Documente Academic
Documente Profesional
Documente Cultură
Efficacy IV Acetaminophen and Lidocaine On Propofol Injection Pain
Încărcat de
ind_kusTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Efficacy IV Acetaminophen and Lidocaine On Propofol Injection Pain
Încărcat de
ind_kusDrepturi de autor:
Formate disponibile
British Journal of Anaesthesia 100 (1): 958 (2008)
doi:10.1093/bja/aem301
Advance Access publication October 23, 2007
PAIN
Efficacy of intravenous acetaminophen and lidocaine
on propofol injection pain
zgen
O. Canbay*, N. Celebi, O. Arun, A. H. Karagoz, F. Sarcaoglu and S. O
Department of Anesthesiology and Reanimation, Hacettepe University Faculty of Medicine,
06100 Shhye/Ankara, Turkey
*Corresponding author. E-mail: ozgurcanbay@yahoo.com
Background. Different methods and propofol formulations have been used to decrease propofol injection pain, but it remains an unresolved problem. We aimed to investigate the effect
of i.v. acetaminophen pretreatment on the propofol injection pain.
Results. Patient characteristics were similar among the groups. Incidence of pain on injection
of propofol in control, i.v. acetaminophen, and lidocaine groups was 64%, 22% and 8%, respectively (P,0.05).
Conclusions. Pretreatment with i.v. acetaminophen seems to be effective in attenuating pain
during i.v. injection of propofol.
Br J Anaesth 2008; 100: 958
Keywords: anaesthetics i.v., propofol; anaesthetics local, lidocaine; analgesics non-opioid,
acetaminophen; pain, injection
Accepted for publication: August 31, 2007
Propofol remains the most common drug for induction of
general anaesthesia, although it causes considerable pain
or discomfort on injection. During induction of anaesthesia, the incidence of injection pain has been shown to vary
between 28% and 90% in adults.1 Several methods have
been proposed over the years in the literature to reduce the
pain associated with i.v. injection of propofol. These
include the addition of lidocaine to propofol;2 cooling or
warming the drug;3 and pretreatment with ephedrine,
ondansetron, metoclopramide, opioids, thiopental, ketamine,3 ketorolac,4 or nafamostat.5
Of the techniques used to decrease the incidence and
intensity of pain resulting from propofol injection, the
most effective method is to inject lidocaine at 0.5 mg kg21
i.v. while applying venous occlusion before administering
propofol. Although the cause of propofol injection pain is
unknown, the activation of pain mediators such as the
release of a kininogen from the vein wall triggering a local
kinin cascade system during i.v. injection has been
suggested. Moreover, non-steroidal anti-inflammatory
drugs (NSAIDs) have been shown to diminish prostaglandin (PG) synthesis and inhibit kinin cascade, thereby reducing pain on injection of propofol.6
As an alternative to NSAIDs and selective COX-2
inhibitors, acetaminophen, whose action at a molecular
level is still not known, is widely used for pain management. Although acetaminophen does not inhibit COX
enzymes at therapeutic concentrations in vitro, it is shown
# The Board of Management and Trustees of the British Journal of Anaesthesia 2007. All rights reserved. For Permissions, please e-mail: journals.permissions@oxfordjournals.org
Downloaded from http://bja.oxfordjournals.org/ by guest on February 20, 2013
Methods. One hundred and fifty ASA I II patients undergoing general anaesthesia were
randomly allocated into three groups. A 20-gauge catheter was inserted into a superficial
radial vein of the left hand, and after the occlusion of venous drainage, Groups I, II, and III were
pretreated with 40 mg of lidocaine in saline, 50 mg of i.v. acetaminophen, and 5 ml of saline,
respectively. The occlusion was released after 2 min and one-fourth of the total propofol dose
was injected into the vein over a period of 5 s. During the injection of both pretreatment
solution and propofol, patients pain was assessed and recorded as 0 3, corresponding to no,
mild, moderate or severe pain, respectively. x2 and Kruskal Wallis tests were used for the
statistical analysis. For all analyses, differences were considered to be significant at P,0.05.
Canbay et al.
to inhibit a variant of COX enzymes in vivo. Simmons and
colleagues7 demonstrated a COX-2 variant, which is sensitive to acetaminophen.
These proposed mechanisms prompted us to investigate
the effect of i.v. acetaminophen on propofol injection
pain. In this randomized, double-blind, placebo-controlled
study, we aimed to compare the effect of i.v. acetaminophen with that of lidocaine for the prevention of
propofol-induced pain during induction of anaesthesia.
Methods
Results
The patient characteristics were similar among all the
groups (Table 1). The data on the severity and incidence of
pain during injection of pretreatment solution in the three
groups are given in Table 2. The overall incidence of pain
during i.v. injection of pretreatment with acetaminophen
was 2%, compared with 20% and 16% in each of the lidocaine and control groups, respectively (P,0.05).
Pretreatment with i.v. acetaminophen produced mild pain in
2% of patients. Pretreatment with lidocaine produced mild
pain in 18% and moderate pain in 2% of the patients.
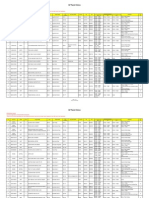
Table 1 Patient characteristics. Data are given as mean (range), mean (SD) or
numbers of patients
Groups
Age (yr)
Sex (M/F) ASA
Weight
class (I/II) (kg)
Group I lidocaine (n50) 35.02 (22 60) 20/30
Group II i.v.
30.7 (20 54) 30/20
acetaminophen (n50)
Group III control (n50) 39.3 (20 60) 26/24
46/4
48/2
68.9 (12.3)
63.7 (11.4)
47/3
70.5 (12.7)
Table 2 Number of patients with pain during i.v. injection of pretreatment
solution. *P,0.05 i.v. acetaminophen vs lidocaine and control
Severity of pain Group I lidocaine
(n550)
Group II i.v.
Group III control
acetaminophen (n550)
(n550)
No pain
Mild pain (A)
Moderate pain (B)
Severe pain (C)
Pain (ABC)
49
1
0
0
1*
96
40
9
1
0
10
42
3
5
0
8
Downloaded from http://bja.oxfordjournals.org/ by guest on February 20, 2013
After ethics committee approval of the hospital and having
obtained informed consent, 150 patients aged 20 60 yr,
ASA I or II, and undergoing general anaesthesia were
included in this study. Patients were randomly allocated to
one of the three groups of 50 each using a table of random
numbers. Patients with vascular diseases, habituation to
analgesics, sedatives or anti-anxiety drugs; allergic diseases or sensitivity to lidocaine, propofol or acetaminophen, and infection on the dorsum of their left hands were
excluded from the study.
None of the patients was premedicated before entering
the operation room. After routine monitoring (ECG, noninvasive arterial pressure, and pulse oximeter), a 20-gauge
catheter was inserted into a superficial radial vein of the
left hand and lactated Ringers solution was infused at 100
ml h21. After 5 min, lactated Ringers infusion was
stopped and the arm with the i.v. line was elevated for 15 s
for gravity drainage of venous blood. After occluding the
venous drainage using a pneumatic tourniquet ( pressure
inflated to 70 mm Hg) on the upper arm, the patients were
pretreated over a period of 10 s with one of the pretreatment solutions; 40 mg of lidocaine diluted to 5 ml (Group
I), 50 mg (5 ml) of acetaminophen (Perfalgan#) (Group
II), or 5 ml of normal saline (Group III). We asked the
patients if they felt any pain during the administration of
the pretreatment solution. The pain that occurred during
propofol injection was assessed on a four-point scale
(none0, mild1, moderate2, and severe3).
An independent anaesthetist prepared the solutions and
the investigator was blind to the contents of the solutions.
After 2 min, the occlusion was released and one-fourth of
the total calculated dose of propofol [Diprivan 1% (Zeneca
Ltd, Macclesfield, Cheshire, UK)] was delivered through
the i.v. line over a period of 5 s. No other analgesics or
sedatives were administered before propofol injection.
During the injection, the patients were asked standard questions regarding comfort of the injection. A clinician blinded
to the group assignment evaluated propofol-induced pain
using a verbal rating scale: none0 (negative response to
questioning), mild pain1 (pain reported only in response
to questioning with no behavioural signs), moderate pain2
(pain reported in response to questioning and accompanied
by a behavioural sign or pain reported spontaneously
without questioning), severe pain3 (strong vocal response
or response accompanied by facial grimacing, arm withdrawal, or tears). Thereafter, induction of anaesthesia continued with i.v. fentanyl 23 mg kg21 followed by the
remainder of the calculated dose of propofol, and vecuronium 0.1 mg kg21 to facilitate endotracheal intubation.
Heart rate, systolic, diastolic, and mean arterial pressures were recorded before the administration of pretreatment solution (considered as baseline), laryngoscopy, and
1 and 5 min after the intubation. Within 24 h after the
operation, the injection site was checked for pain, oedema,
or allergic reaction by an anaesthesiologist who was
blinded to group assignment.
On the basis of previous studies, the expected incidence
of pain was 30% in lidocaine group and 60% in saline
group.8 A power analysis indicated that a sample size of
50 was sufficient to detect a large statistical difference
with an a0.05 and power 12b0.8. The data obtained
were analysed statistically using the x2 test, analysis of
variance for demographic data, and the Kruskal Wallis
test for the incidence of propofol injection pain scores
among the groups. P,0.05 was considered significant.
Acetaminophen for propofol injection pain
Severity of pain
Group I lidocaine
(n550)
Group II i.v.
acetaminophen
(n550)
Group III
control (n550)
No pain
Mild pain (A)
Moderate pain (B)
Severe pain (C)
Pain (ABC)
46*
3
1
0
4*
39*
5
5
1
11*
18
8
14
10
32
When we evaluated the pretreatment pain in saline group,
there was mild pain in 6% and moderate pain in 10% of the
patients.
The overall incidence of pain during i.v. injection of
propofol in the three groups is shown in Table 3. In the
control group, 64% of the patients had pain during i.v.
propofol injection whereas 22% and 8% of the patients
had pain in i.v. acetaminophen and lidocaine groups,
respectively (P,0.05). During the first 24 h after the
operation, there were no complications such as pain,
oedema, or allergic reaction at the injection site. In
addition, haemodynamic variables such as heart rate, systolic, diastolic, and mean arterial pressures that were
recorded at different time intervals were similar between
the groups.
Discussion
In this study, we found that i.v. acetaminophen was effective, although not as much as lidocaine, in decreasing the
incidence of pain during i.v. injection of propofol.
Previous studies have shown that the incidence of pain on
injection of propofol is around 30% with lidocaine pretreatment and 60% in saline group.9 10 The overall incidence of pain during i.v. injection of propofol in the
control group was 64% compared with 22% in i.v. acetaminophen and with 8% in lidocaine group, suggesting that
i.v. acetaminophen injection is effective in reducing propofol injection pain compared with control. Moreover, the
overall incidence of pain during i.v. injection of pretreatment with perfalgan was 2% when it was compared with
20% and 16% that were observed in each of the lidocaine
and control groups, respectively. That is to mean, i.v. acetaminophen causes less pretreatment pain with respect to
lidocaine and control groups (P,0.05 for both comparisons). It was different from the previous studies that the
incidence of pretreatment pain of lidocaine and control
groups was unexpectedly high in our study.11
In our study, the overall incidence of pain during i.v.
injection of propofol in the lidocaine group was 8% and it
was similar to the results of Pang and colleagues12 who
reported it to be 11%. But, in some other studies higher
incidences, such as 18%13 or 42%,11 have been reported.
In these studies, the vein on the dorsum of the hand and
References
1 Tan CH, Onsiong MK. Pain on injection of propofol. Anaesthesia
1998; 53: 468 76
2 Picard P, Tramer MR. Prevention of pain on injection with propofol:
a quantitative systematic review. Anesth Analg 2000; 90: 9639
3 McCrirrick A, Hunter S. Pain on injection of propofol: the effect
of injectate temperature. Anaesthesia 1990; 45: 443 4
97
Downloaded from http://bja.oxfordjournals.org/ by guest on February 20, 2013
the pneumatic tourniquet technique was used, as in the
present study. However, the investigators did not mention
about the gravity drainage of venous blood which could be
the reason of lower incidence for propofol injection pain
in lidocaine group in our study.
We evaluated the pain using a score of 0 3 scale
system. This verbal rating scale has been used in several
previous reports that investigate the intensity of pain on
injection of propofol.14 15
Pain on injection of propofol can be immediate or
delayed. The immediate pain could be the result of a
direct irritant effect, but the kinin cascade is probably
the cause of delayed pain.16 The lipid solvent for propofol
activates the plasma kallikrein kinin system which
results in bradykinin production that increases local vein
permeability and dilation. The aqueous-phase propofol
diffuses into more free nerve endings outside the endothelial layer of the vessel which is more permeable and
dilated because of bradykinin effect, thereby intensifying
pain on injection. Inhibition of bradykinin generation by
nafamostat mesylate is shown to reduce propofol-induced
pain.16 Moreover, cold appears to lessen propofol injection
pain through suppressing the activation of plasma
kallikrein kinin system that in turn initiates enzymatic
cascade.3 17 In addition to cold, non-steroidal antiinflammatory drugs such as ketorolac are also demonstrated to reduce the propofol injection pain aggravated by
the release of local kininogens.18
In a recent study, Lee and colleagues19 showed that acetaminophen selectively suppresses peripheral PG E2 release
and increases COX-2 gene expression in a clinical model of
acute inflammation. Similarly, in another recent study, bradykinin, a bradykinin B2-receptor agonist, has been shown
to enhance both basal and lipopolysaccharide-induced PG
E2 synthesis in rat neonatal glial cells in culture.20 Also in
a recent study of Ando and colleagues,21 they have shown
that propofol characteristically causes vascular pain that
occurs in response to prostanoids, particularly PG E2. The
findings of these studies indicate that there is a relationship
between PG E2, which is selectively suppressed by acetaminophen, and bradykinin, which determines the intensity of
propofol injection pain.
The present results suggest that i.v. acetaminophen
(50 mg) pretreatment appears to be effective in reducing
the pain experienced during i.v. injection of propofol.
Further studies are required to determine the optimal doses
of i.v. acetaminophen to control propofol-induced pain.
Table 3 Number of patients with pain during i.v. injection of propofol.
*P,0.05 drugs vs control
Canbay et al.
13 Dubey PK, Prasad SS. Pain on injection of propofol: the effect of
granisetron pretreatment. Clin J Pain 2003; 19: 121 4
14 Memis D, Turan A, Karamanlioglu B, Sut N, Pamukcu Z. The use
of magnesium sulfate to prevent pain on injection of propofol.
Anesth Analg 2002; 95: 606 8
15 Agarwal A, Ansari MF, Gupta D, et al. Pretreatment with thiopental for prevention of pain associated with propofol injection.
Anesth Analg 2004; 98: 683 6
16 Nakane M, Iwama H. A potential mechanism of propofol-induced
pain on injection based on studies using nafamostat mesilate. Br J
Anaesth 1999; 83: 397 404
17 Barker P, Langton JA, Murphy P, Rowbotham DJ. Effect of prior
administration of cold saline on pain during propofol injection: a
comparison with cold propofol and propofol with lignocaine.
Anaesthesia 1991; 46: 1069 70
18 Yull DN, Barkshire KF, Dexter T. Pretreatment with ketorolac
and venous occlusion to reduce pain on injection of propofol.
Anaesthesia 2000; 55: 284 7
19 Lee YS, Kim H, Brahim JS, Rowan J, Lee G, Dionne RA.
Acetaminophen selectively suppresses peripheral prostaglandin
E2 release and increases COX-2 gene expression in a clinical
model of acute inflammation. Pain 2007; 129: 279 86
20 Levant A, Levy E, Argaman M, Fleisher-Berkovich S. Kinins and
neuroinflammation: dual effect on prostaglandin synthesis. Eur J
Pharmacol 2006; 546: 197 200
21 Ando R, Watanabe C. Characteristics of propofol-evoked vascular pain in anaesthetized rats. Br J Anaesth 2005; 95: 384 92
98
Downloaded from http://bja.oxfordjournals.org/ by guest on February 20, 2013
4 Huang YW, Buerkle H, Lee TH, et al. Effect of pretreatment with
ketorolac on propofol injection pain. Acta Anaesthesiol Scand
2002; 46: 1021 4
5 Iwama H, Nakane M, Ohmori S, et al. Nafamostat mesilate a kallikrein inhibitor prevents pain on injection with propofol. Br J
Anaesth 1998; 81: 963 4
6 Yull DN, Barkshire KF, Dexter T. Pretreatment with ketorolac
and venous occlusion to reduce pain on injection of propofol.
Anaesthesia 2000; 55: 284 7
7 Simmons DL, Botting RM, Robertson PM, Madsen ML, Vane JR.
Induction of an acetaminophen-sensitive cyclooxygenase with
reduced sensitivity to nonsteroid antiinflammatory drugs. Proc
Natl Acad Sci USA 1999; 96: 3275 80
8 Johnson RA, Harper NJ, Chadwick S, Vohra A. Pain on injection of
propofol. Methods of alleviation. Anaesthesia 1990;45: 43942
9 Nathanson MH, Gajraj NM. Reducing the pain on injection of
propofol. Anesth Analg 1996; 82: 1307 8
10 Helmers JH, Kraaijenhagen RJ, van Leeuwen L, Zuurmond WW.
Reduction of pain on injection caused by propofol. Can J Anaesth
1990; 37: 267 8
11 Agarwal A, Dhiraj S, Raza M, et al. Vein pretreatment with
magnesium sulfate to prevent pain on injection of propofol is not
justified. Can J Anaesth 2004; 51: 130 3
12 Pang WW, Mok MS, Huang S, Hwang MH. The analgesic
effect of fentanyl, morphine, meperidine, and lidocaine in the
peripheral veins: a comparative study. Anesth Analg 1998; 86:
382 6
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Estimating Hourly Anaesthetic and Surgical ReimburDocument14 paginiEstimating Hourly Anaesthetic and Surgical Reimburind_kusÎncă nu există evaluări
- Is It Time To Review The RUSH For Start Times inDocument4 paginiIs It Time To Review The RUSH For Start Times inind_kusÎncă nu există evaluări
- MADOM Emergency Preparedness Chapter-FinalDocument32 paginiMADOM Emergency Preparedness Chapter-Finalind_kusÎncă nu există evaluări
- Recommendations For The Minimal Requirements Necessary To Deliver Safe Anesthetic Procedures in Neonatal and Pediatric Age.Document21 paginiRecommendations For The Minimal Requirements Necessary To Deliver Safe Anesthetic Procedures in Neonatal and Pediatric Age.ind_kusÎncă nu există evaluări
- Gen CGRPDocument8 paginiGen CGRPind_kusÎncă nu există evaluări
- Gen CGRPDocument7 paginiGen CGRPind_kusÎncă nu există evaluări
- Ed Algorithms 2014Document52 paginiEd Algorithms 2014JakeusÎncă nu există evaluări
- Klinikal Review Ceftaroline FosamilDocument16 paginiKlinikal Review Ceftaroline Fosamilind_kusÎncă nu există evaluări
- Gen CGRPDocument22 paginiGen CGRPind_kusÎncă nu există evaluări
- Neuroimaging ICHDocument7 paginiNeuroimaging ICHind_kusÎncă nu există evaluări
- Benda Meissner Terhadap Ukuran JariDocument8 paginiBenda Meissner Terhadap Ukuran Jariind_kusÎncă nu există evaluări
- Rinitis AlergiDocument16 paginiRinitis Alergiind_kusÎncă nu există evaluări
- Dialysis in The Elderly Patienten - V35n2a09Document11 paginiDialysis in The Elderly Patienten - V35n2a09ind_kusÎncă nu există evaluări
- Immuno AnalyzerDocument36 paginiImmuno Analyzerind_kusÎncă nu există evaluări
- Sagita, Anggraeni. 2006. Pengaruh Ekstrak Andrographis Paniculata (Sambiloto) Terhadap Kadar Serum Glutamat Oksaloasetat Transaminase Pada Tikus Wistar Yang Diberi ParacetamolDocument21 paginiSagita, Anggraeni. 2006. Pengaruh Ekstrak Andrographis Paniculata (Sambiloto) Terhadap Kadar Serum Glutamat Oksaloasetat Transaminase Pada Tikus Wistar Yang Diberi ParacetamolDimasFajarSaktiÎncă nu există evaluări
- Dialysis in The Elderly Patienten - V35n2a09Document11 paginiDialysis in The Elderly Patienten - V35n2a09ind_kusÎncă nu există evaluări
- PENGARUH PEMBERIAN Curcuma Domestica Terhadap Gambaran Histologi Hepar Mencit Balb/C Yang Diberi ParasetamolDocument30 paginiPENGARUH PEMBERIAN Curcuma Domestica Terhadap Gambaran Histologi Hepar Mencit Balb/C Yang Diberi ParasetamolTutik WulandariÎncă nu există evaluări
- Aria Rhinitis Allergic Pocket GuideDocument8 paginiAria Rhinitis Allergic Pocket GuideAlfani FajarÎncă nu există evaluări
- Hepatotoxicity Associated With Acetaminophen UsageDocument4 paginiHepatotoxicity Associated With Acetaminophen Usageind_kusÎncă nu există evaluări
- Paracetamol and NSAID For Reduction Morphine Side Effect After Major SurgeryDocument6 paginiParacetamol and NSAID For Reduction Morphine Side Effect After Major Surgeryind_kusÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- LA Low Cost Dog NeuteringDocument2 paginiLA Low Cost Dog Neuteringtonys71Încă nu există evaluări
- PDF 20221013 211252 0000Document1 paginăPDF 20221013 211252 0000Meann جرابيللوÎncă nu există evaluări
- 57 2 3 BiologyDocument15 pagini57 2 3 BiologyAadya SinghÎncă nu există evaluări
- STEVENS DRRR Module 6 Opon Christian Joy ADocument7 paginiSTEVENS DRRR Module 6 Opon Christian Joy AAnthony Bryan Cartujano100% (1)
- DoctrineDocument1 paginăDoctrinevinay44Încă nu există evaluări
- Attitude of EMPLOYEES in Terms of Compliance of Health and SafetyDocument6 paginiAttitude of EMPLOYEES in Terms of Compliance of Health and SafetyJanice KimÎncă nu există evaluări
- Bias, Confounding and Fallacies in EpidemiologyDocument68 paginiBias, Confounding and Fallacies in EpidemiologyShakir KhanÎncă nu există evaluări
- Working in A Lab Risk & AssessmentDocument10 paginiWorking in A Lab Risk & AssessmentMariam KhanÎncă nu există evaluări
- Nurse - Resignation LetterDocument1 paginăNurse - Resignation LetterphoenixdashÎncă nu există evaluări
- Job Application LetterDocument12 paginiJob Application LetterIcha Aisah100% (3)
- Behaviorism in Daily LifeDocument8 paginiBehaviorism in Daily LifeMichelleTongÎncă nu există evaluări
- Glossary Mental Terms-FarsiDocument77 paginiGlossary Mental Terms-FarsiRahatullah AlamyarÎncă nu există evaluări
- Advantage CP File - FinalDocument254 paginiAdvantage CP File - FinalvegSpamÎncă nu există evaluări
- GP Panel ClinicsDocument9 paginiGP Panel ClinicsKoh WYhowÎncă nu există evaluări
- No. Kode Dan Nama Kode Diagnosa ICD 10 Nama PenyakitDocument11 paginiNo. Kode Dan Nama Kode Diagnosa ICD 10 Nama PenyakitViki AY15Încă nu există evaluări
- Philippine Science and Technology InnovationDocument7 paginiPhilippine Science and Technology Innovationgabosara298Încă nu există evaluări
- Basic Word Structure (MT)Document19 paginiBasic Word Structure (MT)leapphea932Încă nu există evaluări
- Chapter 020Document59 paginiChapter 020api-263755297Încă nu există evaluări
- PECFASDocument2 paginiPECFASNunik KhoirunnisaÎncă nu există evaluări
- Hypo - RT PC TrialDocument37 paginiHypo - RT PC TrialnitinÎncă nu există evaluări
- Module 3A: Designing Instruction in The Different Learning Delivery ModalitiesDocument30 paginiModule 3A: Designing Instruction in The Different Learning Delivery Modalitiesnel baradi67% (9)
- Urgensi Kepemimpinan Transformasional Dan Kecerdasan Emosional Pada Perusahaan Dalam Merespons Pandemi Covid-19Document11 paginiUrgensi Kepemimpinan Transformasional Dan Kecerdasan Emosional Pada Perusahaan Dalam Merespons Pandemi Covid-19Inspektorat KubarÎncă nu există evaluări
- Substation EarthingDocument5 paginiSubstation EarthingMidhun VargheseÎncă nu există evaluări
- H. Pylori IgA ELISA Package InsertDocument2 paginiH. Pylori IgA ELISA Package Inserttalha saleemÎncă nu există evaluări
- PBHCI - Mental Health ScreeningDocument2 paginiPBHCI - Mental Health ScreeningRoshin Tejero0% (1)
- Hazop PDFDocument18 paginiHazop PDFLuiz Rubens Souza Cantelli0% (1)
- Chevron Phillips Chemical Company Issued Sales SpecificationDocument1 paginăChevron Phillips Chemical Company Issued Sales SpecificationSarmiento HerminioÎncă nu există evaluări
- Rafika RespitasariDocument8 paginiRafika RespitasariYeyen SatriyaniÎncă nu există evaluări
- Stanford CWLP HandbookDocument60 paginiStanford CWLP HandbookDon DoehlaÎncă nu există evaluări
- Child Health Services-1Document44 paginiChild Health Services-1francisÎncă nu există evaluări