Documente Academic
Documente Profesional
Documente Cultură
Comparison of Affirm VPIII and Papanicolaou Tests
Încărcat de
Anonymous owTPhxMKDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Comparison of Affirm VPIII and Papanicolaou Tests
Încărcat de
Anonymous owTPhxMKDrepturi de autor:
Formate disponibile
Anatomic Pathology / Molecular Testing of Infectious Vaginitis
Comparison of Affirm VPIII and Papanicolaou Tests
in the Detection of Infectious Vaginitis
Angelique W. Levi, MD, Malini Harigopal, MD, Pei Hui, MD, PhD, Kevin Schofield, CT(ASCP),
and David C. Chhieng, MD, MBA, MSHI, MA (Hon)
Key Words: Molecular diagnostics; Cytopathology; Infectious disease; Candida species; Trichomonas vaginalis; Gardnerella vaginalis
CME/SAM
DOI: 10.1309/AJCP7TBN5VZUGLZU
Upon completion of this activity you will be able to:
describe the Affirm VPIII test for infectious vaginitis.
list the preanalytic requirements for optimal performance of Affirm
VPIII testing for infectious vaginitis.
summarize the microbiology and pathology of infectious vaginitis.
Abstract
To compare the Affirm VPIII molecular test
(Becton Dickinson, Burlington, NC) with morphologic
identification used in routine Papanicolaou (Pap) test
screening in the detection and identification of Candida
species, Trichomonas vaginalis, and Gardnerella
vaginalis, we identified 431 cases with a concomitant
Pap test and Affirm VPIII assay performed from the
archives of a large academic institution. The study
population consisted of women ranging in age from 17
to 79 years (mean and median ages, 33 and 31 years,
respectively). With a routine Pap test, 60 patients
(13.9%) were found to have bacterial vaginosis, 60
(13.9%) candidiasis, and 3 (0.7%) Trichomonas
infection. With the Affirm VPIII assay, 183 (42.5%)
patients tested positive for G vaginalis, 70 (16.2%)
positive for Candida species, and 10 (2.3%) positive
for T vaginalis. The differences were statistically
significant. The results demonstrate that our patient
population had a high incidence of bacterial vaginosis/
Candida vaginitis; however, the Affirm VPIII was a
more sensitive diagnostic test for the detection and
identification of all 3 organisms compared with the Pap
test.
442
442
Am J Clin Pathol 2011;135:442-447
DOI: 10.1309/AJCP7TBN5VZUGLZU
The ASCP is accredited by the Accreditation Council for Continuing
Medical Education to provide continuing medical education for physicians.
The ASCP designates this educational activity for a maximum of 1 AMA PRA
Category 1 Credit per article. This activity qualifies as an American Board
of Pathology Maintenance of Certification Part II Self-Assessment Module.
The authors of this article and the planning committee members and staff
have no relevant financial relationships with commercial interests to disclose.
Questions appear on p 479. Exam is located at www.ascp.org/ajcpcme.
Infectious vaginitis is one of the most common
womens health care problems in the United States.1 The
3 leading microbial agents that are responsible for 90%
of infectious vaginitis are the organisms causing bacterial
vaginosis (BV), Candida species, and Trichomonas vaginalis.2 Although BV is characterized by a mixed infection
of anaerobic bacteria, Gardnerella vaginalis is considered
one of the major bacteria causing this infection.3 Optimal
treatment relies on the correct identification of these
organisms.
Clinical diagnosis of infectious vaginitis relies on
physical examination and a number of tests, such as microscopic examination, pH testing of vaginal fluid, and potassium hydroxide (KOH) amine odor test, performed at the
point of care. However, such tests are often time-consuming
and somewhat subjective. The Papanicolaou (Pap) test has
become a routine procedure for women at their annual
gynecologic visit because of its success in the prevention
of cervical cancer and precursor lesions. In addition to its
primary benefit as a cancer screening test, other benefits of
the Pap test include the detection of cervicovaginal microorganisms. However, the use of Pap tests to diagnose infectious vaginitis remains controversial.4,5
Recently, a molecular test, Affirm VPIII assay (Becton
Dickinson, Burlington, NC) to detect and specifically identify Candida species, G vaginalis, and T vaginalis from
vaginal fluid specimens has become commercially available. Preliminary results are promising.6-9 The objective
of this study was to compare the Affirm VPIII molecular
test with morphologic identification used in routine Pap
test screening in the detection and identification of these
3 organisms.
American Society for Clinical Pathology
Anatomic Pathology / Original Article
Materials and Methods
Patients who had a Pap test and concomitant Affirm VPIII
molecular testing between August 2008 and March 2009 were
included in this institutional-approved study. Patients who had
Affirm VPIII molecular testing not accompanied by a Pap test
were excluded from the study. The specimens were submitted
by a dozen community-based gynecologists.
All Pap tests were liquid-based preparations; 20% were
ThinPrep (Hologic, Marlboro, MA), and the remaining 80%
were SurePath (Becton Dickinson). The Pap tests were not
initially identified as part of a study because the cytotechnologists and cytopathologists were blinded to the results of the
molecular testing. A diagnosis of BV was made based on the
presence of the following 3 findings: a filmy background of
small coccobacilli, individual squamous cells coated with a
layer of coccobacilli along the cell membranes (so-called clue
cells), and conspicuous absence of lactobacilli10 Image 1. A
diagnosis of Candida infection was made by the identification
of yeast and pseudohyphae Image 2, whereas a diagnosis
of Trichomonas infection was made by the identification of
15- to 30-m, pear-shaped structures with a centrally located
nucleus Image 3.
The samples for the Affirm VPIII molecular test were
collected from the posterior fornix and side walls of the
vagina using a sterile swab. The swab was then placed into
an inactivation medium provided by the vendor (Becton
Dickinson). The medium is designed to preserve the nucleic
acid of microorganisms during specimen transport at room
temperature for up to 72 hours.
Image 1 Individual squamous cells coated with a layer of
coccobacilli along the cell membranes (so-called clue cells)
and conspicuous absence of lactobacilli characteristic of
bacterial vaginosis (Papanicolaou, 400).
The swabs were then tested using the Affirm VPIII
assay on the BD MicroProbe Processor (Becton Dickinson)
according to the manufacturers recommendations. The test
is based on the principle of nucleic acid hybridization in
which complementary nucleic acid strands align to form specific, double-stranded complexes called hybrids. The system
uses 2 distinct single-stranded probes that are complementary to unique genetic sequences of each target organism,
a capture probe, and a color-development probe. The capture probe is immobilized on a bead embedded in a Probe
Analysis Card (Becton Dickinson). The Probe Analysis
Card contains a separate bead for each target organism.
The color-development probes are contained in a multiwell
reagent cassette.
The assay consists of the following 3 steps: denaturing
of the samples to release each target organisms genetically unique nuclei acids, automated assay processing, and
recording of the results after 30 minutes. The assay includes
positive and negative controls on each Probe Analysis Card,
which are tested simultaneously with each patient sample.
After completion of molecular testing, the results of the
Affirm VPIII assay were visually observed and recorded
Image 4.
Pap tests with results that were discrepant from those of
the Affirm VPIII were manually rescreened by a cytotechnologist who was blinded to the results of the original Pap
test interpretation and the molecular test results. Statistical
analysis was performed by using the 2 test and Fisher exact
test. Statistical significance was set at a level of .05 or less.
Image 2 Pseudohyphae characteristic of Candida species
formed by elongated budding hyphae with constrictions along
their length (Papanicolaou, 400).
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:442-447
443
DOI: 10.1309/AJCP7TBN5VZUGLZU
443
443
Levi et al / Molecular Testing of Infectious Vaginitis
Image 3 Trichomonas vaginalis (Papanicolaou, 400). Pearshaped, 15- to 30-m structures with a centrally located
nucleus and eosinophilic cytoplasmic granules. Leptothrix
may be seen in association with Trichomonas.
Image 4 Affirm VPIII Probe Analysis Card for 2 patient
samples. The Probe Analysis Card on top is visually interpreted
as positive for Candida; the Probe Analysis Card on the bottom
is positive for Gardnerella. Each Probe Card includes positive
and negative controls for each patient sample.
We used the statistic to evaluate chance-corrected agreement between the Pap test and the Affirm VPIII assay. A
value of 0 indicates that the observed agreement is the same
as expected by chance, whereas a value of 1 indicates
perfect agreement. The values between 0 and 1 represent the
various extents of agreement as follows: a value of less than
0.2 indicates poor agreement; 0.21 to 0.6, fair to moderate
agreement; 0.61 to 0.8, good agreement; and 0.81 to 1.0,
excellent agreement.11
positive for Gardnerella and Trichomonas. One case was
positive for all 3 organisms with the Affirm VPIII assay.
Coinfection by 2 or more organisms was noted in only 5
cases based on Pap test evaluation. Of the 5 cases, 4 had
BV and candidiasis, and 1 had candidiasis and Trichomonas
infection. No cases were found to have all 3 organisms using
the Pap test.
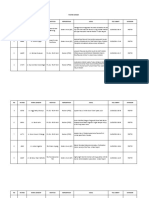
Of the 431 cases with Pap and Affirm VPIII test results,
154 had discrepant cytologic and molecular test results with
regard to the detection and identification of 1 or more of the
3 organisms. Among these 154 discrepant cases, 136 had a
positive molecular test result but a negative cytologic result.
Among the latter, the Affirm VPIII identified 127 cases of
Gardnerella infection, 25 of candidiasis, and 7 of trichomoniasis. On rescreening of the Pap slides, BV was identified in
41 cases, candidiasis in 8, and trichomoniasis in 3 that were
missed by initial cytologic screening.
There were 18 cases in which the Pap tests reported the
presence of organisms, including 13 cases of Candida, 4 of
BV, and 1 of Trichomonas, but the corresponding molecular test results were negative. On rescreening, 8 cases of
candidiasis and 2 of BV were confirmed on the Pap tests.
The case of trichomoniasis negative by molecular testing
was not confirmed by rescreening; the slide demonstrated
extensive cytolysis with many naked nuclei that could have
been misinterpreted as Trichomonas. The Pap tests that were
overinterpreted for BV demonstrated a filmy background
of cocci but lacked evidence of clue cells.
Results
The study included 431 cases. The age of the participants
ranged from 17 to 79 years with a mean of 33 years. With
the Pap test, 60 patients (13.9%) were found to have BV, 60
(13.9%) had candidiasis, and 3 (0.7%) had a Trichomonas
infection. With the Affirm VPIII assay, 183 (42.5%) cases
tested positive for G vaginalis, 70 (16.2%) were positive for
Candida species, and 10 (2.3%) were positive for T vaginalis. The differences were statistically significant.
The diagnosis of Candida infection by Pap test agreed
well with the result of the Affirm VPIII assay ( = 0.66).
There was poor agreement for the diagnosis of BV ( = 0.32)
and Trichomonas infection ( = 0.30).
Coinfection by 2 organisms was noted in 30 cases by
using the Affirm VPIII assay; 26 cases tested positive for
Gardnerella and Candida, and the remaining 4 cases were
444
444
Am J Clin Pathol 2011;135:442-447
DOI: 10.1309/AJCP7TBN5VZUGLZU
American Society for Clinical Pathology
Anatomic Pathology / Original Article
Discussion
Infectious vaginitis is a common medical problem in
women.1 The organisms that cause BV, fungi (candidiasis),
and parasites (T vaginalis) are the 3 leading microbial agents
that are responsible for 90% of all infectious vaginitis. It has
been reported that three quarters of adult women will experience at least 1 episode of vaginal candidiasis during their
lifetimes and about half of the women will have 2 or more
episodes.12 Although the incidence of Trichomonas infection
has been declining for the past 20 years, more than 7.5 million
new cases of Trichomonas infection are reported each year in
the United States.13 BV occurs in up to 30% of the population
and is more common in African Americans than Caucasians
by a factor of 3.14 Although affected patients are often concerned by the troubling symptoms, there are also considerable
morbidities associated with infectious vaginitis. For example,
patients with BV have an enhanced risk of developing postoperative infection after pelvic surgery.14 BV and trichomoniasis
have been associated with adverse pregnancy outcomes such
as premature rupture of membranes, preterm delivery, and
low birth weight.12
The error rate in diagnosing infectious vaginitis using
traditional methods is rather high. Based on clinical signs
and symptoms and bedside testing, including wet mount
microscopy, KOH amine odor test, and a pH test of vaginal
fluid, about two thirds of the cases of Candida and BV were
misdiagnosed by general practitioners and gynecologists in a
cohort of 220 women with vaginal complaints.7 The authors
attributed the error rate to the lack of microscopy-related skills
and the subjectivity of some of the diagnostic criteria. Other
factors that were noted to have contributed to a misdiagnosis included menstruation, douching, and self-medication.
Furthermore, infectious vaginitis can be asymptomatic in as
high as 50% of cases.15 In another study by Lowe et al,16
the accuracy of the clinical diagnosis of BV, Candida vaginitis, and T vaginalis was compared with the Affirm VPIII
DNA probe molecular test for G vaginalis, T vaginalis, and
Candida species. Lowe et al16 found that compared with the
DNA probe standard using the Affirm VPIII, clinical diagnosis is 81% to 85% sensitive and 70% to 99% specific for BV,
Candida vaginitis, and trichomoniasis. While using traditional
standardized clinical diagnostic protocols even under the best
of circumstances, the diagnosis and treatment of these common vaginal problems remains challenging.16
Some authors advocate the use of Gram stain in the diagnosis of BV.3 However, Gram stain diagnosis ranged from
60% to 90% compared with the clinical diagnosis of BV.17-19
Microbial culture is another technique that can be useful in the
diagnosis of vaginitis and vaginosis. Culture for Trichomonas
is highly effective and relatively inexpensive.19,20 However, it
lacks clinical usefulness because it requires a special medium
(Diamond), which is not uniformly available, and an extended
turnaround time of up to 5 days. Cultures for Gardnerella and
Candida species are not recommended because both organisms can be part of the normal vaginal flora without causing
any infection.15,17,19
Because of the success of reducing the incidence and
mortality of cervical squamous carcinoma, Pap tests have
been widely adopted in the United States and other developed
countries. One of the secondary benefits is the detection of
microorganisms. As a result, many clinicians have come to
rely on the identification of microorganisms by the routine
Pap test as part of their patient management.5 The sensitivity
of Pap tests for diagnosing BV varies from 90% to as low
as 43%; the wide range of results reflects the use of different morphologic criteria and whether the specimens were
obtained from the cervix or the vagina.5,21-25 Similarly, the
Pap test lacks sensitivity as a screening test for Trichomonas.
Moreover, in low-prevalence populations, Trichomonas found
by cytomorphologic review and reported by routine Pap testing frequently represented a false-positive result.3
There has been an increase in the use of imaging systems
for primary screening of Pap tests. For a small portion of
scanned slides, no manual review would be performed (if no
abnormalities were noted in the fields selected by the system)
or only a limited number of fields would be examined (if the
system ranks the slides with a low probability of containing
abnormalities) depending on the type of imaging system being
used. This may result in underdetection of infections. One
study observed that the detection rates of Candida (68% vs
77%), Trichomonas (80% vs 85%), and shift in bacterial flora
(63% vs 65%) were lower with the AutoPap imaging system
(Becton Dickinson) compared with manual screening.26
To address these difficulties, a rapid and sensitive tool
is needed. The Affirm VPIII assay allows the simultaneous detection of the presence of clinically significant levels
of Trichomonas, Gardnerella, and Candida from vaginal
specimens. The results of our study show that the Affirm
VPIII assay demonstrated significantly higher detection rates
for all 3 organisms compared with Pap tests. The difference
in the detection rate of Gardnerella between the Affirm VPIII
assay and the Pap test was the most pronounced. One plausible
explanation is that the Pap test is essentially a cervical specimen, while BV is essentially a vaginal condition. Therefore,
BV is more likely to be better represented by vaginal samples
used in the Affirm VPIII assay.27 We also observed poor
agreement between the Affirm VPIII assay and the Pap test
when identifying Trichomonas. As mentioned earlier, in
populations like ours with a low prevalence of Trichomonas, a
higher incidence of false-negatives and false-positives may be
noted in the reporting of Trichomonas by gynecologic cytology staff.3 Therefore, our findings suggest that the Affirm
VPIII assay is more sensitive than the Pap test as a diagnostic
tool for the detection and identification of infectious vaginitis.
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:442-447
445
DOI: 10.1309/AJCP7TBN5VZUGLZU
445
445
Levi et al / Molecular Testing of Infectious Vaginitis
This argument supported the results of rescreening of the Pap
slides with discrepant cytologic and molecular test results.
Organisms were identified on rescreening in about one third of
the cytologic specimens that were initially reported to be negative for organisms but had positive molecular test results.
Our observation is comparable to findings from studies
that compared the Affirm VPIII assay with other methods
of detection of these 3 organisms.6-9,28,29 Based on a cohort
of 425 women, Brown et al6 demonstrated that the Affirm
VPIII assay was significantly more sensitive than wet mount
in identifying Candida (11% vs 7%) and Gardnerella (45%
vs 14%). The Affirm VPIII assay also detected more cases
of Trichomonas infection compared with wet mount (7% vs
5%), but the difference was not statistically significant.6 It has
also been reported that the Affirm VPIII assay correlated well
with the Gram stain in diagnosing BV and candidiasis.9,28,29
Because Gardnerella and Candida species can exist as
normal flora in 50% of women, a too sensitive molecular
diagnostic test may yield false-positive results, resulting in
unnecessary treatment.3,30 To minimize the possibility of
false-positive cases due to microbial colonization, the detection thresholds of the Affirm VPIII assay for each organism
are set above the levels of normal flora, thus ensuring that
only clinically relevant cases are detected. According to
the manufacturer, the detection thresholds for Gardnerella,
Candida, and Trichomonas species are 2 105 colony-forming units (CFU)/mL, 1 104 CFU/mL, and 5 103 CFU/mL,
respectively.31 This may explain some of our false-negative
molecular test results despite a positive cytologic result.
Based on personal communications with clinicians, our clients as a whole use the Affirm VPIII molecular test when
there is a clinical symptom that is reported by the patient and/
or a clinical sign noted during the gynecologic examination.
Depending on the provider, in some cases, before ordering
the molecular test, other diagnostic tools for vaginosis and
vaginitis, such as a wet mount, may be prepared in the office,
although much less commonly given the time constraints of
office practice and diminishing skill sets. If the bedside pointof-care tests are interpreted as negative, then the Affirm VPIII
test is ordered. As a general treatment protocol practiced by
our clients, patients with a clinical symptom and/or sign of
vaginitis or vaginosis in the setting of a positive result for a
given organism(s) (including the Affirm VPIII molecular test
result, a wet mount microscopic examination result, and/or
a positive Pap test result) are offered treatment for the given
organism(s) detected. Using the results of the Affirm VPIII
molecular test in addition to the routine Pap test in cases in
which there is a clinical suspicion of vaginitis or vaginosis
may decrease the likelihood of potential false-positive results
and unnecessary treatment.
About 14% of patients with infectious vaginitis have a
mixed infection.32 In our study, the Affirm VPIII assay identified
446
446
Am J Clin Pathol 2011;135:442-447
DOI: 10.1309/AJCP7TBN5VZUGLZU
30 patients (7.0%) with coinfection by 2 or more microorganisms, whereas the Pap test identified only 5 patients (1.2%)
with coinfection by 2 microorganisms. The difference was
statistically significant (Fisher exact test). In addition, cytologic
rescreening detected only 1 additional case of coinfection by 2
pathogens in the positive for Trichomonas and Gardnerella
category. Our findings suggest that the Affirm VPIII assay is
superior to the Pap test in detecting multiple pathogens.
There are other advantages of the Affirm VPIII assay
over the Pap test, including the objectivity of the assay, the
elimination of the need for special microscopy skills, and the
quick turnaround time of less than 2 hours. Also, there is no
interference with the assay by over-the-counter medications,
lubricants, douching, or menstruation. The specimen transport
medium preserves the specimens up to 72 hours from collection at room temperature, thereby facilitating transportation
from the physician office to the laboratory.6
One of the limitations of our study is that we were not
able to estimate the sensitivity and specificity of the Affirm
VPIII assay and Pap tests because we did not compare our
results with the gold standards such as microbial cultures
or Gram stain. Other studies reported that the sensitivity
and specificity of the Affirm VPIII assay in identifying G
vaginalis ranged from 88% to 90% and from 96% to 97%,
respectively.28,29 For diagnosing Candida species using the
Affirm VPIII assay, Petrikkos et al9 reported a sensitivity of
82% and specificity of 100% when compared with examination using 10% KOH.
We demonstrated that the Affirm VPIII assay using a
DNA hybridization technique was more sensitive in identifying G vaginalis, Candida species, and T vaginalis than the Pap
test. In addition, mixed infection is more readily diagnosed by
the Affirm VPIII assay than the Pap test.
From the Department of Pathology, Yale University, New Haven, CT.
Address reprint requests to Dr Levi: 430 Congress Ave, New
Haven, CT 06519.
References
1. Kent HL. Epidemiology of vaginitis. Am J Obstet Gynecol.
1991;165(4 pt 2):1168-1176.
2. Fleury FJ. Adult vaginitis. Clin Obstet Gynecol.
1981;24:407-438.
3. Sobel JD, Schmitt C, Meriwether C. A new slide latex
agglutination test for the diagnosis of acute Candida vaginitis.
Am J Clin Pathol. 1990;94:323-325.
4. Giacomini G, Calcinai A, Moretti D, et al. Accuracy
of cervical/vaginal cytology in the diagnosis of bacterial
vaginosis. Sex Transm Dis. 1998;25:24-27.
5. Platz-Christensen JJ, Larsson PG, Sundstrom E, et al.
Detection of bacterial vaginosis in wet mount, Papanicolaou
stained vaginal smears and in Gram stained smears. Acta
Obstet Gynecol Scand. 1995;74:67-70.
American Society for Clinical Pathology
Anatomic Pathology / Original Article
6. Brown HL, Fuller DD, Jasper LT, et al. Clinical evaluation
of Affirm VPIII in the detection and identification of
Trichomonas vaginalis, Gardnerella vaginalis, and Candida
species in vaginitis/vaginosis. Infect Dis Obstet Gynecol.
2004;12:17-21.
7. Schwiertz A, Taras D, Rusch K, et al. Throwing the dice
for the diagnosis of vaginal complaints? Ann Clin Microbiol
Antimicrob. 2006;5:4. doi:10.1186/1476-0711-5-4.
8. Pappas S, Makrilakis K, Anyfantis I, et al. Clinical evaluation
of Affirm VP III in the detection and identification of
bacterial vaginosis [letter]. J Chemother. 2008;20:764-765.
9. Petrikkos G, Makrilakis K, Pappas S. Affirm VP III in the
detection and identification of Candida species in vaginitis.
Int J Gynaecol Obstet. 2007;96:39-40.
10. Young NA, Bibbo M, Buckner S, et al. Non-neoplastic
findings. In: Solomon D, Nayar R, eds. The Bethesda System
for Reporting Cervical Cytology. 2nd ed. New York, NY:
Springer; 2004:21-56.
11. Bland JM, Altman DG. Statistical methods for assessing
agreement between two methods of clinical measurement.
Lancet. 1986;1:307-310.
12. Workowski KA, Berman SM. Sexually transmitted
diseases treatment guidelines, 2006. MMWR Recomm Rep.
2006;55(RR-11):1-94.
13. Centers for Disease Control and Prevention. Trichomoniasis:
CDC Fact Sheet. 2007. http://www.cdc.gov/std/trichomonas/
STDFact-Trichomoniasis.htm#Common. Accessed January
21, 2011.
14. Livengood CH. Bacterial vaginosis: an overview for 2009.
Rev Obstet Gynecol. 2009;2:28-37.
15. Carr PL, Felsenstein D, Friedman RH. Evaluation and
management of vaginitis. J Gen Intern Med. 1998;13:335-346.
16. Lowe NK, Neal JL, Ryan-Wenger NA. Accuracy of the
clinical diagnosis of vaginitis compared to a DNA probe
laboratory standard. Obstet Gynecol. 2009;113:89-95.
17. Krohn MA, Hillier SL, Eschenbach DA. Comparison of
methods for diagnosing bacterial vaginosis among pregnant
women. J Clin Microbiol. 1989;27:1266-1271.
18. Eschenbach DA, Hillier S, Critchlow C, et al. Diagnosis and
clinical manifestations of bacterial vaginosis. Am J Obstet
Gynecol. 1988;158:819-828.
19. Spiegel CA, Amsel R, Holmes KK. Diagnosis of bacterial
vaginosis by direct Gram stain of vaginal fluid. J Clin
Microbiol. 1983;18:170-177.
20. Fouts AC, Kraus SJ. Trichomonas vaginalis: reevaluation of its
clinical presentation and laboratory diagnosis. J Infect Dis.
1980;141:137-143.
21. Schnadig VJ, Davie KD, Shafer SK, et al. The cytologist and
bacterioses of the vaginal-ectocervical area: clues, commas
and confusion. Acta Cytol. 1989;33:287-297.
22. Davis JD, Connor EE, Clark P, et al. Correlation between
cervical cytologic results and Gram stain as diagnostic
tests for bacterial vaginosis. Am J Obstet Gynecol.
1997;177:532-535.
23. Hillier SL. Diagnostic microbiology of bacterial vaginosis.
Am J Obstet Gynecol. 1993;169(2 pt 2):455-459.
24. Tokyol C, Aktepe OC, Cevrioglu AS, et al. Bacterial
vaginosis: comparison of Pap smear and microbiological test
results. Mod Pathol. 2004;17:857-860.
25. Eriksson K, Forsum U, Bjornerem A, et al. Validation of the
use of Pap-stained vaginal smears for diagnosis of bacterial
vaginosis. APMIS. 2007;115:809-813.
26. Wilbur DC, Prey MU, Miller WM, et al. AutoPap system
detection of infections and benign cellular changes: results
from primary screener clinical trials. Diagn Cytopathol.
1999;21:355-358.
27. Karani A, De Vuyst H, Luchters S, et al. The Pap smear
for detection of bacterial vaginosis. Int J Gynaecol Obstet.
2007;98:20-23.
28. Witt A, Petricevic L, Kaufmann U, et al. DNA hybridization
test: rapid diagnostic tool for excluding bacterial vaginosis in
pregnant women with symptoms suggestive of infection.
J Clin Microbiol. 2002;40:3057-3059.
29. Gazi H, Degerli K, Kurt O, et al. Use of DNA hybridization
test for diagnosing bacterial vaginosis in women with
symptoms suggestive of infection. APMIS. 2006;114:784-787.
30. Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing
bacterial vaginosis is improved by a standardized method of
Gram stain interpretation. J Clin Microbiol. 1991;29:297-301.
31. Affirm VP III Assay [package insert]. Burlington, NC: Becton
Dickinson; 2009.
32. Ferris DG, Hendrich J, Payne PM, et al. Office laboratory
diagnosis of vaginitis: clinician-performed tests compared
with a rapid nucleic acid hybridization test. J Fam Pract.
1995;41:575-581.
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:442-447
447
DOI: 10.1309/AJCP7TBN5VZUGLZU
447
447
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Formulation and Evaluation of Ibuprofen Topical GEL: Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument12 paginiFormulation and Evaluation of Ibuprofen Topical GEL: Rajiv Gandhi University of Health Sciences Bangalore, Karnatakagina inÎncă nu există evaluări
- Kelompok 10Document24 paginiKelompok 10Nining FauziahÎncă nu există evaluări
- Introduction To Expert Systems - MYCINDocument8 paginiIntroduction To Expert Systems - MYCINVictoria OffomaÎncă nu există evaluări
- HYDRALAZINE HYDROCHLORIDE - (Apresoline)Document1 paginăHYDRALAZINE HYDROCHLORIDE - (Apresoline)wen_pilÎncă nu există evaluări
- Abnormal Psych Question 1Document10 paginiAbnormal Psych Question 1Ronald Jacob Picorro100% (1)
- Liverpool SDL IABPDocument26 paginiLiverpool SDL IABPSathya Swaroop PatnaikÎncă nu există evaluări
- The 5 Levels of Healing - A Guide To Diagnosis and TreatmentDocument1 paginăThe 5 Levels of Healing - A Guide To Diagnosis and TreatmentJAYAKUMAR100% (1)
- Enoxaparin FDADocument40 paginiEnoxaparin FDAImam Nur Alif Khusnudin100% (2)
- Psychiatric Mental Health Nursing 2nd EditionDocument550 paginiPsychiatric Mental Health Nursing 2nd Editiondaria100% (7)
- 5 Day Bodybuilding Workout ScheduleDocument4 pagini5 Day Bodybuilding Workout ScheduleNazri Yusoff100% (1)
- Common Cancers in WomenDocument27 paginiCommon Cancers in Womensuha damagÎncă nu există evaluări
- Current Issues & Trends in Older: Persons Chronic CareDocument12 paginiCurrent Issues & Trends in Older: Persons Chronic CareKeepItSecretÎncă nu există evaluări
- Health Talk - Diet in AnemiaDocument17 paginiHealth Talk - Diet in Anemiameghana88% (8)
- Disruptive Mood Dysregulation Disorder (DMDD)Document14 paginiDisruptive Mood Dysregulation Disorder (DMDD)David PÎncă nu există evaluări
- MRCPass Notes For MRCP 1 - HEMATOLOGYDocument9 paginiMRCPass Notes For MRCP 1 - HEMATOLOGYsabdali100% (1)
- Vitamin B12 DeficiencyDocument2 paginiVitamin B12 DeficiencyFarina AcostaÎncă nu există evaluări
- Surgery Report & RatingsDocument25 paginiSurgery Report & RatingsWXYZ-TV Channel 7 DetroitÎncă nu există evaluări
- How To Use BNF With ScenariosDocument6 paginiHow To Use BNF With ScenariosLuxs23Încă nu există evaluări
- Cystic Fibrosis Patient PamphletDocument2 paginiCystic Fibrosis Patient PamphletfloapaaÎncă nu există evaluări
- Electric Field Distribution in Biological Tissues For Various Electrode Configurations - A FEMLAB StudyDocument5 paginiElectric Field Distribution in Biological Tissues For Various Electrode Configurations - A FEMLAB StudyxlippyfingersÎncă nu există evaluări
- S1 Hippocratic Oath Seminar and Reading NotesDocument7 paginiS1 Hippocratic Oath Seminar and Reading NotesTaraSubba1995Încă nu există evaluări
- Elizabeth L. Samonte BSN Iv Responsibilities of The Nurse To The PatientsDocument7 paginiElizabeth L. Samonte BSN Iv Responsibilities of The Nurse To The PatientsRein VillanuevaÎncă nu există evaluări
- Konker AbstractDocument39 paginiKonker AbstractWigunaÎncă nu există evaluări
- Learning Through PlayDocument2 paginiLearning Through PlayThe American Occupational Therapy Association100% (1)
- Nursing Care Plan For Osteomyelitis: Nursing Diagnosis For Osteomyelitis and Nursing Interventions For OsteomyelitisDocument43 paginiNursing Care Plan For Osteomyelitis: Nursing Diagnosis For Osteomyelitis and Nursing Interventions For Osteomyelitisabe abdiÎncă nu există evaluări
- What Are Mucous CystsDocument10 paginiWhat Are Mucous CystsNena TamaraÎncă nu există evaluări
- Diabetes and Its Permanent Cure With Homeopathic Medicines - DRDocument28 paginiDiabetes and Its Permanent Cure With Homeopathic Medicines - DRkrishna kumar67% (3)
- RanbaxyDocument5 paginiRanbaxy26449659Încă nu există evaluări
- Clinical Surgery NotesDocument214 paginiClinical Surgery Notessarahsarahsarahsarah100% (6)
- Prescription of Exercise For Health and FitnessDocument27 paginiPrescription of Exercise For Health and FitnessedelinÎncă nu există evaluări