Documente Academic
Documente Profesional
Documente Cultură
Jurnal Whipple Procedure
Încărcat de
Muhammad Ichsan PrasetyaDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Jurnal Whipple Procedure
Încărcat de
Muhammad Ichsan PrasetyaDrepturi de autor:
Formate disponibile
Saraee et al.
World Journal of Surgical Oncology (2015) 13:98
DOI 10.1186/s12957-015-0523-8
WORLD JOURNAL OF
SURGICAL ONCOLOGY
RESEARCH
Open Access
Whipple procedure: a review of a 7-year clinical
experience in a referral center for hepatobiliary
and pancreas diseases
Amir Saraee1, Jalal Vahedian-Ardakani2, Ehsan Saraee3, Roshanak Pakzad4 and Massoud Baghai Wadji2*
Abstract
Background: Pancreatic cancer is generally found in the older population Pancreaticoduodenectomy seems to be the
only way in resolving these resectable tumors. Allen. O Whipple was the first to describe pancreaticoduodenectomy in
1935 as a modified procedure. This article is a case series with respect to the 7-year experience of the Whipple
procedure in Firoozgar Teaching Hospital.
Methods: Patient surgery details were gathered from the surgical records of the operating room and their clinical
records from the hospital archives. Data was analyzed with SPSS software (version 16.0.1). Those patients, whose tumor
had invaded the superior mesenteric artery, had extensive portal vein involvement or distant metastasis was
considered as unresectable.
Results: The first Whipple procedure was recorded in our hospital in 2008. From 2008 till 20 March 2014, 70 cases were
collected and analyzed. The mean age of cases was 58.4 years, the mean hospital stay length was 12.9 days
(6.23 days), mean operation time was 376 min (37.3 min),. The most common presenting symptom was jaundice
(78.6 %). Delayed gastric emptying was the most common post-operative complication. The most prevalent cause of
reoperation was intra-abdominal abscess. Major morbidities of these patients consisted of cardiac arrhythmias (21.4%)
and pneumonia (10%). Minor complications were wound infection (17.1%) and delayed gastric emptying (32.9%). The
statistics revealed pancreatic anastomosis failure as 2.9% and a decrease in mortality rate from 50% during the first years
of this study to 16% to 20% during the last years.
Conclusions: In this case series, the time of operation decreased during the recent years .Analysis shows a correlation
between operation time and pack cell transfused during the operation, but no correlation was found between
operation time and post-operation hospitalization course. It is true that hospital setting, socioeconomic level of the
patients including their compliance, and the expertise of the surgeons and surgical staff can have an influence on the
result of this operation, but it seems that the magnitude of the surgical stress of this procedure and the (compromised)
functional reserve of this patient population can be a notable factor influencing the outcome.
Keywords: Pancreatic cancer, Whipple procedure, Periampullary carcinoma
Background
Pancreatic cancer is one of the most important causes of
death in eastern countries and the fourth cause of death
from cancer in the western hemisphere. Only a few percent of patients can survive from this condition for more
than 5 years. Most patients present with an advance
* Correspondence: baghaiw@yahoo.com
2
Department of Surgery, Iran University of Medical Sciences, Firoozgar
General Hospital, Tehran, Iran
Full list of author information is available at the end of the article
stage of the disease, and only in 10% to 20% of them the
mass is resectable. There are some factors for predicting
the prognosis, such as size of the tumor, degree of differentiation, status of resected lymph nodes, and the involvement of the resected margins. In some articles, the
post-resection CA 19-9 level and tumor DNA content
were also mentioned as prognostic factors. Among various treatments for pancreatic cancers, surgery was the
only chance for cure [1].
2015 Saraee et al.; licensee BioMed Central. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain
Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article,
unless otherwise stated.
Saraee et al. World Journal of Surgical Oncology (2015) 13:98
Predisposing factors for pancreatic cancer remain unknown, but tobacco is the most probable reason. Risk increases with longer exposure to smoke and greater
tobacco usage. There is some evidence that alcohol, coffee, and aspirin consumption are among the predisposing factors. Other risk factors are history of diabetes or
chronic pancreatitis, chronic cirrhosis, and patients with
blood type A, B, or AB. Only 5% to 10% of these patients
have a positive familial history of pancreatic cancer [2].
For the first time, Allen. O Whipple described pancreaticoduodenectomy in the year 1935 when he modified the procedure that was performed before by
Alessendro Codinivillan in Italy and Walter Keusch in
Germany [3].
In a similar study at the Massachusetts hospital [4],
pancreatic cancer cases that required surgery were
followed and improvements in Whipple procedure were
reported. The aim of this study is to evaluate the evolution of this procedure from 2008 to 2014 in our hospital
and analyze the statistics pertaining to the presenting
signs and symptoms, Whipple procedure, and the clinical post-operation courses.
Methods
Data regarding the surgery was extracted from the archives of Firoozgar General Hospital, and further information was obtained from the medical records from
2008 to 2014. Data related to the pancreaticoduodenectomy or whipple procedures were gathered using a
checklist designed for this study. The data was analyzed
using the SPSS software (version 16.0.1). The parameters
and variables of the study were patient demographic
data, presenting symptoms, physical signs, past medical
history, intra-operative parameters, post-operative complications, pathology, causes of post-operative death,
cause of readmission, and cause of reoperation. Those
patients, whose tumor had invaded the superior mesenteric artery, had extensive portal vein involvement, or
distant metastasis was considered as unresectable. None
of the patients received neoadjuvant chemotherapy.
Results
A number of 70 procedures were performed till 2014 by
three different surgeons. As a mean, our center performs
10 procedures per year but the number of procedures
had increased from 2 operations in 2008 to 25 operations in 2014.
Analyses have shown the mean age of cases as
58.4 years with 40% of the gender being male. A portion
of patients (35.1%) were greater than 65 years of age.
The minimum age was 29; the oldest patient being
78 years old.
Prevalence of diabetes mellitus before surgery was
13.5%; among them, 5% were on medication with oral
Page 2 of 5
agents and 2.7% with insulin. Meanwhile, 91.9% of the
diabetic patients were not receiving any medication.
After the procedure, 27% of patients had new onset diabetes mellitus. In this case series, the percentage of alcohol consumers was 2.7%, and 21.6% of patients were
smokers. One patient (2.7%) was addicted to opium.
About 13.5% of them had a positive family history of
cancer, and of them, 32.5% had pancreatic cancer.
The most common presenting symptom was jaundice
(78.6%). Among them, 70% complained of abdominal
pain. Other symptoms in order of frequency are weight
loss, anorexia, nausea, vomiting, and fever.
Pathology
Eight and a half percent (8.5%) of cases had benign lesions, but the main indication for pancreaticoduodenectomy was malignancy in the pancreas. In this study, the
most common pathology was adenocarcinoma; 62.2% of
them were well differentiated.
The lymph nodes were involved by the tumor in 35.1%
of cases. The surgical pathology studies were as follows:
two patients had intestine type adenocarcinoma, four
had neuroendocrine tumors, and in one case, granulocytosis paraganglioma was observed. A 29-year-old woman
had duodenal large-cell malignant lymphoma (diffuse
type). Her presenting symptoms were weight loss, anorexia, and vomiting.
There were benign lesions in 5.9% of cases, like adenomatous dysplasia of the duodenum. About 52.9% of malignancies were periampulary lesions, and 38.6% of them
were neoplasms of the pancreas. Liver metastasis and abdominal wall seeding was considered as unresectable.
Among patients who underwent staging before surgery,
stage IIB was the most common stage. Unfortunately,
there was no sufficient data in the archives regarding the
staging of the other 48 patients (Table 1).
Operation course
The mean operation time was 376 min (37.3 min), and
intra-operative blood transfusion was approximately 1.84
pack cells each operation (Table 2).
The mean age of patients was 58.4 years; the mean admission length was 12.9 days (6.23 days). Of them,
Table 1 Stage of tumor before operation
Stage of tumor before operation
Number
IA
IB
IIA
IIB
10
III
No staging was present
2
48
Saraee et al. World Journal of Surgical Oncology (2015) 13:98
Table 2 Changes of operation time, used pack cell during
operation, and post-hospitalization days during the
time spent
Date
Page 3 of 5
Table 3 Complications
Complications
Number
Percent
Delayed emptying
23
32.9%
Mean (hours) SD
operation time
average
Used pack
cell during
operation
Post-op time
hospitalization average
mean (day) SD
Cardiac complications
15
21.4%
Wound infection
12
17.1%
2008
4.9 0.06
17 0.7
Pneumonia
10.0%
2009
5.7 1.12
17 5.7
Hemorrhage
7.1%
2010
5.0 0.51
8 6.4
GI leakage
7.1%
2011
4.2 0.53
10 5.7
Renal failure
5.7%
2012
5.0 0.78
17 13
Biliary fistula
2.9%
2013
4.5 0.33
15 6.9
Pancreatic fistula
0.0%
2014
5.2 1.02
11 5.2
Cholangitis
0.0%
45.9% of patients suffered from abdominal pain, weight
loss was seen in 16.2% of them, and 8.1% of them cases
had foul stool after surgery.
The common technique for reconstruction in our
study was classic pancreaticojejunostomy (83.8%). In one
case, we repaired the transverse mesocolon that was injured inadvertently.
In some cases, the major vessels were involved by the
tumor. If the SMA was involved, the case was considered inoperable and excluded from this study. SMV or
portal vein could be repaired if less than 180 of the circumference of portal vein was involved by the tumor. In
this case series, vascular reconstruction was performed
in 13 patients (11.4% portal reconstruction, 7.1% SMV
reconstruction). Vascular repair was performed due to
vein involvement by tumor or iatrogenic injury.
Complications
The most common complication after surgery was delayed
gastric emptying (32.9%). GI leakage was related to failure
of gastro-jejunostomy anastomosis, and biliary fistula was
secondary to choledocojejunostomy anastomosis disruption or leakage. Major morbidities of these patients consisted of cardiac complications like cardiac arrhythmias
(21.4%), pneumonia (10%), hemorrhage (7.1%), biliary
fistula (2.9 %), and renal failure (5.7%). Minor complications were wound infection (17.1%) and delayed emptying (32.9 %) (Table 3).
Readmission
Thirty-seven (37%) percent of cases were readmitted due
to various problems. After nausea and vomiting as the
most common reason of readmission in 24.2% of cases,
the second reason was pneumonia (19.24%). In order of
decreasing frequency, other readmission causes were
wound infection, controlling blood sugar, intra-abdominal
abscess, GI bleeding, and fever.
Post-operation course
In the early post-operative mortality group (death below
1 month after operation), seven cases died due to septic
shock, three of them had massive gastrointestinal bleeding, and one patient had pulmonary thromboembolism
(Table 4). The patients with septic shock were considered as a probable failure of pancreatic anastomosis
since there was no site of infection in other organs, and
autopsy was not allowed to be performed by one patients family.
Discussion
Pancreatic cancer is the fourth leading cause of cancer
death because of short-term survival time, regardless of
its stage. The main etiology of pancreatic cancer is unknown, though the incidence of pancreatic cancer is 2.5
to 3.6 times more in smokers. There also exists some
evidence that alcohol, coffee, and aspirin consumption
can lead to pancreatic cancer. The presenting symptoms
Table 4 Post-operative death
Reoperation
Early post-op death
Number
Percent
The most common cause for reoperation was intraabdominal abscess (21.4%). Other causes of reoperation
were bleeding in one case and obstruction in two. Biliary
cutaneous fistula was seen in two patients, and one was
operated twice due to bowel obstruction. Other causes
of reoperation consist of wound dehiscence, tracheostomy, and gastrojejunostomy revision.
Septic shock
10
Massive GI bleeding
4.3
PTE
1.4
Hypovolemic shock
1.4
ARDS
1.4
Acute MI
0.0
Saraee et al. World Journal of Surgical Oncology (2015) 13:98
of pancreatic cancer depend on the location, size, and
stage of the tumor [2]. Pancreatic cancer is mostly seen
in the elderly, and the overall 5-year survival rate is
below 5% [5-7].
The histologic precursor best characterizing pancreatic
cancer is intra-epithelial neoplasia [8]. Dens stroma
termed as desmoplastic reaction in pathological assessment is also characteristic of pancreatic cancer [9].
Allen Oldfather Whipple modified the pancreaticoduodenectomy procedure in 1935 [3,10,11]. Surgical biliary and gastric bypass was superior to endoscopic
intervention in terms of quality of life improvement and
decreasing rate of re-hospitalization and re-intervention
[12]. Nowadays, Whipple is an acceptable operation that
is performed in various malignant and benign diseases of
pancreas and periampulary area [13].
During the past 7 years of our experience in this procedure, an improvement in the different aspects of the
technique including lesser time of operation, less intraoperative bleeding, less pancreatic anastomosis failure,
and decrease in hospital staying days. Pancreatic anastomosis was performed in two layers with non-absorbable
suture material and in an end-to-end and invagination
technique. In some cases, omentum was used as a barrier between the site of pancreatic anastomosis and superior mesenteric vein.
Though the statistics reveal a pancreas anastomosis failure of 2.9% but due to the lack of autopsy findings, the authors consider it as 10% because of sepsis with unknown
origin. There was decreasing in mortality rate from 50%
during the first year of this study (among two patients) to
16% to 20% during the last years (among 25 patients).
The number of this procedure has increased in our
center during the recent years due to developing an advanced gastrointestinal department and a referring system from that ward. Although complications of this
surgery are still observed in our hospital, its decreased
rate could be attributed to better surgical techniques,
better post-operation intensive care, and improved surgical staff expertise and more accurate patient selection.
Post-operation hospitalization duration has decreased
too except for in some complicated cases.
We found a meaningful correlation between operation
time and packed blood cell transfused intra-operatively
(P value <0.05) but no correlation has been found between operation time and the length of hospitalization.
According to the surgical pathologic study, four patients had well-differentiated neuroendocrine tumor
(NET). The mean age of this group was 61.75 years, and
the average hospitalization time was 13.5 days. Three of
the four patients were female. It is notable that although
the tumor had invaded the superior mesenteric vein or
portal vein in two patients, none of them had jaundice.
It could be assumed that NET could have enlarged bulk
Page 4 of 5
of mass without resulting in obstructive jaundice, but
adenocarcinoma causes jaundice even with a smaller
tumor size. The most common presenting sign of NET
was vomiting and abdominal pain. In spite of their burden, these tumors could be resected easier than adenocarcinoma. Survival of this group was greater than other
pathologies (average = 36 months). Two cases in this
group survived for 72 and 60 months after surgery.
None of them have expired till date.
Several studies have reported the effect of treating a
high volume of patients on post-operative outcomes.
The definition of high and low volume varied among all
these studies from 15 patients to 40 patients per year.
Birkmeyer et al. have reported a marked difference in
mortality rates of Whipple procedure in very low-volume
(zero or one patient per year) and low-volume (one or two
per year) hospitals compared with higher-volume hospitals
(less than five per year). Surgeons who performed fewer
than four resections per year had more complications than
those who performed more than four [14].
On the other hand, mortality rates at very low and
low-volume hospitals were significantly higher than
those at high-volume hospitals.
Conclusions
Though pancreaticoduodenectomy is the treatment of
choice in the patients with periampulary carcinoma and
in spite of its introduction to the medicine 80 years ago,
it still has significant mortality and morbidity even in
high volume centers.
It is true that hospital setting, socioeconomic level of
the patients including their compliance, and the expertise of the surgeons and surgical staff can have influence
over the result of this operation; it seems that the magnitude of the surgical stress of this technique and the
compromised functional reserve of these patient population can be a notable factor influencing the outcome.
Even though our data strongly suggests - as other
studies - that pancreatic resections should be carried out
at institutions that perform a large number of them annually, it should be kept in mind whether the extent of
operation can be reduced in the future.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
JV and MBW conceived the study and participated in the design of the study.
ES and RP participated in data collecting. AS performed the study and wrote
the first manuscript. The revision and response to the referees was carried out
by MBW and AS. All authors read and approved the final manuscript.
Acknowledgements
The authors are grateful to Dr. Niki Rashidian (Firoozgar Hospital, Tehran,
Iran) for critically reviewing the manuscript and Dr. Nouralshakira Ghaffoor
for editing the paper in its English writing.
Saraee et al. World Journal of Surgical Oncology (2015) 13:98
Page 5 of 5
Author details
1
Iran University of Medical Sciences, Firoozgar General Hospital Tehran,
Tehran, Iran. 2Department of Surgery, Iran University of Medical Sciences,
Firoozgar General Hospital, Tehran, Iran. 3Tehran University of Medical
Sciences, Tehran, Iran. 4Shahed University of Medical Sciences, Tehran, Iran.
Received: 8 August 2014 Accepted: 23 February 2015
References
1. Charles J, Yeo M, John L, Cameron MD. Pancreaticoduodenectomy with or
without extended retroperitoneal lymphadenectomy for periampullary
adenocarcinoma comparison of morbidity and mortality and short-term
outcome. Ann Surg. 1999;229(5):61324.
2. Manuel Hidalgo MD. Pancreatic cancer. N Engl J Med. 2010;362:160517.
3. Whipple AO. Pancreaticoduodenectomy for islet carcinoma: a five-year
follow-up. Ann Surg. 1945;121:84752.
4. Carlos Fernandez-del Castillo M, Vicente M-O. Evolution of the Whipple
procedure at the Massachusetts General Hospital. Surgery. 2012;152:5663.
5. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics 2008.
CA Cancer J Clin. 2008;58:7196.
6. Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic cancer. Lancet. 2004;363:1049.
7. Shi C, Hruban RH, Klein AP. Familial pancreatic cancer. Arch Pathol Lab Med.
2009;133:36574.
8. Hruban RHMA, Hruban RH, Maitra A, Goggins M. Update on pancreatic
intraepithelial neoplasia. Int J Clin Exp Pathol. 2008;1:30616.
9. Chu GC, Kimmelman A, Hezel AF, DePinho RA. Stromal biology of
pancreatic cancer. J Cell Biochem. 2007;101:887907.
10. Schnelldorfer T. Forgotten pioneers of pancreatic surgery: beyond the
favorite few. Ann Surg. 2008;247:191202.
11. Schnelldorfer T. Alessandro Codivilla and the first pancreatoduodenectomy.
Arch Surg. 2009;144:117984.
12. Walter J. Palliative partial pancreaticoduodenectomy impairs quality of life
compared to bypass surgery in patients with advanced adenocarcinoma of
the pancreatic head. EJSO. 2011;37:798804.
13. Huang JJ. Quality of life and outcomes after pancreaticoduodenectomy.
Ann Surg. 2000;231(6):8908.
14. Birkmeyer JD. Hospital volume and surgical mortality in the United States.
N Engl J Med. 2002;346(15):112837.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
S-ar putea să vă placă și
- Anemia and Reduced Kidney Function As Risk Factors For New Onset of Atrial FibrillationDocument6 paginiAnemia and Reduced Kidney Function As Risk Factors For New Onset of Atrial FibrillationMuhammad Ichsan PrasetyaÎncă nu există evaluări
- Global Surgery and Anesthesia Manual (Dragged)Document9 paginiGlobal Surgery and Anesthesia Manual (Dragged)Muhammad Ichsan PrasetyaÎncă nu există evaluări
- Treatment of Recurrent Primary SpontaneousDocument8 paginiTreatment of Recurrent Primary SpontaneousMuhammad Ichsan PrasetyaÎncă nu există evaluări
- Ni Hms 603061Document27 paginiNi Hms 603061Muhammad Ichsan PrasetyaÎncă nu există evaluări
- Ni Hms 603061Document27 paginiNi Hms 603061Muhammad Ichsan PrasetyaÎncă nu există evaluări
- 10 11648 J Ja 20150303 11Document4 pagini10 11648 J Ja 20150303 11Muhammad Ichsan PrasetyaÎncă nu există evaluări
- 10 11648 J Ja 20150303 11Document4 pagini10 11648 J Ja 20150303 11Muhammad Ichsan PrasetyaÎncă nu există evaluări
- Treatment of Recurrent Primary SpontaneousDocument8 paginiTreatment of Recurrent Primary SpontaneousMuhammad Ichsan PrasetyaÎncă nu există evaluări
- The Fox and The LeopardDocument1 paginăThe Fox and The LeopardichsanprasetyaÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Serving North Central Idaho & Southeastern WashingtonDocument12 paginiServing North Central Idaho & Southeastern WashingtonDavid Arndt100% (3)
- Sample Dilapidation ReportDocument8 paginiSample Dilapidation ReportczarusÎncă nu există evaluări
- Siemens Internship ReportDocument84 paginiSiemens Internship Reportujjawalbhojawala100% (1)
- Pref - 2 - Grammar 1.2 - Revisión Del IntentoDocument2 paginiPref - 2 - Grammar 1.2 - Revisión Del IntentoJuan M. Suarez ArevaloÎncă nu există evaluări
- PAG7.1 Student The Effects of Antibiotics On Microbial Growth - v0.3Document3 paginiPAG7.1 Student The Effects of Antibiotics On Microbial Growth - v0.3Habib UddinÎncă nu există evaluări
- Method Statement For Cable Trays & Cable Ladders InstallationDocument7 paginiMethod Statement For Cable Trays & Cable Ladders InstallationJamal Budeiri0% (1)
- Ii 2015 1Document266 paginiIi 2015 1tuni santeÎncă nu există evaluări
- Bahir Dar University BIT: Faculity of Mechanical and Industrial EngineeringDocument13 paginiBahir Dar University BIT: Faculity of Mechanical and Industrial Engineeringfraol girmaÎncă nu există evaluări
- Industrial Internet of Things: Presented To-Presented byDocument18 paginiIndustrial Internet of Things: Presented To-Presented byGaurav RaturiÎncă nu există evaluări
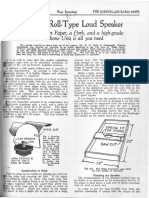
- Simple Roll-Type: A Loud SpeakerDocument1 paginăSimple Roll-Type: A Loud SpeakerEudes SilvaÎncă nu există evaluări
- CAC Bubble DiagramsDocument12 paginiCAC Bubble Diagramsangst6250Încă nu există evaluări
- ASCE Snow Loads On Solar-Paneled RoofsDocument61 paginiASCE Snow Loads On Solar-Paneled RoofsBen100% (1)
- Stanley B. Alpern - Amazons of Black Sparta - The Women Warriors of Dahomey-New York University Press (2011)Document308 paginiStanley B. Alpern - Amazons of Black Sparta - The Women Warriors of Dahomey-New York University Press (2011)georgemultiplusÎncă nu există evaluări
- Differential Geometry of Curves and Surfaces 3. Regular SurfacesDocument16 paginiDifferential Geometry of Curves and Surfaces 3. Regular SurfacesyrodroÎncă nu există evaluări
- Accsap 10 VHDDocument94 paginiAccsap 10 VHDMuhammad Javed Gaba100% (2)
- Intel Stratix 10 Avalon - MM Interface For PCI Express Solutions User GuideDocument173 paginiIntel Stratix 10 Avalon - MM Interface For PCI Express Solutions User Guideenoch richardÎncă nu există evaluări
- Book BindingDocument14 paginiBook Bindingpesticu100% (2)
- By This Axe I Rule!Document15 paginiBy This Axe I Rule!storm0% (1)
- VTA28-G5: Fuel OptimizedDocument3 paginiVTA28-G5: Fuel OptimizedIslam HemdanÎncă nu există evaluări
- Chapter 5 AGVDocument76 paginiChapter 5 AGVQuỳnh NguyễnÎncă nu există evaluări
- A Presentation On-: Dr. Nikhil Oza Intern BvdumcDocument43 paginiA Presentation On-: Dr. Nikhil Oza Intern BvdumcMaheboob GanjalÎncă nu există evaluări
- 1986 EMT Disruption of Microbial Cells For Intracellular ProductsDocument11 pagini1986 EMT Disruption of Microbial Cells For Intracellular ProductsLezid CortesÎncă nu există evaluări
- Engineering Structures: C.X. Dong, A.K.H. Kwan, J.C.M. HoDocument14 paginiEngineering Structures: C.X. Dong, A.K.H. Kwan, J.C.M. HoElieser SinagaÎncă nu există evaluări
- Imbinari Teava Fibra de Sticla PDFDocument1 paginăImbinari Teava Fibra de Sticla PDFplex015Încă nu există evaluări
- Electrical Power System Device Function NumberDocument2 paginiElectrical Power System Device Function Numberdan_teegardenÎncă nu există evaluări
- Module in Pe 103Document79 paginiModule in Pe 103Kym Dacudao100% (1)
- All About PlantsDocument14 paginiAll About Plantsapi-234860390Încă nu există evaluări
- 40 RT-flex Control-System Rev01Document68 pagini40 RT-flex Control-System Rev01Mayvon Botelho100% (2)