Documente Academic
Documente Profesional
Documente Cultură
Routine Dermatologist-Performed Full-Body Skin Examination and Early Melanoma Detection
Încărcat de
Seflan Syahir AhliadiTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Routine Dermatologist-Performed Full-Body Skin Examination and Early Melanoma Detection
Încărcat de
Seflan Syahir AhliadiDrepturi de autor:
Formate disponibile
STUDY
Routine Dermatologist-Performed Full-Body Skin
Examination and Early Melanoma Detection
Jonathan Kantor, MD, MSCE; Deborah E. Kantor, MSN, CRNP
Objective: To determine the proportion of patients in
a private dermatology practice in whom melanoma was
detected but was not the presenting complaint.
Design: Retrospective analytical case series.
Setting: Private dermatology practice in Florida, from
July 2005 through October 2008.
Patients: Patients with 126 melanomas, of which 51 were
invasive and 75 were melanomas in situ.
Main Outcome Measures: Proportion of melanomas detected as a result of patient complaint vs proportion determined by dermatologist-conducted full-body
skin examination (FBSE). As a secondary analysis, we used
logistic regression odds ratios (ORs) of association to examine whether dermatologist detection rather than patient complaint was associated with detecting thinner
melanomas. A post hoc analysis was performed using a
thickness cutoff of 1.0 mm to define a deep melanoma.
Results: Overall, 56.3% (95% confidence interval
[CI], 47.6%-65.1%) of melanomas were found by the
dermatologist and were not part of the presenting
complaint. Of melanomas in situ, 60.0% (95% CI,
48.7%-71.3%) were dermatologist detected. Dermatologist detection was significantly associated with
thinner melanomas, with an OR of 0.42 (P = .04). We
found a significant association between thinner melanomas as a group (thickness 1 mm) and dermatologist detection, with a logistic regression OR of 5.0
(95% CI, 1.0-25.3).
Conclusions: Most melanomas detected in a generalpractice dermatology setting were found as a result of dermatologist-initiated FBSE, not patient complaint. We
found that dermatologist detection was associated with
thinner melanomas and an increasing likelihood of the
melanoma being in situ.
Arch Dermatol. 2009;145(8):873-876
ARLY MELANOMA DETECTION
is the cornerstone of effective
treatment, but guidelines remain sparse regarding appropriate screening procedures
for both the general population as well as
high-risk patients.1-5 Despite an estimated
62 480 new cases of melanoma in the United
States in 2008 alone,6 a 2-year-old call for
increased action on melanoma screening
and awareness remains largely unheeded.7
For editorial comment
see page 926
Author Affiliations: North
Florida Dermatology Associates,
Jacksonville.
In clinical practice, many patients present with focused complaints and may not
request a full-body skin examination
(FBSE). One study8 has suggested that 30%
of dermatologists perform FBSEs on all patients and that 49% examine all patients
felt to be at increased risk.
While it is known that screening identifies melanomas at an earlier stage than
(REPRINTED) ARCH DERMATOL/ VOL 145 (NO. 8), AUG 2009
873
would be found otherwise9,10 and that physicians detect melanomas with less tumor
thickness,11,12 the US Preventive Service Task
Force1 states that current evidence is insufficient to recommend for or against routine screening. The population seen in skin
cancer screenings differs markedly from that
seen in a dermatology practice with a highrisk patient population.13-15
Our aim was to determine the proportion of patients in a private dermatology
practice in whom melanoma was detected
but was not the presenting complaint. If a
substantial proportion of melanomas are detected only after a dermatologists examination, this may suggest that FBSE, and not
simply a problem-focused approach, should
at least be considered for selected patients.
METHODS
A retrospective analytical case series was
conducted over a 3-year period. All patients
seen by one of the authors ( J.K.) and diag-
WWW.ARCHDERMATOL.COM
2009 American Medical Association. All rights reserved.
Downloaded From: http://archderm.jamanetwork.com/ by seflan syahir on 11/03/2015
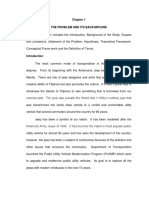
Table. Baseline Patient Characteristics a
Group
Characteristic
Age, mean, y
Male sex
Depth, mm
Clark level, mean
History of melanoma
History of nonmelanoma skin cancer
Family history of melanoma
a Data
Overall
(N=126)
With
Patient-Detected
Melanoma
(n = 55)
With Dermatologist-Detected
Melanoma
(n = 71)
59.9 (57.3-62.5)
61.1 (52.5-69.7)
0.27 (0.17-0.37)
0.75 (0.52-0.98)
13.5 (7.4-19.5)
35.7 (27.2-44.2)
14.3 (8.1-20.5)
57.5 (53.3-61.7)
58.2 (44.7-71.6)
0.40 (0.19-0.62)
0.94 (0.56-1.32)
18.2 (7.7-28.7)
25.5 (13.6-37.3)
16.4 (6.3-26.5)
61.8 (58.5-65.1)
63.4 (51.9-74.9)
0.16 (0.09-0.24)
0.61 (0.32-0.89)
9.9 (2.8-17.0)
43.7 (31.8-55.5)
12.7 (4.7-20.6)
are presented as percentages (95% confidence intervals) except where noted.
nosed as having melanoma or melanoma in situ were
included in the study. The primary study question was what
proportion of melanomas ultimately diagnosed by the dermatologist was not part of the patients presenting complaint
and thus may not have been detected without a FBSE. This
was calculated using the simple proportion of patients
whose melanomas were self-detected and presented with
95% confidence intervals (CIs).
As a secondary analysis, we used logistic regression odds
ratios (ORs) of association to examine whether dermatologist
detection rather than patient complaint was associated with detecting thinner melanomas. A post hoc analysis was performed using a thickness cutoff of 1.0 mm to define a deep
melanoma.
Only patients with biopsy-proven invasive melanoma or
melanoma in situ were included in this study. Melanomas
detected as a result of any nondermatologist actions (eg,
brought to the patients attention by their spouse, friend, or
primary care physician) were classified as patient detected. If
a patient requested an FBSE without noting a particular
lesion, or if they were referred for a different lesion than the
melanoma, the melanoma would be classified as physician
detected. Institutional review board review and exempted
approval were obtained for this study. Statistical analyses
were conducted using Stata for Windows XP (version 10.0;
Stata Corp, College Station, Texas).
A greater proportion of melanomas in the
physician-detected group (mean, 63.4%; 95% CI,
51.9%-74.9%) than in the patient-detected group
(mean, 54.5%; 95% CI, 41.0%-68.1%) were in situ.
Including only invasive melanomas, the median (SD)
melanoma depth for the physician-detected group was
0.33 (0.41) mm, and for the patient-detected group
the median depth was 0.55 (0.96) mm.
We found a statistically significant association
between increasing melanoma depth and patient
detection. The univariate OR of association between a
patient-noted melanoma and increasing depth was
2.39 (P =.04). Conversely, dermatologist detection was
significantly associated with thinner melanomas, with
an OR of 0.42 (P = .04). Univariate logistic regression
ORs failed to demonstrate an association between
other baseline characteristics such as patient sex or
age and melanoma depth. A post hoc analysis was performed using a cutoff of 1.0 mm for classification of
deep melanomas, a cutoff used in other melanoma
studies in the past.16 We found a significant association between thinner melanomas as a group (thickness
1 mm) and dermatologist detection, with a logistic
regression OR of 5.0 (95% CI, 1.0-25.3).
RESULTS
Of the 126 cases of melanoma, 75 were in situ and 51
represented invasive melanoma. Melanoma depth ranged
from 0 (in situ) to 4.0 mm. The mean melanoma depth,
including in situ lesions, was 0.27 mm (95% CI, 0.170.37), and the mean depth including only invasive melanomas was 0.67 mm (95% CI, 0.45-0.88). The median
(SD) depth for invasive melanomas was 0.40 (0.76) mm.
The mean patient age was 60 years (range, 15-92 years),
and 61% of the patients were male. Overall, a total of
56.3% (95% CI, 47.6%-65.1%) of melanomas were found
by the dermatologist and were not part of the presenting complaint. Of melanomas in situ, 60.0% (95% CI,
48.7%-71.3%) were dermatologist detected. Conversely, 43.7% (95% CI, 34.9%-52.4%) of melanomas were
found as a result of being part of the chief complaint. Baseline patient characteristics (Table) did not differ significantly based on whether melanoma was found as a result of the presenting complaint.
COMMENT
The incidence of malignant melanoma is rising in the
United States and worldwide, and investigators continue to struggle with understanding both the etiology
of this trend and its clinical significance. It remains unclear whether this increase may be related to detection
bias, other factors such as increased UV exposure, or other,
as-yet unelucidated causes.17,18
Data on melanoma detection among patients in whom
the pigmented lesion was not the primary complaint may
help to promote education and encourage future patients to avail themselves of FBSE. In addition, there are
no uniform recommendations on FBSEs by clinicians, and
those few studies that have addressed this issue tend to
focus on either detection by primary care physicians,19-21 detection in tertiary referral centers,12,22 or detection in a screening setting.4,23 As highlighted in an editorial by Geller et al,7 randomized controlled trials of
(REPRINTED) ARCH DERMATOL/ VOL 145 (NO. 8), AUG 2009
874
WWW.ARCHDERMATOL.COM
2009 American Medical Association. All rights reserved.
Downloaded From: http://archderm.jamanetwork.com/ by seflan syahir on 11/03/2015
melanoma screening in a high-risk population will likely
never be completed, and holding out for this level of evidence may be both intellectually nave and ethically misguided.
Most melanomas detected in a general-practice
dermatology setting were found as a result of a
dermatologist-initiated FBSE. Melanomas that were
found as a result of cutaneous examination represent
56.3% of the total number of melanomas found over a
3-year period. Fully 60% of melanomas in situ were
detected at this early stage owing to dermatologistprompted examination. Moreover, we found that dermatologist detection was associated with thinner melanomas and an increasing likelihood of the melanoma
being in situ. We also demonstrated a clinically significant association between thinner melanomas as a
group (1 mm) and dermatologist detection. These
findings have obvious and important implications for
clinical practice.
These data suggest that minimizing the substantial public health and financial impact of melanoma may be aided
by an FBSE. While self-examination plays a critical role
in early detection, prior studies12,16,24 have suggested that
physicians, and dermatologists in particular, may be better able to detect melanomas with lesser tumor thickness. Because increasing tumor thickness is closely correlated with decreasing survival, it follows that complete
examination plays an important role, particularly in highrisk populations.25
Prior studies in tertiary referral centers found a
lower proportion of melanomas detected by the physicians, ranging from 14% of melanomas that were physician detected in a University of Michigan study11 to
16% at Memorial Sloan-Kettering Cancer Center,22 and
24% at Johns Hopkins University. 12 A populationbased study from Queensland, Australia, found that
25% of melanomas were physician detected,19 and an
Italian study found 34% of melanomas to be physician
detected.26
This study has several limitations. The population
included in this study may not be generalizable to the
general population, and therefore far-reaching conclusions regarding the broad value of melanoma screening
should be avoided. Moreover, this population also may
not be generalizable to high-risk populations seen in
other communities. Finally, the rate of melanoma
detection by the dermatologist in this study (J.K.) may
not be generalizable to other practicing dermatologists.
Other limitations of this study include its limited
sample size as well as its retrospective nature, but again,
our goal was not to determine the true proportion of melanomas detected by dermatologists but to establish whether
this represents a clinically significant number and, if so,
to advocate for further research in this important area.
Subtle population differences, both in terms of baseline
melanoma incidence as well as self-detection patterns and
practices, may substantially alter the background proportion of melanomas that are detected by the dermatologist. What is important, however, is that a large percentagemore than half in our studyof melanomas may
not have been detected in the absence of a dermatologistconducted FBSE.
Melanoma is one of the few cancers affecting young
adults and will be responsible for some 8420 deaths in
the United States in 2008 alone.6,27 Any intervention
that has the potential to mitigate this toll merits at least
detailed consideration, especially if associated with only
minimal cost and inconvenience. Recently, a randomized controlled trial28 (RCT) was performed to assess
the effectiveness of an education program for patient
self-examination in siblings of patients with melanoma,
and there has been an increasing push to screen for
melanoma on a national basis.7
Early melanoma detection may be accomplished either
by patient self-detection or by physician examination. 2 9 - 3 1 Encouraging patients to perform selfexaminations, while practiced widely, has yielded mixed
results. The Check It Out trial,32 which included motivated subjects actively part of an RCT, demonstrated only
a 55% self-examination rate at 12 months.
Dermatologists frequently detect melanomas, but
the proportion of melanomas that are dermatologist
detected, rather than patient self-detected, remains
unknown. If a substantial proportion of melanomas
are detected by dermatologists, this would argue for
the wider adoption of FBSEs by dermatologists even in
patients who do not request an FBSE.
To our knowledge, this is the first study to examine
the proportion of melanomas detected by a privatepractice dermatologist and not noted by the patient. Because both referral patterns, as well as baseline melanoma risk, differ markedly in the United States, Australia,
and Europe, these data will hopefully be more generalizable to the American population. These data are also
more generalizable than those derived from a referral center. Moreover, future cost-effectiveness studies could
hopefully take some of our data into account to develop
a more robust model. Although the cost-effectiveness of
melanoma screening has been evaluated in the past, the
models findings were sensitive to a number of factors,
thus limiting their broad applicability.33,34 Finally, as noted
herein, most screening programs focus on the general
population or primary care population rather than on the
population seen in dermatologists offices, which may have
dramatic effects on the cost-effectiveness estimates
usefulness.
The value of dermatologist detection is bolstered by
our findings that not only are most melanomas found
by the physician but that dermatologist detection has a
statistically significant association with the detection
of thinner melanomas. This supports both the internal
and external validity of our results. Thus, FBSEs confer both an absolute benefit (detecting most melanomas) as well as a clinically significant marginal benefit
(detecting melanomas with less tumor thickness). We
hope that these findings will help spur large
population-based studies in high-risk populations to
develop an evidence-based approach to determining
appropriate screening practices and intervals.
Although the most recent update from the US Preventive Service Task Force again found the evidence
insufficient to recommend for or against routine melanoma screening, 1 this recommendation applies to
screening by primary care physicians, not examination
(REPRINTED) ARCH DERMATOL/ VOL 145 (NO. 8), AUG 2009
875
WWW.ARCHDERMATOL.COM
2009 American Medical Association. All rights reserved.
Downloaded From: http://archderm.jamanetwork.com/ by seflan syahir on 11/03/2015
of high-risk patients by dermatologists. Further
research in this area, and in the cost-effectiveness of
screening, may lead to important changes in practice
that could potentially reduce melanoma mortality and
improve patient outcomes.
Accepted for Publication: February 26, 2009.
Correspondence: Jonathan Kantor, MD, MSCE, North
Florida Dermatology Associates, 1551 Riverside Ave,
Jacksonville, FL 32204 (jonkantor@gmail.com).
Author Contributions: Both authors had full access to
all the data in the study and take responsibility for the
integrity of the data and the accuracy of the data analysis. Study concept and design: J. Kantor and D.E. Kantor.
Acquisition of data: J. Kantor. Analysis and interpretation
of data: J. Kantor and D.E. Kantor. Drafting of the manuscript: J. Kantor. Critical revision of the manuscript for important intellectual content: J. Kantor and D.E. Kantor. Statistical analysis: J. Kantor. Administrative, technical, and
material support: J. Kantor and D.E. Kantor.
Financial Disclosure: None reported.
Previous Presentation: An earlier version of these data
was presented at the American Society for Dermatologic
Surgery Annual Meeting; October 12, 2007; Chicago,
Illinois.
Additional Contributions: Tiffany White, ST, and Melissa
Khaophachanh, MA, assisted with data collection and abstraction and Lisa Thomas, CCRC, provided regulatory
assistance.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
REFERENCES
25.
1. U.S. Preventive Services Task Force. Screening for skin cancer: U.S. Preventive
Services Task Force recommendation statement. Ann Intern Med. 2009;150
(3):188-193.
2. Wolff T, Tai E, Miller T. Screening for skin cancer: an update of the evidence for
the U.S. Preventive Services Task Force. Ann Intern Med. 2009;150(3):194198.
3. Ferrini RL, Perlman M, Hill L. American College of Preventive Medicine policy
statement: screening for skin cancer. Am J Prev Med. 1998;14(1):80-82.
4. Koh HK. Melanoma screening: focusing the public health journey. Arch Dermatol.
2007;143(1):101-103.
5. Landow K. Skin cancer screening guidelines for older patients? Postgrad Med.
2004;116(5):57.
6. American Cancer Society. Cancer Facts & Figures. Atlanta, GA: American Cancer Society; 2008.
7. Geller AC, Miller DR, Swetter SM, Demierre MF, Gilchrest BA. A call for the development and implementation of a targeted national melanoma screening program.
Arch Dermatol. 2006;142(4):504-507.
8. Federman DG, Kravetz JD, Kirsner RS. Skin cancer screening by dermatologists: prevalence and barriers. J Am Acad Dermatol. 2002;46(5):710-714.
9. Swerlick RA, Chen S. The melanoma epidemic: more apparent than real? Mayo
Clin Proc. 1997;72(6):559-564.
10. Fisher NM, Schaffer JV, Berwick M, Bolognia JL. Breslow depth of cutaneous
melanoma: impact of factors related to surveillance of the skin, including prior
skin biopsies and family history of melanoma. J Am Acad Dermatol. 2005;
53(3):393-406.
11. Schwartz JL, Wang TS, Hamilton TA, Lowe L, Sondak VK, Johnson TM. Thin pri-
26.
27.
28.
29.
30.
31.
32.
33.
34.
(REPRINTED) ARCH DERMATOL/ VOL 145 (NO. 8), AUG 2009
876
mary cutaneous melanomas: associated detection patterns, lesion characteristics, and patient characteristics. Cancer. 2002;95(7):1562-1568.
Epstein DS, Lange JR, Gruber SB, Mofid M, Koch SE. Is physician detection associated with thinner melanomas? JAMA. 1999;281(7):640-643.
Youl PH, Janda M, Elwood M, Lowe JB, Ring IT, Aitken JF. Who attends skin
cancer clinics within a randomized melanoma screening program? Cancer Detect Prev. 2006;30(1):44-51.
Goldberg MS, Doucette JT, Lim HW, Spencer J, Carucci JA, Rigel DS. Risk factors for presumptive melanoma in skin cancer screening: American Academy of
Dermatology National Melanoma/Skin Cancer Screening Program experience
2001-2005. J Am Acad Dermatol. 2007;57(1):60-66.
Azzarello LM, Jacobsen PB. Factors influencing participation in cutaneous screening among individuals with a family history of melanoma. J Am Acad Dermatol.
2007;56(3):398-406.
Carli P, De Giorgi V, Palli D, et al; Italian Multidisciplinary Group on Melanoma.
Dermatologist detection and skin self-examination are associated with thinner
melanomas: results from a survey of the Italian Multidisciplinary Group on
Melanoma. Arch Dermatol. 2003;139(5):607-612.
Berwick M, Armstrong BK, Ben-Porat L, et al. Sun exposure and mortality from
melanoma. J Natl Cancer Inst. 2005;97(3):195-199.
Lamberg L. Epidemic of malignant melanoma: true increase or better detection?
JAMA. 2002;287(17):2201.
McPherson M, Elwood M, English DR, Baade PD, Youl PH, Aitken JF. Presentation and detection of invasive melanoma in a high-risk population. J Am Acad
Dermatol. 2006;54(5):783-792.
Aitken JF, Janda M, Elwood M, Youl PH, Ring IT, Lowe JB. Clinical outcomes
from skin screening clinics within a community-based melanoma screening
program. J Am Acad Dermatol. 2006;54(1):105-114.
Friedman KP, Whitaker-Worth DL, Grin C, Grant-Kels JM. Melanoma screening
behavior among primary care physicians. Cutis. 2004;74(5):305-311.
Brady MS, Oliveria SA, Christos PJ, et al. Patterns of detection in patients with
cutaneous melanoma. Cancer. 2000;89(2):342-347.
Geller AC, Zhang Z, Sober AJ, et al. The first 15 years of the American Academy
of Dermatology skin cancer screening programs: 1985-1999. J Am Acad Dermatol.
2003;48(1):34-41.
Carli P, De Giorgi V, Palli D, et al. Patterns of detection of superficial spreading
and nodular-type melanoma: a multicenter Italian study. Dermatol Surg. 2004;
30(11):1371-1375.
Carli P, Balzi D, de Giorgi V, et al. Results of surveillance programme aimed at
early diagnosis of cutaneous melanoma in high risk Mediterranean subjects. Eur
J Dermatol. 2003;13(5):482-486.
Carli P, De Giorgi V, Palli D, et al. Self-detected cutaneous melanomas in Italian
patients. Clin Exp Dermatol. 2004;29(6):593-596.
Geller AC, Swetter SM, Brooks K, Demierre MF, Yaroch AL. Screening, early detection, and trends for melanoma: current status (2000-2006) and future directions.
J Am Acad Dermatol. 2007;57(4):555-572, quiz 573-576.
Geller AC, Emmons KM, Brooks DR, et al. A randomized trial to improve early
detection and prevention practices among siblings of melanoma patients. Cancer.
2006;107(4):806-814.
Markovic SN, Erickson LA, Rao RD, et al; Melanoma Study Group of the Mayo
Clinic Cancer Center. Malignant melanoma in the 21st century, part 1: epidemiology, risk factors, screening, prevention, and diagnosis. Mayo Clin Proc. 2007;
82(3):364-380.
Martin RA, Weinstock MA, Risica PM, Smith K, Rakowski W. Factors associated
with thorough skin self-examination for the early detection of melanoma. J Eur
Acad Dermatol Venereol. 2007;21(8):1074-1081.
Janda M, Youl PH, Lowe JB, et al. What motivates men age 50 years to participate in a screening program for melanoma? Cancer. 2006;107(4):815-823.
Weinstock MA, Risica PM, Martin RA, et al. Melanoma early detection with thorough skin self-examination: the Check It Out randomized trial. Am J Prev Med.
2007;32(6):517-524.
Losina E, Walensky RP, Geller A, et al. Visual screening for malignant melanoma: a cost-effectiveness analysis. Arch Dermatol. 2007;143(1):21-28.
Freedberg KA, Geller AC, Miller DR, Lew RA, Koh HK. Screening for malignant
melanoma: a cost-effectiveness analysis. J Am Acad Dermatol. 1999;41(5, pt
1):738-745.
WWW.ARCHDERMATOL.COM
2009 American Medical Association. All rights reserved.
Downloaded From: http://archderm.jamanetwork.com/ by seflan syahir on 11/03/2015
S-ar putea să vă placă și
- Research Methodology Multiple Choice QuestionsDocument313 paginiResearch Methodology Multiple Choice QuestionsRaaj Patil100% (2)
- Simple Ultrasound Rules To Distinguish Between Benign and Malignant Adnexal Masses Before Surgery: Prospective Validation by IOTA GroupDocument16 paginiSimple Ultrasound Rules To Distinguish Between Benign and Malignant Adnexal Masses Before Surgery: Prospective Validation by IOTA GroupherryÎncă nu există evaluări
- Diagnostic Errors in Pediatric RadiologyDocument8 paginiDiagnostic Errors in Pediatric Radiologyapi-47872350Încă nu există evaluări
- Template - 4SHS-Module-Practical Research 1Document17 paginiTemplate - 4SHS-Module-Practical Research 1Jeanny Mae Pesebre50% (2)
- Contents of Elementary Science in A Spiral ProgressionDocument11 paginiContents of Elementary Science in A Spiral ProgressionHepshebah De Dios SantuyoÎncă nu există evaluări
- Comparative Analysis-Convenience Between Minibus and Jeepney1.0Document38 paginiComparative Analysis-Convenience Between Minibus and Jeepney1.0Lucia Del Casa100% (2)
- Text-Based MaterialsDocument24 paginiText-Based MaterialsAlfeo Original100% (1)
- Case Studies in Advanced Skin Cancer Management: An Osce Viva ResourceDe la EverandCase Studies in Advanced Skin Cancer Management: An Osce Viva ResourceÎncă nu există evaluări
- Predicting The Risk of Malignancy in Adnexal Masses Based On IOTA AJOG 2016Document14 paginiPredicting The Risk of Malignancy in Adnexal Masses Based On IOTA AJOG 2016Fernando Suarez ChumaceroÎncă nu există evaluări
- Complete Skin Examination Is Essential in The Assessment Dermatology PatientsDocument3 paginiComplete Skin Examination Is Essential in The Assessment Dermatology Patientsseptian88_cahyoÎncă nu există evaluări
- Application of Mohs Micrographic Surgery Appropriate-Use Criteria To Skin Cancers at A University Health SystemDocument7 paginiApplication of Mohs Micrographic Surgery Appropriate-Use Criteria To Skin Cancers at A University Health SystemJose Pablo FrancoÎncă nu există evaluări
- Jurnal Ca KulitDocument10 paginiJurnal Ca Kulitilham darnoÎncă nu există evaluări
- Early Ovarian Cancer PDFDocument5 paginiEarly Ovarian Cancer PDFAndreeaPopescuÎncă nu există evaluări
- Full Title: Accuracy of Clinical Breast Examination's AbnormalitiesDocument21 paginiFull Title: Accuracy of Clinical Breast Examination's AbnormalitiesMaria AyaÎncă nu există evaluări
- Russo Et Al-2019-Journal of The European Academy of Dermatology and Venereology PDFDocument20 paginiRusso Et Al-2019-Journal of The European Academy of Dermatology and Venereology PDFMaria MogosÎncă nu există evaluări
- 2011 Article 342Document4 pagini2011 Article 342Gilang IrwansyahÎncă nu există evaluări
- Breast CA ScreeningDocument8 paginiBreast CA Screeningchristelm_1Încă nu există evaluări
- Comment On “ The First 30  Years of TheDocument1 paginăComment On “ The First 30  Years of TheYilianeth Mena DazaÎncă nu există evaluări
- Relative Importance of Traditional Risk Factors For Malignant Melanoma in The Czech PopulationDocument5 paginiRelative Importance of Traditional Risk Factors For Malignant Melanoma in The Czech PopulationFanialiahsaniÎncă nu există evaluări
- The Benefit of Tru-Cut Biopsy in Breast Masses: Poster No.: Congress: Type: Authors: KeywordsDocument8 paginiThe Benefit of Tru-Cut Biopsy in Breast Masses: Poster No.: Congress: Type: Authors: Keywordsم.محمدولدعليÎncă nu există evaluări
- A Major Issue in MedicineDocument29 paginiA Major Issue in MedicineSiti NajwaÎncă nu există evaluări
- Pediatric Imaging MistakesDocument8 paginiPediatric Imaging MistakesGoran MaliÎncă nu există evaluări
- Residual Breast Tissue After Mastectomy, How Often and Where It Is LocatedDocument11 paginiResidual Breast Tissue After Mastectomy, How Often and Where It Is LocatedBunga Tri AmandaÎncă nu există evaluări
- Research ArticleDocument8 paginiResearch ArticleGrace Juniaty GozaliÎncă nu există evaluări
- Tumores Malignos de Anexos CutáneosDocument7 paginiTumores Malignos de Anexos CutáneostisadermaÎncă nu există evaluări
- Eficacia de Azul de Metileno VO en ColonoDocument11 paginiEficacia de Azul de Metileno VO en ColonoMarielaDiazÎncă nu există evaluări
- Does Tumor Grade Influence The Rate of Lymph Node Metastasis in Apparent Early Stage Ovarian Cancer?Document4 paginiDoes Tumor Grade Influence The Rate of Lymph Node Metastasis in Apparent Early Stage Ovarian Cancer?Herry SasukeÎncă nu există evaluări
- Training Situational Awareness To Reduce Surgical Errors in The Operating RoomDocument11 paginiTraining Situational Awareness To Reduce Surgical Errors in The Operating RoomPaul PereyraÎncă nu există evaluări
- Why Most Gene Expression Signatures of Tumors Have Not Been Useful in The ClinicDocument3 paginiWhy Most Gene Expression Signatures of Tumors Have Not Been Useful in The ClinicSELÎncă nu există evaluări
- The Small Fatal Choroidal Melanoma Study. A Survey by The European Ophthalmic Oncology GroupDocument9 paginiThe Small Fatal Choroidal Melanoma Study. A Survey by The European Ophthalmic Oncology GroupAsti DwiningsihÎncă nu există evaluări
- 1 s2.0 S0002939419300625 Main PDFDocument9 pagini1 s2.0 S0002939419300625 Main PDFAsti DwiningsihÎncă nu există evaluări
- Current and Future Use of Radiological Images in The Management of Gynecological Malignancies - A Survey of Practice in The UKDocument21 paginiCurrent and Future Use of Radiological Images in The Management of Gynecological Malignancies - A Survey of Practice in The UKKrishna PanduÎncă nu există evaluări
- Exact ArticleDocument6 paginiExact ArticleMuhammad WaqasÎncă nu există evaluări
- Chloramphenicol Wound Infection ProphylaxisDocument3 paginiChloramphenicol Wound Infection ProphylaxisSupasit SuerungruangÎncă nu există evaluări
- Knut Tel 2014Document6 paginiKnut Tel 2014IridaeÎncă nu există evaluări
- Trends in Delayed Breast Cancer Diagnosis After ReDocument9 paginiTrends in Delayed Breast Cancer Diagnosis After ReeugeniaÎncă nu există evaluări
- Journal of Surgical Oncology - 2013 - Fortunato - When Mastectomy Is Needed Is The Nipple Sparing Procedure A New StandardDocument6 paginiJournal of Surgical Oncology - 2013 - Fortunato - When Mastectomy Is Needed Is The Nipple Sparing Procedure A New StandardJethro ConcepcionÎncă nu există evaluări
- Jiang 2021Document10 paginiJiang 2021Putri Tamara DasantosÎncă nu există evaluări
- ACCP Cxca Screening 2011Document8 paginiACCP Cxca Screening 2011Lizeth López LeónÎncă nu există evaluări
- Comparative Effectiveness of Digital Breast Tomosynthesis For Breast Cancer Screening Among Women 40-64 Years OldDocument8 paginiComparative Effectiveness of Digital Breast Tomosynthesis For Breast Cancer Screening Among Women 40-64 Years OldAmalia fhyÎncă nu există evaluări
- Breast Cancer Risk Prediction Using Data Mining Classification TechniquesDocument11 paginiBreast Cancer Risk Prediction Using Data Mining Classification TechniquesNeige Devi SamyonoÎncă nu există evaluări
- Topical Application of Photofrin For Photodynamic Diagnosis of Oral NeoplasmsDocument10 paginiTopical Application of Photofrin For Photodynamic Diagnosis of Oral NeoplasmsYerly Ramirez MuñozÎncă nu există evaluări
- Clinical Practice GuidelinesDocument6 paginiClinical Practice GuidelinesFlorina SimniceanuÎncă nu există evaluări
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDocument12 paginiClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieÎncă nu există evaluări
- Philippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Document48 paginiPhilippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Dasha VeeÎncă nu există evaluări
- Clinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceDocument3 paginiClinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceHector ReinozoÎncă nu există evaluări
- Trimethoprim-Sulfamethoxazole Versus Placebo For Uncomplicated Skin AbscessDocument10 paginiTrimethoprim-Sulfamethoxazole Versus Placebo For Uncomplicated Skin AbscessAljavainÎncă nu există evaluări
- The Effect of Anesthetic Technique On - Opioid Receptor Expression and Immune Cell Infiltration in Breast CancerDocument5 paginiThe Effect of Anesthetic Technique On - Opioid Receptor Expression and Immune Cell Infiltration in Breast CanceroliviafabitaÎncă nu există evaluări
- Care Pathway of Women With Interval Breast Cancer in 2016 - 2022 - Clinical BreaDocument9 paginiCare Pathway of Women With Interval Breast Cancer in 2016 - 2022 - Clinical BreaAd AdrianaÎncă nu există evaluări
- Completion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessDocument7 paginiCompletion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessRadita Dwihaning PutriÎncă nu există evaluări
- DV2 - 1007 3432 3 EdDocument12 paginiDV2 - 1007 3432 3 EdZannuba NoorÎncă nu există evaluări
- International Ovarian Tumour Analysis (IOTA) Phase 5Document22 paginiInternational Ovarian Tumour Analysis (IOTA) Phase 5RachnaÎncă nu există evaluări
- Treatment of Wilms TumorDocument10 paginiTreatment of Wilms TumortrysutrisnorahantanÎncă nu există evaluări
- Research Article: Risk Factors of Lymph Edema in Breast Cancer PatientsDocument8 paginiResearch Article: Risk Factors of Lymph Edema in Breast Cancer PatientsidaÎncă nu există evaluări
- Risk Factors For Wound Dehiscence After Laparotomy - Clinical Control TrialDocument9 paginiRisk Factors For Wound Dehiscence After Laparotomy - Clinical Control TrialsaryindrianyÎncă nu există evaluări
- FNAB ParotisDocument4 paginiFNAB ParotissreshtamukhiÎncă nu există evaluări
- Actualizacion en Carcinoma de EndometrioDocument21 paginiActualizacion en Carcinoma de Endometriowilliam.cardales03Încă nu există evaluări
- Rosen's Breast Pathology IntroductionDocument18 paginiRosen's Breast Pathology IntroductionyoussÎncă nu există evaluări
- NIH Public Access: Author ManuscriptDocument18 paginiNIH Public Access: Author ManuscriptYosua_123Încă nu există evaluări
- Symptom Report in Detecting Breast Cancer-Related 34 ItemsDocument8 paginiSymptom Report in Detecting Breast Cancer-Related 34 ItemsGustavo Adolfo Pimentel ParraÎncă nu există evaluări
- Video 6Document6 paginiVideo 6NYONGKERÎncă nu există evaluări
- Study of Fine Needle Aspiration Cytology of Breast Lump: Correlation of Cytologically Malignant Cases With Their Histological FindingsDocument5 paginiStudy of Fine Needle Aspiration Cytology of Breast Lump: Correlation of Cytologically Malignant Cases With Their Histological FindingsArvind Vashi AroraÎncă nu există evaluări
- The Royal College of Radiologists Breast Group Breast Imaging ClassificationDocument4 paginiThe Royal College of Radiologists Breast Group Breast Imaging ClassificationJosé Zaim Delgado RamírezÎncă nu există evaluări
- Garbe2007 PDFDocument7 paginiGarbe2007 PDFArsen NitÎncă nu există evaluări
- Rabbit-Tortoise Model for Cancer CureDe la EverandRabbit-Tortoise Model for Cancer CureÎncă nu există evaluări
- 322 Seflan Syahir Ahliadi Ikatan Dokter Indonesia15481567875c46ff736e76bDocument1 pagină322 Seflan Syahir Ahliadi Ikatan Dokter Indonesia15481567875c46ff736e76bSeflan Syahir AhliadiÎncă nu există evaluări
- 257 Seflan Syahir Ahliadi Ikatan Dokter Indonesia15482157395c47e5bbdf431Document1 pagină257 Seflan Syahir Ahliadi Ikatan Dokter Indonesia15482157395c47e5bbdf431Seflan Syahir AhliadiÎncă nu există evaluări
- Algo Tachycardia PDFDocument1 paginăAlgo Tachycardia PDFYudhistira AdiÎncă nu există evaluări
- 515 Seflan Syahir Ahliadi Ikatan Dokter Indonesia15493567205c594eb108006Document1 pagină515 Seflan Syahir Ahliadi Ikatan Dokter Indonesia15493567205c594eb108006Seflan Syahir AhliadiÎncă nu există evaluări
- Hyper Guidelines 2011Document13 paginiHyper Guidelines 2011Seflan Syahir AhliadiÎncă nu există evaluări
- Pengumuman Pemilihan Peminatan Ns Individual Periode X Tahun 2018 PDFDocument3 paginiPengumuman Pemilihan Peminatan Ns Individual Periode X Tahun 2018 PDFSeflan Syahir AhliadiÎncă nu există evaluări
- Hyper Guidelines 2011Document65 paginiHyper Guidelines 2011wrocha2000Încă nu există evaluări
- WWW Medscape PDFDocument16 paginiWWW Medscape PDFSeflan Syahir AhliadiÎncă nu există evaluări
- Cetoacidosis DiabeticaDocument26 paginiCetoacidosis DiabeticaAbdi OlivaÎncă nu există evaluări
- Non-Melanoma UYD Eng Nov2013 PDFDocument11 paginiNon-Melanoma UYD Eng Nov2013 PDFSeflan Syahir AhliadiÎncă nu există evaluări
- Non MelanomaDocument20 paginiNon MelanomaSeflan Syahir AhliadiÎncă nu există evaluări
- Group Assignment 1-Summarise The article-TT-SET-augmented-with-POT PDFDocument15 paginiGroup Assignment 1-Summarise The article-TT-SET-augmented-with-POT PDFRuan Jin JinÎncă nu există evaluări
- Class Size and Academic Achievement of Secondary SchoolDocument6 paginiClass Size and Academic Achievement of Secondary SchoolBilalÎncă nu există evaluări
- Swati Tripathi: Jayoti Vidyapeeth Womens University, JaipurDocument18 paginiSwati Tripathi: Jayoti Vidyapeeth Womens University, JaipurdrsurendrakumarÎncă nu există evaluări
- Who Does Marketing Research?Document12 paginiWho Does Marketing Research?Stephanie Venenoso0% (1)
- PDF 84043Document20 paginiPDF 84043Ea VillavicencioÎncă nu există evaluări
- Implementasi Persyaratan Administrasi PRDocument28 paginiImplementasi Persyaratan Administrasi PRREZANDI ZAKI RIZQIULLAHÎncă nu există evaluări
- Handbook On Local and Regional Governance (Filipe Teles)Document530 paginiHandbook On Local and Regional Governance (Filipe Teles)Jonathan FerueloÎncă nu există evaluări
- Architectural Engineering and Design ManagementDocument78 paginiArchitectural Engineering and Design ManagementabhishekBajÎncă nu există evaluări
- Doh Ao2016-0009Document10 paginiDoh Ao2016-0009Are Pee EtcÎncă nu există evaluări
- Sorptivity Test 01Document5 paginiSorptivity Test 01Shaheer Ahmed KhanÎncă nu există evaluări
- Statistical Package For The Social Sciences (SPSSDocument8 paginiStatistical Package For The Social Sciences (SPSSAnonymous 0w6ZIvJODLÎncă nu există evaluări
- Biotic Research and MethologyDocument5 paginiBiotic Research and MethologyChinnu SalimathÎncă nu există evaluări
- Senior Associate - Strategy & Transactions - StrategyDocument3 paginiSenior Associate - Strategy & Transactions - Strategyanshul suryanÎncă nu există evaluări
- Social Media Coaching Research Lynnwernham1Document36 paginiSocial Media Coaching Research Lynnwernham1Roger AugeÎncă nu există evaluări
- Ethics Programs and Their Dimensions : &even N. BrennerDocument9 paginiEthics Programs and Their Dimensions : &even N. BrennerBilalAshrafÎncă nu există evaluări
- Mba Assignment SampleDocument5 paginiMba Assignment Sampleabdallah abdÎncă nu există evaluări
- Nepali Consumer SatisfactionDocument4 paginiNepali Consumer SatisfactionPradip SubediÎncă nu există evaluări
- The Effect of Being Orphans in The Socialization Abilities of The Children in DSWD Affiliated CenterDocument67 paginiThe Effect of Being Orphans in The Socialization Abilities of The Children in DSWD Affiliated CenterMarj BaquialÎncă nu există evaluări
- Monitoring The Health-Related Sustainable Development Goals (SDGS)Document10 paginiMonitoring The Health-Related Sustainable Development Goals (SDGS)feyreÎncă nu există evaluări
- DEMONSTRATIONDocument8 paginiDEMONSTRATIONs.leop.jacobmarionÎncă nu există evaluări
- Currency Recognition and Fake Note DetectionDocument8 paginiCurrency Recognition and Fake Note Detectionرامي اليمنيÎncă nu există evaluări
- Bystranowski 2021Document23 paginiBystranowski 2021irmÎncă nu există evaluări
- Enshassi, A., Al Najjar, J., & Kumaraswamy, M. (2009) - Delays and Cost Overruns in The Construction Projects in The Gaza StripDocument26 paginiEnshassi, A., Al Najjar, J., & Kumaraswamy, M. (2009) - Delays and Cost Overruns in The Construction Projects in The Gaza StripdimlouÎncă nu există evaluări
- Some Cost Contributors To Large-Scale ProgramsDocument10 paginiSome Cost Contributors To Large-Scale ProgramsHannah Mae LamedaÎncă nu există evaluări
- PreviewDocument24 paginiPreviewFrediyanto HendrayaniÎncă nu există evaluări