Documente Academic
Documente Profesional
Documente Cultură
1
Încărcat de
Aldo YustiantoDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
1
Încărcat de
Aldo YustiantoDrepturi de autor:
Formate disponibile
Journal of Pediatric Surgery 50 (2015) 20512055
Contents lists available at ScienceDirect
Journal of Pediatric Surgery
journal homepage: www.elsevier.com/locate/jpedsurg
A new 2-step risk-stratication clinical score for suspected appendicitis
in children,,,
Te-Lu Yap a,, Yong Chen a, Wilson Wei Xin Low a, Caroline Choo Phaik Ong a, Shireen Anne Nah a,
Anette S. Jacobsen a, Liang Shen b, Yee Low a
a
b
Department of Paediatric Surgery, KK Womens and Childrens Hospital, Singapore
Department of Biostatistics, National University Health System, Singapore
a r t i c l e
i n f o
Article history:
Received 15 August 2015
Accepted 24 August 2015
Key words:
Appendicitis
Pediatric
Appendicitis score
White blood cell count
C-reactive protein
Diagnosis
a b s t r a c t
Aim: The aim of this study was to develop a new Children's Appendicitis Score (CAS) by combining 3 inammatory markers and a set of predictors for suspected appendicitis in children.
Methods: 374 children aged 416 years with suspicion of appendicitis were prospectively enrolled for the derivation cohort. Demographic characteristics, clinical features, laboratory, and histology data were collected. The outcome measure was the histological presence or absence of appendicitis. Backward logistic regression was
employed to select predictors for construction of a score. Diagnostic performance of CAS was compared with
the Pediatric Appendicitis Score (PAS) on a separate validation cohort.
Results: The combination of normal white blood cell count (WBC), neutrophil percentage, and C-reactive protein
(CRP) had a 100% negative predictive value for appendicitis. We assigned coefcient A as zero when all triple
markers were negative and one when any one markers was positive. A second component of 6 predictors was
identied for construction of the raw score: Localized right-lower-quadrant pain, generalized guarding, constant characteristic of pain, pain on percussion or coughing, WBC 14000/L and CRP 24 g/L. CAS was generated
by multiplying coefcient A by raw score.
Conclusion: CAS is superior to PAS in ruling out appendicitis. Risk stratication of equivocal patients could guide
the need for further diagnostic imaging examination.
2015 The Authors. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license
(http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Background
Accurate and timely diagnosis of appendicitis in children remains
elusive [1]. Negative appendicectomy rates have remained above 6%
and perforation rates above 35% despite the widespread adoption of
computed tomography (CT) scan as the primary diagnostic modality
in some countries [2]. Pediatric appendicitis has been identied as the
principal pathology accounting for a surge in CT scan utilization in children, a trend that needs to be reversed in light of the signicantly higher
risk of radiation exposure in children [3].
Abbreviations: CAS, Children Appendicitis Score; PAS, Pediatric Appendicitis Score;
WBC, White blood cell count; CRP, C-reactive protein; ROC, Receiver operator characteristic curve; AUC, Areas under the curve; LR, Likelihood ratio; Neut%, neutrophil percentage.
Funding source: SingHealth Foundation Research Grant.
Financial disclosure: The authors have no nancial relationships relevant to this
article to disclose.
Conict of interest: The authors have no conict of interest to disclose.
IRB approval: This study was deemed exempt by the institutional review board.
Corresponding author at: Department of Paediatric Surgery, KK Womens and
Childrens Hospital, 100 Bukit Timah Road, Singapore 229899. Tel.: + 65 6394 1113;
fax: +65 6291 0161.
E-mail address: Yap.Te-Lu@kkh.com.sg (T.-L. Yap).
The diagnostic accuracy of pediatric appendicitis may be enhanced by the integration of objective clinical predictors, laboratory
markers and imaging investigations into a clinical prediction rule
(CPR). A number of clinical scoring systems have been developed,
the two most popular for use in children being the Alvarado and
Samuels Pediatric Appendicitis Score (PAS). However, in a recent
systematic review by Kulik et al. both scores failed to meet the current performance benchmarks of CPR. On average, the PAS would
overdiagnose appendicitis by 35%, and the Alvarado score would do
so by 32% [4].
Laboratory inammatory markers, either on its own or as part of a
clinical score, have been employed to improve the predictability of appendicitis. It has been shown that utilizing two markers concurrently
is more accurate than relying on one alone [58]. However, the predictive capability of combining three markers, namely white blood cell
count (WBC), neutrophil percentage (Neut%) and C-reactive protein
(CRP), has not been established in the pediatric population.
The aim of our study is to develop a simple and easily applicable clinical prediction model, incorporating 3 laboratory markers, prioritized to
rule out appendicitis. This is accompanied by a risk-stratication strategy of staged ultrasound examination followed by CT scan only in patients with equivocal diagnosis. The performance of the derived score
will then be validated against the PAS.
http://dx.doi.org/10.1016/j.jpedsurg.2015.08.028
0022-3468/ 2015 The Authors. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
2052
T.-L. Yap et al. / Journal of Pediatric Surgery 50 (2015) 20512055
2. Materials and methods
2.1. Study design
This was a prospective observational cohort study aimed at collecting
data to develop a new clinical scoring system for children with suspected
appendicitis. The study was conducted between July 2012 and March
2014 and enrolled pediatric patients between the ages of 4 and
16 years. The score was developed based on the data from the derivation
group of patients. The discriminative and predictive ability of the developed score was validated in a different group of patients. The study was
approved by the Central Institutional Research Ethics Board. Informed
written consent was obtained from all parents or legal guardians and assent was obtained from children 7 years and older.
The study took place in the surgical wards of an urban, tertiary childrens hospital. All children admitted from the Childrens Emergency
Department with the diagnosis of suspected appendicitis were eligible
for enrollment.
Exclusion criteria included patients with previous appendicectomy
and abdominal surgery, pregnancy, chronic medical or malignant conditions (e.g. inammatory bowel disease) and patients who had CT scan
within the previous month.
Eligible patients were identied and enrolled by the on-duty surgical registrars and data was entered by the on-duty residents. Two research assistants counterchecked this information prior to entry into a
spreadsheet program.
The patients information collected for the derivation set included:
Demographic characteristics (age, gender weight), history of presentation (location of pain according to abdominal quadrants, duration, characteristics, migration, localization of pain, aggravation of pain by
movement or coughing or walking, anorexia, nausea, vomiting, fever,
stool frequency), clinical signs on physical examination (temperature,
localized tenderness, rebound tenderness, pain on percussion/coughing,
psoas sign, Rovsings sign, generalized guarding, bowel sound characteristics, pain on hopping, rectal tenderness), laboratory tests results
(WBC counts, neutrophil percentage, CRP values, urine microscopy),
imaging examination results (ultrasound or CT scan of abdomen), intraoperative ndings at appendicectomy (presence of faecolith, perforation, abscess or mass), and histological diagnosis of appendix specimen.
WBC and neutrophil count measurements were performed by standard laboratory methods using a Sysmex XE-5000 analyzer. CRP levels
were measured with the Abbott Architect c8000 analyzer.
differentiate between the disease and nondisease group model. The
normal-value cutoff referred to the normal reference limits used in
our laboratory: WBC b 10,000/L, neutrophil percentage (%) b 75% and
CRP b 5 g/L.
Statistical analysis was performed with IBM SPSS statistics 19 and
GraphPad Prism6.
2.4. Validation of the score and comparing it to the PAS
The constructed Children's Appendicitis Score (CAS) was then validated by a separate cohort of patients. Receiver operator characteristic
curve (ROC) was analyzed and comparison of the areas under the
curve (AUC) between the nal CAS and the Pediatric Appendicitis
Score was made. A score with perfect discriminatory ability would
have an AUC of 1.0 while one unable to distinguish between appendicitis and nonappendicitis would have an AUC of 0.50.
3. Results
The demographic and clinical characteristics of the derivation and
validation set of patients are shown in Table 1: 374 patients were enrolled in the derivation set and 373 patients were used in the validation
set. The distributions of age and gender as well as prevalence of appendicitis were comparable in both sets.
Statistical analysis of the derivation cohort identied two independent sets of predictors, each with substantial discriminatory capability.
One of them was a set of three combined laboratory inammatory
markers while the other was a combination of clinical and laboratory
predictors that could be formulated into a raw score.
3.1. Diagnostic performance of WBC, neutrophil percentages and CRP
Individually, when each of WBC, Neut% and CRP was normal, 4.5%,
10.7% and 5.3% of our patients were diagnosed with appendicitis respectively. However when all three markers were normal, none of the patients
in the derivation cohort was diagnosed with appendicitis. Therefore when
all three markers were normal, the discriminatory ability to rule out appendicitis had a sensitivity of 100%, negative predictive value of 100%
and negative likelihood ratio of zero (Table A.1).
This capability of the combined triple markers made them an ideal
rule-out instrument. However their low specicity of only 24.7% and
low positive predictive value of 38.3% severely limited their utility as a
standalone predictive tool for appendicitis.
2.2. Outcome measures
3.2. Construction of the raw score and nal score
Appendicitis diagnosis: The histological diagnosis of appendicitis
entailed the presence of transmural and focal inammatory inltrates
or at least mucosal inltrates. The presence of a faecolith, either at surgery or within the resected appendix was diagnostic of appendicitis. The
diagnosis of complicated appendicitis was reserved for perforation or
gangrene of the appendix on histology or presence of abscess or inammatory mass at time of surgery.
Nonappendicitis diagnosis: All patients suspected of appendicitis
were observed in the ward until pain free for at least 24 hours current
institution practice. All equivocal cases were subjected to ultrasound
(US) study, or CT scan if the US was not diagnostic.
From the initial 41 variables, 6 potential predictors met the criteria
for entry into our raw score based on backward logistic regression analysis. The predictors and their corresponding weights were translated to
score points (Table 2). This constitutes the raw score component of our
nal score. Localized right iliac fossa (RIF) tenderness, generalized
guarding and WBC count were given higher weight age than constant
pain, pain on percussion or coughing and CRP level.
Table 1
Demographic and clinical characteristics.
2.3. Statistical methods for construction of the clinical score
The patients information from the derivation cohort was used to develop our new score. Based on the estimated coefcient from backward
logistic regression, candidate predictors and their corresponding
weightage were identied. Six predictors with p value b 0.05 were
retained in the raw score.
Laboratory predictors with continuous values were converted into
categorical variables using ROC analysis to obtain best cutoff points to
Sample Size
Age (years), Median (range)
Males, n (%)
Females, n (%)
Complicated Appendicitis, n (%)
Simple Appendicitis, n (%)
Total Appendicitis, n
Total Nonappendicitis, n
Prevalence (%)
Derivation Set
Validation Set
374
10 (416)
213 (57.0)
161 (43.0)
40 (33.6)
79 (66.4)
119
255
31.8
373
11 (416)
216 (57.9)
157 (42.1)
40 (36.4)
70 (63.6)
110
263
29.5
p Value
0.154
0.883
0.679
0.526
T.-L. Yap et al. / Journal of Pediatric Surgery 50 (2015) 20512055
2053
Table 2
Predictors and weightage of raw score.
Predictors
Weightage
Characteristics of Pain: Constant
Localized Right Iliac Fossa (RIF) Tenderness
Pain on Percussion/Coughing
Generalized Guarding
WBC 14,000/L
CRP 24 g/L
1.0
1.5
1.0
1.5
1.5
1.0
The continuous laboratory variables of WBC and CRP were converted
to categorical variables with the most discriminatory cutoff values as
14,000/L and 24 g/L respectively.
The high predictive capability of the triple markers distinguished itself
and was therefore retained as a decisive coefcient A. A = zero when
all three markers were normal. A = one when any one of the triple
markers was elevated. By incorporating the triple markers coefcient
A and the set of predictors of the raw score into a mathematical formula, we derived the nal score:
Children Appendicitis Score CAS
coefficient A multiply by raw score
The nal CAS totaled up to a score that ranged from 0 to 7.5 points (0.5
does not exist as the minimum score is 1) with interval of ve tenths or 0.5.
The area under the ROC curve for our new score based on the derivation cohort was 0.879 (95% CI 0.8430.914) (Fig. 1).
Fig. 2. Frequency distribution of CAS with 2 cutoffs (Validation Set).
the diagnosis of appendicitis. Within the high probability group, 17 patients with either acute or complicated appendicitis were correctly classied. However one patient with an ovarian pathology fell into this
category thus giving us a negative appendicectomy rate of 5.5%. This patient would still have necessitated surgical exploration.
Within the intermediate probability group of 176 (47.2%) patients,
the diagnosis of nonappendicitis vs. appendicitis was 54.2% and 45.8%
respectively. As such, the discriminatory ability of the score was not distinct enough in this group. Additional imaging study of ultrasound examination of the abdomen was required. The risk-stratication
strategy of the CAS was summarized in Fig. 3.
3.3. Diagnostic performance of CAS with risk stratication in
validation cohort
3.4. Diagnostic performance of the CAS compared with PAS
For the purpose of further risk stratication into 3 diagnostic zones,
two threshold cutpoints were identied on the ROC analysis of the derivation set. The 3 diagnostic zones could be used to categorize patients
into low, intermediate and high probability groups (Fig. 2).
The low probability group (any scores below 1.5), had a sensitivity of 98.2% with a negative predictive value of 98.8% for appendicitis
and a negative likelihood ratio of 0.02: 167 (44.8%) patients were
categorized into this group. Among the 263 patients without appendicitis, 166 (63%) were correctly classied into the low probability
group. However, the score misclassied one patient into the lowprobability category. This patient had appendicitis despite normal
triple marker values.
A high probability group with score above 5 would identify patients
who had appendicitis with certainty. This threshold level had a high
specicity of 99.6% with a 94.4% positive predictive value to rule in
The AUC for our new score based on the derivation cohort was 0.88
(95% CI 0.840.91) as compared to PASs AUC of 0.84 (95% CI 0.800.88).
The AUC of our CAS on the validation cohort was 0.91 (95% CI 0.880.94)
compared to that of PAS 0.89 (95% CI 0.850.92) (Fig. 1). However the
differences did not reach statistical signicance.
However if a similar risk stratication strategy was applied to the
PAS, its diagnostic performance would also be improved (Table 3). Comparing both CAS and PAS with risk stratication, our score still retained a
higher discriminatory performance at the low cutoff threshold with a
higher specicity and positive predictive value which was statistically
signicant. The diagnostic accuracy of both scores at high cutoff points
was comparable in terms of sensitivity, specicity, positive and negative
predictive value. Although the CAS still out performed the PAS on likelihood ratio, this was not statistically signicant.
Fig. 1. ROC curves for detection of appendicitis by CAS and PAS in derivation and validation set.
2054
T.-L. Yap et al. / Journal of Pediatric Surgery 50 (2015) 20512055
Fig. 3. Flowchart of Children Appendicitis Score with risk stratication.
3.5. Diagnostic performance of the CAS according to age groups
The CAS performance was analyzed across 3 age groups: 4 to 8 years,
9 to 12 years and 13 to 16 years (Fig. A.1). The AUC for each was 0.908
(95% CI 0.8530.964), 0.873 (95% CI 0.8170.929) and 0.850 (95% CI
0.7750.926) respectively. It appeared that the CAS was more discriminatory in the youngest age group.
4. Discussion
Using our newly developed CAS, we were able to rule out 63% of the
patients without appendicitis by classifying them correctly to the low
probability group. This capability surpassed the diagnostic performance
of the PAS score even with stratication as proposed by us. This demonstrates the potential of our score to exclude appendicitis accurately and
thereby reducing the large number of patients that would have needed imaging studies or in-hospital observation. However, the predictive capability
of our score in the high probability group was similar to that of the PAS.
To the best of our knowledge this is the rst study utilizing a combination of 3 laboratory inammatory markers (WBC, CRP and neut%) to
improve the diagnostic accuracy for suspected appendicitis in children.
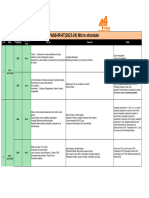
Table 3
Diagnostic characteristics of CAS and PAS according to the cutoff points comparing between Derivation Set and Validation Set.
Cutoff Point
CAS
Diagnostic Value
Derivation Set
Sensitivity
Specicity
PV+
PV
LR+
LR
Validation Set
Sensitivity
Specicity
PV+
PV
LR+
LR
PAS
b1.5 points
N5 points
b3 points
0.97
0.51
0.48
0.97
1.96
0.07
0.19
0.99
0.88
0.72
15.71
0.82
0.97
0.40
0.43
0.97
1.59
0.07
0.21
0.98
0.86
0.72
3.25
0.76
0.98
0.63
0.55
0.99
2.63
0.03
0.15
1.00
0.95
0.72
40.65
0.85
0.98
0.51
0.46
0.99
2.00
0.04
0.15
1.00
0.94
0.74
38.25
0.86
This is also the rst study to incorporate the 3 markers into a clinical
scoring system.
In a systematic review and metaanalysis by Yu et al., CRP had the
best discriminative capability followed by WBC, and was denitely superior to procalcitonin [8,9]. It was rst alluded to by Shogilev et al.
that multiple laboratory markers, when used in combination, would
greatly increase their diagnostic utility [7]. In our study, we had one patient with all triple markers normal but yet conrmed with appendicitis.
This limitation we encountered with CRP values in appendicitis may be
related to its time-dependent response characteristic. For WBC and absolute neutrophil count, the greatest discriminative accuracy for appendicitis is within 24 hours of onset of pain whereas for CRP, it is more
accurate between the 24 and 48 hours period. This only afrms the dynamic and evolving process of inammation in appendicitis [10].
Our scores performance was greatly improved when two threshold
cutoffs with three probability groups were used. This same sentiment
was reected in prior reviews on the validation of the PAS score
[1113]. Goldman et al. recommended that the PAS utilize a low cutoff
of less than 2 for high validity for ruling out appendicitis and a score
of more than 7 for predicting appendicitis [14]. If the original description of PAS with only a single cutoff point was applied to our validation
cohort, we would have misdiagnosed 55% of appendicitis and have a
negative exploration rate of 27%.
We had 8 negative appendicectomies in the validation set. Seven of
them would have been classied into the intermediate group had the
new score been applied. All of them would then have had further preoperative imaging studies that may have obviated the negative exploration. In our institute, the sensitivity of ultrasound study in diagnosing
appendicitis, when the appendix was visualized, was 84%. CT scans are
only performed if the appendix is not visualized on US or if the US ndings are equivocal. Adopting the ALARA concept (as low as reasonably
achievable) of radiation dosing to minimize potential risks, we advocate
such a staged ultrasound and CT scan protocol [3].
The superiority of our score is in the ease of execution. Our score
comprised only 4 clinical and 3 laboratory predictors. The retained predictors in the raw score reect the objective evidence of inammatory
involvement of the appendix. Subjective variables such as migration
of pain, anorexia and nausea were found to be not diagnostic in our
cohort. This could be related to language understanding as English is
not the rst language of many of our children. Furthermore, translation
into different languages such as Chinese, Malay and even Tamil is frequently requested by parents as well as patients.
For clinical predictive rules used in the pediatric population, the
overall benchmark performance requires a sensitivity of .0.98 with a
negative likelihood ratio of b0.01 [4,15]. Our scores performance on
the validation set was able to achieve the sensitivity of 0.98 but a negative likelihood ratio (LR) of 0.02.
N7 points
5. Limitation
PV+ = Positive Predictive Values.
PV = Negative Predictive Value.
LR+ = Positive Likelihood Ratio.
LR = Negative Likelihood Ratio.
p = 0.019.
p = 0.001.
p = 0.003.
One limitation of our study is that it was based on a population of patients from a single center. In addition, the patients were admitted to
the surgical wards after being screened by emergency medicine physicians who had excluded other childhood illnesses. Moreover multiple
surgical registrars and residents assessed the patients and collected
the data, therefore interobserver variability should be taken into account. However, this could be reective of real-life utilization of the
score. In addition, we were not able to ensure the enrollment of consecutive patients which resulted in missing data
Management of children with suspected appendicitis is still challenging and optimal clinical decision making is still being debated. We
have developed and validated a new clinical prediction model, the
CAS, which is composed of a clinical scoring system and a rule-out coefcient utilizing a combination of 3 inammatory markers. The diagnostic efcacy of the CAS is further maximized by risk stratication. The CAS
outperforms the PAS in ruling out appendicitis particularly for children
T.-L. Yap et al. / Journal of Pediatric Surgery 50 (2015) 20512055
2055
Appendix A
Fig. A.1. Age stratied ROC curve of CAS and PAS.
Table A.1
Diagnostic accuracy of WBC, neutrophil, CRP and in combination.
WBC 10,000/L
Neutrophil 75%
CRP 5 g/L
Combined Triple Markers
App
Nonapp
102
17
79
40
99
20
119
0
126
129
80
175
143
112
192
63
aged 12 and below. In addition, it limits the number of patients requiring
further imaging examination by identifying patients with equivocal diagnosis. The score however would need further evaluation by external
centers.
Acknowledgements
The study was supported by the SingHealth Foundation Research Grant.
The authors thank Dr Li Xiangzhen, Fay for editing the nal manuscript.
References
[1] Bundy DG, Byerley JS, Liles EA, et al. Does this child have appendicitis? JAMA 2007;
298:43851.
[2] Martin AE, Vollman D, Adler B, et al. CT scans may not reduce the negative appendectomy rate in children. J Pediatr Surg 2004;39:88690.
[3] Shah NB, Platt SL. ALARA: is there a cause for alarm? Reducing radiation risks from
computed tomography scanning in children. Curr Opin Pediatr 2008;20:2437.
[4] Kulik DM, Uleryk EM, Maguire JL. Does this child have appendicitis? A systematic review of clinical prediction rules for children with acute abdominal pain. J Clin
Epidemiol 2013;66:95104.
Sensitivity (%)
Specicity (%)
PPV (%)
85.7
50.6
44.7
NPV (%)
0.9
66.4
68.6
49.7
81.4
83.2
43.9
40.9
84.8
100.0
24.7
38.3
100.0
[5] Andersson RE. Meta-analysis of the clinical and laboratory diagnosis of appendicitis.
Br J Surg 2004;91:2837.
[6] Sengupta A, Bax G, Paterson-Brown S. White cell count and C-reactive protein measurement in patients with possible appendicitis. Ann R Coll Surg Engl 2009;91:
1135.
[7] Shogilev DJ, Duus N, Odom SR, et al. Diagnosing appendicitis: evidence-based review
of the diagnostic approach in 2014. West J Emerg Med 2014;15:85971.
[8] Yu CW, Juan LI, Wu MH, et al. Systematic review and meta-analysis of the diagnostic
accuracy of procalcitonin, C-reactive protein and white blood cell count for
suspected acute appendicitis. Br J Surg 2013;100:3229.
[9] Wang LT, Prentiss KA, Simon JZ, et al. The use of white blood cell count and left shift
in the diagnosis of appendicitis in children. Pediatr Emerg Care 2007;23:6976.
[10] Kharbanda AB, Cosme Y, Liu K, et al. Discriminative accuracy of novel and traditional
biomarkers in children with suspected appendicitis adjusted for duration of abdominal pain. Acad Emerg Med 2011;18:56774.
[11] Bhatt M, Joseph L, Ducharme FM, et al. Prospective validation of the pediatric appendicitis
score in a Canadian pediatric emergency department. Acad Emerg Med 2009;16:5916.
[12] Fleischman RJ, Devine MK, Yagapen MA, et al. Evaluation of a novel pediatric appendicitis pathway using high- and low-risk scoring systems. Pediatr Emerg Care 2013;
29:10605.
[13] Schneider C, Kharbanda A, Bachur R. Evaluating appendicitis scoring systems using a
prospective pediatric cohort. Ann Emerg Med 2007;49:77884.
[14] Goldman RD, Carter S, Stephens D, et al. Prospective validation of the pediatric appendicitis score. J Pediatr 2008;153:27882.
[15] Maguire JL, Kulik DM, Laupacis A, et al. Clinical prediction rules for children: a systematic review. Pediatrics 2011;128:e66677.
S-ar putea să vă placă și
- Makalah 2Document31 paginiMakalah 2Aldo YustiantoÎncă nu există evaluări
- Tuberculosis and Nephrotic Syndrome in A Child: Case ReportDocument34 paginiTuberculosis and Nephrotic Syndrome in A Child: Case ReportAldo YustiantoÎncă nu există evaluări
- Tuberculosis and Nephrotic Syndrome in A Child: Case ReportDocument34 paginiTuberculosis and Nephrotic Syndrome in A Child: Case ReportAldo YustiantoÎncă nu există evaluări
- Car C0001Document32 paginiCar C0001Aldo YustiantoÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Zener Barrier: 2002 IS CatalogDocument1 paginăZener Barrier: 2002 IS CatalogabcÎncă nu există evaluări
- Microporous and Mesoporous Materials: SciencedirectDocument8 paginiMicroporous and Mesoporous Materials: SciencedirectAssyakurÎncă nu există evaluări
- Microcontroller Based Vehicle Security SystemDocument67 paginiMicrocontroller Based Vehicle Security Systemlokesh_045Încă nu există evaluări
- Chapter 6 AssignmentDocument6 paginiChapter 6 AssignmentRohit RajeevÎncă nu există evaluări
- 9Y011-02704 KubotaDocument143 pagini9Y011-02704 KubotaZaqi SatchÎncă nu există evaluări
- X-Plane Mobile ManualDocument66 paginiX-Plane Mobile ManualRafael MunizÎncă nu există evaluări
- MOVIDRIVE-B Lab7Document6 paginiMOVIDRIVE-B Lab7GrungeokêÎncă nu există evaluări
- Plagiarism - ReportDocument6 paginiPlagiarism - ReportDipesh NagpalÎncă nu există evaluări
- Sewage: Vag Hade Flap ValveDocument4 paginiSewage: Vag Hade Flap ValveAhmedRamadanÎncă nu există evaluări
- Bhagwat Gita in by EB KarkiDocument97 paginiBhagwat Gita in by EB KarkiYogaguru Mohan100% (1)
- 307-01 Automatic Transmission 10 Speed - Description and Operation - DescriptionDocument12 pagini307-01 Automatic Transmission 10 Speed - Description and Operation - DescriptionCARLOS LIMADAÎncă nu există evaluări
- Narayana Xii Pass Ir Iit (2023 24) PDFDocument16 paginiNarayana Xii Pass Ir Iit (2023 24) PDFRaghav ChaudharyÎncă nu există evaluări
- Three - Dimensional Viscous Confinement and Cooling of Atoms by Resonance Radiation PressureDocument6 paginiThree - Dimensional Viscous Confinement and Cooling of Atoms by Resonance Radiation PressureWenjun ZhangÎncă nu există evaluări
- Relay Maintenance and Testing: BenefitsDocument2 paginiRelay Maintenance and Testing: BenefitsojoladapoÎncă nu există evaluări
- Table of Trigonometric IdentitiesDocument2 paginiTable of Trigonometric IdentitiesVaios PeritogiannisÎncă nu există evaluări
- BSIT Nov Dec 2012 2nd CycleDocument59 paginiBSIT Nov Dec 2012 2nd CyclePiyush PriyankÎncă nu există evaluări
- Shaping Plastic Forming1Document24 paginiShaping Plastic Forming1Himan JitÎncă nu există evaluări
- Ss e (Bocr) ManualDocument2 paginiSs e (Bocr) ManualNaveen GuptaÎncă nu există evaluări
- Heat Fusion of Ice ReportDocument8 paginiHeat Fusion of Ice Reporthasifah abdazizÎncă nu există evaluări
- CH 1 Optical Fiber Introduction - 2Document18 paginiCH 1 Optical Fiber Introduction - 2Krishna Prasad PheluÎncă nu există evaluări
- Servodisc CatalogDocument87 paginiServodisc CatalogEstebanRojasKrustofskyÎncă nu există evaluări
- Reverse Circulation Cementing: The Complete PictureDocument104 paginiReverse Circulation Cementing: The Complete PictureJoan Corso100% (1)
- Driver LCI 150W 500-850ma FlexC NF h28 EXC3 enDocument7 paginiDriver LCI 150W 500-850ma FlexC NF h28 EXC3 enMoustafa HelalyÎncă nu există evaluări
- Exercise 1 - Revision StringDocument2 paginiExercise 1 - Revision StringKu H6Încă nu există evaluări
- 3700 RES 5.5.1 Install GuideDocument38 pagini3700 RES 5.5.1 Install Guidejlappi100% (1)
- Power Electronics Circuits Devices and Applications by Muhammad H RashidDocument602 paginiPower Electronics Circuits Devices and Applications by Muhammad H Rashidkartik balojiÎncă nu există evaluări
- Optimization of Decarbonization On Steel IndustryDocument28 paginiOptimization of Decarbonization On Steel Industrymsantosu000Încă nu există evaluări
- Lecture-7 - Line CodingDocument14 paginiLecture-7 - Line CodingFahim Hasan AlifÎncă nu există evaluări
- North Sails Brochure 2007 enDocument24 paginiNorth Sails Brochure 2007 ennorthsailsÎncă nu există evaluări
- Ampla's Technology ArchitectureDocument4 paginiAmpla's Technology ArchitecturesyeadtalhaaliÎncă nu există evaluări