Documente Academic
Documente Profesional
Documente Cultură
Lung Ultrasound in The Evaluation of Pleural Effusion: Elena Prina, Antoni Torres, Carlos Roberto Ribeiro Carvalho
Încărcat de
egerpratamaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Lung Ultrasound in The Evaluation of Pleural Effusion: Elena Prina, Antoni Torres, Carlos Roberto Ribeiro Carvalho
Încărcat de
egerpratamaDrepturi de autor:
Formate disponibile
Editorial
Lung ultrasound in the evaluation of pleural effusion
Ultrassom de pulmo na avaliao de derrame pleural
Elena Prina, Antoni Torres, Carlos Roberto Ribeiro Carvalho
In recent years, there has been an increasing
interest in the use of ultrasound for the evaluation
of chest diseases, especially for the study of
bedridden, critically ill patients. In fact, the
ultrasound method presents various advantages:
it uses no radiation; it is inexpensive; it can
be used at the bedside; it is noninvasive; and
it can be repeated as necessary. In addition,
ultrasound is starting to be a method used by
professionals, other than radiologists, who have
specific clinical questions,(1) having become an
important tool for the pulmonary physician. In
this context, the utility of ultrasound for the
diagnosis and management of pleural effusion
is well documented.
In the present issue of the Brazilian Journal
of Pulmonology, Perazzo et al.(2) present a
randomized controlled trial aimed at assessing
whether ultrasound-assisted thoracentesis, in
contrast with a blinded method, would reduce the
rate of pneumothorax. The authors also aimed to
assess whether ultrasound improves the efficacy
of the procedure (in terms of the number of
successful fluid removal procedures and the
amount of fluid removed). It is of note that, in
that study, experienced operators performed both
methods, following a standardized protocol, in
order to focus attention on the influence of using
ultrasound or not, and removed other factors
that could be responsible for complications. For
these purposes, 160 inpatients and outpatients
with pleural effusion requiring pleural puncture
were randomized into two groups. In the study
group (comprising 80 patients), thoracentesis was
performed with the use of ultrasound, whereas
it was performed without ultrasound in the
control group (also comprising 80 patients). In
comparing the study and control groups, the
authors observed that the former had a significantly
lower pneumothorax rate (1.25% vs. 12.5%; p =
0.009; OR = 0.09), a higher number of patients
with successful drainage (79/80 vs. 72/80), and a
higher amount of fluid drained (mean SD: 960
500 mL vs. 770 480 mL). They concluded
that the use of ultrasound during thoracentesis
reduced the number of cases of pneumothorax
and increased the efficiency of the procedure.
The findings of Perazzo et al.(2) corroborate data
already described in the literaturethoracentesis
involving the use of ultrasound is safer than is
the blinded approach. Nevertheless, the study
is interesting because it confirms the idea that
ultrasound can provide advantages even to more
experienced operators. In addition, the study is
a randomized controlled trial, which increases
the power of their findings.
Despite its utility, ultrasound presents some
limitations. Soft tissue edema, subcutaneous
emphysema, or obesity can reduce the quality of
the images. We also think that physicians need
adequate training in order to avoid misreading
ultrasound images and, consequently, to avoid
mistakes.
Ultrasound and diagnosis of pleural
effusion
The first step in the evaluation of patients
with suspected pleural effusion is to confirm
the diagnosis, especially in the case of a white
hemithorax on chest X-rays. Ultrasound is a
useful method for these purposes because it
allows the distinction between effusion and lung
consolidations(3) and has a higher accuracy in
detecting pleural effusion in comparison with
bedside chest X-rays (93% vs. 47%).(4) In fact,
chest X-rays can detect the presence of pleural
effusion in patients in the orthostatic position
only if the volume of the effusion is at least 200
mL,(5) and the sensitivity of this method decreases
in the supine position, whereas ultrasound can
detect effusions as small as 20 mL.(6)
The ultrasound evaluation of a patient in
a sitting position is better because it allows a
more precise quantification of pleural effusion.
In this position, the free fluid will collect in
the dependent space, whereas it will be found
in a posterior location with the patient in the
supine position. In addition, ultrasound allows
the identification of adjacent structures: chest
J Bras Pneumol. 2014;40(1):1-5
Prina E, Torres A, Carvalho CRR
wall, hemidiaphragm (over the liver or spleen),
and visceral pleural surface. This is important,
especially in the case of an invasive procedure,
in order to avoid organ injury (Figure 1).
A second step is the distinction between
transudative and exudative pleural effusions.
The aspect of pleural effusion on ultrasound
can suggest the nature of the fluid, although a
definitive diagnosis requires a thoracentesis in order
to allow physical, chemical, and microbiological
studies. According to the characteristics of the
pleural effusion on ultrasound, it can appear as
anechoic (black), complex nonseptated (black
with white strands), complex septated (black
with white septa), or homogeneously echogenic
(white).(7) In general, the presence of complex
pleural effusion suggests exudative effusion,
whereas an anechogenic effusion might be
transudative. However, in contrast to what we
expect, transudative effusion can also appear
lung
spleen
d
pe
Figure 1 - Ultrasound identification of pleural effusion
at a specific site (lower image). pe: pleural effusion;
d: diaphragm; and c: chest wall.
as complex nonseptated effusion(8); this is due
to the fact that transudates are not pure water,
having various components (i.e., cells, proteins,
and lipids), and exudative effusions can also
appear as anechogenic effusion. Homogeneous
echogenic effusions are the result of hemorrhagic
effusions or empyema (Table 1).
In some cases, ultrasound images other than
those of the effusion can help assess the nature of
the pleural effusion. For example, the presence of
thickened pleura or of a pulmonary consolidation
with dynamic air bronchogram (suggestive of
an infectious origin) is usually indicative of an
exudate. The presence of a diffuse sign of lung
congestion (B lines) suggests transudative effusion
during heart failure.
Laing & Filly(9) reported that nearly 20% of
the anechogenic images of the pleura revealed a
solid lesion, not the presence of fluid. Therefore,
especially in cases of small or loculated pleural
effusion (Figure 2), or when thoracentesis
is requested, it is important to focus on the
differential diagnosis. One aspect that can
facilitate the diagnosis is that pleural effusions
are associated with a typical movement of the
adjacent structure that determines a change
in the shape of the effusionthe movement of
the collapsed lung into the effusion or that of
particles inside the fluid. The use of the M mode
can help in the visualization of the sinusoidal
movement of the collapsed lung in the fluid
(sinusoid sign).(10) However, very dense or loculated
pleural effusions might present no variation in
the shape.
Although various ultrasound methods have been
described for the quantification of the volume
of pleural effusions,(11) they all require several
measurements. We believe that knowledge of the
exact amount of fluid has limited usefulness in
clinical practice. Therefore, we prefer a qualitative
approach, which is summarized in Table 2. In
addition, ultrasound can help estimate the effect
of pleural effusion on the lung parenchyma by
enabling the visualization of different degrees
Table 1 - Ultrasound patterns and the nature of pleural effusion.
Pattern
Transudative
Exudative
Anechogenic
Complex nonseptated
Complex septated
Echogenic
J Bras Pneumol. 2014;40(1):1-5
Hemorrhagic
Lung ultrasound in the evaluation of pleural effusion
of collapse. This information, combined with
clinical judgment, can help physicians in the
decision-making process regarding thoracentesis
(Figure 3).
requires the involvement of a professional who
is more experienced in the use of ultrasound.
Ultrasound and thoracentesis
The use of ultrasound reduces the risk of
pneumothorax following thoracocentesis from
18% to 3%.(13). As shown in one retrospective
study,(13) that is especially true when the
ultrasound-guided method is used, the rates
of pneumothorax being significantly lower than
when the landmark-based method is used (4% vs.
10%). In addition, Weingardt et al.(14) demonstrated
that ultrasound can be an effective rescue method
in 88% of cases in which blind thoracocentesis
is unsuccessful. The authors noted that, in 69%
of those cases, the site of puncture chosen in
the blind approach was below the diaphragm.
Interestingly, ultrasound-guided thoracentesis
resulted safe for use in mechanically ventilated
patients as well.(15)
Ultrasound is also a more useful method to
detect pneumothorax after thoracentesis than are
chest X-rays using a supine anterior approach.
The sensitivity of these two methods is 78.6%
and 39.8%, respectively, whereas their specificity
is 98.4% and 99.3%, respectively.(16)
As shown in Figure 4, the major
ultrasonographic signs for the diagnosis of
pneumothorax are the absence of lung sliding
movement of the pleura during respiratory
excursionwhich is more evident using the M
mode with the stratosphere sign; the absence
The use of ultrasound in thoracentesis reduces
the rate of complications (i.e., pneumothorax)
and increases the successfulness of fluid removal
when compared with traditional methods.(12)
Ultrasound is especially useful when the pleural
effusion is small or loculated.
Ultrasound allows the identification of the best
site to perform the puncture and the measurement
of the depth of the adjacent organs in order
to avoid organ injury. For experts, ultrasound
allows the study of the intercostal spaces prior to
needle insertion, in order to identify aberrantly
positioned intercostal vessels, thus avoiding
vascular injury.
On ultrasound images, the appearance of
pleural effusion can also provide clues to the
necessary intervention: for example, a complex
septated effusion could require the use of a larger
catheter. There are two different techniques
employed in thoracentesis with the use of
ultrasound: the landmark-based method, in
which ultrasound is used in order to identify the
best site of the puncture; and the ultrasoundguided method, in which the procedure is
closely monitored in real time by continuous
visualization of the needle. This second method
A
Ultrasound and pneumothorax
pe
lung
pe
L
L
Figure 2 - CT (in A) and ultrasound (in B) revealing
loculated pleural effusion. pe: pleural effusion; L:
lung; and r: rib. The thin arrow indicates the parietal
pleural line.
Figure 3 - X-ray (in A) and ultrasound (in B) revealing
pleural effusion and lung collapse. pe: pleural effusion.
Table 2 - Ultrasound quantification of pleural effusion.
Quantification
Ultrasound visualization
Minimal
Costophrenic angle
Small
Range, one probe
Moderate
Range, two probes
Large or massive
Range, three or more probes
Volume estimation, mL
100
100-500
500-1,500
>1,500
J Bras Pneumol. 2014;40(1):1-5
Prina E, Torres A, Carvalho CRR
Ciber de Enfermedades Respiratorias,
Barcelona, Spain
Carlos Roberto Ribeiro Carvalho
Full Professor of Pulmonology, Heart
Institute (InCor), Hospital das Clnicas,
University of So Paulo School of
Medicine, So Paulo, Brazil
References
Figure 4 - Ultrasound signs of pneumothorax. In A,
normal lung, showing the seashore sign in M mode.
In B, pneumothorax, showing the stratosphere sign in
M mode. In C, subcutaneous emphysema. Arrowheads
indicate the pneumothorax.
of B lines (negative predictive value: 100%);
and the presence of the lung point (positive
predictive value: 100%) in the absence of massive
pneumothorax.
In summary, ultrasound represents a highly
useful tool for the evaluation of patients with
pleural effusion during the diagnostic phase
and in combination with invasive procedures.
Elena Prina*
Department of Pulmonology, Heart
Institute, University of So Paulo
School of Medicine Hospital das
Clnicas, So Paulo, Brazil
Institut Clnic del Trax (ICT), Servei
de Pneumologia, Hospital Clnic de
Barcelona, Institut dInvestigacions
Biomdiques August Pi i Sunyer
(IDIBAPS), Universitat de Barcelona,
Ciber de Enfermedades Respiratorias,
Barcelona, Spain
Antoni Torres
Full Professor of Pulmonology,
Institut Clnic del Trax (ICT), Servei
de Pneumologia, Hospital Clnic de
Barcelona, Institut dInvestigacions
Biomdiques August Pi i Sunyer
(IDIBAPS), Universitat de Barcelona,
1. Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography
for the pulmonary specialist. Chest. 2011;140(5):1332-41.
http://dx.doi.org/10.1378/chest.11-0348
2. Perazzo A, Gatto P, Barlascini C, Ferrari-Bravo M,
Nicolini A. Can ultrasound guidance reduce the risk of
pneumothorax following thoracentesis? J Bras Pneumol.
2014;40(1):6-12.
3. Yu CJ, Yang PC, Wu HD, Chang DB, Kuo SH, Luh KT.
Ultrasound study in unilateral hemithorax opacification.
Image comparison with computed tomography. Am Rev
Respir Dis. 1993;147(2):430-4. http://dx.doi.org/10.1164/
ajrccm/147.2.430
4. Lichtenstein D, Goldstein I, Mourgeon E, Cluzel
P, Grenier P, Rouby JJ. Comparative diagnostic
performances of auscultation, chest radiography, and
lung ultrasonography in acute respiratory distress
syndrome. Anesthesiology. 2004;100(1):9-15. http://
dx.doi.org/10.1097/00000542-200401000-00006
5. Blackmore CC, Black WC, Dallas RV, Crow HC. Pleural fluid
volume estimation: a chest radiograph prediction rule.
Acad Radiol. 1996;3(2):103-9. http://dx.doi.org/10.1016/
S1076-6332(05)80373-3
6. Rahman NM, Singanayagam A, Davies HE, Wrightson
JM, Mishra EK, Lee YC, et al. Diagnostic accuracy, safety
and utilisation of respiratory physician-delivered thoracic
ultrasound. Thorax. 2010;65(5):449-53. http://dx.doi.
org/10.1136/thx.2009.128496
7. Lomas DJ, Padley SG, Flower CD. The sonographic
appearances of pleural fluid. Br J Radiol. 1993;66(787):61924. http://dx.doi.org/10.1259/0007-1285-66-787-619
8. Chen HJ, Tu CY, Ling SJ, Chen W, Chiu KL, Hsia TC,
et al. Sonographic appearances in transudative pleural
effusions: not always an anechoic pattern. Ultrasound
Med Biol. 2008;34(3): 362-9. http://dx.doi.org/10.1016/j.
ultrasmedbio.2007.09.009
9. Laing FC, Filly RA. Problems in the application of
ultrasonography for the evaluation of pleural opacities.
Radiology. 1978;126(1):211-4.
10. Lichtenstein DA. Lung ultrasound in the critically
ill. Ann Intensive Care. 2014;4(1):1. http://dx.doi.
org/10.1186/2110-5820-4-1
11. Remrand F, Dellamonica J, Mao Z, Ferrari F, Bouhemad
B, Jianxin Y, et al. Multiplane ultrasound approach to
quantify pleural effusion at the bedside. Intensive Care
Med. 2010;36(4):656-64. http://dx.doi.org/10.1007/
s00134-010-1769-9
12. Diacon AH, Brutsche MH, Solr M. Accuracy of pleural
puncture sites: a prospective comparison of clinical
*Dr. Prina is a research fellow supported by the long-term research fellowship program of the European Respiratory Society.
J Bras Pneumol. 2014;40(1):1-5
Lung ultrasound in the evaluation of pleural effusion
examination with ultrasound. Chest. 2003;123(2):43641. http://dx.doi.org/10.1378/chest.123.2.436
13. Barnes TW, Morgenthaler TI, Olson EJ, Hesley GK, Decker
PA, Ryu JH. Sonographically guided thoracentesis and rate
of pneumothorax. J Clin Ultrasound. 2005;33(9):442-6.
http://dx.doi.org/10.1002/jcu.20163
14. Weingardt JP, Guico RR, Nemcek AA Jr, Li YP, Chiu ST.
Ultrasound findings following failed, clinically directed
thoracenteses. J Clin Ultrasound. 1994;22(7):419-26.
http://dx.doi.org/10.1002/jcu.1870220702
15. Lichtenstein D, Hulot JS, Rabiller A, Tostivint I, Mezire
G. Feasibility and safety of ultrasound-aided thoracentesis
in mechanically ventilated patients. Intensive Care
Med. 1999;25(9):955-8. http://dx.doi.org/10.1007/
s001340050988
16. Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural
ultrasonography versus chest radiography for the
diagnosis of pneumothorax: review of the literature
and meta-analysis. Crit Care. 2013;17(5):R208. http://
dx.doi.org/10.1186/cc13016
J Bras Pneumol. 2014;40(1):1-5
S-ar putea să vă placă și
- E-Catalogue Product List 2021-2023 (1 Des 23)Document104 paginiE-Catalogue Product List 2021-2023 (1 Des 23)deri anggri yarosahÎncă nu există evaluări
- Author Section Editor Deputy Editor Contributor DisclosuresDocument10 paginiAuthor Section Editor Deputy Editor Contributor DisclosuresannisÎncă nu există evaluări
- POCUS NeumotoraxDocument20 paginiPOCUS NeumotoraxRaydel ManuelÎncă nu există evaluări
- Blue Protocol. Lung Ultrasound in The Critically IllDocument12 paginiBlue Protocol. Lung Ultrasound in The Critically IllRomina Alfonsina Decap CarrascoÎncă nu există evaluări
- Ultrasonography in EffusionDocument6 paginiUltrasonography in EffusionRachmat AnsyoriÎncă nu există evaluări
- Content ServerDocument12 paginiContent ServerIrvan Dwi FitraÎncă nu există evaluări
- Rambhia 2016Document24 paginiRambhia 2016Heru SigitÎncă nu există evaluări
- Ultrasound A CL 2021Document17 paginiUltrasound A CL 2021Alejandra SanchezÎncă nu există evaluări
- Usg PneumotoraksDocument7 paginiUsg Pneumotoraksdicky wahyudiÎncă nu există evaluări
- Intervencion Usg EmergenciasDocument22 paginiIntervencion Usg EmergenciasSaul Gonzalez HernandezÎncă nu există evaluări
- PnemotoraksDocument4 paginiPnemotoraksGung Citra PratikaÎncă nu există evaluări
- The V-Line: A Sonographic Aid For The Confirmation of Pleural FluidDocument4 paginiThe V-Line: A Sonographic Aid For The Confirmation of Pleural FluidAlpi ApriansahÎncă nu există evaluări
- Bedside Lung Ultrasound Versus Chest X-Ray Use in The Emergency DepartmentDocument3 paginiBedside Lung Ultrasound Versus Chest X-Ray Use in The Emergency DepartmentharnellaÎncă nu există evaluări
- Jurnal RadiotoraxDocument5 paginiJurnal RadiotoraxKiki D. RestikaÎncă nu există evaluări
- Fluorescein-Enhanced Autofluorescence Thoracoscopy in Patients With Primary Spontaneous Pneumothorax and Normal SubjectsDocument5 paginiFluorescein-Enhanced Autofluorescence Thoracoscopy in Patients With Primary Spontaneous Pneumothorax and Normal SubjectsAmin Kamaril Wahyudi ArrdianÎncă nu există evaluări
- Thora CosDocument20 paginiThora CosDani VélezÎncă nu există evaluări
- Asthma: Further ReadingDocument13 paginiAsthma: Further ReadingcarlosÎncă nu există evaluări
- Guide To USDocument11 paginiGuide To USAdel HamadaÎncă nu există evaluări
- Occult Hemopneumothorax Following Chest Trauma Does Not Need A Chest TubeDocument5 paginiOccult Hemopneumothorax Following Chest Trauma Does Not Need A Chest TubeNoven MezaÎncă nu există evaluări
- Jurnal 3Document5 paginiJurnal 3Caesar RiefdiÎncă nu există evaluări
- A Case of Pneumoperitoneum in A Patient With Blunt Injury ThoraxDocument4 paginiA Case of Pneumoperitoneum in A Patient With Blunt Injury ThoraxRajeev ThilakÎncă nu există evaluări
- (1992) Yang, Pan-Chyr Luh, Kwen-Tay Chang, Dun-Bing Yu, Chong-Jen K - Ultrasonographic Evaluation of Pulmonary ConsolidationDocument6 pagini(1992) Yang, Pan-Chyr Luh, Kwen-Tay Chang, Dun-Bing Yu, Chong-Jen K - Ultrasonographic Evaluation of Pulmonary ConsolidationPer DamiánÎncă nu există evaluări
- Br. J. Anaesth.-2010-Meira-746-50Document5 paginiBr. J. Anaesth.-2010-Meira-746-50Retno SawitriÎncă nu există evaluări
- Eco VA Desde Boca A PulmonesDocument27 paginiEco VA Desde Boca A PulmonesLucila BrañaÎncă nu există evaluări
- Occult PneumotoraxDocument30 paginiOccult PneumotoraxAdif FlysÎncă nu există evaluări
- Journal Reading PulmonologiDocument21 paginiJournal Reading PulmonologiGina ArianiÎncă nu există evaluări
- Internal Medicine Department Dr. M. Djamil Hospital, Padang 2017Document21 paginiInternal Medicine Department Dr. M. Djamil Hospital, Padang 2017Gina ArianiÎncă nu există evaluări
- Doctor Fac Updated 2016Document2 paginiDoctor Fac Updated 2016Thulasi tootsieÎncă nu există evaluări
- Jurnal PneumoniaDocument8 paginiJurnal PneumoniaArmy OktaviantoÎncă nu există evaluări
- Lust StudyDocument7 paginiLust Studyadrianoneto60Încă nu există evaluări
- US Pulmón para Manejo de Atelectasias PerioperatoriasDocument11 paginiUS Pulmón para Manejo de Atelectasias PerioperatoriasJURAGOMAÎncă nu există evaluări
- Respirology - 2011 - KOEGELENBERG - Pleural Controversy Closed Needle Pleural Biopsy or Thoracoscopy Which FirstDocument9 paginiRespirology - 2011 - KOEGELENBERG - Pleural Controversy Closed Needle Pleural Biopsy or Thoracoscopy Which Firstdalozpa23Încă nu există evaluări
- Routine Use of Point-of-Care Lung Ultrasound During The COVID-19 PandemicDocument4 paginiRoutine Use of Point-of-Care Lung Ultrasound During The COVID-19 PandemicOswaldo MontesÎncă nu există evaluări
- Cuantificar Derrame PleuralDocument5 paginiCuantificar Derrame PleuralPhysiolfcaliÎncă nu există evaluări
- PIIS0749070413000729Document25 paginiPIIS0749070413000729Juan Carlos MezaÎncă nu există evaluări
- Role of Endoscopic Ultrasonography and Endoscopic Ultrasonography Guided Fine Needle Aspiration in The Evaluation of Mediastinal LesionsDocument10 paginiRole of Endoscopic Ultrasonography and Endoscopic Ultrasonography Guided Fine Needle Aspiration in The Evaluation of Mediastinal LesionsOssama Abd Al-amierÎncă nu există evaluări
- Advances in Trauma UltrasoundDocument12 paginiAdvances in Trauma UltrasoundBruce Fredy Chino ChambillaÎncă nu există evaluări
- Drowning 3Document6 paginiDrowning 3Auliadi AnsharÎncă nu există evaluări
- Clinical Applications of Transthoracic UltrasoundDocument20 paginiClinical Applications of Transthoracic UltrasoundFabiana Gonzalez da NóbregaÎncă nu există evaluări
- Occult Pneumothorax, Revisited: Review Open AccessDocument6 paginiOccult Pneumothorax, Revisited: Review Open AccessRendy NunuhituÎncă nu există evaluări
- Ecografia Toracica PDFDocument12 paginiEcografia Toracica PDFCristinaLucanÎncă nu există evaluări
- Diagnosis of Traumatic Pneumothorax - Comparison Between Lung Ultrasound and Supine Chest RadiographsDocument5 paginiDiagnosis of Traumatic Pneumothorax - Comparison Between Lung Ultrasound and Supine Chest RadiographssepputriÎncă nu există evaluări
- Lung Ultrasound For Critically Ill Patients - Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. (Am J Respir Crit Care Med. 2019)Document53 paginiLung Ultrasound For Critically Ill Patients - Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. (Am J Respir Crit Care Med. 2019)Mr. IncognitoÎncă nu există evaluări
- Musalar 2017Document5 paginiMusalar 2017SueÎncă nu există evaluări
- Bobillo Perez2019Document21 paginiBobillo Perez2019Nisa Hermina PutriÎncă nu există evaluări
- Emphysema Versus Chronic Bronchitis in COPD: Clinical and Radiologic CharacteristicsDocument8 paginiEmphysema Versus Chronic Bronchitis in COPD: Clinical and Radiologic CharacteristicsChairul Nurdin AzaliÎncă nu există evaluări
- 10 Razones para Usar Eco en CriticosDocument13 pagini10 Razones para Usar Eco en CriticosCurro MirallesÎncă nu există evaluări
- UltrasoundTraumaCh02 Fast ExamDocument23 paginiUltrasoundTraumaCh02 Fast Exam108dudleyÎncă nu există evaluări
- Risk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusDocument4 paginiRisk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusAgus KarsetiyonoÎncă nu există evaluări
- Imaging in Acute Respiratory Distress Syndrome: ReviewDocument13 paginiImaging in Acute Respiratory Distress Syndrome: ReviewIva SeptianingsihÎncă nu există evaluări
- Rastreo Por USG, Una Alternativa A RX Torax Post Colocacion de CVCDocument3 paginiRastreo Por USG, Una Alternativa A RX Torax Post Colocacion de CVCKarla Rosales MoralesÎncă nu există evaluări
- PDF DIR 5932Document5 paginiPDF DIR 5932Yogi PrasetioÎncă nu există evaluări
- Complications of Video-Assisted Thoracoscopic SurgeryDocument13 paginiComplications of Video-Assisted Thoracoscopic SurgeryNicole NewlandÎncă nu există evaluări
- Manual Aspiration Versus Chest Tube Drainage in First Episodes of Primary Spontaneous PneumothoraxDocument5 paginiManual Aspiration Versus Chest Tube Drainage in First Episodes of Primary Spontaneous PneumothoraxAmin Kamaril Wahyudi ArrdianÎncă nu există evaluări
- Thesis Endobronchial UltrasoundDocument4 paginiThesis Endobronchial Ultrasoundafknikfgd100% (2)
- Focusedassessment Withsonographyfor Trauma:Methods, Accuracy, and IndicationsDocument13 paginiFocusedassessment Withsonographyfor Trauma:Methods, Accuracy, and IndicationsOtto Guillermo SontayÎncă nu există evaluări
- NRes1 AssignmentDocument2 paginiNRes1 AssignmentAinee MeuvinÎncă nu există evaluări
- 859 FullDocument6 pagini859 FullAdif FlysÎncă nu există evaluări
- Manejo de Derrame Pleural 2019Document11 paginiManejo de Derrame Pleural 2019Jorge Luis German BecerraÎncă nu există evaluări
- Pulmonary Functional Imaging: Basics and Clinical ApplicationsDe la EverandPulmonary Functional Imaging: Basics and Clinical ApplicationsYoshiharu OhnoÎncă nu există evaluări
- Thoracic Ultrasound and Integrated ImagingDe la EverandThoracic Ultrasound and Integrated ImagingFrancesco FelettiÎncă nu există evaluări
- Currrent and Future Amangement in PsoriasisDocument13 paginiCurrrent and Future Amangement in PsoriasisegerpratamaÎncă nu există evaluări
- P ('t':'3', 'I':'3053520368') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document17 paginiP ('t':'3', 'I':'3053520368') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)alnajÎncă nu există evaluări
- Origins of Syphilis and Management in The Immunocompetent Patient: Facts and ControversiesDocument6 paginiOrigins of Syphilis and Management in The Immunocompetent Patient: Facts and ControversiesegerpratamaÎncă nu există evaluări
- The Neonatal Gastrointestinal Tract:: Developmental Anatomy, Physiology, and Clinical ImplicationsDocument9 paginiThe Neonatal Gastrointestinal Tract:: Developmental Anatomy, Physiology, and Clinical ImplicationsegerpratamaÎncă nu există evaluări
- Beta-Blocker Use and COPD Mortality: A Systematic Review and Meta-AnalysisDocument6 paginiBeta-Blocker Use and COPD Mortality: A Systematic Review and Meta-AnalysisegerpratamaÎncă nu există evaluări
- Bone and Soft Tissue TumorsDocument47 paginiBone and Soft Tissue TumorsegerpratamaÎncă nu există evaluări
- Lesson 3 ReviewDocument4 paginiLesson 3 ReviewHo Yong WaiÎncă nu există evaluări
- 10 4187@respcare 07435Document10 pagini10 4187@respcare 07435Jacqueline ViannaÎncă nu există evaluări
- Medical Exam Revision: Over 58,000 Practice Questions. We'll Help You Pass Your Exam TodayDocument2 paginiMedical Exam Revision: Over 58,000 Practice Questions. We'll Help You Pass Your Exam TodayDocSam048Încă nu există evaluări
- Blunt Thoracic Trauma - Role of Chest Radiography and Comparison With CT - Fndings and Literature ReviewDocument13 paginiBlunt Thoracic Trauma - Role of Chest Radiography and Comparison With CT - Fndings and Literature Revieworalposter PIPKRA2023Încă nu există evaluări
- Practice Mod 6 Case StudyDocument6 paginiPractice Mod 6 Case Studyvanessa100% (1)
- Med Surg Respiratory SystemDocument173 paginiMed Surg Respiratory Systembamfalcon100% (4)
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument7 paginiPhysioex Lab Report: Pre-Lab Quiz ResultsSharumathi ManivannanÎncă nu există evaluări
- Chest Trauma: Nursing 410 Western Carolina University BSN ProgramDocument29 paginiChest Trauma: Nursing 410 Western Carolina University BSN ProgramShimmering MoonÎncă nu există evaluări
- Cough and Dyspnea Case StudyDocument4 paginiCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Diagnosis and Management of COPD A Case StudyDocument4 paginiDiagnosis and Management of COPD A Case StudyZairenee QuizanaÎncă nu există evaluări
- Respiratory Case StudiesDocument6 paginiRespiratory Case Studiesadom09Încă nu există evaluări
- Mechanical Ventilation Skills and Techniques Update 2011Document79 paginiMechanical Ventilation Skills and Techniques Update 2011Juan MenaÎncă nu există evaluări
- Ten Tips To Optimize Weaning and Extubation Success in The Critically IllDocument3 paginiTen Tips To Optimize Weaning and Extubation Success in The Critically IllAurora Barrera100% (1)
- Mechanical VentilationDocument23 paginiMechanical VentilationAjit ThangeÎncă nu există evaluări
- Medicine PulDocument86 paginiMedicine Pulabhijeets3011Încă nu există evaluări
- CEDIVA Dénia, Training Center in Difficult Airway ManagementDocument29 paginiCEDIVA Dénia, Training Center in Difficult Airway ManagementCEDIVA DeniaÎncă nu există evaluări
- Bronchial Asthma Final CompilationDocument51 paginiBronchial Asthma Final CompilationNurdalila ZabaÎncă nu există evaluări
- Inspection, Palpation, Percussion, Auscultation (IPPA) TipsDocument10 paginiInspection, Palpation, Percussion, Auscultation (IPPA) TipsMarjorie Joy GreciaÎncă nu există evaluări
- Lung Volumes and CapacitiesDocument16 paginiLung Volumes and CapacitiesMoses DumbuyaÎncă nu există evaluări
- Terapi OksigenDocument33 paginiTerapi OksigenMirzaÎncă nu există evaluări
- Mip Mep Snif 2022Document4 paginiMip Mep Snif 2022Gabo BalanÎncă nu există evaluări
- NCP - Respiratory DistressDocument3 paginiNCP - Respiratory DistressDarwin QuirimitÎncă nu există evaluări
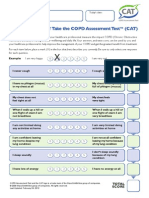
- CATest PDFDocument1 paginăCATest PDFAsrie Sukawatie PutrieÎncă nu există evaluări
- NAME: Neema Tamang Roll No:-20 Subject:-Surgery Assignment Topic:-Pneumothorax Faculty: HA 2Document9 paginiNAME: Neema Tamang Roll No:-20 Subject:-Surgery Assignment Topic:-Pneumothorax Faculty: HA 2Shreekrishna BudhathokiÎncă nu există evaluări
- Evita XL: Initial Start UpDocument4 paginiEvita XL: Initial Start UpscribdbazoÎncă nu există evaluări
- Case Scenario ArfDocument3 paginiCase Scenario ArfPam RomeroÎncă nu există evaluări
- Overview of Neonatal Respiratory Distress - Disorders of TransitionDocument14 paginiOverview of Neonatal Respiratory Distress - Disorders of TransitionAlfredo Junior Delgado PeláezÎncă nu există evaluări
- Airway Control and Ventilation - ACLS 2006 With Pics N0V09Document33 paginiAirway Control and Ventilation - ACLS 2006 With Pics N0V09percivicÎncă nu există evaluări
- DR Artana 3Document8 paginiDR Artana 3novinnaÎncă nu există evaluări