Documente Academic
Documente Profesional
Documente Cultură
Prevalence of Genetic Markers For Trombophilia
Încărcat de
Cojocariu EmanuelTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Prevalence of Genetic Markers For Trombophilia
Încărcat de
Cojocariu EmanuelDrepturi de autor:
Formate disponibile
Human Reproduction Vol.17, No.6 pp.
16331637, 2002
Prevalence of genetic markers for thrombophilia in
recurrent pregnancy loss
Howard Carp1,2,4 Ophira Salomon3, Daniel Seidman1, Rima Dardik3, Nurith Rosenberg3
and Aida Inbal3
1Department of Obstetrics and Gynecology, Sheba Medical Center, Tel Hashomer, 2Department of Embryology, Tel Aviv University
and 3Institute of Thrombosis and Hemostasis, Sheba Medical Center, Tel Hashomer and Sackler Faculty of Medicine, Tel Aviv
University, Israel
4To
whom correspondence should be addressed at: Department of Obstetrics and Gyneology, Sheba Medical Center, Sheba Medical
Center, Tel Hashomer 52621, Israel. E-mail: carp@netvision.net.il
BACKGROUND: The genetic predispositions to venous thrombosis such as factor V Leiden (FVL) mutation (Arg
506 Gln), prothrombin (FII) gene mutation (G20210A), and mutation of the methylenetetrahydrofolate reductase
(MTHFR) gene (C677T) have been reported to be associated with recurrent pregnancy loss. This paper examines
the prevalence of markers for genetic thrombophilias in women with recurrent miscarriage. METHODS: The
prevalence of FVL, FII G20210A and MTHFR C677T was compared in 108 women with three or more pregnancy
losses either exclusively in the first trimester, or mixed first and second trimester losses, with the prevalence found
in 82 fertile parous control women without miscarriages. Markers for the thrombophilias were assessed by PCR
analysis. RESULTS: Twenty-three of the 108 patients (21.3%), had thrombophilia markers, which was similar to
the proportion of patients in the control group (20.7%) with these markers. The prevalences of FVL and FII
G20210A were lower in the study group than in the control group (3.7 versus 6.1% for FVL and 4.6 versus 6.1%
for FII respectively); however, the difference was not statistically significant. In contrast, the prevalence of MTHFR
C677T was higher in the study group than the control population (13 versus 8.5% respectively), but this difference
was not statistically significant. There was no statistically significant prevalence of any particular thrombophilia in
patients with previous first and second trimester pregnancy losses compared with patients with first trimester losses
alone. CONCLUSION: Thrombophilia was not found to be associated with recurrent pregnancy loss.
Key words: habitual abortion/recurrent pregnancy loss/thrombophilia
Introduction
Recurrent miscarriage is usually defined as the loss of three
or more consecutive pregnancies prior to 20 or even 28 weeks
of pregnancy (Salat-Baroux, 1988; Crosignani and Rubin,
1991). However, within this definition is a large and heterogeneous group of patients with many different causes of
miscarriage. Thrombosis in decidual vessels is believed to be
one such cause, leading to intrauterine growth retardation,
fetal death, and possibly recurrent miscarriage. Pregnancy
itself is a hypercoagulable state associated with increased
levels of procoagulant factors (Stirling et al., 1984) and
decreased levels of naturally occurring anticoagulants such as
protein S (Comp et al., 1986). Prothrombotic antibodies such
as lupus anticoagulant and anticardiolipin antibodies have
been suggested as aetiological agents leading to pregnancy
loss (De Wolf et al., 1982). Recently, it has been reported that
genetic tendencies to thrombosis (hereditary thrombophilias)
may also be associated with late pregnancy loss (Preston et al.,
1996; Rai et al., 1996; Grandone et al., 1997; Martinelli
et al., 2000).
European Society of Human Reproduction and Embryology
The three most common genetic thrombophilias known to
predispose to venous thrombosis are: factor V Leiden (FVL),
methylenetetrahydrofolate reductase mutation (MTHFR,
C677T) (Arruda et al., 1997; Nelen et al., 1998) and prothrombin gene mutation (FII, G20210) (Poort et al., 1996). In
FVL, arginine is substituted by glutamine at amino acid residue
506 in coagulation factor V (Bertina et al., 1994). Due to this
substitution, factor Va becomes resistant to degradation by
activated protein C, increasing the risk of venous thromboembolism 35-fold in heterozygous individuals (Dahlback,
1995). In FII G20210A, a G to A transition at position 20210
of the 3 untranslated region of the factor II gene, has been
found to be associated with increased prothrombin levels and
a 3-fold increased risk for venous thrombosis in heterozygotes
(Poort et al., 1996). The homozygous state for the C to T
transition at position 677 of MTHFR gene, is associated
with hyperhomocysteinaemia which predisposes to thrombosis
(Arruda et al., 1996; Guttormsen et al., 1996).
Several studies have reported an association between FVL
and late pregnancy loss (Preston et al., 1996; Grandone et al.,
1633
H.Carp et al.
1997; Martinelli et al., 2000). However, the role of FVL in
early pregnancy loss is unclear. It was reported that there is
no increased prevalence of FVL, FII G20210A and MTHFR
C677T in recurrent early pregnancy loss (Kutteh et al., 1999).
Hence, the relationship between thrombophilia and recurrent
miscarriage is unclear. However, the presumed relationship
between thrombophilia and recurrent pregnancy loss has
become sufficient to allow the presence of thrombophilas to
be an indication for treatment with anticoagulant drugs (Younis
et al., 1997).
The above-quoted papers refer to the pregnancy loss rate
in the presence of thrombophilias. As it is conceivable that
thrombophilias were diagnosed in these series due to
thromboembolic phenomena, we considered it necessary to
assess the prevalence of thrombophilias in patients with
recurrent miscarriage and no previous thromboembolic
phenomena. In the present study, we assessed the prevalence
of the above thrombophilia markers in a cohort of women
with unselected recurrent pregnancy loss as a whole, and
separately for first and second trimester abortions, as well as
whether the patients were primary, secondary or tertiary
aborters (primary aborters are women with no previous live
births, secondary if there was a live birth followed by miscarriages). We also classified a third group of patients whom
we have termed tertiary aborters (Carp, 1994). They had
miscarriages followed by a live birth and at least three
subsequent miscarriages. The results were compared with those
of a control group of fertile parous women.
Materials and methods
Patients
The study was performed in 108 women out of 169 patients presented
to our service with recurrent miscarriage from 1997 to 2000. The
other 61 women were lost to follow-up. The clinical features of
each patient and her miscarriages were recorded, paying particular
attention to whether the previous miscarriages occurred in the first
or second trimesters (fetal death between 13 and 26 weeks), and
whether the patients had a previous live birth. The diagnosis of
trimester of fetal death was made according to the last menstruation,
after confirmation by ultrasound scanning. Patients were excluded
from this study if there was a previous history of thrombosis,
pregnancy at the time of investigation, or if using oral contraceptives.
Patients were only included after other presumptive aetiological
factors were found to be normal: karyotype of both parents,
glucose tolerance test, toxoplasmosis serology, hysterosalpingogram, thereby excluding anatomical abnormalities, intrauterine
adhesions and cervical incompetence, thyroid function, serum
prolactin levels, normal luteal phase of 12 days and plasma
progesterone 24.8 ng/ml, absence of antinuclear factor, or antiphospholipid antibodies.
The control group consisted of 82 women with no miscarriages
who were matched for ethnic origin. Fifty-three of the 82 women
had two or more children, whereas 29 women had one child. The
Human Investigation Review Board of the Sheba Medical Center
approved the study. Each patient was required to sign an informed
consent form prior to enrolment in the study.
Laboratory testing
DNA was extracted from EDTA-anticoagulant blood samples using
standard methods (Miller et al., 1988). FVL was detected by PCR
1634
amplification of a 267 bp fragment and MnII digestion, as previously
described (Salomon et al., 1999). The C677T substitution in the
MTHFR gene was identified using Hinfl cleavage of a 198 bp PCRamplified product (Frosst et al., 1995). For identification of the
G20210A substitution in the factor II gene, a slight modification of
a published method (Poort et al., 1996) was used. A 253 bp fragment
of the 3 untranslated region of the gene was amplified by PCR using
the same primers as described (Salomon et al., 1999) and digested
simultaneously with HindIII and MspI. The A20210 and G20210
alleles were discernible by this procedure since the A20210 allele
bears a restriction site for both enzymes, whereas the G20210
allele bears restriction site only for MspI.
Statistical analysis
Univariate odds ratios (OR) and 95% CI were estimated separately
for each polymorphism. The prevalence of each polymorphism was
compared between patients and controls with the use of the twotailed Fishers exact test. P 0.05 was taken to be statistically
significant.
Results
The median age of the study group was lower than that of the
control group (median 31, range 2342 versus median 36,
range 2155 respectively). The study group was not different
from the control group with respect to ethnic origin; 53% of
the study group were of EuropeanAmerican origin; 41% were
of AsianAfrican origin, and 6% were of mixed origin. The
corresponding figures in the control group were 54, 40 and
6% respectively. The 108 patients in the study group had 440
previous pregnancy losses (mean: 4.07 1.75). Twenty-three
(21.3%) were diagnosed as having at least one thrombophilia
marker, whereas 85 (78.7%) had no thrombophilia (Table I).
None of the study or control group was homozygous for FVL
or FII G20210A mutations. The prevalence of each of the
thrombophilias assessed in comparison with the control population is shown in Table I. There was no statistically significant
difference in the prevalences of either FVL or FII G20210A
between study and control groups, although both were more
common in the controls. The prevalence of homozygous
MTHFR 677T was higher in the study group, but the difference
did not reach statistical significance.
The 22 patients with thrombophilia and 86 patients without
thrombophilia were matched for age and number of pregnancy
losses (Table II). Of the entire study group of 108 women, 55
were primary aborters, whereas 53 were secondary or tertiary
aborters. Among the 22 women with thrombophilia, 14 were
primary aborters (64%) whereas eight were secondary or
tertiary aborters (36%). Of the 55 patients who were primary
aborters, 14 had thrombophilia (25.5%) compared with eight
of 53 who were secondary and tertiary aborters (15.1%);
however, the difference was not statistically significant.
Ten of the 22 women with thrombophilia (45%) had only
experienced first trimester miscarriages, whereas 12 had also
experienced second trimester abortions (55%). In total, 70 of the
108 patients had first trimester miscarriages alone, compared
with 38 who also had second trimester losses. All the second
trimester losses were fetal deaths. There were no abortions of
live fetuses in this series, nor premature ruptures of the
Thrombophilia and recurrent miscarriage
Table I. Prevalence of thrombophilia polymorphisms in women with recurrent pregnancy loss and controls
Factor V Leiden
FII G20210A
MTHFR 677Ta
Total
Recurrent pregnancy
loss (n 108)
Controls
(n 82)
Odds ratio
95% CI
4/108
5/108
14/108
23/108
5/82
5/82
7/82
17/82
NS
NS
NS
NS
0.6
0.7
1.59
1.03
0.122.64
0.173.10
0.564.63
0.482.22
(3.7)
(4.6)
(12.9)
(21.3)
(6.1)
(6.1)
(8.5)
(20.7)
Values in parentheses are percentages.
One patient had a combination of MTHFR 677T and factor V Leiden.
aRefers to the homozygous state.
CI confidence interval; NS not significant.
Table II. Details of patients with and without thrombophilia in the study
group
No. patients
Age
Median
Range
No. of abortions
Mean SD
Range
Thrombophilia
No thrombophilia
All patients
22
86
108
30
2339
31
2342
4.27 1.2
311
31
2342
4.02 1.87
316
4.07 1.75
316
Table III. Prevalence of thrombophilia according to trimester of pregnancy
loss
Factor V Leiden
FII G20210A
MTHFR 677Ta
Total
1st trimester
1st and 2nd trimestera
2/70
2/70
7/70
10/70
2/38
3/38
7/38
12/38
NS
NS
NS
0.03
(2.86)
(2.86)
(10)
(14.3)
(5.3)
(7.9)
(18.4)
(31.6)
Numbers refer to the number of patients with thrombophilia as a proportion
of the total number of patients. Values in parentheses are percentages.
One patient had a combination of MTHFR 677T and factor V Leiden.
aPatients with both first and second trimester losses.
membranes. When the patients with first trimester miscarriages
and those with first and second trimester losses were analysed
separately, 14.3% of women with first trimester miscarriages
were found to have thrombophilia compared with 31.6% of
women with first and second trimester losses (Table III). The
small number of patients with each particular thrombophilia
precluded the numbers from reaching statistical significance
for each particular thrombophilia. However, when the results
were pooled, this difference reached statistical significance
(P 0.03).
Discussion
In this series of 108 patients, 22 (20.3%) were found to have
hereditary thrombophilia. This prevalence was not higher than
that found in the control fertile, parous population. In addition,
there was no statistically significant prevalence of any
particular thrombophilia in patients with previous second
trimester pregnancy losses compared with patients with first
trimester losses alone. When the results of all three markers
for thrombophilia were pooled, there was a significantly higher
prevalence of thrombophilia in patients with at least one
second trimester loss (31.6%) compared with the prevalence
in patients with only first trimester abortions (14.3%). However,
the number of patients with second trimester losses was
relatively small.
These results show that the hereditary thrombophilias studied
seem to be associated with second trimester rather than first
trimester miscarriages. The association of thrombophilia with
second trimester losses rather than first trimester losses
concurs with most of the reports in the literature (Preston
et al., 1996; Rai et al., 1996; Grandone et al., 1997;
Martinelli et al., 2000). There are few reports associating
hereditary thrombophilias with first as well as second trimester
miscarriages (Brenner et al., 1997; Tal et al., 1999; Younis
et al., 2000). In contrast, a recent large series (Rai et al., 2001)
found that the prevalence of FVL was not higher than in
controls for both first and second trimester abortions. Analysis
of the literature with regard to recurrent pregnancy loss shows
a conflicting picture: one study (Kutteh et al., 1999) did not
find a higher prevalence than the general population when
FVL, FII G20210A and MTHFR C677T were assessed, neither
did another study (Dizon-Townson et al., 1997) when assessing
FVL. However, FVL was found in significantly more patients
than in the control population (Brenner et al., 1997). This
discrepancy may stem from the different study design.
As thrombophilias are genetic mutations, they should be
absolute causes of pregnancy loss. Although in the present
study the patients with no live births (primary aborters) had a
higher prevalence of thrombophilia, this difference was not
statistically significant. Additionally, the eight patients with
thrombophilias and previous live births (secondary and tertiary
aborters) had 14 previous deliveries without treatment. This
represents a prior 16.7% live birth rate, indicating that genetic
thrombophilias are not absolute causes of miscarriage. This
live birth rate is similar to that in patients presenting without
thrombophilia (23.5%). Therefore, if thrombosis associated
with thrombophilias leads to pregnancy loss, it is necessary to
determine which patients will have pregnancy loss, and which
will have live births. In the case of antiphospholipid syndrome,
which is also presumed to cause pregnancy loss by thrombosis,
Wilson et al. have defined the pregnancy loss as being either
three or more pregnancy losses prior to the tenth week or one
1635
H.Carp et al.
or more fetal deaths after 10 weeks (Wilson et al., 1999).
However, a typical clinical presentation has been described
(Lockshin et al., 1992). Pregnancies start normally, and a fetal
heart is detected early in the first trimester. Fetal growth slows
in mid pregnancy, oligohydramnios becomes apparent and
fetal death eventually ensues. A high incidence of second and
third trimester losses with antiphospholipid antibodies has also
been reported (Carp et al., 1993).
In the case of first trimester miscarriages, there is a significant
confounding factor. A large number of recurrent first trimester
miscarriages may be lost due to chromosomal aberrations in
the fetus. The incidence has been reported to vary between 29
and 60% (Stern et al., 1996; Ogasawara et al., 2000; Carp
et al., 2001). In one series (Carp et al., 2001), chromosome
16 trisomy and triploidy were relatively common in first
trimester losses. These aberrations will invariably cause
abortion, irrespective of the presence of thrombophilia.
Unfortunately, few centres karyotype the abortus, although
fetal karyotyping is an official recommendation of the Royal
College of Obstetricians and Gynaecologists (1998). Another
confounding factor is the role of lymphokine-activated natural
killer cells, which have also been associated with recurrent
miscarriage (Aoki et al., 1995; Coulam and Beaman, 1995;
Kwak et al., 1995; Clifford et al., 1999). It is conceivable that
if the karyotypically abnormal losses and the patients with
increased natural killer cell activity could have been excluded
from this series, there may have been a different prevalence
in cases of early pregnancy losses. The figures may also have
been skewed by our centre being a tertiary referral centre for
patients with pregnancy loss. Selection bias might have
occurred as primary care physicians may have diagnosed and
treated thrombophilia after two pregnancy losses, (particularly
if these were late losses). These patients might not have been
referred to our service, leaving us with only the patients
with large numbers of first trimester miscarriages and no
thrombophilias. It appears that further studies are necessary
on a larger cohort of patients with acquired as well as hereditary
thrombophilias. Patients losing genetically aberrant embryos
should be excluded from studies that purport to study mechanisms causing fetal demise of normal embryos due to thrombosis
of decidual blood vessels. Until then, thrombophilias will
remain genetic tendencies to thrombosis, not necessarily causes
of early pregnancy loss.
References
Aoki, K., Kajiura, S., Matsumoto, Y., Ogasawara, M., Okada, S., Yagami, Y.
and Gleicher, N. (1995) Preconceptional natural-killer-cell activity as a
predictor of miscarriage. Lancet, 345, 13401342.
Arruda, V.R., Von zuben, P.M., Chiapurini, L.C., Annichino-Bizzachi, J.M.
and Costa, F.F. (1997) The mutation Ala677-Val in the methylene
tetrahydrofolate reductase gene: a risk factor for arterial disease and venous
thrombosis. Thromb. Haem., 77, 818821.
Bertina, R.M., Koelaman, B.P., Koster, T., Rosendaal, F.R., Dirven, R.J., de
Ronde, H.E.T., van der Velden, P.A. and Reitsma, P.H. (1994) Mutation in
the blood coagulation factor V associated with resistance to activated
protein C. Nature, 369, 6467.
Brenner, B., Mandel, H., Lanir, N., Younis, J., Rothbart, H., Ohel, G. and
Blumenfeld, Z. (1997) Activated protein C resistance can be associated
with recurrent fetal loss. Br. J. Hematol., 97, 551554.
1636
Carp, H.J.A. (1994) Abstracts of contributors individual data submitted to the
worldwide prospective observation study on immunotherapy for treatment of
recurrent spontaneous abortion. Am. J. Reprod. Immunol., 32, 261274.
Carp, H.J.A., Menashe, Y., Frenkel, Y., Many, A., Nebel, L., Toder, V., Serr,
D.M. and Mashiach, S. (1993) Lupus anticoagulant: significance in first
trimester habitual abortion. J. Reprod. Med., 38, 549552.
Carp, H.J.A., Toder, V., Orgad, S., Aviram, A., Danieli, M., Mashiach, S. and
Barkai, G. (2001) Karyotype of the Abortus in Recurrent Miscarriage.
Fertil. Steril., 5, 678682.
Clifford, K., Flanagan, A.M. and Regan, L. (1999) Endometrial CD56
natural killer cells in women with recurrent miscarriage: a histomorphometric
study. Hum. Reprod., 14, 27272730.
Comp, P.C., Thurnau, G.R., Welsh, J. and Esmon, C.T. (1986) Functional and
immunologic protein S levels are decreased during pregnancy. Blood, 68,
881885.
Coulam, C.B. and Beaman, K.D. (1995) Reciprocal alteration in circulating
TJ6 CD19 and TJ6 CD56 leukocytes in early pregnancy predicts
success or miscarriage. Am. J. Reprod. Immunol., 34, 219224.
Crosignani, P.C. and Rubin, B.L. (1991) Recurrent spontaneous miscarriage.
The recommendations of the ESHRE workshop on recurrent spontaneous
miscarriage held in Anacapri on September 911, 1990. Hum. Reprod., 6,
609610.
Dahlback, B. (1995) New molecular insights into the genetics of thrombophilia:
resistance to activated protein C caused by Arg506 to Gln mutation in
factor V as pathogenetic risk factor for venous thrombosis. Thromb.
Haemost., 74, 139148.
De Wolf, F., Carreras, L.O., Moerman, P., Vermylen, J., Van Assche, A. and
Renaer, M. (1982) Decidual vasculopathy and extensive placental infarction
in a patient with repeated thromboembolic accidents, recurrent fetal loss,
and a lupus anticoagulant. Am. J. Obstet. Gynecol., 142, 829834.
Dizon-Townson, D.S., Kinney, S., Branch, D.W. and Wand, K. (1997) The
factor V Leiden mutation is not a common cause of recurrent miscarriage.
J. Reprod. Immunol., 34, 21723.
Frosst, P., Blom, H.J., Milos, R., Goyette, P., Sheppard, C.A., Matthews, R.G.,
Boers, G.J., den Heijer, M., Kluijtmans, L.A., van den Heuvel, L.P. and
Rozen, R. (1995) A candidate genetic risk factor for vascular disease: a
common mutation in methylenetetrahydrofolate reductase. Nat. Genet., 10,
111113.
Grandone, E., Margaglione, M., Colaizzo, D., DAddedda, M., Cappucci, G.,
Vecchione, G., Scianname, N., Pavone, G. and Di Minno, G. (1997) Factor
V Leiden is associated with repeated and recurrent unexplained fetal losses.
Thromb. Haemost., 77, 822824.
Guttormsen, A.D., Ueland, P.M., Nesthus, I., Nygard, O., Schneede, J. and
Vollset, S.E. (1996) Determinants and vitamin responsiveness of immediate
hyperhomocysteinemia (40 mols/liter), J. Clin. Invest., 98, 21742183.
Kutteh, W.H., Park, V.M. and Deitcher, S.R. (1999) Hypercoagulable state
mutation analysis in white patients with early first-trimester recurrent
pregnancy loss. Fertil. Steril., 71, 10481054.
Kwak, J.Y., Beaman, K.D., Gilman-Sachs, A., Ruiz, J.E., Schewitz, D. and
Beer, A.E. (1995) Up-regulated expression of CD56, CD56/CD16,
and CD19 cells in peripheral blood lymphocytes in pregnant women with
recurrent pregnancy losses. Am. J. Reprod. Immunol., 34, 9399.
Lockshin, M.D. (1992) Antiphospholipid antibody syndrome. J. Am. Med.
Assoc., 268, 14511453.
Martinelli, I., Taioli, E., Cetin, I., Marinoni, A., Gerosa, S., Villa, M.V.,
Bozzo, M. and Mannucci, P.M. (2000) Mutations in coagulation factors in
women with unexplained late fetal loss. N. Engl. J. Med., 343, 10151018.
Miller, S.A., Dykes, D.D. and Polesky, H.F. (1988) A simple salting out
procedure of extracting DNA from human nucleated cells. Nucl. Acid Res.,
16, 12151217.
Nelen, W.L., Blom, H.J., Thomas, C.M., Steegers, E.A., Boers, C.H. and
Eskes, T.K. (1998) Methylenetetrahydrofolate reductase polymorphism
affects the change in homocysteine and folate concentrations resulting from
low dose folic acid supplementation in women with unexplained recurrent
miscarriages. J. Nutr., 128, 133641.
Ogasawara, M., Aoki, K., Okada, S. and Suzumori, K. (2000) Embryonic
karyotype of abortuses in relation to the number of previous miscarriages.
Fertil. Steril., 73, 300304.
Poort, S.R., Rosendahl, F.R., Reissma, P.H. and Bertina, R.M. (1996). A
common genetic variation in the 3-untranslated region of the prothrombin
gene is associated with elevated plasma prothrombin levels, and an increase
in venous thrombosis. Blood, 88, 36983703
Preston, F.E., Rosendaal, F.R., Walker, I.D., Briot, E., Berntorp, E., Conard, J.,
Fontcuberta, J., Makris, M., Mariani, G., Noteboom, W. et al. (1996)
Thrombophilia and recurrent miscarriage
Increased fetal loss in women with heritable thrombophilia. Lancet, 348,
913916.
Rai, R., Regan, L., Hadley, E., Dave, M. and Cohen, H. (1996) Secondtrimester pregnancy loss is associated with activated C resistance. Br. J.
Haematol., 92, 489490.
Rai, R., Shlebak, A., Cohen, H., Backos, M., Holmes, Z., Marriott, K. and
Regan, L. (2001) Factor V Leiden and acquired activated protein C
resistance among 1000 women with recurrent miscarriage. Hum. Reprod.,
16, 961965.
Royal College of Obstetricians and Gynaecologists (1998) Guideline No. 17.
The Management of Recurrent Miscarriage. RCOG, London.
Salat-Baroux, J. (1988) Recurrent spontaneous miscarriages. Reprod. Nutr.
Dev., 28, 15551568.
Salomon, O., Steinberg, D.M., Zivelin, A., Gitel, S., Dardik, R., Rosenberg,
N., Berliner, S., Inbal, A., Many, A., Lubetsky, A. et al. (1999) Single
and combined prothrombothic factors in patients with idiopathic venous
thromboembolism. Arterioscler. Thromb. Vasc. Biol., 19, 511518.
Stern, J.J., Dorfman, A.D. and Gutierez-Najar, M.D. (1996) Frequency of
abnormal karyotype among abortuses from women with and without a
history of recurrent spontaneous abortion. Fertil. Steril., 65, 250253.
Stirling, Y., Woolf, L., North, W.R., Seghatchian, M.J. and Meade, T.W.
(1984) Haemostasis in normal pregnancy. Thromb. Haem., 52, 176182.
Tal, J., Schliamser, L.M., Leibovitz, Z., Ohel, G. and Attias, D. (1999) A
possible role for activated protein C resistance in patients with first and
second trimester pregnancy failure. Hum. Reprod., 14, 16241627.
Wilson, W.A., Gharavi, A.E., Koike, T., Lockshin, M.D., Ware Branch, D.,
Piete, J.C., Brey, R., Derksen, R., Harris, E.N., Hughes, G.R. et al. (1999)
International concensus statement on preliminary classification criteria for
definite antiphospholipid syndrome. Arth. Rheum., 42, 13091311.
Younis, J.S., Ohel, G., Brenner, B. and Ben-Ami, M. (1997). Familial
thrombophilia|the scientific rationale for thrombophylaxis in recurrent
pregnancy loss. Hum. Reprod., 12, 13891390.
Younis, J.S., Brenner, B., Ohel, G., Tal, J., Lanir, N. and Ben-Ami, M. (2000)
Activated protein C resistance and factor V Leiden mutation can be
associated with first|as well as second|trimester recurrent pregnancy loss.
Am. J. Reprod. Immunol., 43, 3135.
Submitted on July 9, 2001; resubmitted on September 9, 2001; accepted on
December 6, 2001
1637
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Crane Workbox 4398Document4 paginiCrane Workbox 4398hazopman100% (1)
- Marchand 2012Document20 paginiMarchand 2012Elton MatsushimaÎncă nu există evaluări
- Ifosfamide Nephrotoxicity - UpToDateDocument7 paginiIfosfamide Nephrotoxicity - UpToDateZurya UdayanaÎncă nu există evaluări
- Proforma Curriculum VitaeDocument4 paginiProforma Curriculum VitaeSohail IqbalÎncă nu există evaluări
- Women Devlopment-Government Policies and ProgrammesDocument19 paginiWomen Devlopment-Government Policies and ProgrammesVishalMishraÎncă nu există evaluări
- Presentation of Neurogenic Shock Within The Emergency Department - TaylorDocument6 paginiPresentation of Neurogenic Shock Within The Emergency Department - TaylorAnprtma kaunangÎncă nu există evaluări
- Tetanus - AnatomyDocument7 paginiTetanus - AnatomyJoro27Încă nu există evaluări
- 2022 Projects City of BethlehemDocument17 pagini2022 Projects City of BethlehemLVNewsdotcomÎncă nu există evaluări
- F17 Reflection 383 FN - 15 Nov 17Document7 paginiF17 Reflection 383 FN - 15 Nov 17jigsawÎncă nu există evaluări
- Safety Inspection Checklist Project: Location: Inspector: DateDocument2 paginiSafety Inspection Checklist Project: Location: Inspector: Dateyono DaryonoÎncă nu există evaluări
- Aldomet: (Methyldopa)Document6 paginiAldomet: (Methyldopa)Riska AuliahÎncă nu există evaluări
- National Health Policy in India: Dr. Kanupriya ChaturvediDocument38 paginiNational Health Policy in India: Dr. Kanupriya ChaturvediRadhakrishnan TherivilaÎncă nu există evaluări
- Craniofacial SyndromesDocument101 paginiCraniofacial SyndromesSaranya MohanÎncă nu există evaluări
- Intentional InjuriesDocument30 paginiIntentional InjuriesZyryx BartolomeÎncă nu există evaluări
- Potsdam Village Police Dept. Blotter Sept. 10, 2017Document2 paginiPotsdam Village Police Dept. Blotter Sept. 10, 2017NewzjunkyÎncă nu există evaluări
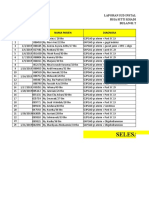
- Laporan Iud 2019Document91 paginiLaporan Iud 2019Yuli AntiÎncă nu există evaluări
- The Myths and Truths About Transcendental MeditationDocument11 paginiThe Myths and Truths About Transcendental MeditationMeditation Fix100% (2)
- Hafiz Fizalia - Acupuncture Hack - The Easiest Way To Learn Classical Theories of Acupuncture (2018) PDFDocument66 paginiHafiz Fizalia - Acupuncture Hack - The Easiest Way To Learn Classical Theories of Acupuncture (2018) PDFkhalid Sijilmassi100% (3)
- About The Author-James Herriot: A Triumph of Surgery Chapter - 1 Footprint Without FeetDocument4 paginiAbout The Author-James Herriot: A Triumph of Surgery Chapter - 1 Footprint Without FeetSunil rathi100% (3)
- Health and Welfare Committee ReportDocument4 paginiHealth and Welfare Committee ReporttncircuitriderÎncă nu există evaluări
- LK 1 Modul 1 ProfesionalDocument2 paginiLK 1 Modul 1 ProfesionalKadek indrawan100% (1)
- Review of The Health Benefits of Peas (Pisum Sativum L.) : Wendy J. Dahl, Lauren M. Foster and Robert T. TylerDocument8 paginiReview of The Health Benefits of Peas (Pisum Sativum L.) : Wendy J. Dahl, Lauren M. Foster and Robert T. TylerCrystal Joan D. MedranoÎncă nu există evaluări
- 8. 학생 핸드북 (영문)Document33 pagini8. 학생 핸드북 (영문)Eylül GülcemalÎncă nu există evaluări
- Groupwork Proposal BSW 3705 June 2022Document17 paginiGroupwork Proposal BSW 3705 June 2022Mtshali Nthuseng100% (1)
- NCP For PostpartumDocument1 paginăNCP For PostpartumMary Hope BacutaÎncă nu există evaluări
- Concurrent Visit Report 7-12Document14 paginiConcurrent Visit Report 7-12Tizita ChakaÎncă nu există evaluări
- Development of A Taste-Masked Orodispersible FilmDocument12 paginiDevelopment of A Taste-Masked Orodispersible FilmKhoa DuyÎncă nu există evaluări
- Chapter 6 QuestionsDocument2 paginiChapter 6 QuestionsGabo DanteÎncă nu există evaluări
- MSDS PDFDocument5 paginiMSDS PDFdang2172014Încă nu există evaluări
- MarriottDocument4 paginiMarriottSheikh Farhan AliÎncă nu există evaluări