Documente Academic
Documente Profesional
Documente Cultură
Shock Notes3
Încărcat de
VanessaMUellerDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Shock Notes3
Încărcat de
VanessaMUellerDrepturi de autor:
Formate disponibile
Shock
Study online at quizlet.com/_1b5yot
1.
4 ways to arrive at cellular hypoxia
(shock)
hypovolemia, cardiac dysfunction, vascular failure,
or obstructive processes that impair cardiac filling.
2.
big overview of shock (key point, Dx,
etc)
A state of organ hypoperfusion with resultant cellular dysfunction and
death.
Mechanisms may involve decreased circulating volume, decreased cardiac
output, and vasodilation, sometimes with shunting of blood to bypass
capillary exchange beds.
Symptoms include altered mental status, tachycardia, hypotension, and
oliguria.
Diagnosis is clinical, including BP measurement and sometimes markers
of tissue hypoperfusion (eg, blood lactate, base deficit).
Treatment is with fluid resuscitation, including blood products if
necessary, correction of the underlying disorder, and sometimes
vasopressors.
3.
pro tip: it's important to recognize
when shock is coming!
...
4.
Shock- Pathophysiology
Reduced perfusion -> hypoxia -> anaerobic metabolism
Lactic acidosis -> cell damage -> cell death
Inflammatory and clotting cascades triggered
cytokines, leukotrienes, tumor necrosis factor, Nitric oxide ("cytokine storm" in influenza A,
H1N1)
Vasodilation -> hypotension -> hypoperfusion
Leukocyte and platelet adhesion to endothelium
clotting system activation with fibrin deposition
Endothelial cell dysfunction -> inc microvascular permeability (causes microvascular
permiability, leads to third space, leads to hyptension)
third space, translocation of enteric bacteria (gives peritonitits)
Neutrophil apoptosis inhibited -> increases inflammatory mediators
(shock is overwhelming display of force)
PRO TIP -- so not only do we need to think about fluids, but a ton of other things.
5.
pathophysiology cont.
Compensation
inc oxygen extraction
adrenergic and sympathetic mediated
vasoconstriction and tachycardia
inc cardiac output
release of corticosteroids, renin, glucose
6.
Graphic Organizer
7.
multiple organ dysfunction
Most common in septic shock
10% of pts with severe traumatic injury
Lungs
inc membrane permeability
alveoli dysfunction and inflammation
hypoxia, acute lung injury, ARDS
Kidneys
acute tubular necrosis -> ARI
Heart
dec. contractility and compliance
dec. cardiac output
GI tract
ileus, submucosal hemorrhage, hepatocellular
necrosis, dec. production of clotting factors
8.
shock sxs
Lethargy, confusion, and somnolence are common.
Pale, cool, clammy, and often cyanosis
earlobes, nose, and nail beds.
capillary filling time is prolonged
Diaphoresis
Peripheral pulses are weak and rapid (Kuhn likes to feel radial pulse);
only femoral or carotid pulses are palpable.
Tachypnea and hyperventilation
BP low (< 90 mm Hg systolic) or unobtainable
Urine output is low.
9.
shock index (used in trauma, used
to clue us into shock)
Shock Index
hypovolemic shock
HR / SBP (HR divided by systolic BP)
0.5 - 0.7 normal
SIRS (also used) (systemic
inflammatory response syndrome)
Temperature <36C(96.8F) or >38C
(100.4F)
Heart rate >90 beats per minute
Tachypnea > 20 breaths per minute
White blood cell count <4000 cells/mm
or >12,000 cells/mm or the presence of
greater than 10% immature neutrophils
(band forms)
2 OR MORE CRITERIA PRESENT (should lead to evaluation to make sure)
10.
SIRS
Infectious and Noninfectious
Sepsis
Trauma, burns, pancreatitis, ischemia, and hemorrhage
Complications of surgery
Adrenal insufficiency
Pulmonary embolism
Complicated aortic aneurysm
Cardiac tamponade
Anaphylaxis
Drug overdose
11.
HYPOVOLEMIC SHOCK
Decrease in intravascular volume, decreased preload > reduced stroke volume.
* Hemorrhage
Increased losses body fluids
Inadequate fluid intake
12.
Signs of Successful Resuscitation
1.
2.
3.
4.
5.
6.
13.
Hypovolemic Shock- Treatment
Stop bleeding or fluid loss
Crystalloid infusion 20cc/kg IV bolus which is a good couple liters (lactated ringers...most use
normal saline except in someone hypovolemic due to renal failure?!?!)
no advantage to colloids (eg, albumin, blood is a colloid)
Reassessment
Massive transfusion protocols
PRBCs : FFP : Platelet : cryoprecipitate (I think he said that now they do a 1:1:1:1 kinda thing)
14.
CARDIOGENIC SHOCK
Reduction in Cardiac Output
primary cardiac disorder
Improved blood pressure
Improving level of consciousness
Improving peripheral perfusion
Decreasing tachycardia
Decreasing lactate
Normalizing pH
15.
Cardiogenic Shock Tx:
Cardiogenic Shock- Treatment
Tachydysrhythmias- cardioversion
Bradydysrhythmias- pacing
STEMI- revascularization
Supportive: ASA, O2, Heparin
Vasopressors (for hypovolemic shock): Norepinephrine,
Dobutamine,
Dopamine
16.
pro tip: when you see multiple organ failure....TREAT
AGGRESSIVELY
...
17.
Pro Tip: 3 most common 'pressors >>
Norepinephrine,
Dobutamine,
Dopamine
18.
Vasoactive receptors
Alpha-1 adrenergic receptors
sympathetic nerve endings on smooth muscle cells and
on myocardial cells
Alpha-2 adrenergic receptors
systemic vasculature leads to vasoconstriction and
increased systemic blood pressure
1 and 2-adrenergic receptors
both located within the myocardium
2 receptors also being located vascular and bronchial
smooth muscle.
positive ionotropic and chronotropic effects within the
myocardium
smooth muscle relaxation in the bronchial tree and
elsewhere
Dopamine receptors
smooth muscle of renal, splanchnic, coronary, and '
cerebrovascular beds
vasodilation within these vascular beds
19.
drugs affecting which receptors
(i think he said norepinephrine is the go to in ED)
20.
DISTRIBUTIVE SHOCK
Distributive Shock
Dec. intravascular volume caused by arterial
or venous vasodilation
Anaphylaxis
Endotoxin induced sepsis
Spinal cord injury
Drugs: nitrates, opioids, Viagra
21.
ANAPHYLACTIC SHOCK (remember this is on a spectrum)
Airway: angioedema and bronchospasm
EpiPen
Beta- agonist aerosol (albuterol is most common)
H1 and H2 blockers (H1...benadryl.....H2 ranitidine)
Steroids (prednisone...classic orally....dexamethasone for
kids.....sodium hydrol IV?!)
22.
NEUROGENIC SHOCK (high thoracic or cervical injury..........legs
and or arms can't move)
Loss of vascular tone from high spinal lesion
loss of feedback loop from autonomic ganglia
Warm skin, hypotension, +/- tachycardia
Fluids and vasopressors with alpha activity
23.
SEPTIC SHOCK (Key
points)
SIRS
Temperature <36C(96.8F) or >38C(100.4F)
Heart rate >90 beats per minute
Tachypnea > 20 breaths per minute
White blood cell count <4000 cells/mm or >12,000 cells/mm or the presence of greater than
10% immature neutrophils (band forms)
2 or more criteria present
SIRS + infection = sepsis
Sepsis + organ dysfunction = severe sepsis
Sepsis + cellular hypoxemia = septic shock
24.
septic shock (points)
SIRS associated with decreased SVR -> hyperdynamic compensation ->
impaired contractility from myocardial depressants and hypoxemia.
Elevated serum lactate levels (> 4) evidence of tissue hypoperfusion.
Gram-negative rods (classic....E Coli...Pseudomonas)
Fluids!!! (eg, 3 liters of fluid for the little old lady exampe.....in ER it's common to get 3 or 4 liters for
sepsis mgmnt. Much more than you'd think is normal)
Antibiotics --- early antibiotic, broad spectrum, even if it's the wrong one just do it and kinda hope you get
lucky
Steroids (maybe...that is, some do and some don't)
Early goal directed therapy
25.
OBSTRUCTIVE SHOCK
Mechanical factors that interfere filling or
emptying of the heart or great vessels.
tension pneumo, cava compression, cardiac tamponade, atrial tumor or clot (mechanical interference with
ventricular filling)
Interference with ventricular emptying (PE)
26.
obstructive shock (Tx),
Tension Pneumo
Tension pneumothorax
dec breath sounds, tracheal deviation
respiratory distress and shock
needle decompression
27.
Tx: pericardial tamponade
Pericardial tamponade
hypotension, JVD, muffled heart sounds
Beck's triad
Pericardiocentesis
(Best way to Dx is ultrasound)
* Not that common
28.
Tx: Massive PE
Chest pain, syncope, tachypnea, hypotension
JVD, RV strain on EKG (and seen on echo)
Surgical embolectomy
Thrombolytics
TPA works great for pt with large PE (not small or moderate PEs though) Also given to Pt in shock. Kuhn
says he's seen TPA work in about 30 min. IV.
"very common"
29.
summary points
A state of organ hypoperfusion with resultant cellular dysfunction and
death.
Mechanisms may involve decreased circulating volume, decreased cardiac
output, and vasodilation, sometimes with shunting of blood to bypass
capillary exchange beds.
Symptoms include altered mental status, tachycardia, hypotension, and
oliguria.
Diagnosis is clinical, including BP measurement and sometimes markers
of tissue hypoperfusion (eg, blood lactate, base deficit).
Treatment is with fluid resuscitation, including blood products if
necessary, correction of the underlying disorder, and sometimes
vasopressors.
S-ar putea să vă placă și
- Dr. Az Rifki, Span - Kic Departemen Anestesiologi Dan Reanimasi Rsi Siti Rahmah/Fk-Fkg Universitas Baiturrahmah PadangDocument62 paginiDr. Az Rifki, Span - Kic Departemen Anestesiologi Dan Reanimasi Rsi Siti Rahmah/Fk-Fkg Universitas Baiturrahmah PadangKamelia MarcshendaÎncă nu există evaluări
- Shock: DR Terence See Consultant Emergency Department, TTSHDocument72 paginiShock: DR Terence See Consultant Emergency Department, TTSHHendri Tamara YudaÎncă nu există evaluări
- The Physiology of ShockDocument37 paginiThe Physiology of ShockGauxy AromboÎncă nu există evaluări
- Shock 19Document7 paginiShock 19Teema UmarÎncă nu există evaluări
- ShockDocument36 paginiShockJohnryan NdiranguÎncă nu există evaluări
- ShockDocument70 paginiShockDawit g/kidanÎncă nu există evaluări
- Cardiac FailureDocument63 paginiCardiac FailureNina OaipÎncă nu există evaluări
- Approach To ShockDocument30 paginiApproach To ShocktigistÎncă nu există evaluări
- Origin That Persists Beyond 24 HoursDocument3 paginiOrigin That Persists Beyond 24 Hourseric epahÎncă nu există evaluări
- Shock Study GuideDocument8 paginiShock Study GuideMadameb1Încă nu există evaluări
- ShockDocument53 paginiShockHassan Ahmed100% (3)
- ShockDocument35 paginiShocktrip100Încă nu există evaluări
- Management of Shock: DR Awoyale R.A 26th June, 2009Document78 paginiManagement of Shock: DR Awoyale R.A 26th June, 2009Ibrahim AkinbolaÎncă nu există evaluări
- Drugs Acting in CVSDocument63 paginiDrugs Acting in CVSMeghan Norico Cristuta100% (1)
- Cardiogenic ShockDocument29 paginiCardiogenic ShockagnescheruseryÎncă nu există evaluări
- EMS Shock LexDocument60 paginiEMS Shock LexIgor StefanetÎncă nu există evaluări
- Shock, Hypovolemic, AnaphylacticDocument17 paginiShock, Hypovolemic, Anaphylacticmhmdalbdyny764Încă nu există evaluări
- ShockDocument33 paginiShockVijith.V.kumarÎncă nu există evaluări
- Introduction To ShockDocument56 paginiIntroduction To ShockPaolo VegaÎncă nu există evaluări
- Pediatrics Shock DR AchuarDocument77 paginiPediatrics Shock DR AchuarShimelis TadesseÎncă nu există evaluări
- Cardiogenic Shock: by Fritzanella LafondDocument42 paginiCardiogenic Shock: by Fritzanella LafondhaphahapÎncă nu există evaluări
- Penatalaksanaan SyokDocument59 paginiPenatalaksanaan SyokArif NurfadhilahÎncă nu există evaluări
- USMLE Step 1 in Final YearDocument33 paginiUSMLE Step 1 in Final YearsehrishÎncă nu există evaluări
- 8.syncope & PresyncopeDocument11 pagini8.syncope & PresyncopeIbrahim RamizÎncă nu există evaluări
- Cardiac FailureDocument13 paginiCardiac FailureButool FatimaÎncă nu există evaluări
- .SHOCK, Alice - 1704638750000Document12 pagini.SHOCK, Alice - 1704638750000Nakintu AliceÎncă nu există evaluări
- Cardiac Tamponade: Pankaj Singh Rana Nurse Practitioner in Critical Care Swami Rama Himalayan UniversityDocument35 paginiCardiac Tamponade: Pankaj Singh Rana Nurse Practitioner in Critical Care Swami Rama Himalayan UniversityBarlonga Yhan YogaÎncă nu există evaluări
- Thea Laurene T. Tonelada BSN Iv-C Dysrhythmia: TachydysrhythmiasDocument5 paginiThea Laurene T. Tonelada BSN Iv-C Dysrhythmia: Tachydysrhythmiasscribd_lostandfoundÎncă nu există evaluări
- Shock: Anil PatidarDocument32 paginiShock: Anil Patidarjinal sutharÎncă nu există evaluări
- СердечнаяDocument70 paginiСердечнаяDaniel FunkÎncă nu există evaluări
- Hypotension & ShockDocument22 paginiHypotension & ShockEkawati ErprismanÎncă nu există evaluări
- Cardiac DysrhytmiasDocument60 paginiCardiac DysrhytmiasPY 01Încă nu există evaluări
- KP 2.5.5.4 112036 - Shock AlfanDocument52 paginiKP 2.5.5.4 112036 - Shock Alfannurul ramadhiniÎncă nu există evaluări
- Syncope: Global Cerebral Blood FlowDocument7 paginiSyncope: Global Cerebral Blood FlowChananÎncă nu există evaluări
- KGD 1 VivianDocument101 paginiKGD 1 VivianVivian SaputraÎncă nu există evaluări
- Diagnosis & Treament: ShockDocument52 paginiDiagnosis & Treament: ShockasepÎncă nu există evaluări
- Multi SistemDocument19 paginiMulti SistemciptaarynÎncă nu există evaluări
- HypertensionDocument34 paginiHypertensionmalikman80% (5)
- Shock CorrectedDocument70 paginiShock CorrectedrajevikramÎncă nu există evaluări
- 5 ShockDocument26 pagini5 Shocknightfury200313Încă nu există evaluări
- Heart FailureDocument4 paginiHeart FailureFaizan AbbasiÎncă nu există evaluări
- Lecture Presentation For Clinical 1 StudentsDocument43 paginiLecture Presentation For Clinical 1 Studentskirubel deribÎncă nu există evaluări
- Athero 2 Dr. Raquid 2021Document93 paginiAthero 2 Dr. Raquid 2021oreaÎncă nu există evaluări
- Schwartz: ShockDocument55 paginiSchwartz: ShockJovy Tan-Amodia100% (9)
- MTE Diagnosis and Manag ShockDocument52 paginiMTE Diagnosis and Manag ShockGarbha JmrsÎncă nu există evaluări
- Hypotension: Sandeep Sharma Priyanka T. BhattacharyaDocument10 paginiHypotension: Sandeep Sharma Priyanka T. Bhattacharyaمحمود محمدÎncă nu există evaluări
- Cerebrovascular DiseaseDocument20 paginiCerebrovascular DiseaseMarco GunawanÎncă nu există evaluări
- Heart Failure and ShockDocument34 paginiHeart Failure and Shockfrenee aradanasÎncă nu există evaluări
- ShockDocument49 paginiShockpaulyn ramos100% (1)
- Shock Management: by Group 7Document87 paginiShock Management: by Group 7Nur Khairah AmalinaÎncă nu există evaluări
- Cardiac Notes NursingDocument16 paginiCardiac Notes NursingYemaya8494% (17)
- Shock 2022 SeminarDocument17 paginiShock 2022 Seminarrosie100% (2)
- Assessment Cardiac SystemDocument51 paginiAssessment Cardiac Systemejarnmd100% (2)
- Prepared By: Madi, Krister: Salvador, Ma. Grace BSN-4ADocument36 paginiPrepared By: Madi, Krister: Salvador, Ma. Grace BSN-4ATap Tap100% (2)
- Shock PathophysiologyDocument63 paginiShock PathophysiologyRani OktasariÎncă nu există evaluări
- 10.15 Edrian Zulkarnain - ShockDocument42 pagini10.15 Edrian Zulkarnain - ShockBintang UbamnataÎncă nu există evaluări
- Cardio and Hema - DR PueyoDocument161 paginiCardio and Hema - DR Pueyoapi-3735995100% (2)
- ShockDocument4 paginiShockdeeÎncă nu există evaluări
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtDe la EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtEvaluare: 5 din 5 stele5/5 (1)
- Orthostatic Hypotension: Causes, Tests, and Treatment OptionsDe la EverandOrthostatic Hypotension: Causes, Tests, and Treatment OptionsÎncă nu există evaluări
- Alcohol Withdrawal Care PlanDocument1 paginăAlcohol Withdrawal Care PlanVanessaMUellerÎncă nu există evaluări
- Fluid/Electrolyte Imbalance S/S Nursing Care Fluid DeficitDocument1 paginăFluid/Electrolyte Imbalance S/S Nursing Care Fluid DeficitVanessaMUellerÎncă nu există evaluări
- Physical Assessment ChartDocument1 paginăPhysical Assessment ChartVanessaMUellerÎncă nu există evaluări
- Lab Values Chart 120511 PDFDocument5 paginiLab Values Chart 120511 PDFVanessaMUeller100% (3)
- Penuemonia Care PalnDocument2 paginiPenuemonia Care PalnVanessaMUellerÎncă nu există evaluări
- Example 1 - Focus: Nausea Related To AnestheticDocument1 paginăExample 1 - Focus: Nausea Related To AnestheticVanessaMUellerÎncă nu există evaluări
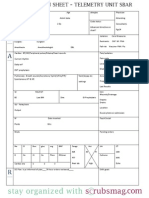
- Updated Clinical SheetDocument1 paginăUpdated Clinical SheetVanessaMUellerÎncă nu există evaluări
- Name Age Room Code Dr. Isolation Activity Diet Allergy: DX: HXDocument1 paginăName Age Room Code Dr. Isolation Activity Diet Allergy: DX: HXVanessaMUellerÎncă nu există evaluări
- Newborn Assessment NORMALDocument2 paginiNewborn Assessment NORMALVanessaMUellerÎncă nu există evaluări
- ManagmentDocument1 paginăManagmentVanessaMUellerÎncă nu există evaluări
- Admission Database PDFDocument6 paginiAdmission Database PDFVanessaMUellerÎncă nu există evaluări
- Nurse Brain Sheet Half SizeDocument1 paginăNurse Brain Sheet Half Sizevsosa624Încă nu există evaluări
- Diseases With Dermatologic ManifestationsDocument1 paginăDiseases With Dermatologic ManifestationsVanessaMUellerÎncă nu există evaluări
- Fluid/Electrolyte Imbalance S/S Nursing Care Fluid DeficitDocument1 paginăFluid/Electrolyte Imbalance S/S Nursing Care Fluid DeficitVanessaMUellerÎncă nu există evaluări
- IV PushDocument3 paginiIV PushVanessaMUeller100% (1)
- Clinical AssessementDocument2 paginiClinical AssessementVanessaMUellerÎncă nu există evaluări
- AdmimDocument2 paginiAdmimVanessaMUellerÎncă nu există evaluări
- AssessingWounds ProcedureDocument3 paginiAssessingWounds ProcedureVanessaMUellerÎncă nu există evaluări
- Alcohol Withdrawal Care PlanDocument1 paginăAlcohol Withdrawal Care PlanVanessaMUeller100% (1)
- COPD Care PLAN PDFDocument2 paginiCOPD Care PLAN PDFVanessaMUeller100% (1)
- Wound Care PDFDocument100 paginiWound Care PDFVanessaMUellerÎncă nu există evaluări
- Example 1 - Focus: Nausea Related To AnestheticDocument1 paginăExample 1 - Focus: Nausea Related To AnestheticVanessaMUellerÎncă nu există evaluări
- (Chapter 3) : Cell BiologyDocument80 pagini(Chapter 3) : Cell BiologyVanessaMUellerÎncă nu există evaluări
- Nurse Brain Sheet Telemetry Unit SBARDocument1 paginăNurse Brain Sheet Telemetry Unit SBARvsosa624Încă nu există evaluări
- HR Ocampo Danilo s2 E10 PDFDocument4 paginiHR Ocampo Danilo s2 E10 PDFVanessaMUellerÎncă nu există evaluări
- MedCards PDFDocument10 paginiMedCards PDFVanessaMUellerÎncă nu există evaluări
- Nurse Brain Sheet With Shift HoursDocument2 paginiNurse Brain Sheet With Shift HoursLauren Cournoyer Foreman100% (4)
- Nurse Brain Sheet Half SizeDocument1 paginăNurse Brain Sheet Half SizeRobyn GrogitskyÎncă nu există evaluări
- Wound Care PDFDocument100 paginiWound Care PDFVanessaMUeller100% (2)
- Comprehensive Head To Toe Assessment PDFDocument22 paginiComprehensive Head To Toe Assessment PDFVanessaMUellerÎncă nu există evaluări
- Prepare Active Directory and Domains For Exchange 2013 PDFDocument18 paginiPrepare Active Directory and Domains For Exchange 2013 PDFAdam DanielÎncă nu există evaluări
- Engg 135 Design of Reinforced Concrete Structures: Bond and Bar Development Reading: Wight and Macgregor Chapter 8Document24 paginiEngg 135 Design of Reinforced Concrete Structures: Bond and Bar Development Reading: Wight and Macgregor Chapter 8Manuel MirandaÎncă nu există evaluări
- Lesson10 Sacraments of InitiationDocument76 paginiLesson10 Sacraments of InitiationInsatiable CleeÎncă nu există evaluări
- Business Law Term PaperDocument19 paginiBusiness Law Term PaperDavid Adeabah OsafoÎncă nu există evaluări
- Soal Passive VoiceDocument1 paginăSoal Passive VoiceRonny RalinÎncă nu există evaluări
- Becg Unit-1Document8 paginiBecg Unit-1Bhaskaran Balamurali0% (1)
- Short StoriesDocument20 paginiShort StoriesPatrick Paul AlvaradoÎncă nu există evaluări
- Food Drug InteractionDocument23 paginiFood Drug Interactionayman_fkirin100% (5)
- I Wanted To Fly Like A ButterflyDocument12 paginiI Wanted To Fly Like A ButterflyJorge VazquezÎncă nu există evaluări
- Listen The Song and Order The LyricsDocument6 paginiListen The Song and Order The LyricsE-Eliseo Surum-iÎncă nu există evaluări
- Chapter 4Document20 paginiChapter 4Alyssa Grace CamposÎncă nu există evaluări
- Kangar 1 31/12/21Document4 paginiKangar 1 31/12/21TENGKU IRSALINA SYAHIRAH BINTI TENGKU MUHAIRI KTNÎncă nu există evaluări
- Barber ResumeDocument6 paginiBarber Resumefrebulnfg100% (1)
- PLM V6R2011x System RequirementsDocument46 paginiPLM V6R2011x System RequirementsAnthonio MJÎncă nu există evaluări
- Seafood Serving Tools Make The Task of Cleaning Seafood and Removing The Shell Much Easier. ForDocument32 paginiSeafood Serving Tools Make The Task of Cleaning Seafood and Removing The Shell Much Easier. Forivy l.sta.mariaÎncă nu există evaluări
- Burger 2005Document7 paginiBurger 2005Stefania PDÎncă nu există evaluări
- SANTHOSH RAJ DISSERTATION Presentation1Document11 paginiSANTHOSH RAJ DISSERTATION Presentation1santhosh rajÎncă nu există evaluări
- Econ 281 Chapter02Document86 paginiEcon 281 Chapter02Elon MuskÎncă nu există evaluări
- Schneider - Ch16 - Inv To CS 8eDocument33 paginiSchneider - Ch16 - Inv To CS 8ePaulo SantosÎncă nu există evaluări
- Human Rights in The Secondary SchoolDocument57 paginiHuman Rights in The Secondary SchoolJacaÎncă nu există evaluări
- Cat Enclosure IngDocument40 paginiCat Enclosure IngJuan Pablo GonzálezÎncă nu există evaluări
- Fila 1Document4 paginiFila 1Karolina Sanchez83% (6)
- Choose The Correct Answer by Crossing A, B, or C (Pilihlah Jawaban Yang Benar Dengan MemberDocument3 paginiChoose The Correct Answer by Crossing A, B, or C (Pilihlah Jawaban Yang Benar Dengan MemberJufriÎncă nu există evaluări
- Polygamy A Very Short Introduction Pearsall Sarah M S Download PDF ChapterDocument51 paginiPolygamy A Very Short Introduction Pearsall Sarah M S Download PDF Chapterharry.bailey869100% (5)
- Design and Implementation of A Computerised Stadium Management Information SystemDocument33 paginiDesign and Implementation of A Computerised Stadium Management Information SystemBabatunde Ajibola TaofeekÎncă nu există evaluări
- Essential Real AnalysisDocument459 paginiEssential Real AnalysisPranay Goswami100% (2)
- The Book of Mark: BY Dr. R. Muzira Skype: Pastorrobertmuzira Cell: 0782 833 009Document18 paginiThe Book of Mark: BY Dr. R. Muzira Skype: Pastorrobertmuzira Cell: 0782 833 009Justice MachiwanaÎncă nu există evaluări
- câu điều kiện loại 1Document5 paginicâu điều kiện loại 1ThuHoàiÎncă nu există evaluări
- Eris User ManualDocument8 paginiEris User ManualcasaleiroÎncă nu există evaluări
- Cookery Week 7 - 8 FinalDocument18 paginiCookery Week 7 - 8 FinalJay CachoÎncă nu există evaluări