Documente Academic
Documente Profesional
Documente Cultură
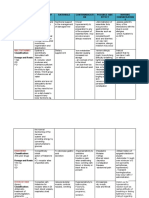
Drug Study For Tracheoesophageal Fistula
Încărcat de
AyaBasilioDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Drug Study For Tracheoesophageal Fistula
Încărcat de
AyaBasilioDrepturi de autor:
Formate disponibile
Generic Name: Albuterol
Brand Name:
Salbutamol, Proventil, Ventolin, Accuneb, airet, Novo-Salbutamol,
Proventil HFA, Gen-salbutamol, Ventodisk, Ventolin HFA, Volmax, VoSpira
ER
Classification:
Bronchodilator (therapeutic); adrenergics (pharmacologic)
Dosages
ADULTS
Oral
Initially, 2 or 4 mg (12 tsp syrup) tidqid PO; may cautiously
increase dosage if necessary to 4 or 8 mg qid, not to exceed 32
mg/day.
PEDIATRIC PATIENTS
Oral, tablets
612 yr: 2 mg tidqid. Do not exceed 24 mg/day.
> 12 yr: Use adult dosage.
Oral, syrup
< 2 yr: Safety and efficacy not established.
26 yr: Initially 0.1 mg/kg tid, not to exceed 2 mg (1 tsp) tid; if
necessary, cautiously increase stepwise to 0.2 mg/kg tid. Do not
exceed 4 mg (2 tsp) tid.
614 yr: 2 mg (1 tsp) tidqid; if necessary, cautiously increase
dosage. Do not exceed 24 mg/day in divided doses.
14 yr: Use adult dosage.
Inhalation
212 yr: For child 1015 kg, use 1.25 mg; for child > 15 kg, use 2.5
mg.
12 yr: Use adult dosage.
Solution for inhalation
1015 kg: 1.25 mg bid or tid by nebulization.
15 kg: 2.5 mg bid or tid by nebulization.
Inhalation capsules
> 4 yr: One 200 mcg capsule inhaled q 46 hr.
Prevention of exercise-induced asthma: One 200 mcg
capsule inhaled 15 min before exercise.
Relief and prevention of bronchospasm in patients with reversible
obstructive airway disease
Inhalation: Treatment of acute attacks of bronchospasm
Prevention of exercise-induced bronchospasm
Unlabeled use: Adjunct in treating serious hyperkalemia in dialysis
patients; seems to lower potassium concentrations when inhaled by
patients on hemodialysis
Mechanism Of Action
Indications
Contraindications& Cautions
Contraindicated with hypersensitivity to albuterol; tachyarrhythmias,
tachycardia caused by digitalis intoxication; general anesthesia with
halogenated hydrocarbons or cyclopropane (these sensitize the
myocardium to catecholamines); unstable vasomotor system
disorders; hypertension; coronary insufficiency, CAD; history of CVA;
COPD patients with degenerative heart disease.
Use cautiously with diabetes mellitus (large IV doses can aggravate
diabetes and ketoacidosis); hyperthyroidism; history of seizure
disorders; psychoneurotic individuals; labor and delivery (oral use
has delayed second stage of labor; parenteral use of beta2adrenergic agonists can accelerate fetal heart beat and cause
hypoglycemia, hypokalemia, pulmonary edema in the mother and
hypoglycemia in the neonate); lactation; the elderly (more sensitive
to CNS effects).
Drug to Drug Interactions
The pharmacologic effects of albuterol sulfate are attributable to activation of
beta2-adrenergic receptors on airway smooth muscle. Activation of beta2adrenergic receptors leads to the activation of adenylcyclase and to an
increase in the intracellular concentration of cyclic-3', 5'-adenosine
monophosphate (cyclic AMP).
Side effects
Nervousness, shaking (tremor), mouth/throat dryness or irritation, cough,
dizziness, headache, trouble sleeping, or nausea may occur
Adverse effect
CNS: Restlessness, apprehension, anxiety, fear, CNS stimulation,
hyperkinesia, insomnia, tremor, drowsiness, irritability, weakness,
vertigo, headache
CV: Cardiac arrhythmias, tachycardia, palpitations, PVCs (rare),
anginal pain
Dermatologic: Sweating, pallor, flushing
GI: Nausea, vomiting, heartburn, unusual or bad taste in mouth
GU: Increased incidence of leiomyomas of uterus when given in
higher than human doses in preclinical studies
Respiratory: Respiratory difficulties, pulmonary edema, coughing,
bronchospasm, paradoxical airway resistance with repeated,
excessive use of inhalation preparations
Nursing Considerations
Use minimal doses for minimal periods; drug tolerance can occur
with prolonged use.
Maintain a beta-adrenergic blocker (cardioselective beta-blocker,
such as atenolol, should be used with respiratory distress) on
standby in case cardiac arrhythmias occur.
Prepare solution for inhalation by diluting 0.5 mL 0.5% solution with
2.5 mL normal saline; deliver over 515 min by nebulization.
Do not exceed recommended dosage; administer pressurized
inhalation drug forms during second half of inspiration, because the
airways are open wider and the aerosol distribution is more
extensive.
Do not exceed recommended dosage; adverse effects or loss of
effectiveness may result. Read the instructions that come with
respiratory inhalant.
You may experience these side effects: Dizziness, drowsiness,
fatigue, headache (use caution if driving or performing tasks that
require alertness); nausea, vomiting, change in taste (eat frequent
small meals); rapid heart rate, anxiety, sweating, flushing, insomnia.
Report chest pain, dizziness, insomnia, weakness, tremors or
irregular heartbeat, difficulty breathing, productive cough, failure to
respond to usual dosage.
Generic Name Furosemide
Brand Name:
Apo-Furosemide (CAN),Furosemide Special (CAN), Lasix
Classification:
Loop diuretic
Pregnancy Category C
Dosages
ADULTS
Available forms :Tablets20, 40, 80 mg; oral solution10 mg/mL, 40 mg/5
mL; injection10 mg/mL
Pediatric Patients
Avoid use in premature infants: stimulates prostaglandin E2 synthesis and
may increase incidence of patent ductus arteriosus and complicate
respiratory distress syndrome.
Edema:
Initially, 2 mg/kg/day PO. If needed, increase by 12 mg/kg in 68
hr. Do not exceed 6 mg/kg.
Adjust maintenance dose to lowest effective level.
Pulmonary edema:
1 mg/kg IV or IM. May increase by 1 mg/kg in 2 hr until the desired
effect is seen. Do not exceed 6 mg/kg.
Patients with Renal Impairment
Up to 4 g/day has been tolerated.
IV bolus injection should not exceed 1 g/day given over 30 min.
Mechanism Of Action
Unclear. Thought to inhibit sodium and chloride reabsorption from
ascending loop of Henle and distal renal tubules. Increases
potassium excretion and plasma volume, promoting renal excretion of
water, sodium, chloride, magnesium, hydrogen, and calcium.
Indications
Contraindications& Cautions
Oral, IV: Edema associated with CHF, cirrhosis, renal disease
IV: Acute pulmonary edema
Oral: Hypertension
Severe sodium and water depletion, hypersensitivity to
sulphonamides and furosemide, hypokalaemia,
hyponatraemia, precomatose states associated with liver
cirrhosis, anuria or renal failure.
Addisons disease
Drug to Drug Interactions
Drug-drug.Aminoglycosides, ethacrynic acid, other ototoxic drugs:
increased risk of ototoxicity
Amphotericin B, corticosteroids, corticotropin, potassium-wasting
diuretics, stimulant laxatives: additive hypokalemia
Antihypertensives, diuretics, nitrates: additive hypotension
Cardiac glycosides: increased risk of glycoside toxicity and fatal
arrhythmias
Side effects
Nervousness, shaking (tremor), mouth/throat dryness or irritation, cough,
dizziness, headache, trouble sleeping, or nausea may occur
Adverse effect
CNS: dizziness, headache, vertigo, weakness, lethargy,
paresthesia, drowsiness, restlessness, light-headedness
CV: hypotension, orthostatic hypotension, tachycardia, volume
depletion, necrotizing angiitis, thrombophlebitis,
arrhythmias
EENT: blurred vision, xanthopsia, hearing loss, tinnitus
GI: nausea, vomiting, diarrhea, constipation, dyspepsia, oral
and gastric irritation, cramping, anorexia, dry mouth, acute
pancreatitis
GU: excessive and frequent urination, nocturia, glycosuria,
bladder spasm, oliguria, interstitial nephritis
Hematologic: anemia, purpura, leukopenia,
thrombocytopenia, hemolytic anemia
Hepatic: jaundice
Metabolic: hyperglycemia, hyperuricemia, dehydration,
hypokalemia, hypomagnesemia, hypocalcemia, alkalosis
Musculoskeletal: muscle pain, muscle cramps
Skin: photosensitivity, rash, diaphoresis, urticaria, pruritus,
exfoliative dermatitis, erythema multiforme
Other: fever, transient pain at I.M. injection site
Nursing Considerations
Record intermittent therapy on a calendar or dated
envelopes. When possible, take the drug early so increased
urination will not disturb sleep. Take with food or meals to
prevent GI upset.
Weigh yourself on a regular basis, at the same time and in
the same clothing, and record the weight on your calendar.
Blood glucose levels may become temporarily elevated in
patients with diabetes after starting this drug.
You may experience these side effects: Increased volume
and frequency of urination; dizziness, feeling faint on arising,
drowsiness (avoid rapid position changes; hazardous
activities, like driving; and consumption of alcohol); sensitivity
to sunlight (use sunglasses, wear protective clothing, or use a
sunscreen); increased thirst (suck on sugarless lozenges; use
frequent mouth care); loss of body potassium (a potassiumrich diet or potassium supplement will be needed).
Report loss or gain of more than 3 pounds in 1 day, swelling
in your ankles or fingers, unusual bleeding or bruising,
dizziness, trembling, numbness, fatigue, muscle weakness or
cramps.
Reduce dosage if given with other antihypertensives; readjust
dosage gradually as BP responds.
Administer with food or milk to prevent GI upset.
Give early in the day so that increased urination will not
disturb sleep.
Avoid IV use if oral use is at all possible.
WARNING: Do not mix parenteral solution with highly acidic
solutions with pH below 3.5.
Do not expose to light, may discolor tablets or solution; do not
use discolored drug or solutions.
Discard diluted solution after 24 hr.
Refrigerate oral solution.
Measure and record weight to monitor fluid changes.
Arrange to monitor serum electrolytes, hydration, liver and
renal function.
Arrange for potassium-rich diet or supplemental potassium as
needed.
Generic Name Diphenhydramine
hydrochloride
Brand Name:
Benadryl, Aler-Tab, Allergy, Allermax, Altaryl, Children's Allergy,
Diphen Cough, Diphenhist, Dytuss, Q-Dryl, Siladryl, Silphen Cough,
Simply Sleep, Sleep-ettes, Sominex Maximum Strength Caplet,
Theraflu Thin Strips Multi Symptom, Triaminic Thin Strips Cough &
Runny Nose, Unisom Sleepgels Maximum Strength, Valu-Dryl
Classification:
Pharmacologic class: Ethanolamine derivative, nonselective
histamine1-receptor antagonist
Therapeutic class: Antihistamine, antitussive, antiemetic,
antivertigo agent, antidyskinetic
Pregnancy risk category B
Dosages
Adults and children over age 12: 25 to 50 mg P.O. q 4 to 6 hours,
or 10 to 50 mg I.V. or I.M. q 2 to 3 hours p.r.n. (Some patients may
need up to 100 mg.) Don't exceed 400 mg/day.
Children ages 6 to 12: 12.5 to 25 mg P.O. q 4 to 6 hours, or 1.25
mg/kg (37.5 mg/m2) I.M. or I.V. q.i.d. Don't exceed 150 mg/day.
Children ages 2 to 5: 6.25 mg P.O. q 4 to 6 hours. Don't exceed 37.5
mg/day.
Mechanism Of Action
Interferes with histamine effects at histamine1-receptor sites;
prevents but doesn't reverse histamine-mediated response.
Also possesses CNS depressant and anticholinergic
properties.
Indications
Oral, IV: Edema associated with CHF, cirrhosis, renal disease
IV: Acute pulmonary edema
Oral: Hypertension
Contraindications& Cautions
Hypersensitivity to drug
Alcohol intolerance
Acute asthma attacks
MAO inhibitor use within past 14 days
Breastfeeding
Neonates, premature infants
Drug to Drug Interactions
Antihistamines, opioids, sedative-hypnotics: additive CNS
depression
Disopyramide, quinidine, tricyclic antidepressants: increased
anticholinergic effects
MAO inhibitors: intensified and prolonged anticholinergic
effects
Side effects
Adverse effect
1
2
3
4
5
6
7
8
9
10
11
Drowsiness
Constipation
Diarrhea
Dizziness
Dry mouth/nose/throat
Headache
Anorexia
N&V
Anxiety
GI upset
Asthenia
CNS: dizziness, headache, vertigo, weakness, lethargy,
paresthesia, drowsiness, restlessness, light-headedness
CV: hypotension, orthostatic hypotension, tachycardia, volume
depletion, necrotizing angiitis, thrombophlebitis,
arrhythmias
EENT: blurred vision, xanthopsia, hearing loss, tinnitus
GI: nausea, vomiting, diarrhea, constipation, dyspepsia, oral
and gastric irritation, cramping, anorexia, dry mouth, acute
pancreatitis
GU: excessive and frequent urination, nocturia, glycosuria,
bladder spasm, oliguria, interstitial nephritis
Hematologic: anemia, purpura, leukopenia,
thrombocytopenia, hemolytic anemia
Hepatic: jaundice
Metabolic: hyperglycemia, hyperuricemia, dehydration,
hypokalemia, hypomagnesemia, hypocalcemia, alkalosis
Musculoskeletal: muscle pain, muscle cramps
Skin: photosensitivity, rash, diaphoresis, urticaria, pruritus,
exfoliative dermatitis, erythema multiforme
Other: fever, transient pain at I.M. injection site
Nursing Considerations
1
2
3
4
5
6
7
8
9
10
Give full prophylactic dose 30min. prior to travel if used as a
prophylaxis for motion sickness
Take similar doses with meals and at bedtime
Do not use more than 2 weeks to treat insomnia
For IV, may give undiluted
Do not exceed IV rate of 25mg/minute
Drug causes drowsiness. Avoid activities requiring mental alertness
Use sun protection as it may cause photosensitivity
Use sugarless candy/gum to diminish dry mouth effects
Avoid alcohol and other CNS depressants
Stop therapy 72-96 hr. prior to skin testing. Report adverse effect
and lack of response Advise patient to avoid alcohol and other
depressants such as sedatives while taking drug.
11 Caution patient to avoid driving and other hazardous activities until he
knows how drug affects concentration and alertness.
12. As appropriate, review all other significant adverse reactions and
interactions, especially those related to the drugs, tests, herbs, and
behaviors mentioned above.
Generic Name Paracetamol,
Acetaminophen
Brand Name:
Biogesic, Panadol, Tylenol
Classification:
Non-narcotic analgesic, Antipyretic, Abenol (CA), Acephen, Anadin
Paracetamol (UK), Apo-Acetaminophen (CA), Aspirin Free Anacin,
Atasol (CA), Calpol (UK), Cetaphen, Children's Tylenol Soft Chews,
Disprol (UK), Feverall, Galpamol (UK), Genapap, Little Fevers,
Mandanol (UK), Mapap, Nortemp, Nortemp Children's, Novo-Gesic
(CA), Pain Eze, Panadol (UK), Pediatrix (CA), Silapap, Tempra (CA),
Tycolene, Tylenol 8 Hour, Tylenol, Tylenol Arthritis, Tylenol Extra
Strength, Valorin
Dosages
Per Orem: 325-650mg q4h up to a maximum of 1 gram q6h.
Suppositories: 650mg q4h not to exceed 4 grams a day for up to 10
days.
Mechanism Of Action
Pain relief may result from inhibition of prostaglandin synthesis
in CNS, with subsequent blockage of pain impulses. Fever
reduction may result from vasodilation and increased peripheral
blood flow in hypothalamus, which dissipates heat and lowers
body temperature.
Indications
Contraindications& Cautions
Drug to Drug Interactions
Side effects
Adverse effect
Nursing Considerations
Oral, IV: Edema associated with CHF, cirrhosis, renal disease
IV: Acute pulmonary edema
Oral: Hypertension
1
2
Renal Insufficiency
Anemia
Antihistamines, opioids, sedative-hypnotics: additive CNS
depression
Disopyramide, quinidine, tricyclic antidepressants: increased
anticholinergic effects
MAO inhibitors: intensified and prolonged anticholinergic
effects
1
2
3
4
5
6
7
8
9
10
11
12
13
14
Minimal GI upset.
Methemoglobinemia
Hemolytic Anemia
Neutropenia
Thrombocytopenia
Pancytopenia
Leukopenia
Urticaria
CNS stimulation
Hypoglycemic coma
Jaundice
Glissitis
Drowsiness
Liver Damage
Hematologic: thrombocytopenia, hemolytic anemia, neutropenia,
leukopenia, pancytopenia Hepatic: jaundice, hepatotoxicity Metabolic:
hypoglycemic coma
Skin: rash, urticaria
Other: hypersensitivity reactions (such as fever)
1
2
3
4
5
6
7
8
9
10
11
12
13
14
Do not exceed 4gm/24hr. in adults and 75mg/kg/day in
children.
Do not take for >5days for pain in children, 10 days for pain
in adults, or more than 3 days for fever in adults.
Extended-Release tablets are not to be chewed.
Monitor CBC, liver and renal functions.
Assess for fecal occult blood and nephritis.
Avoid using OTC drugs with Acetaminophen.
Take with food or milk to minimize GI upset.
Report N&V. cyanosis, shortness of breath and abdominal
pain as these are signs of toxicity.
Report paleness, weakness and heart beat skips
Report abdominal pain, jaundice, dark urine, itchiness or
clay-colored stools.
Phenmacetin may cause urine to become dark brown or
wine-colored.
Report pain that persists for more than 3-5 days
Avoid alcohol.
This drug is not for regular use with any form of liver
disease.
Generic Name ranitidine
hydrochloride
Brand Name:
Acid Reducer (CA), Apo-Ranitidine (CA), Co Ranitidine (CA), Gavilast
(UK), Histac (UK), Raciran (UK), Ranitil (UK), Rantek (UK), Zantac,
Zantac 75, Zantac EFFERdose
Classification:
Pharmacologic class: Histamine2-receptor antagonist
Therapeutic class: Antiulcer drug
Pregnancy risk category B
Dosages
Adults and children over age 12: 25 to 50 mg P.O. q 4 to 6 hours,
or 10 to 50 mg I.V. or I.M. q 2 to 3 hours p.r.n. (Some patients may
need up to 100 mg.) Don't exceed 400 mg/day.
Children ages 6 to 12: 12.5 to 25 mg P.O. q 4 to 6 hours, or 1.25
mg/kg (37.5 mg/m2) I.M. or I.V. q.i.d. Don't exceed 150 mg/day.
Children ages 2 to 5: 6.25 mg P.O. q 4 to 6 hours. Don't exceed 37.5
mg/day.
Mechanism Of Action
Reduces gastric acid secretion and increases gastric mucus
and bicarbonate production, creating a protective coating on
gastric mucosa
Indications
Short-term treatment of active duodenal ulcer
Maintenance therapy for duodenal ulcer at reduced dosage
Short-term treatment of active, benign gastric ulcer
Short-term treatment of GERD
Pathologic hypersecretory conditions (eg, Zollinger-Ellison
syndrome)
Treatment of erosive esophagitis
Treatment of heartburn, acid indigestion, sour stomach
Contraindications& Cautions
Hypersensitivity to drug or its components
Alcohol intolerance (with some oral products)
History of acute porphyria
Drug to Drug Interactions
Antacids: decreased ranitidine absorption
Propantheline: delayed ranitidine absorption and increased
peak blood level
Side effects
Adverse effect
Nursing Considerations
chest pain, fever, feeling short of breath,
coughing up green or yellow mucus;
easy bruising or bleeding, unusual weakness;
fast or slow heart rate;
problems with your vision;
fever, sore throat, and headache with a severe
blistering, peeling, and red skin rash
CNS: headache, agitation, anxiety
GI: nausea, vomiting, diarrhea, constipation, abdominal
discomfort or pain
Hematologic: reversible granulocytopenia and
thrombocytopenia
Hepatic: hepatitis
Skin: rash
Other: pain at I.M. injection site, burning or itching at I.V. site,
hypersensitivity reaction
Take drug with meals and at bedtime. Therapy may continue for 46
weeks or longer.
If you also are using an antacid, take it exactly as prescribed, being
careful of the times of administration.
Have regular medical follow-up care to evaluate your response.
You may experience these side effects: Constipation or diarrhea
(request aid from your health care provider); nausea, vomiting (take
drug with meals); enlargement of breasts, impotence or decreased
libido (reversible); headache (adjust lights and temperature and
avoid noise).
Report sore throat, fever, unusual bruising or bleeding, tarry stools,
confusion, hallucinations, dizziness, severe headache, muscle or
joint pain.
Tell patient smoking may decrease drug effects.
As appropriate, review all other significant and life-threatening adverse
reactions and interactions, especially those related to the drugs,
tests, herbs, and behaviors mentioned above.
Generic Name Amikacin sulfate
Brand Name:
Amikin
Classification:
Anti-infective; Aminoglycoside
Pregnancy Category: C
Dosages
Moderate to Severe Infections
Adult: IV/IM 57.5 mg/kg loading dose, then 7.5 mg/kg q12h
Child: IV/IM 57.5 mg/kg loading dose, then 5 mg/kg q8h or
7.5 mg/kg q12h
Neonate: IV/IM 10 mg/kg loading dose, then 7.5 mg/kg q12
24h
Uncomplicated UTI
Adult: IV/IM 250 mg q12h
Administration
Intramuscular
Use the 250 mg/mL vials for IM injection. Calculate the
required dose and withdraw the equivalent number of mLs
from the vial.
Give deep IM into a large muscle.
Intravenous
Verify correct IV concentration and rate of infusion with
physician for neonates, infants, and children.
Mechanism Of Action
Indications
Contraindications& Cautions
Interferes with protein synthesis in bacterial cells by binding to 30S
ribosomal subunit, leading to bacterial cell death
Severe systemic infections caused by sensitive strains of
Pseudomonas aeruginosa, Escherichia coli, or
Proteus, Klebsiella, Serratia, Enterobacter,
Actinobacter, Providencia, Citrobacter, or
Staphylococcus species
Drug to Drug Interactions
Side effects
History of hypersensitivity or toxic reaction with
an aminoglycoside antibiotic.
Safety during pregnancy (category C), lactation,
neonates and infants, or use period exceeding
14 years old is not established.
Acyclovir, amphotericin B, cephalosporin, cisplatin, diuretics,
vancomycin: increased risk of ototoxicity and nephrotoxicity
Depolarizing and nondepolarizing neuromuscular junction blockers,
general anesthetics: increased amikacin effect, possibly leading to
respiratory depression
Dimenhydrinate: masking of ototoxicity signs and symptoms
Indomethacin: increased trough and peak amikacin levels
Parenteral penicillin: amikacin inactivation
an allergic reaction (shortness of breath; closing
of the throat; hives; swelling of the lips, face, or
tongue; rash; or fainting);
little or no urine;
decreased hearing or ringing in the ears;
dizziness, clumsiness, or unsteadiness;
numbness, skin tingling, muscle twitching, or
seizures; or
severe watery diarrhea and abdominal cramps.
Adverse effect
CNS: dizziness, vertigo, tremor, numbness, depression,
confusion, lethargy, headache, paresthesia, ataxia,
neuromuscular blockade, seizures, neurotoxicity
CV: hypotension, hypertension, palpitations
EENT: nystagmus and other visual disturbances, ototoxicity,
hearing loss, tinnitus
GI: nausea, vomiting, splenomegaly, stomatitis, increased
salivation, anorexia
GU: azotemia, increased urinary excretion of casts, polyuria,
painful urination, impotence, nephrotoxicity Hematologic:
purpura, eosinophilia, leukemoid reaction, aplastic anemia,
neutropenia, agranulocytosis, leukopenia, thrombocytopenia,
pancytopenia, hemolytic anemia
Hepatic: hepatomegaly, hepatic necrosis, hepatotoxicity
Musculoskeletal: joint pain, muscle twitching
Respiratory: apnea
Skin: rash, alopecia, urticaria, itching, exfoliative dermatitis
Other: weight loss, superinfection, pain and irritation at I.M. site
Nursing Considerations
Baseline tests: Before initial dose, C&S; renal function and
vestibulocochlear nerve function (and at regular intervals
during therapy; closely monitor in the older adult, patients
with documented ear problems, renal impairment, or during
high dose or prolonged therapy).
Monitor peak and trough amikacin blood levels: Draw blood 1
h after IM or immediately after completion of IV infusion; draw
trough levels immediately before the next IM or IV dose.
Lab tests: Periodic serum creatinine and BUN, complete
urinalysis. With treatment over 10 d, daily tests of renal
function, weekly audiograms, and vestibular tests are strongly
advised.
Monitor serum creatinine or creatinine clearance (generally
preferred) more often, in the presence of impaired renal
function, in neonates, and in the older adult; note that
prolonged high trough (>8 mg/mL) or peak (>3035 mg/mL)
levels are associated with toxicity.
Monitor S&S of ototoxicity (primarily involves the cochlear
(auditory) branch; high-frequency deafness usually appears
first and can be detected only by audiometer); indicators of
declining renal function; respiratory tract infections and other
symptoms indicative of superinfections and notify physician
should they occur.
Monitor for and report auditory symptoms (tinnitus, roaring
noises, sensation of fullness in ears, hearing loss) and
vestibular disturbances (dizziness or vertigo, nystagmus,
ataxia).
Monitor & report any changes in I&O, oliguria, hematuria, or
cloudy urine. Keeping patient well hydrated reduces risk of
nephrotoxicity; consult physician regarding optimum fluid
intake.
Patient & Family Education
Report immediately any changes in hearing or unexplained
ringing/roaring noises or dizziness, and problems with
balance or coordination.
Do not breast feed while taking this drug without consulting
physician.
S-ar putea să vă placă și
- Pathophysiology Format: Predisposing Factors Precipitating Factors (Contributing) (Triggering)Document2 paginiPathophysiology Format: Predisposing Factors Precipitating Factors (Contributing) (Triggering)AyaBasilioÎncă nu există evaluări
- Flow ChartDocument2 paginiFlow ChartAyaBasilioÎncă nu există evaluări
- Communicating Pathophysiology: Impaired Absorption of The CSF in The Arachnoid SpaceDocument2 paginiCommunicating Pathophysiology: Impaired Absorption of The CSF in The Arachnoid SpaceAyaBasilioÎncă nu există evaluări
- OCT 9 Added Rrls For Table 3Document12 paginiOCT 9 Added Rrls For Table 3AyaBasilioÎncă nu există evaluări
- Review of Related LiteratureDocument2 paginiReview of Related LiteratureAyaBasilio75% (8)
- Flow ChartDocument2 paginiFlow ChartAyaBasilioÎncă nu există evaluări
- Flow ChartDocument2 paginiFlow ChartAyaBasilioÎncă nu există evaluări
- With RRL Relation But Not DoneDocument10 paginiWith RRL Relation But Not DoneAyaBasilioÎncă nu există evaluări
- Oral RevalidaDocument14 paginiOral RevalidaAyaBasilioÎncă nu există evaluări
- COPAR Vs CoM ORGDocument21 paginiCOPAR Vs CoM ORGAyaBasilioÎncă nu există evaluări
- October 15 Rrls With RefDocument13 paginiOctober 15 Rrls With RefAyaBasilioÎncă nu există evaluări
- WalbergDocument14 paginiWalbergAyaBasilioÎncă nu există evaluări
- SymptomatologyDocument2 paginiSymptomatologyAyaBasilioÎncă nu există evaluări
- Communicating Hydrocephalus Pathophysiology ExplainedDocument2 paginiCommunicating Hydrocephalus Pathophysiology ExplainedAyaBasilioÎncă nu există evaluări
- Teaching High Blood PressureDocument16 paginiTeaching High Blood PressureRosa100% (2)
- Stroke Presentation KhanDocument48 paginiStroke Presentation KhanAnahiMDÎncă nu există evaluări
- PBDocument5 paginiPBAyaBasilioÎncă nu există evaluări
- Follow UpDocument7 paginiFollow UpAyaBasilioÎncă nu există evaluări
- FInal Self Assesment QuestionsDocument1 paginăFInal Self Assesment QuestionsAyaBasilioÎncă nu există evaluări
- Ethic CDocument1 paginăEthic CAyaBasilioÎncă nu există evaluări
- Cognitive DisoerderDocument41 paginiCognitive DisoerderAyaBasilioÎncă nu există evaluări
- RRL MotivationDocument3 paginiRRL MotivationAyaBasilio60% (5)
- RRL W: Highlights R:T QuestionsDocument3 paginiRRL W: Highlights R:T QuestionsAyaBasilioÎncă nu există evaluări
- Self Assesment Q With RRL HighlightsDocument1 paginăSelf Assesment Q With RRL HighlightsAyaBasilioÎncă nu există evaluări
- FInal Self Assesment QuestionsDocument1 paginăFInal Self Assesment QuestionsAyaBasilioÎncă nu există evaluări
- Goal Not MetDocument4 paginiGoal Not MetAyaBasilioÎncă nu există evaluări
- SchizphreniaDocument151 paginiSchizphreniaAyaBasilioÎncă nu există evaluări
- AQPsych 1st Week Requiments PDFDocument9 paginiAQPsych 1st Week Requiments PDFAyaBasilioÎncă nu există evaluări
- Labs and SymptoDocument4 paginiLabs and SymptoAyaBasilioÎncă nu există evaluări
- Disaster NursingDocument14 paginiDisaster Nursingangelogrande67% (3)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- AntihistaminesDocument66 paginiAntihistaminesAfif Bastian100% (1)
- Drug InteracttionDocument8 paginiDrug InteracttionMuh. AnugrawanÎncă nu există evaluări
- Gi NelecDocument52 paginiGi NelecJordz PlaciÎncă nu există evaluări
- RLE 118 REVISED Case Scenario No. 10 Anaphylactic ShockDocument2 paginiRLE 118 REVISED Case Scenario No. 10 Anaphylactic ShockKiara Denise TamayoÎncă nu există evaluări
- IV Compatibility Chart (PDF Library)Document19 paginiIV Compatibility Chart (PDF Library)Lynda PerryÎncă nu există evaluări
- 1340v4 GastrosDocument8 pagini1340v4 GastrosRahmanandhikaÎncă nu există evaluări
- LIST OF REGISTERED DRUGS As of December 2012: DR No Generic Brand Strength Form CompanyDocument19 paginiLIST OF REGISTERED DRUGS As of December 2012: DR No Generic Brand Strength Form CompanyBenjamin TantiansuÎncă nu există evaluări
- Cefuroxime sodium treatment of infectionsDocument8 paginiCefuroxime sodium treatment of infectionsIrene CerisseÎncă nu există evaluări
- Pepcid Case AnalysisDocument6 paginiPepcid Case AnalysisessÎncă nu există evaluări
- College Nursing Drug StudyDocument19 paginiCollege Nursing Drug StudyBasema HashhashÎncă nu există evaluări
- Comparison of Omeprazole and Ranitidine For Stress Ulcer ProphylaxisDocument5 paginiComparison of Omeprazole and Ranitidine For Stress Ulcer ProphylaxisAngelica Hurtado CollanteÎncă nu există evaluări
- Lndi 2015 PDFDocument606 paginiLndi 2015 PDFloulouqwerty123Încă nu există evaluări
- HEPATITIS A DRUG STUDY FinalDocument3 paginiHEPATITIS A DRUG STUDY FinalJordz PlaciÎncă nu există evaluări
- Drug Ana Medicine WardDocument5 paginiDrug Ana Medicine WardMark Christian CuiÎncă nu există evaluări
- Is It Ethical to Brand This ConditionDocument4 paginiIs It Ethical to Brand This Conditionfabian dionÎncă nu există evaluări
- Efficacy of Proton Pump Inhibitors and H2 Blocker in The Treatment of Symptomatic Gastroesophageal Reflux Disease in InfantsDocument5 paginiEfficacy of Proton Pump Inhibitors and H2 Blocker in The Treatment of Symptomatic Gastroesophageal Reflux Disease in InfantsAndhika DÎncă nu există evaluări
- Bagong DrugsDocument7 paginiBagong DrugsmcensoredÎncă nu există evaluări
- Evaluation of H 2 - Receptor Antagonists - Cimetidine, Ranitidine and Famotidine in An In-Vivo Gingivitis Model A.G. Snider, J.P. Ebel, H.M. Pickrum, R.E. SingerDocument2 paginiEvaluation of H 2 - Receptor Antagonists - Cimetidine, Ranitidine and Famotidine in An In-Vivo Gingivitis Model A.G. Snider, J.P. Ebel, H.M. Pickrum, R.E. Singer2288RÎncă nu există evaluări
- Drug Study Ranitidine Citicoline Enalapril Aspilet Cefuroxime EtcDocument10 paginiDrug Study Ranitidine Citicoline Enalapril Aspilet Cefuroxime EtcmayeÎncă nu există evaluări
- Drug StudyDocument14 paginiDrug StudyTin BernardezÎncă nu există evaluări
- OtcDocument10 paginiOtcJames PerianayagamÎncă nu există evaluări
- New Drug Development and Approval ProcessDocument152 paginiNew Drug Development and Approval ProcessJhef ebuengaÎncă nu există evaluări
- Pharmaceutical Generics Available As InfusionsDocument7 paginiPharmaceutical Generics Available As InfusionsAmbreen AmirÎncă nu există evaluări
- NitrosaminesDocument31 paginiNitrosaminesJaya AbrahamÎncă nu există evaluări
- Drug StudyDocument4 paginiDrug StudyCharlayne AnneÎncă nu există evaluări
- Ranitidine (Zantac)Document3 paginiRanitidine (Zantac)sshah56Încă nu există evaluări
- Case 3 DengueDocument19 paginiCase 3 DengueJane LaquihonÎncă nu există evaluări
- 11 Drug StudyDocument11 pagini11 Drug Studygreench08Încă nu există evaluări
- Drugs Affecting Gastrointestinal, Endocrine and Renal SystemsDocument35 paginiDrugs Affecting Gastrointestinal, Endocrine and Renal SystemsJewel Ramos GalinatoÎncă nu există evaluări
- 20.Md Musharraf Ali and V.saikishoreDocument9 pagini20.Md Musharraf Ali and V.saikishoreBaru Chandrasekhar RaoÎncă nu există evaluări