Documente Academic
Documente Profesional
Documente Cultură
Breast Cancer
Încărcat de
Ther RayTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Breast Cancer
Încărcat de
Ther RayDrepturi de autor:
Formate disponibile
The British Journal of Radiology, 85 (2012), e212e216
Breast-specific gamma imaging as an adjunct modality for the
diagnosis of invasive breast cancer with correlation to tumour
size and grade
1
R V TADWALKAR, MD, 1J A RAPELYEA, MD, 1J TORRENTE, MD, 1L R RECHTMAN, MA, 2C B TEAL,
A P McSWAIN, MD, 1C DONNELLY, BS, 1A B KIDWELL, BS, 1C M COFFEY, BS and 1R F BREM, MD
MD,
Breast Imaging and Interventional Center, Department of Radiology, The George Washington University, Washington, DC,
USA, and 2Department of Surgery, The George Washington University, Medical Faculty Associates, Washington, DC, USA
Objectives: The purpose of this study was to determine the sensitivity of breastspecific gamma imaging (BSGI) in the detection of invasive breast cancers and to
characterise the sensitivity of BSGI based on tumour size and pathological grade.
Methods: 139 females with invasive carcinoma who underwent BSGI were
retrospectively reviewed. Patients were injected in the antecubital vein with 2030 mCi
(9251110 MBq) of 99mTc-sestamibi. Images were obtained with a high-resolution,
breast-specific gamma camera (Dilon 6800; Dilon Technologies, Newport News, VA) and
were categorised based on radiotracer uptake as normal, normal with heterogeneous
uptake, probably abnormal and abnormal. For a positive examination, the region of
the area of increased uptake had to correlate with the laterality and location of the
biopsy-proven cancer.
Results: 149 invasive cancers in 139 patients with a mean size of 1.8 cm (0.28.5 cm)
were included. 146 were identified with BSGI (98.0%). All cancers which measured
$0.7 cm (n5123) as well as all cancers grade 2 or higher (n5102), regardless of tumour
size, were identified with BSGI (100%). There were 6 cancers that were pathological
grade 1 and measured ,7 mm, of which 50% (3/6) were identified with BSGI. The
overall sensitivity of BSGI for the detection of invasive breast cancer is 98.0%. The
sensitivity for subcentimetre cancers is 88.5% (23/26).
Conclusion: BSGI has a high sensitivity for the detection of invasive breast cancer. Our
results demonstrate that BSGI detected all invasive breast cancers pathological grade 2
and higher regardless of size and all cancers which measured $7 mm regardless of
grade. BSGI can reliably detect invasive breast cancers and is a useful adjunct imaging
modality for the diagnosis of breast cancer.
Mammography has remained the modality of choice
for breast cancer screening. Nevertheless, it is an
imperfect examination with a sensitivity of 7885% that
declines to 68% in females with dense breasts [16]. The
limitations of mammography have resulted in the
development of adjunct imaging modalities to improve
breast cancer detection. Most frequently, ultrasound is
used in conjunction with mammography as an adjunct
imaging modality for breast cancer diagnosis, particularly in females with dense breasts [2].
Mammography and ultrasound are both anatomical
approaches for the diagnosis of breast cancer. Nuclear
medicine techniques that utilise physiological properties
of tumours are increasingly being used. A meta-analysis
of scintimammographic studies using a traditional, general purpose gamma camera demonstrated an average
sensitivity of 84% for breast cancer detection, although
many of the cancers included in these studies were
Address correspondence to: Dr Rachel Brem, Breast Imaging and
Interventional Center, The George Washington University, 2150
Pennsylvania Avenue NW, Washington, DC 20037, USA. E-mail:
rbrem@mfa.gwu.edu
e212
Received 25 August 2010
Revised 18 October 2010
Accepted 11 November
2010
DOI: 10.1259/bjr/34392802
2012 The British Institute of
Radiology
palpable and larger [7]. However, scintimammography
with a general purpose gamma camera is limited in the
detection of non-palpable cancers and cancers less than
1 cm in size because of intrinsic resolution limitations [8
11]. Another limitation is the inability of a general purpose
gamma camera to image in positions comparable to those
obtained with mammography, limiting the ability to
correlate between these two modalities.
To overcome the limitations of a traditional gamma
camera for the detection of breast cancer, a high-resolution,
small-field-of-view gamma camera was developed that
allows for the reliable detection of cancers smaller than
1 cm [12]. This technique is referred to as breast-specific
gamma imaging (BSGI). Studies with BSGI have demonstrated reliable detection of cancers, both invasive and
ductal carcinoma in situ (DCIS), as small as 1 mm [13].
Furthermore, the BSGI camera allows for imaging in
positions comparable to mammography, which allows for
more direct correlation of mammographic imaging and
BSGI [14].
An early study using prototype BSGI cameras reported
an improvement in the sensitivity for detecting breast
cancer when compared with a traditional gamma camera
The British Journal of Radiology, June 2012
Breast-specific gamma imaging for the diagnosis of invasive cancer
[15]. One study of high-risk females with normal clinical
breast examination and a Breast Imaging Reporting and
Data System 1 or 2 mammogram demonstrated that BSGI
was able to locate occult carcinomas in 13.5% of patients
[16]. A recent report demonstrated that BSGI has a
sensitivity of 96.4% for invasive carcinoma and 90.9% in
DCIS [13, 17].
The purpose of this study was to investigate the
sensitivity of BSGI for invasive breast cancers in the
largest reported series to date and to correlate BSGI
sensitivity based on tumour pathological size and grade.
Methods and materials
Data collection and statistical analysis
From November 2004 to June 2007, 139 consecutive
females with biopsy-proven invasive carcinoma who
underwent BSGI were retrospectively reviewed. The
mean patient age was 52.8 years [range 2983 years,
standard deviation (SD) 11.8 years, median 51 years].
Indications for BSGI examination included evaluation for
additional lesions in females with biopsy-proven cancer,
indeterminate palpable breast findings during mammographic or physical examination, and females defined as
high risk by the Breast Cancer Risk Assessment Profile
[18].
The sensitivity of BSGI in detecting invasive breast
cancer was calculated (Microsoft Excel, 2003, Redmond,
WA; Online Clinical Calculator, 2007, Division of General
Internal Medicine, Medical College of Wisconsin, Milwaukee, WA; available at: http://www.intmed.mcw.
edu/clincalc/bayes.html). Tumour size, as determined
by pathology, and the ScarffBloomRichardson threepoint grading system for tumour grade were noted and
correlated to BSGI findings.
Breast-specific gamma imaging
A high-resolution, small-field-of-view breast-specific
gamma camera (Dilon 6800; Dilon Technologies, Newport
News, VA) was used (Figure 1). Patients were injected
intravenously with 2030 mCi (9251110 MBq) of 99mTcsestamibi (CardoliteH; Cardinal Health, Charlotte, NC) in
the antecubital vein. Injection was performed in the
contralateral arm for patients with a suspicious breast
finding prior to the BSGI examination. This was done in
an effort to lessen the uncertainty of increased axillary
radiotracer uptake secondary to extravasation of radiotracer during the injection, even though a recent report
suggested the ability to differentiate metastatic nodes
from nodes with increased radiotracer uptake due to
extravasation [19]. Pedal vein injection was not performed
because of strong patient preference. Imaging began
immediately after injection of the radiotracer. Mediolateral and craniocaudal views were obtained at 710 min
per image with the patient seated for a minimum of
100 000 counts.
Additional views were obtained as deemed necessary
for clinical evaluation by the interpreting radiologist.
Studies were interpreted by one of two breast imagers
with at least 7 years experience in interpretation of BSGI.
The British Journal of Radiology, June 2012
Figure 1. Breast-specific gamma imaging camera (Dilon
6800; Dilon Technologies, Newport News, VA).
The radiologists were blind to pathology results and
categorised the studies based on radiotracer uptake as
normal (no increased radiotracer uptake), normal with
heterogeneous uptake (scattered uptake without focal
increased radiotracer uptake), probably abnormal (heterogeneous uptake with one or more areas of more focal
radiotracer uptake) and abnormal (definitive focus of
increased radiotracer uptake). For analysis, the results
were grouped into two categories: negative (normal and
normal with heterogeneous uptake) and positive (probably abnormal and abnormal). The laterality and quadrant of the focal area of increased radiotracer uptake
were noted and compared with the laterality and
location of the biopsy-proven invasive cancer. If the
cancer was in the same quadrant of the breast as well as
in the same area of the breast from the nipple (anterior,
mid or posterior), the findings were considered concordant. If the pathology report did not indicate the
quadrant of the breast but the laterality was consistent,
the BSGI and pathological findings were considered
concordant. For this study, if the BSGI was performed as
part of the patients clinical evaluation, the BSGI report
in the patients medical record was used and the studies
were not reinterpreted. Patients who met the criteria for
entry but were part of other clinical trials and thus did not
have a BSGI report in their record had their images
reinterpreted by one of the two radiologists (RFB, JAR)
with the radiologists unaware of the pathological findings.
This study was approved by the Institutional Review
Board and was in compliance with the Health Insurance
Portability and Accountability Act.
Results
There were 149 invasive cancers identified in 139
patients. There was a single cancer in 128 patients, 2
cancers in 7 patients and multifocal cancer in 4 patients.
e213
R V Tadwalkar, J A Rapelyea, J Torrente et al
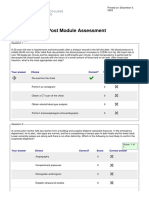
Table 1. Percentage and number of invasive cancers characterised by pathological subtype
Type
Infiltrating ductal
carcinoma
Infiltrating lobular
carcinoma
Mixed infiltrating ductal
and infiltrating lobular
carcinoma
Mucinous carcinoma
Tubulolobular carcinoma
Infiltrating tubular
carcinoma
Infiltrating papillary
carcinoma
Medullary carcinoma
Figure 2. A 32-year-old female with diffuse infiltrating
ductal carcinoma of the left breast visualised clearly by
breast-specific gamma imaging in the mediolateral view:
2.5 cm; grade 2 of 3.
For each of these multifocal cases, only lesions with
associated tumour sizes, as determined pathologically,
were included. There were 126 infiltrating ductal carcinomas (84.6%) (Figure 2), 9 infiltrating lobular carcinomas (6.0%), 7 mixed infiltrating ductal and infiltrating
lobular carcinomas (4.7%) (Figure 3), 2 mucinous carcinomas (1.3%), 2 tubulolobular carcinomas (1.3%), 1 infiltrating tubular carcinoma (0.7%), 1 infiltrating papillary
carcinoma (0.7%), and 1 medullary carcinoma (0.7%)
(Table 1). The four patients with multifocal cancers all
had infiltrating ductal carcinomas (Figure 4).
Number of
cases
Percentage
126
84.6
6.0
4.7
2
2
1
1.3
1.3
0.7
0.7
0.7
Pathological cancer sizes were available for 126 out of
the 149 cancers. The mean cancer size was 1.80 cm
(range, 0.28.5 cm; SD, 1.33 cm; median, 1.45 cm). Individual tumour grades using the ScarffBloomRichardson
grading system were available for 120 out of 149 total
cancers. The mean tumour grade was 2.28 (range, 13;
SD, 0.71; median, 2).
Of the 149 lesions, 146 were identified with BSGI for a
sensitivity of 98.0% for BSGI detection of invasive breast
cancer.
3 of 149 cancers (2%) were not identified with BSGI.
All three were grade 1 infiltrating duct carcinomas, and
all were #0.7 cm (0.7, 0.7 and 0.4 cm). All cancers that
were grade 2 or 3, regardless of size, and all cancers that
were .0.7 cm, regardless of grade, were identified by
BSGI.
The sensitivity of BSGI for invasive ductal carcinoma
was 97.6% (123/126) with 100% sensitivity for the
remaining pathological subtypes of cancer (Table 2).
4 of 149 (2.7%) infiltrating ductal carcinomas were
multifocal. BSGI correctly identified all cases of multifocal breast cancer.
The sensitivity for cancers .0.7 cm was 100% (105/105),
whereas cancers #0.7 cm demonstrated a sensitivity of
Figure 4. Craniocaudal view of a 48-year-old female with
Figure 3. Mediolateral oblique view showing infiltrating
lobular carcinoma in the upper right breast of a 54-year-old
female: 6 cm; grade 2 of 3.
e214
multifocal infiltrating ductal carcinoma of the left breast
seen as separate areas of increased radiotracer uptake: 1.2
and 1.0 cm; grade 3 of 3.
The British Journal of Radiology, June 2012
Breast-specific gamma imaging for the diagnosis of invasive cancer
Table 2. Sensitivity of breast-specific gamma imaging by
pathological subtype of cancer
Table 4. Sensitivity of breast-specific gamma imaging in the
detection of invasive cancers by tumour grade
Type
Percentage
Grade
Percentage
Infiltrating ductal carcinoma
Infiltrating lobular carcinoma
Mixed infiltrating ductal and infiltrating
lobular carcinoma
Mucinous carcinoma
Tubulolobular carcinoma
Infiltrating tubular carcinoma
Infiltrating papillary carcinoma
Medullary carcinoma
97.6
100
100
3
2
1
100
100
83.3
100
100
100
100
100
88.5% (21/24) (Table 3). Cancers which were pathologically
grade 2 and 3 had a sensitivity of 100% (102/102)
regardless of cancer size, whereas grade 1 cancers had a
sensitivity of 83.3% (15/18) (Table 4). Of the 6 cancers that
were grade 1 and #7 mm, BSGI demonstrated 3 of the 6, to
give a sensitivity of 50%.
Discussion
The use of physiological imaging as an adjunct
imaging modality for breast cancer detection can
improve breast cancer detection. The purpose of this
study was to evaluate the sensitivity of BSGI in the
diagnosis of invasive breast cancer and to correlate these
findings with pathological cancer size and grade. Our
study demonstrates that BSGI has a high sensitivity
(98%) for the detection of all invasive breast cancers.
Interestingly, BSGI detected invasive cancers with some
dependency upon tumour size and grade. All cancers of
grade 2 or 3 were detected, regardless of size and as
small as 2 mm. Furthermore, all cancers, whether they
were grade 1, 2 or 3, were detected with BSGI if they
were $7 mm. The only cancers not detected were 3/6
grade 1 cancers that were #7 mm. The reason these three
grade 1, subcentimetre cancers were not identified with
BSGI is not known. However, it is likely that the biology
of these cancers resulted in their non-visualisation with
BSGI. It is of note that the three cancers which were not
detected with BSGI were all low-grade, small cancers;
cancers which are probably of the least clinical significance. As BSGI is increasingly being integrated in clinical
practice, it is noteworthy that all of those cancers that are
likely to be of the greatest clinical significance, that is,
higher grade cancers, were identified with BSGI.
Table 3. Sensitivity of breast-specific gamma imaging in the
detection of invasive cancers by largest pathological size
Size (cm)
Percentage
.7.1
5.17.0
3.15.0
1.13.0
0.811.0
0.610.8
0.410.6
0.210.4
,0.2
100
100
100
100
100
77.8
100
75
100
The British Journal of Radiology, June 2012
MRI is used as an adjunct imaging modality for the
detection of invasive breast cancer. Kuhl et al [20] have
demonstrated that MRI has a sensitivity of 92% for the
detection of DCIS. This is comparable to the recent report
of the sensitivity of BSGI for the detection of DCIS, which
demonstrated a sensitivity of 91% [17]. The similarity in
the detection of DCIS with both MRI and BSGI suggests
that these two physiological-based approaches are comparable in sensitivity [21]. Similarly, this study demonstrated comparable sensitivity of BSGI to MRI for the
diagnosis of invasive breast cancer [22]. It is important to
note that MRI is performed without ionising radiation
and BSGI uses a low-dose radiotracer that has safely
been used in medical imaging for decades with ongoing
studies aimed at further decreasing the dose. Nevertheless, there are advantages to imaging with BSGI. Patients
imaged with BSGI are comfortably seated as compared
with prone in the MRI scanner, and there is no concern
with claustrophobic patients with BSGI. Additionally,
the BSGI examination generates 410 images as compared with 1000 images obtained with breast MRI.
Although there has not been a formal study comparing
the time for radiologist interpretation of MRI and BSGI
examinations, it has been our experience that interpretation of BSGI examinations requires far less time for
interpretation than breast MRI examinations. Further,
nephrogenic systemic fibrosis is not an issue with BSGI.
Although this study did not address the cost of BSGI, nor
was it a comparison with MRI, the cost of a BSGI examination is typically half that of a breast MRI examination.
Additional studies investigating the cost-effectiveness of
MRI and BSGI are needed to better define and compare
BSGI and MRI.
Our study demonstrated that the four multifocal
infiltrating ductal carcinomas were correctly identified
with BSGI. This concurs with recent reports indicating
that BSGI can detect additional foci of occult cancers in
females with one known cancer [13, 22, 23].
BSGI was able to diagnose all pathological subtypes of
invasive breast cancer with 97.6% sensitivity and all
other subtypes of breast cancer with 100% sensitivity.
The three cancers not detected by BSGI were all invasive
ductal carcinoma. However, this is likely to be the result
of the preponderance of this pathological type of
invasive cancer both in our study and in clinical practice.
The limited number of other pathological subtypes of
invasive breast cancer that were not of ductal origin is a
limitation of this study, and is undoubtedly the cause for
the 100% sensitivity of invasive breast cancer not of
ductal origin. Furthermore, a recent report describing the
sensitivity of BSGI in the detection of invasive lobular
carcinoma involving 28 biopsy-proven cancers reported
a 93%, and not 100% sensitivity [24]. Additional larger
studies are needed to more definitively identify the
e215
R V Tadwalkar, J A Rapelyea, J Torrente et al
sensitivity of BSGI in the detection of invasive breast
cancer that is not of ductal origin.
There are limitations to this study. Firstly, it is a
retrospective study. It would be optimal to design and
undertake a prospective trial evaluating the sensitivity of
BSGI in the diagnosis of invasive breast cancer. However, a retrospective approach to study new modalities
for the diagnosis of breast cancer has been used in
evaluating other emerging imaging modalities. Prospective trials investigating BSGI are under way and should
further our understanding of the use of BSGI as an
adjunct imaging modality for the diagnosis of breast
cancer. Secondly, indications for study patients referrals for BSGI were varied and could therefore
introduce bias. Nevertheless, this study, which is the
largest to date evaluating invasive breast cancer with
BSGI, has demonstrated the high sensitivity of BSGI in
the diagnosis of all subtypes, sizes and grades of invasive
breast cancer and even with its limitations increases our
understanding of BSGI in the diagnosis of breast cancer.
Conclusion
Our study demonstrated that BSGI has a very high
sensitivity for all sizes and grades of invasive breast
cancer. In fact, all breast cancers which were grade 2 or 3
and which measured $8 mm or greater were detected
with BSGI and only a subset of invasive breast cancers
that were ,8 mm and grade 1 were not seen with BSGI.
Therefore, BSGI is a highly reliable imaging modality
for the detection of clinically significant invasive breast
cancers.
References
1. Rosenberg RD, Hunt W, Williamson M, Gilliland FD, Wiest
PW, Kelsey CA, et al. Effects of age, breast density,
ethnicity, and estrogen replacement therapy on screening
mammographic sensitivity and cancer stage at diagnosis:
review of 183,134 screening mammograms in Albuquerque,
New Mexico. Radiology 1998;209:51118.
2. Kolb T, Lichy J, Newhouse J. Comparison of the performance of screening mammography, physical examination,
and breast US and evaluation of factors that influence them:
an analysis of 27, 825 patient evaluations. Radiology
2002;225:16575.
3. Mandelson MT, Oestreicher N, Porter PL, White D, Finder
CA, Taplin SH, et al. Breast density as a predictor of
mammographic detection: comparison of interval- and
screen-detected cancers. J Natl Cancer Inst 2000;92:10817.
4. Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK,
Acharyya S, et al. Diagnostic performance of digital versus
film mammography for breast-cancer screening. N Engl J
Med 2005;353:17738.
5. Khalkhali I, Mena I, Jouanne E, Diggles L, Venegas R, Block
J, et al. Prone scintimammography in patients with
suspicion of carcinoma of the breast. J Am Coll Surg
1994;178:4917.
6. Khalkhali I, Cutrone J, Mena I, Diggles LE, Venegas RJ,
Vargas HI, et al. Scintimammography: the complementary
role of Tc-99m sestamibi prone breast imaging for the
diagnosis of breast carcinoma. Radiology 1995;196:4216.
7. Tallifer R. Clinical applications of 99mTc-sestamibi scintimammography. Semin Nucl Med 2005;35:10015.
e216
8. Mekhmandarov S, Sandbank J, Cohen M, Lelcuk S, Lubin E.
Technetium 99-m MIBI scintimammography in palpable
and nonpalpable breast lesions. J Nucl Med 1998;39:8691.
9. Arslan N, Ozturk E, Ilgan S, Urhan M, Karacalioglu O,
Pekcan M, et al. Tc-99m MIBI scintimammography in the
evaluation of breast lesions and axillary involvement: a
comparison with mammography and histopathological
diagnosis. Nucl Med Commun 1999;20:31725.
10. Fenlon H, Phelan N, OSullivan P, Tierney S, Gorey T, Ennis
J. Benign versus malignant breast disease: comparison of
contrast-enhanced MR imaging and Tc-99m tetrofosmin
scintimammography. Radiology 1997;205:21420.
11. Palmedo H, Bender H, Grunwald F, Mallmann P, Zamora
P, Krebs D, et al. Comparison of fluorine-18 fluorodeoxyglucose positron emission tomography and technetium99m methoxyisobutylisonitrile scintimammography in the
detection of breast tumors. Eur J Nucl Med 1997;24:113845.
12. Majewski S, Kieper D, Curran E, Kieper D, Kross B,
Pulumbo A, et al. Optimization of dedicated scintimammography procedure using detector prototypes and compressible phantoms. IEEE Trans Nucl Sci 2001;48:8229.
13. Brem R, Floerke A, Rapelyea J, Teal C, Kelly T, Mathur V.
Breast-specific gamma imaging as an adjunct imaging
modality for the diagnosis of breast cancer. Radiology
2008;247:6517.
14. Brem RF, Michener KH, Zawistowski G. Approaches to
improving breast cancer diagnosis using a high resolution,
breast specific gamma camera. Phys Med 2006;21(Suppl.
1):1719.
15. Brem R, Schoonjans J, Kieper D, Majewski S, Goodman S,
Civelek C. High-resolution scintimammography: a pilot
study. J Nucl Med 2002;43;90915.
16. Coover L, Caravaglia G, Kuhn P. Scintimammography with
dedicated breast camera detects and localizes occult
carcinoma. J Nucl Med 2004;45:5538.
17. Brem RF, Fishman M, Rapelyea JA. Detection of ductal
carcinoma in situ with mammography, breast specific
gamma imaging, and magnetic resonance imaging: a
comparative study. Acad Radiol 2007;14:94550.
18. Gail M, Brinton L, Byar D, Corle DK, Green SB, Schairer C,
et al. Projecting individualized probabilities of developing
breast cancer for white females who are being examined
annually. J Natl Cancer Inst 1989;81:187986.
19. Werner J, Rapelyea JA, Yost KG, Brem RF. Quantification of
radio-tracer uptake in axillary lymph nodes using breast
specific gamma imaging (BSGI): benign radio-tracer extravasation versus uptake secondary to breast cancer. Breast J
2009;15:57982.
20. Kuhl C, Schrading M, Bieling M, Wardelmann E, Leutner
CC, Koenig R, et al. MRI for diagnosis of pure ductal
carcinoma in situ: a prospective observational study. Lancet
2007;370:48592.
21. Brem R, Petrovitch I, Rapelyea J, Young H, Teal C, Kelly T.
Breast-specific gamma imaging with 99mTc-Sestamibi and
magnetic resonance imaging in the diagnosis of breast
cancer: a comparative study. Breast J 2007;13:4659.
22. Cwikla J, Buscombe J, Holloway B, Parbhoo SP, Davidson
T, McDermott N, et al. Can scintimammography with
99mTc-MIBI identify multifocal and multicentric primary
breast cancer? Nucl Med Commun 2001;22:128793.
23. Brem RF, Shahan C, Rapelyea JA, Donnelly CA, Rechtman
LR, Kidwell AB, et al. Detection of occult foci of breast
cancer using breast-specific gamma imaging in women
with one mammographic or clinically suspicious breast
lesion. Acad Radiol 2010;17:73543.
24. Brem RF, Ioffe M, Rapelyea JA, Yost KG, Weigert JM,
Bertrand ML, et al. Invasive lobular carcinoma: detection
with mammography, sonography, MRI, breast specific
gamma imaging. AJR Am J Roentgenol 2009;192:37983.
The British Journal of Radiology, June 2012
S-ar putea să vă placă și
- A Cross-Sectional Population-Based Survey of Trachoma Among Migrant School Aged Children in Shanghai, ChinaDocument8 paginiA Cross-Sectional Population-Based Survey of Trachoma Among Migrant School Aged Children in Shanghai, ChinaTher RayÎncă nu există evaluări
- Medial Cranial Fossa Meningioma Diagnosed As Mixed Anxiety Disorder With Dissociative Symptoms and VertigoDocument4 paginiMedial Cranial Fossa Meningioma Diagnosed As Mixed Anxiety Disorder With Dissociative Symptoms and VertigoTher RayÎncă nu există evaluări
- Isolation, Identification, and in Vitro Antifungal Susceptibility Testing of Dermatophytes From Clinical Samples at Sohag University Hospital in EgyptDocument11 paginiIsolation, Identification, and in Vitro Antifungal Susceptibility Testing of Dermatophytes From Clinical Samples at Sohag University Hospital in EgyptTher Ray100% (1)
- Eappendix. Radiological Screening Methods For MammographyDocument8 paginiEappendix. Radiological Screening Methods For MammographyTher RayÎncă nu există evaluări
- Genetic Suppression Reveals DNA Repair-Independent Antagonism Between BRCA1 and COBRA1 in Mammary Gland DevelopmentDocument9 paginiGenetic Suppression Reveals DNA Repair-Independent Antagonism Between BRCA1 and COBRA1 in Mammary Gland DevelopmentTher RayÎncă nu există evaluări
- Skin Disease and Thyroid Autoimmunity in Atopic South Italian ChildrenDocument6 paginiSkin Disease and Thyroid Autoimmunity in Atopic South Italian ChildrenTher RayÎncă nu există evaluări
- Environmentally Endemic Pseudomonas Aeruginosa Strains With Mutations in Lasr Are Associated With Increased Disease Severity in Corneal UlcersDocument14 paginiEnvironmentally Endemic Pseudomonas Aeruginosa Strains With Mutations in Lasr Are Associated With Increased Disease Severity in Corneal UlcersTher RayÎncă nu există evaluări
- Inhibitory Effect of Valencene On The Development of Atopic Dermatitis-Like Skin Lesions in NC/Nga MiceDocument11 paginiInhibitory Effect of Valencene On The Development of Atopic Dermatitis-Like Skin Lesions in NC/Nga MiceTher RayÎncă nu există evaluări
- Quantitative Proteomic Analyses of Mammary Organoids Reveals Distinct Signatures After Exposure To Environmental ChemicalsDocument9 paginiQuantitative Proteomic Analyses of Mammary Organoids Reveals Distinct Signatures After Exposure To Environmental ChemicalsTher RayÎncă nu există evaluări
- Prevalence of Tinea Capitis Among School Children in Nok Community of Kaduna State, NigeriaDocument6 paginiPrevalence of Tinea Capitis Among School Children in Nok Community of Kaduna State, NigeriaTher RayÎncă nu există evaluări
- Aquagenic Palmoplantar Keratoderma With Dorsal Hand Involvement in An Adolescent FemaleDocument2 paginiAquagenic Palmoplantar Keratoderma With Dorsal Hand Involvement in An Adolescent FemaleTher RayÎncă nu există evaluări
- The first Danish family reported with an AQP5 mutation presenting diffuse nonepidermolytic palmoplantar keratoderma of Bothnian type, hyperhidrosis and frequent Corynebacterium infections: a case reportDocument6 paginiThe first Danish family reported with an AQP5 mutation presenting diffuse nonepidermolytic palmoplantar keratoderma of Bothnian type, hyperhidrosis and frequent Corynebacterium infections: a case reportTher RayÎncă nu există evaluări
- Pyogenic Arthritis, Pyoderma Gangrenosum, Acne, Suppurative Hidradenitis (PA-PASH) Syndrome: An Atypical Presentation of A Rare SyndromeDocument5 paginiPyogenic Arthritis, Pyoderma Gangrenosum, Acne, Suppurative Hidradenitis (PA-PASH) Syndrome: An Atypical Presentation of A Rare SyndromeTher RayÎncă nu există evaluări
- Protective and Therapeutic Effects of Fucoxanthin Against Sunburn Caused by UV IrradiationDocument10 paginiProtective and Therapeutic Effects of Fucoxanthin Against Sunburn Caused by UV IrradiationTher RayÎncă nu există evaluări
- Pyogenic Arthritis, Pyoderma Gangrenosum, Acne, Suppurative Hidradenitis (PA-PASH) Syndrome: An Atypical Presentation of A Rare SyndromeDocument5 paginiPyogenic Arthritis, Pyoderma Gangrenosum, Acne, Suppurative Hidradenitis (PA-PASH) Syndrome: An Atypical Presentation of A Rare SyndromeTher RayÎncă nu există evaluări
- Successful Treatment of Pyoderma Gangrenosum With Cryoglobulinemia and Hepatitis CDocument5 paginiSuccessful Treatment of Pyoderma Gangrenosum With Cryoglobulinemia and Hepatitis CTher RayÎncă nu există evaluări
- Pattern of Pediatric Dermatoses in A Tertiary Care Hospital of Western NepalDocument5 paginiPattern of Pediatric Dermatoses in A Tertiary Care Hospital of Western NepalTher RayÎncă nu există evaluări
- The Effects of Yoga On Shoulder and Spinal Actions For Women With Breast Cancerrelated Lymphoedema of The Arm: A Randomised Controlled Pilot StudyDocument15 paginiThe Effects of Yoga On Shoulder and Spinal Actions For Women With Breast Cancerrelated Lymphoedema of The Arm: A Randomised Controlled Pilot StudyTher RayÎncă nu există evaluări
- Protective and Therapeutic Effects of Fucoxanthin Against Sunburn Caused by UV IrradiationDocument10 paginiProtective and Therapeutic Effects of Fucoxanthin Against Sunburn Caused by UV IrradiationTher RayÎncă nu există evaluări
- O Efeito Antibacterino Das Xantonas Do MangostãoDocument3 paginiO Efeito Antibacterino Das Xantonas Do MangostãoSaude PositivaÎncă nu există evaluări
- Evolution and Adaptation of H5N1 Influenza Virus in Avian and Human Hosts in Indonesia and VietnamDocument11 paginiEvolution and Adaptation of H5N1 Influenza Virus in Avian and Human Hosts in Indonesia and VietnamTher RayÎncă nu există evaluări
- Phenotypic and Marker-Assisted Genetic Enhancement of Parental Lines of Rajalaxmi, An Elite Rice HybridDocument11 paginiPhenotypic and Marker-Assisted Genetic Enhancement of Parental Lines of Rajalaxmi, An Elite Rice HybridTher RayÎncă nu există evaluări
- Prognostic Factor Analysis of Intraocular Pressure With Neovascular GlaucomaDocument10 paginiPrognostic Factor Analysis of Intraocular Pressure With Neovascular GlaucomaTher RayÎncă nu există evaluări
- X AntiOxidants Agriculture FoodChemistry OhioStateDocument6 paginiX AntiOxidants Agriculture FoodChemistry OhioStateTher RayÎncă nu există evaluări
- Abdominal Organ Involvement in Blunt InjuriesDocument3 paginiAbdominal Organ Involvement in Blunt InjuriesTher RayÎncă nu există evaluări
- Assessment of The Antidiabetic Potential of An Aqueous Extract of Honeybush (Cyclopia Intermedia) in Streptozotocin and Obese Insulin Resistant Wistar RatsDocument21 paginiAssessment of The Antidiabetic Potential of An Aqueous Extract of Honeybush (Cyclopia Intermedia) in Streptozotocin and Obese Insulin Resistant Wistar RatsTher RayÎncă nu există evaluări
- Three Indonesian Clusters of H5N1 Virus Infection in 2005: Original ArticleDocument9 paginiThree Indonesian Clusters of H5N1 Virus Infection in 2005: Original ArticleTher RayÎncă nu există evaluări
- Ginkgo Biloba Extract in Alzheimer's Disease: From Action Mechanisms To Medical PracticeDocument17 paginiGinkgo Biloba Extract in Alzheimer's Disease: From Action Mechanisms To Medical PracticeTher RayÎncă nu există evaluări
- Teori PerilakuDocument21 paginiTeori Perilakuslaisa100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- FAST Functional Scale dementia criteria hospiceDocument2 paginiFAST Functional Scale dementia criteria hospicepowerbread780% (2)
- Public Availability of Labeling CBE Guidance PDFDocument6 paginiPublic Availability of Labeling CBE Guidance PDFMichael wangÎncă nu există evaluări
- Mcdonalds Case Study Final ArtifactDocument10 paginiMcdonalds Case Study Final Artifactapi-340015164Încă nu există evaluări
- 5150 Holds in San Diego CountyDocument28 pagini5150 Holds in San Diego CountynoxinqwertyÎncă nu există evaluări
- Ah102 Syllabus 20180417lDocument7 paginiAh102 Syllabus 20180417lapi-399629502Încă nu există evaluări
- Nursing Care Plans For Diabetes MellitusDocument12 paginiNursing Care Plans For Diabetes MellitusRaveen mayi85% (59)
- Social Marketing in Public HealthDocument23 paginiSocial Marketing in Public HealthNurab MartinsÎncă nu există evaluări
- Hormone Therapy IfmDocument16 paginiHormone Therapy IfmRamy LasheenÎncă nu există evaluări
- Neo JaundiceDocument67 paginiNeo Jaundicemanisha thakur100% (1)
- L3 U1 Working As A Close Protection Operative - Dec09Document19 paginiL3 U1 Working As A Close Protection Operative - Dec09twisterxxÎncă nu există evaluări
- Oral Sex - A Closer LookDocument9 paginiOral Sex - A Closer LookiantorresÎncă nu există evaluări
- Snigdha Dasgupta Sexual DisorderDocument13 paginiSnigdha Dasgupta Sexual DisorderSNIGDHA DASGUPTAÎncă nu există evaluări
- Laurie Curtis and Melody RieferDocument5 paginiLaurie Curtis and Melody RieferdwellintheheartÎncă nu există evaluări
- Jejunostomy Feeding Tube Placement in GastrectomyDocument14 paginiJejunostomy Feeding Tube Placement in GastrectomyHarshit UdaiÎncă nu există evaluări
- White Paper Drugdelivery Needles Need Less MinDocument13 paginiWhite Paper Drugdelivery Needles Need Less MinAmit PaulÎncă nu există evaluări
- FMTDocument29 paginiFMTCynfully SweetÎncă nu există evaluări
- Neurological Assessment 1 - Assessing Level of ConsciousnessDocument1 paginăNeurological Assessment 1 - Assessing Level of ConsciousnesskyawswakyawswaÎncă nu există evaluări
- Functions of Agriculture DronesDocument2 paginiFunctions of Agriculture DronesShahraz AliÎncă nu există evaluări
- Agriculture, biotech, bioethics challenges of globalized food systemsDocument28 paginiAgriculture, biotech, bioethics challenges of globalized food systemsperoooÎncă nu există evaluări
- HFpEF Management 2023Document10 paginiHFpEF Management 2023ctsakalakisÎncă nu există evaluări
- The ICF-CY model as a framework for pediatric rehabilitationDocument2 paginiThe ICF-CY model as a framework for pediatric rehabilitationAtet KurniadiÎncă nu există evaluări
- Alternative SystemDocument26 paginiAlternative Systemsameena vÎncă nu există evaluări
- BARITEDocument6 paginiBARITEsajad gohariÎncă nu există evaluări
- Nursing Care PlanDocument10 paginiNursing Care PlanGinel Laquiores100% (1)
- Measuring Burnout 2009Document23 paginiMeasuring Burnout 2009Eduardo Denise100% (1)
- TRACTIONDocument3 paginiTRACTIONCatherineÎncă nu există evaluări
- Ejaculation by Command - Lloyd Lester - Unstoppable StaminaDocument21 paginiEjaculation by Command - Lloyd Lester - Unstoppable StaminaEstefania LopezÎncă nu există evaluări
- Speech & Language Therapy in Practice, Spring 1998Document32 paginiSpeech & Language Therapy in Practice, Spring 1998Speech & Language Therapy in PracticeÎncă nu există evaluări
- Bed Side Conference: College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Document2 paginiBed Side Conference: College of The Holy Spirit of Manila 163 E. Mendiola ST., Manila Telefax: (02) 7347921Jen GarzoÎncă nu există evaluări
- Atls Pre Test SolvedDocument18 paginiAtls Pre Test SolvedDr.Mukesh KumarÎncă nu există evaluări