Documente Academic
Documente Profesional
Documente Cultură
Journal Reading Relaps
Încărcat de
Nafi Yana SaputraDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Journal Reading Relaps
Încărcat de
Nafi Yana SaputraDrepturi de autor:
Formate disponibile
Predictors of Relapse in the Year
After Hospital Discharge Among
Patients With Schizophrenia
Rebecca Schennach, M.D.
Michael Obermeier
Sebastian Meyer
Markus Jger, M.D.
Max Schmauss, M.D.
Gerd Laux, M.D.
Herbert Pfeiffer, M.D.
Dieter Naber, M.D.
Lutz G. Schmidt, M.D.
Wolfgang Gaebel. M.D.
Joachim Klosterktter, M.D.
Isabella Heuser, M.D.
Wolfgang Maier, M.D.
Matthias R. Lemke, M.D.
Eckart Rther, M.D.
Stefan Klingberg, M.D.
Markus Gastpar, M.D.
Florian Seemller, M.D.
Hans-Jrgen Mller, M.D.
Michael Riedel, M.D.
Objective: Relapse and its predictors were examined among patients with schizophrenia in the
year after hospital discharge.
Methods: The sample included
200 patients with schizophrenia
participating in a German multicenter study. Relapse was defined
as a worsening of psychopathological symptoms or rehospitalization in the year after hospital discharge. Predictors examined were
variables related to course of illness and to response and remission at discharge. Results: Fifty-
two percent of participants had a
relapse. Patients whose symptoms
were not in remission at discharge
were more likely to have a relapse,
as were those who had more severe symptoms and more side effects at discharge. Those who experienced a relapse were less likely to be taking a second-generation antipsychotic at discharge,
less likely to have a positive attitude toward treatment adherence,
and less likely to be employed.
Conclusions: The high rate of relapse among patients with schizo-
phrenia highlights the need to improve current treatment strategies. (Psychiatric Services 63:87
90, 2012)
Dr. Schennach, Mr. Obermeier, Mr. Meyer, Prof. Jger, Dr. Seemller, Prof. Mller,
and Prof. Riedel are affiliated with the
Department of Psychiatry and Psychotherapy, Ludwig-Maximilians-University, Nussbaumstreet 7, 80336 Munich,
Germany (e-mail: rebecca.schennach@
med.unimuenchen.de). Prof. Riedel is also
with the Psychiatric Clinic, Vinzenz-vonPaul-Hospital, Rottweil, Germany. Prof.
Schmauss is with the Psychiatric Clinic,
District Hospital Augsburg, Augsburg,
Germany. Prof. Laux is with the Psychiatric Clinic, Inn-Salzach Hospital,
Wasserburg-Inn, Germany. Dr. Pfeiffer
is with the Psychiatric Clinic, Isar-Amper Hospital, Munich-Haar, Germany.
Prof. Naber is with the Department of
Psychiatry and Psychotherapy, University of Hamburg, Hamburg, Germany.
Prof. Schmidt is with the Department of
Psychiatry and Psychotherapy, University of Mainz, Mainz, Germany. Prof.
Gaebel is with the Department of Psychiatry and Psychotherapy, HeinrichHeine-University, Duesseldorf, Germany. Prof. Klosterktter is with the Department of Psychiatry and Psychotherapy, University of Cologne, Cologne, Germany. Prof. Heuser is with the Department of Psychiatry and Psychotherapy,
Charite Berlin, Campus Benjamin
Franklin, Berlin, Germany. Prof. Maier
is with the Department of Psychiatry and
Psychotherapy, University of Bonn,
Bonn, Germany. Prof. Lemke is with the
Department of Psychiatry, Alsterdorf
Hospital, Hamburg, Germany. Prof.
Rther is with the Department of Psychiatry and Psychotherapy, University of
Gttingen, Gttingen, Germany. Prof.
Klingberg is with the Department of Psychiatry and Psychotherapy, University of
Tbingen, Tbingen, Germany. Prof.
Gastpar is with the Fliedner Clinic,
Berlin, Germany.
PSYCHIATRIC SERVICES
o ps.psychiatryonline.org o January 2012 Vol. 63 No. 1
or many patients with schizophrenia, the course of illness is characterized by frequent relapses with exacerbations of psychosis, often resulting
in the need for rehospitalization (1).
Patients with a history of relapse have
been shown to have a more complex
illness profile, associated with more
severe psychopathological symptoms,
substance use, impairments in functioning and poor adherence to treatment (2). Research applying recently
proposed consensus definitions of outcome to examine the association between the status of patients with schizophrenia at hospital dischargesuch
as whether they have responded to
treatment and whether their symptoms are in remissionand subsequent relapse is scarce.
In addition, clinical implications
from earlier studies are limited because many focused only on firstepisode patients or used data from
randomized controlled trials known
to exclude severely ill or suicidal patients. Another difficulty for researchers in this field is the lack of a
consensus definition and generally
accepted criteria for relapse. For example, a recent review that compared
the relapse prevention potential of
various antipsychotics noted that 11
87
different criteria were used in 17
studies (3). In this study we used a
broad definition of relapse to examine
relapse in a heterogeneous group of
patients in order to reduce potential
limitations on our findings.
Methods
Data were collected as part of a multicenter naturalistic follow-up study,
the German Research Network on
Schizophrenia. The study was conducted at 11 university-affiliated psychiatric hospitals and three nonuniversity-affiliated psychiatric hospitals.
All patients between the ages of 18
and 65 who were admitted to one of
the hospitals between January 2001
and December 2004 with a diagnosis
of schizophrenia, schizophreniform
disorder, delusional disorder, or
schizoaffective disorder according to
DSM-IV criteria were selected for inclusion. Exclusion criteria were a head
injury, a history of major general medical illness, and alcohol or drug dependence. All study participants provided written informed consent. The
study protocol was approved by the local ethics committees. After discharge
patients were followed up for assessment at specified time points. The
study reported here used data from
the one-year follow-up assessment.
DSM-IV diagnoses were verified by
clinical researchers. Information was
collected on sociodemographic characteristics and on variables related to
illness course and to attitude toward
treatment and treatment adherence
by using standard forms. Symptom
severity was assessed with the Positive
and Negative Syndrome Scale for
Schizophrenia (PANSS) and the
Hamilton Depression Scale (HAMD17); higher scores on both instruments
indicate greater illness severity. Extrapyramidal symptoms were examined with the Simpson-Angus Scale.
The Global Assessment of Functioning Scale (GAF) and the Social and
Occupational Functioning Assessment
Scale (SOFAS) were used to evaluate
functioning. The short version of the
Subjective Well-Being Under Neuroleptic Treatment Scale assessed
well-being. To evaluate the patients
premorbid adjustment the subscale
for premorbid social-personal adjustment from the Phillips Scale was em88
ployed. The instruments were administered within the first three days after
admission, biweekly during the patients hospital stay, at discharge, and at
follow-up. All raters had been trained
in use of the scales. A high interrater
reliability was achieved (intraclass correlation>.8).
Patients were categorized as experiencing or not experiencing a relapse. Relapse was defined by using
two items from the standard forms.
The first item evaluates an acute exacerbation of the illness, and the second item explicitly examines rehospitalization because of a worsened psychopathological condition. A positive
rating in for either item was defined
as a relapse.
The outcome of inpatient treatment
was defined as a 50% improvement in
PANSS total score from hospital admission to discharge. Remission was
determined by the consensus criteria
proposed by the PANSS developers
a score of 3 or less of the following
items for six months: delusions, unusual thought content, hallucinatory behavior, conceptual disorganization,
mannerisms and posturing, blunted
affect, social withdrawal, and lack of
spontaneity. The time criterion for remission was not considered at discharge if the patient had been hospitalized for six months or less.
First, univariate tests were used to
compare patients with and without a
relapse during the year after discharge. All variables with a p value of
<.10 in the univariate analysis were
tested as predictors of relapse by two
methods: logistic regression analysis
and classification and regression tree
(CART) analysis. The discriminative
ability of the regression model was
evaluated by using a receiver-operating characteristic curve. The area under the curve (AUC) is a measure of
the overall discriminative power. An
AUC value of .5 indicates no discriminative ability, and an AUC value of
1.0 indicates perfect discriminative
power. All statistical analyses were
performed with the statistical program R2.11.1.
Overall, 474 patients were enrolled
in the naturalistic multicenter study.
Forty-six patients dropped out for various reasons, 28 were discharged from
the hospital within seven days of adPSYCHIATRIC SERVICES
mission, and 167 dropped out during
the acute treatment phase and followup. Patients who dropped out were
significantly older than patients who
did not (p=.006) and scored significantly lower at discharge on the
PANSS total score (p<.001). The two
groups did not differ in sociodemographic and clinical characteristics.
Because of missing PANSS data at the
one-year follow-up assessment, 33 patients were excluded. Thus data were
analyzed for a sample of 200 patients.
Results
The sample included 107 men and 93
women. The meanSD age was
36.310.1 years, and the mean duration of illness was 8.39.4 years. The
mean number of lifetime hospitalizations was 3.45.1. The mean age at
first treatment was 28.19.6 years. At
one-year follow-up 50 patients (25%)
were receiving first-generation antipsychotics, 130 (65%) were receiving second-generation antipsychotics,
18 (9%) were receiving first- as well as
second-generation antipsychotics, 22
(11%) were receiving tranquilizers,
and 27 (14%) were receiving mood
stabilizers. Forty-six patients (23%)
were also receiving antidepressants.
From hospital discharge to the oneyear assessment, no significant change
in patients psychopathology, functioning, occurrence of extrapyramidal
symptoms, and subjective well-being
was observed. At discharge, 114 patients (57%) were classified as treatment responders, and symptoms were
in remission for 114 patients (57%). At
follow-up, 108 (54%) were classified as
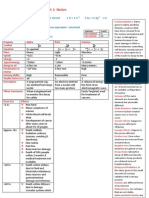
responders, and symptoms were in remission for 102 (51%) (Figure 1).
A total of 104 patients (52%) had at
least one relapse during the follow-up
period, and 34 (17%) had more than
one. At the one-year follow-up assessment, those who had experienced a relapse scored significantly higher on the
PANSS total score (p<.001) and all
PANSS subscale scores; they also had
significantly greater impairments as
measured by the GAF and SOFAS
(p<.001). Among patients who experienced a relapse, 78 (75%) were hospitalized as a result of the exacerbation of
their illness, and 26 (25%) were treated
for the relapse in an outpatient setting.
Patients who had a relapse during
o ps.psychiatryonline.org o January 2012 Vol. 63 No. 1
20
60%
No relapse
Relapse
40
54%
40
%
60
Remission
Percentage
No relapse
80
No remission
59%
Relapse
20
54%
41
%
40
Response
60
No response
Percentage
80
100
PSYCHIATRIC SERVICES
100
46
The aim of this study was to identify
sociodemographic and clinical factors
that predicted relapse among patients
with schizophrenia so that these variables could be monitored during
treatment and specific strategies
could be adopted to prevent relapse.
In our sample, 52% of patients had a
relapse in the first year after hospital
dischargean alarmingly high proportion. One possible explanation is
that the sample included chronically
Relapse during the year after hospital discharge among 200 patients, by whether
their symptoms had responded to treatment or were in remission at discharge
Discussion
Figure 1
46
the follow-up period were significantly
less likely to be employed at hospital
discharge (p=.002). In addition, those
with a relapse were significantly less
likely at discharge to be treated with a
second-generation antipsychotic (p=
.04) and had a significantly worse attitude toward treatment (p=.007). Also,
patients who had a relapse were significantly more likely to report side effects (p<.001) at discharge, even
though no significant between-group
differences were observed at discharge in the defined daily dose of the
second-generation or first-generation
antipsychotics. Furthermore, patients
who relapsed scored significantly higher at discharge on the PANSS total
score (p=.02), the PANSS negative
subscore (p=.02), and the HAMD-17
total score (p=.01), indicating more
negative and depressive symptoms.
Patients whose symptoms were not in
remission at discharge were significantly more likely to relapse within the
year after discharge than those whose
symptoms were in remission at discharge (p=.05) (Figure 1).
Four significant relapse predictors,
as measured at hospital discharge, were
identified: a higher HAMD-17 score
(p<.001), more side effects (p<.001), a
worse attitude to treatment (p=.002),
and not having a job (p=.01). The prediction model reached significance
(p<.001), with satisfactory predictive
power (AUC=.76). The CART model
confirmed that reporting more side effects at discharge (p<.001) and having a
worse attitude toward treatment adherence at discharge (p=.007) were significant predictors of relapse. Significant
predictors by CART analysis at discharge also included a higher PANSS
negative subscore (p=.04) and an independent living situation (p<.001).
0
Discharge
1 year
ill patients with a history of distinct
cycles of relapse. In addition, this
study was observational, and patients
received only monthly telephone calls
during follow-up. Unlike randomized
controlled studies, no extensive visits
or interventions were provided. However, the relapse rate in our study is
comparable to the rate of 42% found
in a study of relapse among patients
taking oral antipsychotics (4). In a
study that compared maintenance
treatment of first-episode patients
with risperidone and haloperidol for
one year and that defined relapse as a
marked clinical deterioration, Gaebel
and colleagues (5) found that no relapses occurred. This finding may be
at least partly explained by the inclusion of only first-episode patients in
the sample. In line with the findings
of that study, our results indicated
that patients experiencing a first
episode had a lower risk of relapse
during follow-up; however, the difference did not reach statistical significance, which may be explained by the
small sample of first-episode patients
and therefore the limited statistical
power in our study.
As others have found, depressive
symptoms at hospital discharge in our
study were significant predictors of
relapse during the one-year followup. In a three-year prospective, observational study in which 2,228 patients with schizophrenia were examined at 12-month intervals, Conley
(6) found that depressed patients
were significantly more likely than
those without depression to use re-
o ps.psychiatryonline.org o January 2012 Vol. 63 No. 1
Discharge
1 year
lapse-related mental health services.
Also, Olfson and colleagues (7) assessed clinical predictors of early rehospitalization among 262 patients
with schizophrenia three months after discharge and found early readmission to be significantly associated
with major depressive symptoms.
Consistently, negative symptoms have
also been associated with a worse
course of schizophrenia and a higher
rate of relapse, which our results confirm. Leifker and colleagues (8) have
shown that blunted affect and passive-apathetic social withdrawal accounted for all of the variance in predicting social outcome among 194
outpatients with schizophrenia.
The fact that we found that patients
whose symptoms were in remission at
discharge were significantly less likely
to experience a relapse than those
whose symptoms were not in remission is not surprising, because one
would strongly expect that a patient
with greater improvement during the
acute treatment phase would have a
more favorable course of illness (9).
Several studies have demonstrated
that early and adequate symptom
control is the precondition of achieving a favorable long-term course of
the illness. Lambert and colleagues
(10), for example, followed over three
years 392 patients with schizophrenia
who had never received treatment
and found that remission within the
first three months after baseline as
the strongest predictor of subsequent
remission. Also, Wobrock and colleagues (11) found that nonremission
89
of symptoms after two weeks of treatment was a significant predictor of
not achieving remission after three
months of treatment.
In our study side effects at discharge were a significant predictor of
relapse in both prediction models.
Chabungbam and colleagues (12) examined sociodemographic and clinical factors associated with relapse
among patients with schizophrenia
and found that those who experienced a relapse were significantly
more likely to complain of moderate
to severe side effects of medication. A
possible explanation offered by the
authors was that patients with more
severe side effects may be those receiving a higher dosage of antipsychotics to combat relapse. In regard
to antipsychotic treatment, we found
that patients treated with first-generation antipsychotics at discharge were
more likely to have a relapse during
follow-up, which is supported by research data (3).
Like other researchers who have
assessed relapse predictors, we found
that a worse attitude toward adherence at discharge was a significant
predictor; this is believed to be one of
the most reliable predictors of relapse
in schizophrenia research. In a study
of 477 patients with schizophrenia,
Laan and colleagues (13) found that
160 patients relapsed within six
months of hospital discharge. The authors found that the relapse risk was
substantially lower when a patient
was properly adherent to the antipsychotic therapy that was prescribed
during inpatient treatment. We also
found that having a job at discharge
was protective against relapse during
follow-up. The association between
employment status and relapse has
been previously noted. In an analysis
of three years of data for 6,516 patients with schizophrenia, Haro and
colleagues (14) found that social functioning, as measured primarily by
having paid employment, was one of
the most important predictors of the
course of illness. The authors concluded that the association between
paid employment and a more favorable course was due not only to the
positive influence of work itself but
also to other factors such as social
support and patient competencies.
90
This finding is somewhat in line with
our finding that independent living
status at discharge was protective
against relapse.
A strength of this study is the inclusion of treatment outcome at hospital
discharge in the prediction model,
which also applied standardized definitions of outcome. Also, the naturalistic study design is closer to a realworld setting than a randomized controlled trial. However, the naturalistic
design lacked sufficient control for
the effect of pharmacological treatments. Rehospitalization was included in the definition of relapse, but rehospitalization may not reflect exacerbation of the illness, which should
be considered in interpreting these
results. In addition, the study was
conducted in a single European
country, and the generalizability of
the results may thus be limited. Another limitation is that substance
abuse, a well-known factor in relapse,
could not be examined because patients with comorbid substance use
disorders were not included in the
study.
Conclusions
In this study, 52% of patients with
schizophrenia experienced a relapse
within the first year of hospital discharge. Patients without a job, with a
higher HAMD-17 score, more medication side effects, and a poorer attitude
about treatment at the time of discharge were more likely to have a relapse during the year after discharge.
Therefore, providers should develop
strategies to enhance adherence and
diminish side effects before patients
are discharged from the hospital.
Helping patients maintain employment after discharge should also be
considered in treatment approaches.
Acknowledgments and disclosures
The study was performed within the framework of the German Research Network on
Schizophrenia, which is funded by the German
Federal Ministry for Education and Research
BMBF (grant 01 GI 0233).
The authors report no competing interests.
References
1.
Rabinowitz J, Lichtenberg P, Kaplan Z, et
al: Rehospitalization rates of chronically ill
schizophrenic patients discharged on a
regimen of risperidone, olanzapine, or
PSYCHIATRIC SERVICES
conventional antipsychotics. American
Journal of Psychiatry 158:266269, 2001
2. Ascher-Svanum H, Zhu B, Faries DE, et
al: The cost of relapse and the predictors of
relapse in the treatment of schizophrenia.
BMC Psychiatry 10:2, 2010
3. Leucht S, Barnes TR, Kissling W, et al: Relapse prevention in schizophrenia with
new-generation antipsychotics: a systematic review and exploratory meta-analysis of
randomized, controlled trials. American
Journal of Psychiatry 160:12091222, 2003
4. Schooler NR: Relapse and rehospitalization: comparing oral and depot antipsychotics. Journal of Clinical Psychiatry
64(suppl 16):1417, 2003
5. Gaebel W, Riesbeck M, Wolwer W, et al:
Maintenance treatment with risperidone
or low-dose haloperidol in first-episode
schizophrenia: 1-year results of a randomized controlled trial within the German
Research Network on Schizophrenia. Journal of Clinical Psychiatry 68:17631774,
2007
6. Conley RR: The burden of depressive
symptoms in people with schizophrenia.
Psychiatric Clinics of North America 32:
853861, 2009
7. Olfson M, Mechanic D, Boyer CA, et al:
Assessing clinical predictions of early rehospitalization in schizophrenia. Journal of
Nervous and Mental Disease 187:721729,
1999
8. Leifker FR, Bowie CR, Harvey PD: Determinants of everyday outcomes in schizophrenia: the influences of cognitive impairment, functional capacity, and symptoms. Schizophrenia Research 115:8287,
2009
9. Lader M: What is relapse in schizophrenia? International Journal of Clinical Psychopharmacology 9(suppl 5):59, 1995
10. Lambert M, Schimmelmann BG, Naber
D, et al: Prediction of remission as a combination of symptomatic and functional remission and adequate subjective well-being in 2960 patients with schizophrenia.
Journal of Clinical Psychiatry 67:1690
1697, 2006
11. Wobrock T, Kohler J, Klein P, et al: Achieving symptomatic remission in out-patients
with schizophrenia: a naturalistic study
with quetiapine. Acta Psychiatrica Scandinavica 120:120128, 2009
12. Chabungbam G, Avasthi A, Sharan P: Sociodemographic and clinical factors associated with relapse in schizophrenia. Psychiatry and Clinical Neuroscience 61:587
593, 2007
13. Laan W, Does YV, Sezgi B, et al: Low treatment adherence with antipsychotics is associated with relapse in psychotic disorders within six months after discharge.
Pharmacopsychiatry 43:221224, 2010
14. Haro JM, Novick D, Suarez D, et al: Remission and relapse in the outpatient care
of schizophrenia: three-year results from
the Schizophrenia Outpatient Health Outcomes study. Journal of Clinical Psychopharmacology 26:571578, 2006
o ps.psychiatryonline.org o January 2012 Vol. 63 No. 1
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Sunidhi Final PrintDocument79 paginiSunidhi Final PrintrthrthgÎncă nu există evaluări
- The Art of Ageing WellDocument3 paginiThe Art of Ageing WellDrhaidee BassÎncă nu există evaluări
- Chronic Apical Periodontitis.Document24 paginiChronic Apical Periodontitis.Alina EsanuÎncă nu există evaluări
- Block K Distribution by MMCDocument6 paginiBlock K Distribution by MMCMuhammad FaizanÎncă nu există evaluări
- The Cholesterol Myths by Uffe RavnskovDocument26 paginiThe Cholesterol Myths by Uffe Ravnskov2361983Încă nu există evaluări
- Diuretics TutorialDocument2 paginiDiuretics TutorialAbdul MosheenÎncă nu există evaluări
- Diet Prevents Polio by Maintaining Normal Blood SugarDocument69 paginiDiet Prevents Polio by Maintaining Normal Blood SugarIyemhetepÎncă nu există evaluări
- Healthy Diet Plans (Anemia)Document21 paginiHealthy Diet Plans (Anemia)Rohan GulavaniÎncă nu există evaluări
- Manifestations of Miasms in DiseaseDocument3 paginiManifestations of Miasms in Diseaselydia2301100% (2)
- PHARMACOLOGY - Midterms 1.6-Fluid and Electrolyte TRANSDocument13 paginiPHARMACOLOGY - Midterms 1.6-Fluid and Electrolyte TRANSNooneÎncă nu există evaluări
- Prepu Chapter 2 PsychDocument43 paginiPrepu Chapter 2 PsychnanaÎncă nu există evaluări
- Dialysis Basics: DR - Ashutosh Ojha MD, DNB (Gen Med) PDCC-Nephro (Student) GMCH..GuwahatiDocument36 paginiDialysis Basics: DR - Ashutosh Ojha MD, DNB (Gen Med) PDCC-Nephro (Student) GMCH..GuwahatiManish Arya JaiswalÎncă nu există evaluări
- Measles case study with Koplik's spots and rubeola virusDocument3 paginiMeasles case study with Koplik's spots and rubeola virusApex Torres0% (1)
- Measles PathophysiologyDocument1 paginăMeasles PathophysiologyAl TheóÎncă nu există evaluări
- Milk Thistle - Product PresentationDocument14 paginiMilk Thistle - Product PresentationAABHIRAMÎncă nu există evaluări
- Arthur Jones - Arthur Jones - Strength Curve AnalysisDocument15 paginiArthur Jones - Arthur Jones - Strength Curve AnalysisRafael Tavares LacerdaÎncă nu există evaluări
- Staphylococcal Food PoisoningDocument18 paginiStaphylococcal Food PoisoningMuhammad Hafidz Bin HasanÎncă nu există evaluări
- 2922radioactivity Summary Cheat Sheet..Aidan MatthewsDocument3 pagini2922radioactivity Summary Cheat Sheet..Aidan MatthewsSyed Mairaj Ul HaqÎncă nu există evaluări
- مهم للمزاولةDocument13 paginiمهم للمزاولةbelal nurseÎncă nu există evaluări
- Gem Stone Wearing MathodDocument3 paginiGem Stone Wearing MathodPandit Pramod Shukla AstroJotishÎncă nu există evaluări
- Lesson Plan in Circulatory SystemDocument10 paginiLesson Plan in Circulatory SystemRey Sarsoza92% (38)
- Chapter 69Document24 paginiChapter 69نمر نصارÎncă nu există evaluări
- Anatomy and Classification of Body Fluid ChangesDocument31 paginiAnatomy and Classification of Body Fluid ChangesRajarshi KumarÎncă nu există evaluări
- Clinical Presentation and Management of GERDDocument18 paginiClinical Presentation and Management of GERDAnnisa Ayu NabilaÎncă nu există evaluări
- BandagingDocument42 paginiBandagingMuhammad Shahzad ChandiaÎncă nu există evaluări
- GI News - November 2008: Food For ThoughtDocument13 paginiGI News - November 2008: Food For ThoughtdraganÎncă nu există evaluări
- A Comparative Study of The Clinical Efficiency of Chemomechanical Caries Removal Using Carisolv® and Papacarie® - A Papain GelDocument8 paginiA Comparative Study of The Clinical Efficiency of Chemomechanical Caries Removal Using Carisolv® and Papacarie® - A Papain GelA Aran PrastyoÎncă nu există evaluări
- Managing Hypertension in Older AdultsDocument21 paginiManaging Hypertension in Older Adultslanguha NgatiÎncă nu există evaluări
- Immunologic and Infectious DisordersDocument38 paginiImmunologic and Infectious Disordersdarla ryanÎncă nu există evaluări
- Homeopathy For Body and Soul (PDFDrive)Document707 paginiHomeopathy For Body and Soul (PDFDrive)angelobuffalo100% (5)