracic surgery.
Exercise testing Exercise testing has been studied most extensively in preparation for lung resection
surgery. (See "Preoperative evaluation for lung resection".)
In addition, cardiopulmonary exercise testing with a calculation of maximum oxygen intake and ventilatory
anaerobic threshold may have a role in the evaluation of patients with unexplained dyspnea who are undergoing
noncardiopulmonary surgery. In one systematic review, a majority of nine eligible studies found that both
measurements predicted survival and overall postoperative complications [59]. The studies did not measure
postoperative pulmonary complication as a separate outcome. It is unknown to what extent this test adds value
to the risk estimate obtained after a careful history and physical examination.
ASSESSMENT OF POSTOPERATIVE PULMONARY RISK Risk prediction tools use preoperative factors to
estimate the risk of postoperative pulmonary complications. These tools are useful to stratify risk when advising
patients before surgery and, in some cases, to identify patients most likely to benefit from risk-reduction
interventions For example, patients predicted to be at high risk of postoperative respiratory failure may be
scheduled for postoperative care in a more intensive care location. A variety of tools are available. All four risk
indices offer the advantage of providing a numerical estimate of risk, rather than a qualitative category of risk.
(see "Strategies to reduce postoperative pulmonary complications")
The ARISCAT (Canet) tool offers the advantage of the use of readily available clinical information and provides an
estimate of the risk of any postoperative pulmonary complication, but the disadvantage of the inclusion of minor
complications that may not impact outcome or contribute importantly to morbidity. The two Gupta risk
calculators will be particularly helpful to establish the risk of a single complication, either pneumonia or
respiratory failure, although they need to be downloaded to a personal device to perform the calculations. The
Arozullah index will be of use primarily in research settings, as the tool is too complicated to use in clinical
practice.
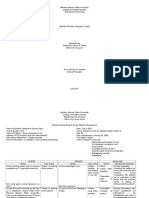
ARISCAT (Canet) The ARISCAT Risk Index (calculator 1) predicts the overall incidence of postoperative
pulmonary complications (of any severity), by assigning a weighted point score to seven independent risk
factors (table 2) [49]:
Advanced age
Low preoperative oxygen saturation
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
8/19
14/1/2016
Evaluation of preoperative pulmonary risk
Respiratory infection within the past month
Preoperative anemia
Upper abdominal or thoracic surgery
Surgery lasting more than two hours
Emergency surgery
The incidence of pulmonary complications in patients with scores stratified as low-, intermediate-, and high-risk
is 1.6, 13.3, and 42.2 percent, respectively.
This index has the advantage of being simple to calculate manually at the bedside with readily available clinical
information, but the disadvantage of inclusion of minor complications of little clinical significance (eg, new
wheezing treated with bronchodilators). It was derived from a prospective evaluation of 2464 surgical patients
and validated in a cohort of 5099 patients in Europe [60].
Arozullah respiratory failure index The Arozullah respiratory failure index predicts the incidence of
postoperative respiratory failure (mechanical ventilation for 48 hours) based on several factors, including type of
surgery, laboratory results, functional status, history of COPD, and age (table 3A-B) [36]. Point scores are
stratified into five classes with risk of respiratory failure ranging from 0.5 to 26.6 percent.
This index was based on multivariate analysis of a cohort of 81,719 patients from the National Veterans
Administration Surgical Quality Improvement Program and validated on another 99,390 patients. It is also simple
to calculate manually at the bedside and relies upon readily available clinical information.
Gupta calculator for postoperative respiratory failure The Gupta calculator for postoperative respiratory
failure uses multiple preoperative factors to predict risk of failure to wean from mechanical ventilation within 48
hours of surgery or unplanned intubation/reintubation postoperatively [61]. It is derived from the American
College of Surgeons National Surgical Quality Improvement 2007 data set (211,410 patients for training) and
2008 data set (257,385 patients for validation) using logistic regression techniques to determine the weight of
preoperative predictors. Although this calculator is too complicated to perform manually, it may be downloaded
for free, or accessed online [62].
Gupta calculator for postoperative pneumonia The Gupta calculator for postoperative pneumonia was
derived in a similar manner to the respiratory failure calculator [63]. It also may be downloaded for free online
[64].
SUMMARY AND RECOMMENDATIONS
Postoperative pulmonary complications are an important source of perioperative morbidity and mortality.
They represent an extension of the normal physiologic changes in the lung that occur with anesthesia.
Definite risk factors for these complications include the following: age >50 years, chronic obstructive
pulmonary disease, congestive heart failure, poor general health status (ASA class >2), functional
dependence, obstructive sleep apnea, current cigarette use, pulmonary hypertension, low oxygen
saturation, serum albumin <35 gm/L, surgery lasting greater than three hours, emergency surgery, use of
pancuronium as a neuromuscular blocker, and upper abdominal, thoracic, aortic, head and neck,
neurosurgery, and abdominal aortic aneurysm surgery. (See 'Patient-related risk factors' above and
'Procedure-related risk factors' above.)
Probable risk factors include the following: general anesthesia (compared to spinal or epidural anesthesia),
PaCO2 >45 mmHg, abnormal chest radiograph, cigarette use within the previous eight weeks, and current
upper respiratory tract infection. (See 'Patient-related risk factors' above and 'Procedure-related risk factors'
above.)
A careful history and physical examination are the most important tools for preoperative risk assessment
in evaluating patients for potential postoperative pulmonary complications. Attention should be paid to
symptoms that suggest the possibility of occult underlying lung disease, including exercise intolerance,
cough, and unexplained dyspnea. In addition, the clinician should seek a history of the risk factors for
postoperative pulmonary complications. A high-risk patient will benefit from aggressive strategies to reduce
pulmonary complications (algorithm 1). (See 'Preoperative risk assessment' above and "Strategies to
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchTe
9/19
14/1/2016
Evaluation of preoperative pulmonary risk
reduce postoperative pulmonary complications".)
Potential preoperative laboratory tests include pulmonary function tests (PFTs), chest radiographs, and
exercise testing.
All candidates for lung resection should have preoperative pulmonary function tests performed. For all other
procedures, laboratory tests serve as adjuncts to the clinical evaluation and should be obtained only in
selected patients.
In patients undergoing high-risk surgery who are over age 50 years, or who have cardiac or pulmonary
disease suggested by the clinical evaluation, a chest radiograph within the past six months is needed.
Pulmonary function tests should be reserved for patients with uncharacterized dyspnea or exercise
intolerance and for those with COPD or asthma where clinical evaluation cannot determine if airflow
obstruction has been optimally reduced. The benefit of PFTs in other situations is unproven. There is no
role for preoperative arterial blood gas analyses to identify high-risk patients or to deny surgery. (See
'Preoperative risk assessment' above.)
Four different pulmonary risk indices are available to provide a quantitative estimate of the risk of
respiratory failure, pneumonia, or general pulmonary complications. Each risk index has different strengths
and weaknesses. We use the ARISCAT index (calculator 1). These tools are a useful starting point when
estimating pulmonary risk after major noncardiac surgery, and they guide conversations with the patient
and surgeon. (See 'Assessment of postoperative pulmonary risk' above.)
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. Lawrence VA, Hilsenbeck SG, Mulrow CD, et al. Incidence and hospital stay for cardiac and pulmonary
complications after abdominal surgery. J Gen Intern Med 1995; 10:671.
2. Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report
from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004; 199:531.
3. Wightman JA. A prospective survey of the incidence of postoperative pulmonary complications. Br J Surg
1968; 55:85.
4. Mohr DN, Jett JR. Preoperative evaluation of pulmonary risk factors. J Gen Intern Med 1988; 3:277.
5. O'Donohue WJ Jr. Postoperative pulmonary complications. When are preventive and therapeutic
measures necessary? Postgrad Med 1992; 91:167.
6. Hall JC, Tarala RA, Hall JL, Mander J. A multivariate analysis of the risk of pulmonary complications after
laparotomy. Chest 1991; 99:923.
7. Gracey DR, Divertie MB, Didier EP. Preoperative pulmonary preparation of patients with chronic
obstructive pulmonary disease: a prospective study. Chest 1979; 76:123.
8. Smetana GW, Lawrence VA, Cornell JE, American College of Physicians. Preoperative pulmonary risk
stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann
Intern Med 2006; 144:581.
9. Meyers JR, Lembeck L, O'Kane H, Baue AE. Changes in functional residual capacity of the lung after
operation. Arch Surg 1975; 110:576.
10. Craig DB. Postoperative recovery of pulmonary function. Anesth Analg 1981; 60:46.
11. Ford GT, Whitelaw WA, Rosenal TW, et al. Diaphragm function after upper abdominal surgery in humans.
Am Rev Respir Dis 1983; 127:431.
12. Marshall BE, Wyche MQ Jr. Hypoxemia during and after anesthesia. Anesthesiology 1972; 37:178.
13. Sugimachi K, Ueo H, Natsuda Y, et al. Cough dynamics in oesophageal cancer: prevention of
postoperative pulmonary complications. Br J Surg 1982; 69:734.
14. Tisi GM. Preoperative evaluation of pulmonary function. Validity, indications, and benefits. Am Rev Respir
Dis 1979; 119:293.
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
10/19
14/1/2016
Evaluation of preoperative pulmonary risk
15. Djokovic JL, Hedley-Whyte J. Prediction of outcome of surgery and anesthesia in patients over 80. JAMA
1979; 242:2301.
16. Mller AM, Maale R, Pedersen T. Postoperative intensive care admittance: the role of tobacco smoking.
Acta Anaesthesiol Scand 2001; 45:345.
17. Kroenke K, Lawrence VA, Theroux JF, Tuley MR. Operative risk in patients with severe obstructive
pulmonary disease. Arch Intern Med 1992; 152:967.
18. Thomas DR, Ritchie CS. Preoperative assessment of older adults. J Am Geriatr Soc 1995; 43:811.
19. Smetana GW. Preoperative pulmonary evaluation. N Engl J Med 1999; 340:937.
20. Kroenke K, Lawrence VA, Theroux JF, et al. Postoperative complications after thoracic and major
abdominal surgery in patients with and without obstructive lung disease. Chest 1993; 104:1445.
21. Lawrence VA, Dhanda R, Hilsenbeck SG, Page CP. Risk of pulmonary complications after elective
abdominal surgery. Chest 1996; 110:744.
22. Straus SE, McAlister FA, Sackett DL, Deeks JJ. The accuracy of patient history, wheezing, and laryngeal
measurements in diagnosing obstructive airway disease. CARE-COAD1 Group. Clinical Assessment of
the Reliability of the Examination-Chronic Obstructive Airways Disease. JAMA 2000; 283:1853.
23. Gupta H, Ramanan B, Gupta PK, et al. Impact of COPD on postoperative outcomes: results from a
national database. Chest 2013; 143:1599.
24. Milledge JS, Nunn JF. Criteria of fitness for anaesthesia in patients with chronic obstructive lung disease.
Br Med J 1975; 3:670.
25. Grnkjr M, Eliasen M, Skov-Ettrup LS, et al. Preoperative smoking status and postoperative
complications: a systematic review and meta-analysis. Ann Surg 2014; 259:52.
26. Warner MA, Divertie MB, Tinker JH. Preoperative cessation of smoking and pulmonary complications in
coronary artery bypass patients. Anesthesiology 1984; 60:380.
27. Pasulka PS, Bistrian BR, Benotti PN, Blackburn GL. The risks of surgery in obese patients. Ann Intern
Med 1986; 104:540.
28. Dales RE, Dionne G, Leech JA, et al. Preoperative prediction of pulmonary complications following
thoracic surgery. Chest 1993; 104:155.
29. Brooks-Brunn JA. Predictors of postoperative pulmonary complications following abdominal surgery.
Chest 1997; 111:564.
30. McAlister FA, Khan NA, Straus SE, et al. Accuracy of the preoperative assessment in predicting
pulmonary risk after nonthoracic surgery. Am J Respir Crit Care Med 2003; 167:741.
31. Price LC, Montani D, Jas X, et al. Noncardiothoracic nonobstetric surgery in mild-to-moderate pulmonary
hypertension. Eur Respir J 2010; 35:1294.
32. Ramakrishna G, Sprung J, Ravi BS, et al. Impact of pulmonary hypertension on the outcomes of
noncardiac surgery: predictors of perioperative morbidity and mortality. J Am Coll Cardiol 2005; 45:1691.
33. Lai HC, Lai HC, Wang KY, et al. Severe pulmonary hypertension complicates postoperative outcome of
non-cardiac surgery. Br J Anaesth 2007; 99:184.
34. Memtsoudis SG, Ma Y, Chiu YL, et al. Perioperative mortality in patients with pulmonary hypertension
undergoing major joint replacement. Anesth Analg 2010; 111:1110.
35. Tait AR, Malviya S. Anesthesia for the child with an upper respiratory tract infection: still a dilemma?
Anesth Analg 2005; 100:59.
36. Arozullah AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting postoperative
respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical
Quality Improvement Program. Ann Surg 2000; 232:242.
37. Qaseem A, Snow V, Fitterman N, et al. Risk assessment for and strategies to reduce perioperative
pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the
American College of Physicians. Ann Intern Med 2006; 144:575.
38. Smetana GW, Macpherson DS. The case against routine preoperative laboratory testing. Med Clin North
Am 2003; 87:7.
39. Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for
predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001; 135:847.
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
11/19
14/1/2016
Evaluation of preoperative pulmonary risk
40. Celli BR, Rodriguez KS, Snider GL. A controlled trial of intermittent positive pressure breathing, incentive
spirometry, and deep breathing exercises in preventing pulmonary complications after abdominal surgery.
Am Rev Respir Dis 1984; 130:12.
41. Pedersen T, Eliasen K, Henriksen E. A prospective study of risk factors and cardiopulmonary
complications associated with anaesthesia and surgery: risk indicators of cardiopulmonary morbidity.
Acta Anaesthesiol Scand 1990; 34:144.
42. Cohen MM, Duncan PG, Tate RB. Does anesthesia contribute to operative mortality? JAMA 1988;
260:2859.
43. Tarhan S, Moffitt EA, Sessler AD, et al. Risk of anesthesia and surgery in patients with chronic bronchitis
and chronic obstructive pulmonary disease. Surgery 1973; 74:720.
44. Yeager MP, Glass DD, Neff RK, Brinck-Johnsen T. Epidural anesthesia and analgesia in high-risk surgical
patients. Anesthesiology 1987; 66:729.
45. Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or
spinal anaesthesia: results from overview of randomised trials. BMJ 2000; 321:1493.
46. Berg H, Roed J, Viby-Mogensen J, et al. Residual neuromuscular block is a risk factor for postoperative
pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary
complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand 1997; 41:1095.
47. Murphy GS, Szokol JW, Marymont JH, et al. Residual neuromuscular blockade and critical respiratory
events in the postanesthesia care unit. Anesth Analg 2008; 107:130.
48. Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive
sleep apnea. Anesthesiology 2008; 108:812.
49. Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a populationbased surgical cohort. Anesthesiology 2010; 113:1338.
50. Lawrence VA, Page CP, Harris GD. Preoperative spirometry before abdominal operations. A critical
appraisal of its predictive value. Arch Intern Med 1989; 149:280.
51. De Nino LA, Lawrence VA, Averyt EC, et al. Preoperative spirometry and laparotomy: blowing away
dollars. Chest 1997; 111:1536.
52. Gass GD, Olsen GN. Preoperative pulmonary function testing to predict postoperative morbidity and
mortality. Chest 1986; 89:127.
53. Wong DH, Weber EC, Schell MJ, et al. Factors associated with postoperative pulmonary complications in
patients with severe chronic obstructive pulmonary disease. Anesth Analg 1995; 80:276.
54. Fuso L, Cisternino L, Di Napoli A, et al. Role of spirometric and arterial gas data in predicting pulmonary
complications after abdominal surgery. Respir Med 2000; 94:1171.
55. Warner DO, Warner MA, Offord KP, et al. Airway obstruction and perioperative complications in smokers
undergoing abdominal surgery. Anesthesiology 1999; 90:372.
56. Fan ST, Lau WY, Yip WC, et al. Prediction of postoperative pulmonary complications in oesophagogastric
cancer surgery. Br J Surg 1987; 74:408.
57. Rucker L, Frye EB, Staten MA. Usefulness of screening chest roentgenograms in preoperative patients.
JAMA 1983; 250:3209.
58. Archer C, Levy AR, McGregor M. Value of routine preoperative chest x-rays: a meta-analysis. Can J
Anaesth 1993; 40:1022.
59. Smith TB, Stonell C, Purkayastha S, Paraskevas P. Cardiopulmonary exercise testing as a risk
assessment method in non cardio-pulmonary surgery: a systematic review. Anaesthesia 2009; 64:883.
60. Mazo V, Sabat S, Canet J, et al. Prospective external validation of a predictive score for postoperative
pulmonary complications. Anesthesiology 2014; 121:219.
61. Gupta H, Gupta PK, Fang X, et al. Development and validation of a risk calculator predicting postoperative
respiratory failure. Chest 2011; 140:1207.
62. http://www.surgicalriskcalculator.com/prf-risk-calculator.
63. Gupta H, Gupta PK, Schuller D, et al. Development and validation of a risk calculator for predicting
postoperative pneumonia. Mayo Clin Proc 2013; 88:1241.
64. http://www.surgicalriskcalculator.com/postoperative-pneumonia-risk-calculator.
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
12/19
14/1/2016
Evaluation of preoperative pulmonary risk
Topic 6917 Version 23.0
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
13/19
14/1/2016
Evaluation of preoperative pulmonary risk
GRAPHICS
American Society of Anesthesiologists (ASA) Physical Status
Classification System
ASA 1
A normal healthy patient
ASA 2
A patient with mild systemic disease
ASA 3
A patient with severe systemic disease
ASA 4
A patient with severe systemic disease that is a constant threat to life
ASA 5
A moribund patient who is not expected to survive without the operation
ASA 6
A declared brain-dead patient whose organs are being removed for donor
purposes
ASA Physical Status Classification System is reprinted with permission of the American Society of
Anesthesiologists, 520 N. Northwest Highway, Park Ridge, Illinois 60068-2573.
Graphic 87504 Version 5.0
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
14/19
14/1/2016
Evaluation of preoperative pulmonary risk
ARISCAT (Canet) risk index: Independent predictors of
postoperative pulmonary complications
Adjusted odds ratio
(95% CI)
Factor
Risk score
Age, years
50
51-80
1.4 (0.6-3.3)
>80
5.1 (1.9-13.3)
16
Preoperative O 2 saturation
96 percent
91-95 percent
2.2 (1.2-4.2)
90 percent
10.7 (4.1-28.1)
24
Respiratory infection in the
last month
5.5 (2.6-11.5)
17
Preoperative anemia hemoglobin 10 g/dL
3 (1.4-6.5)
11
Upper abdominal
4.4 (2.3-8.5)
15
Intrathoracic
11.4 (1.9-26.0)
24
Surgical incision
Duration of surgery
2 hours
2-3 hours
4.9 (2.4-10.1)
16
>3 hours
9.7 (2.4-19.9)
23
2.2 (1.0-4.5)
Emergency surgery
Risk class
Number of points in
risk score
Pulmonary
complication rate
(validation sample)
Low
<26 points
1.6 percent
Intermediate
26-44 points
13.3 percent
High
45 points
42.1 percent
Adapted with permission from: Canet J, Gallart L, Gomar C, et al. Prediction of postoperative
pulmonary complications in a population-based surgical cohort. Anesthesiology 2010; 113:1338.
Graphic 76906 Version 12.0
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
15/19
14/1/2016
Evaluation of preoperative pulmonary risk
Performance of the Arozullah respiratory failure index
Class
Point total
Percent respiratory failure
10
0.5
11 to 19
1.8
20 to 27
4.2
28 to 40
10.1
>40
26.6
Data from: Arozulla AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting
postoperative respiratory failure in men after major noncardiac surgery. The National Veterans
Administration Surgical Quality Improvement Program. Ann Surg 2000; 232:242.
Graphic 52339 Version 4.0
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
16/19
14/1/2016
Evaluation of preoperative pulmonary risk
Arozullah respiratory failure index
Preoperative predictor
Point value
Type of surgery
Abdominal aortic aneurysm
27
Thoracic
21
Neurosurgery, upper abdominal, peripheral vascular
14
Neck
11
Emergency surgery
11
Albumin <3.0 g/dL
BUN >30 mg/dL
Partially or fully dependent functional status
History of chronic obstructive pulmonary disease
Age
70 years
60 to 69 years
From: Arozulla AM, Daley J, Henderson WG, Khuri SF. Multifactorial risk index for predicting
postoperative respiratory failure in men after major noncardiac surgery. The National Veterans
Administration Surgical Quality Improvement Program. Ann Surg 2000; 232:242. Reproduced with
permission from Lippincott Williams & Wilkins. Copyright 2000 American Surgical Association and
European Surgical Association. Unauthorized reproduction of this material is prohibited.
Graphic 62775 Version 3.0
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
17/19
14/1/2016
Evaluation of preoperative pulmonary risk
Assessing the risk of postoperative pulmonary
complications
ASA: American Society of Anesthesiologists; PFTs: pulmonary function tests;
COPD: chronic obstructive pulmonary disease.
Graphic 56866 Version 3.0
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
18/19
14/1/2016
Evaluation of preoperative pulmonary risk
Disclosures
Disclosures: Gerald W Sm etana, MD Nothing to disclose. Talm adge E King, Jr, MD Consultant/Advisory Boards: InterMune
[pulmonary fibrosis (pirfenidone)]; ImmuneWorks [pulmonary fibrosis]; Boehringer Ingelheim [IPF (nintedanib)]; GlaxoSmithKline
[pulmonary fibrosis]; Daiichi Sankyo [pulmonary fibrosis]. Andrew D Auerbach, MD, MPH Nothing to disclose. Natalie F Holt, MD,
MPH Employment: ExamMaster Corp [USMLE step 3 test preparation material]; First Consult [Acquired disorders of complement
system]; American Society of Anesthesiologists [SEE Editorial Board]; Lippincott Williams & Wilkins [literature-based updates for
Clinical Anesthesia]. Lee Park, MD, MPH Nothing to disclose.
Contributor disclosures are review ed for conflicts of interest by the editorial group. When found, these are addressed by vetting
through a multi-level review process, and through requirements for references to be provided to support the content. Appropriately
referenced content is required of all authors and must conform to UpToDate standards of evidence.
Conflict of interest policy
http://www.uptodate.com/contents/evaluation-of-preoperative-pulmonary-risk?topicKey=PC%2F6917&elapsedTimeMs=0&source=search_result&searchT
19/19
S-ar putea să vă placă și
- NURS402 ResearchPaperDocument11 paginiNURS402 ResearchPaperldhendersonÎncă nu există evaluări
- Nurse Patient Ratio PDFDocument7 paginiNurse Patient Ratio PDFSafrina WaldiniÎncă nu există evaluări
- Preanesthesia Evaluation For Noncardiac Surgery - UpToDate PDFDocument86 paginiPreanesthesia Evaluation For Noncardiac Surgery - UpToDate PDFCharlie Bellow100% (1)
- 07 Nurse-Patient Ratios As A Patient Safety Strategy PDFDocument7 pagini07 Nurse-Patient Ratios As A Patient Safety Strategy PDFAmanda DavisÎncă nu există evaluări
- Post Op DeliriumDocument26 paginiPost Op DeliriumKannan GÎncă nu există evaluări
- Overview of Complications Occurring in The Post-Anesthesia Care UnitDocument14 paginiOverview of Complications Occurring in The Post-Anesthesia Care UnitShahabuddin ShaikhÎncă nu există evaluări
- High Patient Nurse RatiosDocument2 paginiHigh Patient Nurse Ratiosrachel lorenÎncă nu există evaluări
- Airway Management Inside and Outside Operating Rooms 2018 British Journal ofDocument3 paginiAirway Management Inside and Outside Operating Rooms 2018 British Journal ofSeveNÎncă nu există evaluări
- A Guide To Nursing, Midwifery and Care Staffing Capacity and CapabilityDocument59 paginiA Guide To Nursing, Midwifery and Care Staffing Capacity and CapabilityArisCahyoPurnomoÎncă nu există evaluări
- RRLDocument8 paginiRRLAlloiBialbaÎncă nu există evaluări
- Monitored Anesthesia Care in Adults: Considerations During Covid-19 PandemicDocument29 paginiMonitored Anesthesia Care in Adults: Considerations During Covid-19 PandemicGanda Impola TBAÎncă nu există evaluări
- Pediatric Regional Anesthesia 2005Document66 paginiPediatric Regional Anesthesia 2005tameem89Încă nu există evaluări
- Evidence Based Standards For Measuring Nurse Staffing and PerformanceDocument208 paginiEvidence Based Standards For Measuring Nurse Staffing and PerformanceA As'ad MaoÎncă nu există evaluări
- Pre Op 2010Document37 paginiPre Op 2010Tawona DhlakamaÎncă nu există evaluări
- Novel Tools For Hemodynamic Monitoring in Critically Ill Patients With Shock - UpToDateDocument26 paginiNovel Tools For Hemodynamic Monitoring in Critically Ill Patients With Shock - UpToDateAlex KuliaÎncă nu există evaluări
- Factors That Affect The Development of Nurses' Competencies PDFDocument4 paginiFactors That Affect The Development of Nurses' Competencies PDFDwi NopriyantoÎncă nu există evaluări
- Relationship Between Nurses Job Satisfaction and Quality of HealDocument64 paginiRelationship Between Nurses Job Satisfaction and Quality of HealAnonymous NaV1o37hÎncă nu există evaluări
- Vaishali Syal Moderator - Prof. J. R. ThakurDocument34 paginiVaishali Syal Moderator - Prof. J. R. ThakurTasha NurfitrianiÎncă nu există evaluări
- Non-Pharmacological Pain Management PDFDocument15 paginiNon-Pharmacological Pain Management PDFEndy JuliantoÎncă nu există evaluări
- Enhanced Recovery After Surgery (ERAS) in Emergency Abdominal Surgery: Background, Preoperative Components of ERAS, Intraoperative Components of ERASDocument9 paginiEnhanced Recovery After Surgery (ERAS) in Emergency Abdominal Surgery: Background, Preoperative Components of ERAS, Intraoperative Components of ERASAndre F SusantioÎncă nu există evaluări
- Quality of Health Care and Patient SatisfactionDocument10 paginiQuality of Health Care and Patient SatisfactionIulia MicÎncă nu există evaluări
- Prevalence of Human Immunodeficiency Virus Infection Among Tuberculosis Patients at Infectious Disease Hospital, Kano State, NigeriaDocument8 paginiPrevalence of Human Immunodeficiency Virus Infection Among Tuberculosis Patients at Infectious Disease Hospital, Kano State, NigeriaUMYU Journal of Microbiology Research (UJMR)Încă nu există evaluări
- Overview of The Management of Primary Colon Cancer - UpToDateDocument30 paginiOverview of The Management of Primary Colon Cancer - UpToDateCaio AmaralÎncă nu există evaluări
- Postoperative Cognitive Dysfunction Preoperative Risk Assessment and Perioperative Risk Minimization A Pragmatic Review of The LitDocument5 paginiPostoperative Cognitive Dysfunction Preoperative Risk Assessment and Perioperative Risk Minimization A Pragmatic Review of The Litade_liaÎncă nu există evaluări
- Overview of Anesthesia - UpToDateDocument11 paginiOverview of Anesthesia - UpToDateFernandoVianaÎncă nu există evaluări
- Physics Andits Laws in AnaesthesiaDocument111 paginiPhysics Andits Laws in AnaesthesiaRobin TolentinoÎncă nu există evaluări
- 2017 ASA Refresher Courses in Anesthesiology (165-172)Document8 pagini2017 ASA Refresher Courses in Anesthesiology (165-172)Edelweis JavanicaÎncă nu există evaluări
- Obstetrics AnesthesiaDocument31 paginiObstetrics AnesthesiaNorfarhanah ZakariaÎncă nu există evaluări
- Informed ConsentDocument25 paginiInformed ConsentMaylodie ingallaÎncă nu există evaluări
- Perioperative Laboratorytesting - The ClinicsDocument6 paginiPerioperative Laboratorytesting - The Clinicsapi-265532519Încă nu există evaluări
- Preoxygenation During Induction of Anesthesia in Noncritically Ill PatientsDocument6 paginiPreoxygenation During Induction of Anesthesia in Noncritically Ill PatientsasfwegereÎncă nu există evaluări
- Cuthbert Ethics PaperDocument14 paginiCuthbert Ethics Papershawnee11Încă nu există evaluări
- Anesthesia For Genitourinary SurgeryDocument76 paginiAnesthesia For Genitourinary SurgeryWenny Eka FildayantiÎncă nu există evaluări
- Water Hyacinth ( (Eichhornia Crassipes (Mart.) Solms) Chopper Cum CrusherDocument9 paginiWater Hyacinth ( (Eichhornia Crassipes (Mart.) Solms) Chopper Cum CrusherAlexander DeckerÎncă nu există evaluări
- General Anesthetics: General Anesthesia - Characteristics Balanced AnesthesiaDocument7 paginiGeneral Anesthetics: General Anesthesia - Characteristics Balanced AnesthesiarisanataliasiburianÎncă nu există evaluări
- Stress Ulcer ProphylaxisDocument24 paginiStress Ulcer ProphylaxisredyhataÎncă nu există evaluări
- Review Course Vascular - AnaesthesiaDocument36 paginiReview Course Vascular - AnaesthesiazaidÎncă nu există evaluări
- GUIDELINE For IMPROVING OUTCOME After Anaesthesia and Critical Care - 2017 - College of AnaesthesiologistsDocument83 paginiGUIDELINE For IMPROVING OUTCOME After Anaesthesia and Critical Care - 2017 - College of AnaesthesiologistsSanj.etcÎncă nu există evaluări
- Emergency Surgery FrameworkDocument36 paginiEmergency Surgery Frameworkhalosunyrtimr6Încă nu există evaluări
- Anesthesia For Patients With Renal DiseaseDocument4 paginiAnesthesia For Patients With Renal DiseasejoninhabÎncă nu există evaluări
- Evaluation of Headache in AdultsDocument21 paginiEvaluation of Headache in AdultsMaicon RamosÎncă nu există evaluări
- Prevalence and MorbidityDocument6 paginiPrevalence and MorbidityasuratosÎncă nu există evaluări
- Hypothermia and Temperature Regulation Considerations During AnesthesiaDocument20 paginiHypothermia and Temperature Regulation Considerations During AnesthesiaAgung Bhaktiyar100% (1)
- KP 1.1.1.6 - Interprofessional CommunicationDocument37 paginiKP 1.1.1.6 - Interprofessional CommunicationKirana AnaÎncă nu există evaluări
- AFP MigrañaDocument9 paginiAFP MigrañaJuaan AvilaÎncă nu există evaluări
- 1.05 (Surgery) General Anesthesia - Airway ManagementDocument3 pagini1.05 (Surgery) General Anesthesia - Airway ManagementLeo Mari Go LimÎncă nu există evaluări
- Color Code AnesthesiaDocument6 paginiColor Code AnesthesiaYusnia Gulfa MaharaniÎncă nu există evaluări
- Smart Beds For Hospitals With Internet o PDFDocument6 paginiSmart Beds For Hospitals With Internet o PDFDokumentasi FPA XVIÎncă nu există evaluări
- Operating Room Care of The Surgical Patient: Teaching PlanDocument9 paginiOperating Room Care of The Surgical Patient: Teaching PlanscribdnijoizÎncă nu există evaluări
- Principles of Bariatric and Metabolic SurgeryDocument51 paginiPrinciples of Bariatric and Metabolic SurgeryDr Shahzad Alam ShahÎncă nu există evaluări
- Bier Block (Intravenous Regional Anesthesia), Handout PDFDocument8 paginiBier Block (Intravenous Regional Anesthesia), Handout PDFjahangirealamÎncă nu există evaluări
- Critical Care Update PDFDocument25 paginiCritical Care Update PDFHugo PozoÎncă nu există evaluări
- Dopamine Antagonists in ICU DeliriumDocument2 paginiDopamine Antagonists in ICU DeliriumRodrigoSachiFreitasÎncă nu există evaluări
- Anesthesia For The Patient With Peripartum Hemorrhage - UpToDateDocument25 paginiAnesthesia For The Patient With Peripartum Hemorrhage - UpToDateZurya UdayanaÎncă nu există evaluări
- Cardiovascular Pharmacology PDFDocument20 paginiCardiovascular Pharmacology PDFMelanie PrinceÎncă nu există evaluări
- DIVITI Slide Prophylaxis VTE SPPD Ringkas-1Document11 paginiDIVITI Slide Prophylaxis VTE SPPD Ringkas-1Fera NurrizaÎncă nu există evaluări
- Lakshminarasimhachar 2016Document18 paginiLakshminarasimhachar 2016mel.espinoza90Încă nu există evaluări
- Review Article: Peri-Operative Pulmonary Dysfunction and ProtectionDocument5 paginiReview Article: Peri-Operative Pulmonary Dysfunction and ProtectionmeldaerÎncă nu există evaluări
- Perioperative Lung ProtectionDocument6 paginiPerioperative Lung ProtectionWilliamRayCassidyÎncă nu există evaluări
- Essentials in Lung TransplantationDe la EverandEssentials in Lung TransplantationAllan R. GlanvilleÎncă nu există evaluări
- Opioid - and Motor-Sparing With Proximal, Mid-, and Distal Locations For Adductor Canal Block in Anterior Cruciate Ligament ReconstructionDocument11 paginiOpioid - and Motor-Sparing With Proximal, Mid-, and Distal Locations For Adductor Canal Block in Anterior Cruciate Ligament ReconstructionCharlieBrown_QBÎncă nu există evaluări
- Upper Trunk Block For Shoulder Analgesia With Potential Phrenic Nerve Sparing: A Preliminary Anatomical ReportDocument3 paginiUpper Trunk Block For Shoulder Analgesia With Potential Phrenic Nerve Sparing: A Preliminary Anatomical ReportCharlieBrown_QBÎncă nu există evaluări
- Spinalorgeneralanaesthesiaforsurgicalrepairofhipfractureandsubsequentriskofmortalityandmorbidity:adatabaseanalysisusingpropensityscore MatchingDocument7 paginiSpinalorgeneralanaesthesiaforsurgicalrepairofhipfractureandsubsequentriskofmortalityandmorbidity:adatabaseanalysisusingpropensityscore MatchingCharlieBrown_QBÎncă nu există evaluări
- Rheumatoid Arthritis: Perioperative Manage - Ment of Biologics and DMARDsDocument21 paginiRheumatoid Arthritis: Perioperative Manage - Ment of Biologics and DMARDsCharlieBrown_QBÎncă nu există evaluări
- Huang Et Al-2020-Annals of Intensive CareDocument13 paginiHuang Et Al-2020-Annals of Intensive CareCharlieBrown_QBÎncă nu există evaluări
- Choice of Fluid Type Physiological Concepts and Perioperative IndicationsDocument13 paginiChoice of Fluid Type Physiological Concepts and Perioperative IndicationsCharlieBrown_QBÎncă nu există evaluări
- Airway Management (Anesthesia Text)Document18 paginiAirway Management (Anesthesia Text)CharlieBrown_QBÎncă nu există evaluări
- Emergency Department Hyperoxia Is Associated With Increased Mortality in Mechanically Ventilated Patients A Cohort StudyDocument10 paginiEmergency Department Hyperoxia Is Associated With Increased Mortality in Mechanically Ventilated Patients A Cohort StudyCharlieBrown_QBÎncă nu există evaluări
- Adductor Canal Block Provides Noninferior Analgesia and Superior Quadriceps Strength Compared With Femoral Nerve Block in Anterior Cruciate Ligament ReconstructionDocument12 paginiAdductor Canal Block Provides Noninferior Analgesia and Superior Quadriceps Strength Compared With Femoral Nerve Block in Anterior Cruciate Ligament ReconstructionCharlieBrown_QBÎncă nu există evaluări
- Adductor Canal Block Versus Femoral Nerve Block For Total Knee ArthroplastyDocument11 paginiAdductor Canal Block Versus Femoral Nerve Block For Total Knee ArthroplastyJessica CÎncă nu există evaluări
- Pulmonary Function TestingDocument6 paginiPulmonary Function TestingCharlieBrown_QBÎncă nu există evaluări
- NYSORA Educational Poster LE V8Document1 paginăNYSORA Educational Poster LE V8pimpollopittÎncă nu există evaluări
- Anaesthesia For Laparoscopic SurgeryDocument5 paginiAnaesthesia For Laparoscopic SurgeryCharlieBrown_QBÎncă nu există evaluări
- Preoperative Evaluation For Lung ResectionDocument12 paginiPreoperative Evaluation For Lung ResectionCharlieBrown_QBÎncă nu există evaluări
- Are You Ready: An In-Depth Guide To Citizen PreparednessDocument204 paginiAre You Ready: An In-Depth Guide To Citizen PreparednessAndrew Mack100% (2)
- Anesthesia For The Obese PatientDocument24 paginiAnesthesia For The Obese PatientCharlieBrown_QBÎncă nu există evaluări
- Writing A Cover LetterDocument2 paginiWriting A Cover LetterCharlieBrown_QBÎncă nu există evaluări
- Recovery Framework 2013 Guide Practitioners ProvidersDocument96 paginiRecovery Framework 2013 Guide Practitioners ProvidersAyuy Welliss MedusaÎncă nu există evaluări
- AclsDocument13 paginiAclsAllah YarÎncă nu există evaluări
- P. Mathiyalagan-FAKE NBA-SAR-MECHANICALDocument457 paginiP. Mathiyalagan-FAKE NBA-SAR-MECHANICALgalgotias universityÎncă nu există evaluări
- Patient Safety and Quality Care MovementDocument9 paginiPatient Safety and Quality Care Movementapi-300362983Încă nu există evaluări
- Noel Vs NoaelDocument4 paginiNoel Vs NoaelyehezkieldwardÎncă nu există evaluări
- Clerks Manual Ay 2016-2017 PDFDocument20 paginiClerks Manual Ay 2016-2017 PDFJan Marvin Lichauco MendozaÎncă nu există evaluări
- Acm 20072Document16 paginiAcm 20072numbnessÎncă nu există evaluări
- What Are The Benefits of Chiropractic CareDocument2 paginiWhat Are The Benefits of Chiropractic CaretomÎncă nu există evaluări
- Design Brief 2nd Year 4th Sem ADDocument8 paginiDesign Brief 2nd Year 4th Sem ADChinmay KumtakarÎncă nu există evaluări
- 2-3. G.R. No. 88265 Del Rosario V Bengzon (Digest)Document2 pagini2-3. G.R. No. 88265 Del Rosario V Bengzon (Digest)Iter Mercatabant0% (1)
- NPI NCMH StephDocument12 paginiNPI NCMH StephAnonymous 2fUBWme6wÎncă nu există evaluări
- Journal CoroDocument5 paginiJournal Corogiantejada23Încă nu există evaluări
- MarketingDocument4 paginiMarketingAliaa Marie H. GoingoÎncă nu există evaluări
- To Taste or Not To TasteDocument3 paginiTo Taste or Not To TasteSpeech & Language Therapy in PracticeÎncă nu există evaluări
- Cancer Informative OutlineDocument2 paginiCancer Informative OutlinetuanmalikÎncă nu există evaluări
- Issues Related To Blood DonationDocument8 paginiIssues Related To Blood DonationPennyTanÎncă nu există evaluări
- A Step by Step Guide To Mastering The OSCEsDocument20 paginiA Step by Step Guide To Mastering The OSCEsAl Imari60% (10)
- Biotechnology: From Idea To MarketDocument4 paginiBiotechnology: From Idea To MarketTim Sandle100% (1)
- Advisory On Reiteration of Ao 2021 0012 Implementing Guidelines On The Medicine Access Program For Health 2Document7 paginiAdvisory On Reiteration of Ao 2021 0012 Implementing Guidelines On The Medicine Access Program For Health 2ncd.bulacanÎncă nu există evaluări
- Mental Health and Aging in The 21st CenturyDocument17 paginiMental Health and Aging in The 21st CenturyNatasha AlbaShakiraÎncă nu există evaluări
- Psychiatry An Illustrated Colour Text PDFDocument125 paginiPsychiatry An Illustrated Colour Text PDFDoris Smith100% (6)
- 01 - CHCCCS015 - Provide Individualised Support - Ageing v1.1.v1.0Document26 pagini01 - CHCCCS015 - Provide Individualised Support - Ageing v1.1.v1.0Pradhiksha ArulÎncă nu există evaluări
- DOLE Template OSHprogram Asof 290119Document13 paginiDOLE Template OSHprogram Asof 290119Marco EsguerraÎncă nu există evaluări
- Case Presentation (Exam)Document42 paginiCase Presentation (Exam)JAHNAVI KAYASTHAÎncă nu există evaluări
- 1hospital ProfileDocument2 pagini1hospital ProfileVenkatesh VenkatÎncă nu există evaluări
- Curriculum PTDocument3 paginiCurriculum PTphysiosharmajÎncă nu există evaluări
- Quality of Life of Patients With Hypertension in Primary Health Care in Bandar LampungDocument7 paginiQuality of Life of Patients With Hypertension in Primary Health Care in Bandar Lampungwidya astutyloloÎncă nu există evaluări
- Pediatric Pain Assessment in TDocument6 paginiPediatric Pain Assessment in TnurtiÎncă nu există evaluări
- Alabama Physicians LetterDocument12 paginiAlabama Physicians LetterJohn ArchibaldÎncă nu există evaluări
- Emergency BangkokDocument3 paginiEmergency Bangkoksaadchalid100% (1)