Documente Academic
Documente Profesional
Documente Cultură
ACOG Practice Bulletin Obesity
Încărcat de
noella deckbar0 evaluări0% au considerat acest document util (0 voturi)
250 vizualizări2 paginiSummary of ACOG Obesity Guidelines
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentSummary of ACOG Obesity Guidelines
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
250 vizualizări2 paginiACOG Practice Bulletin Obesity
Încărcat de
noella deckbarSummary of ACOG Obesity Guidelines
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 2
ACOG Practice Bulletin - #156 Dec 2015
OBESITY IN PREGNANCY
Classified based on BMI (kg/m^2): underweight: <18.5, normal: 18.5-24.9, overweight
25-29.9, obesity class I: 30-34.9, obesity class II: 35-39.9, obesity class III: 40 or >
Obesity= most common problem in women of reproductive age (20-39 yrs)
o Prevalence in U.S. women of repro age = 31.8%, 58.8% if add those overweight
Effects on pregnancy
o Increased risk of spontaneous abortion, recurrent miscarriage, and certain
congenital anomalies (neural tube defects, spina bifida, hydrocephaly, cleft
lip/palate, anorectal atresia, and cardiovascular, septal, orofacial, and limb
reduction anomalies)
o Reduced risk of gastroschisis in the neonates among obese gravidas
Antepartum Complications
o Obese women are at increased risk of cardiac dysfunction, proteinuria, sleep
apnea, nonalcoholic fatty liver disease, gestational DM, and preeclampsia
o Obese gravidas are 40% more likely to experience stillbirth
Black obese gravidas > risk vs white
Increasing risk w/ increasing gestational age per obesity class trend
observed
Intrapartum Complications
o Increased risk of cesarean delivery, failed trial of labor, endometritis, wound
rupture or dehiscence, and venous thrombosis
o Associations with indicated preterm birth clear, less so for spontaneous preterm
birth
o Trial of labor after previous c-section in obese gravidas presents 2x increase in
composite maternal morbidity (prolonged hospital stay, endometritis, rupture or
dehiscence) and 5x increase risk in neonatal injury ((fractures, brachial plexus
injuries, and lacerations))
o Pregnant women w/ class III obesity have a significantly increased risk of
postpartum atonic hemorrhage (bleeding > 1,000 mL) after a vaginal delivery
(5.2%) but not after cesarean delivery
Postpartum Complications and Long-Term Outcomes
o Associations with future maternal metabolic dysfunction; risks compounded by
excess gestational weight gain which is also a factor for postpartum weight
retention
o Pregravid obesity is associated with early termination of breastfeeding,
postpartum anemia, and depression
Fetal Complications and Childhood Morbidities
o Fetus: increased risk of macrosomia and impaired growth
o Infants: increased body weight
o Longer term risks: increased risk of metabolic syndrome, childhood obesity,
childhood asthma
o Maternal obesity also linked to autism spectrum disorders, childhood
developmental delay, and attention-deficit/hyperactivity disorder
o Note confounding variables in metabolic outcome analysis: family socioeconomic
issue, behavior, activity, and diet
Managing obesity before and during pregnancy
o Optimal control begins before conception: surgical or nonsurgical, though
medications not recommended during the time of conception or pregnancy i.e.
anorectics
Primary weight management strategies during pregnancy are dietary
control, exercise, and behavior modification alone or in combination
Even small weight reductions before pregnancy may have improved
pregnancy outcomes
Motivational interviewing: a significant decrease in weight; a nonsignificant
decrease in BMI; however a weight loss of 57% over time can significantly
improve metabolic health
o IOM Weight gain recommendations in pregnancy for overweight and obese
women
total weight gain of 6.811.3 kg (1525 lb) for overweight pregnant
women
& 5.09.1 kg (1120 lb) for all obese women (limited data by obesity
class)
Current data also seems indicates that inadequate weight gain and
gestational weight loss should not be encouraged for obese pregnant
women due to an association with SGA (contrasts w/ perceived benefits
such as decreases in the rate of cesarean delivery, decreased risk of
LGA, and postpartum weight retention)
o Maternal obesity alone is not an indication for induction; however w/ increased
risk of a prolonged pregnancy-> increased rate of labor induction
o Allowing a longer first stage of labor before performing cesarean delivery for
labor arrest should be considered
Antenatal care: Detection of congenital anomalies by ultrasonography is significantly
reduced with increasing maternal BMI; counsel patients on limitations
Metabolic Disorders
o Increased risk of metabolic syndrome
o Increased insulin resistance may trigger cardiometabolic dysfunction to emerge
as preeclampsia, gestational diabetes, and OSA
o First antenatal visit: screen for glucose intolerance & OSA
OSA associated w/ preeclampsia, eclampsia, cardiomyopathy, PE, and
in-hospital mortality
Also: increased risk of hypoxemia, hypercapnia, and sudden
death
Stillbirth & Antenatal Fetal Surveillance: no recommendation for or against routine
antenatal fetal surveillance in obese pregnant women (no clear evidence w/ improved
outcomes)
Epidural Issues
o Risk of epidural analgesic failure is greater; consider early labor epidural catheter
placement
o Combo of spinal anesthesia & obesity significantly impairs respiratory function for
up to 2 hours after the procedure
Cesareans
o SubQ drains increase the risk of postpartum cesarean wound complications -do
not use routinely
o Risk of venous thromboembolism
Pneumatic compression devices: placed before a cesarean delivery and
continue postpartum
In very-high-risk groups: add LMWH (enoxaparin 40 mg daily is
commonly used)
Weight-based dosage may be more effective than BMI-stratified
dosage strategies in class III obesity post cesarean
Post pregnancy
o Behavioral interventions employing diet and exercise seen to improve
postpartum weight reduction in contrast to exercise alone
o Weight loss between pregnancies in obese women has been shown to decrease
the risk of a LGA and vice versa
o
S-ar putea să vă placă și
- Obesity in Pregnancy - UPTO DATEComplications and Maternal Management - UpToDateDocument43 paginiObesity in Pregnancy - UPTO DATEComplications and Maternal Management - UpToDateCristinaCaprosÎncă nu există evaluări
- Diabetes Acog 2017Document15 paginiDiabetes Acog 2017Holger Vicente Guerrero Guerrero100% (1)
- ACOG Practice BulletinDocument2 paginiACOG Practice Bulletinnoella deckbarÎncă nu există evaluări
- PROLOG: Obstetrics, Ninth Edition (Assessment & Critique)De la EverandPROLOG: Obstetrics, Ninth Edition (Assessment & Critique)Încă nu există evaluări
- Dewhurst's Textbook of Obstetrics & GynaecologyDe la EverandDewhurst's Textbook of Obstetrics & GynaecologyChristoph LeesEvaluare: 2 din 5 stele2/5 (1)
- Dr. Sharda Jain: Director: Secretary GeneralDocument91 paginiDr. Sharda Jain: Director: Secretary GeneraljijaniÎncă nu există evaluări
- Nausea and Vomiting of Pregnancy and Hyperemesis GravidarumDocument27 paginiNausea and Vomiting of Pregnancy and Hyperemesis GravidarumxxdrivexxÎncă nu există evaluări
- Instruction Manual in Obstetrics: Volume OneDe la EverandInstruction Manual in Obstetrics: Volume OneÎncă nu există evaluări
- Acog Practice Bulletin Summary: Pregestational Diabetes MellitusDocument3 paginiAcog Practice Bulletin Summary: Pregestational Diabetes MellitusMaría Fernanda Palma AcostaÎncă nu există evaluări
- Repair of Obstetric Perineal LacerationsDocument7 paginiRepair of Obstetric Perineal LacerationsadriantiariÎncă nu există evaluări
- Green Top Guidelines 13Document29 paginiGreen Top Guidelines 13garfield1Încă nu există evaluări
- Menstrual Disorders: Olufemi Aworinde Lecturer/ Consultant Obstetrician and Gynaecologist, Bowen University, IwoDocument36 paginiMenstrual Disorders: Olufemi Aworinde Lecturer/ Consultant Obstetrician and Gynaecologist, Bowen University, IwoAkinbani MoyosoreÎncă nu există evaluări
- MRCOG Module SummaryDocument4 paginiMRCOG Module SummaryAmadeus KQÎncă nu există evaluări
- 2023 OB/GYN Coding Manual: Components of Correct CodingDe la Everand2023 OB/GYN Coding Manual: Components of Correct CodingÎncă nu există evaluări
- Abortion and Sterilization: Medical and Social AspectsDe la EverandAbortion and Sterilization: Medical and Social AspectsJane E. HodgsonÎncă nu există evaluări
- RCOG Guideline 2011Document24 paginiRCOG Guideline 2011John DoeÎncă nu există evaluări
- Uterinefibroids 130120064643 Phpapp02Document73 paginiUterinefibroids 130120064643 Phpapp02Tharun KumarÎncă nu există evaluări
- Poly Hi DR AmnionDocument7 paginiPoly Hi DR Amnionwanwan_adongÎncă nu există evaluări
- Singer and Monaghan's Cervical and Lower Genital Tract Precancer: Diagnosis and TreatmentDe la EverandSinger and Monaghan's Cervical and Lower Genital Tract Precancer: Diagnosis and TreatmentEvaluare: 5 din 5 stele5/5 (1)
- Gestational Trophoblastic DiseaseDocument6 paginiGestational Trophoblastic DiseaseSJ IraaÎncă nu există evaluări
- GTG From 2010 To 2015Document857 paginiGTG From 2010 To 2015Hasan Dahamsheh100% (1)
- Queenan's Management of High-Risk Pregnancy: An Evidence-Based ApproachDe la EverandQueenan's Management of High-Risk Pregnancy: An Evidence-Based ApproachÎncă nu există evaluări
- KEMH Guidelines On Cardiac Disease in PregnancyDocument7 paginiKEMH Guidelines On Cardiac Disease in PregnancyAyesha RazaÎncă nu există evaluări
- Fetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsDe la EverandFetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsPeter RolfeÎncă nu există evaluări
- The Nurse Practitioner in UrologyDe la EverandThe Nurse Practitioner in UrologyMichelle LajinessÎncă nu există evaluări
- Acute Uterine InversionDocument6 paginiAcute Uterine InversionBima GhovaroliyÎncă nu există evaluări
- Urinary IncontinenceDocument0 paginiUrinary Incontinencemango91286Încă nu există evaluări
- Advanced Gynecologic Endoscopy: Edited by Atef DarwishDocument344 paginiAdvanced Gynecologic Endoscopy: Edited by Atef DarwishSandu Alexandra100% (1)
- Cardiff CountDocument16 paginiCardiff CountmohiiieÎncă nu există evaluări
- Genetics For MrcogDocument4 paginiGenetics For MrcogsriniÎncă nu există evaluări
- Benign and Malignant Tumors of Female Genital TractDocument14 paginiBenign and Malignant Tumors of Female Genital TractDimitrios PapadopoulosÎncă nu există evaluări
- Green Top Guidelines 1Document22 paginiGreen Top Guidelines 1garfield1Încă nu există evaluări
- PROLOG: Patient Management in the Office, Eighth EditionDe la EverandPROLOG: Patient Management in the Office, Eighth EditionÎncă nu există evaluări
- GTG 17 PDFDocument18 paginiGTG 17 PDFFlorida RahmanÎncă nu există evaluări
- Drug Therapy During PregnancyDe la EverandDrug Therapy During PregnancyTom K. A. B. EskesEvaluare: 5 din 5 stele5/5 (1)
- Yamada's Handbook of GastroenterologyDe la EverandYamada's Handbook of GastroenterologyDr. Tadataka YamadaÎncă nu există evaluări
- Practical Cases in Obstetrics and Gynecology by Kanan Yelikar 2015 05 31 B01K04YXO4 PDFDocument2 paginiPractical Cases in Obstetrics and Gynecology by Kanan Yelikar 2015 05 31 B01K04YXO4 PDFSaeed HasanÎncă nu există evaluări
- Your Breast Health: Presented By: Eric Lachman and Kim LeDocument23 paginiYour Breast Health: Presented By: Eric Lachman and Kim Leeric_lachman5234Încă nu există evaluări
- 8surgical Management of Dysfunctional Uterine Bleeding - KabilanDocument14 pagini8surgical Management of Dysfunctional Uterine Bleeding - KabilanNavani TharanÎncă nu există evaluări
- RCOG - Management of Suspected Ovarian Masses in Premenopausal WomenDocument14 paginiRCOG - Management of Suspected Ovarian Masses in Premenopausal Womenestridente81Încă nu există evaluări
- Practice Bulletin: Antiphospholipid SyndromeDocument8 paginiPractice Bulletin: Antiphospholipid SyndromeSus ArÎncă nu există evaluări
- Obs History Taking FormatDocument24 paginiObs History Taking FormatBibek PandeyÎncă nu există evaluări
- AMTSL BrieferDocument2 paginiAMTSL BrieferNewborn2013Încă nu există evaluări
- Ectopic PregnancyDocument24 paginiEctopic PregnancybertouwÎncă nu există evaluări
- Rcog PpromDocument7 paginiRcog PpromDevi SyamÎncă nu există evaluări
- PROLOG: Gynecologic Oncology and Critical Care, Eighth Edition (Assessment & Critique)De la EverandPROLOG: Gynecologic Oncology and Critical Care, Eighth Edition (Assessment & Critique)Încă nu există evaluări
- GTG 55 Late Intrauterine Fetal Death and Stillbirth 10 11 10-2Document33 paginiGTG 55 Late Intrauterine Fetal Death and Stillbirth 10 11 10-2fahlevyÎncă nu există evaluări
- Essentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2De la EverandEssentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2Încă nu există evaluări
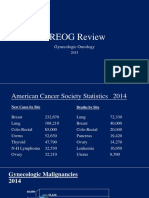
- 2015 Oncology CREOG Review PDFDocument76 pagini2015 Oncology CREOG Review PDFRima HajjarÎncă nu există evaluări
- Sbas and Emqs For Mrcog IiDocument16 paginiSbas and Emqs For Mrcog Iiasfh hgoreÎncă nu există evaluări
- GTG 37bDocument32 paginiGTG 37bKadelsy BristolÎncă nu există evaluări
- Pre Eclampsia Case StudyDocument39 paginiPre Eclampsia Case StudyAnton RossiniÎncă nu există evaluări
- Intrauterine Growth Restriction IUGR Etiology andDocument11 paginiIntrauterine Growth Restriction IUGR Etiology andFlavia Angelina SatopohÎncă nu există evaluări
- 10-Primary Care - AAFP Flashcards - Quizlet PDFDocument870 pagini10-Primary Care - AAFP Flashcards - Quizlet PDFehabb350% (2)
- Prenatal Care - Questions 1 - 5Document5 paginiPrenatal Care - Questions 1 - 5Monde BernalÎncă nu există evaluări
- Study of Calcified Placenta and Its Correlation WithDocument4 paginiStudy of Calcified Placenta and Its Correlation Withcut normaya putriÎncă nu există evaluări
- Educating Preeclampsia Management Using Case Studies of Disease PDocument30 paginiEducating Preeclampsia Management Using Case Studies of Disease PANUM NOORIÎncă nu există evaluări
- Preeclampsia Pathophysiology andDocument15 paginiPreeclampsia Pathophysiology andYojhaida Zarate CasachahuaÎncă nu există evaluări
- Undergraduate Manual of Clinical Cases in Obstetrics GynaecologyDocument621 paginiUndergraduate Manual of Clinical Cases in Obstetrics GynaecologyTony StarkÎncă nu există evaluări
- Nuhra Region7 AgendaDocument59 paginiNuhra Region7 AgendaEuna Patricia AguilarÎncă nu există evaluări
- Nursing Role and Nursing Care During Pregnancy ComplicationsDocument21 paginiNursing Role and Nursing Care During Pregnancy Complicationsvienny kayeÎncă nu există evaluări
- The Internet Journal of Gynecology and ObstetricsDocument8 paginiThe Internet Journal of Gynecology and Obstetricsrett_ttaÎncă nu există evaluări
- Diabetes and Pregnancy Review ArticleDocument9 paginiDiabetes and Pregnancy Review ArticleGabyliz Gonzalez CastilloÎncă nu există evaluări
- Cmca2 (Prelim) 1Document10 paginiCmca2 (Prelim) 1NOEL YRIGONÎncă nu există evaluări
- Hypertension in Pregnancy - DerianDocument59 paginiHypertension in Pregnancy - Deriankevin jonathanÎncă nu există evaluări
- SOAL UJIAN MCQ Jan 2022Document22 paginiSOAL UJIAN MCQ Jan 2022densus awÎncă nu există evaluări
- Pregnancy Induced HypertensionDocument43 paginiPregnancy Induced HypertensionDesty Adjaahh LaahhÎncă nu există evaluări
- Pre-Eclampsia Risk Monitoring and Alert System Using Machine Learning and IoTDocument6 paginiPre-Eclampsia Risk Monitoring and Alert System Using Machine Learning and IoTBOHR International Journal on GynaecologyÎncă nu există evaluări
- Article FGRDocument18 paginiArticle FGRAngélica MuñozÎncă nu există evaluări
- Obstetric Nursing Practice Test Part 1Document10 paginiObstetric Nursing Practice Test Part 1yanee06Încă nu există evaluări
- Hypertensive Disorders in PregnancyDocument96 paginiHypertensive Disorders in PregnancySalman Habeeb100% (4)
- Pre Eclampsia: Preeclampsia Is A Pregnancy Complication Characterized by High Blood Pressure and Signs of Damage ToDocument3 paginiPre Eclampsia: Preeclampsia Is A Pregnancy Complication Characterized by High Blood Pressure and Signs of Damage ToSahaaneiy IlmeeÎncă nu există evaluări
- Alexander 2006Document7 paginiAlexander 2006Yosua Butar ButarÎncă nu există evaluări
- High Risk PregnancyDocument113 paginiHigh Risk PregnancyVivian Lajara100% (2)
- Tissue Pathway For Histopathological Examination of The PlacentaDocument18 paginiTissue Pathway For Histopathological Examination of The PlacentaArifah Azizah ArifinÎncă nu există evaluări
- Anxiety During Pregnancy and Preeclampsia: A Case-Control StudyDocument7 paginiAnxiety During Pregnancy and Preeclampsia: A Case-Control StudyCek GuevaraÎncă nu există evaluări
- Jurnal Plasenta PreviaaDocument41 paginiJurnal Plasenta PreviaacimyÎncă nu există evaluări
- CP On Pre-EclampsiaDocument152 paginiCP On Pre-Eclampsiakathy100% (2)
- Nueroprotección Fetal (Efectos Neuroprotectores de La Exposición Intrauterina Al Sulfato de Magnesio)Document14 paginiNueroprotección Fetal (Efectos Neuroprotectores de La Exposición Intrauterina Al Sulfato de Magnesio)GbrielÎncă nu există evaluări
- Nutrition: Pregnancy AND Lactation: Enriquez R. Cayaban, RN, LPT, MANDocument44 paginiNutrition: Pregnancy AND Lactation: Enriquez R. Cayaban, RN, LPT, MANCarl Josef C. GarciaÎncă nu există evaluări
- Stages of Labor: 4. Dilatation & EffacementDocument7 paginiStages of Labor: 4. Dilatation & EffacementDeejune TorrinoÎncă nu există evaluări