Documente Academic
Documente Profesional
Documente Cultură
Female Reproductive System
Încărcat de
JayricDepalobosDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Female Reproductive System
Încărcat de
JayricDepalobosDrepturi de autor:
Formate disponibile
[PHYSIOLOGY LECTURE DR.
URSUA ] January 9, 2014
Gonadotropic Hormones and Their Effects on the
Ovaries
The ovarian changes that occur during the sexual
cycle depend completely on the gonadotropic
hormones FSH and LH, secreted by the anterior
pituitary gland
In the absence of these hormones, the ovaries
remain inactive.
At age 9 to 12 years, the pituitary begins to secrete
progressively more FSH and LH, which leads to onset
of normal monthly sexual cycles beginning between
the ages of 11 and 15 years.
This period of change is called puberty, and the time
of the first menstrual cycle is called menarche
Hypothalamo-pituitary-ovary axis disruption and
stress may cause disrupted menstruation
Ovarian Follicle Growth-"Follicular" Phase of the
Ovarian Cycle
This accelerated growth is caused by the following:
primordial follicle - ovum surrounded by a single layer of
granulosa cells.
The granulosa cells provide nourishment for the ovum and
secrete an oocyte maturation-inhibiting factor that keeps
the ovum suspended in its primordial state in the prophase
stage of meiotic division.
The first stage of follicular growth is moderate enlargement of
the ovum itself, which increases in diameter twofold to
threefold. Then follows growth of additional layers of
granulosa cells in some of the follicles; these follicles are
known as primary follicles.
During the first few days of each monthly female
sexual cycle- the concentrations of both FSH and LH
increase where FSH> LH.
These hormones, especially FSH, cause accelerated
growth of 6 to 12 primary follicles each month.
This causes:
a. Rapid proliferation of the granulosa cells, giving
rise to many more layers of these cells.
b. Spindle cells derived from the ovary interstitium
collect in several layers outside the granulosa
cells, giving rise to a second mass of cells called
the theca.
Layers: theca interna = secrete additional
steroid sex hormones (estrogen and
progesterone).
(1) Estrogen causes the granulosa cells to form
increasing numbers of FSH receptors; this causes a
positive feedback effect, making the granulosa cells
even more sensitive to FSH.
(2) FSH and the estrogens combine to promote LH
receptors on the original granulosa cells, thus
allowing LH stimulation to occur in addition to FSH
stimulation and creating an even more rapid increase
in follicular secretion.
(3) The increasing estrogens from the follicle plus the
increasing LH from the anterior pituitary gland act
together to cause proliferation of the follicular thecal
cells and increase their secretion as well.
Only One Follicle Fully Matures Each Month, and the
Remainder Undergo Atresia.*
Development of Antral and Vesicular Follicles
theca externa = develops into a highly vascular
connective tissue capsule that becomes the
capsule of the developing follicle.
After the early proliferative phase of growth- the mass
of granulosa cells secretes a follicular fluid that
contains high concentration of estrogen
Accumulation of this fluid causes an antrum to
appear within the mass of granulosa cells
The early growth of the primary follicle up to the
antral stage is stimulated mainly by FSH alone. Then
greatly accelerated growth occurs, leading to still
larger follicles called vesicular follicles
After a week or more of growth-but before ovulation
occurs-one of the follicles begins to outgrow all the
others; the remaining 5 to 11 developing follicles
involute (a process called atresia)-follicles are said to
become atretic.
The single follicle reaches a diameter of 1 to 1.5
centimeters at the time of ovulation and is called the
mature follicle.
Ovulation in a woman who has a normal 28-day
female sexual cycle occurs 14 days after the onset of
menstruation.
Shortly before ovulation, the protruding outer wall of
the follicle swells rapidly, and a small area in the
center of the follicular capsule, called the stigma,
protrudes like a nipple
In another 30 minutes or so- fluid begins to ooze from
the follicle through the stigma, and about 2 minutes
later, the stigma ruptures widely
This viscous fluid carries with it the ovum surrounded
by a mass of several thousand small granulosa cells,
called the corona radiata.
Surge of LH Is Necessary for Ovulation. LH is
necessary for final follicular growth and ovulation.
Without this hormone, even when large quantities of
FSH are available, the follicle will not progress to the
stage of ovulation.
Initiation of Ovulation
LH -causes rapid secretion of follicular steroid hormones that
contain progesterone.
(1) The theca externa release proteolytic enzymes
from lysosomes, causing dissolution and weakening of
the follicular wall, resulting in further swelling of the
entire follicle and degeneration of the stigma.
(2) Simultaneously, there is rapid growth of new
blood vessels into the follicle wall, and at the same
time, prostaglandins (local hormones that cause
vasodilation) are secreted into the follicular tissues.
These two effects cause plasma transudation into the
follicle, which contributes to follicle swelling.
[PHYSIOLOGY LECTURE DR. URSUA ] January 9, 2014
Finally, the combination of follicle swelling and
simultaneous degeneration of the stigma causes
follicle rupture, with discharge of the ovum.
hormones are also converted by the granulosa cells
into the female hormones.
In the normal female, the corpus luteum grows to
about 1.5 centimeters in diameter, reaching this
stage of development 7 to 8 days after ovulation.
About 12 days after ovulation it begins to involute,
becoming the corpus albicans. Then replaced by
connective tissue and over months is absorbed.
Luteinizing Function of LH
The change of granulosa and theca interna cells into
lutein cells is dependent mainly on LH.
This function gives LH its name-"luteinizing," for
"yellowing.
Luteinization also depends on extrusion of the ovum
from the follicle.
A hormone in the follicular fluid called luteinizationinhibiting factor, holds the luteinization process
until after ovulation.
*Once LH (mainly that secreted during the ovulatory surge)
has acted on the granulosa and theca cells to cause
luteinization, the newly formed lutein cells seem to be
programmed to go through a preordained sequence of :
(1) proliferation,
(2) enlargement, and
(3) secretion, followed by
(4) degeneration. All this occurs in about 12 days
** chorionic gonadotropin, which is secreted by the placenta,
can act on the corpus luteum to prolong its life-usually
maintaining it for at least the first 2 to 4 months of pregnancy
Involution of the Corpus Luteum and Onset of the Next
Ovarian Cycle
Postulated mechanism of ovulation
First few hours after expulsion of the ovum from the
follicle, the remaining granulosa and theca interna
cells change rapidly into lutein cells.
They enlarge in diameter and become filled with lipid
inclusions that give them a yellowish appearance.
This process is called luteinization, and the total
mass of cells together is called the corpus luteum.
The granulosa cells in the corpus luteum develop
extensive intracellular smooth endoplasmic reticula
that form large amounts of progesterone and
estrogen (more progesterone than estrogen).
The theca cells form mainly the androgens
androstenedione and testosterone rather than
female sex hormones. However, most of these
Estrogen in particular and progesteron, secreted by
the corpus luteum during the luteal phase of the
ovarian cycle, have strong feedback effects on the
anterior pituitary gland to maintain low secretory
rates of both FSH and LH.
The lutein cells secrete small amounts of the
hormone inhibin, the same as the inhibin secreted
by the Sertoli cells
This hormone inhibits secretion by the anterior
pituitary gland, especially FSH secretion.
Low in concentrations or loss of both FSH and LH
result, causes the corpus luteum to degenerate
completely, a process called involution
Final involution normally occurs at the end of almost
exactly 12 days of corpus luteum life- which is around
the 26th day of the normal female sexual cycle- 2
days before menstruation begins.
The sudden cessation of secretion of estrogen,
progesterone, and inhibin by the corpus luteum
removes the feedback inhibition of the anterior
pituitary gland, allowing it to begin secreting
increasing amounts of FSH and LH again- initiate the
growth of new follicles- beginning a new ovarian
cycle.
The paucity of secretion of progesterone and estrogen
at this time also leads to menstruation by the uterus.
About every 28 days, gonadotropic hormones from
the anterior pituitary gland cause about 8 to 12 new
follicles to begin to grow in the ovaries. One of these
follicles finally becomes "mature" and ovulates on the
14th day of the cycle. During growth of the follicles,
mainly estrogen is secreted.
After ovulation, the secretory cells of the ovulating
follicle develop into a corpus luteum that secretes
large quantities of both the major female hormones,
progesterone and estrogen.
[PHYSIOLOGY LECTURE DR. URSUA ] January 9, 2014
After another 2 weeks, the corpus luteum
degenerates, whereupon the ovarian hormones
estrogen and progesterone decrease greatly, and
menstruation begins.
A new ovarian cycle then follows.
The two types of ovarian sex hormones are the estrogens
and the progestins. *
The most important of the estrogens is the hormone
estradiol, and by far the most important progestin is
progesterone.
Estrogens mainly promote proliferation and growth of
specific cells in the body that are responsible for the
development of most secondary sexual
characteristics of the female.
The progestins function mainly to prepare the uterus
for pregnancy and the breasts for lactation.
***
Clomiphene citrate (50mg 1x/day for 5 days) ovulation
induction;
Side effect: multiple gestation
Injection of HCG positive urine effects:
Frogs sperm formation
Rabbits ovulation
Mid-cycle pain due to irritation and prostaglandins
Ovary Folliculogenesis and Hormogenesis
KY jelly interferes with sperm
LH test ovulation kit
If LH (+) - ovulation after 24-36 hours
Notetakers:
Ang, Adrian
Dagdagen, Roselyn
S-ar putea să vă placă și
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Document3 pagini"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosÎncă nu există evaluări
- Sample Child Dedication ProgramDocument1 paginăSample Child Dedication ProgramJayricDepalobos100% (2)
- Paeds Crack Notes-1Document111 paginiPaeds Crack Notes-1Ashutosh Krishna JadhavÎncă nu există evaluări
- Gen-126 Leave Out of Island PDFDocument3 paginiGen-126 Leave Out of Island PDFNalin HettiarachchiÎncă nu există evaluări
- Clinical Pastoral OrientationDocument3 paginiClinical Pastoral OrientationJayricDepalobos100% (1)
- Phillip Serrano. OIS ReportDocument5 paginiPhillip Serrano. OIS ReportReno Gazette JournalÎncă nu există evaluări
- 6 Velasquez, Jr. V Lisondra LandDocument2 pagini6 Velasquez, Jr. V Lisondra LandAngelica Bautista100% (1)
- CA3 Therapeutic Modalities EXAMM KingDocument10 paginiCA3 Therapeutic Modalities EXAMM KingKing Ebarle WangÎncă nu există evaluări
- Brothers in Arms - Road To Hill 30 - 2005 - UbisoftDocument18 paginiBrothers in Arms - Road To Hill 30 - 2005 - UbisoftWanderson PereiraÎncă nu există evaluări
- The Menstrual CycleDocument6 paginiThe Menstrual CycleiwennieÎncă nu există evaluări
- Major Depressive Disorder PDFDocument22 paginiMajor Depressive Disorder PDFapi-545811586Încă nu există evaluări
- Disorders of Motility2Document46 paginiDisorders of Motility2valdomiroÎncă nu există evaluări
- Afrisya Bimo Siwendro Marisha Yadian Putri Preceptor: DR - Liza Nursanty, Spb. FinacsDocument32 paginiAfrisya Bimo Siwendro Marisha Yadian Putri Preceptor: DR - Liza Nursanty, Spb. FinacsirmaÎncă nu există evaluări
- Medad Andrology Special Note NMT13 PDFDocument70 paginiMedad Andrology Special Note NMT13 PDFSelim TarekÎncă nu există evaluări
- Acute Urinary ObstructionDocument34 paginiAcute Urinary ObstructionHafizur RashidÎncă nu există evaluări
- PE, Tamponade, Constrictive PericarditisDocument1 paginăPE, Tamponade, Constrictive PericarditisKaylee HvezdaÎncă nu există evaluări
- Musculoskeletal: Unit 553 September 2018Document34 paginiMusculoskeletal: Unit 553 September 2018dragon66Încă nu există evaluări
- Check Unit 557 Jan-Feb Genetics v3 PDFDocument36 paginiCheck Unit 557 Jan-Feb Genetics v3 PDFdragon66Încă nu există evaluări
- Heart SoundsDocument2 paginiHeart Soundsdanny_awwadÎncă nu există evaluări
- Pneumothorax & Hemothorax: Farshid MokhberiDocument32 paginiPneumothorax & Hemothorax: Farshid MokhberiYan Sheng HoÎncă nu există evaluări
- Ophthalmology - Passmedicine 2012 - 62013146Document18 paginiOphthalmology - Passmedicine 2012 - 62013146abuahmed&janaÎncă nu există evaluări
- Leg UlcerDocument28 paginiLeg UlcerRanindya PutriÎncă nu există evaluări
- Neuromuscular DisordersDocument73 paginiNeuromuscular Disordersnurwahidah100% (1)
- Precocious PubertyDocument30 paginiPrecocious PubertyNeha SharmaÎncă nu există evaluări
- Urinary Incontinence, Kegel Exercises, Nabothian Cyst, Postpartum ThyroiditisDocument7 paginiUrinary Incontinence, Kegel Exercises, Nabothian Cyst, Postpartum ThyroiditisAbedDabajaÎncă nu există evaluări
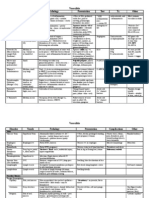
- Contraception TableDocument3 paginiContraception Tableapi-341691306Încă nu există evaluări
- Respiratory DiseasesDocument2 paginiRespiratory Diseasessarguss14Încă nu există evaluări
- Growth & Development of An Adolescent (2380)Document8 paginiGrowth & Development of An Adolescent (2380)ta CÎncă nu există evaluări
- Sexual Precocity PDFDocument5 paginiSexual Precocity PDFmist73Încă nu există evaluări
- Obstetrics - GynecologyDocument214 paginiObstetrics - Gynecologyteena6506763Încă nu există evaluări
- Neurology - Saif.wesmosis.2013 104907Document68 paginiNeurology - Saif.wesmosis.2013 104907Helene AlawamiÎncă nu există evaluări
- Puberty Normal and AbnormalDocument41 paginiPuberty Normal and AbnormalTonyScariaÎncă nu există evaluări
- 2m Male SystemDocument6 pagini2m Male SystemfrabziÎncă nu există evaluări
- LV RV FailureDocument118 paginiLV RV FailureMirza Thaariq HapsitoÎncă nu există evaluări
- GI and Hemagology & Oncology QuizDocument41 paginiGI and Hemagology & Oncology Quizwalt65Încă nu există evaluări
- PATHO 4-3 Diseases of The EsophagusDocument7 paginiPATHO 4-3 Diseases of The EsophagusMiguel Cuevas DolotÎncă nu există evaluări
- Anti Maniac DrugsDocument32 paginiAnti Maniac DrugsMohamad SamirÎncă nu există evaluări
- 3 - Precocious PubertyDocument9 pagini3 - Precocious PubertyJohnM.GiraldoÎncă nu există evaluări
- Scrotal MassesDocument19 paginiScrotal MassesJohnÎncă nu există evaluări
- Precocious VS Early Puberty, SiskaDocument21 paginiPrecocious VS Early Puberty, SiskapuspaÎncă nu există evaluări
- Physiology and PubertyDocument8 paginiPhysiology and PubertynofiajahÎncă nu există evaluări
- Treatment and Outcomes of Precocious Puberty: An UpdateDocument11 paginiTreatment and Outcomes of Precocious Puberty: An UpdateAbdurrahman Hasanuddin100% (1)
- Puberty Normal and AbnormalDocument8 paginiPuberty Normal and Abnormalclear mindÎncă nu există evaluări
- Systolic Dysfunction:: Types of Heart FailureDocument13 paginiSystolic Dysfunction:: Types of Heart FailureElisabeth F. OjhaÎncă nu există evaluări
- Cardiac Emergencies PDFDocument57 paginiCardiac Emergencies PDFJohn Paulo CatacutanÎncă nu există evaluări
- NEPHROTIC SYNDROME - HamidDocument20 paginiNEPHROTIC SYNDROME - HamidAbdul Hamid OmarÎncă nu există evaluări
- Quizlet (4) MMMMMMDocument30 paginiQuizlet (4) MMMMMMnaimÎncă nu există evaluări
- USMLE Step 2 (3) - Thyroid DiseaseDocument4 paginiUSMLE Step 2 (3) - Thyroid DiseaseMavra zÎncă nu există evaluări
- Aldomet Altace Atenolol Verapamil: Medication Brand Name Drug ClassDocument11 paginiAldomet Altace Atenolol Verapamil: Medication Brand Name Drug Classshellyrn2010Încă nu există evaluări
- Gyne - Congenital AnomaliesDocument170 paginiGyne - Congenital Anomaliesonijino100% (1)
- Endocrine System - Internal MedicineDocument39 paginiEndocrine System - Internal MedicineDaanishÎncă nu există evaluări
- Motor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)Document2 paginiMotor Neuron Disease: Amyotrophic Lateral Sclerosis (ALS)james cordenÎncă nu există evaluări
- Idiopathic Central Precocious Puberty A Case ReportDocument8 paginiIdiopathic Central Precocious Puberty A Case ReportCarolyn CapisnonÎncă nu există evaluări
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 paginiVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesÎncă nu există evaluări
- 8.1b. Systole-Diastole & Cardiac CycleDocument34 pagini8.1b. Systole-Diastole & Cardiac Cycleverysedatedx100% (1)
- Types of Anxiety Disorder Panic DisorderDocument8 paginiTypes of Anxiety Disorder Panic DisordermananggulayÎncă nu există evaluări
- REVISED-Med TaperingDocument3 paginiREVISED-Med TaperingDwi HerawatiÎncă nu există evaluări
- VASCULITISDocument79 paginiVASCULITISSol CamusÎncă nu există evaluări
- طب الاطفالDocument36 paginiطب الاطفالziad ayman100% (1)
- Female Reproductive System: UterusDocument44 paginiFemale Reproductive System: UterusBeni KurniawanÎncă nu există evaluări
- (MED II) 1.05 Emergencies in Cancer PatientsDocument17 pagini(MED II) 1.05 Emergencies in Cancer PatientsJearwin AngelesÎncă nu există evaluări
- Approach To Pleura LeffusionDocument91 paginiApproach To Pleura Leffusionrodie1050% (1)
- CSF AnalysisDocument6 paginiCSF Analysisfrederico_Încă nu există evaluări
- Pregnancy Preparation: The Menstrual CycleDocument4 paginiPregnancy Preparation: The Menstrual CycleTobias GummÎncă nu există evaluări
- Monthly Ovarian CycleDocument54 paginiMonthly Ovarian CycleSalman KhanÎncă nu există evaluări
- ILA4Document7 paginiILA4Fadhlina OmarÎncă nu există evaluări
- TP Anglais FinalDocument7 paginiTP Anglais FinalGift NgongoÎncă nu există evaluări
- The LightDocument2 paginiThe LightJayricDepalobosÎncă nu există evaluări
- Chapter 01 ChoicesDocument9 paginiChapter 01 ChoicesJayricDepalobosÎncă nu există evaluări
- Bill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341Document1 paginăBill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341JayricDepalobosÎncă nu există evaluări
- FWD: Schedule Change AdvisoryDocument2 paginiFWD: Schedule Change AdvisoryJayricDepalobosÎncă nu există evaluări
- Shipping Confirmation 1264941Document1 paginăShipping Confirmation 1264941JayricDepalobosÎncă nu există evaluări
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocument13 paginiConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosÎncă nu există evaluări
- Medical Ward 1 Service 2 CensusDocument13 paginiMedical Ward 1 Service 2 CensusJayricDepalobosÎncă nu există evaluări
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocument2 paginiWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosÎncă nu există evaluări
- Female BW - 3800 BL - 55 AS - 8,9 PA - 40Document3 paginiFemale BW - 3800 BL - 55 AS - 8,9 PA - 40JayricDepalobosÎncă nu există evaluări
- Thalassemia: Presentor: Don Jayric DepalobosDocument19 paginiThalassemia: Presentor: Don Jayric DepalobosJayricDepalobosÎncă nu există evaluări
- YHH Strategic Plan 2016-2017Document5 paginiYHH Strategic Plan 2016-2017JayricDepalobosÎncă nu există evaluări
- Acquaintance Party ParticipantsDocument1 paginăAcquaintance Party ParticipantsJayricDepalobosÎncă nu există evaluări
- Peer Evaluation For Group 5Document1 paginăPeer Evaluation For Group 5JayricDepalobosÎncă nu există evaluări
- CAA Concert ProgramDocument2 paginiCAA Concert ProgramJayricDepalobosÎncă nu există evaluări
- Teen Parenting Brochure AssignmentDocument1 paginăTeen Parenting Brochure AssignmentJayricDepalobosÎncă nu există evaluări
- Department of Community & Family Medicine Md-Dcfmc-046-O1: CBHP June 01, 2017Document1 paginăDepartment of Community & Family Medicine Md-Dcfmc-046-O1: CBHP June 01, 2017JayricDepalobosÎncă nu există evaluări
- Acute Gastroenteritis: By: Madhavi Pandya Priyanka NandiDocument16 paginiAcute Gastroenteritis: By: Madhavi Pandya Priyanka NandiJayricDepalobosÎncă nu există evaluări
- Parasitology 18 Lung FlukesDocument25 paginiParasitology 18 Lung FlukesJayricDepalobosÎncă nu există evaluări
- Basic Physical Examination in ENT PDFDocument44 paginiBasic Physical Examination in ENT PDFJayricDepalobosÎncă nu există evaluări
- Microbiology Lecture Series Luz Gregoria Lazo-Velasco, MDDocument105 paginiMicrobiology Lecture Series Luz Gregoria Lazo-Velasco, MDJayricDepalobos100% (1)
- ABDULMANAFBINMAHMUD - 2020514971 - PI005U11CASE NOTE (Amar Sufian Bin Sulaiman V PP)Document6 paginiABDULMANAFBINMAHMUD - 2020514971 - PI005U11CASE NOTE (Amar Sufian Bin Sulaiman V PP)Manaf Mahmud0% (1)
- Aisha (Ra)Document2 paginiAisha (Ra)Arif Mohammed100% (2)
- Anna BoleynDocument22 paginiAnna BoleynDianaÎncă nu există evaluări
- L300 WHN853 Deed of SaleDocument1 paginăL300 WHN853 Deed of Salelip100% (1)
- CH 17 OutlineDocument3 paginiCH 17 Outlineapi-366289413Încă nu există evaluări
- Cui V CuiDocument3 paginiCui V CuiLawdemhar CabatosÎncă nu există evaluări
- Superior Court of California County of Santa Clara Civil DivisionDocument30 paginiSuperior Court of California County of Santa Clara Civil DivisionMitchÎncă nu există evaluări
- 109-Pepsi-Cola Bottling Co. vs. NLRC 210 Scra 277Document8 pagini109-Pepsi-Cola Bottling Co. vs. NLRC 210 Scra 277wewÎncă nu există evaluări
- Saint Rose of LimaDocument10 paginiSaint Rose of Limaapi-346281719Încă nu există evaluări
- ĐỀ THI ANH CHUYÊN KHXH NHÂN VĂN - 2022Document11 paginiĐỀ THI ANH CHUYÊN KHXH NHÂN VĂN - 2022Tú BíÎncă nu există evaluări
- Challenges Solutions How It Will Help The People in Darfur: With Local Integration Gives Refugees With FullDocument3 paginiChallenges Solutions How It Will Help The People in Darfur: With Local Integration Gives Refugees With FullMarcos DmitriÎncă nu există evaluări
- Flanker 2 - Manual - PCDocument131 paginiFlanker 2 - Manual - PCЕвгений ПшеничныйÎncă nu există evaluări
- Delegate Lefranc Fortuno - Report September 2021Document16 paginiDelegate Lefranc Fortuno - Report September 2021Delegate Lefranc Fortuno60% (5)
- Holy Child Catholic School v. Sto. Tomas TemplateDocument5 paginiHoly Child Catholic School v. Sto. Tomas TemplatekathrynmaydevezaÎncă nu există evaluări
- Pastor's Meeting With Sam LangfordDocument7 paginiPastor's Meeting With Sam LangfordthatdoodÎncă nu există evaluări
- Distinction / Difference Between Criminal Misappropriation and Criminal Breach of TrustDocument2 paginiDistinction / Difference Between Criminal Misappropriation and Criminal Breach of TrustShangavi SÎncă nu există evaluări
- Catalog 2012 RossiDocument19 paginiCatalog 2012 Rossitublin601Încă nu există evaluări
- First Information ReportDocument4 paginiFirst Information ReportYedavelli BadrinathÎncă nu există evaluări
- Colorado's First Year of Extreme Risk Protection OrdersDocument7 paginiColorado's First Year of Extreme Risk Protection OrdersMichael_Roberts2019Încă nu există evaluări
- REPUBLIC FLOUR MILLS INC Vs Commissioner of Customs TarrayoDocument1 paginăREPUBLIC FLOUR MILLS INC Vs Commissioner of Customs TarrayoMae Clare D. BendoÎncă nu există evaluări
- Constitutional Law NotesDocument38 paginiConstitutional Law NotesMarius Damian100% (1)
- Equity and Trust en AnglaisDocument24 paginiEquity and Trust en AnglaisyveshansassambaÎncă nu există evaluări
- Jeffry Dahmer: Into The Mind of A Serial Killer A Case StudyDocument18 paginiJeffry Dahmer: Into The Mind of A Serial Killer A Case StudyBen Lerner100% (1)
- Voa AuthorsDocument126 paginiVoa AuthorsMatt WilliamsÎncă nu există evaluări
- Cheatham ResumeDocument1 paginăCheatham Resumeapi-275022283Încă nu există evaluări