Documente Academic
Documente Profesional
Documente Cultură
CH 08
Încărcat de
savyasachinTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
CH 08
Încărcat de
savyasachinDrepturi de autor:
Formate disponibile
8
The Larynx:
Advanced Stage Disease
JOHN F. CAREW, MD
Of the 295,000 cases of cancer of the head and neck
accrued by the National Cancer Data Base over a 10year period, larynx was the most common site
accounting for more than 20 percent of all head and
neck cancers.1 Squamous cell carcinoma which arises
from the mucosa lining the larynx accounted for over
90 percent of all cancers in this site.2 In one of the
larger studies of patients with larynx cancer, 40 percent of patients presented with advanced stage disease
(stage III or IV).2 Despite the use of aggressive multimodality treatment in patients with advanced stage
cancer of the larynx, overall survival for these patients
ranges from 42 to 77 percent.214 As mentioned in the
section on early stage disease, other neoplasms such
as lymphomas, minor salivary gland tumors, mucosal
melanomas and sarcomas may affect this site,
although large series evaluating these specific
pathologies at this site are lacking in the literature.
Unless otherwise specified, squamous cell carcinomas of the larynx will be the subject of this chapter.
The larynx performs several unique and vital
functions related to phonation, breathing and swallowing, and the treatment of patients with neoplasms
of this organ requires consideration of these critical
functions. Specifically, the impact of therapeutic
options on both the extent as well as the quality of
life needs to be taken into account. As this section
focuses on advanced cancer of the larynx, most
treatment options involve multimodality therapy in
the form of either chemotherapy and radiation therapy or surgery and radiation therapy. The critical
decision, which continues to evolve, is selecting the
appropriate treatment for each individual patient.
156
Additionally, the optimal treatment plan which combines chemotherapy and radiation therapy with
regards to timing (sequential vs. concomitant), radiation fractionation, chemotherapeutic agents and
adjuvants remains undefined. In this section, the
diagnosis, treatment and outcome of patients with
advanced cancer of the larynx will be presented.
ANATOMY
While the basic anatomy of the larynx already has
been described in the section on early larynx cancer,
this section will highlight the critical points relevant
to treating patients with advanced cancers of the larynx. The majority of larynx cancers are found in the
glottic region (56%) followed by the supraglottic
region (41%), while tumors of the subglottic region
are relatively infrequent (1 to 2%) (Figure 81).2,15 It
is important to realize that tumors in these different
regions of the larynx have different clinical behaviors. Supraglottic tumors, for example, have a much
higher rate of occult and bilateral metastasis than
glottic primaries.10,16 The regional lymph nodes of
the neck in patients with advanced stage supraglottic tumors and clinically negative necks must therefore be addressed in treatment planning.
The connective tissue barriers which lie between
the mucosa and cartilaginous skeleton of the larynx,
namely the conus elasticus and quadrangular membrane, are critical to the understanding of patterns of
spread and clinical behavior of advanced cancers of
the larynx (Figure 82). These membranes provide a
barrier to the spread of cancer but are often breached
The Larynx:Advanced Stage Disease
Supraglottic
41%
Glottic
56%
Subglottic
3%
Figure 81.
Site distribution of larynx cancers.
by advanced tumors (Figure 83).17 Once a tumor
has broken through these boundaries, it can spread
into the soft tissues of the neck as well as vertically
within the larynx.
Two regions that are deep to the quadrangular
membrane and conus elasticus are the preepiglottic
and paraglottic space. Advanced tumors often enter
these spaces when they transgress these connective
tissue barriers within the larynx and thus enter a
compartment where further spread is less hindered.
The preepiglottic space is bounded by the thyrohyoid membrane anteriorly, the valleculae superiorly,
the epiglottis posteriorly and the hyoid inferiorly.
This space is commonly involved by local spread of
supraglottic tumors. Once this space is involved, a
supraglottic tumor is staged as a T3.18 Tumors
157
involving this area can then spread into the soft tissues of the neck via the foramen in the thyrohyoid
membrane or inferiorly via the paraglottic space. In
some patients, however, a connective tissue barrier
separates the preepiglottic and paraglottic space.19
The paraglottic space is the compartment which
is bounded by the thyroid lamina laterally, the
conus elasticus medially-inferiorly and the quadrangular membrane and preepiglottic space medially-superiorly. Loose connective tissue and adipose tissue lying between thyroid lamina and the
connective tissue membranes of the larynx occupy
this space. This area is most commonly involved by
advanced glottic tumors. Once this compartment is
entered, tumors can spread relatively freely in a
superior and inferior direction, as well as outside
the confines of the larynx via the cricothyroid
membrane or the preepiglottic space. Involvement
of this space frequently results in decreased vocal
fold movement.
Cancers of the larynx can be classified as
advanced (stage III or IV) either by virtue of an
advanced primary tumor or by the presence of
regional lymph node metastasis. When regional
lymph node metastases are present they are
described by their location, number and size. The
location of the lymph nodes is described by levels in
the neck as illustrated in the chapter on neck metastasis. Levels II, III and IV are at highest risk for
lymph node metastasis from cancers in the larynx.
Figure 82. A, Sagittal section of larynx demonstrating the preepiglottic and B, coronal section of larynx
demonstrating the paraglottic space.
158
CANCER OF THE HEAD AND NECK
Diagnosis
Patients with advanced glottic cancers will present
with symptoms similar to patients with early glottic
cancers. As listed earlier these include hoarseness or
a change in the quality of voice, odynophagia, halitosis or otalgia. Not suprisingly the more ominous
symptoms, such as hemoptysis, dysphagia, airway
compromise and neck mass are more common in
advanced stage disease. Additionally, the supraglottic
and subglottic lesions tend to be less symptomatic
and their insidious growth results in a high percent of
patients presenting with advanced stage disease.
As mentioned earlier, adequate examination of
the larynx by use of the laryngeal mirror or a rigid
telescope or fiberoptic flexible nasopharyngoscope
is essential to staging and treatment planning (Figure 84).20 Critical in this evaluation is assessment
of the epicenter of the tumor, vocal fold mobility,
extra-laryngeal involvement and regional lymph
nodes in the neck. Although early tumors are often
adequately assessed by history and physical exam
alone, appropriate evaluation of advanced lesions
usually requires radiographic imaging to ascertain
the depth of the tumor involvement, preepiglottic
space extension, paraglottic extension, cartilage
involvement and extra-laryngeal spread. High-resolution CT scans with thin cuts through the larynx
usually give adequate information regarding these
aspects (Figure 85).21 Additionally, in patients with
necks which are difficult to assess clinically, radiographic evaluation may add information in establishing the regional lymph node status.
The staging of patients with advanced cancers of
the larynx is outlined in Table 81.18 As with other
sites in the head and neck, the complex anatomy in
this region makes accurate staging challenging. At
times, the location of the lesion appears to carry
more weight than the tumor burden. For example, a
relatively small tumor on the posterior aspect of the
larynx which involves the post-cricoid area will be
stage T3, while a bulky tumor replacing the
aryepiglottic fold, epiglottis and spilling down the
medial wall of the pyriform sinus will be staged a T2
as long as the vocal cord remains mobile. While survival has been related to both T stage and N stage, it
B
Figure 83. Whole organ sections showing tumor involving the
preepiglottic and paraglottic space.
The Larynx:Advanced Stage Disease
is most profoundly affected by the nodal status of the
patient.2,10,11 It has long been known that regional
lymph node involvement in head and neck cancer
patients decreases survival by approximately 50 percent.10,11 The present staging system of the American
Joint Committee for Cancer (AJCC) groups both
patients with locally advanced tumors (T3N0) and
patients with regional lymph node metastasis (T1-
159
3N1) together into stage III.18 This may arbitrarily
group 2 subsets of patients together who have vastly
different prognoses. Both the stage as well as the
nodal status must thus be considered when interpreting results from the treatment of larynx cancer.
Just as there are ominous symptoms in patients
with advanced cancer of the larynx, there are also
several physical findings that are harbingers of clin-
D
Figure 84. Endoscopic view and assessment of a laryngeal cancer using the A-0; B-30; C-70; D-120 telescopes.
160
CANCER OF THE HEAD AND NECK
A
Figure 85. A, Axial CT of advanced laryngeal primary tumor
demonstrating paraglottic involvement and cartilage destruction but
without extension into the soft tissues of the neck. B, Axial CT of
advanced laryngeal primary tumor demonstrating cartilage destruction and extension into the soft tissues of the neck.
ically aggressive behavior. Extensive spread into the
soft tissues of the neck, involvement of the overlying
skin, regional lymph node metastases which are
fixed or limited in vertical mobility, and bulky disease low in the neck all suggest a poor prognosis.
Treatment Goals and Treatment
AlternativesThe Role
of Multidisciplinary Treatment
In the last 2 decades, 5-year survival of patients with
laryngeal cancer has not changed dramatically.22
Maximizing survival, therefore, continues to be the
ultimate goal in treating patients with advanced
stage larynx cancer. Recently, however, due to the
lack of improvement in survival, significant efforts
have been made to improve the quality of life in
these patients. Paramount to this is preservation of a
functional larynx. Toward this goal, treatment
options have been formulated with the hopes of
increasing laryngeal preservation without sacrificing survival. Multimodality treatment paradigms, in
the form of chemotherapy, radiotherapy and surgical
salvage, has emerged as a viable treatment option
allowing anatomical preservation of the larynx without decreasing survival.3 Now that a method of
laryngeal preservation has been established, future
goals in treatment are directed at increasing both the
rate of laryngeal preservation and survival.
Factors Affecting Choice of Treatment
Factors affecting choice of treatment can be divided
into patient factors and tumor factors. As demonstrated in multiple clinical trials, survival is statistically equivalent in selected patients with advanced
cancer of the larynx who are treated with either
chemotherapy and radiation therapy or surgery and
radiation therapy.3,6,7,9,2325 Given this, patients who
wish to utilize a treatment paradigm that may preserve their larynx, such as chemotherapy and radiation therapy, should be given this nonsurgical option.
Alternatively, there is a cohort of patients who are of
the mindset that they would rather have all cancer
removed and would prefer surgery and radiation therapy, understanding that their ability to communicate
will be significantly affected. Finally, any patient
who is considering chemotherapy and radiation therapy as a treatment option must be reliable and must
enroll a multidisciplinary team experienced in treating patients with advanced cancer of the larynx.
Many tumor factors also contribute to the decision process in determining the optimal treatment
for each patient. If a tumor or lymph node metasta-
The Larynx:Advanced Stage Disease
sis shows ominous clinical signs suggesting unresectability, then certainly a surgical option should
not be contemplated and consideration given to
chemotherapy and radiation therapy.26,27 A clinical
situation which is interesting but infrequent arises
when a patient presents with an early stage primary
lesion and clinically apparent regional lymph node
metastasis. In this situation several treatment options
exist. If the primary lesion is best treated by radia-
Table 8-1. AJCC STAGING OF CARCINOMA OF THE LARYNX
Supraglottis
T1: Tumor limited to one subsite of the supraglottis with normal
vocal cord mobility
T2: Tumor invades mucosa of more than one adjacent subsite
of the supraglottis or glottis or region outside the supraglottis (eg, mucosa of the base of tongue, valleculae, medial
wall of pyriform sinus) without fixation of the larynx
T3: Tumor limited to the larynx with vocal cord fixation and/or
invades any of the following: postcricoid area, preepiglottic
tissues
T4: Tumor invades through the thyroid cartilage, and/or extends
into the soft tissues of the neck, thyroid and/or esophagus
Glottis
T1: Tumor limited to the vocal cord(s) (may involve anterior or
posterior commissure) with normal vocal cord mobility
T1A: Tumor limited to one vocal cord
T1B: Tumor involves both vocal cords
T2: Tumor extends to the supraglottis and/or subglottis, and/or
with impaired vocal cord mobility
T3: Tumor limited to the larynx with vocal cord fixation
T4: Tumor invades through the thyroid cartilage and/or extends
to other tissues beyond the larynx (eg, trachea, soft tissues
of the neck, including thyroid, pharynx)
Subglottis
T1: Tumor limited to the subglottis
T2: Tumor extends to the vocal cord(s) with normal or impaired
mobility
T3: Tumor limited to the larynx with vocal cord fixation
T4: Tumor invades through the cricoid or thyroid cartilage
and/or extends to other tissues beyond the larynx (eg, trachea, soft tissues of the neck, including thyroid, esophagus)
Neck
N0: No regional lymph node metastasis
N1: Ipsilateral lymph node metastasis 3 cm
N2: Lymph node metastasis in a single ipsilateral lymph node
> 3 cm and 6 cm, or in multiple lymph nodes none more
than 6 cm (including bilateral nodal metastasis)
N2A: Lymph node metastasis in single ipsilateral lymph
node > 3 cm and 6 cm
N2B: Lymph node metastasis in multiple ipsilateral lymph
nodes all 6 cm
N2C: Lymph node metastasis in bilateral or contralateral
lymph nodes all 6 cm
N3: Lymph node metastasis > 6 cm
161
tion therapy, one could consider a comprehensive
neck dissection followed by radiation therapy to the
primary site and the neck. Alternatively, if the primary lesion is best treated by a surgical approach,
one could consider a partial laryngectomy and neck
dissection with the addition of adjuvant radiation
therapy as indicated based on pathologic findings.
Of the most important factors in deciding the
optimal treatment are the characteristics of the primary tumor. Tumors which are endophytic, show
extensive cartilage invasion, involve the soft tissues
of the neck, or involve the airway to such an extent
that a tracheostomy is required, often demonstrate
aggressive clinical behavior and respond poorly to
treatment. Whether these patients fare better in a
surgical treatment arm as opposed to a nonsurgical
plan has yet to be substantiated in a randomized
prospective trial. The ideal treatment in these
patients, therefore, remains controversial. In such
patients, aggressive early surgical intervention will
improve the chances for locoregional control and
thus improve the quality of life that would otherwise
be significantly deteriorated with persistent or recurrent disease. Early aggressive surgical intervention
may not improve survival or risk of distant metastasis, but would certainly offer avoidance of airway
obstruction, asphyxiation or intractable pain.
Surgical Treatment
In the majority of patients with advanced primary
tumors of the larynx, the surgical treatment consists
of a total laryngectomy. It should be remembered,
however, that partial laryngectomy and conservational surgical procedures which preserve the function of the larynx may be options in selected
patients. As discussed in the section on early larynx
cancer, vertical partial, supraglottic partial and
supracricoid partial laryngectomies can be performed in carefully selected patients. In patients
with advanced lesions, however, the more extensive
partial laryngectomies are utilized more frequently
and even more selectively. These procedures,
although categorized in broad terms such as neartotal laryngectomy or supracricoid partial laryngectomy with cricohyoidopexy, are usually individually
designed to adequately encompass each patients
162
CANCER OF THE HEAD AND NECK
particular tumor while sparing as much functional
tissue as oncologically feasible (Figure 86).2831
Appropriate management of the neck is critical
to maximizing survival in patients with advanced
cancer of the larynx. The treatment of the neck
depends in part on the treatment of the primary. If
the primary is to be treated by surgical means, then
an elective dissection of the lymph nodes at risk
should be planned in the clinically negative neck.
For a glottic lesion, the ipsilateral levels II to IV
should be cleared, while for a supraglottic lesion,
bilateral levels II to IV are at risk and should be dissected. If there is clinically apparent lymph node
metastasis in the neck and the primary is to be
treated by surgery, then a comprehensive neck dissection (levels I to V) should be performed.
B
Figure 86. Schematic diagram of two well-described voice-preserving, extended laryngeal procedures: A, supracricoid laryngectomy with cricohyoidoepiglottopexy and B, supracricoid laryngectomy with cricohyoidopexy (dotted lines represent line of surgical excision).
The Larynx:Advanced Stage Disease
Alternatively, if a patient with a clinically negative
neck is to be treated by chemotherapy and radiation
therapy to the primary lesion, the neck at risk should
also be treated electively by radiation therapy. A
somewhat more controversial situation exists if there
is a clinically positive neck and the primary is to be
treated by chemotherapy and radiation therapy. The
options that exist include performing a comprehensive neck dissection prior to chemotherapy/radiation
therapy, performing a planned comprehensive or
selective neck dissection after chemotherapy/
radiation therapy or assessing response following
chemotherapy/radiation therapy and performing
appropriate neck dissection based on response. At
this time, data is lacking to substantiate an advantage
in any of these approaches and all are acceptable.
Nonsurgical Treatment
The appreciation of the psychosocial consequences
of total laryngectomy has been the impetus for the
development of treatment options which could preserve the larynx of patients with advanced stage larynx cancer. In the early 1990s, a prospective, randomized trial of patients treated at Veterans Affairs
Hospitals with stage III and stage IV squamous cell
carcinoma of the larynx, comparing conventional
treatment of surgery and postoperative radiotherapy,
with induction chemotherapy followed by radiotherapy was performed.3 In this study, patients in the
chemotherapy-radiation therapy (chemo/RT) arm
who did not display at least a 50 percent response to
induction chemotherapy, or who showed persistent
or recurrent disease following radiation, were salvaged with surgery. This landmark study demonstrated survivals which were not statistically different between treatment arms (68%), and allowed 64
percent of patients within chemo/RT arms to preserve their larynx.3 With the results of the Veterans
Affairs Larynx Cancer Study Group (VALCSG)
trial, the combination of induction chemotherapy
and radiation therapy has emerged as a treatment
option which allows preservation of the larynx in
nearly two-thirds of patients. Since this trial, many
other studies have been performed to confirm
chemo/RT as an effective treatment for patients with
advanced larynx cancer.6,7,9,2325,32
163
Sequelae, Complications and
their Management
Surgery and Radiotherapy
The complications associated with total laryngectomy can be divided into acute and chronic. The
acute complications include those related to surgery
and general anesthesia. These include bleeding,
infection, pneumonia and fistula. The most troublesome of these is the pharyngocutaneous fistula. The
fistula rate following total laryngectomy remains
relatively high, ranging from 8 to 22 percent.3335
Appropriate treatment of a pharyngocutaneous fistula requires early recognition and then wide opening of the wound with appropriate wound care. The
patient should stop all oral intake and an alternative
route of alimentation should be established. If significant carotid exposure is seen, then consideration
should be given to coverage with a regional flap to
afford carotid protection, especially in the setting of
previous radiation therapy. Often the fistula will
close spontaneously with aggressive wound care. In
those cases where it does not, local, regional and
even free flaps may be used to obtain closure.
The most common chronic complication of total
laryngectomy is stricture formation with dysphagia. It
is crucial to rule out recurrent tumor whenever a
patient develops new dysphagia or worsening dysphagia. This is usually best evaluated by endoscopy
with direct visualization of the mucosa of the
neopharynx. Preoperative esophagrams are often
helpful in defining the location and extent of stricture.
If a stricture is seen, it can usually be dilated, although
repeated treatments are often required. Ultimately, if
a stricture is unresponsive to these conservative measures, consideration can be given to free tissue transfer to reconstruct an adequate neopharynx.
The early sequelae of radiation therapy relate primarily to the acute tissue reactions with characteristic skin changes and mucositis. These are managed
symptomatically with oral hygiene and topical medications. The late sequelae of radiation therapy
include skin changes, xerostomia and, very rarely,
chondroradionecrosis of the laryngeal skeleton.
Xerostomia is treated symptomatically with oral
hygiene and humidification. In severe cases where
chondroradionecrosis profoundly impairs swallow-
164
CANCER OF THE HEAD AND NECK
ing and breathing, a total laryngectomy may need to
be performed to restore the ability to swallow.
Chemotherapy and Radiotherapy
Treatment protocols using chemo/RT to preserve
organ function have successfully demonstrated their
ability to anatomically preserve the larynx without
compromising survival. One aspect of these protocols that is often underappreciated is the functional
capacity of the retained organs. Few investigators
have clearly documented the functional sequelae of
chemotherapy and radiation therapy. Recently,
Lazarus retrospectively studied patients being
treated with chemotherapy and radiation therapy and
found that 40 percent had swallowing difficulties.36
Clinical evidence of disorders in the pharyngeal
phase of swallowing has been demonstrated in
patients who have undergone chemotherapy and
radiation therapy for tumors of the upper aerodigestive tract. Specifically, reduced laryngeal closure,
reduced laryngeal elevation and reduced posterior
tongue base movement relative to age-matched controls has been documented.36 Certainly, patients who
successfully undergo chemo/RT treatments to preserve their larynx have a much improved quality of
life relative to patients requiring total laryngectomy.37 Nevertheless, it should be realized that
anatomic preservation does not always result in
functional preservation. Very rarely, total laryngectomy is performed in order to restore the ability to
swallow when a larynx is incompetent and nonfunctional but clinically free of cancer.
In addition to functional sequelae, chemotherapy
(specifically when given in combination with radiation therapy) has some definite toxicities. Toxicity
from induction chemotherapy has prevented 7 to 18
percent of patients from receiving a full course of
chemotherapy.3,4,6,8 Even mortality, as a result of
chemotherapy and radiation-related toxicity, has
been reported to range from 0.6 to 6 percent.3,59,25
Rehabilitation and Quality of Life
In the past, conventional treatment of advanced stage
laryngeal cancer consisted of surgery and postoperative external beam radiation. Surgical resection of the
majority of advanced stage laryngeal lesions con-
sisted of total laryngectomy with the resultant deleterious effects on deglutition, phonation and the creation of a permanent tracheostoma. The psychosocial
consequences of total laryngectomy have been well
studied.14,3739 Not suprisingly, quality of life measurements and psychosocial indicators are significantly affected by total laryngectomy. Although techniques for voice rehabilitation have improved, studies
have shown that the psychosocial effects of laryngectomy are as much related to loss of voice as they
are to other factors such as the necessity of a permanent tracheostoma.14,38,39 When the patients treated in
the Veterans Affairs Laryngeal Cancer Study Group
were evaluated, an improved long-term quality of life
was seen in the cohort who were randomized to
chemotherapy and radiation therapy compared to
those treated by surgery and radiation therapy.37
Interestingly, this difference was primarily related to
freedom from pain, better emotional well-being and
lower levels of depression rather than the preservation of the ability to speak.
Nevertheless, several methods are available to
rehabilitate the ability of a patient to communicate
following total laryngectomy. Many patients are able
to acquire esophageal speech, in which air is swallowed and then used to create a voice. Approximately 2 decades ago a significant advance in the
rehabilitation of patients with laryngectomies took
place when the tracheoesophageal puncture was
developed.40 This is a relatively minor procedure
where a fistula is created between the trachea and
esophagus (Figure 87). A prosthesis with a oneway valve is placed into this fistula, which allows
the creation of a lung powered voice. In the motivated patient, this voice can be quite good.
Outcomes and Results of Treatment
Historically, surgery in the form of total laryngectomy
followed by adjuvant postoperative radiation therapy
has been the standard treatment for most patients with
advanced stage cancer of the larynx.1012,41,42 Additionally, selected patients with advanced stage larynx
cancer have been treated with definitive radiation
therapy alone.13,42,43 The results of these treatments
are summarized in Table 82 with 5-year survival
ranging from 54 to 91 percent.1013,4143
The Larynx:Advanced Stage Disease
Figure 87.
Schematic diagram of tracheoesophageal puncture (TEP).
More recently, chemotherapy/radiation therapy
has evolved as an effective treatment for advanced
stage cancer of the larynx. A summary of results
from the various studies evaluating chemo/RT in the
treatment of patients with advanced stage laryngeal
cancer, with the goal of larynx preservation, are
listed in chronologic order in Table 83.39,25 In all
but one study, more than 90 percent of patients evaluated had stage III or IV disease. Most studies
included only those patients who would have
required a total laryngectomy if treated by conventional means with surgery and postoperative radiotherapy. Treatment results for patients treated with
chemo/RT in these studies are fairly consistent with
2-year survival ranging from 50 to 77 percent, lar-
Table 82. RESULTS OF CONVENTIONAL TREATMENT
OF ADVANCED CARCINOMA OF THE LARYNX
Author
12
Kirchner
Harwood13
Harwood43
Yuen41
Year
No.
Type of
Therapy
1977
1979
1983
1984
308
353
410
192
50
100
65
116
65
S/RT
RT
RT
S
S/RT
RT
SRT
S/RT
SRT
Mendenhall42 1992
Nguyen11
Myers10
1996
1996
165
5 yr
Stage
Survival
III/IV (%)
(%)
100
54
66
100
100
100
100
100
100
5456*
70
57
77
91
74
63
68
62
Survival rates refer to disease-free survival when available, otherwise they
refer to overall survival.
* study included both laryngeal and non-laryngeal sites.
S = Surgery; RT = Radiation therapy; 2-year survival.
ynx preservation rates ranging from 64 to 79 percent, locoregional failure rates ranging from 20 to
33 percent and distant failure rates ranging from 8 to
21 percent.39,25 It should be noted, however, that
only one of these studies was limited only to patients
with laryngeal primaries,3 while the remainder of
the studies included patients with hypopharynx,
oropharynx, oral cavity and even paranasal sinuses
as sites of primary tumors.49,25 The majority of
these studies that included non-laryngeal sites did so
because surgical treatment of the primary would
have required total laryngectomy. The data presented
Table 83. RESULTS OF TREATMENT OF ADVANCED
CARCINOMA OF THE LARYNX UTILIZING
CHEMOTHERAPY AND RADIATION THERAPY
2 yr.
Type of
Stage
Survival
Therapy III/IV (%)
(%)
Author
Year
No.
Jacobs4
Demard5
1987
1990
30
50
C/RT
C/RT
100
64
Veterans Affairs
Larynx Group3
Pfister6
Karp7
Urba8
Clayman9
(includes data
from Shirinian)25
1991
166
166
13
14
8
26
52
C/RT
S/RT
C/RT
C/RT
C/RT
C/RT
S/RT
100
100
98
92
93
96
96
1991
1991
1994
1995
52*
74*
(Response
rate)
68
68*
77*
50*
75*
68*
81*
Survival rates refer to disease-free survival when available, otherwise they
refer to overall survival.
* Study included both laryngeal and non-laryngeal sites. C = chemotheapy;
S = surgery; RT = radiation therapy.
166
CANCER OF THE HEAD AND NECK
in this table refers, whenever possible, to the subset
of patients with laryngeal primaries, although this
information was not always available.
In several of these aforementioned studies, single
modality therapy in the form of definitive radiotherapy was utilized and yielded disease-specific survivals similar to those seen with the combination of
induction chemotherapy and radiation therapy.39,13,25,42,43 Although the selected cohort of
patients who received radiation therapy alone had
less stage IV and node-positive patients, the contribution of chemotherapy to these larynx preservation
protocols remains undetermined. While previous
randomized prospective trials have not included a
radiation therapy-only arm, an ongoing prospective
randomized trial has included a radiation therapyonly arm, to address this question. This phase III trial
has 3 treatment arms including: (1) radiotherapy
alone, (2) sequential chemotherapy and radiotherapy
and (3) concomitant chemotherapy and radiotherapy.
Data from this study will help to further define the
optimal treatment for patients with advanced larynx
cancer. Additionally, 2 studies have recently been
published which compared radiotherapy alone to
concurrent chemotherapy (cisplatin/5-fluorouracil)
and radiotherapy in patients with locoregionallyadvanced squamous cell carcinoma of the head and
neck.44,45 In these studies, between 36 and 56 percent
of patients had either laryngeal or hypopharyngeal
primaries. In both studies, a statistically significant
increase in 3-year relapse-free survival was seen in
the concurrent chemo/RT arm as compared to the
RT-alone arm (p < 0.00444 and p < 0.0345).
The debate also continues regarding the optimal
fractionation of radiation therapy, chemotherapeutic
agents, and optimal timing of chemotherapy and
radiation therapy (sequential vs. concomitant). Protocols with accelerated fractionation of radiotherapy
and plans using concomitant chemotherapy and
radiotherapy have been investigated. It has been postulated that part of the cause of increased locoregional failures seen with chemo/RT protocols result
from an accelerated tumor cell repopulation during
the prolonged course of treatment.46,47 Clinical and
experimental evidence suggest that tumor cell populations, after a lag period of several weeks, will
decrease their doubling time and increase their rate
of regrowth after the commencement of cytotoxic
treatment, regardless of whether it is chemotherapy
or radiation therapy.46,47 A longer treatment time will
therefore result in high rates of failure.48
In order to minimize these problems, investigators
have evaluated accelerated radiotherapy regimens and
concomitant chemo/RT protocols. In the past, accelerated (twice a day) courses of radiation therapy have
improved 3-year local control of advanced laryngeal
tumors (T3-4) from 26 to 59 percent (p < 0.0001).48,49
These gains in local control are not accomplished
without cost with regards to treatment related morbidity. In this study, although the larynx was anatomically preserved, its function was profoundly impaired
in a subset of patients, and significant long-term treatment related morbidity was seen in one-quarter of
patients. Additionally, all patients in this series undergoing salvage surgery after radiotherapy experienced
major wound complications.50 Ultimately a benefit in
local or regional control or survival was not seen,
although the power of this study was limited.
Another method of shortening treatment time,
decreasing the effects of accelerated tumor cell
repopulation and improving results involves the use
of concomitant chemotherapy and radiation therapy.
Prior studies using concomitant chemotherapy and
radiation in advanced stage head and neck cancer
have shown promising results with regard to locoregional control, organ preservation and survival.51,52
Prospective randomized trials assessing the benefit
of concomitant chemotherapy and radiation therapy
as it applies to advanced stage laryngeal cancer,
however, are limited. As mentioned earlier, a randomized prospective trial comparing sequential to
concomitant chemotherapy and radiation therapy is
currently underway.
Additionally, randomized prospective studies
comparing sequential chemotherapy and radiation
therapy to concomitant chemo/RT in patients with
unresectable tumors of the head and neck have been
reported.27,53 While an improvement in locoregional
control was seen in the concomitant arm in the larger
study,53 neither study showed a difference in overall
survival.27,53 At this time, neither accelerated fraction
radiation therapy nor concomitant chemo/RT have
conclusively demonstrated a benefit in treating
advanced stage laryngeal cancer relative to induc-
The Larynx:Advanced Stage Disease
tion chemotherapy followed by conventional fraction radiation therapy. For this reason, along with the
potential for treatment related morbidity, it remains
investigational at this time.
Finally, novel treatment strategies continue to
evolve which intend to further improve the survival
and functional outcome in patients with advanced
cancer of the larynx. One such unique strategy utilizes the high-dose intra-arterial cisplatin with a systemic neutralizing agent along with conventional
radiation therapy.54 In this study, where the majority
of patients had stage IV disease (86%) and clinically
involved regional lymph nodes (79%), a major
response rate was seen in 95 percent of patients. Nine
of 10 patients retained their larynx and 2-year disease-specific survival was 76 percent. It should be
noted that 3 of the 42 patients experienced central
nervous system complications as a result of catheritization of the carotid system. Nevertheless, this
remains a promising option and a novel approach in
the treatment of advanced laryngeal cancer.
5.
6.
7.
8.
9.
10.
11.
CONCLUSION
The treatment of patients with advanced cancers of
the larynx has changed dramatically over the last 2
decades. While anatomic preservation of the larynx
can now be achieved in a large fraction of patients,
overall survival remains unchanged. The continued
optimization of multimodality treatment paradigms
along with the incorporation of biological markers,
novel treatment approaches, novel chemotherapeutic
agents and innovative biologic and gene transfer
techniques will hopefully further increase our ability
to improve survival in these patients.
12.
13.
14.
15.
16.
REFERENCES
17.
1. Hoffman HT, Karnell LH, Funk GF, et al. The National Cancer Data Base report on cancer of the head and neck. Arch
Otolaryngol Head Neck Surg 1998;124(9):95162.
2. Shah JP, Karnell LH, Hoffman HT, et al. Patterns of care for
cancer of the larynx in the United States. Arch Otolaryngol Head Neck Surg 1997;123(5):47583.
3. Induction chemotherapy plus radiation compared with
surgery plus radiation in patients with advanced laryngeal
cancer. The Department of Veterans Affairs Laryngeal
Cancer Study Group [see comments]. N Engl J Med
1991;324(24):168590.
4. Jacobs C, Goffinet DR, Goffinet L, et al. Chemotherapy as a
18.
19.
20.
21.
167
substitute for surgery in the treatment of advanced
resectable head and neck cancer. A report from the Northern California Oncology Group. Cancer 1987;60(6):
117883.
Demard F, Chauvel P, Santini J, et al. Response to
chemotherapy as justification for modification of the
therapeutic strategy for pharyngolaryngeal carcinomas.
Head Neck 1990;12(3):22531.
Pfister DG, Strong E, Harrison L, et al. Larynx preservation
with combined chemotherapy and radiation therapy in
advanced but resectable head and neck cancer. J Clin
Oncol 1991;9(5):8509.
Karp DD, Vaughan CW, Carter R, et al. Larynx preservation
using induction chemotherapy plus radiation therapy as
an alternative to laryngectomy in advanced head and neck
cancer. A long-term follow-up report. Am J Clin Oncol
1991;14(4):2739.
Urba SG, Forastiere AA, Wolf GT, et al. Intensive induction
chemotherapy and radiation for organ preservation in
patients with advanced resectable head and neck carcinoma. J Clin Oncol 1994;12(5):94653.
Clayman GL, Weber RS, Guillamondegui O, et al. Laryngeal
preservation for advanced laryngeal and hypopharyngeal
cancers. Arch Otolaryngol Head Neck Surg 1995;121(2):
21923.
Myers EN, Alvi A. Management of carcinoma of the supraglottic larynx: evolution, current concepts, and future
trends. Laryngoscope 1996;106(5 Pt 1):55967.
Nguyen TD, Malissard L, Theobald S, et al. Advanced carcinoma of the larynx: results of surgery and radiotherapy
without induction chemotherapy (19801985): a multivariate analysis. Int J Radiat Oncol Biol Phys 1996;36(5):
10138.
Kirchner JA, Owen JR. Five hundred cancers of the larynx
and pyriform sinus. Results of treatment by radiation and
surgery. Laryngoscope 1977;87(8):1288303.
Harwood AR, Hawkins NV, Beale FA, et al. Management of
advanced glottic cancer. A 10-year review of the Toronto
experience. Int J Radiat Oncol Biol Phys 1979;5(6):
899904.
Harwood AR, Rawlinson E. The quality of life of patients following treatment for laryngeal cancer. Int J Radiat Oncol
Biol Phys 1983;9(3):3358.
Dahm JD, Sessions DG, Paniello RC, Harvey J. Primary subglottic cancer. Laryngoscope 1998;108(5):7416.
Levendag P, Sessions R, Vikram B, et al. The problem of neck
relapse in early stage supraglottic larynx cancer. Cancer
1989;63(2):3458.
Meyer-Breiting E, Burkhardt A. Tumours of the larynx:
Histopathology and clinical inferences. New York (NY):
Springer-Verlag; 1988.
Oliver H. Beahrs OH. Manual for staging of cancer/ American Joint Commission on Cancer. Philadelphia (PA): JB
Lippincott Co; 1997.
Reidenbach MM. The paraglottic space and transglottic cancer:
anatomical considerations. Clin Anat 1996;9(4):24451.
Cummings CW, Fredrickson JM, Harker LA, et al. Otolaryngologyhead & neck surgery: St. Louis (MO): MosbyYear Book, Inc.; 1998.
Som PM, Curtin HD. Head and neck imaging. St. Louis
(MO): Mosby-Year Book, Inc.; 1996.
168
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
CANCER OF THE HEAD AND NECK
Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics,
1999 [see comments]. CA Cancer J Clin 1999;49(1):
831, 1.
Pfister D, Armstrong J, Strong E, et al. A matched pair analysis of cisplatin/5-fluorouracil versus other cisplatin based
regimens as induction chemotherapy for larynx preservation treatment. Proceedings of the American Society of
Clinical Oncology 1993;12:280.
Pfister D, Harrison L, Kraus D, et al. Larynx preservation:
does induction cisplatin based chemotherapy compromise
the delivery of concomitant chemotherapy with radiation
therapy. Proceedings of the American Society of Clinical
Oncology 1994;13:292.
Shirinian MH, Weber RS, Lippman SM, et al. Laryngeal
preservation by induction chemotherapy plus radiotherapy in locally advanced head and neck cancer: the M. D.
Anderson Cancer Center experience. Head Neck 1994;
16(1):3944.
Harrison LB, Raben A, Pfister DG, et al. A prospective phase
II trial of concomitant chemotherapy and radiotherapy with
delayed accelerated fractionation in unresectable tumors of
the head and neck. Head Neck 1998;20(6):497503.
Pinnaro P, Cercato MC, Giannarelli D, et al. A randomized
phase II study comparing sequential versus simultaneous
chemo-radiotherapy in patients with unresectable locally
advanced squamous cell cancer of the head and neck. Ann
Oncol 1994;5(6):5139.
Laccourreye H, Laccourreye O, Weinstein G, et al.
Supracricoid laryngectomy with cricohyoidopexy: a partial
laryngeal procedure for selected supraglottic and transglottic carcinomas. Laryngoscope 1990;100(7):73541.
Laccourreye H, Menard M, Fabre A, et al. [Partial supracricoid
laryngectomy. Techniques, indications and results]. Ann
Otolaryngol Chir Cervicofac 1987;104(3):16373.
Laccourreye O, Salzer SJ, Brasnu D, et al. Glottic carcinoma
with a fixed true vocal cord: outcomes after neoadjuvant
chemotherapy and supracricoid partial laryngectomy with
cricohyoidoepiglottopexy. Otolaryngol Head Neck Surg
1996;114(3):4006.
Pearson BW. Subtotal laryngectomy. Laryngoscope 1981;
91(11):190412.
Clark JR, Busse PM, Norris CM Jr, et al. Induction chemotherapy with cisplatin, fluorouracil, and high-dose leucovorin
for squamous cell carcinoma of the head and neck: longterm results. J Clin Oncol 1997;15(9):310010.
Soylu L, Kiroglu M, Aydogan B, et al. Pharyngocutaneous fistula following laryngectomy. Head Neck 1998;20(1):225.
Shemen LJ, Spiro RH. Complications following laryngectomy. Head Neck Surg 1986;8(3):18591.
Parikh SR, Irish JC, Curran AJ, et al. Pharyngocutaneous fistulae in laryngectomy patients: the Toronto Hospital experience. J Otolaryngol 1998;27(3):13640.
Lazarus CL, Logemann JA, Pauloski BR, et al. Swallowing
disorders in head and neck cancer patients treated with
radiotherapy and adjuvant chemotherapy. Laryngoscope
1996;106(9 Pt 1):115766.
Terrell JE, Fisher SG, Wolf GT. Long-term quality of life
after treatment of laryngeal cancer. The Veterans Affairs
Laryngeal Cancer Study Group. Arch Otolaryngol Head
Neck Surg 1998;124(9):96471.
Maas A. A model for quality of life after laryngectomy. Soc
Sci Med 1991;33(12):13737.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
DeSanto LW, Olsen KD, Perry WC, et al. Quality of life after
surgical treatment of cancer of the larynx. Ann Otol Rhinol Laryngol 1995;104(10 Pt 1):7639.
Singer MI. Blom ED. Tracheoesophageal puncture: A surgical prosthetic method for post laryngectomy speech
restoration. Third International Symposium on Plastic
Reconstructive Surgery of the Head and Neck, 1979.
Yuen A, Medina JE, Goepfert H, Fletcher G. Management of
stage T3 and T4 glottic carcinomas. Am J Surg 1984;
148(4):46772.
Mendenhall WM, Parsons JT, Stringer SP, et al. Stage T3
squamous cell carcinoma of the glottic larynx: a comparison of laryngectomy and irradiation. Int J Radiat Oncol
Biol Phys 1992;23(4):72532.
Harwood AR, Beale FA, Cummings BJ, et al. Supraglottic
laryngeal carcinoma: an analysis of dose-time-volume
factors in 410 patients. Int J Radiat Oncol Biol Phys
1983;9(3):3119.
Wendt TG, Grabenbauer GG, Rodel CM, et al. Simultaneous
radiochemotherapy versus radiotherapy alone in
advanced head and neck cancer: a randomized multicenter study. J Clin Oncol 1998;16(4):131824.
Adelstein DJ, Saxton JP, Lavertu P, et al. A phase III randomized trial comparing concurrent chemotherapy and
radiotherapy with radiotherapy alone in resectable stage
III and IV squamous cell head and neck cancer: preliminary results. Head Neck 1997;19(7):56775.
Withers HR, Taylor JM, Maciejewski B. The hazard of accelerated tumor clonogen repopulation during radiotherapy.
Acta Oncol 1988;27(2):13146.
Bourhis J, Wilson G, Wibault P, et al. Rapid tumor cell proliferation after induction chemotherapy in oropharyngeal
cancer. Laryngoscope 1994;104(4):46872.
Fowler JF, Lindstrom MJ. Loss of local control with prolongation in radiotherapy. Int J Radiat Oncol Biol Phys
1992;23(2):45767.
Wang CC, Blitzer PH, Suit HD. Twice-a-day radiation therapy for cancer of the head and neck. Cancer 1985;55(9
Suppl):21004.
Eisbruch A, Thornton AF, Urba S, et al. Chemotherapy followed by accelerated fractionated radiation for larynx
preservation in patients with advanced laryngeal cancer. J
Clin Oncol 1996;14(8):232230.
Adelstein DJ, Saxton JP, Van Kirk MA, et al. Continuous
course radiation therapy and concurrent combination
chemotherapy for squamous cell head and neck cancer.
Am J Clin Oncol 1994;17(5):36973.
Glicksman AS, Wanebo HJ, Slotman G, et al. Concurrent
platinum-based chemotherapy and hyperfractionated
radiotherapy with late intensification in advanced head
and neck cancer. Int J Radiat Oncol Biol Phys
1997;39(3):7219.
Taylor SG, Murthy AK, Vannetzel JM, et al. Randomized
comparison of neoadjuvant cisplatin and fluorouracil
infusion followed by radiation versus concomitant treatment in advanced head and neck cancer. J Clin Oncol
1994;12(2):38595.
Robbins KT, Fontanesi J, Wong FS, et al. A novel organ
preservation protocol for advanced carcinoma of the larynx and pharynx. Arch Otolaryngol Head Neck Surg
1996;122(8):8537.
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Radiotherapy in Penile Carcinoma: Dr. Ayush GargDocument32 paginiRadiotherapy in Penile Carcinoma: Dr. Ayush GargMohammad Mahfujur RahmanÎncă nu există evaluări
- Saints and Mahatmas of IndiaDocument290 paginiSaints and Mahatmas of IndiaRajeswari Ranganathan100% (2)
- TNM Classification 8th Edition 2017Document8 paginiTNM Classification 8th Edition 2017Mohammed Mustafa Shaat100% (1)
- Clinical Presentation, Diagnosis, and Staging of Colorectal Cancer - UpToDate PDFDocument41 paginiClinical Presentation, Diagnosis, and Staging of Colorectal Cancer - UpToDate PDFVali MocanuÎncă nu există evaluări
- Sant TukArAm English BiographyDocument16 paginiSant TukArAm English BiographyGanesh RahaneÎncă nu există evaluări
- Part II Color Oral Pathology Picture Booklet (2007-2008) PDFDocument14 paginiPart II Color Oral Pathology Picture Booklet (2007-2008) PDFaerowongÎncă nu există evaluări
- Sant Jarnail Singh Bhindranwale - Life, Mission, and MartyrdomDocument62 paginiSant Jarnail Singh Bhindranwale - Life, Mission, and MartyrdomAmandeep Singh AujlaÎncă nu există evaluări
- TMP 2243-Instructions For Candidates-1462031165Document7 paginiTMP 2243-Instructions For Candidates-1462031165savyasachinÎncă nu există evaluări
- VitaminDocument8 paginiVitamindrusmansaleemÎncă nu există evaluări
- Food Sources of CalciumDocument4 paginiFood Sources of CalciumsavyasachinÎncă nu există evaluări
- Fluorine NMRDocument35 paginiFluorine NMRDrHamadÎncă nu există evaluări
- Uch 015741Document2 paginiUch 015741savyasachinÎncă nu există evaluări
- TMP - 2243-Inst. Advt. No. 02 of 2016 - 12 Posts281220077Document51 paginiTMP - 2243-Inst. Advt. No. 02 of 2016 - 12 Posts281220077savyasachinÎncă nu există evaluări
- TheoreticalExamWithAnswers 2012 PDFDocument50 paginiTheoreticalExamWithAnswers 2012 PDFiugulescu laurentiuÎncă nu există evaluări
- Relevance To Public Health: 2.1 Background and Environmental Exposures To Boron in The United StatesDocument13 paginiRelevance To Public Health: 2.1 Background and Environmental Exposures To Boron in The United StatesKhayrunnisa BMÎncă nu există evaluări
- Essential Mineral Calcium and Its Role in Bone HealthDocument14 paginiEssential Mineral Calcium and Its Role in Bone HealthHabsah Omar MasrunaÎncă nu există evaluări
- ReadMe PDFDocument1 paginăReadMe PDFsavyasachinÎncă nu există evaluări
- Nutfluoride PDFDocument12 paginiNutfluoride PDFsavyasachinÎncă nu există evaluări
- Dragon NaturallySpeaking 11Document71 paginiDragon NaturallySpeaking 11savyasachinÎncă nu există evaluări
- Ppssastri Adiparva Part1Document1.005 paginiPpssastri Adiparva Part1savyasachinÎncă nu există evaluări
- Nut FluorideDocument4 paginiNut FluoridesavyasachinÎncă nu există evaluări
- MGM Dental Coll Navi Mumbai 130214Document2 paginiMGM Dental Coll Navi Mumbai 130214savyasachinÎncă nu există evaluări
- Dragon Naturally Speaking 10Document1 paginăDragon Naturally Speaking 10Norazaliza LizaÎncă nu există evaluări
- ReadMe PDFDocument1 paginăReadMe PDFsavyasachinÎncă nu există evaluări
- Fellowship Revision by Government of IndiaDocument3 paginiFellowship Revision by Government of Indiaatul_saraf001Încă nu există evaluări
- Prospectus Jan2017Document59 paginiProspectus Jan2017savyasachinÎncă nu există evaluări
- AIIMS PG July 2016 ProspectusDocument56 paginiAIIMS PG July 2016 ProspectussavyasachinÎncă nu există evaluări
- ApplicationForm PDFDocument1 paginăApplicationForm PDFsavyasachinÎncă nu există evaluări
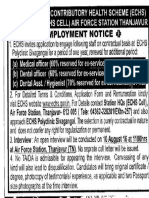
- Ex-Servicemen Contributory Health Scheme (Echs) Jamnagar & Rajkot Employment NoticeDocument1 paginăEx-Servicemen Contributory Health Scheme (Echs) Jamnagar & Rajkot Employment NoticesavyasachinÎncă nu există evaluări
- Adv PcscoimDocument1 paginăAdv PcscoimsavyasachinÎncă nu există evaluări
- Prospectus Jan2017Document59 paginiProspectus Jan2017savyasachinÎncă nu există evaluări
- Ex-Servicemen Contributory Health Scheme (Echs) Jamnagar & Rajkot Employment NoticeDocument1 paginăEx-Servicemen Contributory Health Scheme (Echs) Jamnagar & Rajkot Employment NoticesavyasachinÎncă nu există evaluări
- JRADEDocument2 paginiJRADEsavyasachinÎncă nu există evaluări
- TesticularDocument79 paginiTesticularAndryanto リクア SutantoÎncă nu există evaluări
- SCLCDocument80 paginiSCLCraj patelÎncă nu există evaluări
- 02.TNM 8 - 2017 PDFDocument26 pagini02.TNM 8 - 2017 PDFThiago TinôcoÎncă nu există evaluări
- IVMS Cell Biology and Pathology Flash Facts IDocument4.999 paginiIVMS Cell Biology and Pathology Flash Facts IMarc Imhotep Cray, M.D.0% (2)
- CI-01 - Cancer (Kanser)Document2 paginiCI-01 - Cancer (Kanser)jijiqÎncă nu există evaluări
- 681 FullDocument6 pagini681 FullKurnia AnharÎncă nu există evaluări
- Pathology Outlines - StagingDocument1 paginăPathology Outlines - StagingHarshit ChoudharyÎncă nu există evaluări
- Integumentary System: Anatomy, Functions, and Skin CancerDocument12 paginiIntegumentary System: Anatomy, Functions, and Skin CancerCaereel LopezÎncă nu există evaluări
- Axillary ClearenceDocument9 paginiAxillary ClearencelakanthÎncă nu există evaluări
- Mid QuestionsDocument4 paginiMid QuestionsMAMA LALAÎncă nu există evaluări
- The Satisfaction of Ruqyah On Cancer PatientsDocument5 paginiThe Satisfaction of Ruqyah On Cancer PatientsNinaÎncă nu există evaluări
- Classification and Treatment of Bone TumorsDocument6 paginiClassification and Treatment of Bone TumorsRonald TejoprayitnoÎncă nu există evaluări
- Anees Ahmed Corrected Thesis - RecentDocument135 paginiAnees Ahmed Corrected Thesis - RecentAbdul MunimÎncă nu există evaluări
- NEW AJCC/UICC STAGING SYSTEM FOR HPV-RELATED CANCERSDocument36 paginiNEW AJCC/UICC STAGING SYSTEM FOR HPV-RELATED CANCERSGalgalo GarbichaÎncă nu există evaluări
- Rectal CancerDocument20 paginiRectal CancerSantosh BabuÎncă nu există evaluări
- WJRV 4 I 8Document59 paginiWJRV 4 I 8Wenny EudensiaÎncă nu există evaluări
- Esophageal Cancer - A Review of Epidemiology, Pathogenesis, Staging Workup and Treatment Modalities PDFDocument10 paginiEsophageal Cancer - A Review of Epidemiology, Pathogenesis, Staging Workup and Treatment Modalities PDFLUCIANAÎncă nu există evaluări
- Protocol Update Dec 2019Document13 paginiProtocol Update Dec 2019Aarzu ChoudharyÎncă nu există evaluări
- Children With Cancer PDFDocument92 paginiChildren With Cancer PDFThalani NarasiyaÎncă nu există evaluări
- Clinical Practice Guidelines: Biliary Cancer: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDocument10 paginiClinical Practice Guidelines: Biliary Cancer: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpPutri MauraÎncă nu există evaluări
- Clinico-Radiological Co-Relation of Carcinoma Larynx and Hypopharynx: A Prospective StudyDocument7 paginiClinico-Radiological Co-Relation of Carcinoma Larynx and Hypopharynx: A Prospective StudyDede MarizalÎncă nu există evaluări
- Iota AdnexDocument10 paginiIota Adnexlinh hoàngÎncă nu există evaluări
- New Horizons in The Treatment of Osteosarcoma: Review ArticleDocument11 paginiNew Horizons in The Treatment of Osteosarcoma: Review ArticleRucelia Michiko PiriÎncă nu există evaluări
- Value of Pre-Operative Serum CA125 Level For Prediction of Prognosis in Patients With Endometrial CancerDocument7 paginiValue of Pre-Operative Serum CA125 Level For Prediction of Prognosis in Patients With Endometrial CancerFerdina NidyasariÎncă nu există evaluări
- Au 2003Document7 paginiAu 2003Didi Nurhadi IllianÎncă nu există evaluări
- Enneking Stadializare OS MSKDocument15 paginiEnneking Stadializare OS MSKVlad RakoczyÎncă nu există evaluări
- NCM 119 - Rle (Prelim) Week 1: Immune Response Immunity: Natural and Acquired Immunity - Ma'am VAB Immune ResponseDocument13 paginiNCM 119 - Rle (Prelim) Week 1: Immune Response Immunity: Natural and Acquired Immunity - Ma'am VAB Immune ResponseJamaica Leslie Noveno100% (1)