Documente Academic
Documente Profesional
Documente Cultură
The UK Prospective Diabetes Study (UKPDS) : Clinical and Therapeutic Implications For Type 2 Diabetes
Încărcat de
Laila KurniaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
The UK Prospective Diabetes Study (UKPDS) : Clinical and Therapeutic Implications For Type 2 Diabetes
Încărcat de
Laila KurniaDrepturi de autor:
Formate disponibile
The UK Prospective Diabetes Study (UKPDS): clinical and therapeutic
implications for type 2 diabetes
Paromita King,1 Ian Peacock1 & Richard Donnelly1,2
1
Jenny ONeill Diabetes Centre, Derbyshire Royal Infirmary, Derby and Division of Vascular Medicine, School of Medical and Surgical Sciences,
University of Nottingham, UK
Keywords: antihypertensives, diabetic complications, glycaemic control, oral hypoglycaemic agents, type 2 diabetes, UKPDS
The burden of type 2 diabetes
Diabetes was first recognized 3500 years ago by the
Ancient Egyptians. One of the first clinical descriptions
was by Aretaeus, who practised in Cappadocia around
120 AD. He wrote that the condition was fortunately
rare, but short will be the life of the man in whom the
disease is fully developed [1].
In modern society, the first statement is far from true.
The incidence of diabetes has doubled every 20 years
since 1945 [2]. In 1994 the world wide prevalence of
type 2 (non-insulin dependent) diabetes was 99 million
(1.8% of the population); by 2010 it is estimated that this
figure will rise to 215 million (3.8%) [3].
The second statement is as true today as it was almost
2000 years ago. In the West, 44% of patients with type 2
diabetes die within 10 years of diagnosis [4], mostly from
macrovascular disease; the incidence of and mortality
from cardiovascular disease are 23 times greater than in
the general population [5]. As the majority of patients
develop complications, which are present in up to 50%
even at the time of diagnosis [6], type 2 diabetes imposes
a significant burden on health services, as well as on the
individuals who suffer from this progressive and incurable
disease. Currently the 2% of the UK population with
diabetes consume 5% of the health service budget; by
comparison the 12% with arthritis consume just 1.9% [7].
With the increasing prevalence of the condition, these
figures will escalate. Prevention would be the ideal
solution, but is currently a remote prospect. In the
meantime any way of significantly reducing the burden
of diabetes-related complications will have a major impact
on patient well-being and on cost effectiveness of
management.
incidence of vascular complications. On the contrary,
the pioneering study of the 1960s, the University Group
Diabetes Program (UGDP) [8], suggested that treatment
with tolbutamide might be harmful. The study was
designed to assess the impact of blood glucose lowering
therapies on complications, with patients being randomly
allocated to placebo, tolbutamide, phenformin, or insulin.
The study was stopped after 8 years because of an increase
in cardiovascular deaths in those receiving tolbutamide.
However, for many years the design and conduct of the
UGDP were subject to fierce debate which was never
satisfactorily resolved; uncertainty continued about treatment and glycaemic targets for type 2 diabetes.
The Diabetes Control and Complications Trial
(DCCT), published in 1993 [9], showed that intensive
glycaemic control (i.e. keeping blood glucose as near to
normal as possible) reduces the incidence and progression
of microvascular complications (retinopathy, nephropathy
and neuropathy) in type 1 diabetes. Whether the same
holds true in type 2 diabetes remained uncertain. Intensive
treatment often results in hyperinsulinaemia, with weight
gain and an increase in hypoglycaemia [9], both of which
have theoretical adverse effects on macrovascular disease,
the major life threatening complication of type 2 diabetes.
Patients with type 2 diabetes frequently have other risk
factors for macrovascular disease, such as hypertension
and hyperlipidaemia, the former having a prevalence of
40%-60% [10, 11]. Antihypertensive therapy reduces the
risk of both cardiovascular and cerebrovascular disease in
the general population [12], but to what extent these
findings apply to type 2 diabetes was again not clear.
The United Kingdom Prospective Diabetes Study
(UKPDS) was conceived to explore these uncertainties
and provide clearer guidelines for the management of
type 2 diabetes.
The benefits of treatment?
Until the early 1990s, there was no evidence that our
management of diabetes had any beneficial impact on the
Correspondence: Dr I. Peacock, Derbyshire Royal Infirmary, London Road,
Derby, DE1 2QY, UK.
Received 15 March 1999, accepted 24 August 1999.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
Design of the UKPDS (Figures 13)
The UKPDS was set up in the late 1970s, by Dr Robert
Turner and colleagues in Oxford. Over 7600 subjects at
23 centres across the UK were considered for inclusion;
5102 took part. It was the largest and longest study ever
643
P. King et al.
does improved blood glucose control reduce
the incidence of complications?
do different treatments have specific advantages
or disadvantages?
Figure 1 UKPDSthe principal questions.
Hypertension in Diabetes Study
does tight control of blood pressure have an impact
on complications?
do atenolol or captopril have specific advantages
or disadvantages?
glycaemic control using combination treatment
(Glucose study 2)
acarbose
quality of life
cost-effectiveness
many incidental scientific, epidemiological and
clinical studies
Figure 2 UKPDSembedded studies.
undertaken in diabetes; median follow-up was 10 years.
As well as attempting to resolve unanswered clinical
issues, the study generated a huge epidemiological
database, comprising over 20 million data items.
The primary aim was to determine the effect of
intensive glycaemic control on the incidence of complications; the secondary aim was to assess whether there
were differences between treatments (Figure 1). Protocol
amendments were made to add topics not originally
included. These strengthened the study by broadening its
scope, but at the cost of complicating the treatment
allocation, conduct and analysis of the study. Numerous
substudies were embedded (Figure 2), the most notable
being the Hypertension in Diabetes Study. Over 30
papers have been published from the UKPDS database,
and many more are in preparation or planned.
Key points (Figure 4)
Glucose control studies [13, 14]
Subjects were randomized to receive conventional or
intensive therapy. In the former, the intention was to
keep patients aymptomatic, with a fasting plasma glucose
1
less than 15 mmol l ; in the latter, the target fasting
1
glucose was 6 mmol l . When diet failed to achieve
these targets, subjects were randomized to sulphonylureas,
insulin or metformin, the latter in obese patients only.
When single treatments failed, combinations were used.
The results were primarily expressed in terms of
aggregate end points: any diabetes related end point,
644
which included both microvascular and macrovascular
events, and diabetes related death. Twenty-one single
end points were also defined. The emphasis on aggregate
end-points allowed the study outcomes to be presented
in a clinically meaningful way, i.e. overall risk. Their use
also reduced the number of treatment comparisons, thus
minimizing the chances of false-positive results, but had
the disadvantage of concealing the magnitude of effects
on individual end points.
Intensive glucose control significantly reduced any
diabetes-related end point, but had no effect on mortality.
The predominant effect of tighter control was a reduction
of microvascular disease by a quarter, largely due to a
reduction in laser photocoagulation. There was also a
trend, just short of statistical significance, towards a
reduction in macrovascular disease. No threshold was
seen, i.e. any improvement in glycaemic control is
beneficial. These findings are similar to those of the
DCCT and a more recent study in Japanese patients with
type 2 diabetes, in whom 6 years intensive therapy with
insulin reduced the incidence of microvascular complications [15]. That the reduced occurrence of myocardial
infarction was not significant may be due to type 2
statistical error. The study was set up to detect a 15%
difference in events over the 10 years study period, and
a larger number of macrovascular than microvascular
events occurred, but the separation of HbA1c between
intensive and conventionally treated groups was disappointingly low: 0.9% (half that in the DCCT). Had
the separation of HbA1c between groups been greater, a
significant effect of intensive control on macrovascular
disease might have been demonstrated.
The secondary aim of the study was to compare the
effects of different treatments for diabetes, since some have
theoretical advantages and disadvantages. For example,
sulphonylureas close myocardial ATP-sensitive potassium
channels, which could impair ischaemia induced vasodilatation [16], perhaps explaining the results of the UGDP. In
addition, some studies have suggested that hyperinsulinaemic states are atherogenic [17], and the increased incidence
of hypoglycaemia with intensive control with insulin could
theoretically precipitate a cerebrovascular or cardiovascular
event. The UKPDS showed no difference in outcome
between treatments, which is at first sight reassuring, but
the study was powered to assess the effects of intensive
therapy in general and it is unclear whether there is adequate
power in this subgroup analysis. In addition, actual therapy
often differed from allocated treatment, especially as patients
required additional treatment over time. The results of this
aspect of the study should therefore be interpreted with
caution.
The results of metformin treatment are the most
controversial [14]. Metformin use was associated with
fewer aggregate end-points (including overall mortality)
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
Therapeutic implications of the UKPDS
Newly diagnosed diabetes
Fasting plasma glucose >6mmoll1
Prudent diet
for 34 months
>6mmoll1
6mmoll
Diet satisfactory
>6 and 15mmoll1
>15mmoll1
Primary diet failure
randomization
Main randomization
if becomes
>6mmoll1
Conventional policy
target <15mmoll1
Diet only
Intensive policy
target <6mmoll1
Sulphonylurea
Insulin
Metformin
(obese patients only)
Figure 3 Design of UKPDS.
intensive glucose control, using existing treatments,
improved microvascular morbidity, but not mortality
insulin and sulphonylureas were similarly effective
metformin was advantageous in the obese
intensive blood pressure control was more
beneficial, improving morbidity (both micro- and
macrovascular), and mortality
ideal targets: HbAlc < 7%, BP < 140/80 mmHg
any reduction was beneficial
An unexpected finding was that the addition of metformin to sulphonylureas (in both obese and nonobese
patients) was associated with increased mortality. The
numbers involved in this subgroup analysis were very small,
with few deaths (26 vs 14 in the group treated with
sulphonylureas alone) and no difference in the incidence of
heart attacks or strokes between the groups, only in the
proportion who died. Furthermore, the mortality in the
group treated by sulphonylureas alone was unexpectedly
low. The authors therefore concluded that this anomalous
result was likely to be have been due to chance.
Figure 4 Key points.
Hypertension in Diabetes Study [18, 19]
in obese patients. However the number of patients
allocated to metformin was less than 10% of all those
randomised. The findings could also be interpreted as
indicating that insulin and sulphonylureas are equally
harmful in the obese, possibly as a consequence of
hyperinsulinaemia.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
One thousand one hundred and forty-eight patients took
part. Half the participants were allocated to tight control
(target blood pressure less than 150/85 mm Hg ) and
were randomised to either atenolol or captopril, with
other agents added as necessary. The remainder were
allocated to less tight control (target blood pressure less
645
P. King et al.
than 180/105 mm Hg); in these patients, drugs other
than b-adrenoceptor blockers and ACE inhibitors were
used. Mean blood pressure was 144/82 mm Hg in the
tight control group, compared with 154/87 mm Hg in
the less tight control group. One-third of patients
allocated to tight control required three more drugs in
the attempt to achieve the target blood pressure.
Tight control of blood pressure reduced both diabetesrelated morbidity and mortality. Unlike glycaemic control,
there was a significant effect on macrovascular as well as
microvascular complications, with strokes and heart failure
reduced by a half. Myocardial infarction was reduced by
a fifth, but this was not statistically significant. As in the
glucose control study, no threshold for risk was seen in
the hypertension study. These are very impressive results,
establishing that blood pressure control is at least as
important as glycaemic control, if not more so, in the
prevention of complications in type 2 diabetes.
In the last 2 years, the results of several other studies
of hypertension which have included patients with
diabetes have been published. These also demonstrated a
reduction in macrovascular risk, including myocardial
infarction [20, 21]. A variety of agents was used, but
blood pressure differences between treatment and control
groups were comparable with the UKPDS, and protective
effects were observed despite shorter periods of follow
up (25 years). Thus there is no doubt of the significance
of blood pressure control in type 2 diabetes, but there
remains the question whether particular drugs have
advantages or disadvantages.
The UKPDS compared captopril and atenolol, both
drugs having theoretical benefits. In the general population with hypertension, b-adrenoceptor blockers reduce
macrovascular events and are specifically cardioprotective,
reducing sudden death and further myocardial events in
those with prior myocardial infarction[22]. ACE inhibitors
improve survival in patients with heart failure [23, 24];
in type 1 diabetes, they reduce the progression of
nephropathy [25, 26] and possibly retinopathy [27], but
whether ACE inhibitors have specific advantages over
other antihypertensive agents in type 2 diabetes is not yet
agreed. Recently the ABCD trial showed a reduction in
myocardial infarction in diabetic hypertensive subjects
treated with an ACE inhibitor compared with a calcium
channel blocker [28], but it was not clear whether the
ACE inhibitor was especially beneficial or the calcium
channel blocker relatively harmful, particularly as the
groups were inadequately matched for concomitant
medication. The UKPDS found that captopril and
atenolol were equally effective as antihypertensive agents,
in preventing macrovascular complications and in reducing the progression of retinopathy and albuminuria. The
ACE inhibitor was however, better tolerated. These
results are again reassuring at first sight, but, as with the
646
glucose control study, type 2 errors cannot be excluded;
there was a trend in favour of the atenolol treated group.
Therapeutic implications, study limitations and
outstanding questions (Figures 57)
The UKPDS demonstrated that any improvement in
glycaemic control and blood pressure reduces diabetesrelated complications. In trials such as this, patients are
selected both by investigators and by themselves. The
observation that UKPDS patients had a lower mortality
than the general population with type 2 diabetes may be
a reflection of this. What was achievable and acceptable
to a trial population cannot be necessarily translated to
everyone with type 2 diabetes. This must be remembered
when applying the results of the study to clinical practice.
There is no doubt that aggressive management of
blood pressure is important, particularly in reducing
macrovascular disease, the main cause of morbidity and
mortality in these patients. A target blood pressure of less
than 140/80 is suggested by the authors. The fact that
benefits are achieved within 2 or 3 years means that all
patients should be treated irrespective of age. Clearly,
achieving this goal will require aggressive follow up
( patients in the UKPDS were seen 3 monthly), and this
may not be acceptable to all patients. With one third
requiring 3 or more agents to maintain target blood
pressures, compliance will certainly be a problem in some.
Whether intensive glycaemic control should be routinely introduced in type 2 diabetes is more controversial.
limited separation between conventional and intensive glucose groups (patient compliance?)
insufficient statistical power for subgroup analyses
Figure 5 Limitations of the study.
how worthwhile are the benefits achieved?
can targets be achieved in routine practice?
benefit of increasing insulin dose?
benefit of insulin/tablet combinations
place of aspirin, statins, anti-oxidants, etc.
Figure 6 Outstanding questions.
treatment with several drugs will often be necessary
increased resources will be needed to realize
benefits of better control
treatment is cost effective, when benefits are
taken into account
screening programmes should be considered
Figure 7 Therapeutic implications.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
Therapeutic implications of the UKPDS
Despite achieving statistical significance, the absolute risk
reduction from intensive glycaemic control is small, with
a reduction of 5 events over 10 years compared with 16
for blood pressure (Table 1). Furthermore, the benefits of
glucose reduction did not accrue for several years, unlike
intensive blood pressure control. Intensive glycaemic
control, particularly with insulin, also leads to morbidity
from hypoglycaemia and weight gain. Thus, unlike blood
pressure control, intensive glycaemic control is not
suitable for all patients, particularly the elderly, or those
with existing severe complications. The small absolute
risk reduction also needs to be compared with the
possible effects of other risk factor interventions, e.g.
treatment with aspirin, lipid lowering drugs or antioxidants. Despite these limitations, the UKPDS provides
evidence and quantitative guidelines for those in whom
intensive control is achievable.
The study also assessed effects of intensive treatment
on quality of life; no adverse effect was apparent. One
scale demonstrated that poor quality of life is related to
complications rather than the treatments given [unpublished]. This is reassuring in implementing the results of
the study, though the results may not apply equally to an
unselected population.
One aspect of management inadequately addressed by
the study is the optimal combination of drugs to be used
either for glucose or blood pressure control. Different
agents seemed equally effective, but the possibility of
type 2 errors in these subgroup analyses cannot be
excluded, as already discussed. To date, the effectiveness
of insulin and oral hypoglycaemic agent combinations is
not known, although there are unpublished data from
the study on the combination of insulin and sulphonylureas. Data on possible dose-dependent effects of
insulin, and the combination of insulin and metformin
are lacking. For now, until further information is available,
clinical practice should be based on achieving glucose
and blood pressure reduction by whatever means best
suits an individual patient.
In the study, patients were reviewed 3 monthly, rather
than 612 monthly as in routine clinical practice, which
has considerable resource implications. The reduction in
blood pressure [29] and glucose [unpublished] achieved
were relatively cheap, 48 and 22 per patient per year,
Table 1 Absolute risk.
Number of events
Intensive
Conventional
Glucose control
Blood pressure
control
41
51
46
67
*NNT
20 (95% CI 10500)
6 (310)
*number needed to treat for 10 years to prevent 1 event.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
respectively, when the benefits were discounted. These
figures are valuable ammunition in the battle to improve
services for patients. With 50% of patients presenting
with complications, the issue of screening should also be
addressed.
The UKPDS provides management guidelines for
selected patients, but leaves many questions unanswered.
The advantages of good care have been more clearly
defined than ever before, but the huge gulf between the
benefits achieved in the study and the many frustrations
of everyday practice remains. In most centres, there are
large numbers of patients with poor control of both
blood glucose and blood pressure. Type 2 diabetes must
at least be taken more seriously.
References
1 Reed JA. Aretaeus, the Cappadocian. Diabetes 1954; 3:
419421.
2 Barnett T. Epidemiology, complications and costs of diabetes
mellitus. In The insulin treatment of diabetes: a practical guide,
ed. Tony Barnett, London, E-map healthcare: 69, 1998.
3 McCarty D, Zimnet P. Diabetes 19942010: global
estimates and projections. Leverkusen, Bayer.: 146,
1994.
4 Panzam G. Mortality and survival in type II (non-insulin
dependent) diabetes mellitus. Diabetologia 1987; 30:
123131.
5 Garcia MJ, McNamara PM, Gordon T, Kannell WB.
Morbidity and mortality in diabetics in the Framingham
population. Sixteen year follow-up study. Diabetes 1974; 23:
105111.
6 UK Prospective Diabetes Study (UKPDS) Group. UK
prospective diabetes study VIII. study design, progress and
performance. Diabetologia 1991; 34: 877890.
7 Leese B. Economic evaluations of Type II diabetes. In The
social and cost implications of Type II diabetes, ed Bengt
Jonsson H, Krans MJ, PharmacoEconomics 8(Suppl, 1995; 1):
2327.
8 University Group Diabetes Programme. A study on the
effects of hypoglycaemic agents on vascular complications in
patients with adult-onset diabetes. Diabetes 1976; 25:
11291153.
9 The Diabetes Control and Complications Trial Research
Group. The effect of intensive treatment of diabetes on the
development and progression of long-term complications in
insulin-dependent diabetes mellitus. N Engl J Med 1993; 329:
977986.
10 Hypertension in Diabetes Study Group HDS. 1. Prevalence
of hypertension in newly presenting type 2 diabetic patients
and the association with risk factors for cardio-vascular and
diabetic complications. J Hypertens 1993; 11: 309317.
11 Prescott-Clarke P, Primatesa P. Health Survey for England
1995 London HMSO, 1997.
12 Collins R, Macmahon S. Blood pressure, antihypertensive
drug treatment and the risks of stroke and coronary heart
disease. Br Med J 1994; 50: 272298.
13 UK Prospective Diabetes Study (UKPDS) Group. Intensive
blood-glucose control with sulphonylureas or insulin
647
P. King et al.
14
15
16
17
18
19
20
21
648
compared with conventional treatment and risk of
complications in patients with type 2 diabetes (UKPDS 33).
Lancet 1998; 352: 837853.
UK Prospective Diabetes Study (UKPDS) Group. Effect of
intensive blood-glucose control with metformin on
complications in overweight patients with type 2 diabetes
(UKPDS 34). Lancet 1998; 352: 854865.
Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin
therapy prevents the progression of diabetic microvascular
complications in Japanese patients with non-insulin
dependent diabetes mellitus: a randomised prospective 6-year
study. Diabet Res Clin Pract 1995; 28: 103117.
Ashford ML, Bond CT, Blair TA, Adelman JP. Cloning and
functional expression of a rat heart K-ATP channel. Nature
1994; 370: 456459.
Stout RW. Insulin and atherosclerosis. In Diabetes and
Atherosclerosis, ed Stout RW, Dordrecht, The Netherlands.
Kluwer Academic publishers., 1992: 165201.
UK Prospective Diabetes Study Group. Tight blood pressure
control and risk of macrovascular and microvascular
complications in type 2 diabetes: UKPDS 38. Br Med J
1998; 317: 703713.
UK Prospective Diabetes Study Group. Efficacy of atenolol
and captopril in reducing risk of macrovascular and
microvasvular complications in type 2 diabetes: UKPDS 39.
Br Med J 1998; 317: 713720.
Curb JD, Pressel SL, Cutler JA, et al. Effect of diuretic-based
antihypertensive treatment on cardiovascular disease risk in
older diabetic patients with isolated systolic hypertension.
Systolic hypertension in the Elderly Program Cooperative
Resaerch Group. JAMA 1996; 276: 18861892.
Hansson L, Zanchetti A, Carruthers SG, et al. for the HOT
Study Group. Effects of intensive blood-pressure lowering
and low-dose aspirin in patients with hypertension: principal
results of the Hypertension Optimal Treatment (HOT)
randomised trial. Lancet 1998; 351: 17551762.
22
23
24
25
26
27
28
29
Yusef S, Peto R, Lewis J, Collins R, Sleight P. Betablockade during and after myocardial infarction; an overview
of the randomised trials. Progr Cardiovascular Dis 1997; 30:
335371.
CONSENSUS Trial Study Group. Effects of enalapril on
mortality in severe congestive heart failure. New Eng J Med
1987; 316: 14291435.
SOLVD Investigators. Effect of enalapril on mortality and
the development of heart failure in asymptomatic patients
with reduced left ventricular ejection fractions. New Eng
J Med 1992; 327: 685691.
Bjorck S, Mulec H, Johnsen SA, Norden G, Aurell M.
Renal protective effects in diabetic nephropathy. Br Med J
1992; 304: 339343.
Lewis EJ, Hunsicker LG, Bain RP, Rhode RD. for the
Colloborative Study Group. The effect of angiotensinconverting enzyme inhibition on diabetic nephropathy. New
Engl J Med 1993; 329: 14561462.
Chaturvedi N, Sjolie AK, Stevenson JM, et al. Effect of
lisinopril on progression of retinopathy in normotensive
people with type 1 diabetes. The EUCLID Study Group.
EURODIAB Controlled Trial of Lisinopril in InsulinDependent Diabetes Mellitus. Lancet 1998; 351: 2831.
Estacio RO, Schrier RW. Antihypertensive therapy in
type 2 diabetes: implications of the Appropriate Blood
pressure Control in Diabetes (ABCD) trial. Am J Cardiol
1998; 82: 9R14R.
UK Prospective Diabetes Study Group. Cost effectiveness
analysis of improved blood pressure control in hypertensive
patients with type 2 diabetes: UKPDS 40. Br Med J 1998;
317: 720726.
Note added in proof
We wish to pay tribute to Robert Turner whose recent
untimely death is such a tragedy.
1999 Blackwell Science Ltd Br J Clin Pharmacol, 48, 643648
S-ar putea să vă placă și
- Implications of The United Kingdom Prospective Diabetes StudyDocument5 paginiImplications of The United Kingdom Prospective Diabetes StudyAgustin MendezÎncă nu există evaluări
- Br. J. Anaesth. 2011 Nicholson 65 73Document9 paginiBr. J. Anaesth. 2011 Nicholson 65 73Adán 'OlveeraÎncă nu există evaluări
- ADA - UKPD StudyDocument5 paginiADA - UKPD StudyMagdalena MercyanaÎncă nu există evaluări
- Diabetologia: UK Prospective Diabetes Study (UKPDS)Document14 paginiDiabetologia: UK Prospective Diabetes Study (UKPDS)GuadalupeÎncă nu există evaluări
- Diabetes and Cardiovascular Disease: Story of DiscoveryDocument5 paginiDiabetes and Cardiovascular Disease: Story of DiscoveryMahesh DmÎncă nu există evaluări
- Ban JASH2009Document15 paginiBan JASH2009Adek FahmialdiÎncă nu există evaluări
- Hypoglycemia - The Neglected ComplicationDocument23 paginiHypoglycemia - The Neglected Complication4g5xwdvh9sÎncă nu există evaluări
- Jurnal 1Document17 paginiJurnal 1convenienceÎncă nu există evaluări
- Emerging Role of Dipeptidyl Peptidase-IV (DPP-4) Inhibitor Vildagliptin in The Management of Type 2 DiabetesDocument9 paginiEmerging Role of Dipeptidyl Peptidase-IV (DPP-4) Inhibitor Vildagliptin in The Management of Type 2 DiabetesIndrasuari Anak Agung AyuÎncă nu există evaluări
- Nutrition, Metabolism & Cardiovascular Diseases: B.A. Kappel, N. Marx, M. FedericiDocument9 paginiNutrition, Metabolism & Cardiovascular Diseases: B.A. Kappel, N. Marx, M. Federicirachel0301Încă nu există evaluări
- Review Article: Anti-Diabetic Medications: How To Make A Choice?Document10 paginiReview Article: Anti-Diabetic Medications: How To Make A Choice?Made ChandraÎncă nu există evaluări
- Perspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsDocument7 paginiPerspectives in Diabetes: Postprandial Hyperglycemia and Diabetes ComplicationsHania Asmarani RahmanitaÎncă nu există evaluări
- Impact of Cardiovascular Outcomes On The Development and Approval of Medications For The Treatment of Diabetes MellitusDocument11 paginiImpact of Cardiovascular Outcomes On The Development and Approval of Medications For The Treatment of Diabetes MellitusBayu Setyo NugrohoÎncă nu există evaluări
- Polypharmacy in The Aging Patient A Review of Glycemic Control in Older Adults With Type 2 DiabetesDocument12 paginiPolypharmacy in The Aging Patient A Review of Glycemic Control in Older Adults With Type 2 Diabetesapi-311409998Încă nu există evaluări
- Dia Care-2006-Nathan-1963-72Document10 paginiDia Care-2006-Nathan-1963-72Sorin ParalescuÎncă nu există evaluări
- Control GlicemicoDocument20 paginiControl GlicemicomiguelalmenarezÎncă nu există evaluări
- Diabetes Mellitus and Oral Health: An Interprofessional ApproachDe la EverandDiabetes Mellitus and Oral Health: An Interprofessional ApproachÎncă nu există evaluări
- A New Perspective On Metformin Therapy in Type 1 DiabetesDocument7 paginiA New Perspective On Metformin Therapy in Type 1 DiabetesdeckardmaxÎncă nu există evaluări
- Diabetes ManagementDocument13 paginiDiabetes ManagementdanielmanuÎncă nu există evaluări
- Hypoglycemia: Table 1Document8 paginiHypoglycemia: Table 1erik1585Încă nu există evaluări
- Versiones y Preserciones UKPDS BMJ 2000Document4 paginiVersiones y Preserciones UKPDS BMJ 2000Luis MorochoÎncă nu există evaluări
- Accepted Manuscript: Diabetes Research and Clinical PracticeDocument27 paginiAccepted Manuscript: Diabetes Research and Clinical PracticeHendra Dandi DaengÎncă nu există evaluări
- Gastrointestinal Surgery Can Be A "Cure" For Types 2 DiabetesDocument2 paginiGastrointestinal Surgery Can Be A "Cure" For Types 2 DiabetesJonna Mae TurquezaÎncă nu există evaluări
- ADVANCE: Action in Diabetes and Vascular Disease: Original ArticleDocument6 paginiADVANCE: Action in Diabetes and Vascular Disease: Original ArticleMade LascanoÎncă nu există evaluări
- Pharmacological Management of Type 2 Diabetes ComplicationsDocument3 paginiPharmacological Management of Type 2 Diabetes ComplicationsDarra Nilam SariÎncă nu există evaluări
- Clinical Inertia in T2DM ManagementDocument11 paginiClinical Inertia in T2DM ManagementEva GabrielÎncă nu există evaluări
- 1996 Diabetes and Hypertension: ADS Position StatementsDocument14 pagini1996 Diabetes and Hypertension: ADS Position StatementsRahmad Budi PrasetyoÎncă nu există evaluări
- My Nature CureDocument16 paginiMy Nature Curehemraj.koiralaÎncă nu există evaluări
- Diabetes Emergencia Umpierrez 2016Document11 paginiDiabetes Emergencia Umpierrez 2016Nathalie GandoÎncă nu există evaluări
- Hypoglycaemia Documented With Real-Time Continuous Glucose Sensing in A Case of Dead in Bed' SyndromeDocument106 paginiHypoglycaemia Documented With Real-Time Continuous Glucose Sensing in A Case of Dead in Bed' Syndromemimran1974Încă nu există evaluări
- Hypoglycemia, Diabetes, and Cardiovascular Events: C V. D, G B. B, V FDocument6 paginiHypoglycemia, Diabetes, and Cardiovascular Events: C V. D, G B. B, V FHervi LaksariÎncă nu există evaluări
- Management of Diabetes Mellitus in Patients With Chronic Kidney DiseaseDocument9 paginiManagement of Diabetes Mellitus in Patients With Chronic Kidney DiseasezakyÎncă nu există evaluări
- Canadian: Hypoglycemia: Understanding The EnemyDocument8 paginiCanadian: Hypoglycemia: Understanding The EnemyndistantiÎncă nu există evaluări
- Adua Et Al-2017-Clinical and Translational MedicineDocument11 paginiAdua Et Al-2017-Clinical and Translational MedicineSam Asamoah SakyiÎncă nu există evaluări
- Editorial: Preventing Diabetic Retinopathy ProgressionDocument3 paginiEditorial: Preventing Diabetic Retinopathy ProgressionRashellya RasyidaÎncă nu există evaluări
- UKPDSDocument39 paginiUKPDSIsaac TellezÎncă nu există evaluări
- tmpFF74 TMPDocument2 paginitmpFF74 TMPFrontiersÎncă nu există evaluări
- Hypoglycemia: The Neglected Complication: Review ArticleDocument16 paginiHypoglycemia: The Neglected Complication: Review Articlesiti nur aishah jalilÎncă nu există evaluări
- Diabetes 5Document16 paginiDiabetes 5patricia osei-owusuÎncă nu există evaluări
- CT2 316 CruzPaolaDocument2 paginiCT2 316 CruzPaolaPaola CruzÎncă nu există evaluări
- 1 AnDocument9 pagini1 AnDana GrigorescuÎncă nu există evaluări
- Discover The Best Exercises For Overall Health & Longevity - Based On The Teachings Of Dr. Andrew Huberman: The Ultimate Workout Guide For Lifelong Well-BeingDe la EverandDiscover The Best Exercises For Overall Health & Longevity - Based On The Teachings Of Dr. Andrew Huberman: The Ultimate Workout Guide For Lifelong Well-BeingÎncă nu există evaluări
- Management of Diabetic Ketoacidosis in Adults - A Narrative ReviewDocument12 paginiManagement of Diabetic Ketoacidosis in Adults - A Narrative Reviewghr9cjy5npÎncă nu există evaluări
- Diabetic Retinopathy - Endotext - NCBI BookshelfDocument24 paginiDiabetic Retinopathy - Endotext - NCBI BookshelfANDREW OMAKAÎncă nu există evaluări
- PP Lancet 1998 Ukpds33Document17 paginiPP Lancet 1998 Ukpds33HelloÎncă nu există evaluări
- DCC White PaperDocument7 paginiDCC White PaperSteveEpsteinÎncă nu există evaluări
- Clinician Guide Inpx LCD For Remission T2DM Toward STD Care Protocol Diabetes Manag 2019 9-Cucuzzella Hite Patterson EtalDocument28 paginiClinician Guide Inpx LCD For Remission T2DM Toward STD Care Protocol Diabetes Manag 2019 9-Cucuzzella Hite Patterson Etaldonmd98Încă nu există evaluări
- Metabolic Syndrome As A Predictor of Type 2 Diabetes, and Its Clinical Interpretations and UsefulnessDocument10 paginiMetabolic Syndrome As A Predictor of Type 2 Diabetes, and Its Clinical Interpretations and UsefulnessChiranjeeviÎncă nu există evaluări
- Legacy Effect in Diabetes MnanagementDocument9 paginiLegacy Effect in Diabetes MnanagementSouradipta GangulyÎncă nu există evaluări
- DM and CHFDocument7 paginiDM and CHFCecilia Casandra UneputtyÎncă nu există evaluări
- Yùquán WānDocument14 paginiYùquán Wānmiguelzhuangzi09Încă nu există evaluări
- Metformina y Estrés Oxidativo en Pacientes DiabéticosDocument14 paginiMetformina y Estrés Oxidativo en Pacientes DiabéticosJesus D. Hernandez GuitianÎncă nu există evaluări
- 349 FullDocument3 pagini349 FullsenkonenÎncă nu există evaluări
- 1 Andoni Prevalența Bolii Cardiovasculare Ro-EnDocument1 pagină1 Andoni Prevalența Bolii Cardiovasculare Ro-EnCristian CarpÎncă nu există evaluări
- Article 1Document12 paginiArticle 1jessisxpÎncă nu există evaluări
- The Pathological Effects of Hyperglycaemia On The Cardiovascular (CV) System and BrainDocument5 paginiThe Pathological Effects of Hyperglycaemia On The Cardiovascular (CV) System and BrainRyzka Izza MayFanyÎncă nu există evaluări
- Imune DeseaseDocument6 paginiImune DeseaseGeorge NicoloiuÎncă nu există evaluări
- DerosaDocument13 paginiDerosaAmeliana KamaludinÎncă nu există evaluări
- Use Only: Diabetes and ThalassaemiaDocument5 paginiUse Only: Diabetes and ThalassaemiadesilasarybasriÎncă nu există evaluări
- Jurnal 3Document8 paginiJurnal 3Laila KurniaÎncă nu există evaluări
- Dianosis Dan Resusitasi Pada Pasien Syok Perdarahan & Syok DehidrasiDocument31 paginiDianosis Dan Resusitasi Pada Pasien Syok Perdarahan & Syok DehidrasiLaila KurniaÎncă nu există evaluări
- Cur 0009 0062Document5 paginiCur 0009 0062Laila KurniaÎncă nu există evaluări
- Urinary Retention: Catheter Drainage Bag or Catheter Valve?: Gurnam Virdi David HendryDocument3 paginiUrinary Retention: Catheter Drainage Bag or Catheter Valve?: Gurnam Virdi David HendryLaila KurniaÎncă nu există evaluări
- Ureteroscopy Outcomes, Complications and Management of Perforations in Impacted Ureter StonesDocument5 paginiUreteroscopy Outcomes, Complications and Management of Perforations in Impacted Ureter StonesLaila KurniaÎncă nu există evaluări
- (Medline) : J Dermatopathol. 2014 Mar. 36 (3) :260-2Document3 pagini(Medline) : J Dermatopathol. 2014 Mar. 36 (3) :260-2Laila KurniaÎncă nu există evaluări
- Resume CDocument3 paginiResume Capi-409607977Încă nu există evaluări
- Garcinia Cambogia MonographDocument5 paginiGarcinia Cambogia Monographeddee90Încă nu există evaluări
- VaccinationDocument22 paginiVaccinationFareed KhanÎncă nu există evaluări
- Prescription of Exercise For Health and FitnessDocument27 paginiPrescription of Exercise For Health and FitnessedelinÎncă nu există evaluări
- Course Syllabus For Leadership and Management in Physical Therapy LMP 301Document4 paginiCourse Syllabus For Leadership and Management in Physical Therapy LMP 301beaÎncă nu există evaluări
- The Lateral Trochanteric Wall Gotfried 2004 PDFDocument5 paginiThe Lateral Trochanteric Wall Gotfried 2004 PDFluis perezÎncă nu există evaluări
- Mass Balance CalculationDocument16 paginiMass Balance Calculationmirdza94100% (3)
- A HOFFER Review Niacin The Real StoryDocument2 paginiA HOFFER Review Niacin The Real StoryAna Lu100% (1)
- Homoeopathy For Frost BiteDocument2 paginiHomoeopathy For Frost BiteDr Dushyant Kamal DhariÎncă nu există evaluări
- Ebook CoreDocument38 paginiEbook CoreDiana GoldÎncă nu există evaluări
- Jarvis 2012 Practical UroflowmetryDocument2 paginiJarvis 2012 Practical UroflowmetryFoxglove83Încă nu există evaluări
- Prostate GlandDocument54 paginiProstate Glanddr_shamimrÎncă nu există evaluări
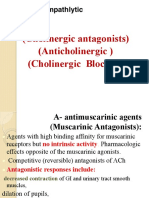
- AnticholinergicsDocument34 paginiAnticholinergicskityamuwesiÎncă nu există evaluări
- Diaphyseal Fractures in Children Final - 2Document62 paginiDiaphyseal Fractures in Children Final - 2Arlina Wiyata GamaÎncă nu există evaluări
- Part B-13-Night Shift SleepDocument4 paginiPart B-13-Night Shift Sleepfernanda1rondelliÎncă nu există evaluări
- OM Extended Aeration PDFDocument25 paginiOM Extended Aeration PDFHendra SusantoÎncă nu există evaluări
- Psychiatric Mental Health Nursing 2nd EditionDocument550 paginiPsychiatric Mental Health Nursing 2nd Editiondaria100% (7)
- Nasal Surgery For Sleep-Disordered BreathingDocument6 paginiNasal Surgery For Sleep-Disordered Breathinglaljadeff12Încă nu există evaluări
- Documentation Techniques PDFDocument24 paginiDocumentation Techniques PDFPooja varmaÎncă nu există evaluări
- Marijuana and Treatment of Drug Addiction in The Philippines - Nathaniel Dela CruzDocument38 paginiMarijuana and Treatment of Drug Addiction in The Philippines - Nathaniel Dela CruzJek RicoÎncă nu există evaluări
- UK Info & LabelDocument28 paginiUK Info & LabelJenn LamÎncă nu există evaluări
- Imaging Infections Jain 2017Document263 paginiImaging Infections Jain 2017johnalan100% (2)
- Reiki Ryoho: Questions & AnswersDocument49 paginiReiki Ryoho: Questions & AnswersJames Deacon100% (2)
- Montano NCP TbiDocument6 paginiMontano NCP TbiKarl Angelo MontanoÎncă nu există evaluări
- Conversation Questions - Drugs and Medicine Nov25thDocument2 paginiConversation Questions - Drugs and Medicine Nov25thDiego Peinador PascuaÎncă nu există evaluări
- Introduction Cysts of JawsDocument62 paginiIntroduction Cysts of JawsEnass Alhadi50% (2)
- Macro Teaching - Care of Baby in VentilatorDocument13 paginiMacro Teaching - Care of Baby in VentilatorSheena SharmaÎncă nu există evaluări
- Solian SMPCDocument20 paginiSolian SMPCyanal.bisharat.mspharmaÎncă nu există evaluări
- Pulse OximetryDocument16 paginiPulse OximetryDineshkumarÎncă nu există evaluări
- Learning Plan Tle 9 Nail Care NewDocument9 paginiLearning Plan Tle 9 Nail Care NewJoselito CepadaÎncă nu există evaluări