Documente Academic
Documente Profesional
Documente Cultură
Test Escenas Alzh
Încărcat de
Vicente CáceresDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Test Escenas Alzh
Încărcat de
Vicente CáceresDrepturi de autor:
Formate disponibile
NIH Public Access
Author Manuscript
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
NIH-PA Author Manuscript
Published in final edited form as:
Geriatr Gerontol Int. 2010 April ; 10(2): 183190. doi:10.1111/j.1447-0594.2009.00576.x.
Scenery Picture Memory Test: A new type of quick and effective
screening test to detect early stage Alzheimers disease patients
Hajime Takechi1 and Hiroko H Dodge2,3
1 Department of Geriatric Medicine, Graduate School of Medicine, Kyoto University, Kyoto, Japan
2
Department of Neurology, Oregon Health & Science University, Portland, Oregon
Institute for Social Research, University of Michigan, Ann Arbor, Michigan, USA
Abstract
NIH-PA Author Manuscript
AimIt is highly desirable to develop a neuropsychological screening test which is sensitive to the
early stage of Alzheimers disease (AD), and is easy to administer at the primary care physicians
(PCPs) office.
MethodsParticipants were 128 AD patients and 54 healthy volunteers. Brief cognitive screening
tests were administered to the participants including the Mini-Mental State Examination (MMSE),
Clock Drawing Test (CDT), Verbal Fluency Test (VFT), a Verbal Category Cued Memory test
(CCMT) and the Scenery Picture Memory Test (SPMT). In the SPMT, a scenery picture of a living
room containing 23 familiar objects was used. The administration of the SPMT comprised the first
shallow memory session (Pict 1) and the second deep memory session (Pict 2). The area under the
receiveroperator curve (AUC) was used to compare the efficacy of SPMT with other cognitive tests.
ResultsPict 1, which requires less than 2 min to complete, had the same AUC as Pict 2, and
showed significantly larger AUC than MMSE, CDT and VFT for all (MMSE 1923) and very mild
(MMSE 24) AD patients. When we conducted the similar analysis separately for those younger
than 75 years and those aged 75 years or older, we obtained the same results as above among the
older age group. Pict 1 showed larger AUC than CCMT in overall sample and also in the older age
group, although the difference was not statistically significant.
NIH-PA Author Manuscript
ConclusionThe SPMT could be useful for detection of mild and very mild AD in settings even
where time is limited.
Keywords
dementia; picture superiority; primary care physician; screening test; visual memory
Introduction
As the population ages, the number of those afflicted with AD is expected to increase sharply.
Early detection of AD is important for disease management but it is often difficult to distinguish
early AD from normal cognitive aging. Early diagnosis is a particular challenge in the primary
care setting where there is a lack of time and specialized expertise.13
Correspondence: Dr Hajime Takechi MD PhD, Department of Geriatric Medicine, Graduate School of Medicine, Kyoto University, 54
Shogoin Kawahara-cho, Sakyo-ku, Kyoto 606-8507, Japan. takechi@kuhp.kyoto-u.ac.jp.
Author contributions: H. T. designed the study, collected data and drafted the manuscript; H. D. contributed to data analysis and made
critical revisions to the manuscript.
Takechi and Dodge
Page 2
NIH-PA Author Manuscript
It is generally agreed that those with early AD show memory decline greater than that expected
for their age group.4 Changes in cognitive test performance can be powerful diagnostic tools,
if neuropsychological assessment could be included in the clinical diagnosis of AD. However,
the majority of the familiar cognitive tests are not ideal for detecting early AD; some are too
difficult, even for the healthy elderly (floor effect), while others are too easy for patients with
early AD (ceiling effect). Tests developed to overcome these shortfalls include memory tests
which provide cues during both the encoding and retrieval period,58 and show reasonably
high sensitivity and specificity in distinguishing early AD from normal aging. These tests are,
however, time-consuming and their administration requires expertise not available in all
primary care physician (PCP) offices. Further, older adults are sometimes reluctant to take long
and effortful tests.
NIH-PA Author Manuscript
Visual memory is a key component of everyday life and healthy elderly have a relatively large
capacity for memory for visual information encountered in daily life even without active
conscious effort.912 Because a central feature of AD is the decline in episodic memory,13
several well-established visual memory tests, such as the Benton Visual Retention Test and
the Rey-Osterrieth complex figure, can be used to assess non-verbal memory.14,15 However,
the abstract figures to be encoded and retrieved in these tests do not reflect daily life and both
tests suffer from floor effects among the elderly. The third edition of the Wechsler Memory
Scale (WMS-III) introduced the Family Pictures subtest which was designed to assess recall
for scene characters, character activity and character location. This test uses non-abstract
figures combined with verbal answers.16 However, the test is time-consuming and complex in
scoring, and has been used primarily to study cognition in schizophrenia or temporal epilepsy.
17,18 In the current study, we developed a new type of short and simple memory test assessing
visual memory encoded as scenery, combined with verbal answers, to be used to detect mild
AD.
Methods
Participants
NIH-PA Author Manuscript
The patients in the AD group came from outpatient referrals to the memory clinic of the
Department of Geriatrics in Kyoto University Hospital. All patients underwent brain computed
tomography or magnetic resonance imaging as well as a battery of laboratory tests including
thyroid function, vitamin B12, folate and serum calcium concentration. A diagnosis of AD was
made according to the fourth edition of the Diagnostic and Statistical Manual of Mental
Disorders (DSM-IV) criteria and the National Institute of Neurological and Communicative
Disorders and StrokeAlzheimers Disease and Related Disorders Association (NINCDSADRDA) criteria.19,20 We defined mild and very mild AD according to operational criteria
using Mini-Mental State Examination (MMSE) scores:21 1923, mild; and 24 and over, very
mild. Of the 128 individuals with AD, 44 were classified as mild AD and 84 very mild AD by
this criterion. Those with MMSE scores below 19 were excluded from the current analysis.
Separately, 39 consecutive patients attending the memory clinic were recruited to test
reliability, regardless of dementia diagnosis or subtype; 14 AD patients and three non-AD
patients (two vascular dementia, one Fahr disease) for assessing inter-rater reliability, and 16
AD patients and six non-AD patients (three vascular dementia, one fron-totemporal dementia,
one depression, one delusion) for assessing testretest reliability.
Fifty-four healthy volunteers with a Clinical Dementia Rating (CDR) of 0 were recruited from
two sources: community-dwelling elderly who belonged to the Sakyo Geriatric Welfare Center,
and outpatients in the Department of Geriatrics in Kyoto University Hospital. The inclusion
criteria also included being free from depression, cerebral vascular disease, cerebral vascular
accident or any other psychological disorder. This study was carried out according to the ethical
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 3
guidelines for biomedical research involving human subjects set by Kyoto University, and
written informed consent was obtained.
NIH-PA Author Manuscript
Cognitive assessment
Neuropsychologists administered the Scenery Picture Memory Test (SPMT) as part of a
neuropsychological test battery that included the MMSE, Clock Drawing Test (CDT), Verbal
Fluency Test (VFT) and Verbal Category Cued Memory test (CCMT), independently from the
diagnostic assessments. For the CDT, the subject was asked to draw a clock with all the numbers
on a blank piece of paper and indicate the time as 10 min after 11 oclock. We used the 10point scoring system by Rouleau et al.22 The CCMT, a modified version of Buschkes Double
Memory Test reported previously, is a verbal memory test which contains 16 words from eight
categories and uses category cues during encoding and recall.4,23 In the CCMT, only cued
recall but not free recall is tested. The score is the number of items recalled correctly with the
maximum score being 16.23 In VFT, the subject was instructed to name as many vegetables
and sports as possible, each within 1 min.23 The score was the total number of items mentioned
in both categories.
NIH-PA Author Manuscript
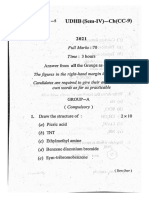
The SPMT used a line drawing scenery picture (Fig. 1) of a living room in a house where 23
objects commonly observed in daily life are drawn on an A4 piece of paper: a telephone, a
bookshelf, books, a table, chairs, two cups with saucers, a flower vase, a framed picture on the
wall, a clock, a ceiling lamp, a couch, a cushion, a cat, a low table, a hat on the table, a briefcase,
a television, a desk for the television, a calendar on the wall, a flower pot with a cactus, a flower
pot with a foliage plant, a table lamp and a window. We collected scores in two ways, which
we call Pict 1 and Pict 2, respectively. In the first trial, Pict 1, the examinee studies the
picture for 1 min and is instructed to remember the items. After this encoding period, we
distracted participants by asking them to conduct a brief digits forward test (four digit strings
consisting of 4, 5, 6 and 7 digits, respectively). Participants were then asked to recall the objects
in the picture without time limitation. This recall time usually takes less than 1 min. The number
of items recalled is the score for Pict 1 with no credit for duplicates.
NIH-PA Author Manuscript
In Pict 2, to enhance the encoding process, following the first trial, Pict 1, we asked participants
to recall the locations of three specific items (telephone, hat and calendar), for example, do
you remember where the telephone was located in the picture? After these questions, we
presented the picture again and asked participants to name the items in the picture. Participants
were asked to name at least 12 items. All participants in the current study could name at least
12 items. These tasks were not scored because our intention was to enhance memory by
encouraging greater depth of processing. After this deep memory processing period,
participants were distracted by the digits forward and backward subtest of the WAIS-R.24
Finally, they were asked again to recall the items in the picture. The number of the items recalled
here was used as the score for Pict 2. The mean approximate administration time of the SPMT
is 2 min for Pict 1 and 6 min overall.
Statistical analyses
All data are presented as mean standard deviation (SD). Students t-tests were used to assess
differences between group means on continuous variables. Pearsons 2-tests were used to
assess differences between groups on categorical variables. To measure the accuracy of the
tests in discriminating between controls and patients, the area under the curve (AUC) of the
receiveroperator curve (ROC) was assessed using the total sample as well as by two age groups
(<75 years vs 75 years). Because controls in this study were younger and had higher education
than AD patients in the total sample, we confirmed the validity of the SPMT in two age groups.
We conducted the ROC analysis first using all AD patients and controls, and second using only
very mild AD patients (AD with MMSE 24) and controls. Inter-rater and testretest
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 4
NIH-PA Author Manuscript
reliabilities were analyzed using the Spearmans rank correlation coefficient. The correlation
between Pict 1 and Pict 2 was examined using Pearsons correlation coefficient. Testretest
and inter-rater reliabilities of SPMT were tested in the separate group of outpatients from a
memory clinic. In this series of tests, two testers participated: one psychologist and one speech
therapist. In both cases, two examinations were carried out at least 1 month apart; the average
duration between test and retest was 2.3 1.5 months, and the duration between inter-rater
examinations was 2.8 2.1 months.
Results
Demographic and basic neuropsychological characteristics of AD patients and controls are
presented in Table 1. In each age group (<75 and 75 years), there was no difference in age
and education distributions between control and AD groups. The SPMT scores in patients and
controls suggest no apparent ceiling and floor effects in either group (Fig. 2).
NIH-PA Author Manuscript
Sensitivity and specificity to detect AD cases by Pict 1 were 85.2% and 88.9% (cut-off 9/10),
respectively, and 84.4% and 90.7% (cut-off 12/13) by Pict 2, respectively. Positive and negative
predictive values were 94.8% and 71.6% by Pict 1, respectively, and 95.6% and 71.0% by Pict
2, respectively. Given the similar levels of sensitivity, the specificity of MMSE and CCMT
were lower than those of the SPMT. Sensitivity and specificity by MMSE were 83.6% and
75.9% (cut-off 27/28), respectively, and 81.3% and 81.5% (cut-off 7/8) by CCMT,
respectively. These results were almost the same for very mild AD cases (data not shown).
Table 2 shows AUC of different tests. Among the total sample, the AUC of Pict 1 was
significantly larger than those of MMSE, CDT and VFT. Among the younger age group (<75
years), the AUC of Pict 1 was significantly larger than those of CDT and VFT. Among the
older age group (75 years), the AUC of Pict 1 was significantly larger than those of MMSE,
CDR and VFT. The AUC of Pict 1 and Pict 2 were very similar among the total sample (Table
2, Fig. 3) as well as within each age group (Table 2). Pict 1 showed a larger AUC than CCMT
in the overall sample and also in the older age group, although the difference was not
statistically significant (Table 2, Fig. 3). The results of ROC analysis restricted to very mild
patients remained the same as above.
In both Pict 1 and Pict 2, comparison of the testretest examination showed excellent
correlations (r = 0.898, P < 0.001 for Pict 1; r = 0.929, P < 0.001 for Pict 2). Inter-rater reliability
was also high (r = 0.750, P < 0.001 for Pict 1; r = 0.795, P < 0.001 for Pict 2).
NIH-PA Author Manuscript
Although the utility of Pict 1 and Pict 2 to detect AD is similar in terms of validity and reliability,
to further examine the difference between shallow and deep encoding processes and a learning
effect, we compared the result of Pict 1 with that of Pict 2 as a post-hoc analysis. In both control
and AD groups, very high correlations between the two test scores were found (controls: r =
0.726, P < 0.001; patients: r = 0.773, P < 0.001). We examined the difference between Pict 2
and Pict 1 (i.e. Pict 2 Pict 1) among patients and controls. The difference in scores was
significantly larger among the control than the AD groups (3.8 6.8 vs 2.3 8.3, P < 0.001).
Discussion
With ongoing advances in the treatment of AD, early detection will become increasingly
important for intervention, and counseling of patients and families. It would be highly
beneficial for both patients and caregivers if the PCP could assess memory deficits in a simple
and easy manner. In this study, we examined a new screening test, SPMT, to distinguish patients
with early stages of AD from cognitively healthy elderly individuals. The SPMT had a larger
AUC to identify even the very mild AD cases (AD with MMSE 24) compared with those of
MMSE, VFT and CDT. The SPMT also demonstrated satisfactory testretest and inter-rater
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 5
reliabilities. Moreover, the test format was acceptable to elderly participants, without being
intimidating or taxing.
NIH-PA Author Manuscript
There are several potential reasons for the high efficacy of this test in detecting early AD
patients. First, pictorial material is usually easier to remember than materials presented by
words, a phenomenon known as the picture superiority effect.9,10,12,25 Superiority of
memory for pictorial material over verbal material was often applied as a mnemonic aid for
elderly.26,27 Potentially, the memory decline associated with normal cognitive aging could be
ameliorated by the picture superiority effect, making it easier to distinguish AD patients from
control participants.
NIH-PA Author Manuscript
Second, we used a picture of a living room with common furniture and objects familiar to most
elderly. The scene may have multiple cues to enhance recall; each object in the scene becomes
a cue for another object. In other words, once a part of the scene is recalled, other parts could
be recalled because the scene is not unique but shares many common aspects of daily life.
Categorically related or visually integrated cues are shown to be more effective in terms of
encoding than unrelated or non-interacting cues.28 It has been also shown that the recognition
of a scene as a context enhances memory of specific details.29,30 Buschke et al. reported in
their casecontrol study that subjects free from dementia could encode and retrieve more
effectively in the category cued recall memory tests than the demented. They suggested
encoding specificity deficit in dementia patients.5 The multiple cues in the scenery picture in
the SPMT may have resulted in facilitated encoding and retrieval of the items in the scene by
the healthy elderly but not by AD patients, making it more effective in distinguish the two
groups.
Additionally, in a recent functional imaging study, Gutches et al. reported that older adults
compensate for their decrement of memory function in medial temporal lobe by activation of
frontal systems, when pictorial materials are presented.31 Possibly, the pathological process of
AD may hamper this compensatory function, resulting in the discrepancy in SPMT scores
between the control and AD groups.
We examined the effect of shallow and deep memory processing on the performance of SPMT.
Although the results showed more benefit for deep memory processing or a potential learning
effect for cognitively normal elderly, Pict 1 and Pict 2 seem to be equivalent in the effectiveness
of distinguishing AD patients from the controls. Because Pict 1 takes only 2 min to administer
and has sufficient validity, Pict 1 may be more useful.
NIH-PA Author Manuscript
Limitations of the present study include the following. As mentioned above, because controls
in this study were younger and had higher education than AD patients in the total sample, we
confirmed the validity of the SPMT in two age groups. Further study in a large sample size
would be required to generalize our results. Second, we tested in this study utility of the SPMT
to distinguish early stage AD patients from controls. It would be important to further investigate
how to use it in a PCPs office or a memory clinic, because other types of patients with memory
deficit such as those with vascular dementia and depression may appear. Third, we used here
only the CCMT to test specifically the memory domain of cognition. Although the CCMT is
assumed to be an effective memory test as well as other standard memory tests such as the
Logical Memory Subtest of the Wechsler Memory Scale Revised or the California Verbal
Learning Test, direct comparison of the SPMT with such memory tests would be required.32,
33
Finally, AD patients who participated in this study came from outpatient referral to the
memory clinic. These subjects might be different in various characteristics from those with
AD, but do not visit memory clinics. Therefore, the generalization of our results could be
limited.
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 6
NIH-PA Author Manuscript
In conclusion, we present a new type of memory test which seems to be very useful in
identifying early stage AD patients. The distribution of test scores had neither ceiling nor floor
effects, and it was very easy to administer. We believe the scenery picture test will be a useful
tool for routine clinical evaluations.
Acknowledgments
We thank Drs Judith A. Saxton, Mary Ganguli and Katherine Wild for their helpful suggestions. This paper was
presented as a poster at the Mild Cognitive Impairment Symposium at Miami, Florida, March, 2007. This study was
supported by grants from the Japan Ministry of Education, Culture, Sports, Science and Technology (no. 18590598)
and National Institute on Aging in the United States (K01AG023014).
References
NIH-PA Author Manuscript
NIH-PA Author Manuscript
1. Ganguli M, Rodriguez E, Mulsant B, et al. Detection and management of cognitive impairment in
primary care: The Steel Valley Seniors Survey. J Am Geriatr Soc 2004;52:16681675. [PubMed:
15450043]
2. Borson S, Scanlan JM, Watanabe J, et al. Improving identification of cognitive impairment in primary
care. Int J Geriatr Psychiatry 2006;21:349355. [PubMed: 16534774]
3. Jitapunkul S, Chansirikanjana S, Thamarpirat J. Undiagnosed dementia and value of serial cognitive
impairment screening in developing countries: a population-based study. Geriatr Gerontol Int
2009;9:4753. [PubMed: 19260979]
4. Petersen RC, Smith GE, Waring SC, et al. Mild cognitive impairment: clinical characterization and
outcome. Arch Neurol 1999;56:303308. [PubMed: 10190820]
5. Buschke H, Sliwinski MJ, Kuslansky G, et al. Diagnosis of early dementia by the Double Memory
Test: encoding specificity improves diagnostic sensitivity and specificity. Neurology 1997;48:989
997. [PubMed: 9109889]
6. Solomon PR, Hirschoff A, Kelly B, et al. A 7 minute neurocognitive screening battery highly sensitive
to Alzheimers disease. Arch Neurol 1998;55:349355. [PubMed: 9520009]
7. Buschke H, Kuslansky G, Katz M, et al. Screening for dementia with the memory impairment screen.
Neurology 1999;52:231238. [PubMed: 9932936]
8. Nasreddine ZS, Phillips NA, Bedirian V, et al. The Mont-real Cognitive Assessment, MoCA: a brief
screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695699. [PubMed:
15817019]
9. Shepard RN. Recognition memory for words, sentences, and pictures. J Verbal Learn Verbal Behav
1967;6:156163.
10. Nickerson RS. A note on long-term recognition memory for pictorial material. Psychon Sci
1968;11:58.
11. Hasher L, Zacks RT. Automatic and effortful processes in memory. J Exp Psychol 1979;108:356
388.
12. Park DC, Puglisi JT, Sovacool M. Memory for pictures, words, and spatial location in older adults:
evidence for pictorial superiority. J Gerontol 1983;38:582588. [PubMed: 6886314]
13. Mayes AR. Learning and memory disorders and their assessment. Neuropsychologia 1986;24:25
39. [PubMed: 3517679]
14. Benton, AL. Revised Visual Retention Test. 4. New York: Psychological Corporation; 1974.
15. Lezak, MD. Neuropsychological Assessment. 3. New York: Oxford University Press; 1995.
16. Psychological Corporation. WAIS-III-WMS-III Technical Manual. San Antonio, TX: Psychological
Corporation; 1997.
17. Doss RC, Chelune GJ, Naugle RI. WMS-III performance in epilepsy patients following temporal
lobectomy. J Int Neuropsychol Soc 2004;10:173179. [PubMed: 15012837]
18. Gold JM, Poet MS, Wilk CM, et al. The family pictures test as a measure of impaired feature binding
in schizophrenia. J Clin Exp Neuropsychol 2004;26:511520. [PubMed: 15512938]
19. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4.
Washington, DC: American Psychiatric Association; 1994.
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 7
NIH-PA Author Manuscript
NIH-PA Author Manuscript
20. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of
Alzheimers disease: report of the NINCDS-ADRDA Work Group under the auspices of Department
of Health and Human Services Task Force on Alzheimers Disease. Neurology 1984;34:939944.
[PubMed: 6610841]
21. Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the
cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189198. [PubMed: 1202204]
22. Rouleau I, Salmon DP, Butters N, et al. Quantitative and qualitative analyses of clock drawings in
Alzheimers and Huntingtons disease. Brain Cogn 1992;18:7087. [PubMed: 1543577]
23. Funabiki Y, Takechi H, Akamatsu T, et al. Development of a short neuropsychological battery to
screen early dementia in elderly. Geriatr Gerontol Int 2002;2:179186.
24. Wechsler, D. WAIS-R Manual. New York: The Psychological Corporation; 1981.
25. Paivio A, Csapo K. Picture superiority in free recall: imagery or dual encoding? Cogn Psychol
1973;5:176206.
26. Cavanaugh JC, Grady JG, Perlmutter M. Forgetting and use of memory aids in 2070 year olds
everyday life. Int J Aging Hum Dev 1983;17:113122. [PubMed: 6671811]
27. McDowd J, Botwinick J. Rote and gist memory in relation to type of information, sensory mode, and
age. J Genet Psychol 1984;145:167178. [PubMed: 6527134]
28. Park DC, Smith AD, Morrell RW, et al. Effects of contextual integration on recall of pictures by older
adults. J Gerontol 1990:45.
29. Biederman I. Perceiving real-world scenes. Science 1972;177:7780. [PubMed: 5041781]
30. Loftus GR, Bell SM. Two types of information in picture memory. J Exp Psychol 1975;104:103
113.
31. Gutchess AH, Welsh RC, Hedden T, et al. Aging and the neural correlates of successful picture
encoding: frontal activations compensate for decreased medial-temporal activity. J Cogn Neurosci
2005;17:8496. [PubMed: 15701241]
32. Psychological Corporation. Wechsler Memory Scale-Revised. San Antonio, TX: Psychological
Corporation; 1987.
33. Delis, DC.; Kramer, JH.; Kaplan, E.; Ober, BA. California Verbal Learning Test Manual. San Antonio,
TX: Psychological Corporation; 1987.
NIH-PA Author Manuscript
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 8
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 1.
A line drawing scenery picture of a living room used in the Scenery Picture Memory Test.
NIH-PA Author Manuscript
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 9
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 2.
Score distribution of Pict 1 (a) and Pict 2 (b). In (a) and (b), horizontal axes indicate the number
of items in the picture reported by participants. Vertical axes indicate number of participants.
Closed bars indicate results from Alzheimers disease patients, and open bars from control
participants.
NIH-PA Author Manuscript
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 10
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 3.
Receiveroperator curve (ROC) curves indicating results from control participants vs
Alzheimers disease (MMSE >19). MMSE, Mini-Mental State Examination; CCMT, Category
Cued Memory Test; Pict 1, Scenery Picture Memory Test 1; Pict 2, Scenery Picture memory
Test 2.
NIH-PA Author Manuscript
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
NIH-PA Author Manuscript
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
12.2
53.3%
13.3
16.8
27.7
9.7
Female %
Pict 1
Pict 2
MMSE
CDT
33.5
VFT
Education
10.4
CCMT
n = 15
9.6
CDT
81.1
28.5
MMSE
Age
17.7
Age 75 years
13.8
Pict 2
VFT
Pict 1
25.5
CCMT
43.5%
10.3
CDT
12.2
9.6
MMSE
Female %
28.3
Pict 2
Education
17.5
Pict 1
n = 39
13.6
Female %
69.2
46.3%
Education
Age
12.2
Age
Age <75 years
n = 54
72.5
Both age groups
2.5
0.9
1.3
3.6
3.7
2.7
3.3
6.5
2.4
0.8
1.5
3.6
3.5
2.7
6.5
SD
0.8
1.8
3.6
3.0
2.9
4.5
10.4
Control
Average
AD
9.1
24.4
8.2
6.0
64.9%
11.1
79.5
n = 77
19.8
5.0
8.9
25.0
10.0
7.5
66.7%
11.6
69.0
n = 51
16.7
5.1
9.0
24.6
8.9
6.6
65.6%
11.3
75.3
n = 128
Average
1.4
3.0
4.6
3.2
2.7
3.9
12.2
2.8
1.5
2.7
4.2
3.1
2.9
4.7
5.9
2.6
1.5
2.9
4.5
3.2
2.8
6.7
SD
0.124
<0.001
<0.001
<0.001
NS
NS
NS
<0.001
<0.001
0.009
<0.001
<0.001
<0.001
0.034
NS
NS
<0.001
<0.001
0.004
<0.001
<0.001
<0.001
0.024
0.04
0.009
P-value
NIH-PA Author Manuscript
Characteristics of study participants
NIH-PA Author Manuscript
Table 1
Takechi and Dodge
Page 11
24.1
VFT
8.3
2.2
12.9
5.1
Average
11.1
2.5
SD
<0.001
<0.001
P-value
AD, Alzheimers disease; CCMT, Category Cued Memory Test; CDT, Clock Drawing Test; MMSE, Mini-Mental State Examination; NS, not significant; Pict 1 and Pict 2, Scenery Picture Memory Test 1 and
2; SD, standard deviation; VFT, Verbal Fluency Test (vegetables and sports/1 min each).
10.1
CCMT
SD
NIH-PA Author Manuscript
Average
NIH-PA Author Manuscript
AD
NIH-PA Author Manuscript
Control
Takechi and Dodge
Page 12
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
Takechi and Dodge
Page 13
Table 2
Area under the curves and the differences among tests
NIH-PA Author Manuscript
Control vs all AD
AUC (95% CI)
Control vs very mild AD
P-value
AUC (95% CI)
P-value
Both age groups
Pict 1
0.93 (0.890.96)
Reference
0.90 (0.850.95)
Reference
Pict 2
0.92 (0.880.96)
NS
0.89 (0.840.94)
NS
CCMT
0.92 (0.880.95)
NS
0.89 (0.840.94)
NS
MMSE
0.87 (0.820.92)
0.046
0.80 (0.730.87)
0.027
VFT
0.82 (0.760.88)
<0.001
0.76 (0.680.83)
0.001
CDT
0.63 (0.560.71)
<0.001
0.60 (0.520.68)
<0.001
Age <75 years
NIH-PA Author Manuscript
Pict 1
0.90 (0.840.96)
Reference
0.88 (0.800.95)
Reference
Pict 2
0.90 (0.840.96)
NS
0.89 (0.810.96)
NS
CCMT
0.91 (0.860.96)
NS
0.88 (0.810.95)
NS
MMSE
0.89 (0.820.95)
NS
0.85 (0.770.93)
NS
VFT
0.79 (0.700.88)
0.03
0.73 (0.620.85)
0.02
CDT
0.65 (0.550.75)
<0.001
0.61 (0.510.72)
<0.001
Age 75 years
Pict 1
0.95 (0.900.99)
Reference
0.92 (0.860.99)
Reference
Pict 2
0.92 (0.870.98)
NS
0.89 (0.810.97)
NS
CCMT
0.92 (0.870.98)
NS
0.90 (0.830.98)
NS
MMSE
0.82 (0.720.92)
0.023
0.70 (0.540.86)
0.014
VFT
0.79 (0.690.88)
0.003
0.72 (0.590.85)
0.009
CDT
0.64 (0.520.76)
<0.001
0.60 (0.470.73)
<0.001
P-value indicates differences in area under the curve (AUC) compared with Pict 1. AD, Alzheimers disease; CCMT, Category Cued Memory Test;
CDT, Clock Drawing Test; MMSE, Mini-Mental State Examination; NS, not significant; Pict 1 and Pict 2, Scenery Picture Memory Test 1 and 2;
VFT, verbal fluency (vegetables and sports/1 min each).
NIH-PA Author Manuscript
Geriatr Gerontol Int. Author manuscript; available in PMC 2011 April 1.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- High Intelligence and The Risk of ADHD and Other PsychopathologyDocument7 paginiHigh Intelligence and The Risk of ADHD and Other PsychopathologyVicente CáceresÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- THE Apostolic Bible: Polyglot Greek-English InterlinearDocument16 paginiTHE Apostolic Bible: Polyglot Greek-English InterlinearEsperdidesÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Antonello - Hesiod's Calendar and The Star SpicaDocument7 paginiAntonello - Hesiod's Calendar and The Star SpicamilosmouÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- 2015 Article 65Document6 pagini2015 Article 65Vicente CáceresÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- How To ReadDocument28 paginiHow To ReadVicente CáceresÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Walk Through The Scripture #6 - Passion Week Chronology r.4.4.0Document186 paginiWalk Through The Scripture #6 - Passion Week Chronology r.4.4.0Vicente CáceresÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Olivares y Gar CA 2015Document10 paginiOlivares y Gar CA 2015Vicente CáceresÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- 2015 Article 65Document6 pagini2015 Article 65Vicente CáceresÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- A Short Vocabulary List of Names and Words r.3.3Document16 paginiA Short Vocabulary List of Names and Words r.3.3Vicente CáceresÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Read Me First For IRENT With Online Up-Loading Notice: WWW - Academia.eduDocument11 paginiRead Me First For IRENT With Online Up-Loading Notice: WWW - Academia.eduVicente CáceresÎncă nu există evaluări
- Introduction To Pauline Epistles + Acrostic Bible PDFDocument12 paginiIntroduction To Pauline Epistles + Acrostic Bible PDFVicente CáceresÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Egō Eimi & Yeshua in The New TestamentDocument6 paginiEgō Eimi & Yeshua in The New TestamentVicente CáceresÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Outline of Pauline and General Epistles r.1.0.4Document3 paginiOutline of Pauline and General Epistles r.1.0.4Vicente CáceresÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Epistles 3Document23 paginiEpistles 3Vicente CáceresÎncă nu există evaluări
- HistoriaDocument2 paginiHistoriaVicente CáceresÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Edwards - 1992 - The Tale of Cupid and PsycheDocument20 paginiEdwards - 1992 - The Tale of Cupid and PsycheAshlar TrystanÎncă nu există evaluări
- Early NT TextsDocument26 paginiEarly NT TextsVicente CáceresÎncă nu există evaluări
- Philippians - Readers Edition July 1, 2020 Update r.2.4.1: Alas, Time and Tomorrow Do Not Wait For Us!Document22 paginiPhilippians - Readers Edition July 1, 2020 Update r.2.4.1: Alas, Time and Tomorrow Do Not Wait For Us!Vicente CáceresÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Readers Edition of IRENT - Revelation: Alas, Time and Tomorrow Do Not Wait For Us!Document81 paginiReaders Edition of IRENT - Revelation: Alas, Time and Tomorrow Do Not Wait For Us!Vicente CáceresÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Greene MA Dissertation PDFDocument118 paginiGreene MA Dissertation PDFSanda MaycaÎncă nu există evaluări
- SSRN Id2862330 102 QuadranglesDocument7 paginiSSRN Id2862330 102 QuadranglesVicente CáceresÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- A Web-Based Normative Calculator For The Uniform Data Set (UDS) Neuropsychological Test BatteryDocument9 paginiA Web-Based Normative Calculator For The Uniform Data Set (UDS) Neuropsychological Test BatteryVicente CáceresÎncă nu există evaluări
- Edinburgh Research Explorer: A Large-Scale Retrospective Study of Closing-In Behavior in Alzheimer's DiseaseDocument7 paginiEdinburgh Research Explorer: A Large-Scale Retrospective Study of Closing-In Behavior in Alzheimer's DiseaseVicente CáceresÎncă nu există evaluări
- Schoolagecbcl PDFDocument4 paginiSchoolagecbcl PDFVicente CáceresÎncă nu există evaluări
- ParietalDocument59 paginiParietalVicente CáceresÎncă nu există evaluări
- FRS Stages PDFDocument1 paginăFRS Stages PDFVicente CáceresÎncă nu există evaluări
- NormsSDQ5 10a PDFDocument5 paginiNormsSDQ5 10a PDFVicente CáceresÎncă nu există evaluări
- NormsSDQ5 10a PDFDocument5 paginiNormsSDQ5 10a PDFVicente CáceresÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Installation of The Attention Network Task (ANT) ProgramDocument2 paginiInstallation of The Attention Network Task (ANT) ProgramVicente CáceresÎncă nu există evaluări
- Task Design: Wack-A-Mole TaskDocument1 paginăTask Design: Wack-A-Mole TaskVicente CáceresÎncă nu există evaluări
- Air Pollutants Transport ModelsDocument12 paginiAir Pollutants Transport ModelsRahul DandautiyaÎncă nu există evaluări
- WSU Presentation 20220407Document63 paginiWSU Presentation 20220407debapriyoÎncă nu există evaluări
- Random Numbers in PythonDocument3 paginiRandom Numbers in PythonShubham RawatÎncă nu există evaluări
- 07a80809 OperationsresearchDocument11 pagini07a80809 OperationsresearchSharanya ThirichinapalliÎncă nu există evaluări
- Rodriguez-Castro Et Al 2022 Human Highly Modified Landscapes Restrict Gene FlowDocument20 paginiRodriguez-Castro Et Al 2022 Human Highly Modified Landscapes Restrict Gene FlowShara MotaÎncă nu există evaluări
- TMS Advanced TreeViewDocument64 paginiTMS Advanced TreeViewDanilo CristianoÎncă nu există evaluări
- C++ NotesDocument11 paginiC++ NotesVedant AmonkarÎncă nu există evaluări
- GTG Centaur 50 TurbomachineryDocument86 paginiGTG Centaur 50 TurbomachineryAlfian Aditya100% (3)
- TM 9-4110-241-23PDocument41 paginiTM 9-4110-241-23PwwwsurvivalebookscomÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Body FluidsDocument85 paginiBody FluidsShanta BharÎncă nu există evaluări
- Wa Wa40-3 Komatsu s3d84Document2 paginiWa Wa40-3 Komatsu s3d84james foxÎncă nu există evaluări
- 2021 SEM 4 CC 9 OrganicDocument3 pagini2021 SEM 4 CC 9 OrganicGaurav KumarÎncă nu există evaluări
- Astar - 23b.trace - XZ Bimodal Next - Line Next - Line Next - Line Next - Line Drrip 1coreDocument4 paginiAstar - 23b.trace - XZ Bimodal Next - Line Next - Line Next - Line Next - Line Drrip 1corevaibhav sonewaneÎncă nu există evaluări
- Chapter 4 Structure EditedDocument9 paginiChapter 4 Structure Editedyeshi janexoÎncă nu există evaluări
- Biology Paper 6 NotesDocument5 paginiBiology Paper 6 NotesbÎncă nu există evaluări
- Draft NADCADocument8 paginiDraft NADCAPierre MackenzieÎncă nu există evaluări
- HCL McQs SET-3Document8 paginiHCL McQs SET-3ThorÎncă nu există evaluări
- Abnormal Labour: Perceptor: Dr. Nurul Islamy, M. Kes., Sp. OGDocument54 paginiAbnormal Labour: Perceptor: Dr. Nurul Islamy, M. Kes., Sp. OGramadhiena destia100% (1)
- BMTC 132Document16 paginiBMTC 132Deepak Chaudhary JaatÎncă nu există evaluări
- SO100K Installation InstructionDocument32 paginiSO100K Installation InstructionAlwin Anno SastraÎncă nu există evaluări
- A) I) Define The Term Variable Costs Variable Costs Are Costs That Change With The Quantity of Products SoldDocument2 paginiA) I) Define The Term Variable Costs Variable Costs Are Costs That Change With The Quantity of Products SoldAleksandra LukanovskaÎncă nu există evaluări
- Calibration of The Continuous Surface Cap Model For ConcreteDocument19 paginiCalibration of The Continuous Surface Cap Model For ConcreteAbhijit KulkarniÎncă nu există evaluări
- PHYSICS Lab Manual - 2023-24Document30 paginiPHYSICS Lab Manual - 2023-24Vinushree Santhoshkumar100% (4)
- Compaction Factor ExperimentDocument23 paginiCompaction Factor ExperimentYI HEN ONGÎncă nu există evaluări
- 1.bitwise OperatorsDocument2 pagini1.bitwise OperatorsPaul kollamÎncă nu există evaluări
- Immediate Settlement Analysis Using Finite Element Analysis Models of Fb-MultipierDocument22 paginiImmediate Settlement Analysis Using Finite Element Analysis Models of Fb-MultipierRaaf RifandiÎncă nu există evaluări
- Fds 8878Document12 paginiFds 8878Rofo2015Încă nu există evaluări
- Kinetic Energy Recovery SystemDocument2 paginiKinetic Energy Recovery SystemInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări