Documente Academic
Documente Profesional
Documente Cultură
Obstetrics - The Menstrual Cycle
Încărcat de
Bea SamonteDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Obstetrics - The Menstrual Cycle
Încărcat de
Bea SamonteDrepturi de autor:
Formate disponibile
The
Menstrual Cycle | Obstetrics
THE MENSTRUAL CYCLE
Predictable, regular, cyclical, and spontaneous ovulatory
menstrual cycles are regulated by:
o Hypothalamic-pituitary axis
o Ovaries
o Genital Tract
Average cycle duration: 28 days
Average cycle range: 25-32 days
The Ovarian Cycle
1. Follicular or Pre-ovulatory Ovarian Phase
Average length: 10-14 days
The human ovary:
o At birth: 2,000,000 oocytes
o Puberty: 400,000 follicles
o Follicles are depleted at a rate of 1000
follicles/month until age 35
o Only 400 follicles are released (normal) during the
female reproductive life 99.9% of follicles
undergo atresia
GDF9 (Growth Differentiation Factor 9) and BMP-15
(Bone Morphogenetic Protein 15)
o Produced by the oocytes
o Regulates granulosa cell proliferation and
differentiation as the primary follicles grow
o Stabilizes and expands the cumulus oocyte complex
in the oviduct
Follicle-Stimulating Hormone (FSH)
o Required for further development of the large antral
follicles
o Cohort group of antral follicles that begin a phase
of semisynchronous growth based on their
maturation state
o Selection window FSH rise leading to follicle
development
Estrogen levels rise in parallel to the growth of the
dominant follicle and to the increase in the number of
granulosa cells (exclusive site of FSH receptor
expression)
After the appearance of the LH receptors, the
preovulatory granulosa cells begin to secrete
progesterone in small quantities
Preovulatory progesterone secretion positive
feedback on the estrogen primed pituitary to cause (or
augment) LH release
Early follicular phase:
o Granulosa cells produce inhibin B feedback on the
pituitary to inhibit FSH release
Late follicular phase:
o LH stimulates thecal cell production of androgens
(androstenedione) transfer to adjacent follicles
aromatization into estradiol
Growth of the dominant follicle increase in the
production of estradiol and inhibin decline in the
follicular phase FSH
Drop in FSH is the cause of the failure of other follicles
to reach the preovulatory status (Graafian follicle
stage) 95% of plasma estradiol is produced by the
dominant follicle (the one that will ovulate)
Contralateral ovary is relatively inactive
The Menstrual Cycle | Obstetrics
2. Ovulation
Increasing
estrogen
secretion
by
preovulatory
follicles
onset
of
gonadotropin
surge
(good
indicator
of
ovulation)
Occurs
34-26
hours
before
the
release
of
the
ovum
from
the
follicle
LH
secretion
peaks
at
10-12
hours
before
ovulation
stimulates
the
continuation
of
meiosis
in
the
ovum
+
release
of
the
first
polar
body
Progesterone
and
Prostaglandin
production
by
the
cumulus
cells
+
GDF9
and
BMP-15
activates
expression
of
genes
essential
to
the
formation
of
the
ECM
by
the
cumulus
complex
Expansion
20-fold
increase
in
the
cumulus
complex
volume
brought
about
by
the
outward
movement
of
the
cumulus
cells
LH-induced
remodeling
of
the
ovarian
ECM
release
of
the
mature
oocyte
and
its
surrounding
cumulus
cells
through
the
surface
epithelium
LH controls theca cell
production
of
androstenedione
diffuses into the
adjacent granulosa
cells acts as
precursor for estradiol
biosynthesis
FSH controls the ability
of the granulosa cell
to convert
androstenedione to
estradiol.
3. Luteal or Postovulatory Ovarian Phase
Luteinization
o The development of the corpus luteum from the
Graafian follicle
o Hypertrophy of the theca-lutein and granulosa-
lutein cells increased capacity for hormone
synthesis
Breakdown of the basement membrane separating the
ganulosa-lutein and theca-lutein cells
Day 2 postovulation invasion of blood vessels and
capillaries into the granulosa cell layer
Factors contributing to the rapid neovascularization of
the avascular granulosa:
o Vascular Endothelial Growth Factor (VEGF),
produced in response to the LH secretion by the
theca-lutein and granulosa-lutein cells
Luteinizing Hormone
o Primary luteotropic factor responsible for corpus
luteum maintenance
o Extends the life span of the corpus luteum in normal
women (at least 2 weeks)
o Maintains corpus luteum by means of low-
frequency, high-amplitude pulses that are secreted
by the gonadotropes
Hormone secretion pattern of the Corpus Luteum
o Increased access to considerably more steroidogenic
precursors through blood-borne LDL-derived
cholesterol increased capacity to produce
progesterone (granulosa-lutein cells)
o Low LDL minimal progesterone secretion during
the luteal phase
o HDL contributes to progesterone production
Estrogen Pattern of Secretion
o After ovulation, estrogen levels decrease
secondary rise that reaches a peak of 0.25 mg/day at
the midluteal phase (17B-estradiol)
o Secondary decline in estradiol production follows
toward the end of the luteal phase
Ovarian Progesterone Production
o Peaks during the midluteal phase (25-50 mg/day)
o In pregnancy:
Corpus
luteum
continues
progesterone
production in response to hCG
Human Corpus Luteum
o Transient endocrine organ
o In the absence of pregnancy, regresses (luteolysis)
9-11 days after ovulation (apoptotic cell death)
o Luteolysis is in part due to the decreased levels of
circulating LH during the late luteal phase and
decreased LH sensitivity of luteal cells
o Endocrine effects (drop in circulating estradiol and
progesterone) are important for folliculat
development and ovulation
o CL regression and decline signals the
endometrium to initiate menstruation.
4. Estrogen and Progesterone Action
17B-estradiol
o Most biologically potent naturally-occurring
estrogen
o Secreted by granulosa cells of the Graafian
(dominant) follicle and luteinized granulosa cells of
the corpus luteum
Estrogen
o Essential hormonal signals where most events of the
menstrual cycle depend
o Action involves ERa and ERB (nuclear hormone
receptors)
o Regulates
follicular
development,
uterine
receptivity, or blood flow
Progesterone
o Actions are mediated through the progesterone
receptor types A and B (PRA and PRB)
o Enters cells by diffusion
o Evokes rapid responses in intracellular free calcium
levels
The Menstrual Cycle | Obstetrics
After ovulation, the
CL forms and both
theca-
and
granulosa-lutein
cells respond to LH.
Theca-lutein cells
continue
androstenedione
production while
the
granulosa-
lutein cells gets
increased capacity
to
produce
progesterone and
convert
androstenedione
into estradiol. LH
and hCG bind to
the same receptor and if pregnancy occurs, the hCG rescues the
corpus luteum.
The
Endometrial
Cycle
Cyclic
changes
that
occur
in
the
endometrium
in
response
to
ovarian
steroids
Phases:
o Proliferative
o Secretory
1. Proliferative
or
Preovulatory
Endometrial
Phase
The
Endometrium
o Stratum
functionalis
(superficial
layer)
Stratum
compactum
Stratum
spongiosum
o Stratum
basalis
The
deep
layer
where
the
stratum
functionalis
is
regenerated
from
Follicular
phase
estradiol
most
important
factor
in
endometrial
recovery
after
menstruation
Normal
Range
5-7
days
or
21-30
days
1st
day
of
bleeding
=
1st
day
of
the
cycle
2/3
of
the
functional
endometrium
is
shed
off
after
menstruation
5th
day
of
bleeding
epithelial
surface
of
the
endometrium
is
restored
Preovulatory
endometrium
characterized
by
glandular,
stromal,
and
vascular
endothelial
cells
Early
Proliferative
Phase
o Endometrium
is
<2
mm
thick
o Glands
are
narrow,
tubular
structures
that
pursue
an
almost
straight
and
parallel
course
from
the
basalis
layer
towards
the
endometrial
cavity
o 5th
cycle
day
mitotic
figures
in
the
glandular
epithelium
are
identified
o Mitotic
activity
persists
up
to
the
16th
or
17th
day
(approx..
2-3
days
after
ovulation)
o Absent
extravascular
or
leukocyte
infiltration
in
the
endometrium
o Re-epithelialization
and
angiogenesis
are
important
to
stop
endometrial
bleeding.
Both
are
dependent
on
estrogen-regulated
tissue
growth
o Other pertinent factors:
Epidermal Growth Factor (EGF) and Transforming
Growth Factor a regulates epithelial cell growth
Estrogen and Fibroblast Growth Factor-9 (FGF-9)
increases stromal cell proliferation
VEGF causes angiogenesis through vessel
elongation in the basalis
Late Proliferative Phase
o Endometrium thickens due to glandular hyperplasia
and increased stromal ground substance (edema
and proteinaceous material)
o Prominent loose stroma
o Glands in the functionalis layer become widely
separated
o Glands in the basalis later are more crowded, with a
denser stroma
o Midcycle glandular epithelium becomes taller and
pseudostratified
o Microvilli in the surface epithelial cells increase the
surface area
o Cilia aids in movement of endometrial secretions
2. Secretory or Postovulatory Endometrial Phase
Constantly occurs at 12-14 days
Early Secretory Phase
o Estrogen-primed endometrium responds to rising
progesterone levels predictably
o Day 17 Glycogen accumulates in the basal portion
of the glandular epithelium subnuclear vacuole
and pseudostratification formation (1st sign of
histologically-evident ovulation)
o Day 18 vacuoles move to the apical portion of the
secretory nonciliated cells
o Day 19 secretory non-ciliated cells begin to secrete
glycoprotein and mucopolysaccharide contents into
the lumen; rising progesterone levels cessation of
glandular cell mitosis (it antagonizes estrogen
effects)
Mid- to Late-Secretory Phase
o Day 21-24 stroma becomes edematous
o Day 22-25 stromal cells surrounding the spiral
arterioles begin to enlarge; stromal mitosis apparent
Predecidual formation of the upper 2/3 of the
functionalis layer
Extensive coiling of the glands
Luminal secretions become visible
o Day 23-28 predecidual cells surround the spiral
arterioles
o Day 20-24 window of implantation
Decreased microvilli and cilia on the cell surfaces
Pinopods appear in preparation for blastocyst
implantation
Continuing growth and development of spiral
arterioles is seen
Spiral arterioles arise from radial arteries
(myometrial branches of the arcuate and
uterine vessels)
The Menstrual Cycle | Obstetrics
Essential for blood flow changes during
menstruation of implantation
Endometrium Dating
o Endometrial biopsy
o Luteal phase defect discrepancy by more than 2
days
o Failure of implantation and early pregnancy
3. Menstruation
In
the
absence
of
implantation,
glandular
secretion
ceases
and
the
breakdown
of
the
deciduas
functionalis
occur
Death
of
the
corpus
luteum
drop
in
progesterone
Luteal
progesterone
decrease
menstruation
is
initiated
Leukocyte
infiltration
key
to
endometrial
and
extracellular
matrix
breakdown
and
repair
of
the
functionalis
layer
Inflammatory
tightrope
ability
of
the
macrophages
to
assume
phenotypes
that
vary
from
pro-
inflammatory
and
phagocytic
to
immunosuppressive
and
reparative
Tissue
breakdown
and
restoration
occur
simultaneously
during
menstruation
Secretion
of
enzymes
by
the
leukocytes
in
addition
to
the
proteases
produced
by
endometrial
stromal
cells
initiate
matrix
degradation
Completion
of
tissue
shedding
microenvironment-
regulated
changes
promote
repair
and
resolution
Anatomical
Events
o Marked
changes
in
endometrial
blood
flow
o Spiral
artery
coiling
becomes
severe
resistance
to
blood
flow
endometrial
hypoxia
o Stasis
becomes
the
primary
cause
of
endometrial
ischemia
and
tissue
degeneration
o Vasoconstriction
precedes
menstruation
most
striking
and
constant
event
in
the
cycle
Limits
menstrual
blood
loss
Prostaglandins
and
Menstruation
o Produced
throughout
the
menstrual
cycle,
highest
during
menstruation
o Progesterone
withdrawal
Increases COX-2 expression increased
prostaglandin synthesis
Decreases 15-hydroxyprostaglandin expression
(degrades prostaglandin)
Net result: increased prostaglandin production
and prostaglandin-receptor density
o PGF2a vasoconstrictor produced by the
endometrium
o Prostaglandin causes:
Vasoconstriction
Myometrial contraction
Upregulation of proinflammatory responses
Activation of Lytic Mechanisms
o Protease activation degrades the endometrial
interstitial matrix
o Matric metalloproteases (MMP-1 and MMP-3)
released from the stromal cells and activate other
neutrophilic proteases
Origin of Menstrual Blood
o Arterial > Venous Bleeding
o Follows rupture of a spiral arterial hematoma
formation distention of the endometrium
rupture fissures develop in the functionalis layer
blood and tissue fragments begin to detach
o Arteriolar constriction stops the hemorrhage
o Partial tissue necrosis seals the vessel tips
o Endometrial surface is restored by growth of flanges
(collars) that form everted free ends of the
endometrial glands
Interval Between Menses
o Modal interval: 28 days 7 days
o Interval: 28 days 7 days
o Range: 21-35 days
o Duration: 2-6 days of flow
o Average Blood Loss: 20-60 mL
Education is what remains after one has forgotten everything he learned in
school.
Albert Einstein
S-ar putea să vă placă și
- Pelvic Inflammatory Disease: N. GonorrhoeaeDocument2 paginiPelvic Inflammatory Disease: N. GonorrhoeaeBea SamonteÎncă nu există evaluări
- Bone Marrow Failure StatesDocument2 paginiBone Marrow Failure StatesBea SamonteÎncă nu există evaluări
- 1.3b Medico-Legal Aspect of Sex CrimesDocument2 pagini1.3b Medico-Legal Aspect of Sex CrimesJaybee SarmientoÎncă nu există evaluări
- 1.1k Coronary Artery DiseaseDocument6 pagini1.1k Coronary Artery DiseaseBea SamonteÎncă nu există evaluări
- 1.1e Sudden Cardiac ArrestDocument4 pagini1.1e Sudden Cardiac ArrestBea SamonteÎncă nu există evaluări
- Bleeding Disorders & Disseminated Intravascular CoagulationDocument5 paginiBleeding Disorders & Disseminated Intravascular CoagulationBea SamonteÎncă nu există evaluări
- MOH Pocket Manual in Obstetrics and GynaecologyDocument194 paginiMOH Pocket Manual in Obstetrics and GynaecologyBea SamonteÎncă nu există evaluări
- 1.3G Forensic Path PDFDocument17 pagini1.3G Forensic Path PDFBea SamonteÎncă nu există evaluări
- 1.1b AutopsyDocument3 pagini1.1b AutopsyBea SamonteÎncă nu există evaluări
- 3rd Year Clinical Nephrology Preceptorial-1Document1 pagină3rd Year Clinical Nephrology Preceptorial-1Bea SamonteÎncă nu există evaluări
- Collection of Biological Sample For Dna-Oct 9Document84 paginiCollection of Biological Sample For Dna-Oct 9Bea SamonteÎncă nu există evaluări
- 1.1d EvidenceDocument2 pagini1.1d EvidenceBea SamonteÎncă nu există evaluări
- 1.1c Identification & Medicolegal Aspects of DeathDocument4 pagini1.1c Identification & Medicolegal Aspects of DeathBea SamonteÎncă nu există evaluări
- Clinpharm SGD Organophosphayte PoisoningDocument2 paginiClinpharm SGD Organophosphayte PoisoningBea SamonteÎncă nu există evaluări
- Small Group DiscussionDocument3 paginiSmall Group DiscussionBea SamonteÎncă nu există evaluări
- 1.4A Intro To HemaDocument4 pagini1.4A Intro To HemaBea SamonteÎncă nu există evaluări
- Clinical Pharmacology SGD 3 - HypertensionDocument2 paginiClinical Pharmacology SGD 3 - HypertensionBea SamonteÎncă nu există evaluări
- 1.1a Prescription WritingDocument4 pagini1.1a Prescription WritingBea SamonteÎncă nu există evaluări
- 1.6e CopdDocument6 pagini1.6e CopdBea SamonteÎncă nu există evaluări
- Clinpharm SGD Bronchial AsthmaDocument9 paginiClinpharm SGD Bronchial AsthmaBea SamonteÎncă nu există evaluări
- 1.1c Rdu ProcessDocument3 pagini1.1c Rdu ProcessBea SamonteÎncă nu există evaluări
- History PEDocument6 paginiHistory PEBea SamonteÎncă nu există evaluări
- 1.1b Clinical PharmacologyDocument1 pagină1.1b Clinical PharmacologyBea SamonteÎncă nu există evaluări
- CPC-Patho Version 6Document20 paginiCPC-Patho Version 6Bea SamonteÎncă nu există evaluări
- Thyroid CA Case Pres EditDocument42 paginiThyroid CA Case Pres EditBea SamonteÎncă nu există evaluări
- 1.2a PhlebotomyDocument7 pagini1.2a PhlebotomyBea SamonteÎncă nu există evaluări
- Semen AnalysisDocument8 paginiSemen AnalysisBea SamonteÎncă nu există evaluări
- 1.1A Total Quality Management in Health Care: Hospital ErrorsDocument3 pagini1.1A Total Quality Management in Health Care: Hospital ErrorsBea SamonteÎncă nu există evaluări
- Dilatation Clock Time Hour of Labor: Department of Obstetrics and Gynecology PartographDocument1 paginăDilatation Clock Time Hour of Labor: Department of Obstetrics and Gynecology PartographBea SamonteÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Andrew Loomis - Successful DrawingDocument211 paginiAndrew Loomis - Successful Drawingdiogo.chagas02Încă nu există evaluări
- The Marketing Plan For 2014 PETLAN CompanyDocument18 paginiThe Marketing Plan For 2014 PETLAN CompanyJared Atanerwitzy M100% (1)
- AV3 - SpeakingDocument11 paginiAV3 - SpeakingHuân MinhÎncă nu există evaluări
- Forest and Wildlife ResourcesDocument15 paginiForest and Wildlife ResourcesNazia NaushinÎncă nu există evaluări
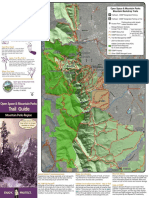
- Trail Guide: Open Space & Mountain ParksDocument2 paginiTrail Guide: Open Space & Mountain ParksKeith GruberÎncă nu există evaluări
- Evaluación Física y Clínica de Sementales Bovinos en Dos Municipios de La Costa Chica de Guerrero, MéxicoDocument7 paginiEvaluación Física y Clínica de Sementales Bovinos en Dos Municipios de La Costa Chica de Guerrero, MéxicoChacharitas IxtapalucachalcoÎncă nu există evaluări
- Covid-19 Vaccination Microplan Date - (06-05-2021) District: Kanpur NagarDocument4 paginiCovid-19 Vaccination Microplan Date - (06-05-2021) District: Kanpur NagarAditi GuptaÎncă nu există evaluări
- Gram Negative BacilliDocument15 paginiGram Negative BacilliFabasyira JamalÎncă nu există evaluări
- The Larynx: StructureDocument7 paginiThe Larynx: StructureJohn DroughtÎncă nu există evaluări
- Guppy WikiDocument11 paginiGuppy Wikiglh00Încă nu există evaluări
- Embark ReportDocument28 paginiEmbark Reportapi-149926365Încă nu există evaluări
- Happy Healthy HungDocument30 paginiHappy Healthy HungPanther Prime83% (6)
- 20084222614756Document24 pagini20084222614756masoodaeÎncă nu există evaluări
- Organisation of Living Things Study PresentationDocument26 paginiOrganisation of Living Things Study PresentationRUIZ CANO EnriqueÎncă nu există evaluări
- EDLDocument2 paginiEDLHannahÎncă nu există evaluări
- Jack Kerouac Haiku PDFDocument8 paginiJack Kerouac Haiku PDFErwin KroonÎncă nu există evaluări
- Mechanism of BreathingDocument2 paginiMechanism of BreathingMonikita PerezÎncă nu există evaluări
- Hotspots Magazine - 2015-09-01Document104 paginiHotspots Magazine - 2015-09-01Holstein PlazaÎncă nu există evaluări
- Temporal FossaDocument6 paginiTemporal Fossaوجيه الوجيهÎncă nu există evaluări
- Gayatri Mantra MudraDocument3 paginiGayatri Mantra Mudradineshgomber100% (1)
- Difhtheria in ChildrenDocument9 paginiDifhtheria in ChildrenFahmi IdrisÎncă nu există evaluări
- Biomechanics: A Course Project Submitted To Avantika University ForDocument21 paginiBiomechanics: A Course Project Submitted To Avantika University ForHarshit KarirÎncă nu există evaluări
- Intrusion With Mini ImplantDocument13 paginiIntrusion With Mini Implantdrzana78100% (1)
- Evaluation of Antiulcer Activity of Protocatechuic Acid Ethyl Ester in RatsDocument7 paginiEvaluation of Antiulcer Activity of Protocatechuic Acid Ethyl Ester in RatsZudan Ady Wijaya AptÎncă nu există evaluări
- Katia Crochet MagazineDocument159 paginiKatia Crochet MagazineMaria Louisa Wessels100% (5)
- Ex234.1 Ascaris Eggz PDFDocument7 paginiEx234.1 Ascaris Eggz PDFCarlo MendozaÎncă nu există evaluări
- Druid Handbook Part 3 Druid Spells ExaminedDocument30 paginiDruid Handbook Part 3 Druid Spells Examinedvtz06966Încă nu există evaluări
- 7th Grade Considering Cockroaches Text - QuestionsDocument3 pagini7th Grade Considering Cockroaches Text - QuestionsSubhash_iimaÎncă nu există evaluări
- The White Tiger Creative ProjectDocument3 paginiThe White Tiger Creative Projectzregina96100% (1)
- Anatomy Unit 4 Skin and Body MembranesDocument45 paginiAnatomy Unit 4 Skin and Body MembranesJaren BalbalÎncă nu există evaluări