Documente Academic
Documente Profesional
Documente Cultură
Review On Pathogenesis of Pemphigus: Dr. P. T. Chan Social Hygiene Service (Dermatology), Department of Health, Hong Kong
Încărcat de
Meuthia AlamsyahTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Review On Pathogenesis of Pemphigus: Dr. P. T. Chan Social Hygiene Service (Dermatology), Department of Health, Hong Kong
Încărcat de
Meuthia AlamsyahDrepturi de autor:
Formate disponibile
Review Articles
Review on Pathogenesis of Pemphigus
Dr. P. T. Chan
Social Hygiene Service (Dermatology), Department of Health, Hong Kong
ABSTRACT
With recent advances in laboratory techniques, the pathogenesis of pemphigus has been better understood.
The common mechanism involves the development of antibodies against desmosomal proteins. Different clinical,
pathological and immunological features define the subgroups of pemphigus diseases. This review article
will summarize the current knowledge on the pathogenesis of pemphigus, with emphasis on the different
antigens involved in the autoimmune process. The mechanism of immune intolerance leading to recognition
of self-antigens is still unknown.
Keywords: Antigens, pathogenesis, pemphigus, review
INTRODUCTION
Pemphigus (from the Greek pemphix, meaning
bubble or blister) is a blistering disease involving
the skin and mucous membrane. The disease is
characterized histologically by acantholysis
which means loss of adhesion between keratinocytes,
and immuno-pathologically by the presence of
immunoglobulin directed towards the cell surface of
ker a t i n o cy t e s . 1 T h e l a n d m a r k a r t i c l e i n t h e
understanding of pathogenesis of pemphigus was
published in 1964, which demonstrated the presence
of anti-skin antibodies in the sera of pemphigus
patients by indirect immunofluorescence staining. 2
Since then, with the improvement in immunological
techniques, the antigens responsible for the disease
were identified. These medical advances not
only provide us with a better knowledge of the
pathogenesis of pemphigus but also lead to the
development of recombinant proteins, which are
employed in enzyme linked immunosorbent assay
(ELISA) for the diagnosis of pemphigus.
Correspondence address:
Dr. P. T. Chan
Cheung Sha Wan Dermatology Clinic
3/F, West Kowloon Health Centre
303 Cheung Sha Wan Road
Kowloon
Hong Kong
62
Hong Kong Dermatology & Venereology Bulletin
Pemphigus comprises a group of autoimmune
skin diseases. The two major groups are pemphigus
vulgaris (PV) and pemphigus foliaceus (PF). Their
difference lies in the level of acantholysis, with
the former in the suprabasilar level and the latter
in the subcorneal level. Recently, new forms of
pemphigus have been described, namely pemphigus
herpetiformis, IgA pemphigus and paraneoplastic
pemphigus (PNP). 3 This article reviews the current
understanding in the antigens involved (Table 1) and
the pathogenesis of these entities.
THE STRUCTURE OF DESMOSOME
It is essential to have a basic knowledge of the
desmosome in order to understand the pathogenesis of
pemphigus. Desmosomes (or maculae adherens) are
organelles responsible for cell-to-cell adhesion in
keratinocytes. The extra cellular part, desmoglea, is
composed of transmembrane adhesion glycoproteins
belonging to the cadherin superfamily, which includes
desmogleins and desmocollins. The intracellular part,
desmosomal plaques, has two groups of proteins. The
first group, plakin family (desmoplakins, envoplakin,
periplakin, plectin), binds to cytokeratin filaments. The
second group of proteins, namely plakoglobin and
plakophilin, bind to the intracellular domain of
cadherins. The pemphigus antibodies bind to the
antigens in the desmosome and hence resulting in
acantholysis.4
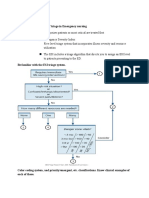
Review Articles
Table 1. Antigens in various pemphigus diseases
Pemphigus type
Superficial pemphigus
Pemphigus foliaceus
Endemic pemphigus (Fogo Selvagem)
Pemphigus vulgaris
Mucosal involvement
Mucocutaneous type
Antigens targeted by antibodies
Desmoglein 1 (160 kD)
Desmoglein 1 (160 kD)
Desmoglein 3 (130 kD)
Desmoglein 1 (160 kD) and
Desmoglein 3 (130 kD)
Paraneoplastic pemphigus
Desmoplakin I (250 kD)
Bullous pemphigoid antigen I (230 kD)
Desmoplakin II (210 kD)
Envoplakin (210 kD)
Periplakin (190 kD)
Unknown (170 kD)
Desmoglein 1 (160 kD)
Desmoglein 3 (130 kD)
Pemphigus herpetiformis
Desmoglein 1 (160 kD)
Desmoglein 3 (130 kD)
IgA pemphigus
Subcorneal pustular dermatosis type
Intraepithelial type
THE PATHOGENICITY OF
PEMPHIGUS ANTIBODIES
Clinical observations
There are several clinical observations that suggest
pemphigus is an antibody mediated disease.1 Firstly,
there is a correlation between disease activity and
antibody titres in both PV and PF. Secondly, neonates
born by women with active PV may develop a selflimiting form of pemphigus disease that terminates
spontaneously with the clearance of maternal antibodies.
Children of mother with active PF, however, seldom
develop neonatal pemphigus because of the difference
in desmoglein composition between neonatal and adult
skin (see section on desmoglein compensation
hypothesis).
Experimental models
In vitro models utilizing skin explants and cultured
keratinocytes have demonstrated the acantholytic effects
Desmocollin I (105-115 kD)
Unknown, some cases desmoglein 3 & 1
of pemphigus antibodies. 5 Animal models have also
been developed for the investigation of disease
pathogenesis. Anhalt et al was able to reproduce blisters
in neonatal mice by daily intraperitoneal injection of
pemphigus serum. 6 These blisters were histopathologically similar to the human counterpart. Besides
PV, passive transfer of disease by intraperitoneal IgG
injection has been performed for PF and PNP. 4
Moreover, by transferring antibodies affinity-purified
on different recombinant desmoglein fragments, it was
shown that the pathogenic antibodies were directed to
the extracellular part of desmogleins.7 Passive transfer
of pemphigus has also been achieved in severe combined
immunodeficiency disease mice by grafting with human
skin and reconstitution with peripheral blood
lymphocyte from patient.8 The other two animal models
belong to the active group, in which pathogenic
antibodies are generated by immunization of animals
with desmoglein. Thus, BALB/c mice synthesize blisterproducing antibodies upon immunization with
recombinant human desmoglein 3.9 And Rag-/- mice
Vol.10 No.2, June 2002
63
Review Articles
developed cutaneous and mucosal disease when they
were given splenocytes from desmoglein 3 knockout
mice immunized with mouse desmoglein 3.10 Besides
helping us to understand the pathogenesis of disease,
these animal models provide us with the opportunity
for evaluation of new treatment.
The pemphigus antibodies
Direct immunofluorescence examination of
lesional skin from patient with pemphigus shows
staining on the surface of keratinocyte, indicating the
presence of immunoglobulins on these cells. Patients
with PV and PF may display similar direct
immunofluorescence findings on IgG on the cell surface
throughout the epidermis. Therefore the two diseases
cannot be separated by the pattern of immunofluorescence in all cases.1 The deposited immunoglobulins are mainly IgG, with IgG1 and IgG4
predominate. Indirect immunofluorescence study also
revealed that circulating antibodies are mainly IgG1 and
IgG4.4 Support for the pathogenic importance of IgG4
lies on the fact that IgG4 is the major antibody in active
PV cases while IgG1 remains detectable in remitted
cases. 4 Moreover, in comparing antidesmoglein
antibody subclass in pemphigus patients and their
healthy relatives, IgG4 was the only one that was found
to be significantly lowered in the relative group.11 But
IgG4, unlike IgG1 to IgG3, does not bind complement.
As complement deposition is usually present in active
cases of PV, a combination of IgG subclasses seems to
be necessary in the formation of blister.11 A more recent
finding is the presence of desmoglein 3 reactive IgA
and IgE in pemphigus patient with active disease by
using baculovirus expressed desmoglein 3 in an
immunoblot assay.12 As the concentration of desmoglein
3 reactive IgA and IgE is much lower than that of IgG1
and IgG4, the pathological importance of these antibody
subclasses in blister formation remain to be determined.
In pemphigus herpetiformis, 3 IgG is found
primarily in the upper epidermis. The IgG4 subclass is
the predominant type of in vivo bound and circulating
antibody. In IgA pemphigus,3 IgA is deposited on to
keratinocyte cell surface in all cases. In the subcorneal
pustular dermatosis (SPD) type of IgA pemphigus, IgA
deposition occurs on the upper epidermal cell surfaces,
whereas in the intraepidermal neutrophilic (IEN) type
of IgA pemphigus, the deposition occurs in the lower
epidermis or throughout the entire epidermis. The
64
Hong Kong Dermatology & Venereology Bulletin
subclass of IgA antibody belongs to IgA1. In PNP, 3
direct immunofluorescence of perilesional skin shows
IgG deposition along the basement membrane zone and
on the keratinocyte surface. The IgG subclasses are
found in the following descending order: IgG1, IgG2,
IgG4 and IgG3. Unlike PV sera, PNP sera can bind to
nonstratified epithelium (such as rodent urinary bladder)
as well as stratified squamous epithelium because of
their antigens specificity (see section on pemphigus
antigens).13
THE PEMPHIGUS ANTIGENS
Antigens in pemphigus vulgaris and foliaceus4
Immunoprecipitation assays using keratinocyte
extracts identified 210 kD complex and 260 kD complex
in PV and PF respectively. The 210 kD complex is
composed of a 130 kD protein named desmoglein 3 and
a 85 kD protein named plakoglobin. The 260 kD
complex is composed of a 165 kD protein named
desmoglein 1 and a 85 kD plakoglobin. Immunoblotting
experiment has shown the desmoglein 1 and 3 are the
only part of the complex recognized by patients with
PF and PV respectively, and the plakoglobin is
coprecipitated. Cloning and sequencing of the
desmogleins 1 and 3 genes have confirmed that they
has high sequence homology and belong to the cadherin
family.
The desmoglein compensation hypothesis14
The desmoglein compensation hypothesis has been
proposed to explain the localization of lesions of PV
and PF. In PF, blisters occur at the granular layer of
superficial epidermis, and the mucus membrane is not
involved. In PV, two third of the patients develop blisters
over the mucous membrane and then the blisters develop
over the skin as well, the histological cleavage is located
at the basal and suprabasal levels of epidermis.
Desmoglein 1 is expressed mostly in the upper
epidermis. As antibody to desmoglein 1 is present in
PF, acantholysis develops in the superficial epidermis.
Because of the coexpression of desmoglein 3 in mucous
membrane and lower epidermis of skin, these sites are
spared. In PV, the antibody to desmoglein 3 causes
acantholysis in the mucous membranes, as desmoglein
3 is the major cadherin expressed in these sites. Later
as the disease progresses, many patients will experience
cutaneous disease, at the time when antibodies to both
Review Articles
desmoglein 3 and 1 develop.15 The development of
additional antibodies in the disease course may represent
an example of 'epitope spreading' seen in autoimmune
disease.15
The desmoglein compensation hypothesis is also
supported by experimental study, in which pemphigus
antibodies are passively transferred to normal and
desmoglein 3null neonatal mice.16 In areas of epidermis
coexpressing both desmoglein 1 and 3, antibodies to
either one desmoglein do not induce blister, but
antibodies to both desmogleins do. In areas of epidermis
where only desmoglein 1 is present, antibody to
desmoglein 1 alone can induce blister. This hypothesis
explains the clinical and microscopic localization of
blister in pemphigus. It also allows the prediction of
antibody profile from clinical phenotype:17 antibody to
desmoglein 1 in PF, antibody to desmoglein 3 in mucosal
predominant PV, antibody to desmoglein 1 and 3 in
mucocutaneous PV.
Desmoglein 1 antibody causes PF in adults, but
the transplacental passage of this antibody does not
produce disease in neonate. This is different from the
case in PV, when transplacental passage of desmoglein
antibody causes neonatal disease. Neonates from PF
mother are free from the blistering disease because of
the presence of both desmoglein 1 and desmoglein 3 on
the cell surface of superficial and basal keratinocytes.18
Pemphigus antigens other than desmoglein
The pathogenesis of pemphigus has been so well
characterized as above with the desmoglein
compensation hypothesis that explains the clinical,
immunological and pathological aspects of pemphigus.
Nonetheless, there are several observations that remain
to be explained. There are about 20 self-antigens, the
number of which depends on patient status and the
detection technique, that react with pemphigus IgGs.
In experimental study, PV serum (which only contains
anti-desmoglein 3 activity but not anti-desmoglein 1
activity) can induce blisters even in desmoglein 3
deficient mice. Therefore, although desmoglein 1 may
compensate for the absence of desmoglein 3, the effect
of pemphigus serum cannot be ascribed by a blockade
of desmoglein 1 alone.19
The presence of antibodies to keratinocyte
cholinergic receptors, including pemphaxin and a
50 kD -9 acetylcholine receptor, has been recently
demonstrated to be present in pemphigus sera.20 Both
antibodies induce acantholysis in keratinocyte culture,
but do not induce blister in vivo. Human keratinocytes
express cholinergic receptors of both nicotinic and
muscarinic classes; stimulation of either receptor can
alter the adhesive interaction of keratinocytes at least in
part by the regulation of intracellular calcium level.
Recent studies showed that calcium mediated actin
polymerization is the major driving force for cell to cell
adhesion and the assembly of desmosomes is a passive
process that occurs when stable cell contact is made.21
The importance of calcium in mediating cellular
adhesion is also demonstrated by two acantholytic
disease, Darier's disease and Hailey-Hailey disease.
Mutation of the ATP2A2 occurs in Darier's disease22 and
mutation of ATP2C1 occurs in Hailey-Hailey disease,23
in both diseases the gene products are calcium pumps.
Further research is needed to determine whether there
is an active role of these non-desmoglein antibodies in
the pathogenesis of pemphigus or whether they are just
'bystander' in the phenomenon of epitope spreading.
Antigens in the pemphigus variants
Pemphigus herpetiformis combines the clinical
features of dermatitis herpetiformis with the
immunologic and histologic features of pemphigus.
Patient's sera react most often with desmoglein 1 and
sometimes with desmoglein 3. Sera from patients with
pemphigus herpetiformis induce spongiosis with
eosinophil infiltration, but rarely is acantholysis
prominent, in contrast with classical pemphigus. It is
thought that sera from pemphigus herpetiformis patients
recognize different epitopes on desmoglein molecules
and has a different post antigen binding sequelae as
compared with classical pemphigus.3
The antigens in IgA pemphigus are less well
defined.24 Previous immunoblotting experiment had
shown reactivity with bovine desmocollin 1, but not with
human skin extracts. This is probably because of
conformational dependent epitope for IgA pemphigus
antibody. By using a cDNA transfection assay, the
antigen in SPD type of IgA pemphigus was shown to
be human desmocollin 1. In the IEN type of IgA
pemphigus, ELISA demonstrated the presence of
reactivity with desmoglein 1 and 3 in a few cases only.
Therefore the antigens in IEN type of IgA pemphigus
were more heterogeneous.
Vol.10 No.2, June 2002
65
Review Articles
PNP is an autoimmune disease with a
polymorphous mucocutaneous eruption and an
underlying neoplasm. The most common association is
that of benign and malignant haematological tumours
such as lymphomas, chronic lymphocytic leukaemia and
Castleman's disease, although other solid tumours have
also been described. The diagnostic criteria had been
reviewed. 3 The antigens identified by immunoprecipitation include cytoplasmic proteins of the plakin
family, desmoplakin I (250 kD), desmoplakin II (210
kD), bullous pemphigoid antigen I (230 kD), envoplakin
(210 kD), periplakin (190 kD) and an 170 kD protein,
the identity of which remained to be determined.3 By
ELISA, antibodies to desmoglein 1 and 3 are also present
in PNP sera. Antibodies from patients with PNP differ
from classical pemphigus in their ability to react with
nonstratified epithelium. Rat urinary bladder is the
preferred substrate as it has a high density of
desmosomes. Antibodies from patients with PF and PV
do not bind to transitional epithelium as desmoglein 1
and 3 are only expressed in squamous cell epithelia.
Plakins are proteins that link keratin filaments to the
cell surface and they are inaccessible to antibodies in
intact cell because of their intracytoplasmic location.
The antibodies against desmogleins (transmembrane
proteins) are important in the initiation of PNP based
on the observation that: (1) all patients with PNP have
anti-desmoglein 3 antibody and about 60% have antidesmoglein 1 as well by ELISA; (2) passive transfer of
whole IgG from PNP sera produce blisters in neonatal
mice and (3) immunoabsorption of desmoglein 1 and 3
antibodies from PNP sera prevent blister formation in
neonatal mice.25
ACANTHOLYTIC MECHANISM OF
PEMPHIGUS ANTIBODIES
Although ample evidences are present for the
aetiologic role of pemphigus antibodies, there are
controversies over the mechanism of acantholysis.
Majority of the research work had been concentrated
on the classical pemphigus and was reviewed.4 Release
of plasminogen activator has been shown in vitro on
addition of pemphigus antibodies to keratinocyte
cultures. In vivo, urokinase type plasminogen activator
has been demonstrated in blister fluid. But elevation of
plasminogen activator has been reported in lesional skin
of other non-acantholytic disease and passive transfer
of PV and PF IgG to plasminogen activator knockout
66
Hong Kong Dermatology & Venereology Bulletin
neonatal mice can induce acantholysis. Therefore, the
plasminogen-plasmin system may act secondarily in
the amplification of lesions. The same assistant
amplification role has also been proposed for
complement. In vitro, pemphigus antibodies alone
can induce acantholysis without complement. In vivo,
passive transfer of F(ab')2 fragment, which does not
activate complement, into neonatal mice induces
blister formation. Cytokines are also possible
mediators in acantholysis, with increase in IL-1, IL6, and TNF- demonstrated in PV cases, 26 and
increase in IL-8 in pemphigus herpetiformis cases. 3
In PNP, some lymphomas and leukemia secrete
massive amounts of IL-6 which may drive autoimmune
antibody production. 3 However, the nonspecific
destruction by proteases and inflammatory cells
recruitment is not compatible with the desmoglein
compensation hypothesis which predicts the level of
acantholysis by the compensation of adhesive
function of desmoglein in the presence of another.
Thus, a direct inhibitory action of pemphigus
antibody on desmoglein adhesive function has been
suggested.14
ROLE OF GENETIC AND
ENVIRONMENTAL FACTORS
Genetic factors may affect susceptibility to
autoimmune diseases. Familial cases of pemphigus have
been described and relatives of pemphigus patients may
have anti-skin antibodies. PV is more common in
Ashkenazi Jews and Japanese, and Fogo Selvagem
(endemic PF) may have genetic and environmental
factors that account for its prevalence in Central and
South America. The genetics of pemphigus has been
reviewed.4 In both PV and PF, association with HLA
class II genes is found, in particular, DR4 and DR14
genes. Different susceptibility alleles have been
described in PV, with the prevalent allele differs in
different populations, for example, DRB1*0402, 0403,
0404, 0406 and DRB1*1401, 1404, 1405, 1406. In Fogo
Selvagem, besides the DR4 and DR14 alleles, a
susceptibility allele of DR1 (DRB1*0102) and
protective alleles of DQ class (e.g. DQB1*0201) are
found.27 The association of HLA alleles with pemphigus
is probably related to the ability of susceptible alleles
to present desmoglein derived peptides in the antigen
presentation process and these alleles have conserved
residues at key positions of the DR beta chain.
Review Articles
Environmental factors such as drugs, virus, burns,
and irradiation have been described in triggering or
exacerbating pemphigus, but their exact importance and
pathogenic mechanisms are not well defined.4 Fogo
Selvagem is the endemic form of PF found in Brazil and
other parts of South America. While familial clustering of
the disease can be explained by genetic association or
shared environmental exposure in the same family, other
epidemiological data suggest that environmental exposure
alone is important. These include geographical clustering,
often near to tributaries of river, its occurrence in different
ethnic groups and at risk occupation of agricultural
work.27 A case control study demonstrated that insect bite
by black fly was a risk factor for development of Fogo
Selvagem.27 Whilst insect bite may act through molecular
mimicry in generating an autoimmune reaction, there is
no concrete data that suggests how insect bite can lead to
Fogo Selvagem.4
CONCLUSIONS
In the last few decades, there have been significant
advances in the understanding in the pathogenesis of
pemphigus. The knowledge has been transformed into
improvement in diagnosis (with the use of immunofluorescence, immunoprecipitation, immunoblotting,
ELISA), in treatment (with decrease in mortality by the
use of immunosuppressant) and disease monitoring (as
antibodies titre are related to disease activity). But there
are also a number of crucial questions remained to be
answered. These include the mechanism leading to
immune intolerance of self-antigen, role of
acetylcholine antibodies, and mechanism of
acantholysis by antibodies.20 Further research in these
areas may provide opportunity for the generation of new
treatment strategies and/or prevent the disease
occurrence in susceptible individuals.4
References
1. Stanley JR. Pemphigus. In: Freedberg IM, Eisen AZ, Wolff K,
et al, editors. Dermatology in General Medicine, 5th ed., New
York: McGraw-Hill, 1999:654-66.
2. Beutner EH, Jordan RE. Demonstrations of skin antibodies in
sera of pemphigus vulgaris patients by indirect immunofluorescence staining. Pro Soc Exp Biol Med 1964;117:50510.
3. Robinson ND, Hashimoto T, Amagai M, Chan LS. The new
pemphigus variants. J Am Acad Dermatol 1999;40(5 Pt 1):649-
71.
4. Martel P, Joly P. Pemphigus: autoimmune diseases of
keratinocyte's adhesion molecules. Clin Dermatol 2001;19:66274.
5. Jordan RE, Samuel FB. Pemphigus Vulgaris. In: Jordan RE
editor. Atlas of bullous disease, New York: Churchill
Livingstone, 2000:1-16.
6. Anhalt GJ, Labib RS, Voorhees JJ, Beals TF, Diaz LA. Induction
of pemphigus in neonatal mice by passive transfer of IgG from
patients with the disease. N Eng J Med 1982;306:1189-96.
7. Amagai M, Karpati S, Prussick R, Klaus-Kovtun V, Stanley
JR. Autoantibodies against the amino-terminal cadherin-like
binding domain of pemphigus vulgaris antigen are pathogenic.
J Clin Invest 1992;90:919-26.
8. Juhasz I, Lazarus GS, Murphy GF, Shih IM, Herlyn M.
Development of pemphigus vulgaris-like lesions in severe
combined immunodeficiency disease mice reconstituted with
lymphocytes from patients. J Clin Invest 1993;92:2401-7.
9. Fan JL, Memar O, McCormick DJ, Prabhakar BS. BALB/c mice
produce blister-causing antibodies upon immunization with a
recombinant human desmoglein 3. J Immunol 1999;163:622835.
10. Amagai M, Tsunoda K, Suzuki H, Nishifuji K, Koyasu S,
Nishikawa T. Use of autoantigen-knockout mice in developing
an active autoimmune disease model for pemphigus. J Clin
Invest 2000;105:625-31.
11. Kricheli D, David M, Frusic-Zlotkin M, et al. The distribution
of pemphigus vulgaris-IgG subclasses and their reactivity with
desmoglein 3 and 1 in pemphigus patients and their first-degree
relatives. Br J Dermatol 2000;143:337-42.
12. Spaeth S, Riechers R, Borradori L, Zillikens D, Budinger L,
Hertl M. IgG, IgA and IgE autoantibodies against the
ectodomain of desmoglein 3 in active pemphigus vulgaris. Br
J Dermatol 2001;144:1183-8.
13. Nousari HC, Anhalt GJ. Paraneoplastic pemphigus. In: Jordan
RE editor. Atlas of bullous disease, New York: Churchill
Livingstone, 2000:29-41.
14. Udey MC, Stanley JR. Pemphigus diseases of antidesmosomal
autoimmunity. JAMA 1999;282:572-6.
15. Anhalt GJ. Making sense of antigens and antibodies in
pemphigus. J Am Acad Dermatol 1999;40(5 Pt 1):763-6.
16. Mahoney MG, Wang Z, Rothenberger K, Koch PJ, Amagai M,
Stanley JR. Explanations for the clinical and microscopic
localization of lesions in pemphigus foliaceus and vulgaris. J
Clin Invest 1999;103:461-8.
17. Amagai M, Tsunoda K, Zillikens D, Nagai T, Nishikawa T.
The clinical phenotype of pemphigus is defined by the antidesmoglein autoantibody profile. J Am Acad Dermatol 1999;
40(2 Pt 1):167-70.
18. Wu H, Wang ZH, Yan A, et al. Protection against pemphigus
foliaceus by desmoglein 3 in neonates. N Engl J Med 2000;
343:31-5.
19. Nguyen VT, Ndoye A, Shultz LD, Pittelkow MR, Grando SA.
Antibodies against keratinocyte antigens other than desmogleins
1 and 3 can induce pemphigus vulgaris-like lesions. J Clin Invest
Vol.10 No.2, June 2002
67
Review Articles
2000;106:1467-79.
20. Kalish RS. Pemphigus vulgaris: the other half of the story. J
Clin Invest 2000;106:1433-5.
21. Vasioukhin V, Bauer C, Yin M, Fuchs E. Directed actin
polymerization is the driving force for epithelial cell-cell
adhesion. Cell 2000;100:209-19.
22. Sakuntabhai A, Ruiz-Perez V, Carter S, et al. Mutations in
ATP2A2, encoding a Ca2+ pump, cause Darier disease. Nat Genet
1999;21:271-7.
23. Hu Z, Bonifas JM, Beech J, et al. Mutations in ATP2C1, encoding
a calcium pump, cause Hailey-Hailey disease. Nat Genet 2000;
24:61-5.
24. Hashimoto T. Immunopathology of IgA pemphigus. Clin
Dermatol 2001;19:683-9.
25. Ohyama M, Amagai M, Hashimoto T, Nousari HC, Anhalt GJ,
Nishikawa T. Clinical phenotype and anti-desmoglein
autoantibody profile in paraneoplastic pemphigus. J Am Acad
Dermatol 2001;44:593-8.
26. Lopez-Robles E, Avalos-Diaz E, Vega-Memije E, et al. TNFalpha
and IL-6 are mediators in the blistering process of pemphigus.
Int J Dermatol 2001;40:185-8.
27. Zaitz C, Campbell I, Alves GF. Commentary/millenium: endemic
pemphigus foliaceus (fogo selvagem). Int J Dermatol 2000;39:
812-4.
Web sites of Dermatology & Venereology in Hong Kong
The homepage of the Hong Kong Society of Dermatology & Venereology
http://www.medicine.org.hk/hksdv/
Hong Kong Dermatology & Venereology Bulletin
(Official Publication of the Hong Kong Society of Dermatology & Venereology)
http://www.medicine.org.hk/hksdv/bulletin.htm
Handbook of Dermatology & Venereology
(Published by Social Hygiene Service, Department of Health)
http://www.hkmj.org.hk/skin/
CME Online (Dermatology)
(CME Programme accredited by the Hong Kong College of Family Physicians)
http://www.medicine.org.hk/cme/
The Homepage of the Asian Dermatological Association
http://www.medicine.org.hk/ada/
68
Hong Kong Dermatology & Venereology Bulletin
S-ar putea să vă placă și
- Pemphigus vulgarisPPTDocument23 paginiPemphigus vulgarisPPTSiti HanisaÎncă nu există evaluări
- Immunopathogenesis of Pemphigus Vulgaris: A Brief ReviewDocument3 paginiImmunopathogenesis of Pemphigus Vulgaris: A Brief ReviewAnonymous SPrI0gbTr0Încă nu există evaluări
- CANINE-Pemphigus Complex-Pathogenesis and Clinical PresentationDocument5 paginiCANINE-Pemphigus Complex-Pathogenesis and Clinical Presentationtaner_soysuren100% (4)
- Bullous Disease: Farah Alsheikh Dima ArabiyatDocument58 paginiBullous Disease: Farah Alsheikh Dima ArabiyatAhmad AltarefeÎncă nu există evaluări
- Direct Immmuno Flourescence Study in Auto Immune Bullous DisordersDocument3 paginiDirect Immmuno Flourescence Study in Auto Immune Bullous DisordersInternational Organization of Scientific Research (IOSR)Încă nu există evaluări
- Biomedicines 10 01197 v2Document10 paginiBiomedicines 10 01197 v2Silvia Montejo FareloÎncă nu există evaluări
- Autoimmunity in Atopic Dermatitis: Biomarker or Simply Epiphenomenon?Document8 paginiAutoimmunity in Atopic Dermatitis: Biomarker or Simply Epiphenomenon?Miguel RomeroÎncă nu există evaluări
- Pemphigus: by Demetris Ioannides, MD Associate Professor of DermatologyDocument43 paginiPemphigus: by Demetris Ioannides, MD Associate Professor of DermatologyYulita PurbaÎncă nu există evaluări
- Chapter 53:: Paraneoplastic Pemphigus:: Grant J. Anhalt & Daniel MimouniDocument15 paginiChapter 53:: Paraneoplastic Pemphigus:: Grant J. Anhalt & Daniel MimouniFiraÎncă nu există evaluări
- Pathogenesis of PemphigusDocument47 paginiPathogenesis of PemphigusChampak PaulÎncă nu există evaluări
- PemphigusDocument32 paginiPemphigusAlondra CastilloÎncă nu există evaluări
- Pediatric Immunology: A Case-Based Collection with MCQs, Volume 2De la EverandPediatric Immunology: A Case-Based Collection with MCQs, Volume 2Încă nu există evaluări
- Iga Pemphigus: Clinics in Dermatology (2011) 29, 437-442Document6 paginiIga Pemphigus: Clinics in Dermatology (2011) 29, 437-442Rafiqa Zulfi UmmiahÎncă nu există evaluări
- 2 5456181012360856193Document70 pagini2 5456181012360856193Maha KhalidÎncă nu există evaluări
- Seminar: Enno Schmidt, Detlef ZillikensDocument13 paginiSeminar: Enno Schmidt, Detlef ZillikensUssiy RachmanÎncă nu există evaluări
- Pemphigus Foliaceous: A Rare Case Report AbstractDocument5 paginiPemphigus Foliaceous: A Rare Case Report AbstractVpatelÎncă nu există evaluări
- 2020 - Pemphigus Vulgaris and Bullous Pemphigoid Update On Diagnosis and TreatmentDocument12 pagini2020 - Pemphigus Vulgaris and Bullous Pemphigoid Update On Diagnosis and TreatmentnancyerlenÎncă nu există evaluări
- Pemphigus Diseases ExplainedDocument23 paginiPemphigus Diseases ExplainedPutkurÎncă nu există evaluări
- Pemhigus Lancet Schmidt2019Document13 paginiPemhigus Lancet Schmidt2019Faten HayderÎncă nu există evaluări
- Implication of Allergy and Atopy in IgG4 Related DDocument18 paginiImplication of Allergy and Atopy in IgG4 Related DjosehannaÎncă nu există evaluări
- Chapter 54. PemphigusDocument28 paginiChapter 54. PemphigusChristo LimbongÎncă nu există evaluări
- HHS Public Access: PemphigusDocument40 paginiHHS Public Access: Pemphiguszahra tsaniaÎncă nu există evaluări
- The Gell and Coombs classification of hypersensitivity reactionsDocument25 paginiThe Gell and Coombs classification of hypersensitivity reactionsanandiprÎncă nu există evaluări
- Pemphigus Vulgaris Review: Etiology, Clinical Features, Diagnosis and TreatmentDocument6 paginiPemphigus Vulgaris Review: Etiology, Clinical Features, Diagnosis and TreatmentMiftahul JannahÎncă nu există evaluări
- Paraneoplastic Pemphigus With Clinical Features of Lichen Planus Associated With Low-Grade B Cell LymphomaDocument7 paginiParaneoplastic Pemphigus With Clinical Features of Lichen Planus Associated With Low-Grade B Cell LymphomalizasilvianaÎncă nu există evaluări
- Pemphigus: Box IDocument1 paginăPemphigus: Box IAsaid HezamÎncă nu există evaluări
- Lecture 5/ Medical Microbiology / 2ed Class StreptococcusDocument9 paginiLecture 5/ Medical Microbiology / 2ed Class Streptococcusهدى قحطان جليلÎncă nu există evaluări
- Omalizumab For Asthma Nejm 2006Document7 paginiOmalizumab For Asthma Nejm 2006Sachin VermaÎncă nu există evaluări
- IgG4-Related Disease: A Guide for PathologistsDocument8 paginiIgG4-Related Disease: A Guide for PathologistsMariela Judith UCÎncă nu există evaluări
- Plasmodiumfalciparum: Characterization Immune Malaria. II. of Anti-P. FakiparumDocument8 paginiPlasmodiumfalciparum: Characterization Immune Malaria. II. of Anti-P. FakiparumderekwwillisÎncă nu există evaluări
- Patogenesis IMNDocument23 paginiPatogenesis IMNshiloinÎncă nu există evaluări
- Igg4-Related Disease: An Orphan Disease With Many Faces: Review Open AccessDocument14 paginiIgg4-Related Disease: An Orphan Disease With Many Faces: Review Open Accessmiguel roldanÎncă nu există evaluări
- Yang 2019Document11 paginiYang 2019RaissaÎncă nu există evaluări
- Panko 2009Document6 paginiPanko 2009Lee제노Încă nu există evaluări
- Case Report: Subcorneal Pustular Dermatosis An Immnohisto-Pathological PerspectiveDocument4 paginiCase Report: Subcorneal Pustular Dermatosis An Immnohisto-Pathological PerspectiveLewishoppusÎncă nu există evaluări
- Bullous Pemphigoid and Pemphigus GuideDocument22 paginiBullous Pemphigoid and Pemphigus GuideDanielÎncă nu există evaluări
- Neisseria meningitidis: Pathogenesis, Clinical Syndromes, Diagnosis and TreatmentDocument3 paginiNeisseria meningitidis: Pathogenesis, Clinical Syndromes, Diagnosis and TreatmentSajjad Hossain ShuvoÎncă nu există evaluări
- Postgrad Med J 1999 Burkhart 328 31Document5 paginiPostgrad Med J 1999 Burkhart 328 31Yoser ThamtonoÎncă nu există evaluări
- Page Four 100509ToxoplasmaGondiinfectsMostSpeciesPage4Document4 paginiPage Four 100509ToxoplasmaGondiinfectsMostSpeciesPage4Ralph Charles Whitley, Sr.Încă nu există evaluări
- Age Specific References For IgDDocument8 paginiAge Specific References For IgDBassem AhmedÎncă nu există evaluări
- Differential Regulation of Igg Subclasses and Ige Antimalarial Antibody Responses in Complicated and Uncomplicated MalariaDocument9 paginiDifferential Regulation of Igg Subclasses and Ige Antimalarial Antibody Responses in Complicated and Uncomplicated MalariaJarwoto RoestanajieÎncă nu există evaluări
- Diagnosis and Clinical Features of Pemphigus VulgarisDocument1 paginăDiagnosis and Clinical Features of Pemphigus VulgarisDwiKamaswariÎncă nu există evaluări
- Immunological Basis of Infertility in AnimalsDocument13 paginiImmunological Basis of Infertility in AnimalsRamachandran Ram100% (3)
- Area Composita of The Heart El Bagre-EPFDocument6 paginiArea Composita of The Heart El Bagre-EPFAna Maria Abreu VelezÎncă nu există evaluări
- Immunointervention in Autoimmune Diseases: Papers Based on an International Meeting in Paris, France, in June 1988De la EverandImmunointervention in Autoimmune Diseases: Papers Based on an International Meeting in Paris, France, in June 1988J. F. BachÎncă nu există evaluări
- Bullous PemphigoidDocument13 paginiBullous PemphigoidSharifah HanimÎncă nu există evaluări
- Epidermal Permeability Barrier Defects and Barrier Repair Therapy in Atopic DermatitisDocument12 paginiEpidermal Permeability Barrier Defects and Barrier Repair Therapy in Atopic DermatitisMisaeldpdÎncă nu există evaluări
- Current Concepts in The Pathophysiology of Atopic Dermatitis in HumanDocument15 paginiCurrent Concepts in The Pathophysiology of Atopic Dermatitis in Humanwe sagara dewiÎncă nu există evaluări
- 1989 - Cookson Et Al. - Linkage Between Immunoglobulin E Responses Underlying Asthma and Rhinitis and Chromosome 11qDocument4 pagini1989 - Cookson Et Al. - Linkage Between Immunoglobulin E Responses Underlying Asthma and Rhinitis and Chromosome 11qpond_1993Încă nu există evaluări
- Correlation of Serum Ige Levels and Clinical Manifestations in Patients With Actinic PrurigoDocument4 paginiCorrelation of Serum Ige Levels and Clinical Manifestations in Patients With Actinic PrurigoMaría José VázquezÎncă nu există evaluări
- Targeting Ig EDocument15 paginiTargeting Ig ESisilia ZulkarnainÎncă nu există evaluări
- Neisseria meningitidis and gonorrhoeae overviewDocument34 paginiNeisseria meningitidis and gonorrhoeae overviewFarah ZahidÎncă nu există evaluări
- Pemphigus_improving_with_gluten-free_diet_13Document2 paginiPemphigus_improving_with_gluten-free_diet_13thaysamaxs3Încă nu există evaluări
- Chronic Spontaneous Urticaria-Status Quo and Future: Susanne Melchers Jan P. NicolayDocument11 paginiChronic Spontaneous Urticaria-Status Quo and Future: Susanne Melchers Jan P. NicolayRizka ZulaikhaÎncă nu există evaluări
- Chronic Desquamative Gingivitis GuideDocument52 paginiChronic Desquamative Gingivitis GuidePrathik RaiÎncă nu există evaluări
- 1 s2.0 S2095881118301379 MainDocument7 pagini1 s2.0 S2095881118301379 MainAnita DewiÎncă nu există evaluări
- IgG and IgM Antibodies at Lead City UniversityDocument14 paginiIgG and IgM Antibodies at Lead City UniversityVivianÎncă nu există evaluări
- Serological Test For Viral DetectionDocument3 paginiSerological Test For Viral DetectionDibyakÎncă nu există evaluări
- Cellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsDe la EverandCellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsCharles G. CochraneÎncă nu există evaluări
- JADWALDocument5 paginiJADWALMeuthia AlamsyahÎncă nu există evaluări
- 917 1683 1 SMDocument14 pagini917 1683 1 SMMeuthia AlamsyahÎncă nu există evaluări
- JADWALDocument5 paginiJADWALMeuthia AlamsyahÎncă nu există evaluări
- Getting The FoodDocument3 paginiGetting The FoodMeuthia AlamsyahÎncă nu există evaluări
- ABSTRACdocxDocument3 paginiABSTRACdocxMeuthia AlamsyahÎncă nu există evaluări
- Cover Depan & BelakangDocument2 paginiCover Depan & BelakangMeuthia AlamsyahÎncă nu există evaluări
- Pubmed ResultDocument1 paginăPubmed ResultMeuthia AlamsyahÎncă nu există evaluări
- Cover Proposal LengkapDocument1 paginăCover Proposal LengkapMeuthia AlamsyahÎncă nu există evaluări
- Ramadhan Dwi CahyoDocument1 paginăRamadhan Dwi CahyoMeuthia AlamsyahÎncă nu există evaluări
- Jurnal Fungsi Produksi 1Document4 paginiJurnal Fungsi Produksi 1Meuthia AlamsyahÎncă nu există evaluări
- ABSTRACdocxDocument3 paginiABSTRACdocxMeuthia AlamsyahÎncă nu există evaluări
- Skenario CDocument23 paginiSkenario CMeuthia AlamsyahÎncă nu există evaluări
- Company Assets and Financial Report 2012Document8 paginiCompany Assets and Financial Report 2012Meuthia AlamsyahÎncă nu există evaluări
- Pemfigus 9 PDFDocument14 paginiPemfigus 9 PDFMeuthia AlamsyahÎncă nu există evaluări
- Pemphigus: Nasal Dermatitis VulgarisDocument2 paginiPemphigus: Nasal Dermatitis VulgarisMeuthia AlamsyahÎncă nu există evaluări
- Nsg241 Study Guide Exam 5Document76 paginiNsg241 Study Guide Exam 5NatalieAndersonÎncă nu există evaluări
- Keratosis Obturans Is Commonly Associated WithDocument11 paginiKeratosis Obturans Is Commonly Associated WithAbouzr Mohammed ElsaidÎncă nu există evaluări
- 2.3 Living Processes in Multicellular Organisms: D.salleh2021Document21 pagini2.3 Living Processes in Multicellular Organisms: D.salleh2021Dewi SallehÎncă nu există evaluări
- Final 1 (12TH June) - 230530 - 115919Document26 paginiFinal 1 (12TH June) - 230530 - 115919Arda DumanÎncă nu există evaluări
- Act07 Toad External Anatomy DiscussionDocument4 paginiAct07 Toad External Anatomy DiscussionSofia A.Încă nu există evaluări
- Gingiva Anatomy and Microscopic FeaturesDocument225 paginiGingiva Anatomy and Microscopic FeaturesJoji IsacÎncă nu există evaluări
- Respiratory HistologyDocument25 paginiRespiratory HistologyUttari DalemÎncă nu există evaluări
- Anatomy AdhyapakDocument50 paginiAnatomy AdhyapakChief Nike - Clash RoyaleÎncă nu există evaluări
- CONJUNCTIVADocument17 paginiCONJUNCTIVACHIMA ONWUKA MONGÎncă nu există evaluări
- Swim Bladder Malformation in Hatchery-Reared Striped Trumpeter Latris Lineata LatridaeDocument14 paginiSwim Bladder Malformation in Hatchery-Reared Striped Trumpeter Latris Lineata LatridaenareÎncă nu există evaluări
- Pathology 5.05b Vagina and Vulva - DR - Dy (Final Edit)Document11 paginiPathology 5.05b Vagina and Vulva - DR - Dy (Final Edit)Dranreb Berylle MasangkayÎncă nu există evaluări
- Comprehensive Periodontics For The Dental HygienistDocument1.567 paginiComprehensive Periodontics For The Dental HygienistHyunsung100% (3)
- Best Aid To OphthalmologyDocument501 paginiBest Aid To OphthalmologyMilthon Catacora Contreras67% (3)
- Module 17 - Urinary SystemDocument18 paginiModule 17 - Urinary SystemSam TagardaÎncă nu există evaluări
- Histology of The Upper GITDocument43 paginiHistology of The Upper GITBenedict OkotÎncă nu există evaluări
- Ophthalmology - EmbryologyDocument3 paginiOphthalmology - EmbryologyOscar Daniel MendezÎncă nu există evaluări
- Biolab: Animal Tissues Lab Report Name, Date, Course and Section Required For Password: 1409Document5 paginiBiolab: Animal Tissues Lab Report Name, Date, Course and Section Required For Password: 1409RosaÎncă nu există evaluări
- Characteristics of Living Beings and Diversity in the Animal KingdomDocument40 paginiCharacteristics of Living Beings and Diversity in the Animal KingdomNickOoPandeyÎncă nu există evaluări
- KMU Foundation ModuleDocument20 paginiKMU Foundation ModuleShafiq Ur RahmanÎncă nu există evaluări
- In Vivo Reprogramming of Wound-Resident Cells Generates Skin Epithelial TissueDocument28 paginiIn Vivo Reprogramming of Wound-Resident Cells Generates Skin Epithelial Tissueender000Încă nu există evaluări
- Short Notes Form 4 Biology (Chapter 1-4)Document6 paginiShort Notes Form 4 Biology (Chapter 1-4)Ema Fatimah75% (8)
- Dimensions and Relations of The Dentogingival Junction in Humans. Gargiulo 1961Document7 paginiDimensions and Relations of The Dentogingival Junction in Humans. Gargiulo 1961Linda Garcia PÎncă nu există evaluări
- Neoplasms of The Biliary TractDocument186 paginiNeoplasms of The Biliary Tracthgr58patologiaÎncă nu există evaluări
- Class IX Science - Tissues - Lesson PlanDocument16 paginiClass IX Science - Tissues - Lesson PlanShailaja Mestry100% (2)
- Odontogenic Cysts of The JAW: Seminar Presented byDocument31 paginiOdontogenic Cysts of The JAW: Seminar Presented byankita sethi100% (1)
- Amelogenesis: 2 - Secretory Stage (Formative Stage)Document16 paginiAmelogenesis: 2 - Secretory Stage (Formative Stage)debby yeun-yee hahÎncă nu există evaluări
- Histology Krok StudyDocument8 paginiHistology Krok StudyErnesto PadronÎncă nu există evaluări
- Epithelium SummaryDocument7 paginiEpithelium SummaryElena ArvanitiÎncă nu există evaluări
- AVBS2001Document81 paginiAVBS2001Celine Berjot100% (1)
- The Logic of Immunity Deciphering An EnigmaDocument204 paginiThe Logic of Immunity Deciphering An EnigmaSatyabrataSahaÎncă nu există evaluări