Documente Academic
Documente Profesional
Documente Cultură
Acne Vulgaris: Prevalence and Clinical Forms in Adolescents From São Paulo, Brazil
Încărcat de
Alyani Akramah BasarTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Acne Vulgaris: Prevalence and Clinical Forms in Adolescents From São Paulo, Brazil
Încărcat de
Alyani Akramah BasarDrepturi de autor:
Formate disponibile
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 428
428
INVESTIGATION
Acne vulgaris: prevalence and clinical forms in adolescents
from So Paulo, Brazil*
Edilia Bagatin1
Lilia Ramos dos Santos Guadanhim1
Luiz Roberto Terzian3
Mercedes Florez4
Denise Loureno Timpano1
Vanessa Mussupapo Andraus Nogueira2
Denise Steiner2
DOI: http://dx.doi.org/10.1590/abd1806-4841.20142100
Abstract: BACKGROUND: Acne is a common disease in adolescents, but there are no epidemiological data for acne
in Brazil.
OBJECTIVES: To estimate the prevalence and degree of acne in adolescents from Sao Paulo and study socio-demographic factors, family history and lifestyle, associated with the disease.
METHODS: Cross-sectional study with 452 adolescents aged between 10 and 17 (mean=13.3 years), students from
elementary and high school, examined by 3 independent evaluators.
RESULTS: 62.4% were female, 85.8% white and 6.4% were aged 14. The prevalence was 96.0% and increased with
age - all students over 14 had acne. The most prevalent form of acne was comedonal (61.1%), followed by mild
(30.6%) and moderate (7.6%) papular-pustular, which affected mostly the face (97.5%). About half of the adolescents reported family history for acne in mother or father, and 20.6% reported previous treatment for acne. There
was a higher chance of presenting non-comedonal acne with increased age (p<0.001).
DISCUSSION: The prevalence of acne in adolescents varies widely due to the clinical features and diagnostic methods used. Adolescents whose brothers/sisters had acne (OR=1.7-p=0.027) and those over 13 (OR=8.3p<0.001), were more likely to have non-comedonal acne.
CONCLUSION: This study showed high prevalence of acne in adolescents from Sao Paulo, predominantly the comedonal form on the face, with a higher chance of presenting non-comedonal acne with increased age.
Keywords: Acne vulgaris; Demographic data; Family characteristics; Prevalence; Socioeconomic factors
INTRODUCTION
Acne vulgaris is a chronic inflammatory disease
of the pilosebaceous follicles, common in adolescents,
characterized by comedones, papules, pustules, cysts,
nodules, and occasionally scars. Its pathogenesis
includes follicular hyperkeratinization, sebaceous
hypersecretion due to androgen stimulation, follicular
colonization by Propionibacterium acnes, immune and
inflammatory responses. It affects the face, anterior
chest and upper back.1
The prevalence of acne in adolescents and
2-11
adultsvaries among countries and ethnic groups. In
Australia, acne was observed in 27.7% of students
aged 10-12 and in 93.3% of adolescents aged 16-18. A
study in Peru reported a prevalence of 16.33% and
71.23%, in students aged 12 and 17, respectively.2 In
Received on 31.08.2012.
Approved by the Advisory Board and accepted for publication on 02.03.2013.
* Work performed at the Department of Dermatology - Federal University of Sao Paulo (UNIFESP) - Sao Paulo (SP), Brazil.
Financial Support: Laboratrio Stiefel.
Conflict of Interest: Estudo apoiado pelo Laboratrio Stiefel.
1
2
3
4
Universidade Federal de So Paulo (UNIFESP) So Paulo (SP), Brazil.
Universidade de Mogi das Cruzes (UMC) Mogi das Cruzes (SP), Brazil.
Faculdade de Medicina do ABC (FMABC) Santo Andr (SP), Brazil.
Private clinic - Miami, FL, Estados Unidos.
2014 by Anais Brasileiros de Dermatologia
An Bras Dermatol. 2014;89(3):428-35.
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 429
Acne vulgaris: prevalence and clinical forms in adolescents from So Paulo, Brazil
countries including Belgium and China, prevalence in
adolescents is high, about 90%, while in England it is
estimated at 50%. It is generally assumed that acne
occurs in 70-80% of adolescentes.12,13
A Chinese study observed no disease in children under 10 and a prevalence of 1.6% at the age of
10, which increased with age, reaching 46.8% by the
age of 19, then decreased progressively, and was rare
in individuals aged over 50. In this study, 68.4% of
subjects had mild acne, 26.0% moderate and 5.6%
severe. Only a third of them had been treated before
(39.0% female and 29.6% males). Acne was more
prevalent in adolescent men and adult women.1 Two
studies in the UK reported similar results.4,8
In the US, acne is the fourth most common reason for seeking medical consultation among patients
aged 11- 21, and it accounts for 4% of all visits from
patients aged 15-19.14-16 Different studies have shown
prevalence rates ranging from 28.9-91.3% in adolescents.2,6,14,17,18
In Brazil, acne accounts for approximately 14%
of dermatological consultations and affects both genders, different ethnicities and all age groups, predominantly in the first three decades of life.19
As there are no epidemiological data on the
prevalence of acne in Brazil, the objective of this study
was: to estimate the prevalence and degree of acne in
adolescents from So Paulo (by gender and age
group); analyze the diagnostic convergence regarding
acne among three dermatologists; and study sociodemographic factors, family history and lifestyle associated with the occurrence and severity of the disease.
METHODS
Cross-sectional study including 452 adolescents
aged 10-17, elementary and high school students from
two public and two private institutions in So Paulo,
examined by three evaluators (A, B, C).
The study population lives in So Paulo city,
which has 11,253,503 inhabitants, 867,351 aged 10-14,
and 841,081 aged 15-19 (Source: IBGE, Brazilian
Demographic Census, 2010). In addition to those born
in the city, there are citizens from all regions of Brazil,
as it is the greatest economic and industrial center in
the country, with numerous employment opportunities, as well as a large number of academic and cultural options. However, because of its size and heterogeneous living conditions, many social problems exist. It
is estimated that there are 2,895 public schools and
2,748 private schools. Regarding elementary education, 644,804 students are registered at public schools
and 137,024 at private schools; while the numbers for
high school are 380,035 students at public schools and
78,274 at private schools (Source: School Census MEC
/ Inep and Educational Information Center of State
429
Department of Education 2008).
The sample size was based on Rademakers
study (1989),20 in which the prevalence of acne in girls
ranged from 61% at the age of 12, to 83% at the age of
16 and, for boys, the equivalent rates were 40% and
95%, respectively. Assuming an average prevalence of
acne of 50%, at a confidence interval of 95%, and a
maximum error of 7.5%, the estimated sample was
of 171 adolescents from each gender. Taking into
account a possible loss of 50%, 257 male and 257
female adolescents were necessary.
Three reviewers assessed the presence or
absence of acne and its characteristics: clinical form
(comedonal, papular-pustular - mild, moderate or
severe, nodular-cystic - moderate or severe), age of
onset, location (face, trunk or both) and treatment
(age, duration and medication used).21 The characteristics of parents (education, previous history and age
of onset), socio-demographic factors and lifestyle conditions of the adolescents (age, gender, race, current
school grade, smoking and age of onset of smoking),
were also analyzed. For girls, the age of menarche and
oral contraceptive use were considered.
Agreement between the three evaluators was
gauged using kappa statistics (for presence or absence
of acne) and weighted kappa statistics (for the degree
of acne). Agreement is considered moderate
when0.4<0.6, good when 0.6<0.8 and very good
(almost perfect) when0.8.
The prevalence of acne, according to sex and
age, was estimated at a confidence interval of 95% (CI
= 95%). Factors associated with the occurrence of acne
were analyzed via the association test, using the chisquare test.
Upon analysis of factors associated with severity of acne, the dependent variable was the disease
form (comedonal or non comedonal) and the independent variables were gender, age, skin color (white,
black/brown and yellow), education levels of father
and mother, occurrence of acneandacne scarsin parents, and smoking. This analysis was conducted by
the association chi-square test or chi-square test for
trendand multiple logistic regression model. The final
result was assessed by the Hosmer-Lemeshow test.
The variables, presence of acne and acne scars in
parents were selected to illustrate the possible role of
genetic factors in the development and severity of the
disease. We also planned to correlate parents educational levels with willingness to seek medical treatment.
The double entry software Epi-Info (version
6.04) was used to treat all data, while consistency was
assessed through the validate command. Afterwards,
the databases were exported to the extensions xls
(Excel) and sav (SPSS), using the StatTransfer software
(version 2001 for Windows).
An Bras Dermatol. 2014;89(3):428-35.
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 430
430
Bagatin E, Timpano DL, Guadanhim LRS, Nogueira VMA, Terzian LR, Steiner D, Florez M
In all analyses, we used SPSS for Windows (version 12.0) and the significance level considered was 5%.
RESULTS
In order to analyze diagnostic convergence for
acne among the three evaluators, 52 students (27 male,
25 female) from two classrooms at one school, aged
12-15 years were randomly selected.
The comparison between examiners A and B
revealed only one disagreement regarding the presence or absence of acne, and it was not possible to calculate the kappa statistic, because examiner B considered that all students had acne. In assessing the degree
of acne, the weighted kappa was 0.6, showing strong
agreement between the examiners.
Comparing evaluators A and C, there were four
disagreements concerning the presence of acne ( =
0.31) and strong agreement over the degree of acne
(p = 0.6).
The data provided by examiners B and C
revealed five discrepancies in comparing the presence
of acne, and it was not possible to calculate the kappa
statistic because examiner B considered that all students had acne. There was strong agreement between
examiners B and C when comparing the degree of
acne (p = 0.6).
Among the 452 adolescents evaluated, 62.4%
were female, 85.8% white and 6.4% were aged 14. The
age ranged from 10-17, with a mean of 13.3 (SD = 2.02
years), and median of 13.0.
Acne was present in 434 adolescents examined,
i.e., the prevalence was 96.0% (CI 95% [94.2;
97.8]). There was no difference between sexes (p =
0.856): male, 95.9% (IC 95% [92.9; 98.9]) and female,
96.1%(IC 95% [93.8; 98.4]).The prevalence increased
with age, but there were no differences at ages 10, 11,
12 and 13 (90.9%, 93.3%, 91.6% and 95.5% respectively, p=0,726 chi-square test of trend). All students
over 14 had acne and therefore the confidence interval
of 95% was not calculated.
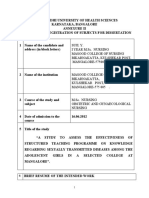
Graph 1 shows that the most prevalent form of
acne was comedonal (61.1% - CI 95% [56.5%;
65.7%]), followed by mild (30.6% - CI 95% [26.3%;
34.9%]) and moderate (7.6% - CI 95% [5.1%; 10.1%])
papular-pustular.
Table 1 presents a description of the location and
age of acne onset. The most commonly affected site
was the face (97.5%) or the face and trunk(2.3%). The
age at which students experienced their first episodes
ranged from 2 to 16; a mean of 11.5 (SD = 1.6 years) and
median of 11.0, and the most prevalent age groups
were 11 and 12 years (50.4% of patients with acne).
Use of oral contraceptives was reported by only
four adolescents (0.9%). The age of menarche ranged
from 8 to 15, with a mean of 11.8 (SD = 1.1 years) and
An Bras Dermatol. 2014;89(3):428-35.
GRAPH 1: Distribution of adolescents according to presence
and degree of acne
median of 12. Previous treatment for acne, such as
topical products, with or without skin cleansing
and oral medications, skin cleansing associated or
not with pill intake, and the use of oral medications,
was reported by 93 (20.6%) of the 452 adolescents.
Only 18 adolescents were able to recall the duration of
the treatment, which ranged from 1 to 35 months
(mean 6.3 months, SD = 8.1 months and median = 3.5
months).
Most parents had a college degree and about
half of the adolescents reported a family history of
acne in mothers or fathers. Almost all reported that
acne in parents occurred during adolescence. The
presence of acne scars was reported in 15.3% of fathers
and 13.3% of mothers (Table 2).
Presence of acne in other relatives was mentioned by 61.1% of the students, 32.5% in siblings,
34.1% in cousins and 14.4% in uncles/aunts.
Given that all teenagers over the age of 14 had
acne, analysis of associated factors was restricted to
those aged 10-13. There was no difference in acne
prevalence regarding skin color (92.1%, 100.0% and
93.3% for white, black / brown and yellow, respectively, p = 0.371), parents educational level (94.0 % vs.
92.4%, = 0.664 for father and 92.4% vs. 93.0%, p = 0.874
for mother) and family history of acne (96.8% vs.
90.6%, p = 0.118 for father; 90.6% vs. 94.2%, p = 0.289,
for mother; 91.4% vs. 93.6%, p = 0.558, for other relatives). At this age, no adolescents smoked and, therefore, the association has not been tested. Thus, since
there was no significant association between the presence of acne and the variables studied, analysis with
logistic regression models was not continued.
As there were few cases of non-comedonal
acne, lesions were classified into comedonal or noncomedonal acne. Table 3 shows a significant association between the form of acne, age and previous treatment, with a higher prevalence of comedonal acne (p
<0.001 for both). In accordance with Table 3, the
chances of presenting non-comedonal acne are higher
with increased age (chi-square test of trend - p for
trend <0.001).
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 431
Acne vulgaris: prevalence and clinical forms in adolescents from So Paulo, Brazil
431
TABLE 1: Number and percentage of teenagers with acne, regarding affected area and age of onset
No.
CI 95%
Face
Face and trunk
Trunk
Age of onset
9 years
10 years
11 years
12 years
13 years
14 17 years
Dont know
423
10
1
97.5
2.3
0.2
[95.5% ; 98.6%]
[1.3% , 4.2%]
[0.0% ; 1.3%]
27
70
116
103
72
36
10
6.2
16.2
26.7
23.7
16.6
8.3
2.2
[4.3% ; 8.9%]
[13.0% ; 19.9%]
[22.8% ; 31.1%]
[20.0% ; 28.0%]
[13.4% ; 20.4%]
[6.1% ; 11.3%]
[1.3% ; 4.2%]
Total
434
100
Affected area
TABLE 2: Number and percentage of adolescents, according to parental characteristics
No.
CI 95%
Incomplete Basic Education
Basic Education
Incomplete High School
High School
Incomplete College
College
Unkown father/ignored
Father with acne
No
Yes. in adolescence
Yes. in adulthood
Unkown father/ignored
Father with acne scars
No
Yes
Unkown father/ignored
Mothers Educational level
Incomplete Basic Education
Basic Education
Incomplete High School
High School
Incomplete College
College
Unkown mother/ignored
Mother with acne
No
Yes. in adolescence
Yes. in adulthood
Unkown mother/ignored
Mother with acne scars
No
Yes
Unkown mother/ignored
26
9
5
63
17
284
48
5.8
2.0
1.1
13.9
3.8
62.8
10.6
[4.0% ; 8.3%]
[1.1% ; 3.7%]
[0.5% ; 2.6%]
[11.0% ; 17.4%]
[2.4% ; 5.9%]
[58.3% ; 67.2%]
[8.1% ; 13.8%]
165
144
1
142
36.5
31.9
0.2
31.4
[32.2% ; 41.0%]
[27.7% ; 36.3%]
[0.0% ; 1.2%]
[27.3% ; 35.8%]
333
69
50
73.6
15.3
11.1
[69.4% ; 77.5%]
[12.2% ; 18.9%]
[8.5% ; 14.3%]
25
16
6
79
14
284
28
5.5
3.5
1.3
17.5
3.1
62.8
6.3
[3.8% ; 8.0%]
[2.2% ; 5.7%]
[0.6% ; 2.9%]
[14.3% ; 21.2%]
[1.9% ; 5.1%]
[58.3% ; 67.2%]
[4.3% ; 8.8%]
189
165
7
91
41.8
36.5
1.5
20.1
[37.4% ; 46.4%]
[32.2% ; 41.0%]
[0.8% ; 3.2%]
[16.7% ; 24.1%]
368
60
24
81.4
13.3
5.3
[77.6% ; 84.7%]
[10.5% ; 16.7%]
[3.6% ; 7.8%]
Total
452
100
Fathers Educational level
An Bras Dermatol. 2014;89(3):428-35.
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 432
432
Bagatin E, Timpano DL, Guadanhim LRS, Nogueira VMA, Terzian LR, Steiner D, Florez M
TABLE 3: Number and percentage of adolescents according to acne severity and characteristics of the adolescent.
Acne
Inflammatory
Comedonal
OR
CI 95%
Gender
p-value
0.615
Male
Female
108 (39.9%)
61 (37.4%)
163 (60.1%)
102 (62.6%)
1.108
1.000
Age (Years)
10/11
12
13
14
15
16
17
11 (11.7%)
22 (22.4%)
20 (47.6%)
23 (47.9%)
45 (58.4%)
18 (56.2%)
30 (69.8%)
83 (88.3%)
76 (77.6%)
22 (52.4%)
25 (52.1%)
32 (41.6%)
14 (43.8%)
13 (30.2%)
1.000
2.184
6.860
6.942
10.611
9.701
17.413
Skin color
White
Black/Brown
Yellow
146 (39.4%)
15 (36.6%)
8 (36.4%)
225 (60.6%)
26 (63.4%)
14 (63.6%)
1.000
0.889
0.881
Smoking
No
Yes
163 (38.4%)
6 (60.0%)
261 (61.6%)
4 (40.0%)
1.000
2.402
Previous Treatment
No
Yes
118 (34.6%)
47 (55.3%)
223 (65.4%)
38 (44.7%)
1.000
2.337
<0.001
[0.993 ; 4.802]
[2.865 ; 16.423]
[2.978 ; 16.181]
[4.888 ; 23.036]
[3.790 ; 24.831]
[7.044 ; 43.043]
0.912
[0.456 ; 1.735]
[0.360 ; 2.151]
0.198
[0.668 ; 8.640]
<0.001
[1.443 ; 3.786]
p: test Chi-square test
Gender, ethnicity and smoking did not reveal a
significant association with acne type (p> 0.05 for all).
Table 4 demonstrates a significant association
between the severity of acne and parents educational
level (p = 0.008 for father and p = 0.001 for mother),
with a higher prevalence of non-comedonal acne
among those who had studied up to high school level.
There was also a significant association between noncomedonal acne and the presence of the disease in siblings (p = 0.002), and no significant association regarding family history in fathers (p = 0.052),mothers (p =
0.085), uncles (p = 0.942) andcousins (p=0.365).
Table 5 presents the results of multiple analyses.
Independent factors associated with the severity of
acne were age and the presence of brothers/sisters with
acne, adjusted according to mothers educational level.
Adolescents whose brothers/sisters had acne and those
over 13 were more likely to have non-comedonal acne.
DISCUSSION
The prevalence of acne in adolescents varies
widely in different studies, especially due to the clinical features and methods used, namely interviews
and/or clinical examinations by a dermatologist.
An Bras Dermatol. 2014;89(3):428-35.
Clearly, patients perception of acne does not always
correspond to the diagnosis made by the doctor,
which explains discordant results when such comparisons are made.22 Moreover, we share the opinion of
some authors that the presence of open or closed
comedones, in any location, is sufficient to consider
the diagnosis of acne.23 Others defend that the presence of more than 20 lesions, including inflammatory
ones, is required for the diagnosis.24 A study with
4,191 subjects revealed an acne prevalence rate of
68.5% in boys and 59.6% in girls, with the presence of
one comedone considered suffiecient for the diagnosis. Another study encompassing 914 patients,
described a prevalence rate of only 27.9% for boys and
20.8% for girls.23 The average prevalence rate in adolescents ranges from 70 to 87%, without significant
differences between countries.23
In this study, the three evaluators diasagreed on
the diagnosis of acne. One reported that all adolescents
had acne. The presence of acne ranged from 90 to 100%
among the three examiners, and the average prevalence was 96%, higher than previously reported in the
literature.23 The examiners agreed on the severity of
acne, with a predominance of the comedonal form.
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 433
Acne vulgaris: prevalence and clinical forms in adolescents from So Paulo, Brazil
433
TABLE 4: Number and percentage of adolescents according to acne severity and characteristics of parents and
other relatives. p: test Chi-square test
Acne
Inflammatory
Comedonal
OR
CI 95%
Fathers
Educational level
p-value
0.008
High School
College
70 (47.6%)
99 (34.6%)
77 (52.4%)
188 (65.5%)
1.726
1.000
[1.151 ; 2.588]
Mothers
Educational level
High School
College
74 (49.7%)
95 (33.3%)
75 (50.3%)
190 (66.7%)
1.973
1.000
[1.317 ; 2.958]
Father with acne?
No
Yes
52 (32.5%)
89 (42.6%)
108 (67.5%)
120 (57.4%)
1.000
1.540
Mother with acne?
No
Yes
62 (34.1%)
93 (42.5%)
120 (65.9%)
126 (57.5%)
1.000
1.429
Sibling with
acne?
No
Yes
78 (33.5%)
70 (49.3%)
155 (66.5%)
72 (50.7%)
1.000
1.932
Cousin with acne?
No
Yes
85 (37.6%)
63 (42.3%)
141 (62.4%)
86 (57.7%)
1.000
1.215
188 (60.5%)
39 (60.9%)
1.000
0.980
0.001
0.052
[1.002 ; 2.367]
0.085
[0.951 ; 2.146]
0.002
[1.261 ; 2.961]
0.365
Uncle/Aunt with acne
No
123 (39.5%)
Yes
25 (39.1%)
[0.797 ; 1.853]
0.942
A study that analyzed gender and age demonstrated that, among girls, 61% had acne at the age of
12, and 83% at 16, with higher incidence between the
ages of 15 and 17. Among boys, the prevalence of acne
was 40% at the age of 12, but increased to 95% at 16,
with a peak between 17 and 19 years. 20,23 Our analysis
found that the prevalence of acne in male adolescents
was 95.9%, with no difference in female adolescents
(96.1%), which increased with age.
Ninety three (20.6%) of the 452 adolescents
evaluated, reported previous treatment for acne. A
study in New Zealand showed that 67.3% of the students surveyed reported having acne and significantly more difficulty in accessing medical treatment,
compared with those who did not mention acne
(46.0% vs. 13.3%, OR 5.29). These differences persisted
after controlling for socioeconomic factors.17
Acne in younger patients is predominantly
non-inflammatory and differs from that observed
when onset occurs later. With age, the increased pro-
[0.565 ; 1.700]
duction of sebum settles, favoring skin colonization
by Propioniumbacterium acnes and other bacteria,
which trigger immune response and the development
of inflammatory lesions, such as papules, pustules,
and nodules. In the young, there are follicular plugs
and comedones, but the production of sebum is insufficient for bacterial growth.25
In this study, we observed a predominance of
comedonal acne up to the age of 12 and a tendency for
non-comedonal acne in adolescents over 13.
Currently, it is considered that the onset of acne occurs
earlier in girls (11 years) than in boys (12 years).12 A
study in Brazil showed that the average age of onset
of acne symptoms in females was 14.3 4.1
years.19 Recently, studies have reported early onset of
acne, at the age of 8 or 9, in line with epidemiological
data, suggesting earlier start of puberty.25
Table 3 shows an increase in the prevalence of
inflammatory acne and a decreased prevalence of
comedonal acne with increased age. According to
An Bras Dermatol. 2014;89(3):428-35.
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 434
434
Bagatin E, Timpano DL, Guadanhim LRS, Nogueira VMA, Terzian LR, Steiner D, Florez M
TABLE 5: Multiple logistic regression model for factors associated with the severity of acne.
p (Hosmer-Lemeshow) = 0.546
OR Adjusted
Age (years)
10/11
12
13
14
15
16
17
1.0
2.2
8.3
7.1
10.1
9.4
17.0
Mothers Educational level
High School
College
1.5
1.0
Siblings with acne?
No
Yes
1.0
1.7
p-value
<0.001
0.061
<0.001
<0.001
<0.001
<0.001
<0.001
0.110
0.027
Table 5, adolescents over 13 were more likely to have
non-comedonal acne. This study, along with others,
therefore confirms a higher severity of acne with
increased age.25
There is a possible bias in this cross-sectional
study. From the age of 13, the chances of presenting
inflammatory acne increased and, after 14, 100% of
the adolescents were diagnosed as having acne. Acne
severity usually increases with age. As the severe
forms are more persistent, the incidence of acne may
be higher when older students are examined.
Regarding the affected area, a study conducted
in five US cities noted that approximately 50% of
patients with acne vulgaris experienced lesions on the
trunk and/or back, while over 3% had lesions only on
the trunk. Approximately 1 in 4 patients did not mention the presence of acne in the trunk that was detected by clinical examination. Most cases of acne vulgaris
on the trunk were mild to moderate in severity, and
over 75% were interested in treatment for trunk
lesions.26 In constrast, our study reported acne on the
trunk in2.5%of the adolescents, and the face was the
most frequently affected site (97.5%).
An epidemiological study conducted in French
schools, comprising 913 adolescents aged 11-18,
An Bras Dermatol. 2014;89(3):428-35.
reported that 16% of those with acne had positive
family histories for acne in their fathers, versus 8% of
those without acne.23,24 The equivalent data with
respect to mothers was 25%, versus 14% of those without acne. Among adolescents with acne, 68% of brothers and sisters also had acne, versus 57% in those
without the disease. It is known that family history of
acne in parents is most often associated with severe
acne or weaker response to oral drugs such as
cyclins.23 About half of the patients reported a parent
with history of acne, almost all during adolescence,
but there was no significant correlation between the
presence of acne in adolescents and fathers (p = 0.052)
or mothers (p = 0.085). The risk of inflammatory acne,
although slight, was greater among adolescents
whose siblings had the disease, which is consistent
with the literature and probably related to genetic factors. The same pattern was observed in relation to
lower educational levels of parents, which may mean
less concern with the disease or greater difficulty in
accessing early treatment.
This study demonstrated the presence of moderate and severe inflammatory acne in 8.3% of adolescents, which is lower than that reported in the literature (around 20%).12 The occurrence of these forms
ranged from 14% in Iranand 48% in Singapore.12,13
A Brazilian study that evaluated the prevalence
of dermatosis in school children aged 7-14, found
prevalence rates of 9% and 11% for comedonal acne,
and 19% and 5% for papular-pustular acne, respectively, in public and private schools.27 In our study,
there was no difference in prevalence between public
and private schools.
Limitations of this study include the sample
size and characteristics of the selected population.
Multicenter studies should be conducted to estimate
the prevalence of acne vulgaris in Brazil.
CONCLUSION
This study revealed a high prevalence of acne in
adolescents from So Paulo, Brazil, with a higher
prevalence of the comedonal form.Up to the age of 12,
we observed a predominance of comedonal acne and
a tendency for non-comedonal acne in adolescents
over 13.The only factor that determined the presence
of the disease was age, since 100% of the adolescents
over 14 were diagnosed with acne vulgaris. q
Revista3Vol89ingles-Bruno_Layout 1 5/20/14 1:10 PM Pgina 435
Acne vulgaris: prevalence and clinical forms in adolescents from So Paulo, Brazil
435
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
Shen Y, Wang T, Zhou C, Wang X, Ding X, Tian S, et al. Prevalence of acne vulgaris in
chinese adolescents and adults: a community-based study of 17,345 subjects in six
cities. Acta Derm Venereol. 2012;92:40-4.
Kilkenny M, Merlin K, Plunkett A, Marks R. The prevalence of common skin conditions
in Australian school students: 3. acne vulgaris. Br J Dermatol. 1998;139:840-5.
Freyre EA, Rebaza RM, Sami DA, Lozada CP. The prevalence of facial acne in
Peruvian adolescents and its relation to their ethnicity. J Adolesc Health.
1998;22:480-4.
Cunliffe WJ, Gould DJ. Prevalence of facial acne vulgaris in late adolescence and in
adults. Br Med J. 1979;1:1109-10.
Yahya H. Acne vulgaris in Nigerian adolescents - prevalence, severity, beliefs, perceptions, and practices. Int J Dermatol. 2009;48:498-505.
Smithard A, Glazebrook C, Williams HC. Acne prevalence, knowledge about acne and
psychological morbidity in mid-adolescence: a community-based study. Br J
Dermatol. 2001;145:274-9.
Yeung CK, Teo LH, Xiang LH, Chan HH. A community-based epidemiological study of
acne vulgaris in Hong Kong adolescents. Acta Derm Venereol. 2002;82:104-7.
Goulden V, Stables GI, Cunliffe WJ. Prevalence of facial acne in adults. J Am Acad
Dermatol. 1999;41:577-80.
Stern RS. The prevalence of acne on the basis of physical examination. J Am Acad
Dermatol. 1992;26:931-5.
Collier CN, Harper JC, Cafardi JA, Cantrell WC, Wang W, Foster KW, et al. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008;58:56-9.
Poli F, Dreno B, Verschoore M. An epidemiological study of acne in female adults:
results of a survey conducted in France. J Eur Acad Dermatol Venereol.
2001;15:541-5.
Drno B. Recent data on epidemiology of acne. Ann Dermatol Venereol.
2010;137:S49-51
Ghodsi SZ, Orawa H, Zouboulis CC. Prevalence, severity, and severity risk factors of
acne in high school pupils: a community-based study. J Invest Dermatol.
2009;129:2136-41
Law MP, Chuh AA, Lee A, Molinari N. Acne prevalence and beyond: acne disability
and its predictive factors among Chinese late adolescents in Hong Kong. Clin Exp
Dermatol. 2010;35:16-21.
Ziv A, Boulet JR, Slap GB. Utilization of physician offices by adolescents in the United
States. Pediatrics. 1999;104:35-42.
Stern RS. Acne therapy. Medication use and sources of care in office-based practice. Arch Dermatol. 1996;132:776-80.
17. Purvis D, Robinson E, Watson P.. Acne prevalence in secondary school students and
their perceived difficulty in accessing acne treatment. N Z Med J. 2004;117:U1018.
18. Stathakis V, Kilkenny M, Marks R. Descriptive epidemiology of acne vulgaris in the
community. Australas J Dermatol. 1997;38:115-23.
19. Schmitt JV, Masuda PY, Miot HA. Acne in women: clinical patterns in different agegroups. An Bras Dermatol. 2009;84:349-54.
20. Rademaker M, Garioch JJ, Simpson NB. Acne in school children: no longer a concern for dermatologists. Br Med J. 1989;298:1217-9.
21. Gollnick H, Cunliffe W, Berson D, Dreno B, Finlay A, Leyden JJ, et al. Management of
acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad
Dermatol. 2003;49:S1-37.
22. Bagatin E, Kamamoto CS, Guadanhim LR, Sanudo A, Dias MC, Barraviera IM, et al.
Prevalence of acne vulgaris in patients with Down syndrome. Dermatology.
2010;220:333-9.
23. Dreno B, Poli F. Epidemiology of acne. Dermatology. 2003;206:7-10.
24. Daniel F, Dreno B, Poli F, Auffret N, Beylot C, Bodokh I, et al. Descriptive epidemiological study of acne on scholar pupils in France during autumn. Ann Dermatol
Venereol. 2000;127:273-8.
25. Friedlander SF, Eichenfield LF, Fowler JF Jr, Fried RG, Levy ML, Webster GF. Acne epidemiology and pathophysiology. Semin Cutan Med Surg. 2010;29:2-4.
26. Del Rosso JQ, Bikowski JB, Baum E, Smith J, Hawkes S, Benes V, et al. A closer look
at truncal acne vulgaris: prevalence, severity, and clinical significance. J Drugs
Dermatol. 2007;6:597-600.
27. Laczynski CM, Cestari S da C. Prevalence of dermatosis in scholars in the region of
ABC paulista. An Bras Dermatol. 2011;86:469-76.
MAILING ADDRESS:
Denise Loureno Timpano
Rua Borges Lagoa, 508
Vila Clementino
04038-000 - So Paulo - SP
Brazil
E-mail: denise_timpano@yahoo.com.br
How to cite this article: Bagatin E, Timpano DL, Guadanhim LRS, Nogueira VMA, Terzian LR, Steiner D, Florez
M. Acne vulgaris: prevalence and clinical forms in adolescents from Sao Paulo, Brazil. An Bras Dermatol.
2014;89(3):428-35.
An Bras Dermatol. 2014;89(3):428-35.
S-ar putea să vă placă și
- Social Determinants of Health and Knowledge About Hiv/Aids Transmission Among AdolescentsDe la EverandSocial Determinants of Health and Knowledge About Hiv/Aids Transmission Among AdolescentsÎncă nu există evaluări
- Eglobal, 6413iDocument15 paginiEglobal, 6413iinsanofaksÎncă nu există evaluări
- Risk Factors for Childhood TuberculosisDocument5 paginiRisk Factors for Childhood TuberculosisAnthony Huaman MedinaÎncă nu există evaluări
- Downloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Document28 paginiDownloaded From Uva-Dare, The Institutional Repository of The University of Amsterdam (Uva)Indah Putri permatasariÎncă nu există evaluări
- vaz2011Document7 paginivaz2011MonicaÎncă nu există evaluări
- Autism Congress Analyzes ASD Prevalence Research in EuropeDocument12 paginiAutism Congress Analyzes ASD Prevalence Research in EuropeMarieta Díez-JuanÎncă nu există evaluări
- Suji. Y. I Year M.Sc. Nursing Masood College of Nursing Bikarnakatta, Kulshekar Post, MANGALORE-575005Document15 paginiSuji. Y. I Year M.Sc. Nursing Masood College of Nursing Bikarnakatta, Kulshekar Post, MANGALORE-575005pavinÎncă nu există evaluări
- Risk Factors for Dengue Incidence in Brazilian PreschoolersDocument5 paginiRisk Factors for Dengue Incidence in Brazilian PreschoolersAsri RachmawatiÎncă nu există evaluări
- Knowledge, Attitude and Practices of Students Enrolled in Health Related Courses at Saint Louis University Towards Human Papillomavirus (Philippines)Document8 paginiKnowledge, Attitude and Practices of Students Enrolled in Health Related Courses at Saint Louis University Towards Human Papillomavirus (Philippines)Alexander DeckerÎncă nu există evaluări
- Are Mental Health Problems and Depression Associated With Bruxism in ChildrenDocument12 paginiAre Mental Health Problems and Depression Associated With Bruxism in ChildrenAhmad Ulil AlbabÎncă nu există evaluări
- Stunting and Soil-Transmitted-Helminth Infections Among School-Age Pupils in Rural Areas of Southern ChinaDocument6 paginiStunting and Soil-Transmitted-Helminth Infections Among School-Age Pupils in Rural Areas of Southern ChinaRohit GehiÎncă nu există evaluări
- Journal Pone 0258219Document14 paginiJournal Pone 0258219liasarieriwan05Încă nu există evaluări
- Macedo 2010 Risk Factors For Type Diabetes Mel PDFDocument7 paginiMacedo 2010 Risk Factors For Type Diabetes Mel PDFZayÎncă nu există evaluări
- Diabetes Prevention Knowledge and Perception of Risk AmongDocument7 paginiDiabetes Prevention Knowledge and Perception of Risk AmongMuhammad AgussalimÎncă nu există evaluări
- Leprosy Among Children Under 15 Years of Age: Literature ReviewDocument8 paginiLeprosy Among Children Under 15 Years of Age: Literature ReviewCecep HermawanÎncă nu există evaluări
- Systematic Review of The Epidemiology of Acne Vulgaris: Anna Hwee Sing Heng & Fook Tim ChewDocument29 paginiSystematic Review of The Epidemiology of Acne Vulgaris: Anna Hwee Sing Heng & Fook Tim ChewRita MantovanÎncă nu există evaluări
- Leprosy in Children Under 15 Years of Age in Brazil: A Systematic Review of The LiteratureDocument13 paginiLeprosy in Children Under 15 Years of Age in Brazil: A Systematic Review of The LiteratureThadira RahmanÎncă nu există evaluări
- Identify Etiology of Morbidity Events of Earlier Children Among Multigravida Women.Document11 paginiIdentify Etiology of Morbidity Events of Earlier Children Among Multigravida Women.snehal DharmadhikariÎncă nu există evaluări
- Lepra Pada AnakDocument5 paginiLepra Pada AnakAdrian AldrinÎncă nu există evaluări
- Knowledge On Acne Vulgaris and Menstrual Cycle: A Study On Adolescent GirlsDocument8 paginiKnowledge On Acne Vulgaris and Menstrual Cycle: A Study On Adolescent GirlsChristina WiyaniputriÎncă nu există evaluări
- Significant Oral Cancer Risk Associated With Low Socioeconomic StatusDocument2 paginiSignificant Oral Cancer Risk Associated With Low Socioeconomic StatusWJÎncă nu există evaluări
- Incidence of Plasmodium Infections and Determinant Factors Among Febrile Children in A District of Northwest Ethiopia A Cross-Sectional StudyDocument18 paginiIncidence of Plasmodium Infections and Determinant Factors Among Febrile Children in A District of Northwest Ethiopia A Cross-Sectional StudyMegbaruÎncă nu există evaluări
- EhrenkraDocument9 paginiEhrenkraedwingiancarlo5912Încă nu există evaluări
- Level of Awareness and Attitude of Grade 12 GAS Students On Selected Sexually Transmitted Diseases Quantitative Research ProposalDocument37 paginiLevel of Awareness and Attitude of Grade 12 GAS Students On Selected Sexually Transmitted Diseases Quantitative Research ProposalCharlz HizonÎncă nu există evaluări
- Clinical Epidemiological Profile of Vitiligo in Children and AdolescentsDocument3 paginiClinical Epidemiological Profile of Vitiligo in Children and AdolescentsKarla KaluaÎncă nu există evaluări
- JurnalDocument18 paginiJurnalEry ShaffaÎncă nu există evaluări
- Nutritional Status of School-Aged Children in Buenos AiresDocument9 paginiNutritional Status of School-Aged Children in Buenos AiresFlori GeorgianaÎncă nu există evaluări
- Environmental Factors Associated With Acute Diarrhea Among Children Under Five Years of Age in Derashe District, Southern EthiopiaDocument10 paginiEnvironmental Factors Associated With Acute Diarrhea Among Children Under Five Years of Age in Derashe District, Southern Ethiopiadefitri sariningtyasÎncă nu există evaluări
- Super Final Output (For Hardbound)Document108 paginiSuper Final Output (For Hardbound)Melody Kaye MonsantoÎncă nu există evaluări
- Investigating Key Determinants of Childhood Diarrheal Incidence Among Patients at Hoima Regional Referral Hospital, Western UgandaDocument14 paginiInvestigating Key Determinants of Childhood Diarrheal Incidence Among Patients at Hoima Regional Referral Hospital, Western UgandaKIU PUBLICATION AND EXTENSIONÎncă nu există evaluări
- Internal Assesment For Caribbean StudiesDocument20 paginiInternal Assesment For Caribbean StudiesBrandonÎncă nu există evaluări
- Effects of Sociodemographic Factors On Febrile Convulsion PrevalenceDocument6 paginiEffects of Sociodemographic Factors On Febrile Convulsion PrevalenceNur UlayatilmiladiyyahÎncă nu există evaluări
- Level of Knowledge and Evaluation of Perceptions Regarding Pediatric Diabetes Among Greek TeachersDocument25 paginiLevel of Knowledge and Evaluation of Perceptions Regarding Pediatric Diabetes Among Greek Teachers1130223060Încă nu există evaluări
- Ijrtsat 3 1 3Document9 paginiIjrtsat 3 1 3STATPERSON PUBLISHING CORPORATIONÎncă nu există evaluări
- Socioeconomic Risk Markers of LeprosyDocument20 paginiSocioeconomic Risk Markers of LeprosyRobert ThiodorusÎncă nu există evaluări
- Epidemiologic Study of Langerhans Cell Histiocytosis in Children.Document9 paginiEpidemiologic Study of Langerhans Cell Histiocytosis in Children.marioÎncă nu există evaluări
- Gingival Disease in Adolescents Related To Puberal Stages and Nutritional StatusDocument6 paginiGingival Disease in Adolescents Related To Puberal Stages and Nutritional StatusRosa WeilerÎncă nu există evaluări
- Literature Review On Infant Mortality RateDocument4 paginiLiterature Review On Infant Mortality Rateaflsjfmwh100% (1)
- Journal of Pediatric Nursing: MSC, MSC, MSC, BSC, BSCDocument6 paginiJournal of Pediatric Nursing: MSC, MSC, MSC, BSC, BSCClaudia BuheliÎncă nu există evaluări
- Stunting, Prevalence, Associated Factors, Wondo Genet, EthiopiaDocument14 paginiStunting, Prevalence, Associated Factors, Wondo Genet, EthiopiaJecko BageurÎncă nu există evaluări
- Daft Arp Us TakaDocument12 paginiDaft Arp Us TakaAnonymous bHeH00uobÎncă nu există evaluări
- Research ProposalDocument45 paginiResearch ProposalCasey Jon VeaÎncă nu există evaluări
- Predictors of StuntingDocument12 paginiPredictors of Stuntingrezky_tdÎncă nu există evaluări
- HIV/AIDS Awareness Evaluation in The Junior and Senior High School Students of University of The East Caloocan (UEC)Document11 paginiHIV/AIDS Awareness Evaluation in The Junior and Senior High School Students of University of The East Caloocan (UEC)Sebastian Miguel CarlosÎncă nu există evaluări
- ROL FinalDocument28 paginiROL FinalSiyona BansodeÎncă nu există evaluări
- Review: Helicobacter Pylori Infection in Paediatrics: J. Nguyen, K. Kotilea, V.Y. Miendje Deyi, P. BontemsDocument8 paginiReview: Helicobacter Pylori Infection in Paediatrics: J. Nguyen, K. Kotilea, V.Y. Miendje Deyi, P. Bontemsps piasÎncă nu există evaluări
- High Rates of Undiagnosed Leprosy and Subclinical Infection Amongst School Children in The Amazon RegionDocument8 paginiHigh Rates of Undiagnosed Leprosy and Subclinical Infection Amongst School Children in The Amazon RegionMedÎncă nu există evaluări
- Childhood psoriasis literature reviewDocument9 paginiChildhood psoriasis literature reviewFranciscus BuwanaÎncă nu există evaluări
- The Prevalence of Obesity Among School-Aged Children in VietnamDocument7 paginiThe Prevalence of Obesity Among School-Aged Children in VietnamE192Rahmania N. SabitahÎncă nu există evaluări
- Lister, 2015Document7 paginiLister, 2015Bianca HlepcoÎncă nu există evaluări
- Factors Influencing Child Growth and Developmental DelaysDocument34 paginiFactors Influencing Child Growth and Developmental DelaysJablack Angola MugabeÎncă nu există evaluări
- Socioeconomic Position and Childhood-Adolescent Weight Status in Rich Countries A Systematic Review, 1990-2013.Document15 paginiSocioeconomic Position and Childhood-Adolescent Weight Status in Rich Countries A Systematic Review, 1990-2013.StephanyÎncă nu există evaluări
- Childhood Psoriasis: A Review of Onset, Presentation and TreatmentDocument8 paginiChildhood Psoriasis: A Review of Onset, Presentation and TreatmentyuriskamaydaÎncă nu există evaluări
- The Impact of Perinatal HIV Infection On Older School-Aged Children's and Adolescents' Receptive Language and Word Recognition SkillsDocument9 paginiThe Impact of Perinatal HIV Infection On Older School-Aged Children's and Adolescents' Receptive Language and Word Recognition SkillsAndrew MoriartyÎncă nu există evaluări
- Prevalence and Evolution of Cases of Sexually Transmitted Infections in Adolescents in BrazilDocument13 paginiPrevalence and Evolution of Cases of Sexually Transmitted Infections in Adolescents in BrazilADRIANA CUNHA VARGAS TOMAZÎncă nu există evaluări
- HIVAIDS-related Knowledge and Behavior Among School-AttendingDocument11 paginiHIVAIDS-related Knowledge and Behavior Among School-Attendingcarmen lopezÎncă nu există evaluări
- Scabies Among Children in EthiopiaDocument9 paginiScabies Among Children in EthiopiaIJPHSÎncă nu există evaluări
- Risk Factors For Pregnancy Among Adolescent Girls in Ecuador's Amazon Basin: A Case-Control StudyDocument8 paginiRisk Factors For Pregnancy Among Adolescent Girls in Ecuador's Amazon Basin: A Case-Control StudyJose Carlos Romero SanchezÎncă nu există evaluări
- Knowledge and Awareness On Hiv-Aids of Senior High School Students Towards An Enhanced Reproductive Health Education ProgramDocument20 paginiKnowledge and Awareness On Hiv-Aids of Senior High School Students Towards An Enhanced Reproductive Health Education ProgramGlobal Research and Development ServicesÎncă nu există evaluări
- Modern Surgical Management of Tongue Carcinoma - A Clinical Retrospective Research Over A 12 Years PeriodDocument8 paginiModern Surgical Management of Tongue Carcinoma - A Clinical Retrospective Research Over A 12 Years PeriodAlyani Akramah BasarÎncă nu există evaluări
- The Relationship Between Snoring and LeftDocument8 paginiThe Relationship Between Snoring and LeftAlyani Akramah BasarÎncă nu există evaluări
- Daftar PustakaDocument1 paginăDaftar PustakaAlyani Akramah BasarÎncă nu există evaluări
- Profile and Survival of Tongue Cancer Patients in "Dharmais" Cancer Hospital, JakartaDocument5 paginiProfile and Survival of Tongue Cancer Patients in "Dharmais" Cancer Hospital, JakartaAlyani Akramah BasarÎncă nu există evaluări
- Acne Vulgaris Acne Vulgaris Acne Vulgaris Acne Vulgaris Acne VulgarisDocument8 paginiAcne Vulgaris Acne Vulgaris Acne Vulgaris Acne Vulgaris Acne VulgarisEga JayaÎncă nu există evaluări
- 11.av HywelDocument12 pagini11.av HywelAlyani Akramah Basar100% (1)
- Short-Term Efficacy of Intravitreal Dobesilate inDocument5 paginiShort-Term Efficacy of Intravitreal Dobesilate inAlyani Akramah BasarÎncă nu există evaluări
- Effects of Age and Radiation Treatment On Function of Extrinsic Tongue MusclesDocument15 paginiEffects of Age and Radiation Treatment On Function of Extrinsic Tongue MusclesAlyani Akramah BasarÎncă nu există evaluări
- The Tipping Point Tamoxifen Toxicity, Central SerousDocument6 paginiThe Tipping Point Tamoxifen Toxicity, Central SerousAlyani Akramah BasarÎncă nu există evaluări
- Factors Associated With Fear of Falling in PeopleDocument7 paginiFactors Associated With Fear of Falling in PeopleAlyani Akramah BasarÎncă nu există evaluări
- Advances in Treating Central Serous ChorioretinopathyDocument9 paginiAdvances in Treating Central Serous ChorioretinopathyAlyani Akramah BasarÎncă nu există evaluări
- Treatment of CondilomaDocument4 paginiTreatment of CondilomaAlyani Akramah BasarÎncă nu există evaluări
- Short-Term Efficacy of Intravitreal Dobesilate inDocument5 paginiShort-Term Efficacy of Intravitreal Dobesilate inAlyani Akramah BasarÎncă nu există evaluări
- Kjo 26 260Document5 paginiKjo 26 260Alyani Akramah BasarÎncă nu există evaluări
- Timed Up & Go As A Measure For LongitudinalDocument7 paginiTimed Up & Go As A Measure For LongitudinalAlyani Akramah BasarÎncă nu există evaluări
- 1.nerve Growth Factor For Bell's PalsyDocument6 pagini1.nerve Growth Factor For Bell's PalsyAlyani Akramah BasarÎncă nu există evaluări
- Journal of Medical MicrobiologyDocument8 paginiJournal of Medical Microbiologybianti nurainiÎncă nu există evaluări
- Epidemiologi AnogenitalDocument18 paginiEpidemiologi AnogenitalAlyani Akramah BasarÎncă nu există evaluări
- Outcome in Patients With BacterialDocument6 paginiOutcome in Patients With BacterialAlyani Akramah BasarÎncă nu există evaluări
- Epidemiologi AnogenitalDocument18 paginiEpidemiologi AnogenitalAlyani Akramah BasarÎncă nu există evaluări
- Copd 2 273Document10 paginiCopd 2 273zano_adamÎncă nu există evaluări
- ATS GuidelinesDocument46 paginiATS Guidelinesapi-3847280100% (1)
- Res Lounge Anemia of PrematurityDocument10 paginiRes Lounge Anemia of PrematurityAlyani Akramah BasarÎncă nu există evaluări
- 1.nerve Growth Factor For Bell's PalsyDocument6 pagini1.nerve Growth Factor For Bell's PalsyAlyani Akramah BasarÎncă nu există evaluări
- Steroid-Antivirals Treatment Versus Steroids Alone For The Treatment of Bell's PalsyDocument9 paginiSteroid-Antivirals Treatment Versus Steroids Alone For The Treatment of Bell's PalsyAlyani Akramah BasarÎncă nu există evaluări
- 1 s2.0 S002838431400139X MainDocument10 pagini1 s2.0 S002838431400139X MainAlyani Akramah BasarÎncă nu există evaluări
- The Fourth Step in The World HealthDocument8 paginiThe Fourth Step in The World HealthAlyani Akramah BasarÎncă nu există evaluări
- NNNNNDocument11 paginiNNNNNAlyani Akramah BasarÎncă nu există evaluări
- Epidemiologi Hiv AidsDocument3 paginiEpidemiologi Hiv AidsZathisaSabilaÎncă nu există evaluări
- Videocon ProjectDocument54 paginiVideocon ProjectDeepak AryaÎncă nu există evaluări
- EINC ChecklistDocument3 paginiEINC ChecklistMARK JEFTE BRIONESÎncă nu există evaluări
- Historical Source Author Date of The Event Objective of The Event Persons Involved Main ArgumentDocument5 paginiHistorical Source Author Date of The Event Objective of The Event Persons Involved Main ArgumentMark Saldie RoncesvallesÎncă nu există evaluări
- 2.7.3 Lab Use Steganography To Hide Data Answer KeyDocument3 pagini2.7.3 Lab Use Steganography To Hide Data Answer KeyVivek GaonkarÎncă nu există evaluări
- Digitrip 520Document40 paginiDigitrip 520HACÎncă nu există evaluări
- Bahasa InggrisDocument8 paginiBahasa InggrisArintaChairaniBanurea33% (3)
- Echt Er Nacht 2014Document8 paginiEcht Er Nacht 2014JamesÎncă nu există evaluări
- F&B Data Analyst Portfolio ProjectDocument12 paginiF&B Data Analyst Portfolio ProjectTom HollandÎncă nu există evaluări
- Self ReflectivityDocument7 paginiSelf ReflectivityJoseph Jajo100% (1)
- Business Plan1Document38 paginiBusiness Plan1Gwendolyn PansoyÎncă nu există evaluări
- Jeremy Hughes ReviewDocument5 paginiJeremy Hughes ReviewgracecavÎncă nu există evaluări
- Complimentary JournalDocument58 paginiComplimentary JournalMcKey ZoeÎncă nu există evaluări
- S 212 Pre Course WorkDocument5 paginiS 212 Pre Course Workafiwierot100% (2)
- Measures of CentralityDocument13 paginiMeasures of CentralityPRAGASM PROGÎncă nu există evaluări
- Electronics Foundations - Basic CircuitsDocument20 paginiElectronics Foundations - Basic Circuitsccorp0089Încă nu există evaluări
- Indian ChronologyDocument467 paginiIndian ChronologyModa Sattva100% (4)
- Rock Laboratory PricelistDocument1 paginăRock Laboratory PricelistHerbakti Dimas PerdanaÎncă nu există evaluări
- Management and Breeding of Game BirdsDocument18 paginiManagement and Breeding of Game BirdsAgustinNachoAnzóateguiÎncă nu există evaluări
- New Japa Retreat NotebookDocument48 paginiNew Japa Retreat NotebookRob ElingsÎncă nu există evaluări
- Anatomy 090819Document30 paginiAnatomy 090819Vaishnavi GourabathiniÎncă nu există evaluări
- Primavera Inspire For Sap: Increased Profitability Through Superior TransparencyDocument4 paginiPrimavera Inspire For Sap: Increased Profitability Through Superior TransparencyAnbu ManoÎncă nu există evaluări
- Assessment in Southeast AsiaDocument17 paginiAssessment in Southeast AsiathuckhuyaÎncă nu există evaluări
- GEHC DICOM Conformance CentricityRadiologyRA600 V6 1 DCM 1030 001 Rev6 1 1Document73 paginiGEHC DICOM Conformance CentricityRadiologyRA600 V6 1 DCM 1030 001 Rev6 1 1mrzdravko15Încă nu există evaluări
- Topic1 Whole NumberDocument22 paginiTopic1 Whole NumberDayang Siti AishahÎncă nu există evaluări
- Assignment 2Document4 paginiAssignment 2maxamed0% (1)
- Non Deterministic Finite AutomataDocument30 paginiNon Deterministic Finite AutomataAnikÎncă nu există evaluări
- D2DDocument2 paginiD2Dgurjit20Încă nu există evaluări
- Professional Builder - Agosto 2014Document32 paginiProfessional Builder - Agosto 2014ValÎncă nu există evaluări
- Arts9 q4 Mod1 Theatricalforms v5Document30 paginiArts9 q4 Mod1 Theatricalforms v5Harold RicafortÎncă nu există evaluări
- The Daily Tar Heel For September 18, 2012Document8 paginiThe Daily Tar Heel For September 18, 2012The Daily Tar HeelÎncă nu există evaluări