Documente Academic
Documente Profesional
Documente Cultură
Upper Gastrointestinal Bleeding Case Study
Încărcat de
Claudine Lacaden0%(1)0% au considerat acest document util (1 vot)
1K vizualizări5 paginipathophy
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentpathophy
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0%(1)0% au considerat acest document util (1 vot)
1K vizualizări5 paginiUpper Gastrointestinal Bleeding Case Study
Încărcat de
Claudine Lacadenpathophy
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 5
https://www.scribd.
com/doc/196845328/UpperGastrointestinal-Bleeding-Ncp
https://www.scribd.com/doc/62262158/UGIB-NCP
http://nursingcrib.com/nursing-notesreviewer/fundamentals-of-nursing/nursing-diagnosis-forgastrointestinal-diseasesdisorders/
Upper Gastrointestinal/ Esophageal
Bleeding
1.
Deficient fluid volume (isotonic)
2.
Risk for ineffective tissue perfusion
3.
Fear or anxiety (specify level)
4.
Acute or chronic pain
5.
Knowledge deficient (learning need) regarding condition,
prognosis, treatment regimen, self-care, and discharge
needs
Upper gastrointestinal bleeding is characterized by the sudden
onset of bleeding from the GI tract at a site (or sites) proximal to the
ligament of Treitz. Most upper GI bleeds are a direct result of peptic ulcer
erosion, stress related- mucosal disease, that may evidence as
superficial erosive gastric lesion to frank ulcerations, erosive gastritis
(secondary to use or abuse of NSAIDs, oral corticosteroids, or alcohol)
or esophageal varices (secondary to hepatic failure). In addition to these,
Mallory-Weiss tears can cause gastroesophageal bleeding as a result of
severe retching and vomiting, but the bleeding tends to be less severe
than in other types. Hospitalized critically ill patients are at heightened
risk for stress related mucosal disease, particularly if they are intubated
and mechanically ventilated and/or evidencing coagulopathies.
Signs and Symptoms
Melena and hematemesis
Pain
Hypovolemic shock
Physical Examination
Vital signs
BP < 90 mm Hg
HR > 100 beats/min
RR: tachycardia
Temperature: maybe elevated
Other
Hematemesis
Melena
Bloody stool with fetid odor
Coffee ground gastric aspirate
Skin
Pale, diaphoretic
Cool, clammy
Jaundice
Cardiovascular
Weak, thready pulse
Capillary refill > 3 sec
Abdominal
Maybe tender with guarding
Bowel sounds hyperactive or absent
Acute Care Patient Management
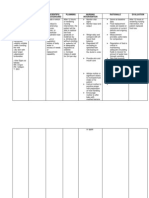
Nursing Diagnosis: Deficient fluid volume related to blood loss from
hemorrhage.
Outcome Criteria
Patient alert and oriented
Skin, pink, warm, and dry
CVP 2 to 6 mm Hg
PAS 15 TO 30 mm Hg
PAD 5 to 15 mm Hg
BP 90 to 120 mm Hg
MAP 70 to 105 mm Hg
HR 60 to 100 beats/min
Urine output 30 ml/hr
Patient Monitoring
1.
Obtain pulmonary artery pressure, central venous pressure
and blood pressure every 15 minutes during acute episodes
to evaluate fluid needs and the patients response to
therapy.
2.
Monitor fluid volume status. Measure intake and output
hourly to evaluate renal perfusion.
3.
Measure blood loss if possible.
4.
Continuously monitor ECG for dysrythmias and myocardial
ischemia.
Patient Assessment
1.
Assess patient for increases restlessness, apprehension or
altered consciousness, which may indicate decreased
cerebral perfusion.
2.
Assess hydration status.
3.
Be alert for recurrence of bleedings.
Diagnostic Assessment
1.
Review Hgb and Hct levels to determine the effectiveness
of treatment or worsening of the patients condition.
2.
Review clotting factors and serum calcium levels if
multiple transfusions have been give.
3.
Review serial BUN levels.
4.
Review serial ABGs to evaluate oxygenation and acid-base
status.
5.
Review the result of endoscopic evaluation.
Patient Management
1.
Maintain a patent airway. Administer supplemental oxygen
as ordered.
2.
Administer colloids as ordered to restore intravascular
volume.
3.
Type and crossmatch for anticipated blood products.
4.
Evacuate stomach contents with nasogastric tube and
initiate lavages with room temperature water or saline to
clear blood clots from the stomach.
5.
Continue to monitor the patient closely once stabilized.
6.
Vitamin K or fresh-frozen plasma (FFP) may be ordered to
correct coagulation deficiencies.
7.
Explain all procedures and tests to the patient to help
alleviate anxiety and decreased tissue oxygen demands.
S-ar putea să vă placă și
- Risk For Bleeding - Cirrhosis NCPDocument2 paginiRisk For Bleeding - Cirrhosis NCPPaula AbadÎncă nu există evaluări
- NCP T2DMDocument5 paginiNCP T2DMFrancym R. BatengaÎncă nu există evaluări
- NCP Fluid Volume DeficitDocument3 paginiNCP Fluid Volume DeficitNecheal BaayÎncă nu există evaluări
- Upper Gastrointestinal Bleeding: Anthony Alexander University of The West Indies at MonaDocument40 paginiUpper Gastrointestinal Bleeding: Anthony Alexander University of The West Indies at MonaAy Alex0% (1)
- Case Study Ugib.Document19 paginiCase Study Ugib.Mary Ann Garcia100% (1)
- NCP Liver CirrhosisDocument5 paginiNCP Liver CirrhosisEsther O. CorreaÎncă nu există evaluări
- Diarrhea Care PlanDocument2 paginiDiarrhea Care Planzepoli_zepoly6232100% (1)
- AGE PathophysiologyDocument1 paginăAGE PathophysiologyZhenmeiÎncă nu există evaluări
- Risk Reduction and Preparedness Equipment ProtectDocument2 paginiRisk Reduction and Preparedness Equipment ProtectR ArcegaÎncă nu există evaluări
- NCP Gastritis NewDocument3 paginiNCP Gastritis NewNova Triska Purnama Sari0% (1)
- Pathophysiology of ESRDDocument3 paginiPathophysiology of ESRDjake90210100% (1)
- Vii. NCP and Case Study: Learn The DemonstrateDocument4 paginiVii. NCP and Case Study: Learn The DemonstrateVenus Glaze Verzola100% (2)
- Ncp'sDocument8 paginiNcp'sDuchess Kleine RafananÎncă nu există evaluări
- NCPDocument3 paginiNCPranee diane0% (1)
- Oresol Drug StudyDocument8 paginiOresol Drug StudyLeslie PaguioÎncă nu există evaluări
- NCP Making (Ulcerative Colitis & Crohn's Disease)Document2 paginiNCP Making (Ulcerative Colitis & Crohn's Disease)R Hornilla ArcegaÎncă nu există evaluări
- Course Task CU 7Document7 paginiCourse Task CU 7Kyla PamaÎncă nu există evaluări
- Nursing Management of Patient With Upper Gastrointestinal BleedingDocument10 paginiNursing Management of Patient With Upper Gastrointestinal BleedingVia Katherine PanganibanÎncă nu există evaluări
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDocument2 paginiNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaÎncă nu există evaluări
- VIGOCIDDocument2 paginiVIGOCIDKaren DamoÎncă nu există evaluări
- Doctors OrderDocument2 paginiDoctors Ordermarc_alvin0% (1)
- NCP-fluid Volume DeficitDocument4 paginiNCP-fluid Volume DeficitChrissa Mae Aranilla MayoÎncă nu există evaluări
- Deficit)Document2 paginiDeficit)Lee DeeÎncă nu există evaluări
- Problem Nursing Diagnosis Outcome Plan Intervention Evaluation Subjective Data: "Masakit Po Yung Sa Short Term: IndependentDocument2 paginiProblem Nursing Diagnosis Outcome Plan Intervention Evaluation Subjective Data: "Masakit Po Yung Sa Short Term: IndependentkyawÎncă nu există evaluări
- NCP Con ConstipationDocument2 paginiNCP Con ConstipationChristine Marie Bucio OraizÎncă nu există evaluări
- D5LR VS PLRDocument27 paginiD5LR VS PLRgerrilynwayneÎncă nu există evaluări
- NCP - Acute Pain Stomach CancerDocument2 paginiNCP - Acute Pain Stomach CancerJohn Michael TaylanÎncă nu există evaluări
- Hypertensive NephrosclerosisDocument14 paginiHypertensive Nephrosclerosisreysanne100% (1)
- Ugib Case StudyDocument36 paginiUgib Case StudyRJ MarquezÎncă nu există evaluări
- Revised NCP (Baiae)Document9 paginiRevised NCP (Baiae)Jennifer BactatÎncă nu există evaluări
- NCP Background, Demographic Data, Dordon's Functional Health, Drug Study SAint Louis UniversityDocument21 paginiNCP Background, Demographic Data, Dordon's Functional Health, Drug Study SAint Louis Universitypa3kmedinaÎncă nu există evaluări
- Multi Noduar Colloid GoiterDocument1 paginăMulti Noduar Colloid GoiterVincent John Faller100% (1)
- Risk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.Document2 paginiRisk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.eleinsamÎncă nu există evaluări
- NCP For Ruptured AppendicitisDocument2 paginiNCP For Ruptured AppendicitisJansen Arquilita RiveraÎncă nu există evaluări
- NCP PSHDocument17 paginiNCP PSHMargareth OrtizÎncă nu există evaluări
- Burns - Airway Clearance, Risk For IneffectiveDocument2 paginiBurns - Airway Clearance, Risk For Ineffectivemakyofrancis20Încă nu există evaluări
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Document5 paginiSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenÎncă nu există evaluări
- Ugib NCPDocument5 paginiUgib NCPJhuRise Ann Mangana100% (1)
- NCP - Poststreptococcal GlomerulonephritisDocument12 paginiNCP - Poststreptococcal GlomerulonephritisAya BolinasÎncă nu există evaluări
- Scribd 020922 Case Study-Oncology A&kDocument2 paginiScribd 020922 Case Study-Oncology A&kKellie DÎncă nu există evaluări
- Fluid Volume DeficitDocument3 paginiFluid Volume Deficitprickybiik100% (1)
- NCPDocument3 paginiNCPJezza RequilmeÎncă nu există evaluări
- Concept Map FormatDocument2 paginiConcept Map FormatIAN MAVERICK LIMÎncă nu există evaluări
- Gout N C P BY BHERU LALDocument1 paginăGout N C P BY BHERU LALBheru LalÎncă nu există evaluări
- Subjective: No Subjective Cues. ObjectiveDocument2 paginiSubjective: No Subjective Cues. Objective1S VILLEGAS GabrielÎncă nu există evaluări
- Diabetes InsipidusDocument48 paginiDiabetes InsipidusAhmed Fraz MamoonÎncă nu există evaluări
- Nursing Responsibilities For Oxygen AdministrationDocument3 paginiNursing Responsibilities For Oxygen AdministrationJahseh WolfeÎncă nu există evaluări
- NCP. MOuth SoreDocument1 paginăNCP. MOuth SoreChriszanie CruzÎncă nu există evaluări
- NafarinDocument2 paginiNafarinianecunar100% (2)
- Ncp-Impaired Gas ExchangeDocument2 paginiNcp-Impaired Gas ExchangeRaymond Zamora Hijara100% (1)
- No. 10 SANAANI Topic For Esophagogastric Balloon Tamponade Tubes Billroth 1 and 11Document12 paginiNo. 10 SANAANI Topic For Esophagogastric Balloon Tamponade Tubes Billroth 1 and 11Nur SanaaniÎncă nu există evaluări
- Case Study AppendicitisDocument6 paginiCase Study AppendicitisPrincess Camille ArceoÎncă nu există evaluări
- Fluid Volume Loss NCP - PediaDocument2 paginiFluid Volume Loss NCP - PediaAdrian MallarÎncă nu există evaluări
- Management of Patients With Vascular Disorders: Venous ArterialDocument56 paginiManagement of Patients With Vascular Disorders: Venous ArterialHamss AhmedÎncă nu există evaluări
- Upper GI BleedDocument8 paginiUpper GI BleedbbyesÎncă nu există evaluări
- Nur 111 Session 11 Sas 1Document9 paginiNur 111 Session 11 Sas 1Zzimply Tri Sha UmaliÎncă nu există evaluări
- Clinical Evaluation Test Result Trends: DiagnosisDocument3 paginiClinical Evaluation Test Result Trends: DiagnosisStephen CrossÎncă nu există evaluări
- Blood Transfusion: By: Dr. Hira HanifDocument51 paginiBlood Transfusion: By: Dr. Hira HanifTariq sattarÎncă nu există evaluări
- GI Bleeding (Text)Document11 paginiGI Bleeding (Text)Hart ElettÎncă nu există evaluări
- Case Alcohol Abuse and Unusual Abdominal Pain in A 49-Year-OldDocument7 paginiCase Alcohol Abuse and Unusual Abdominal Pain in A 49-Year-OldPutri AmeliaÎncă nu există evaluări
- Jpoa 2023 Feb PDFDocument163 paginiJpoa 2023 Feb PDFOscar MontilvaÎncă nu există evaluări
- CHAPTER 5 Nursing Care PlanDocument5 paginiCHAPTER 5 Nursing Care PlanMiguelito Galagar GultianoÎncă nu există evaluări
- Oncology Drills With Answers and RationalesDocument41 paginiOncology Drills With Answers and RationalesCarol Kayas100% (1)
- Parasitology Lec 3.01a Intestinal NematodesDocument16 paginiParasitology Lec 3.01a Intestinal NematodesEnaWahahaÎncă nu există evaluări
- A Detailed Lesson Plan in Health 7 I. Content Standard: Teacher's Activity Students' ActivityDocument10 paginiA Detailed Lesson Plan in Health 7 I. Content Standard: Teacher's Activity Students' ActivityGladys Javier PatoÎncă nu există evaluări
- Workshop 0708Document3 paginiWorkshop 0708Manojkumar NairÎncă nu există evaluări
- Acute Otitis Media (Ready) PPTDocument71 paginiAcute Otitis Media (Ready) PPTMegawati Abubakar100% (1)
- Testicular Torsion Torsio TestisDocument34 paginiTesticular Torsion Torsio TestisAira Kelly50% (2)
- Peripheral Vascular DiseaseDocument53 paginiPeripheral Vascular DiseaseShenbagam Mahalingam100% (1)
- Technical Manual: For Installation, Operation and Maintenance ofDocument129 paginiTechnical Manual: For Installation, Operation and Maintenance ofMegan Pierce100% (1)
- Principles Involved in Bioassay by Different Methods A Minireview PDFDocument18 paginiPrinciples Involved in Bioassay by Different Methods A Minireview PDFPankaj KushwahÎncă nu există evaluări
- Wilhelm Reich Contact With SpaceDocument6 paginiWilhelm Reich Contact With Spacebubbaclem100% (2)
- M1 Introduction To Manual TherapyDocument101 paginiM1 Introduction To Manual TherapySylvia LoongÎncă nu există evaluări
- NCP 1Document4 paginiNCP 1Ke EjieÎncă nu există evaluări
- Master Kinesiotaping HandoutDocument11 paginiMaster Kinesiotaping HandoutcosasdeangelÎncă nu există evaluări
- Working With Mandated Substance Abusers - Language of SolutionsDocument33 paginiWorking With Mandated Substance Abusers - Language of SolutionsbmckÎncă nu există evaluări
- Bi-Preterax Slide Set CI 15 - 16Document35 paginiBi-Preterax Slide Set CI 15 - 16drnasim20088171Încă nu există evaluări
- NSAID Safety Audit Jan2019 Vs6Document10 paginiNSAID Safety Audit Jan2019 Vs6Shokooh MansouriÎncă nu există evaluări
- A Dictionary For Psychotherapists PDFDocument1.375 paginiA Dictionary For Psychotherapists PDFMonica100% (2)
- Nomenklatur IBS Edit THTDocument291 paginiNomenklatur IBS Edit THTriezki_pattikratonMDÎncă nu există evaluări
- Guinea Pigs PDFDocument1 paginăGuinea Pigs PDFYaserAbbasiÎncă nu există evaluări
- Salami Flow ChartDocument1 paginăSalami Flow Charttiffanyleecraig50% (2)
- Is 2Document10 paginiIs 2intan juitaÎncă nu există evaluări
- Hand AssessmentDocument22 paginiHand AssessmentVaikunthan RajaratnamÎncă nu există evaluări
- Funda Prof - Ad LMR AnswersDocument35 paginiFunda Prof - Ad LMR AnswersFreeNursingNotesÎncă nu există evaluări
- Nutritional Considerations in Geriatrics: Review ArticleDocument4 paginiNutritional Considerations in Geriatrics: Review ArticleKrupali JainÎncă nu există evaluări
- The Simpson Protocol: Working in Deep States For Optimum Outcomes??Document52 paginiThe Simpson Protocol: Working in Deep States For Optimum Outcomes??Delia Psychedelia50% (4)
- Narrative Therapy Tree of Life ProjectDocument2 paginiNarrative Therapy Tree of Life ProjecttduongÎncă nu există evaluări
- Swyer James MacLeod SyndromeDocument12 paginiSwyer James MacLeod Syndromeflori.bÎncă nu există evaluări
- Journal ClubDocument25 paginiJournal ClubAnonymous Val05Blj100% (1)