Documente Academic
Documente Profesional
Documente Cultură
Determination of Efficacy of Isoxyl A Mycolic Acid Inhibitor in Vitro Against Mycobacterium - Tuberculosis Strains
Încărcat de
Global Research and Development ServicesTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Determination of Efficacy of Isoxyl A Mycolic Acid Inhibitor in Vitro Against Mycobacterium - Tuberculosis Strains
Încărcat de
Global Research and Development ServicesDrepturi de autor:
Formate disponibile
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Shashikant Vaidya et al.
Special Issue, 2015, pp. 1-24
DETERMINATION OF EFFICACY OF ISOXYL, A MYCOLIC
ACID INHIBITOR, IN VITRO AGAINST
MYCOBACTERIUM.TUBERCULOSIS STRAINS
Shashikant Vaidya
Department of Clinical Pathology, Haffkine Institute for Training, Research and Testing,
Mumbai, India, shashikantvaidya@hotmail.com
Kapil Punjabi
Department of Clinical Pathology, Haffkine Institute for Training, Research and Testing,
Mumbai, India, kapil9372@gmail.com
Shreyasi Muley
Haffkine Bio-pharmaceutical Corporation Ltd. Mumbai, India shreyasi.mulye@gmail.com
Geeta Koppikar
Breach Candy Hospital Trust, Mumbai, India info@breachcandyhospital.org
Mohan Kulkarni
T.N. Medical College and B.Y.L. Nair Charitable Hospital, Mumbai, India
AbhayChowdhary
Grant Government Medical College and Sir JJ Hospital, Mumbai India,
abhaychowdhary@yahoo.com
Abstract
The enzymes involved in the biosynthetic pathways of the critical components including mycolic
acids offer attractive and selective targets for the developments of novel anti-mycobacterial
agents. Isoxyl (ISO), a mycolic acid inhibitor, is an old drug, which was used for the treatment of
tuberculosis was evaluated. Determination of Minimum Inhibitory Concentration (MIC) pattern
of clinical isolates of Mycobacterium tuberculosis (M. tuberculosis) to mycolic acid inhibitors
namely ISO, Isoniazid (INH) and Ethionamide (ETH) by agar and broth dilution Method was
done. Also the Minimum bactericidal concentrations were evaluated. Total 40 MDR and 20
susceptible strains of M tuberculosis were tested. The result of the MIC studies showed that ISO
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
is capable of inhibiting the growth of M. tuberculosis in a range of 1-20g/ml. Inhibitory activity
of ISO was higher than activity of ETH in solid media. Amongst three antituberculosis drugs,
INH showed highest bactericidal activity against M. tuberculosis strains followed by ETH. While
ISO exhibited lowest bactericidal activity. Amongst, three drugs tested, ISO shows highest
MBC/MIC ratio with lowest bactericidal activity. ISO showed significantly lower bactericidal
activity against MDR strains than susceptible strains of M. tuberculosis. MBC/ MIC ratio of ISO
was similar to MDR and susceptible strains of M. tuberculosis. Overall study implies that ISO
may be suitable for the treatment of Tuberculosis, particularly multi-drug resistant kind.
Keywords
MDR TB, Isoxyl, Mycolic Acid Inhibitor
1. Introduction
Developing new antituberculosis drugs is an expensive exercise and tuberculosis (TB) is
not a disease of rich nations. Some development projects are underway, but more are needed. TB
still remains a neglected disease in relation to drug development (Chopra, Meena, & Singh,
2003). The needs, challenges and recent advances towards development of novel chemical
molecules against TB have been reviewed recently (Lienhardt, 2012).
Approximately 2 billion people of the worlds population are latently infected with
Mycobacterium tuberculosis ( M. tuberculosis) and are at risk of reactivation to active disease
(Diel et al., 2013). Even though an inexpensive and effective quadruple drug therapy regimen
comprising Isoniazid (INH), Rifampicin (RF), Ethambutol (EMB) and Pyrazinamide (PZ) was
introduced 40 years ago, TB continues to spread in every corner of the globe (Raviglione et al.,
2012).
The current treatment regimen has several drawbacks, including prolonged treatment
time to completely eradicate the bacteria. This increases the opportunity for development of
resistant strains of M. tuberculosis documented in almost every country where the disease is
prevalent. These obstacles, in addition to an increasing prevalence of MDR, XDR and currently
TDR strains, call for an urgent need to search for and develop novel agents against TB.
Pulmonary TB remains a major health hazard in Asia, Africa and the Western Pacific region,
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
despite its sharp decline in the Western world since the beginning of the 20th century (Mitra,
2012).
A number of approaches are considered to identify targets for novel anti-mycobacterial
agents. They range from biochemical studies of essential pathways to the use of genome scale
tools such as transposon mutagenesis, proteomics and transcript mapping on micro arrays. In
combination with modern approaches, such as structure based drug design and combinatorial
chemistry will lead to the development of new drugs that are not only active against drug
resistant TB but shorten the chemotherapy schedule. Several targets have been identified and
combination of high throughput screening and rational structure based design is being used to
identify lead molecule (Chopra et al., 2003). Current chemotherapy for TB relies on
Mycobacteria specific drugs that inhibit bacterial metabolism with a heavy emphasis on
inhibitors of the cell wall polymer. (Balows et al., 1975).
These critical components of the cell envelope have been the subject of intense research
for a number of years because of the fact that enzymes involved in their biosynthetic pathways
including mycolic acids, offer attractive and selective targets for the developments of novel antimycobacterial agents (Brennan, 2002).
There is an urgent need to develop new effective antituberculosis compounds that can
increase the permeability of the Mycobacterial cell wall by inhibiting the synthesis of cell wall
components and enhance the activity of conventional drugs as a result of increased penetration of
these latter agents to susceptible internal targets (David et al., 1988). This enhancement of
antimicrobial activity theoretically affords the use of lower concentration of antibiotics
associated with toxicity (Matlola, Steel, & Anderson, 2001). As drug development is a long and
expensive process, it becomes predominant to re-examine drugs that were formerly deemed
effective against TB and increase the permeability of the Mycobacterial cell wall. One such drug
is Isoxyl (ISO). ISO is an old drug, used for the clinical treatment of TB in 1960s (Winder,
1982). Some authors demonstrated modest therapeutic efficacy of ISO monotherapy in cases of
untreated pulmonary TB of various degree of difficulty (Tischer, 1966; Urbancik, 1970). While
some concluded that INH and ISO were more effective than monotherapy with either drug
(Schmid, 1970). The NCDDG group led by DR Patrick Brennan recently evaluated this drug and
found it to be effective against MDR strains of M. tuberculosis. ISO, a thiourea (thiocarlide, 4, 4
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
diisoamyloxythiocarbanilide) demonstrated potent activity against standard strain of M.
tuberculosis (Phetsuksiri et al., 1999).It had been noted that it strongly inhibited mycolic acid
synthesis in M. bovis (Winder, 1982).
Hence there was a thought to do more work on this compound, as it is an old drug and
have proven its efficacy. Present study was conducted with the objective of determining the
efficacy of ISO in vitro against M. tuberculosis strains.
2. Material and methods
2.1 Mycobacterial Strains
Total 60 Clinical isolates of M. tuberculosis were collected from Department of
Microbiology of P.D. Hinduja Hospital and Medical Research Centre, Mumbai. The clinical
isolates were defined as M. tuberculosis according to their growth rates, pigmentation properties
of colonies, susceptibility to para-nitro benzoic acid, semi-quantitative catalase test, nitrate
reduction test and niacin accumulation tests (Vestal, 1975). Drug susceptibility pattern of 60
clinical isolates of M. tuberculosis was determined by Bactec460TB system by modified
Proportion Method (Siddiqui, S. H., Libonati, J.P. and Middlebrook G, 1981).
2.2 Determination of Minimum Inhibitory Concentration using Agar dilution method
Minimum Inhibitory Concentration (MIC) pattern of clinical isolates of M. tuberculosis
to mycolic acid inhibitors was ascertained by agar dilution method. (Hawkins, et al., 1991). Total
40 MDR and 20 susceptible strains of M. tuberculosis along with standard strain of M.
tuberculosis H37Rv were included in the study. Mycolic acid synthesis inhibitors studied were
ISO (Cayman Chemical Co., U.S. A.), INH (Lupin Pharmaceuticals, India) and Ethionamide
(ETH) ( Lupin Pharmaceuticals, India).
Sterile Middlebrook 7H10 agar with Oleic acid,
Dextrose and Catalase (OADC) supplement (HiMedia Laboratories Pvt Ltd, India) was used for
this method. Serial two fold dilutions of individual drug were prepared in sterile water for
injection after dissolving it in suitable diluents. 1ml of test drug solution (20X) was mixed with
19 ml of sterile molten Middlebrook 7H11 medium with OADC supplements (HiMedia
Laboratories Pvt Ltd, India) and poured in sterile petri plates. Media was cooled and agar was
set. Test strains were inoculated in sterile Dubos broth with glucose and albumin supplement
with 0.05% Tween 80 (HiMedia Laboratories Pvt Ltd, India) and incubated at 37 C for 7 to 10
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
days. Cultures were shaken daily on vortex mixture for 30 seconds. The cultures were adjusted to
an optical density of 0.1 at 540 nm and then diluted 10 fold in 0.1% Tween 80 containing normal
saline. Bacterial suspension in 5-microlt quantities was spotted on agar plates containing various
drug concentrations. The control plates, containing no drug were also inoculated along with it.
Plates were incubated at 37 C for 14 days. The MIC was defined as the minimum
concentrations of drugs that completely inhibited the growth of the test organism or allowed
growth of not more than five colonies.
Following drugs concentrations (g/ml) were used for the test:
ISO: 0.07, 0.15, 0.3, 0.6, 1.2, 2.5, 5, 10, 20 and 40 g/ml
INH: 0.0125, 0.025, 0.05, 0.1, 0.2, 0.4, 0.8, 1.6, 3.2 and 6.4 g/ml
ETH: 0.15, 0.3, 0.6, 1.2, 2.5, 5, 10, 20, 40 and 80 g/ml
2.3 Determination of Minimum Inhibitory Concentration using Broth dilution method
Determination of MIC pattern of clinical isolates of M. tuberculosis to mycolic acid
inhibitors by carried out using broth dilution method (Cruikshank, Duguid, & Swain, 1968;
Tomioka, Saito, Fujii, Sato, & Hidaka, 1993).
MIC pattern of 40 MDR and 20 susceptible strains of M. tuberculosis along with standard
strain of M. tuberculosis H37Rv were determined to mycolic acid synthesis inhibitors. Sterile
Dubos broth with glucose and albumin supplement was used in the test. Serial two-fold dilution
of individual drug was prepared in sterile Dubos broth with glucose and albumin supplement
after dissolving it in suitable diluents. It was dispensed in 4.5-ml quantities in sterile tubes.
Required drug concentration in 10 X concentrations was put in 0.5 ml quantity in medium to
obtain desired concentration. Each of the drug containing tube and drug free tube were
inoculated with 0.1 ml. of test culture adjusted to McFarland No. 1 turbidity. The original
inoculum size of each test strain was determined by appropriately diluting the culture and
inoculating 0.1 ml of culture on sterile LJM slants. A tube containing the highest concentration
of the drug without any culture was also incubated as a drug control to check if the drug agent
contributed to the turbidity of the medium. Drug free tube inoculated with test culture was kept
as positive control. Medium control was also kept. Inoculated and un-inoculated tubes were
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
incubated at 37C for 15 days. Results were obtained by observing the tubes for inhibition of
growth which was judged by a lack of opacity in tube.
The MICs were defined as the minimum concentrations of drugs that completely
inhibited the growth of the test organism.
Following drugs concentrations (g/ml) were used in the study:
ISO: 0.035, 0.07, 0.15, 0.3, 0.6, 1.2, 2.5, 5, 10, 20, 40, 80 and 160 g/ml
INH: 0.0125, 0.025, 0.05, 0.1, 0.2, 0.4, 0.8, 1.6, 3.2, and 6.4 g/ml
ETH: 0.15, 0.3, 0.6, 1.2, 2.5, 5, 10, 20, 40, and 80 g/ml
2.4 Determination of Minimum Bactericidal Concentration (MBC)
MBC pattern of
40 MDR strains and 20 susceptible strains of M. tuberculosis along
with standard strain of M. tuberculosis H37Rv was determined to ISO, INH and ETH by broth
dilution method (Heifets, 1991; Reddy, V. M., Nadadhur, G., Daneluzzi, D., Dimora, V. and
Gangadharam, P.R.J. 1995).
After 15 days of incubation for MIC determination of the drug, drug concentrations
higher than or same as those used to determine the MIC was selected. Those drug containing
tubes showing no turbidity were included in the study and made dilutions of
drug
concentrations to 10-3 to 10-4 in 10 ml quantity.
These dilutions were inoculated on sterile LJM slants in 0.1 ml quantity in duplicate.
Further slants were incubated at 370C for three weeks. Numbers of colony forming units (CFU)
were counted on LJM. Number of CFUs developed after incubation was compared with the
number of CFUs of originally inoculated culture. The lowest concentration of the drug that
killed 99.9% of organisms was considered the MBC of that drug.
Following drugs concentrations (g/ml) were used in the study:
ISO: 0.07,0.15, 0.3, 0.6, 1.2, 2.5, 5, 10, 20, 40, 80 and 160 g/ml
INH: 0.003,0.006,0.0125, 0.025, 0.05, 0.1, 0.2, 0.4, 0.8, 1.6, 3.2 and 6.4 g/ml
ETH: 0.035,0.07,0.15, 0.3, 0.6, 1.2, 2.5, 5, 10, 20, 40 and 80 g/ml
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
3. Results
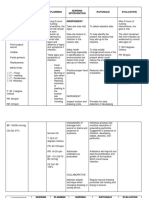
Table 3.1: MIC pattern of Mycolic acid inhibitors to MDR strains of M. tuberculosis in solid and
liquid media
INH
Geometric mean (GM)
MIC (g/ml)
Liquid
Solid media
media
0.29
1.21
ETH
15.94
2.51
2.5 to 40
0.3 to 5.0
ISO
5.76
1.62
1.2 to 20
0.3 to 5.0
Serial
No.
Mycolic acid
inhibitors
MIC Range
( g/ml)
Solid media
Liquid media
0.2 to 3.2
0.05 to 0.8
On solid media, Inhibitory activity of ISO was 4.76 times lower than activity of INH,
while it was 2.77 times higher than activity of ETH. MIC range was narrower for ISO than
ETH.In liquid media inhibitory activity of ISO was 5.59 times lower than the activity of INH,
while it was 1.55 times higher than activity of ETH.MIC rage was similar for ISO and ETH.
[Table 3.1]
Table 3.2: MIC pattern of Mycolic acid inhibitors to MDR strains of M .tuberculosis in solid and
liquid media in combination
Group
Mycolic acid
inhibitors
Geometric
mean MIC
(g/ml)
(+/-)SD
P value
Remark
Solid
media
Liquid Solid Liquid
media media media
INH
1.21
0.29
0.92
0.23
3.00E-
2.07E-
ISO
5.76
1.62
3.65
1.07
10
09
ISO
5.76
1.62
3.65
1.07
2.99E-
ETH
15.94
2.51
11.98
1.78
07
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
Solid
media
Liquid
media
Difference
is
significant
Difference
0.002
is
significant
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
INH
1.21
0.29
0.92
0.23
8.60E-
3.90E-
ETH
15.94
2.51
11.98
1.78
10
10
Difference
is
significant
Difference between MIC values between INH and ISO; ISO and ETH; INH and ETH to to MDR
strains of M .tuberculosis in solid and liquid media in combination were statistically significant .
[Table 3.2]
MIC distribution of MDR strains of M.tuberculosis in solid media
No. of strains ( cumulative %)
120
100
100
82.5
80
97.5
100
100
85
82.5
INH
75
ISO
60
55
55
55
40
ETH
32.5
32.5
20
10
2.5
0
0.2
0.4
0.6
2.5
7.5
7.5
25
25
12.5
12.5
0.8 1.2 1.6 2.5 3.2
Drug concentrations (mcg/ml)
25
10
20
40
Figure 1: MIC distribution of MDR strains of M.tuberculosis in solid media
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
MIC distribution of MDR strains of M.tuberculosis in liquid media
No. of strains ( cumulative %)
120
100
100
87.5
80
87.5
INH
67.5
60
57.5
100
95
70
ISO
57.5
47.5
40
ETH
37.5
20
17.5
7.5
0.05
5
0.1
0.2
17.5
0.3
0.4
0.6
0.8
Drug concentrations
1.2
2.5
Figure 2: MIC distribution of MDR strains of M.tuberculosis in liquid media
Table 3.3: MIC pattern of Mycolic acid inhibitors to susceptible strains of M. tuberculosis in
solid and liquid media
Serial
Mycolic acid
No.
inhibitors
Geometric mean MIC
MIC Range
(g/ml)
( g/ml)
Solid media
Liquid
media
Solid media
Liquid media
INH
0.08
0.02
0.025 to 0.1
0.012 to 0.05
ETH
3.5
0.54
1.2 to 10
0.3 to 2.5
ISO
1.07
0.50
0.3 to 2.5
0.3 to 2.5
In solid media inhibitory activity of ISO was13.38 times lower than the activity of INH,
while it was 3.27 times higher than activity of ETH.MIC rage was narrower for ISO than ETH.
In liquid media, Inhibitory activity of ISO was 25 times lower than activity of INH, while it was
1.08 times lower than activity of ETH. MIC range was similar for ISO than ETH. [Table 3.3]
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Table 3.4: MIC pattern of Mycolic acid inhibitors to susceptible strains of M. tuberculosis in
solid and liquid media in combination
Mycolic acid
Group
inhibitors
Geometric
mean MIC
(g/ml)
(+/-)SD
P value
Remark
INH
Solid Liquid Solid Liquid
media media media media
0.8
0.02
0.1777 0.01
Solid
media
Liquid
media
2.8E-14
0.00038
ISO
1.07
0.50
0.3830 0.52
ISO
0.08
0.50
0.1777 0.52
1.30E-
ETH
3.5
0.54
0.2728 0.51
25
INH
1.07
0.02
0.3830 0.01
4.11E-
ETH
3.5
0.54
0.2728 0.51
07
0.604
.00017
Difference is
significant
Difference is
significant
Difference is
significant
Difference between MIC values between INH and ISO; ISO and ETH; INH and ETH to
susceptible strains of M .tuberculosis in solid and liquid media in combination was statistically
significant . [Table 3.4]
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
10
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
no. of strains ( cumulative %)
120
MIC distribution of susceptible strains of M.tuberculosis in liquid
media
100
100
90
100
95
90
80
100
95
80
INH
60
ISO
55
50
40
ETH
40
20
15
15
0
0.012
0.025
0.05
0.15
0.3
0.6
1.2
2.5
Drug concentrations (mcg/ml)
Figure 3: MIC distribution of susceptible strains of M.tuberculosis in liquid media
Table 3.5: Comparison of MIC of Mycolic acid inhibitors to MDR and susceptible strains of M.
tuberculosis in solid media
Drugs
INH
ISO
ETH
Susceptible
GM MIC
(g/ml)
0.08
MDR
1.21
Susceptible
1.07
MDR
5.76
Susceptible
3.50
MDR
15.94
Strains
Ratio
15.13
3.39
4.55
(+/-)SD
0.03
0.92
1.11
3.65
2.46
11.98
P value
6.56E-07
3.50E-07
1.68E-05
Remark
Difference is
significant
Difference is
significant
Difference is
significant
MIC ratio of ISO was lowest when compared for susceptible and MDR strains followed by ETH
and INH in solid media. The difference between the MIC for each compound was statistically
significant.[Table 3.5]
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
11
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Table 3.6: Comparison of MIC of Mycolic acid inhibitors to MDR and susceptible strains of M.
tuberculosis in liquid media
Susceptible
GM MIC
(g/ml)
0.02
MDR
0.29
Susceptible
0.50
MDR
1.62
Susceptible
0.54
MDR
2.51
Drugs
INH
ISO
ETH
Strains
Ratio
14.5
3.24
4.65
(+/-)SD
0.014
0.233
0.52
1.066
0.511
1.776
P value
1.97E-06
3.14E-05
6.21E-06
Remark
Difference is
significant
Difference is
significant
Difference is
significant
MIC ratio of ISO was lowest when compared for susceptible and MDR strains followed by ETH
and INH in liquid media. The difference between the MIC for each compound was statistically
significant. [Table 3.6]
Table 3.7: Comparison of activity of INH, ISO and ETH in solid and liquid media
Drugs
INH
ISO
ETH
Broth
GM MIC
(g/ml)
0.20
Agar
0.82
Broth
1.24
Agar
4.15
Broth
1.83
Agar
11.66
Medium
Ratio
(+/-)SD
0.23
4.1
0.92
1.06
3.35
3.76
1.74
6.37
11.44
P value
1.21E-06
4.88E-08
9.96E-10
Remark
Difference is
significant
Difference is
significant
Difference is
significant
MIC ratio of ISO was lowest when compared in solid and liquid medium to M. tuberculosis
strains followed by INH and ETH. The difference between the MIC for each compound was
statistically significant.[Table 3.7]
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
12
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Table 3.8: MBC pattern Mycolic acid inhibitors to MDR strains of M. tuberculosis
Sr. No.
Mycolic acid inhibitors
Geometric mean MBC
(g/ml)
MBC Range (g/ml)
INH
0.36
0.1 to 1.6
ETH
6.41
1.2 to 10
ISO
18.63
5.0 to 40
Bactericidal activity of ISO was 51.75 times lower than the activity of INH and 2.9 times
lower than the activity of ETH.MBC range was wider for ISO than ETH. [Table 3.8]
Distribution of MBC of MDR strains of M.tuberculosis
No. of strains ( cumulative %)
120
100
87.5
80
95
95
100
100
100
87.5
INH
ISO
60
ETH
50
47.5
40
35
35
22.5
20
2.5
0
0.1
0.2
0.4
0.8
2.5
1.2 1.6 2.5
5
Drug concentrations
7.5
10
20
40
Figure 4: Distribution of MBC of MDR strains of M. tuberculosis
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
13
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Table 3.9: MBC pattern mycolic acid inhibitors to MDR strains of M. tuberculosisin
combination
Group
Mycolic acid
inhibitors
Geometric
mean MBC
(+/-) SD
P value
Remark
(g/ml)
INH
0.36
0.35
ISO
18.63
9.74
ISO
18.63
9.74
2
ETH
6.41
3.14
INH
0.36
0.35
3
ETH
6.41
9.58E-15
Difference is significant
4.30E-09
Difference is significant
8.42E-15
Difference is significant
3.14
Difference between MBC values between INH and ISO; ISO and ETH; INH and ETH to MDR
strains of M .tuberculosis in combination was statistically significant . [Table 3.9]
Table 3.10: MBC pattern mycolic acid inhibitors to susceptible strains of M. tuberculosis
Serial No.
Mycolic acid inhibitors
Geometric mean
MBC(g/ml)
MBC Range (g/ml)
INH
0.03
0.1 to 1.6
ETH
2.26
1.2 to 10
ISO
6.40
5.0 to 40
Bactericidal activity of ISO was 213 times lower than the activity of INH and 2.83 times lower
than the activity of ETH.MBC range was wider for ISO than ETH [Table 3.10]
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
14
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Distribution of MBC of susceptible strains of M.tuberculosis
No. of strains( cumulative %)
120
100
100
90
85
80
100
95
90
100
90
INH
ETH
65
60
55
45
40
ISO
40
25
20
5
0
0.012
0.025
0.05
0.1
0.6
1.2
2.5
10
20
Drug concentrations
Figure 5: Distribution of MBC of susceptible strains of M. tuberculosis
Table 3.11: MBC pattern mycolic acid inhibitors to susceptible strains of M. tuberculosis in
combination
Group Mycolic acid inhibitors Geometric mean MBC (+/-)SD
P value
Remark
INH
0.03
0.03
1
ISO
6.40
5.77
ISO
6.40
5.77
2
ETH
2.26
2.08
INH
0.03
0.03
3
ETH
2.26
2.08
9.24E-05
Difference is
significant
0.011
Difference is
significant
0.000126
Difference is
significant
Difference between MIC values between INH and ISO; ISO and ETH; INH and ETH to
susceptible strains of M .tuberculosis in solid and liquid media in combination was statistically
significant . [Table 3.11]
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
15
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Table 3.12: MIC/MBC Ratio
Mycolic acid
Serial no.
MDR strains
inhibitors
Susceptible strains
INH
1.24
1.5
ETH
2.55
4.18
ISO
11.5
11.85
Highest MIC/MBC ratio was shown by ISO followed by ETH and the INH[Table 3.12]
Table 3.13: Comparison of MBC of ISO against MDR and susceptible (s)strains of
M.tuberculosis
Drugs
Strains
S
Mean
Ratio
0.03
(+/-)SD
0.36
6.40
12
18.63
2.26
MDR
6.41
8.44E-05
Difference is significant
3.05E-06
Difference is significant
1.63E-06
Difference is significant
0.35
5.77
ISO
MDR
Remark
0.03
INH
MDR
P value
2.9
9.74
2.08
ETH
2.84
3.14
MBC ratio of ETH was lowest when compared for susceptible and MDR strains followed by ISO
and then INH in liquid media. The difference between the MBC for each compound was
statistically significant.[Table 3.13]
4. Discussion
MIC is the method used for evaluation of the antimicrobial activity of conventional and
experimental agents. The results obtained by these techniques can provide information on the
inhibitory (bacteriostatic) activity of an agent if the test is performed in a qualitative manner and
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
16
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
if inactivation of a drug in the medium is minimal, allowing the obtained MIC values to be
reasonably compared with the pharmacokinetic data (Andrews, 2001).
In present study, total 40 MDR and 20 susceptible strains of M. tuberculosis were
processed to determine in vitro inhibitory activity of ISO, INH and ETH in solid and liquid
media. Values obtained in the present study for MICs of INH and ETH in solid and liquid media
for MDR and susceptible strains of M tuberculosis are comparable with various studies (Heifets,
1991).
We reported potent anti-mycobacterial activity of ISO against all MDR and susceptible
strains of M. tuberculosis. They were susceptible in the range of 1 to 20 g/ml. MIC values for
susceptible strains were significantly lower than MDR strains of M. tuberculosis in solid media.
Many authors in the past have shown powerful inhibitory action of ISO on human species of
tubercle bacilli in vitro with minimum inhibitory concentration varying from 0.15 to 1.2 g/ml in
various media (Robinson, & Hunter, 1966).Another study showed MIC range of INH resistant
strains to be 0.25 to 2 mg/ml for ISO and 1.25 to 10 g/ml for ETH (Debarber, A. E., Mdluli, K.,
Basman, M. Bekkar, L. and Barry, C.E. (2000).
While in recent study it was reported that, ISO showed anti-mycobacterial activity
against all strains of M. tuberculosis resistant to major first-line drugs and they were susceptible
in the range of 1 to 10 mg/ml (Phetsuksiri et al., 1999). Another study showed MIC range of INH
resistant strains to be 0.25 to 2 mg/ml for ISO and 1.25 to 10 g/ml for ETH (Debarber, A. E.,
Mdluli, K., Basman, M. Bekkar, L. and Barry, C.E, 2000).We have reported the MIC range of
ISO from 0.3 to 20 g /ml
Our data particularly the MICs found in either in Dubos broth or 7H10 agar plates were
in agreement with other authors data on MICs found in other types of liquid and solid media
(Lord, 1966; Phetsuksiri et al., 1999). Some authors reported MIC range of ISO from 3.75 to 40
g/ml, they lie within the value of attainable serum concentrations (Lord, 1966).
These
variations in the MIC range against strains of M. tuberculosis might be due to the geographical
variations in the strains under study. The important point here is that ISO has potent
antimycobacterial activity against MDR strains of M. tuberculosis.
We have reported the MIC range of ISO from 0.3 to 20 g /ml in solid media, while in
liquid media MIC range was 0.3to 5 g/ml for MDR and susceptible strains of M. tuberculosis.
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
17
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
ISO was significantly more active on susceptible strains than MDR strains of M. tuberculosis in
solid and liquid media .These variations in MIC values for ISO in solid media and liquid media
could be due the use of different methodologies to determine MIC and the type of media used for
it. The inhibitory action of ISO on MDR and susceptible strains of M. tuberculosis in liquid
media seems to be significantly higher than in solid media. The difference between broth and
agar determined MICs was related to the bactericidal potency of the drug in the type of medium
used. This difference was minimal for ISO and larger for ETH, with INH in the intermediate
position.
Some studies suggest that it is more favourable to use solid media when testing ISO. A
fluid medium is not convenient for the examination of sensitivity because of a great asymmetry
of the distribution of the MIC (Lord, 1966). Our study reported MIC of ISO for M. tuberculosis
H37Rv strain to be 1.5g/ml. While MIC value of ISO for M. tuberculosis H37Rv strain was in
the range of 1.0 to 2.5 g/ml compared to published values of 0.02 to 0.2 g/ml to INH & 5 to
10 mg/ml for ETH (Lord, 1966).
Our study showed that inhibitory activity of ISO was higher than activity of ETH in solid
media for MDR and susceptible strains of M. tuberculosis. While it was almost similar to the
activity of ETH in liquid media for susceptible strains of M. tuberculosis. No cross resistance
was observed between ISO and ETH for strains of M. tuberculosis. While it is reported that cross
resistance between Thiacetazone, ISO and ETH exist but not in 100 % of the cases (Gallen,
1970). With regard to the cross resistance between ISO and ETH study in the past, shows there
seems to be a difference between strains with primary resistance and strains with acquired
resistance to these drugs. None of the strains with primary resistance showed cross-resistance,
while strains with acquired resistance to ETH after treatment with this drug, showed crossresistance to ISO that was not administered (Meissner & Stottmeier, 1965). Experiments have
shown that the tuberculostatic activity of ISO clearly exceeds that of PAS and is comparable
with that of ETH (Hekking & De Voogd, 1970).
ISO, one of the second line drugs proved to be very useful in the treatment of pulmonary
TB, in the past, particularly as a substitute for PAS, when later was not tolerated for some
reason. In the case of resistance to one or several first line drugs, too, it is advisable to use ISO in
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
18
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
combination with other second line drugs. The tuberculostatic effect of ISO slightly exceeds that
of PAS, while its toxicity is less than that of PAS (Hekking & De Voogd, 1970).
The therapeutically efficacy of ISO, both in vitro and in vivo, has been clearly
demonstrated by some studies (Robinson & Hunter, 1966).Thus the results of the MIC studies
show that ISO is capable of inhibiting the growth of various Mycobacteria within a narrow range
of low concentrations. The suggestion is that ISO may be suitable for the treatment of TB,
particularly multi-drug resistant kind.
In our study we tested total 40 MDR and 20 susceptible strains of M. tuberculosis to
determine MBC of INH, ETH and ISO. Amongst three antituberculosis drugs, INH showed
highest bactericidal activity against M. tuberculosis strains followed by ETH. While, ISO
showed lowest bactericidal activity. ISO was found to be significantly more bactericidal to
susceptible strains than MDR strains of M. tuberculosis like INH and ETH. By describing the
results of the MIC and MBC determinations, categorization of a drug is avoided as bactericidal
and bacteriostatic. It can be assumed that it is most likely that the drug whose MBC is within the
concentration achievable in blood or tissue, will produce a killing effect against the bacteria
actively multiplying in vivo.
Still, such a drug may not be able to kill some parts of the bacterial populations in vivo,
particularly the bacteria in a semi-dormant or dormant state or multiplying within macrophages.
On the other hand, it is difficult to imagine that the drug whose MBC is very much greater than
its achievable concentration would produce any substantial killing effect in vivo. Conclusions,
about the bactericidal potency of certain drugs, derived from in vivo observations, sometimes
contradict this logic. In the literature on tuberculosis, the sterilizing activity of a drug in vivo (in
patients or in mice) is often interpreted as its bactericidal activity. The sterilizing activity of a
drug measures the duration of treatment and is therefore crucial in the design of short -course
regimen .The early bactericidal activity of drug has, however, little bearing on its use in therapy,
except perhaps as an indication of the period during which a patient may be considered to be
infectious to others.
It can be concluded that despite similarities in mode of action of INH, ETH and ISO, they
showed different activity in vitro, especially the bactericidal activity. The difference between
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
19
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
broth and agar determined MICs was related to the bactericidal potency of the drug. This
variation could be due the use of different methodologies to determine MIC.
The MBC/MIC ratio is the usual standard for expression of bactericidal potency. This
ratio can be used to estimate the probability of a bactericidal effect upon the patients strain if the
degree its susceptibility has been expressed as the MIC (Mitchison, 1979).
The high bactericidal activity of INH was suggested in several publications
(Middlebrook, 1952). Though the results usually have not been described in MBC values or in
MBC MIC ratios, many authors have reported that INH kills most of the bacterial population at
very low concentrations, equivalent to the MIC or only slightly higher. Same observations were
made in the present study. ETH has often been considered primarily a bacteriostatic drug due to
its low sterilizing activity in vivo, though tuberculocidal concentrations can be reached with
doses applicable to animals and man (Offen, 1988). MBC MIC ratios for ETH were found to be
in the range of 3 to 4.5 in the present study. Similar observations were made in other studies
(Offen, 1988). These data confirms that ETH can produce a bactericidal effect (99%) killing in
concentrations close to those attainable in vivo, especially when higher dosages are administered.
Therefore, despite the relatively low sterilizing activity of ETH in vivo, this drug should not be
labelled as bacteriostatic only.
MBC MIC ratio was found to be high for ISO indicating low bactericidal activity of this
drug. This ratio was similar for susceptible and MDR strains of M. tuberculosis. These data show
that ISO cannot produce 99% killing in concentrations close to those attainable in vivo,
especially when lower doses are administered. These findings can be correlated by past clinical
studies, in which ISO was found to be more bacteriostatic than bactericidal drug. One study
reported ISO as one of the second line drugs, proved to be useful in the treatment of pulmonary
TB, particularly as a substitute for PAS, when later was not tolerated for some reason (Hekking
& Voogd, 1970). It was advisable in the case of resistance to one or several first line drugs, too,
to use ISO in combination with other second line drugs.
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
20
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
5. Conclusion
This study reports potent anti-mycobacterial activity of ISO against MDR and susceptible
strains of M. tuberculosis. They were susceptible in the range of 1 to 20 g/ml and 0.3 to 5 g/ml
in solid and liquid medium respectively.. There was significant difference in MICs of MDR
strains and susceptible strains of M. tuberculosis in solid and liquid media. Amongst three
antituberculosis drugs, INH showed highest bactericidal activity against M. tuberculosis strains
followed by ETH. While ISO showed lowest bactericidal activity. ISO showed significantly
lower bactericidal activity against MDR strains than susceptible strains of M. tuberculosis.
.Following conclusions can be drawn from these studies. Inhibitory activity of ISO is better than
ETH in solid media and it is far better for susceptible strains in comparison to ETH. Inhibitory
activity of ISO was similar to ETH for susceptible strains of M. tuberculosis in liquid media. No
cross-resistance between ISO, INH and ETH was observed. Though inhibitory activity of ISO
seems to be comparable to ETH, it is more of a bacteriostatic drug than bactericidal. ISO showed
significantly lower bactericidal activity against MDR strains than susceptible strains of M.
tuberculosis. .Despite similarities in mode of action of INH, ETH and ISO, they showed different
activity in vitro, especially the bactericidal activity.
REFERENCES
Andrews, M. J. (2001). Determination of minimum inhibitory concentrations Suppl.S1. Journal
of Antimicrobial Chemotherapy, 46, 5-16.
Balows, A., Hausler, W., Herrmann, K., Isenberg, H., & Shadomy, H. (1975) Paper presented at
the American Society For Microbiology, Washington DC.
Brennan, P. J. (2002). Plenary lecture, Current developments in drug Discovery for Tuberculosis.
Targeting Cell wall Biogenesis. Introduction symposium on current developments in drug
discovery for tuberculosis, 5-6.
Chopra, P., Meena, L., & Singh, Y. (2003). New drug targets for Mycobacterium tuberculosis.
Indian Journal of Medical Research, 117, 1-9.
Cruikshank, R., Duguid, J. P., & Swain, R. H. A. (1968). In Medical Microbiology (Vol. 53).
Edinburgh and London: The ELBS and ES Livington Ltd.
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
21
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
David, H. L., Rastogi, N., Clavel-Seres, S., & Clement, F. (1988). Alterations on the outer wall
architecture caused by the inhibition of mycoside C biosynthesis in Mycobacterium
avium. Current microbiology, 17, 61-68.
Debarber, A. E., Mdluli, K., Basman, M. Bekkar, L. and Barry, C.E. (2000):. , U. S. A. 15 (97)
17: 96779682. (2000). Ethionamide activation and sensitivity in MDR M. tuberculosis.
Proc Natl Acad Sci, 15(97)(17), 9677- 9682.
Diel, R., Loddenkemper, R., Zellweger, J., Sotgiu, G., DAmbrosio, L., & Centis, R. (2013). Old
ideas to innovate TB control: preventive treatment to achieve elimination. Eur. Respir.,
42, 785801.
Gallen, C. (1970). Isoxyl: a review of the results of its use over a five-year period in the
tuberculosis field service of a large urban area. Antibitics and Chemotherapy, 16(2),13948
Hawkins, J. E., Wallace Jr, R. J., & Brown, B. A. (1991). Antibacterial susceptibility tests:
Mycobacteria. In Manual of Clinical Microbiology, 5th Edn, Balows A, Hausler WJ,
Herrmann KL, Isenberg HD and Shadomy HJ, Eds. Am Society For Microbilogy,
Washington DC. 1138-52.
Heifets, L. (1991). Drug susceptibility in the chemotherapy of mycobacterial infections. Boca
Raton, Fla: CRC Press.
Hekking, A., & De Voogd, K. (1970). Clinical Data on 4-4 Diisoamyloxythiocarbanilide
(Isoxyl). Antibitics and Chemotherapy, 16(2),128-35
Lienhardt, C. (2012). New drugs for the treatment of tuberculosis: needs, challenges, promise
and prospects for the future. J. Infect. Dis. , 205, S241S249.
Lord. (1966). Sensitivity to Thiocarlide and thiacetazone of far eastern strains of M.tuberculosis.
Tubercle, 47, 400.
Matlola, N. M., Steel, H. C., & Anderson, R. (2001). Antimycobacterial action of B4128, a novel
tetramethylpiperidyl-substituted phenazine. J. of Antimicrob. Chemoth., 47, 199-202.
Meissner, G., & Stottmeier, D. (1965). Die Empfindlichkeit der Mycobakterien fr 4-4Diisoamyloxythiocarbanilid (Isoxyl) und ihre Bestimmung auf Lwenstein-JensenNhrboden. Beitrge zur Klinik und Erforschung der Tuberkulose und der
Lungenkrankheiten, 130(4), 289-295.
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
22
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Middlebrook, G. (1952). Sterilization of tubercle bacilli by isonicotinic acid hydrazine and the
incidence of variants resistant to the drug in vitro. Am Rev Tuberc, 65, 765.
Mitchison, D. (1979). Basic mechanisms of chemotherapy. CHEST Journal, 76(6_Supplement),
771-781.
Mitra, P. P. (2012). Drug discovery in tuberculosis: a molecular approach. Indian J. Tuberc, 59,
194206.
Offen, H. (1988). Thiomides:ethionamide , protionamide,. In K. Bartmann (Ed.),
Antituberculosis Drugs (pp. 167). Berlin: Springer Verlg.
Phetsuksiri, B., Baulard, A. R., Cooper, A. M., Minnikin, D. E., Douglas, J. D., Besra, G. S., &
Brennan, P. J. (1999). Antimycobacterial activities of isoxyl and new derivatives through
the inhibition of mycolic acid synthesis. Antimicrobial agents and chemotherapy, 43(5),
1042-1051.
Raviglione, M., Marais, B., Floyd, K., Lonroth, K., Getahun, H., & Migliori, G. B. (2012).
Scaling up interventions to achieve global tuberculosis control: progress and new
developments. Lancet, 379, 19021913.
Reddy, V. M., Nadadhur, G., Daneluzzi, D., Dimora, V. and Gangadharam, P.R.J. (1995).
Antimycobacterial activity of new Rifamycin derivative 3-(4-cinnamylpiperazinyl
Iminomethyl Rifamycin SV (T9). Antimicrob Agents Chemother, 39(10), 2320-2324.
Robinson, O., & Hunter, P. A. (1966). Absorption and excretion studies with thiocarlide (4 4diisoamyloxythiocarbanilide) in man. Tubercle, 47(2), 207-213.
Schmid, C. (1970). Clinical experience in cases of primary tuberculosis with tuberculostaticum
isixyl. Antibiot chemother, 16, 108-116.
Siddiqui, S. H., Libonati, J.P. and Middlebrook, G. (1981). Evaluation of a rapid radiometric
method for drug susceptibility testing of Mycobacterium tuberculosis. J Clin Microbiol,
13, 908-912.
Tischer, R. (1966). Monotherapie mit isoxyl/DAT bei tuberculose-asylierungfallen. Prax
Pnemoniol: , 202.
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
23
LIFE: International Journal of Health and Life-Sciences
ISSN 2454-5872
Tomioka, H., Saito, H., Fujii, K., Sato, K., & Hidaka, T. (1993). In vitro antimicrobial activity of
benzoxazinorifamycin, KRM-1648, against Mycobacterium avium complex, determined
by the radiometric method. Antimicrobial agents and chemotherapy, 37(1), 67-70.
Urbancik, B. (1970). Clinical experiences with thiocarlide ( Isoxyl). Antibiot Chemother, 16,
117-123.
Vestal, A. L. (1975). Procedures for the isolation and identification of Mycobacteria. Atlanta
center for disease control.
Winder, F. G. (1982). Mode of action of the antimycobacterial agents and associated aspects of
the molecular biology of the mycobacteria. The biology of the mycobacteria, 1, 353-438.
2015 The author and GRDS Publishing. All rights reserved.
Available Online at: http://grdspublishing.org/LIFE/life.html
24
S-ar putea să vă placă și
- Resolving A Realistic Middle Ground Towards The Sustainability Transition in The Global Political and Economic Landscape: A Comprehensive Review On Green CapitalismDocument29 paginiResolving A Realistic Middle Ground Towards The Sustainability Transition in The Global Political and Economic Landscape: A Comprehensive Review On Green CapitalismGlobal Research and Development ServicesÎncă nu există evaluări
- The Ethical Perception On Utang Na Loob As Basis of Voter's ChoiceDocument18 paginiThe Ethical Perception On Utang Na Loob As Basis of Voter's ChoiceGlobal Research and Development Services100% (1)
- Analyzing The Relationship Between Industrial Policy and Entrepreneurial EcosystemDocument13 paginiAnalyzing The Relationship Between Industrial Policy and Entrepreneurial EcosystemGlobal Research and Development ServicesÎncă nu există evaluări
- Examine The Effects of Goods and Services Tax (GST) and Its Compliance: Reference To Sierra LeoneDocument18 paginiExamine The Effects of Goods and Services Tax (GST) and Its Compliance: Reference To Sierra LeoneGlobal Research and Development ServicesÎncă nu există evaluări
- Interpretation and Justification of Rules For Managers in Business Organizations: A Professional Ethics PerspectiveDocument10 paginiInterpretation and Justification of Rules For Managers in Business Organizations: A Professional Ethics PerspectiveGlobal Research and Development ServicesÎncă nu există evaluări
- Teacher Educators' Perceptions of Utilizing Mobile Apps For English Learning in Secondary EducationDocument28 paginiTeacher Educators' Perceptions of Utilizing Mobile Apps For English Learning in Secondary EducationGlobal Research and Development ServicesÎncă nu există evaluări
- Perceived Self-Efficacy and Academic Performance of Stem Senior High School StudentsDocument13 paginiPerceived Self-Efficacy and Academic Performance of Stem Senior High School StudentsGlobal Research and Development ServicesÎncă nu există evaluări
- Implementation of Biorhythm Graph With Trigonometric Functions Using PythonDocument8 paginiImplementation of Biorhythm Graph With Trigonometric Functions Using PythonGlobal Research and Development ServicesÎncă nu există evaluări
- Potential Factors Influence Failure of The Village-Owned Business: The Entity Village Autonomy of Indonesian Government's ProgramDocument12 paginiPotential Factors Influence Failure of The Village-Owned Business: The Entity Village Autonomy of Indonesian Government's ProgramGlobal Research and Development ServicesÎncă nu există evaluări
- Challenges in The Implementation of Schoolbased Management of Developing Schools: Basis For A Compliance FrameworkDocument14 paginiChallenges in The Implementation of Schoolbased Management of Developing Schools: Basis For A Compliance FrameworkGlobal Research and Development ServicesÎncă nu există evaluări
- Effect of Metacognitive Intervention Strategies in Enhancing Resilience Among Pre-Service TeachersDocument12 paginiEffect of Metacognitive Intervention Strategies in Enhancing Resilience Among Pre-Service TeachersGlobal Research and Development ServicesÎncă nu există evaluări
- Design and Implementation of An Arabic Braille Self-Learning WebsiteDocument17 paginiDesign and Implementation of An Arabic Braille Self-Learning WebsiteGlobal Research and Development ServicesÎncă nu există evaluări
- Loss Analysis in Bread Production Process Using Material Flow Cost Accounting TechniqueDocument16 paginiLoss Analysis in Bread Production Process Using Material Flow Cost Accounting TechniqueGlobal Research and Development ServicesÎncă nu există evaluări
- Influence of Iot On Smart LogisticsDocument12 paginiInfluence of Iot On Smart LogisticsGlobal Research and Development ServicesÎncă nu există evaluări
- Using Collaborative Web-Based Maps To Promote Geography Teaching and LearningDocument13 paginiUsing Collaborative Web-Based Maps To Promote Geography Teaching and LearningGlobal Research and Development ServicesÎncă nu există evaluări
- Refining The English Syntax Course For Undergraduate English Language Students With Digital TechnologiesDocument19 paginiRefining The English Syntax Course For Undergraduate English Language Students With Digital TechnologiesGlobal Research and Development ServicesÎncă nu există evaluări
- Bank-Specific and Macroeconomic Determinants of Banks Liquidity in Southeast AsiaDocument18 paginiBank-Specific and Macroeconomic Determinants of Banks Liquidity in Southeast AsiaGlobal Research and Development ServicesÎncă nu există evaluări
- The Development of Nursing Care Model in Patients With Total Knee Replacement Reconstructive SurgeryDocument17 paginiThe Development of Nursing Care Model in Patients With Total Knee Replacement Reconstructive SurgeryGlobal Research and Development ServicesÎncă nu există evaluări
- How Bi-Lingual Fathers Support Their Children To Learn Languages at HomeDocument35 paginiHow Bi-Lingual Fathers Support Their Children To Learn Languages at HomeGlobal Research and Development ServicesÎncă nu există evaluări
- Study of Urban Heat Island in Yogyakarta City Using Local Climate Zone ApproachDocument17 paginiStudy of Urban Heat Island in Yogyakarta City Using Local Climate Zone ApproachGlobal Research and Development ServicesÎncă nu există evaluări
- Development of A Topical Gel Containing A Dipeptidyl Peptidase-4 Inhibitor For Wound Healing ApplicationsDocument15 paginiDevelopment of A Topical Gel Containing A Dipeptidyl Peptidase-4 Inhibitor For Wound Healing ApplicationsGlobal Research and Development ServicesÎncă nu există evaluări
- "Higher, Faster, Stronger": Championing Classroom TeachingDocument13 pagini"Higher, Faster, Stronger": Championing Classroom TeachingGlobal Research and Development ServicesÎncă nu există evaluări
- Work-Related Problems and Performance Level of Senior High School TeachersDocument22 paginiWork-Related Problems and Performance Level of Senior High School TeachersGlobal Research and Development ServicesÎncă nu există evaluări
- Global E-Learning and Experiential Opportunities For Programs and StudentsDocument12 paginiGlobal E-Learning and Experiential Opportunities For Programs and StudentsGlobal Research and Development ServicesÎncă nu există evaluări
- Investigating The Effects of Social Media On The Well-Being of TeenagersDocument18 paginiInvestigating The Effects of Social Media On The Well-Being of TeenagersGlobal Research and Development ServicesÎncă nu există evaluări
- The Relationship of Teaching Clarity and Student Academic Motivation in Online ClassesDocument9 paginiThe Relationship of Teaching Clarity and Student Academic Motivation in Online ClassesGlobal Research and Development ServicesÎncă nu există evaluări
- The Hijiri Calendar and Its Conformance With The Gregorain Calendar by Mathematical CalculationsDocument19 paginiThe Hijiri Calendar and Its Conformance With The Gregorain Calendar by Mathematical CalculationsGlobal Research and Development ServicesÎncă nu există evaluări
- Thai and Non-Thai Instructors' Perspectives On Peer Feedback Activities in English Oral PresentationsDocument22 paginiThai and Non-Thai Instructors' Perspectives On Peer Feedback Activities in English Oral PresentationsGlobal Research and Development ServicesÎncă nu există evaluări
- Review of Vibration-Based Surface & Terrain Classification For Wheel-Based Robot in Palm Oil PlantationDocument14 paginiReview of Vibration-Based Surface & Terrain Classification For Wheel-Based Robot in Palm Oil PlantationGlobal Research and Development ServicesÎncă nu există evaluări
- Building A Scale of Competence To Apply Interdisciplinary Integrated Knowledge Into Practice For StudentDocument10 paginiBuilding A Scale of Competence To Apply Interdisciplinary Integrated Knowledge Into Practice For StudentGlobal Research and Development ServicesÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Cell Organelles Worksheet-PrintDocument2 paginiCell Organelles Worksheet-PrintmuraliMuÎncă nu există evaluări
- Nutrition 1Document5 paginiNutrition 1Christine PunsalanÎncă nu există evaluări
- MCQDocument20 paginiMCQanuj sharma100% (2)
- Portfolio Clinical Case Study 2Document29 paginiPortfolio Clinical Case Study 2api-277136509Încă nu există evaluări
- Cell TheoryDocument31 paginiCell TheoryMarc Ian Young100% (1)
- CSEC Study Guide - March 1, 2011Document11 paginiCSEC Study Guide - March 1, 2011ChantelleMorrisonÎncă nu există evaluări
- Med-Surg Practice Test 100Document73 paginiMed-Surg Practice Test 100Muyan Bearneza100% (1)
- NEET GT-5 SolutionsDocument12 paginiNEET GT-5 Solutionsabcxyz7799Încă nu există evaluări
- ICMR Award 2017-18 Citation Booklet PDFDocument30 paginiICMR Award 2017-18 Citation Booklet PDFHarshendra GuduruÎncă nu există evaluări
- What Is Sclerosis of The LiverDocument2 paginiWhat Is Sclerosis of The LiverLuinel PlasenciaÎncă nu există evaluări
- Metabolic EngineeringDocument9 paginiMetabolic EngineeringArup ChakrabortyÎncă nu există evaluări
- General Biology Last Set of ActivitiesDocument2 paginiGeneral Biology Last Set of ActivitiesAubrey GuilaranÎncă nu există evaluări
- FTPDocument16 paginiFTPGia AisaÎncă nu există evaluări
- BINUS University: Bioinformatics Road MapDocument16 paginiBINUS University: Bioinformatics Road MapIndonesian Journal of CancerÎncă nu există evaluări
- CO2 Liquefied Gas MSDSDocument9 paginiCO2 Liquefied Gas MSDSsalcabes100% (1)
- Fallout TTRPG v2.0 PDFDocument179 paginiFallout TTRPG v2.0 PDFJavontay PeoplesÎncă nu există evaluări
- Biomedical Engineering Presentation With VideoDocument13 paginiBiomedical Engineering Presentation With VideoJi Hun YangÎncă nu există evaluări
- Unit 3 Different Stages of Human Development: 3.0 ObjectivesDocument27 paginiUnit 3 Different Stages of Human Development: 3.0 ObjectivesLucienneÎncă nu există evaluări
- Quiz BankDocument12 paginiQuiz Banknadim1241335Încă nu există evaluări
- Antiseptics and DisinfectantsDocument28 paginiAntiseptics and DisinfectantszaydeeeeÎncă nu există evaluări
- 041 - Endocrinology Physiology) Antidiuretic Hormone (ADH)Document3 pagini041 - Endocrinology Physiology) Antidiuretic Hormone (ADH)یوسف رمضان100% (1)
- General Biology Modules 1 3Document36 paginiGeneral Biology Modules 1 3Glen MillarÎncă nu există evaluări
- NCP - JaundiceDocument5 paginiNCP - JaundiceQueen Shine0% (1)
- CancerDocument228 paginiCancerCrystal Grace100% (1)
- Medical TechnologistDocument2 paginiMedical Technologistapi-329932534Încă nu există evaluări
- I Am Joes Cell Article and QuestionsDocument5 paginiI Am Joes Cell Article and Questionsapi-263230840Încă nu există evaluări
- Nyas12203Becoming Conscious The Science of MindfulnessDocument18 paginiNyas12203Becoming Conscious The Science of MindfulnesscgrossÎncă nu există evaluări
- Panic Disorder - Etiology & Clinical FeaturesDocument49 paginiPanic Disorder - Etiology & Clinical Featuresdrkadiyala2Încă nu există evaluări
- X-Gal Manual - 5prime - 1044374 - 032007Document8 paginiX-Gal Manual - 5prime - 1044374 - 032007Miguel Montero VazquezÎncă nu există evaluări
- Msds HCL 0,1 NDocument6 paginiMsds HCL 0,1 NRinie Aeryn Nayndine'netzzÎncă nu există evaluări