Documente Academic
Documente Profesional
Documente Cultură
Path o Physiology
Încărcat de
Diorella Marie López GonzálezDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Path o Physiology
Încărcat de
Diorella Marie López GonzálezDrepturi de autor:
Formate disponibile
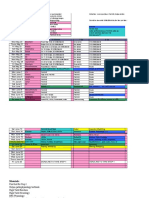
PATHOPHYSIOLOGY
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Question List
Pathophysiology Q No:
Cardiology
Pathophysiology Q No:
42 Endocrinology
Pathophysiology Q No:
Pulmonology
Pathophysiology Q No:
43 Hepatobiliary system
Pathophysiology Q No:
Pulmonology
Pathophysiology Q No:
44 Cardiology
Pathophysiology Q No:
Cardiology
Pathophysiology Q No:
45 Cardiology
Pathophysiology Q No:
Renal
Pathophysiology Q No:
46 Gastrointestinal system
Pathophysiology Q No:
Hepatobiliary system
Pathophysiology Q No:
47 Pulmonology
Pathophysiology Q No:
Genitourinary
Pathophysiology Q No:
48 Hepatobiliary system
Pathophysiology Q No:
Renal
Pathophysiology Q No:
49 Musculoskeletal
Pathophysiology Q No:
Endocrinology
Pathophysiology Q No:
50 Endocrinology
Pathophysiology Q No:
10 Endocrinology
Pathophysiology Q No:
51 Endocrinology
Pathophysiology Q No:
11 Cardiology
Pathophysiology Q No:
52 Blood vessels
Pathophysiology Q No:
12 Endocrinology
Pathophysiology Q No:
53 Cardiology
Pathophysiology Q No:
13 Endocrinology
Pathophysiology Q No:
54 Endocrinology
Pathophysiology Q No:
14 Reproductive system
Pathophysiology Q No:
55 Cardiology
Pathophysiology Q No:
15 Pulmonology
Pathophysiology Q No:
56 Endocrinology
Pathophysiology Q No:
16 Pulmonology
Pathophysiology Q No:
57 Endocrinology
Pathophysiology Q No:
17 Endocrinology
Pathophysiology Q No:
58 Cardiology
Pathophysiology Q No:
18 Cardiology
Pathophysiology Q No:
59 Cardiology
Pathophysiology Q No:
19 Blood vessels
Pathophysiology Q No:
60 Endocrinology
Pathophysiology Q No:
20 Cardiology
Pathophysiology Q No:
61 Musculoskeletal
Pathophysiology Q No:
21 Endocrinology
Pathophysiology Q No:
62 Gastrointestinal system
Pathophysiology Q No:
22 Neurology
Pathophysiology Q No:
63 Musculoskeletal
Pathophysiology Q No:
23 Pulmonology
Pathophysiology Q No:
64 Cardiology
Pathophysiology Q No:
24 Pulmonology
Pathophysiology Q No:
65 Cardiology
Pathophysiology Q No:
25 Endocrinology
Pathophysiology Q No:
66 Endocrinology
Pathophysiology Q No:
26 Cardiology
Pathophysiology Q No:
67 Cardiology
Pathophysiology Q No:
27 Gastrointestinal system
Pathophysiology Q No:
68 Cardiology
Pathophysiology Q No:
28 Gastrointestinal system
Pathophysiology Q No:
69 Endocrinology
Pathophysiology Q No:
29 Cardiology
Pathophysiology Q No:
70 Endocrinology
Pathophysiology Q No:
30 Cardiology
Pathophysiology Q No:
71 Pulmonology
Pathophysiology Q No:
31 Endocrinology
Pathophysiology Q No:
72 Pulmonology
Pathophysiology Q No:
32 Blood vessels
Pathophysiology Q No:
73 Endocrinology
Pathophysiology Q No:
33 Cardiology
Pathophysiology Q No:
74 Genitourinary
Pathophysiology Q No:
34 Cardiology
Pathophysiology Q No:
75 Gastrointestinal system
Pathophysiology Q No:
35 Blood vessels
Pathophysiology Q No:
76 Endocrinology
Pathophysiology Q No:
36 Cardiology
Pathophysiology Q No:
77 Hepatobiliary system
Pathophysiology Q No:
37 Endocrinology
Pathophysiology Q No:
78 Endocrinology
Pathophysiology Q No:
38 Endocrinology
Pathophysiology Q No:
79 Endocrinology
Pathophysiology Q No:
39 Endocrinology
Pathophysiology Q No:
80 Gastrointestinal system
Pathophysiology Q No:
40 Gastrointestinal system
Pathophysiology Q No:
81 Gastrointestinal system
Pathophysiology Q No:
41 Endocrinology
Pathophysiology Q No:
82 Blood vessels
Pathophysiology Q No:
83
Cardiology
Pathophysiology Q No:
101 Blood vessels
Pathophysiology Q No:
84
Cardiology
Pathophysiology Q No:
102 Cardiology
181
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Pathophysiology Q No:
85
Cardiology
Pathophysiology Q No:
103 Cardiology
Pathophysiology Q No:
86
Gastrointestinal system
Pathophysiology Q No:
104 Cardiology
Pathophysiology Q No:
87
Endocrinology
Pathophysiology Q No:
105 Gastrointestinal system
Pathophysiology Q No:
88
Musculoskeletal
Pathophysiology Q No:
106 Cardiology
Pathophysiology Q No:
89
Endocrinology
Pathophysiology Q No:
107 Cardiology
Pathophysiology Q No:
90
Genitourinary
Pathophysiology Q No:
108 Blood vessels
Pathophysiology Q No:
91
Blood vessels
Pathophysiology Q No:
109 Cardiology
Pathophysiology Q No:
92
Endocrinology
Pathophysiology Q No:
110 Cardiology
Pathophysiology Q No:
93
Endocrinology
Pathophysiology Q No:
111 Endocrinology
Pathophysiology Q No:
94
Hepatobiliary system
Pathophysiology Q No:
112 Musculoskeletal
Pathophysiology Q No:
95
Pulmonology
Pathophysiology Q No:
113 Endocrinology
Pathophysiology Q No:
96
Musculoskeletal
Pathophysiology Q No:
114 Hepatobiliary system
Pathophysiology Q No:
97
Gastrointestinal system
Pathophysiology Q No:
115 Endocrinology
Pathophysiology Q No:
98
Pulmonology
Pathophysiology Q No:
116 Pulmonology
Pathophysiology Q No:
99
Pulmonology
Pathophysiology Q No:
117 Endocrinology
Pathophysiology Q No:
100 Cardiology
182
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 1: A 62-year-old Caucasian female hospitalized with acute myocardial
infarction dies suddenly on day four of her hospitalization. The autopsy
findings are pictured below (RV = right ventricle, LAD = left anterior
descending coronary artery). The patient most likely died from which of the
following?
A. Profound hypotension
B. Hypertensive emergency
C. Left-to-right shunt
D. Increased venous return
E. Right-to-left shunt
Explanation:
The gross autopsy specimen shows a ruptured left ventricular (LV) free wall. This
complication of transmural (ST-elevation) myocardial infarction generally occurs 3 to
7 days after the onset of total ischemia, when coagulative necrosis neutrophil
infiltration and enzymatic lysis of connective tissue have substantially weakened the
infarcted myocardium (mean 4-5 days; range 1-10 days).
Free wall rupture causes cardiac tamponade, which greatly limits ventricular filling
during diastole. As the pressure increases in the pericardial cavity, venous return to
the heart is reduced. This leads to profound systemic hypotension and pulseless
electrical activity. Failure to relieve the obstruction will lead to death.
Clinically, these patients present with profound hypotension and shortness of breath.
On physical examination, the heart sounds are muffled and the jugular venous
pressure is elevated.
(Choice C) Left-to-right shunting would occur as a result of ventricular septal
rupture.
(Choice E) Right-to-left shunting is seen in patients with Eisenmenger syndrome, a
complication of certain congenital heart diseases. This would be unusual as a
complication of Ml.
Educational Objective:
The triad of muffled heart sounds elevated jugular venous pressure and profound
hypotension indicates pericardial tamponade. Rupture of the ventricular free wall as
a consequence of an acute transmural Ml can cause tamponade. Rupture usually
occurs 3 to 7 days after the onset of total ischemia, when coagulative necrosis,
neutrophil infiltration, and enzymatic lysis of connective tissue have sufficiently
weakened the infarcted myocardium.
183
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 2: A 65-year-old male presents to your office with exertional dyspnea. He has
had four respiratory infections over the course of the past year. For the past 30
years he has smoked 1 packs of cigarettes a day. Physical examination reveals
diffusely decreased breath sounds, increased chest anteroposterior diameter, and
decreased diaphragmatic excursion. Pulmonary function testing will most likely
show which of the following patterns of findings (TLC total lung capacity; FEV 1
forced expiratory volume in 1 second; FVC forced vital capacity; RV, residual
volume)?
Explanation:
This patients clinical picture is consistent with chronic obstructive pulmonary disease
(COPD). COPD encompasses chronic bronchitis and emphysema. Heavy smoking is
the most common cause. Chronic bronchitis and emphysema have similar effects on
FEV1/FVC during pulmonary function testing (PFT). The hallmark of an obstructive
PFT profile is decreased FEV1/FVC (FEV1%) due to expiratory airflow obstruction.
Emphysema also causes a decrease in EVC and an increase in both TLC and RV due
to destruction of interalveolar walls, decrease in lung elastic recoil, and distal
airspace enlargement. Choice C is the only option with a decreased (FEV1%) and an
increase in both TLC and RV.
(Choice E) This PFT profile is characteristic of restrictive lung disease (e.g.
pulmonary fibrosis). In restrictive lung disease, lung volumes particularly TLC and
EVC are decreased due to reduced lung expansion. FEV1/FVC may be increased
above the normal value of approximately 80%. This FEV1% increase is the combined
result of reduced FVC, decreased lung compliance, and increased elastic recoil.
Educational Objective:
Chronic obstructive pulmonary disease (COPD) in a heavy smoker may consist of
both emphysema and chronic bronchitis and thus may present with both progressive
exertional dyspnea (characteristic of emphysema) and frequent respiratory
infections (characteristic of chronic bronchitis). On pulmonary function testing all
COPD yields a decreased FEV1/FVC ratio. Emphysema also tends to increase TLC
and RV. In contrast, restrictive lung diseases can cause reduced lung volumes and
increased FEV1/FVC.
184
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 3: A 45-year-old male presents to the ER with severe dyspnea of recent
onset. He says he has never experienced symptoms like this before. Arterial
blood gases show a Pa02 of 54 mmHg and a PaCO2 of 26 mmHg. The process
most likely responsible for this patients condition is:
Upper airway obstruction
B. Poor respiratory drive
C. Respiratory muscle fatigue
D. Respiratory acidosis
E. Alveolar hyperventilation
r F. Decreased chest wall compliance
A.
Explanation:
This patient has a combination of hypoxemia and hypocapnia. PaCO2 is inversely
related to alveolar ventilation, and is considered the main indicator of alveolar
ventilation. Assuming a normal rate of metabolic CO2 production, hypocapnia
implies alveolar hyperventilation.
PaCO2 = Basal metabolic rate / alveolar ventilation
His hypoxia could be from pulmonary embolism pulmonary edema, pneumonia etc.
All these conditions can cause tachypnea resulting in low PaCO2.
(Choice A) Significant upper airway obstruction would impair alveolar ventilation and
would result in an increase in PaCO2 with a proportionate decrease in Pa02.
(Choice B) This patients degree of alveolar hyperventilation indicates that his
peripheral arterial chemoreceptors sense the hypoxemia and are sending neural
impulses to his CNS respiratory centers to increase respiratory drive above normal
levels, resulting in hypocapnia.
(Choice C) Significant respiratory muscle fatigue would impair alveolar ventilation
and would result in an increase in PaCO2.
(Choice D) Respiratory acidosis is caused by deficient alveolar ventilation, resulting
in an increase in PaCO2 (hypercapnia).
(Choice F) A decrease in chest wall compliance could increase the work of breathing
and thereby result in respiratory muscle fatigue. Alveolar hypoventilation and
increased PaCO2 with a proportionate decrease in PaO2 could result.
Educational Objective:
Arterial PaCO2 is a direct indicator of the status of alveolar ventilation. Hypocapnia
implies ongoing alveolar hyperventilation. Upper airway obstruction, reduced
ventilatory drive, respiratory muscle fatigue, and decreased chest wall compliance
are possible cause alveolar hypoventilation, which would cause hypercapnia.
185
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 4: A 52-year-old Caucasian male presents to your office with two week history
of progressive fatigue and exertional dyspnea. He brings with him the report from a
recent cardiac catheterization (shown below). Cardiac auscultation reveals a murmur
that is best heard when the patient sits up and leans forward. Which of the time
points pictured below corresponds to the peak murmur intensity?
A.
B.
C.
D.
E.
A
B
C
D
E
Explanation:
Cardiac catheterization shows a hemodynamic profile consistent with aortic
regurgitation (AR). Note the high peaking left ventricular and aortic pressures during
systole and the steep diastolic decline in aortic pressure. A normal catheterization
report is shown below for purposes of comparison:
The peak intensity of an AR murmur occurs after closure of the incompetent aortic
valve, at the point when the pressure gradient between the aorta and the left
ventricle is at its maximum i.e. time C.
(Choice A) This time point corresponds to the opening of the aortic valve during
systole. The murmur of aortic stenosis would be heard best here.
(Choice B) This point corresponds to the closure of the aortic valve. The A2 heart
sound is heard here. At this instant there is not yet regurgitant flow from the aorta
to the left ventricle, so no murmurs are audible.
186
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice D) Time point D occurs in mid-diastole. The murmur of AR might be heard
here, as there is a pressure gradient between the aorta and left ventricle (LV).
However the intensity of the murmur would be less than at time C because the
magnitude of the gradient is less. Because the AR murmur decreases in intensity
with the falling aortic pressure, it is a decrescendo diastolic murmur.
(Choice E)Time E marks the onset of left atrial contraction at the end of ventricular
diastole. If the murmur of AR were still audible at this time, its intensity would be
further reduced by the increase in left ventricular end diastolic pressure.
Educational Objective:
The murmur of AR is a diastolic decrescendo murmur heard loudest in early diastole
when the pressure gradient between the aorta and the left ventricle is maximal.
187
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 5: A 34-year-old male who is being treated for acute leukemia develops
oliguria. His serum creatinine level is 2.7 mg/dL. Renal biopsy reveals
multiple uric acid crystals obstructing renal tubular lumen. The principal site
of uric acid precipitation would be which of the following?
Proximal tubules due to high solute concentration
B. Proximal tubules due to impaired uric acid transport
C. Loop of Henle due to urine hyposmolarity
D. Distal tubules due to high urine flow rate
E. Collecting ducts due to low urine pH
A.
Explanation:
Tumor lysis syndrome is an oncologic emergency. It often develops during
chemotherapy for high-grade lymphomas, leukemias, and other tumors that have
rapid cell turnover and high sensitivity to chemotherapy. When a large number of
tumor cells are destroyed during chemotherapy, intracellular ions, such as
potassium, phosphorous, and uric acid (a metabolite of tumor nucleic acid), are
released into the serum and are then filtered by the kidneys.
Uric acid (pKa = 5.4) is soluble at physiologic pH, but precipitates in an acidic
environment. The lowest pH along the nephron is found in the distal tubules and
collecting ducts; so these are the segments of the nephron that become obstructed
by uric acid crystals. Obstructive uropathy and acute renal failure follow.
The risk of tumor lysis syndrome can be reduced by urine alkalinization and
hydration. Additionally allopurinol (a xanthine oxidase inhibitor) is used to reduce
uric acid production during the breakdown of tumor cells.
(Choice D) Ignore the anatomy portion of choice D and evaluate the latter portion. A
high urine flow rate would universally decrease uric acid crystallization and
precipitation. Therefore, this cannot possibly be the correct answer.
(Choices A, B and C) Uric acid does not precipitate in proximal tubules or in Henles
loop.
Educational Objective:
Tumor cell syndrome occurs when tumors with a high cell turnover are treated with
chemotherapy. The lysis of tumor cells causes intracellular ions such as potassium
and phosphorous, and uric acid (metabolite of tumor nucleic acid) to be released into
serum. Uric acid is soluble at physiologic pH, but it can precipitate in the normally
acidic environment of distal tubules and collecting ducts. The prevention of tumor
lysis syndrome includes urine alkalinization and hydration, as high urine flow and
high pH along the nephron prevents crystallization and precipitation of uric acid.
188
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 6: A 54-year-old known alcoholic is brought to the emergency room because
of hematemesis. By the following morning he has developed altered mental status.
Physical examination shows abdominal distention, flapping tremor, and
gynecomastia. Liver span is decreased. Which of the following is the most likely
cause of his altered mental status?
A. Occlusion of the middle cerebral artery
B. Accumulation of blood urea nitrogen
C. Increased absorption of nitrogenous substances from gut
D. Decreased concentrations of y-aminobutyric acid (GABA)
E. Bacterial infection of the meninges
Explanation:
Hepatic encephalopathy is a reversible decline in neurologic function precipitated by
hepatic damage. The pathogenesis of this condition is likely related to increased
levels of ammonia in circulation which cause inhibitory neurotransmission via the
GABA receptors in the central nervous system.
Ammonia initially enters circulation through the gastrointestinal tract, after having
been created during the enterocytic catabolism of glutamine and the bacterial
catabolism of dietary protein in the colon. The ammonia then enters the liver
through the portal vein for detoxification to urea. Because the damaged liver has
impaired detoxification ability however, ammonia accumulates in the blood instead.
Frequently, hepatic encephalopathy is precipitated by a stressor that alters the
ammonia balance (eg, hypovolemia, gastrointestinal bleeding hypokalemia,
metabolic alkalosis, hypoxia, sedative usage, hypoglycemia, or infection).
Lowering of the blood ammonia level is typically accomplished with continuous
administration of a disaccharidase such as lactulose. Bacterial action on the lactulose
results in acidification of colonic contents, which converts the absorbable ammonia
into nonabsorbable ammonium ion (an ammonia trap).
(Choice A) The middle cerebral artery is the largest cerebral artery and is most
commonly involved in cerebrovascular accidents (CVAs). This patients presentation
is suggestive of hepatic encephalopathy, however, and not stroke.
(Choice B) Accumulation of blood urea nitrogen is suggestive of renal failure, heart
failure, or dehydration. Liver disease is associated with decreased blood urea
nitrogen because less ammonia is converted to urea.
(Choice D) Increased (not decreased) activity of the GABA neurotransmitter system
is thought to be directly responsible for the altered mental status seen in hepatic
encephalopathy.
(Choice E) Bacterial infection of the meninges is characteristic of meningitis which
does not fit this patients presentation as well as hepatic encephalopathy does.
Educational Objective:
Hepatic encephalopathy appears to be secondary to increased levels of ammonia in
circulation which cause inhibitory neurotransmission via the GABA receptors in the
central nervous system. Frequently hepatic encephalopathy is precipitated by a
stressor that alters the ammonia balance (eg, gastrointestinal bleeding).
189
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 7: Which of the following interventions would be most likely to increase the
threshold for crystal precipitation in a solution of calcium, phosphate and oxalate
salts?
A. Increased ionized calcium concentration
B. Increased ionized phosphate concentration
C. Decreased free water
D. Acidification of the urine
E. Saturation with uric acid
F. Saturation with citrate
Explanation:
Urine is a complex solution with a large number of compounds in a dynamic balance.
Changes to concentrations and ratios of components such as calcium, phosphate
oxalate, uric acid, and citrate can shift this balance to cause salt precipitation and
stone formation.
Increased excretion of stone-forming compounds can cause urine supersaturation.
When fluid intake is low, the concentrations of these ions in urine are increased
(without affecting absolute amounts). When supersaturation occurs precipitation and
aggregation of crystals follows. The crystal mass may attach to the surface of the
renal papillae, facilitating the continued aggregation of salts around this nidus.
High fluid intake decreases the concentrations of stone-forming ingredients, thus
preventing stone formation. A high urine citrate concentration has a stonepreventing effect as well. Citrate binds to free (ionized) calcium, preventing its
precipitation and facilitating its excretion.
(Choices A, B and C) Increasing ionized calcium and ionized phosphate
concentrations, and decreasing water intake will all promote urine supersaturation.
(Choice D) Low urine pH is required for the formation of uric acid and cystine stones.
Calcium salts can precipitate at acidic as well as neutral pHs. Thus, urine
acidification would encourage crystals to precipitate in this solution. (Struvite stones
are unique in that they occur at an alkaline pH.)
(Choice E) Hyperuricosuria is associated with a number of conditions, including gout
myeloproliferative disorders, and situations of high purine and alcohol intake. It can
also be idiopathic. Increased urine uric acid concentration promotes the formation of
calcium and uric acid stones.
Educational Objective:
Renal calculi occur when there is an imbalance of the factors that facilitate and
prevent stone formation. Increased concentrations of calcium, phosphate, oxalate,
and uric acid promote salt crystallization, whereas increased citrate and high fluid
intake help prevent calculi formation.
190
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 8: A 44-year-old male presents to your office for a routine check-up. His past
medical history is significant for mild hypercholesterolemia that he has been able to
control through diet. His father died of a myocardial infarction at the age of 56, and
his mother, who is still living, has a history of stroke. On physical examination, the
patient has a blood pressure of 160/100 mmHg and a heart rate of 70 beats per
minute. You start him on enalapril. Over the first several days of therapy, the
patients glomerular filtration rate (GER) adjusts in the following fashion: Enalaprils
effects on which of the following structures is most likely responsible for this renal
response
A. Afferent arterioles
B. Afferent arterioles
C. Vasa recta
D. Distal tubules
E. Proximal tubules
Explanation:
Enalapril is an ACE-inhibitor. All ACE-inhibitors decrease the amount of circulating
angiotensin II, a substance that causes: a) systemic vasoconstriction, b) preferential
constriction of the glomerular efferent arteriole, and c) enhancement of adrenal
cortical aldosterone secretion. Thus, reduction of available angiotensin II by an ACEinhibitor would be expected to acutely decrease systemic vascular and efferent
arteriolar resistance. Selective efferent arteriolar dilation and decreased systemic
vascular resistance both have the effect of reducing the GFN.
Educational Objective:
In the kidney, angiotensin II preferentially constricts the efferent arteriole, thereby
maintaining the GER. ACE-inhibitors promote efferent arteriolar dilation, causing
GFN reductions.
191
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 9: A 40-year-old female presents with amenorrhea. Her family history is
unremarkable. Labs reveal an increased prolactin level. MRI shows a 6-mm
pituitary adenoma. The patient refuses medical and surgical therapy, as she is
happy about not having menstrual period. An untreated prolactin secreting
pituitary adenoma puts this patient at greatest risk of developing which of the
following?
Osteoporosis
B. Gastric ulcers
C. Myocardial infarction
D. Stroke
E. Rapid enlargement of adenoma
A.
Explanation:
High levels of prolactin suppress gonadotropin-releasing hormone (GnRH) secretion
from the hypothalamus, leading to hypogonadism. (High levels of prolactin in
females can also cause milk discharge from the breasts, known as galactorrhea.) As
hyperprolactinemia causes hypogonadism, ie low estrogen in females, affected
patients are at risk for accelerated bone loss. Estrogens maintain bone mass in
females so any loss of estrogenwhether from menopause, hormone imbalances, or
surgical removal of the ovariesleads to loss of bone density. Severe loss of bone
density is described by the word osteoporosis.
(Choice B) Multiple endocrine neoplasia (MEN) type I consists of the triad of
hyperparathyroidism, hypergastrinemia, and pituitary adenoma. A good mnemonic is
to remember 3Ps: para thyroidism (hyper), peptic ulcer due to a gastrin secreting
tumor (usually in the pancreas), and pituitary adenoma. If this patient did have the
MEN syndrome, her family history would most likely have some red flags. The
chances of this patient developing a gastric ulcer are no higher than the general
populations.
(Choices C and D) Patients with hyperprolactinemia are not at increased risk for
myocardial infarction or stroke. Estrogen was once thought to be cardioprotective,
but that is now a very controversial belief.
(Choice E) Most prolactinomas in females are smaller than 10mm
microprolactinoma. Most males present with macroprolactinoma (tumor larger than
10mm in size) because men typically do not have symptoms until a pituitary tumor
is very large. Even without treatment, the risk of rapid enlargement of a
microadenoma is low.
Educational Objective:
Hyperprolactinemia causes hypogonadism, which leads to reduced estrogen in
women. Low estrogen due to any cause is risk factor for accelerated bone loss.
192
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 10: Soon after birth, a neonate develops vomiting and hypotension. Physical
examination shows clitoromegaly. Laboratory studies show:
Chemistry panel
Serum sodium 120 mEq/L
Serum potassium 5.6 mEq/L
Chloride 90 mEq/L
Bicarbonate 6 mEq/L
Blood glucose 60 mg/dL
Abdominal imaging shows bilateral adrenal hyperplasia. Further evaluation will most
likely show?
Explanation:
193
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
The patient described in the vignette has clinical features of cortisol deficiency
(hyponatremia, hyperkalemia, acidosis and hypoglycemia) as well as androgen
excess (clitoromegaly). Her pattern of laboratory abnormalities in combination with
the results of her abdominal imaging point to a diagnosis of congenital adrenal
hyperplasia (CAH). CAH encompasses a group of disorders that stem from various
defects in the enzymes involved in cortisol biosynthesis by the adrenal gland. The
result is an increase in cortisol precursors proximal to the enzyme deficiency. The
specific pattern of precursor excess can be used to make the biochemical diagnosis
of these disorders.
Deficiency of 21-hydroxylase is the most common cause of CAH, accounting for 90%
of patients. This enzyme is responsible for the conversion of 17
hydroxyprogesterone to 11-deoxycortisol in the zona fasciculata, and for the
conversion of progesterone to deoxycorticosterone in the zona glomerulosa. Thus,
serum 1 7-hydroxyprogesterone levels are elevated in this condition because the
enzymatic blockade prevents its conversion to 11-deoxycorlisol.
As a result of this enzyme deficiency, the adrenal gland cannot synthesize cortisol
efficiently. This causes an increased production of adrenal androgens, because the
accumulating cortisol precursors are diverted towards the adrenal androgen
biosynthetic pathway. The resultant low cortisol levels stimulate pituitary production
of ACTH, which increases the production of adrenal androgens even further.
Educational Objective:
Deficiency of 21-hydroxylase is the most common type of congenital adrenal
hyperplasia. Patients with classic 21- hydroxylase deficiency present with clinical
manifestations of cortisol and aldosterone deficiency combined with androgen
excess. (The genitalia of female infants maybe masculinized to some degree; male
infants, however, are normal in appearance.)
194
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 11: A 45-year-old Caucasian male presents to your office with exertional
dyspnea and easy fatigability. He has not seen a physician for 10 years and
has no knowledge of any medical problems. He does not take any medications.
and admits to cigarette smoking and alcohol use. His BP is 170/90 mmHg and
his heart rate is 80 beats per minute. There are bilateral lung crackles on
physical exam. Which of the following set of laboratory findings would be most
consistent with diastolic heart failure in this patient?
Left Ventricular
Left Ventricular
Left Ventricular
Cavity
Ejection Fraction
End-Diastolic
Pressure
A.
Dilated
Decreased
Increased
B.
Dilated
Decreased
Normal
C.
Normal
Decreased
Decreased
D.
Normal
Decreased
Increased
E.
Normal
Normal
Increased
F.
Dilated
Normal
Normal
Explanation:
This patient has symptoms of heart failure, defined broadly as a pathophysiological
state wherein the heart either cannot pump enough blood to meet tissue metabolic
requirements, or can do so only from an elevated ventricular filling pressure.
Heart failure may be systolic and/or diastolic. Diastolic heart failure designates a
pathologic reduction in diastolic ventricular compliance. Left ventricular end-diastolic
volume (LVEDV) and therefore stroke volume and cardiac output are reduced at
normal filling pressures (LVEDP). The Frank-Starling curve relating stroke volume to
LVEDV, and therefore ejection fraction (EF)I is normal. LVEDP must be increased to
abnormally high values to achieve a normal LVEDV and thereby restore cardiac
output to near normal.
Left ventricular systolic failure implies that stroke volume and cardiac output are
reduced at a normal LVEDV. The FrankStarling curve relating stroke volume to
LVEDVI and therefore EF, is depressed. To maintain a near normal cardiac output,
both LVEDV and thus LVEDP must be abnormally increased.
In summary, LVEDP must be abnormally increased to restore cardiac output in both
systolic and diastolic heart
failure. However, LVEDV remains normal in diastolic failure but is increased in
systolic failure. Thus we can eliminate
Choices A, B, and F. Choice E is correct because it indicates a normal LVEDV and a
normal ventricular performance (EF) with an elevated LVEDP. Isolated diastolic
failure may result from hypertrophic or restrictive cardiomyopathy.
(Choice A) This choice characterizes isolated systolic left ventricular failure which
could result from an acute massive myocardial infarction, for example.
(Choices B and C) These choices describe states with systolic left ventricular failure
(reduced EF) and increased diastolic left ventricular compliance.
(Choice D) This option represents a state with both decreased left ventricular
contractile performance (EF) and decreased diastolic left ventricular compliance
indicating a combination of both systolic and diastolic left ventricular failure, which
may be seen in chronic ischemic heart disease.
(Choice F) This choice describes a state with normal left ventricular contractile
function (EF), but increased diastolic left ventricular compliance.
195
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Diastolic heart failure is characterized by normal ventricular contractile performance
(EF) but a decrease in ventricular diastolic compliance. As a result, ventricular enddiastolic pressure (EDP) must be increased to achieve a normal ventricular enddiastolic volume (EDV) and stroke volume. Systolic heart failure is a decrease in
ventricular contractile performance which requires increases of ventricular EDV and
therefore also EDP to achieve a normal stroke volume. In summary, diastolic failure
increases only FDP, whereas systolic failure increases both EDP and FDV.
196
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 12: A 34-year-old female with a recently diagnosed intrasellar microadenoma
presents with recent weight gain, fatigue and hypertension. Plasma ACTH levels are
persistently high on repeated measurements. Which of the following pathologic
changes in the adrenal glands are most likely responsible for this patients
symptoms?
A. Hypertrophy of the glomerular layer of the cortex
B. Hypertrophy of the fasciculate layer of the cortex
C. Hyperplasia of the adrenal medulla
D. Hyperplasia of the fasciculate layer of the cortex
E. Diffuse atrophy of the cortex
Explanation:
The adrenal gland is separated into an outer cortex and an inner medulla. The outer
cortex is further divided into three zones: the zona glomerulosa, the zona
fasciculata, and the zona reticularis. The zona glomerulosa contains cells that
secrete mineralocorticoid hormones (primarily aldosterone). The zona fasciculata is
the broadest of the three zones and contains cells that secrete glucocorticoid
hormones (primarily cortisol). Lastly, the zona reticularis contains cells that secrete
small amounts of androgens.
Individuals who have ACTH-secreting pituitary adenomas gradually develop diffuse
hyperplasia of the adrenocortical zona fasciculata a condition termed Cushings
syndrome. Early in the course of the disease the ACTH causes increased adrenal
blood flow. The conversion of cholesterol to delta-5-pregnenolone (the initial, ratelimiting step in cortisol synthesis) is increased. As time passes, the high levels of
ACTH increase the total RNA and protein synthesis, as well as the amount of DNA
present and the adrenal weight. The enzymes in the steroidogenic pathway are
produced in larger amounts as well.
(Choice A) Hypertrophy of the glomerular layer of the cortex is associated with
Conns syndrome, a condition characterized by increased aldosterone secretion.
(Choice B) While hypertrophy of the fasciculate layer of the cortex may occur to a
limited extent in patients with Cushings syndrome, the primary histologic feature of
this condition is hyperplasia of the zona fasciculata.
(Choice C) Hyperplasia of the adrenal medulla is nota common concern. The
pathology more often observed in the adrenal medulla includes pheochromocytoma
(associated with excessive adrenaline and noradrenaline production) or
neuroblastomas (highly malignant embryonal tumors that present in childhood).
(Choice E) Diffuse atrophy of the cortex is associated with Addisons disease, an
autoimmune condition in which the adrenal glands become markedly atrophic. The
adrenal medulla is spared.
Educational Objective:
Prolonged ACTH stimulation causes hyperplasia of the adrenocortical zona
fasciculata, resulting in excessive cortisol production (Cushings syndrome).
197
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 13: A 24-year-old male who was diagnosed with diabetes two years ago
temporarily loses consciousness after he skipped a meal that was to follow his
insulin injection. His girlfriend administered glucagon immediately, as
instructed by the physician and the patient recovered consciousness in ten
minutes. Metabolic changes in which of the following organs are mostly
responsible for this patients recovery?
Small intestine
B. Liver
C. Pancreas
D. Skeletal muscles
E. Adrenals
F. Adipose tissue
G. Kidney
A.
Explanation:
Glucagon increases serum glucose by increased production of glucose from the liver.
This is achieved by increasing glycogenolysis (breakdown of glycogen) and increase
in gluconeogenesis (production of glucose from non- carbohydrate sources).
(Choice C) Glucagon stimulates insulin secretion from the pancreas. However,
patients with type 1 diabetes typically do not have residual beta cells. Therefore,
glucagon will not have a significant effect on the pancreas of type 1 diabetics.
(Choices D, E and F) Epinephrine increases glucose by multiple mechanisms,
including increased glycogenolysis and gluconeogenesis in the liver. In skeletal
muscle, epinephrine decreases glucose uptake. Epinephrine also causes increased
alanine release from skeletal muscle, which serves as a source of gluconeogenesis in
the liver. In adipose tissue, epinephrine increases the breakdown of triglycerides
thereby increasing free fatty acids and glycerol in the circulation: these can be
utilized as gluconeogenetic substrates as well. Glucagon has insignificant effect on
skeletal muscle cells and adipocytes.
(Choice G) During first 24-hours of fasting the liver is the main organ responsible for
providing glucose. When hypoglycemia is sustained gluconeogenesis in the kidneys
becomes an important source. Glucagon does not have any substantial effect on
gluconeogenesis in the kidneys.
Educational Objective:
Glucagon increases serum glucose by increased production of glucose from the liver.
Glucagon stimulates insulin secretion from the pancreas. However, patients with
type 1 diabetes rarely have significant residual beta cells. Unlike epinephrine,
glucagon has an insignificant effect on skeletal muscle cells and adipocytes.
198
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 14: A 23-year-old Caucasian male is evaluated for bilateral breast
enlargement. He has a tall stature and little body hair. His testicles are
small and Hair. Which of the following findings would you expect most
on laboratory evaluation?
B. Low plasma androstenedione
C. Low plasma estradiol
D. Increased plasma ESH
E. Increased plasma prolactin
A. Low
plasma
TSH
Explanation:
Klinefelter syndrome is characterized by a karyotype with two or more X
chromosomes (47XXY is present in 82% of all cases). It is one of the most common
causes of male hypogonadism, reduced spermatogenesis, and male infertility.
Histologic examination of the test is in these patients reveals some or all of the
testicular tubules to be completely atrophied and replaced by pink hyalinized tissue.
Afflicted individuals demonstrate a distinctive body habitus of an elongated body
with abnormally long legs, small atrophic testes and small penis, and absent
secondary male characteristics (including deep voice, beard, and male pattern pubic
hair). Gynecomastia and a mildly decreased 10 are common. Laboratory findings
include consistent elevation of plasma gonadotropins (primarily follicle-stimulating
hormone) and estradiol, with a reduction in testosterone. The estrogen: testosterone
ratio determines the extent of feminization.
(Choice A) Significant variation in thyroid stimulating hormone levels is nota classic
finding in Klinefelter syndrome.
(Choice B) Significant variation in plasma androstenedione (an intermediate step in
the biochemical synthesis of testosterone or the estrogens estrone and estradiol) is
not a classic finding in Klinefelter syndrome.
(Choice C) Estradiol is elevated, not decreased, in patients with Klinefelter
syndrome.
(Choice E) While elevated prolactin levels can cause gynecomastia, they are not
classically associated with Klinefelter syndrome.
Educational Objective:
Increased plasma follicle-stimulating hormone (ESH) reflects gonadal failure in
patients with Klinefelter syndrome. The estrogen: testosterone ratio determines the
extent of feminization.
199
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 15: A 35-year-old male who works as a nurse in local hospital is brought to
the emergency room with confusion and lethargy. His temperature is 36.7C
(98E), blood pressure is 86/48 mm Hg, pulse is 120/mm, and respirations are
12/mm. Arterial blood gas reveals pH 7.59, pC0249 mmHg and p0285 mmHg.
Which of the following is most useful in diagnosing the cause of this patients
condition?
A. Serum osmolarity
B. Serum sodium
C. Serum ketones
D. Urine glucose
E. Urine chloride
Explanation:
Serum pH greater than 7.40 indicates alkalosis. This acid-base disturbance may
occur due to decreased pCO2 (respiratory alkalosis) or due to a relative increase in
the concentration of HCO3 (metabolic alkalosis). Respirator alkalosis is characterized
by a high pH, a low pCO2 and a compensatory decrease in HCO3. Metabolic alkalosis
is associated with a high pH, a high HCQ3 and a compensatory increase in pCO2.
High pCO2 in association with an increased pH in the patient described in the
question stem is suggestive of metabolic alkalosis. The most common causes of
metabolic alkalosis are:
1. Loss of hydrogen ions from the body: Vomiting and nasogastric suction cause loss
of hydrochloric acid present in gastric secretions. This causes the serum chloride to
decrease leading to a decrease in urinary chloride to less than 10 mEq/L. Such
metabolic alkalosis is called saline-responsive. It is associated with volume loss and
can be corrected by volume repletion with isotonic saline.
2. Thiazide and loop diuretics increase renal losses of Na, which is followed by
excretion of Cl. Reabsorption of HCO3 increases to maintain electric neutrality in the
cells. The volume contraction caused by diuretics stimulates increased aldosterone
secretion, and aldosterone acts to resorb sodium and water from the distal tubule
while wasting potassium and hydrogen in urine. Urinary Cl concentration during
diuretic therapy is increased; however, metabolic alkalosis associated with diuretic
use is chloride-responsive. The overall chloride concentration in the body is low due
to increased renal losses, and administration of saline improves acid-base status.
This is known as contraction alkalosis.
3. The increased aldosterone secretion seen in primary hyperaldosteronism (Conn
syndrome) is also associated with metabolic alkalosis. Aldosterone increases renal
Na reabsorption and urinary losses of K, Cl and H with a relative increase in HCO3
resulting from H losses. The urinary Cl concentration is increased (20 mEq/L) in
these cases, but administration of chloride does not correct the alkalosis (salineresistant metabolic alkalosis). Checking the urine chloride (choice C) and
ascertaining the patients volume status is an important step in the workup of
metabolic alkalosis. (Choices A and B) Serum sodium and osmolarity are useful for
evaluation of hyponatremia.
(Choices C and D) Measurement of urinary and serum glucose and ketones is helpful
for the evaluation of metabolic acidosis.
Educational Objective:
Metabolic alkalosis is characterized by a high arterial blood pH, HCO3 and pCO2. It is
most commonly caused by vomiting, NO suction, diuretic use or hyperaldosteronism.
Measuring the urinary chloride concentration and determining the patients volume
status helps to identify the cause of metabolic alkalosis.
200
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 16: A 6-year-old Caucasian male with recurrent otitis media and sinusitis is
found to have a higher than normal nasal transepithelial potential difference.
Which of the following processes most likely underlies this finding?
A. Increased chloride secretion
B. Increased sodium absorption
C. Intracellular potassium depletion
D. High bicarbonate transport rate
E. High mucus water content
Explanation:
Recurrent otitis media and sinusitis in a young Caucasian should raise suspicion for
cystic fibrosis, as these infections can be caused be the secretion of abnormally thick
mucus by the paranasal sinuses and middle ear epithelium.
The diagnosis of cystic fibrosis (CF) is usually based on high sweat chloride
concentrations, characteristic clinical findings (including sinopulmonary infections)
and/or family history. However, a small portion of patients with CF, especially those
with a mild mutations of the CF transmembrane regulator ion channel (CFTR),
have near-normal sweat tests (sweat chloride <60 Mm/L). In these cases,
measuring the nasal transepithelial potential difference in vivo can be a diagnostic
adjunct. Individuals with CF have a significantly more negative baseline nasal
potential difference than normal, due to abnormalities in ion and water transport in
the apical luminal membrane of exocrine and mucous gland ductal epithelia. The
figure below illustrates these abnormalities, applicable to most exocrine glands, but
not sweat glands. (In sweat glands the tissue-specific effect of the CFTR mutation on
electrolyte transport is different.)
Here we see that the abnormal CFTR reduces ductal epithelial chloride secretion and
increases sodium and water resorption. The result is dehydrated mucus and a
widened transepithelial potential difference.
(Choice C) CFTR mutations do not dramatically alter transmembrane potassium
transport or homeostasis.
201
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice D) CFTR mutations can impair transmembrane bicarbonate conductance and
lower the rate of exocrine duct bicarbonate secretion, promoting mucin precipitation
particularly in pancreatic ducts. A widened transepithelial voltage gradient across the
nasal mucosal epithelium would be more likely to involve increased sodium
absorption than a high rate of bicarbonate transport.
Educational Objective:
In cystic fibrosis abnormalities of the CFTR transmembrane protein (in exocrine
glands other than sweat glands) reduce ductal epithelial chloride secretion and
increase sodium and net water reabsorption, resulting in dehydrated mucus and a
widened transepithelial potential difference.
202
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 17: A 56-year-old Caucasian female presents to your office with recent weight
gain and easy fatigability. Her blood pressure is 160190 mmHg and her heart rate is
80 beats per minute. Her fasting plasma glucose level is 135 mg/dL and her 24-hour
urine cortisol excretion is elevated. Further evaluation reveals that her serum
cortisol is suppressed by high-dose but not low-dose dexamethasone. Her serum
ACTH is borderline elevated. Which of the following is the most likely cause of this
patients problem?
A. Lung cancer
B. Adrenal adenoma
C. Adrenal malignancy
D. Pituitary adenoma
E. Exogenous glucocorticoid intake
Explanation:
This patients clinical presentation is consistent with Cushing syndrome, the
syndrome of glucocorticoid excess. Causes of Cushing syndrome include:
pharmacological doses of exogenous glucocorticoids (commonest cause) ACTHsecreting pituitary adenoma, ectopic production of ACTH or CRH, primary
adrenocortical hyperplasia or adrenocortical adenoma. Of these only pituitary
adenoma and ectopic ACTH syndrome will have elevated ACTH. The other causes will
have suppressed serum ACTH levels. Cushing syndrome that results from an ACTH
secreting pituitary microadenoma is termed Cushings disease.
The screening tests for endogenous Gushing syndrome include overnight low-dose
dexamethasone suppression test and 24-hour urine free cortisol. Administration of
dexamethasone, a potent glucocorticoid, should suppress AGTH and cortisol levels in
normal individuals. However, patients with endogenous Cushing syndrome do not
suppress serum cortisol levels following administration of low-dose dexamethasone.
Typically, in patients with Cushings disease cortisol levels do not suppress with lowdose dexamethasone but do suppress with high-dose dexamethasone. This test is
useful in differentiating Cushings disease from Cushing syndrome caused by ectopic
ACTH production. When there is an ectopic source of ACTH, ACTH levels are typically
markedly elevated, and there is no suppression of ACTH or cortisol with even highdose dexamethasone.
(Choice A) Ectopic ACTH production may be seen with small cell lung cancer. Serum
ACTH levels are generally markedly elevated in ectopic ACTH secretion by malignant
tumors. High-dose dexamethasone suppression test does not suppress cortisol or
AGTH levels.
(Choices B, C and E) Adrenal adenoma and carcinoma will have low ACTH levels in
combination with the clinical features of Cushing syndrome. The case described has
slightly elevated ACTH levels, making adrenal adenoma and adrenal cancer unlikely.
Serum ACTH is also low in exogenous glucocorticoid-induced Cushing syndrome.
Educational Objective:
Adrenal adenoma and carcinoma will have low levels of ACTH in combination with
the clinical features of Gushing syndrome. AGTH levels are elevated in pituitary
adenomas, and are suppressed by high-dose, but not low-dose, dexamethasone.
Serum ACTH levels are generally markedly elevated in ectopic ACTH production by
malignant tumors: even high-dose dexamethasone does not suppress these levels.
203
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 18: Atherosclerotic lesions of coronary artery limit the potential for increase in
blood flow to the myocardium. Some preparations can cause coronary steal
phenomenon due to redistribution of blood flow. Which of the following effects of a
drug is most likely to be associated with the coronary steal phenomenon?
A. Epicardial vessel dilation
B. Coronary microvessel dilation
C. Capacitance vessel dilation
D. Arterial dilation
E. Mixed arterial and venous dilation
Explanation:
In coronary artery disease, coronary vessel occlusion can be bypassed by the natural
existence and compensatory recruitment of coronary collateral vessels to help
support blood flow. These collateral microvessels are a network of arterioles that
form passageways to major vessels and can supplement blood flow to the
myocardium distal to occluded vessels. In the event of myocardial ischemia,
collateral microvessels vasodilate and increase collateral blood flow, diverting blood
to ischemic areas. This collateral circulation helps to alleviate ischemia and preserve
myocardial function.
Drugs like adenosine and dipyridamole are selective vasodilators of coronary
vessels. Consequently, these agents are often employed in myocardial perfusion
imaging studies. In certain conditions, these agents may cause redistribution of
blood flow through coronary microvessels or arterioles, possibly reversing collateral
blood flow. Vessels within ischemic areas are often maximally dilated and
administration of these agents can lead to selective vasodilation of vessels in nonischemic regions. Decreased pressure and vasodilation of collateral microvessels
may then divert blood flow from ischemic areas to non-ischemic areas. This
phenomenon, known as coronary steal, decreases blood flow to ischemic areas and
may lead to hypoperfusion and potentially worsen existing ischemia.
(Choice A) The epicardial vessels refer to the large coronary arteries of the heart and
include the right coronary left main, left anterior descending, and circumflex
arteries. (Choice C) Capacitance vessels or veins are the main blood vessels that
return blood to the heart. They have significant storage capacity and serve as low
resistance reservoirs. Veno dilation decreases ventricular volume and allows for a
reduction in myocardial oxygen demand secondary to decreased wall tension. Drugs
that cause capacitance vessel dilation will have beneficial effects in coronary heart
disease. Veno dilation does not normally cause coronary steal.
(Choice D) Systemic arterial vasodilation decreases arterial pressure and allows for a
reduction in myocardial oxygen demand by decreasing wall tension.
(Choice E) Mixed arterial and venous dilation decreases wall tension by reducing
arterial pressure and ventricular volume, respectively. The combined effects help to
decrease myocardial oxygen demand and are very effective in treating coronary
heart disease.
Educational Objective: Collateral microvessels are arterioles that form adjacent
pathways for blood flow to areas that are distal to occluded vessels. Vasodilators like
adenosine and dipyridamole are selective vasodilators of coronary vessels that are
often used in myocardial perfusion imaging studies. In coronary steal, blood flow is
redistributed from ischemic areas to non-ischemic areas through vasodilate collateral
microvessels. Coronary steal can lead to hypoperfusion and worsen ischemia in the
occluded artery.
204
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 19: A 65-year-old Caucasian male presents to the ER with sudden onset of
right-sided calf and foot pain. His past medical history is significant for
hypertension, type II diabetes mellitus, atrial fibrillation and stable angina.
Physical examination reveals paleness of the right leg and diminished right
popliteal pulse. Immediate angiography is ordered that reveals an obstructive
thrombus in the right common femoral artery. The thrombus extraction is
followed by a rapid surge of serum creatine kinase level, which is best explained
by:
A. Cellular swelling
B. Cell membrane damage
C. Glutathione peroxidase production
D. Mitochondrial vacuolization
E. Nuclear shrinkage
Explanation:
Ischemia is characterized by the reduction of blood flow, usually as a result of
mechanical obstruction within the arterial system (eg, thrombus). If the flow of
blood to the ischemic tissue is restored in a timely manner those cells that were
reversibly injured will typically recover. Sometimes however, the cells within the
damaged tissue will paradoxically die at an accelerated pace through apoptosis or
necrosis after resumption of blood flow. This process is termed reperfusion injury,
and is thought to occur secondary to one or more of the following mechanisms: 1)
oxygen free radical generation by parenchymal cells endothelial cells, and
leukocytes; 2) severe irreversible mitochondrial damage described as mitochondrial
permeability transition; 3) inflammation which attracts circulating neutrophils that
cause additional injury; and 4) activation of the complement pathway. Causing cell
injury and further inflammation. When the cells within heart, brain, or skeletal
muscle are injured the enzyme creatine kinase leaks across the damaged cell
membrane and into circulation (as seen in this patient).
(Choice A) Cellular swelling arises secondary to changes in ion concentration and the
influx of water. This state is considered a hallmark of reversible injury, and is not
directly associated with the leakage of intracellular proteins such as creatine kinase.
(Choice C) Glutathione peroxidase actually reduces cellular injury by catalyzing free
radical breakdown. The presence of this enzyme is not responsible for the release of
creatine kinase.
(Choice D) Mitochondrial vacuolization reduces the cellular capacity for ATP
generation and is associated with irreversible injury. Creatine kinase release is not
directly associated with this mitochondrial change however.
(Choice E) Nuclear shrinkage (pyknosis), fragmentation and dissolution characterize
irreversible injury of the cell. Creatine kinase release is not directly associated with
such nuclear changes however.
Educational Objective:
Reperfusion injury is thought to occur secondary to oxygen free radical generation
mitochondrial damage and inflammation.
205
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 20: A 72-year-old Caucasian male who was diagnosed with severe aortic
stenosis six months ago presents to the ER with acute pulmonary edema. His
blood pressure is 90/60 mmHg and his heart rate is 130 beats per minute with
a rhythm that is irregularly irregular. EGG shows atrial fibrillation without
significant ST-segment or T-wave changes. Which of the following
hemodynamic changes most likely contributed to this patients condition?
Sudden increase of left ventricular after load
B. Sudden increase in left ventricular filling
C. Sudden decrease of left ventricular preload
D. Sudden decrease in left ventricular contractility
E. Insidious right ventricular hypertrophy
A.
Explanation:
Acute atrial fibrillation most likely precipitated the sudden onset of heart failure in
this patient. Atrial fibrillation occurs in up to 1O% of patients with severe aortic
stenosis (AS). Patients with severe AS may already have a reduced cardiac output.
The sudden loss of the contribution of normal atrial contraction to ventricular filling
(loss of the atrial systolic kick) decreases left ventricular (LV) preload (end diastolic
volume) which can further reduce cardiac output and produce severe hypotension.
Additionally, many patients with chronic AS have concentric LV hypertrophy and
therefore reduced left ventricular (LV) compliance. Loss of the atrial kick in these
patients may mean that a significant increase in mean pulmonary venous pressure is
required to maintain the new steady state LV preload. The result may be acute
pulmonary edema in addition to hypotension as occurred in this patient. Because of
these dangers, cardioversion is indicated for acute atrial fibrillation in patients with
severe chronic AS.
(Choice A) An acute increase in left ventricular (LV) afterload (mean systolic
intraventricular pressure) would be unlikely in a patient with degenerative aortic
valve calcification. An increased LV afterload in the setting of reduced mean arterial
pressure would have to result from an acute increase in resistance across the aortic
valve, whereas in degenerative calcific AS and most other forms of adult AS, the
transvalvular obstruction gradually increases over years to decades.
(Choices B and D) Since this patient has no evidence of myocardial ischemia on
ECGI we may assume that myocardial contractility is roughly unchanged. We may
also assume that the degree of aortic stenosis is relatively fixed. Under these
circumstances an increase in LV preload would increase net cardiac output
(according to the Frank-Starling curve relating preload and stroke volume). Since
there is also no reason to suspect any acute change in total peripheral resistance in
this patient an increase in cardiac output would increase mean arterial pressure not
decrease it as was the case here.
In order for there to be a sudden increase in left ventricular (LV) preload (end
diastolic volume) there would have to be: a sudden increase in mean left atrial
pressure without any change in mitral valve resistance a sudden decrease in mitral
valve stenosis an acute increase in LV compliance an acute decrease in LV
contractility, and/or a sudden increase in aortic valve regurgitation.
(Choice E) As the word insidious implies right ventricular hypertrophy (RVH)
develops gradually in response to pulmonic outflow tract obstruction pulmonary
hypertension or RV volume overload. RVH is not an acute hemodynamic change
rather it is a cardiac structural adaptation to chronic hemodynamic changes. Thus,
RVH is rarely responsible for acute symptoms or signs.
Educational Objective:
206
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
In patients with chronic aortic stenosis (AS) and concentric left ventricular
hypertrophy:
1. the loss of the contribution of atrial contraction to ventricular filling that occurs
with acute atrial fibrillation (AF) can reduce left ventricular preload and cardiac
output sufficiently to result in dangerous systemic hypotension, and
2. Acute AF might also increase steady state pulmonary venous pressures
sufficiently to cause acute pulmonary edema.
207
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 21: A 34-year-old Caucasian male comes to your office with a 3-month
history of impotence. Physical examination reveals bitemporal visual Held
deficit. Lab results show elevated serum prolactin. Which of the following
changes in gonadotropin-releasing hormone (GnRH), luteinizing hormone
(LH) and testosterone are most likely responsible for this patients
symptoms?
GnRH
LH
Testosterone
A.
Decreased
Decreased
Decreased
B.
Increased
Decreased
Decreased
C.
Increased
Increased
Decreased
D.
Increased
Increased
Increased
E.
Decreased
Increased
Decreased
Explanation:
Bitemporal hemianopsia is a buzzword symptom for a pituitary tumor.
Approximately 60% of functional (secreting) pituitary tumors are prolactinomas.
Prolactin is a 199 amino acid peptide secreted by the lactotroph cells of the pituitary.
Prolactin is responsible for milk production and lactation in postpartum women. The
role of prolactin in males is not completely understood. Scientists do know, however,
that increased serum levels of prolactin in men or women, from any cause, suppress
GnRH.
GnRH stimulates the release of LH from the pituitary, which stimulates testosterone
production; consequently, suppression of GnRH causes decreased LH and decreased
testosterone. Prolactinomas in males generally have a delayed diagnosis for a few
reasons; men with prolactinomas do not experience galactorrhea or amenorrhea,
and men are often reluctant to report erectile dysfunction. Henceforth,
prolactinomas in men are typically much larger at the time of presentation than in
women. We know that this particular patient has a large prolactinoma because itis
compressing the optic chiasm, as demonstrated by bitemporal hemianopsia.
Prolactinomas in females of reproductive age typically cause galactorrhea,
amenorrhea, and infertility. Postmenopausal women with prolactinomas are already
amenorrheic and infertile, so they present mainly with headaches and visual field
defects.
(Choices B, C, and D) The choices with increased GnRH levels are incorrect because
prolactinomas suppress GnRH production. We can be confident that this patient has
a prolactinoma because his serum prolactin level is high, and he has bitemporal
hemianopsia.
(Choice E) The suppression of GnRH in patients with prolactinomas causes a
decrease in LH and testosterone; therefore, Choice E is incorrect.
Educational Objective:
Anytime a patient has bitemporal hemianopsia, a pituitary tumor should be
suspected. The most common functional pituitary tumor is a prolactinoma. Secreting
prolactinomas inhibit the entire axis of GnRHLH/ESHsex hormones, causing
impotence in men and amenorrhea in women of reproductive age (hypogonadotropic
amenorrhea).
208
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 22: In experimental studies the mechanisms of opioid tolerance are
investigated. It is shown that ketamine can block tolerance development
to morphine. Which of the following neurotransmitter actions is most
likely modulated to achieve the effect described above?
Glutamate
C. Acetylcholine
D. Norepinephrine
E. Serotonin
A.
Glycine
B.
Explanation:
The use of opioids can lead to the development of tolerance or a decrease in opioid
effectiveness and physiological response with continued use. The mechanism for
acute opioid tolerance is still uncertain but is postulated to involve phosphorylation
of opioid receptors by protein kinase. Chronic tolerance may involve increased
adenylyl cyclase activity or nitric oxide levels.
In the case of morphine, the neurotransmitter glutamate has also been shown to
interact with opioid pathways to modulate morphine tolerance. Glutamate is an
excitatory neurotransmitter that binds and activates NMDA receptors. NMDA
receptor activation can cause increased phosphorylation of opioid receptors and
increased nitric oxide levels which ultimately leads to morphine tolerance. In animal
studies, NMDA receptor antagonists, like ketamine, block the actions of glutamate
and effectively block morphine tolerance. Additionally, dextromethorphan has also
been shown to reverse opioid tolerance through its NMDA antagonistic properties.
Thus it appears that glutamate may play a significant role in morphine tolerance.
(Choice A) Glycine is a co-agonist for glutamate and is required for the binding of
glutamate to NMDA receptors. Binding of both glutamate and glycine is necessary
for activation of NMDA receptors. Although glycine is necessary for glutamate
binding, it plays no significant role in modulating morphine tolerance.
(Choice C) Acetycholine is a neurotransmitter that functions in both the peripheral
and central nervous system. It binds to both nicotinic and muscarinic receptors to
produce proper nervous system and muscle function. It plays no role in modulating
morphine tolerance.
(Choice D) Norepinephrine is both a hormone released from the adrenal glands and
a neurotransmitter released from noradrenergic neurons. As a hormone, it mainly
acts to work on attention and impulsivity. As a neurotransmitter, it mainly functions
at postganglionic neurons to activate the sympathetic nervous system. Although
norepinephrine dysregulation may have a role in neuropathic pain, it has no role in
modulating morphine tolerance.
(Choice E) Serotonin is a monoamine neurotransmitter synthesized and released
from serotonergic neurons located in the central nervous system and the
gastrointestinal system. Although dysregulation of serotonin may play a role in
neuropathic pain, it is not involved in modulating morphine tolerance.
Educational Objective:
Morphine tolerance is a common problem in the treatment of pain. The exact
mechanism of tolerance is unknown buy may involve increased phosphorylation of
opioid receptors, increased adenylyl cyclase activity, or increased nitric oxide levels.
Activation of NMDA receptors by glutamate is believed to enhance morphine
tolerance by increasing phosphorylation of opioid receptors and increasing nitric
oxide levels. NMDA receptor blockers, like ketamine, block the actions of glutamate
and effectively decrease morphine tolerance.
209
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 23: Serum from patient A seems impairs elastin degradation by neutrophil
products in vitro whereas serum from patient B does not have that ability.
Patient B should be strongly warned to avoid:
Phenylalanine-containing food
B. High-fat diet
C. Smoking
D. Iron-containing pills
E. Strenuous physical activity
F. Direct sunlight exposure
A.
Explanation:
Neutrophil elastase is the major protease of extracellular elastin degradation. It is
released by neutrophils and macrophages. The major serum inhibitor of extracellular
elastase is alpha-antitrypsin (al-AT). Patient B likely has al-AT deficiency, a condition
associated with panacinar emphysema and liver cirrhosis. Panacinar emphysema
results from the unopposed action of neutrophil elastase on alveolar walls. Smoking
dramatically increases the risk of panacinar emphysema in patients with al-AT
deficiency. This may be because oxidant products of smoke (including free radicals)
can inactivate endogenous al-AT, producing a functional l-AT deficiency as well.
Smoking also enhances elastase activity in macrophages and macrophage elastase
(unlike neutrophil derived elastase) is not inhibited by al-antitrypsin.
(Choice A) A phenylalanine-restricted diet is given to patients with phenylketonuria
due to a deficiency of the enzyme phenylalanine hydroxylase.
(Choice B) High fat diets have been variably associated with obesity and
nonalcoholic fatty liver disease. Dietary fat is not known to affect the development of
emphysema or hepatic cirrhosis that may result from al-antitrypsin deficiency.
(Choice D) Avoidance of excess dietary iron would be important in conditions
associated with systemic iron overload such as hemochromatosis or anemias (e.g.
thalassemias) requiring chronic transfusion protocols.
(Choice E) Strenuous physical activity would not be contraindicated in such a patient
unless the patient had already developed severe panacinar emphysema and/or
cirrhosis associated with this antiprotease deficiency.
(Choice F) Avoidance of sunlight might be indicated in a patient with a
photodermatosis such as cutaneous porphyria or lupus photosensitivity.
Educational Objective:
In patients with an al-antitrypsin deficiency, smoking dramatically increases the risk
of developing panacinar emphysema.
210
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 24: A protein isolated from the granules of the cell shown on the slide below
is believed to cause damage to the bronchial epithelium in patients with atopic
asthma. Which of the following is a known function of this protein?
A. Kills viruses
B. Opsonizes bacteria
C. Kills helminths
D. Inhibits fungal growth
E. Stimulates fibroblasts
Explanation:
The cell shown has a bibbed nucleus and is packed with large granules of relatively
uniform size. We are told that these granules contain a protein capable of damaging
the respiratory epithelium in atopic asthma. The late phase of an atopic asthma
attack involves mucosal infiltration by eosinophils, basophils, and neutrophils.
Neutrophil proteases could theoretically damage epithelial cells, but neutrophils tend
to have multilobed nuclei. Basophil granules contain heparin, histamine, and SRS-A
(slow reacting substance of anaphylaxis, a mixture of leukotrienes), which would be
unlikely to cause direct damage to epithelial cells. Thus the cell shown is most likely
an eosinophil. Eosinophils release major basic protein, a potent anthelminthic toxin
that is capable of causing damage to epithelial and endothelial cells.
(Choice A) Natural killer cells kill viruses.
(Choice B) Major basic protein is an antiparasitic cytotoxin. It is not known to play a
role in the opsonization of bacteria.
(Choice D) Major basic protein attaches to and disrupts the outer membrane of
helminths. It is not known to have an antifungal action.
(Choice E) Major basic protein is an antiparasitic cytotoxin not known to directly
stimulate fibroplasia or fibrogenesis.
Educational Objective:
Major basic protein released by eosinophils normally functions to kill helminths. It is
also thought to contribute to the bronchial epithelial damage sustained by patients
with atopic (extrinsic allergic) asthma.
211
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 25: A 35-year-old Caucasian female comes to your office complaining of
excessive thirst and frequent urination. Her blood glucose level is 86 mg/dL.
You proceed with the standard water deprivation test in this patient. The
results of urine osmolality (in mOsm/L) during 4 hours of dehydration are
presented below.
1 hour
2 hour
3 hour
4 hour
150
160
160
550
* 5 units of vasopressin administered
Which of the following is the most likely diagnosis in this patient?
Primary polydipsia
B. Complete central diabetes insipidus
C. Partial central diabetes insipidus
D. Nephrogenic diabetes insipidus
E. Post obstructive polyuria
A.
Explanation:
Vasopressin or antidiuretic hormone (ADH)I is responsible for the maintenance of
water balance by regulating water absorption in the kidney. Without ADH, the
kidneys collecting duct cells are impermeable to water causing water to be lost to
the body via urine. When ADH is present however water is free to osmotically move
across the collecting duct cells.
ADH activates G protein-coupled V2 receptors which allow the transposition of
aquaporin 2 from their intracellular locations to the luminal cell membrane. At the
cell membrane aquaporin lives up to its name by serving as a water channel a pore
that water passes through.
Diabetes insipidus (Dl) is a disease of this water balance system. Patients with Dl
pass very watery (dilute) urine making them dehydrated. Because they are
dehydrated these patients are also always thirsty. Dl can be partial or complete and
is caused by one of two mechanismsdeficiency of ADH called central Dl; or
resistance to ADHs action on the kidneys called nephrogenic Dl. In patients with
suspected Dl, a water deprivation is performed. This testis usually done in a hospital
setting under close observation. Bodyweight, blood pressure heart rate, urine and
plasma osmolality, urine volume, and serum sodium are monitored closely. When
two consecutive urine samples show very little change in urine osmolality(<30
mOsm/kg), five units of aqueous vasopressin are given subcutaneously. One hour
after injection, the aforementioned values (bodyweight, blood pressure etc.) are
measured again.
This vasopressin injection differentiates between central and nephrogenic Dl. If
following the injection the urine osmolality changes less than 10%, nephrogenic Dl is
diagnosed. This scant response to exogenous vasopressin makes perfect sense
because patients with nephrogenic Dl already produce enough vasopressin but their
kidneys do not respond to the hormone properly. In fact, sometimes levels of
vasopressin are drawn in patients with suspected Dl. Normal-to-elevated levels
indicate nephrogenic Dl, whereas low levels demonstrate central Dl.
Since central Dl is caused by lack of vasopressin one can expect a more robust
response to its administration. If urine osmolality increases by 10% or more central
Dl is the diagnosis. Furthermore, in patients with complete central Dl, the rise in
urine osmolality is typically more than 50%. This particular patient had a robust
response indicating that she has complete central Dl. A more moderate response
would indicate partial central Dl, which means that some vasopressin is present but
not enough to allow normal kidney function.
212
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice A) Primary polydipsiaalso called psychogenic polydipsiais simply
excessive consumption of water. The patients urine will be dilute (have a low urine
osmolality) because the body is trying to get rid of the excess water. Water
deprivation will result in a reliable increase in urine osmolality, and vasopressin
administration will not alter test results significantly. Primary polydipsia is a
psychological illness; excessive thirst will not have a medical cause. Classically, it is
seen in female patients with overt mental illness. Children sometimes present with
this disorder as well.
(Choice E) Post obstructive polyuria is increased urinary output after surgical (Foley
catheter) relief from some sort of urinary obstruction. Suspect it in a patient who
has had recently relieved bilateral ureteral or subvesical obstruction. Patients
exhibiting this phenomenon will show a normal response to water deprivation.
Educational Objective:
More than a 10% increase in urine osmolality following administration of vasopressin
during a water deprivation test suggests central Dl. A urine osmolality increase
above 50% is strongly suggestive of complete central Dl.
213
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 26: A thrombus originating in the deep veins of the lower extremities is most
likely to cause a stroke in a patient with which of the following physical findings?
A. Splitting of S1 that is accentuated on inspiration
B. Ejection-type systolic murmur that increases on standing
C. Diastolic decrescendo-type murmur that decreases following amyl nitrite
inhalation
D. Presystolic murmur that disappears with atrial fibrillation
E. Splitting of S2 that does not change with respiration
Explanation:
A patent connection between the right and left atria is a defect that would make a
paradoxical embolism possible. Paradoxical emboli originate in the venous system,
but cross over into the arterial circulation (bypassing the lungs) via an abnormal
connection between the right and left heart. Wide splitting of S2 that does not vary
with respiration can result from an atrial septal defect (ASD) a defect that would
permit a paradoxical embolism.
(Choice A) Assuming the patient had no S4 gallops or aortic ejection click, a split S1
accentuated on inspiration would indicate delayed closure of the tricuspid valve. This
could be caused by a right bundle branch block and need not indicate any abnormal
connection between the right and left cardiac chambers.
(Choice B) A systolic ejection murmur (SEM) generally refers to a mid-systolic
crescendo-decrescendo murmur, most commonly the result of aortic stenosis.
Hypertrophic obstructive cardiomyopathy may also cause SEM. When in the upright
position, venous return to the heart is decreased and the left ventricular enddiastolic volume and stroke volume are reduced, increasing the SEM of hypertrophic
obstructive cardiomyopathy. Neither of these lesions by themselves would permit a
paradoxical embolus.
(Choice C) An early diastolic decrescendo murmur is characteristic of aortic
regurgitation (AR). Inhaled amyl nitrite produces marked vasodilatation, resulting in
reduction of systemic arterial pressure and decreasing this regurgitant murmur.
Isolated AR does not result in an abnormal right-to-left heart connection that would
permit paradoxical embolism.
(Choice D) Presystolic accentuation occurs when the intensity of a diastolic
murmur becomes louder just prior to S1 or when a diastolic murmur appears just
prior to S1. A presystolic (late diastolic) murmur can result from mitral or tricuspid
valve stenosis and/or physiologically increased blood flow across these valves.
Presystolic accentuation occurs due to atrial contraction. Atrial fibrillation could
eliminate an atrioventricular valve stenotic murmur by removing the atrial
contraction during late diastole. However, tricuspid and/or mitral stenosis alone
would not permit a paradoxical embolus.
Educational Objective:
Paradoxical thromboembolism occurs when a blood clot from the venous system
crosses directly into the arterial circulation via an abnormal connection between
right and left cardiac chambers, such as an ASD or ventricular septal defect.
Auscultatory findings in an ASD include a wide and fixed splitting of S2. Additional
associations between auscultatory findings and cardiac lesions are as follows:
1. Systolic ejection murmur accentuated by standing: hypertrophic obstructive
cardiomyopathy
2. Early diastolic decrescendo murmur decreased by amyl nitrite: aortic regurgitation
3. Late diastolic murmur eliminated by atrial fibrillation: mitral (and/or tricuspid)
stenosis
214
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 27: A 32-year-old homeless male presents to the FR with severe chest pain
when he swallows food. He has been hospitalized several times recently with
pneumocystic pneumonia (PCP). Endoscopic findings include hyperemia and
ulcerations of esophageal mucosa. This patients condition is most likely caused
by which of the following organisms?
A. Cytomegalovirus
B. Babesia divergens
C. Toxoplasma gondii
D. Isospore belli
E. Herpes zoster
F. Trypanosoma cruzi
D. Cryptococcosis
Explanation:
This homeless patient is most likely HI V-infected as Pneumocystis carinii affects
exclusively immunocompromised individuals. Now, the patient presents with painful
swallowing, which is a characteristic symptom of esophagitis.
There are three main causes of HI V-associated esophagitis: Candida,
Cytomegalovirus, and Herpes virus. Clinically it is not possible to distinguish which of
the three is present as all cause dysphagia (difficulty swallowing) and/or
odynophagia (pain on swallowing). Accurate diagnosis, however, is essential for
treatment of these patients. Endoscopic and microscopic criteria are given in the
table below.
(Choice B) Babesia divergens is transmitted by a tick bite and causes babesiosis. It
is endemic in the northeastern United States and manifests with influenza-like
symptoms hepatosplenomegaly, and anemia. It often affects asplenic patients.
(Choice C) In HI V-positive patients Toxoplasma causes ring-enhancing brain lesions
and chorioretinitis.
(Choice D) Isospore belli causes profuse, watery diarrhea in HIV patients. It doesnt
play any role in the development of esophagitis.
(Choice E) Herpes simplex, not herpes zoster causes esophagitis in HIV patients.
(Choice F) Trypanosome cruzi causes Chagas disease (American Trypanosomiasis).
Chronic disease leads to cardiomyopathy, achalasia, megacolon, and megaureter.
(Choice C) Cryptococcosis causes meningitis in HIV patients, but not esophagitis.
Educational Objective:
Infectious esophagitis is common in HI V-positive patients. The most common cause
is Candida albicans, although CMV and HSV-1 are also frequently implicated.
Diagnosis relies on endoscopic and microscopic findings.
215
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 28: Esophageal manometric studies performed on a 38-year-old Caucasian
male demonstrate periodic non-peristaltic contractions of a large amplitude and
long duration. Clinical manifestations of this patients condition would most
closely mimic which of the following?
A. Esophageal cancer
B. Gastroesophageal reflux disease
C. Duodenal ulcer
D. Angina pectoris
E. Pulmonary infarction
F. Acute cholecystitis
Explanation:
Periodic non-peristaltic contractions of the esophagus describe diffuse esophageal
spasm (DES). Normally, esophageal muscle contractions are coordinated.
Contractions are normally stimulated by esophageal distention by a food bolus; the
contractions originate above the site of distention and propel the bolus downwards.
In DES, several segments of the esophagus contract at the same time which
prevents the propagation of the food bolus towards the stomach. Additionally, these
involuntary muscle contractions can be painful. Esophageal manometry studies show
disorganized non-peristaltic contractions of the body of esophagus. Simultaneous
contractions cause a so-called corkscrew esophagus, as seen on barium
esophagogram.
Symptoms of DES are intermittent dysphagia and occasional chest pain. In typical
cases, the chest pain is not associated with exertion and is not relieved by rest.
Sometimes, however, the pain may mimic unstable angina in intensity and location.
Complete cardiac work-up should be considered in every patient suspected of having
DES to rule out a cardiac cause of chest pain.
(Choice A) Esophageal cancer causes progressive dysphagia first to solids, later to
both solids and liquids. Eventually, patients are unable to eat.
(Choice B) The most common symptom of gastroesophageal reflux disease (GERD)
is heartburn. This burning, central pain most frequently occurs after a meal or at
night. Patients describe DES pain as crampy, not burning.
(Choice C) Duodenal ulcers cause epigastric pain that usually occurs 1-3 hours after
a meal or at night. Duodenal ulcer pain is relieved by intake of food or antacids,
unlike DES pain.
(Choice E) Chest pain from a pulmonary embolism is pleuritic (associated with deep
breathing) and is often associated with dyspnea, cough, and hemoptysis.
(Choice F) Pain from acute cholecystitis is localized to the right upper quadrant of
the abdomen. This pain can radiate to the back or the neck. Cholecystitis is often
triggered by a large meal and maybe accompanied by fever, nausea, and vomiting.
Educational Objective:
Diffuse esophageal spasm (DES) occurs due to uncoordinated contractions of the
esophagus. These contractions are both inefficient in propelling food into the
stomach and may cause symptoms of dysphagia and chest pain. This chest pain may
mimic unstable angina: thus, complete cardiac work-up should be considered in
every patient suspected of having DES, so that a cardiac cause may be ruled out.
216
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 29: A 34-year-old Caucasian male presents to the emergency department
with recent-onset dyspnea and fatigue. There is no significant past medical histo
except for a mild respiratory illness one week ago. His blood pressure is 80/60
mmHg. His pulse is 120 beats per minute, regular, but weak. The pulse
becomes undetectable to palpation during each inspiration. The jugular veins
are distended. The lungs are clear to auscultation. Which of the following do you
most suspect in this patient?
Acute fibrinous pericarditis
B. Acute myocardial infarction
C. Septic shock
D. Constrictive pericarditis
E. Cardiac tamponade
F. Tension pneumothorax
A.
Explanation:
The physical finding of jugular venous distension (JVD) is key here. JVD indicates
that there is elevation of the central venous pressure (CVP) in the superior vena
cava. The combination of acute-onset CVP elevation (>15cm H2O) with hypotension
and tachycardia can occur with cardiac tamponade or tension neumothorax. Because
there is no history of chest trauma and no abnormalities on lung auscultation,
tension pneumothorax is unlikely. Given the history of an antecedent respiratory
illness, the most likely diagnosis is cardiac tamponade due to a serous viral
pericarditis and a significant acute pericardial effusion.
Observation of Becks triad on physical examination hypotension, distended neck
veins, and distant or muffled heart sounds on auscultation as well as tachycardia,
are together indicative of tamponade. A rising CVP in a hypotensive patient signifies
that normal compensatory mechanisms are unable to maintain an adequate cardiac
output. Low cardiac output and its associated hypoxemia likely explain the patients
dyspnea and fatigue. The loss of a palpable pulse during inspiration is most likely
due to an inspiratory fall in systolic blood pressure. Pulsus paradoxus, or a drop in
systolic blood pressure of >10 mmHg on inspiration, is a non-specific sign, but is
suggestive of tamponade when coupled with acute onset hypotension, tachycardia,
and JVD.
(Choice A) Acute fibrinous pericarditis may follow an upper respiratory infection, but
would only be expected to cause pleuritic chest pain and a pericardial friction rub. In
contrast, the patient in this vignette has signs and symptoms of significant
pericardial effusion and cardiac tamponade.
(Choice B) A myocardial infarction resulting in a degree of cardiogenic shock could
produce the findings of hypotension, tachycardia jugular venous distension, and
weak pulses. However, there would likely also be pulmonary edema producing rales
on lung auscultation. Moreover, myocardial infarction would be quite unusual in a
34-year-old patient. Finally, ventricular contractile dysfunction and congestive failure
would not necessarily cause a significant drop in systolic blood pressure on
inspiration (pulsus paradoxus).
(Choice C) The initial stage of septic shock is a hyperdynamic circulatory state with a
lowered systemic vascular resistance and an increased cardiac output (warm shock).
Weak pulses and pulsus paradoxus would not be found.
(Choice D) Constrictive pericarditis is a chronic process that requires months to
years to produce constriction sufficient to cause tamponade. This patients signs and
symptoms occurred much more acutely.
217
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Cardiac (or pericardial) tamponade presents clinically with hypotension, tachycardia,
and an elevated central venous pressure that produces jugular venous distension
(JVD). Heart sounds may be muffled on cardiac auscultation and systolic blood
pressure may drop more than 10 mmHg on inspiration (pulsus paradoxus).
218
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 30: A 45-year-old Caucasian female is hospitalized with exertional dyspnea
and fatigue. She recently emigrated from Eastern Europe and has no significant
past medical history. Her blood pressure is 110/80 mmHg and her heart rate is
90 beats per minute and regular. You suspect mitral stenosis. Which of the
following is the best indicator of the severity of stenosis?
A. Diastolic murmur intensity
B. Presystolic accentuation of the murmur
C. S2-to-opening snap time interval
D. Audible S3
E. Audible S4
Explanation:
The best auscultatory indicator of the severity of mitral stenosis (MS) is the length of
the interval between A2 and the opening snap (OS). The shorter the interval the
more severe the stenosis. The OS occurs due to tensing of the mitral valve (MV)
leaflets after the valve cusps have completed their opening excursion. The more
thickened and fibrotic the MV the earlier this tensing occurs. The A2-OS interval is
also inversely correlated with mean diastolic left atrial pressure. (In modern practice
the standard for the diagnosis and determination of MS severity is measurement of
mean transvalvular pressure gradients via 2-D Doppler echocardiography).
(Choice A) Although the intensity of the diastolic rumble of mitral stenosis (MS) may
increase as the degree of MS increases this sign is a less reliable indicator of MS
severity. This is because the transmission of the flow murmur at a given
transvalvular pressure gradient varies among patients depending upon thoracic
anatomy. The diastolic rumble is heard best at the cardiac apex (mitral area) with
the bell of a stethoscope.
(Choice B) There is presystolic accentuation of the murmur of mitral stenosis (MS)
because of the increased transvalvular flow associated with left atrial contraction.
This accentuation is heard across a range of MS severity. More significant than the
degree of presystolic accentuation is its presence or absence. When MS becomes
severe enough to precipitate atrial fibrillation, presystolic accentuation of the MS
murmur disappears.
(Choices D and E) Left-sided SS and/or S4 gallops are generally absent in mitral
stenosis (MS), since left ventricular filling is subnormal to normal. When MS is
severe enough to produce pulmonary hypertension, patients may develop rightsided heart failure, with dilatation of the right ventricle (RV) and its annulus and
possible secondary tricuspid or pulmonic regurgitation. Tricuspid and pulmonic
regurgitation might cause a right-sided S3 and/or S4. However these EN gallops
would only arise when the maximal degree of MS had been reached and thus are
poor indicators of the severity of less serious MS.
Educational Objective:
The best, most reliable and most continuous auscultatory indicator of the severity of
mitral stenosis is the A2-OS interval. The shorter this interval the more severe the
stenosis. Other auscultatory findings that may accompany MS include a diastolic
rumble (intensity varies depending on patient anatomy) and pre-systolic
accentuation due to left atrial contraction. A right-sided S3 and/or S4 might arise
with end-stage MS critical enough to produce severe pulmonary hypertension.
219
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 31: A 20-year-old female presents to the ER with extreme weakness,
abdominal pain, and nausea. For the past few weeks, she has had polyuria
and excessive thirst. She unintentionally lost 10 lbs in last month. Physical
examination shows tachycardia and dry mucus membranes. Laboratory
studies show:
Chemistry panel
Serum sodium
130 mEq/L
Chloride
93 mEq/L
Bicarbonate
12 mEq/L
Blood urea nitrogen (BUN)
30 mg/dL
Serum creatinine
1.2 mg/dL
Calcium
10.0 mg/dL
Blood glucose
698 mg/dL
Which of the following potassium values would be most likely in this patient?
A.
B.
C.
D.
E.
Intracellular potassium
Decreased
Increased
Increased
Decreased
No Change
Extracellular potassium
increased
decreased
increased
decreased
No change
Explanation: This young patient has both clinical and biochemical features of
diabetic ketoacidosis (DKA); she has high blood glucose, low bicarbonate, a high
anion gap, and decreased sodium.
Most patients in DRA have decreased levels of intracellular potassium with normal to
increased extracellular potassium levels. Potassium loss occurs via osmotic diuresis
induced by glycosuria. Acidosis also pulls potassium from the intracellular
compartment leading to normal to elevated serum potassium levels. Lack of insulin
is also responsible for movement of potassium outside the cells because insulin
normally promotes the intracellular movement of potassium. The net result of all
these events is low total body potassium and low intracellular potassiumwith
normal to increased extracellular potassium. Then when insulin and intravenous
fluids are given to resuscitate the dehydrated and hyperglycemia patient, they push
the potassium back into the cells, which cause a precipitous drop in serum
potassium because there is still an overall potassium deficiency. When a patient
comes to the hospital in DKAI that patient will have low total potassium, even
though labs will return with a normal or even elevated serum potassium level.
(Choice B) Increase in intracellular potassium with decreased extracellular potassium
is seen with glucose and insulin administration. Stimulation of beta-adrenergic
receptors also causes an increased transfer of potassium to the intracellular
compartment.
(Choice C) The renal excretion of potassium is impaired in most patients with chronic
renal failure, resulting in high intra- as well as extracellular potassium.
(Choice D) A decrease in both intra- and extravascular potassium is seen with
mineralocorticoids excess, diuretic use, and gastrointestinal losses.
Educational Objective:
Most patients with diabetic ketoacidosis have normal to increased serum potassium
levels despite low intracellular potassium. Replacement of potassium is a crucial step
in management of patients with diabetic ketoacidosis.
220
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 32: A 78-year-old Caucasian male presents bra routine check-up. His blood
pressure is 180/70mm Hg and his heart rate is 75 beats per minute. Physical
examination findings are within normal limits. You explain to the patient that his
hypertension is most likely caused by age-related:
A. Decrease in cardiac output
B. Increase in sympathetic tone
C. Decrease in lung capacity
D. Renal artery atherosclerosis
E. Aortic stiffening
Explanation:
This patients systolic blood pressure (SBP) exceeds the 140/90 mmHg cutoff for the
diagnosis of hypertension (and initiation of antihypertensive therapy). However, the
patients diastolic blood pressure (DBP) is within a normal range. After age 50, the
pattern of isolated systolic hypertension (ISH) becomes quite common. SBP greater
than 160 mm Hg with a DBP below 90 mm Hg is found in approximately 20% to
30% of all people 80 and older.
ISH is caused by age-related decreases in the compliance of the aorta and its
proximal major branches. Numerous alterations in vessel wall structure and function,
including atherosclerotic changes, have been proposed to explain this stiffening.
(Choice A) A primary decrease in cardiac output (CO) tends to decrease mean
arterial pressure at any given value of total peripheral resistance (TPR), as MAP=CO
x TPR. In contrast this patients MAP = DBP + (1/3) (SBPDBP) = 106mm Hg1
which is elevated above normal adult values of 90100mm Hg.
(Choice B) Although sympathetic cardio vascular tone does generally increase with
age this tends to increase TPR more than it affects aortic compliance. Increased
sympathetic vasoconstriction in muscular arteries and arterioles (the vessels
contributing to the majority of systemic vascular resistance) would tend to elevate
both SBP and DBP.
(Choice C) A decrease in (total) lung capacity might be associated with some
increase in pulmon avascular resistance. However, this would not necessarily have a
significant effect on arterial pressures in the systemic circulation.
(Choice D) Renal artery atherosclerosis and renal artery stenosis in particular, can
result in renovascular hypertension due to excess activation of the reninangiotensin-aldosterone system. Any resultant hypervolemia or increased total
peripheral (systemic) vascular resistance would tend to elevate both SBP and DBP.
Educational Objective:
An age-related decrease in compliance (increased stiffness) of the aorta and its
proximal major branches often causes isolated systolic hypertension (ISH).
221
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 33: A 73-year-old Caucasian male presents to your office following repeated
episodes of exertional dyspnea. Physical examination reveals a cardiac murmur.
The patient is referred to cardiologist or further evaluation. Cardiac catheterization
is performed and the findings are shown on the slide below. Which of the time
points indicated on the slide best corresponds to the peak of the murmur intensity
in this patient?
A.
B.
C.
D.
E.
F.
A
B
C
D
E
F
Explanation:
The hemodynamic profile shows an abnormal pressure gradient between the left
ventricle (LV) and the aorta (Ac) during systole (see arrows in graph below),
indicating significant aortic stenosis (AS).
The intensity of the murmur of AS is directly related to the magnitude of the LV-toaorta pressure gradient. Thus the murmur in this patient would be loudest at point B
and less intense at point A.
(Choices A and C) The murmur of AS is a systolic ejection-type crescendodecrescendo murmur that starts after the first heart sound, following the opening of
the aortic valve (time A). It typically ends before the A2 component of the second
heart sound (time C). At times A and C, the left ventricular and aortic pressures are
nearly equal so that a murmur due to flow across the aortic valve would be unlikely
at these points.
(Choices D and E) These points occur during diastole, when the aortic valve is closed
and the mitral valve is open. There is no abnormally elevated pressure gradient
between the left atrium and left ventricle, consistent with normal unobstructed
222
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
diastolic filling of the left ventricle. Since turbulent flow due to a high pressure
gradient is generally required to produce a murmur the patient would not have a
murmur at times D or E.
(Choice F) This time point corresponds to atrial contraction just prior to ventricular
systole. There is no abnormally elevated pressure gradient between the left atrium
and left ventricle consistent with normal unobstructed filling of the left ventricle.
Educational Objective:
Aortic stenosis (AS) may cause exertional syncope. The murmur of AS is a systolic
ejection-type, crescendo- decrescendo murmur that starts after the first heart sound
and typically ends before the A2 component of the second heart sound. The intensity
of the AS murmur is proportional to the magnitude of the left ventricle-to-aorta
pressure gradient during systole.
223
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 34: A 52-year-old Caucasian male presents to your office for a routine checkup. He says that some cardiac problems were detected during his previous visit to
the doctor. Physical examination reveals a holosystolic murmur at the apex that
radiates to the axilla. Which of the following is the best indicator of the severity of
this patients problem?
A. Holosystolic murmur intensity
B. Presystolic component of the murmur
C. S2 to opening snap (OS) time interval
D. Presence of audible S3
E. Presence of audible S4
Explanation:
Under most modern clinical circumstances, the anatomy and severity of mitral
regurgitation (MR) are best delineated by2D and Doppler echocardiography. Among
auscultator findings, the best indicator of a high regurgitant volume indicating
severe MR with left ventricular volume overload is the presence of a left ventricular
S3 gallop. A left ventricular (LV) S3 gallop reflects an increased rate of filling of the
LV during mid diastole. It can be heard as a consequence of MR and in this condition
reflects the relatively high volume of regurgitant flow which is recycled back into
the LV during diastole.
(Choice A) If the volume of left ventricular blood pumped backed into the left atrium
during systole, or regurgitant volume, is used as a measure of severity of mitral
regurgitation (MR), then one might expect the murmur of MR to become louder as
regurgitant volume increased. However, this would only apply to an anatomically
fixed effective regurgitant orifice (ERO). In the clinical setting, patients with higher
regurgitant volumes may also have larger EROs, such that systolic transvalvular flow
resistance and the degree of turbulence in the regurgitant jet (which accounts for
the intensity of the murmur of MR) may not be strongly correlated with regurgitant
volume.
(Choice B) The murmur of mitral regurgitation is either holosystolic or, in some
cases of mitral valve prolapse, midsystolic. In some cases of severe MR, a diastolic
rumble produced by a high rate of flow across a normal sized diastolic mitral orifice
may be heard. The latter amounts to a functional murmur (relative mitral stenosis)
but is a less reliable finding with a high regurgitant volume than is the presence of
an S3. (Choice C) The S2 to opening snap interval is a diastolic interval between the
second heart sound (specifically A2) and the tensing of a stenotic mitral valve. It is a
parameter of mitral stenosis, not mitral regurgitation.
(Choice E) In a patient with mitral regurgitation, a left ventricular S4 gallop would
most likely be a sign of left heart failure, indicating LV dilatation and the reaching of
the limit of LV compliance during end diastole. However, many patients with severe
MR have not yet developed left sided heart failure. In the latter group of patients, a
left sided S3 would be a more likely finding on cardiac auscultation than a left sided
S4.
Educational Objective:
In a patient with mitral regurgitation (MR), the most reliable auscultator finding
indicating a high regurgitant volume (severe MR) and left ventricular volume
overload is a left sided S3 gallop intensity of a holosystolic murmur due to MR may
not correlate well with regurgitant volume. A left sided S4 would suggest end stage
decompensation of severe MR to left ventricular failure; however, many patents with
severe MR may not have developed left heart failure.
224
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 35: A 53-year-old male with a heavy smoking history suffers from progressive
exertional dyspnea and wheezing. Echocardiogram shows moderate dilatation of the
right ventricle and increased central venous pressure. No lower extremity edema is
observed on physical examination. The absence of edema is best explained by which
of the following compensatory mechanisms?
A. Increased plasma oncotic pressure
B. Increased interstitial fluid pressure
C. Decreased capillary permeability
D. Increased tissue lymphatic drainage
E. Decreased circulating aldosterone level
Explanation:
Progressive exertional dyspnea in a heavy smoker suggests chronic
bronchitis/emphysema (COPD). The right ventricular dilatation and elevated central
venous pressure indicate secondary cor pulmonale. A high central venous pressure
raises the hydrostatic pressure in capillary bed venules, thereby increasing net
plasma filtration, especially in dependent tissues. If there is a compensator increase
in tissue lymphatic drainage to counteract the interstitial fluid increase, edema does
not develop. Only when the venous pressure and net capillary filtration have risen
sufficiently to overwhelm the resorptive capacity of tissue lymphatics does edema
appear.
(Choice A) While an increase in plasma oncotic pressure would oppose edema
formation, this does not occur in COPD.
(Choice B) The interstitial fluid pressure is increased in edema.
(Choice C) A decrease in capillary permeability (filtration coefficient) would oppose
edema formation, but patients with chronic bronchitis are not known to have
decreased capillary permeability.
(Choice E) A decrease in circulating aldosterone could decrease intravascular
volumes and pressures, counteracting edema formation. However, patients with cor
pulmonale tend to have elevated levels of aldosterone in response to the low cardiac
output.
Educational Objective:
When the central venous pressure (CVP) is increased, as in right heart failure, the
interstitial fluid pressure rises due to an increase in net plasma filtration. As the
interstitial fluid pressure increases, so does lymphatic drainage. Increased lymphatic
drainage can compensate for moderate CVP elevations to prevent the development
of clinically apparent interstitial edema. With large CVP elevations, the net capillary
filtration increases in excess of the lymphatic reabsorptive capacity and overt edema
develops.
225
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 36: Two left atrial (LA) compliance curves in patients with mitral regurgitation
are given in the diagram below. Compared to the patient having LA compliance
shown by curve the patient with the curve 2 reading is most likely to suffer:
A. Severe fatigue and exhaustion
B. Atrial fibrillation
C. Acute pulmonary edema
D. Lower extremity swelling
E. Arterial embolism
Explanation:
The patient with curve 2 has reduced left atrial compliance (dV/dP). As a result,
severe mitral regurgitation results in a large increase in the new steady state left
atrial, pulmonary venous, and pulmonary arterial pressures. This picture
characterizes acute mitral regurgitation (MR) that may be due to spontaneous
rupture of chordae tendineae, infective endocarditis with destruction of valve leaflets
or chordal rupture ischemia or rupture of a papillary muscle or failure of a prosthetic
valve. Such acute severe MR does not provide enough time for left atrial adaptation
to the regurgitant volume overload. Acute pulmonary edema therefore is likely to
result. Patients with severe MR (characterized by a high ratio of regurgitant to
forward left ventricular stroke volume) may be hemodynamically classified along a
spectrum of associated left atrial compliance. Severe acute MR is generally
accompanied by a normal left atrial (LA) compliance. More chronically developing
MR1 as could result from myxomatous degeneration or mitral valve prolapse permits
adaptive dilatation of the LA and thinning of its wall accompanied by an increase in
LA compliance corresponding to curve 1. In the latter case, a given regurgitant
volume from the left ventricle results in a lower steady state elevation in LA
pressures. There is also a lesser elevation in pulmonary vascular pressures than
occurs with normal LA compliance in acute MR.
(Choice A) Fatigue and exhaustion are symptoms of a low cardiac output state. The
latter may be found in any patient with severe MR. Thus, patients with severe MR
can experience these symptoms whether they have a low or a high left atrial
compliance.
(Choices B and E) Atrial fibrillation would be more likely to occur in a patient with
curve corresponding to chronic severe mitral regurgitation. As explained above, the
latter permits left atrial dilatation, which, in addition to increasing age, increases the
probability of atrial fibrillation. Atrial mural thrombosis and thromboembolism are
also more likely with left atrial dilatation.
(Choice D) Lower extremity swelling is a sign of right sided heart failure. Right
ventricular (RV) failure can occur either in acute mitral regurgitation with normal left
atrial (LA) compliance (curve 2) and marked pulmonary hypertension or in
decompensation of chronic mitral regurgitation with increased LA compliance (curve
1).
226
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Patients with severe acute mitral regurgitation (MR) who have a near normal left
atrial (LA) compliance tend to develop marked pulmonary hypertension and
pulmonary edema. Patients with severe mitral regurgitation that develops chronically
acquire an increase in LA compliance. They are therefore less prone to pulmonary
hypertension/edema but are more prone to atrial enlargement, fibrillation, and
mural thromboembolism. Any patient with severe MR can develop fatigue and also
eventual signs of right sided heart failure.
227
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 37: A group of investigators is studying central nervous system control
mechanisms of hormone balance. During an experiment, they destroy a
significant portion of the hypothalamus in a lab animal. Which of the
following substances is most likely to be elevated as a result of this
experiment?
Cortisol
B. Thyroxine
C. Vasopressin
D. Prolactin
E. Somatomedin C
A.
Explanation:
Unlike secretion of other pituita hormones prolactin is under tonic (constant)
inhibition by dopamine secretion from the hypothalamus. Hypothalamic destruction
causes hyperprolactinemia by loss of this tonic inhibition. Dopamine inhibits prolactin
production by acting on the D2 dopamine receptor of lactotrophs (the prolactinproducing cells of the pituitary). Medications such as phenothiazines also act on this
receptor and cause hyperprolactinemia at certain doses. On the other hand there are
several putative prolactin-releasing factors that do not yet have clear physiological
roles. Some of the hormones that may increase prolactin levels are thyrotrophinreleasing hormone vasoactive intestinal peptide, oxytocin, and vasopressin.
(Choices A, B, and E) in contrast to prolactin, other pituitary hormones (growth
hormone thyroid-stimulating hormone adrenocorticotropic hormone luteinizing
hormone and follicle-stimulating hormone) are inhibited by hypothalamic lesions
because the dominant effect of the hypothalamus on these hormones is stimulatory.
Thus hypothalamic lesions will ultimately decrease cortisol, thyroxine, and insulinlike growth factor (somatomedin C).
(Choice C) Vasopressin is produced in the supraoptic and paraventricular nuclei of
the hypothalamus and transported to the posterior pituitary for release. Lesions of
the hypothalamus decrease vasopressin levels.
Educational Objective:
The dominant effect of the hypothalamus on prolactin secretion is inhibitory via
dopamine production. Prolactin regulation by dopamine is a commonly tested
concept on USMLE Step 1.
228
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 38: A 60-year-old smoker is brought to the hospital because of altered mental
status. Chest x-ray showed a mass in the lung. Labs are as follows:
Chemistry panel
Serum sodium
120 mEq/L
Serum potassium
4.0 mEq/L
Blood urea nitrogen (BUN)
20 mg/dL
Serum creatinine
0.8 mg/dL
Calcium
9.0 mg/dL
Blood glucose
98 mg/dL
Urine osmolality
360 mOsmol/kg
Which of the following additional finding is most likely to be present in this patient?
A. Peripheral edema
B. Bilateral crackles at the bases
C. Increased B-type natriuretic peptide
D. Dilute urine
E. Normal total body volume
Explanation:
This patient most likely has the syndrome of inappropriate antidiuretic hormone
(SIADH). Small cell carcinomas of the lung, formerly called oat cell carcinomas
consist of cells that contain dense neurosecretory granules and can produce
hormones like ADH. The production of ADH is constitutive, meaning that the lung
tumor pumps out ADH regardless of feedback. Especially because there is a strong
correlation between smoking and small cell carcinomas, we can deduce that this
mans lung mass is most likely one such tumor. It is common for patients with small
cell carcinomas to present with symptoms related to the hormones produced by the
tumor. In this case, the patients low sodium level caused his altered mental status.
Low sodium levels can even cause seizures.
Initially in SIADHI the extra ADH leads to excessive water absorption from the
kidneys, causing a mild hypervolemia early in the disease. The excess body water
suppresses the renin-aldosterone axis, causing low aldosterone. As aldosterone is
responsible for sodium absorption from the distal tubule, low aldosterone levels lead
to natriuresis (salt- wasting via the urine). Eventually, most patients with SIADH will
equilibrate with a near-normal total body volume and low plasma osmolality
(because of the salt-wasting).
Normal ADH secretion by the hypothalamus is regulated by changes in plasma
osmolality and intravascular volume. In this patient, the ADH levels is elevated
despite low plasma osmolality because the secretion of ADH is not regulated by
changes in osmolality; it is produced constitutively. Characteristically, patients with
SIADH do not have gross hypervolemia, nor do they have peripheral edema.
(Choices A, B, and C) Pedal edema bibasilar crackles and increased serum B-type
natriuretic peptide (BNP) are the features of congestive heart failure volume
overload. Although patients with SIADH have mild hypervolemia early in the disease
these patients do not experience the degree of volume overload that would present
with the above symptoms.
(Choice D) The patient cannot have dilute urine because we are told the urine
osmolality (360 mOsmol/kg): memory or a lab reference will reveal that this
patients urine osmolality is high. Dilute urine with low plasma osmolality indicates
primary polydipsia, an excess of water consumption. Characteristic features of
229
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
SIADH are a near-normal intravascular volume high urinary osmolality, high urinary
sodium and low plasma osmolality.
Educational Objective:
SIADH is characterized by concentrated urine low plasma osmolality, increased
urinary sodium and relatively normal body volume. Hypothyroidism and
hypercortisolism should be ruled out before the diagnosis of SIADH is made in real
practice although the lung mass described makes SIADH the most likely disease
present in this patient.
230
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 39: A group of investigators is studying calcium homeostasis. They administer
calcium gluconate by continuous IV infusion and take blood samples. Which of the
following changes from baseline values would occur?
A.
B.
C.
D.
E.
PTH
Increase
Increase
Decrease
Decrease
Increase
Calcitonin
Decrease
Increase
Decrease
Increase
Decrease
1, 25-dihydrocholecalciferol
Increase
Decrease
Decrease
Decrease
Decrease
231
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Explanation:
Serum calcium is tightly regulated: calcium enters the bloodstream from the bones
and from intestinal absorption and calcium is excreted in the urine. This balance is
mainly regulated by circulating PTH and 1, 25-dihydrox vitamin
D. PTH battles low serum calcium levels by three mechanisms: increasing bone
resorption, which releases calcium from the bone into the circulation: increasing the
gastrointestinal absorption of calcium by creating the active form of calciumabsorbing vitamin D, and increasing the renal absorption of calcium. PTH release is
inversely related to serum calcium concentrations in a negative feedback loop.
Calcitonin is secreted by parafollicular C cells in the thyroid and is mainly regulated
by serum calcium. In contrast to PTH calcitonin provides negative feedback for
calcium concentrations. That is calcitonin battles high serum calcium by decreasing
bone absorption via osteoclast inhibition. In normal physiology, however calcitonin is
not a dominant hormone. For instance, total thyroidectomy, which causes virtually
negligible levels of calcitonin, does not cause significant calcium level alterations.
Infusion of intravenous calcium directly raises serum calcium. As calcium and PTH
are inversely related PTH levels will decline; hence, the formation of 1, 25dihydroxyvitamin D will diminish. The increase in calcium levels will prompt the
release of calcitonin, a calcium antagonist, as the body tries to reestablish
homeostasis.
(Choice A) These are the values expected in hypocalcemia. A decrease in serum
calcium will increase PTH release and decrease calcitonin release. Elevated PTH
levels will increase the formation of 1 25 dihydroxy vitamin D.
(Choice B) These are the values one would expect from chronic renal disease, a
condition often accompanied by secondary hyperparathyroidism. Chronic renal
failure decreases the activity of 1-alpha hydroxylase causing the formation of 1, 25dihydrox vitamin D to be decreased, ultimately resulting in hypocalcemia. PTH
release is encouraged both by these low calcium levels and by loss of negative
inhibition from 1, 25 dihydroxy vitamin D. Despite the relative hypocalcemia of renal
failure, levels of calcitonin are increased because the excretion of calcitonin is
impaired.
(Choice C) Low levels of circulating PTH in hypoparathyroidism result in the
decreased formation of 1, 25-hydroxy vitamin D. The ensuing hypocalcemia causes
serum calcitonin to decrease as well.
Educational Objective:
In response to calcium loading, PTH decreases, calcitonin increases, and the renal
synthesis of the active form of vitamin D decreases.
232
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 40: A 43-year-old male (Patient A) is being evaluated for an esophageal
disorder. Esophageal manometry tracings after a single swallow of 5 ml of
water are shown on the slide below.
UE: upper esophagus
ME: middle esophagus
LES: lower esophageal sphincter
Which of the following is the most likely diagnosis in this patient?
A. Cricopharyngeal dysfunction
B. Diffuse esophageal spasm
C. Achalasia
D. Gastroesophageal reflux
E. Mallory-Weiss syndrome
Explanation:
After the contents of the oral cavity are collected on the tongue and propelled into
the pharynx, involuntary contraction of the pharyngeal muscles pushes the material
into the esophagus. The cricopharyngeus muscle contracts behind the food bolus
initiating a peristaltic wave to propel the bolus downward; this contraction is shown
on the first diagram as an upward deflection on both the normal and patient graphs.
The second diagram shows normal peristalsis of the middle esophagus. Under
normal conditions when the food bolus reaches the lower esophagus, the lower
esophageal sphincter relaxes to allow the material to enter the stomach. The third
diagram portrays the decrease in LES pressure that corresponds to its relaxation in
the normal patient.
Esophageal manometry of the patient A reveals normal contraction of upper
esophageal sphincter, decreased peristalsis of the midesophagus illustrated by a
lower amplitude of pressure increase on the second diagram, and no LES relaxation.
These manometric findings are consistent with a diagnosis of achalasia (Choice C).
This motor dysfunction is associated with an elevated resting pressure of the LES
and inability of the LES to relax during swallowing.
(Choice A) Cricopharyngeal dysfunction results from a failure of the cricopharyngeus
to relax during swallowing and causes a choking or food sticking sensation and
pain with swallowing. A video fluoroscopic swallowing study is used for diagnosis.
(Choice B) Diffuse esophageal spasm (DES) is an esophageal motility disorder that
presents with severe, non- cardiac chest pain. It occurs due to uncoordinated
233
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
contractions of the esophageal body. Esophageal manometry shows multiple
contractions on tracings from middle and lower esophagus.
(Choice D) Reflux of gastric contents into the distal esophagus occurs due to low
tone of lower esophageal sphincter and its failure to contract after the transfer of
food to stomach. Esophageal manometry in patients with GERD would show
decreased LES pressure.
(Choice E)Tears of esophageal mucosa at the esophagogastric junction are called
Mallory-Weiss tears. These tears are caused by forceful retching and vomiting and
are common in alcoholics. Mallory-Weiss tear is nota motility disorder and is not
associated with abnormalities of esophageal manometry.
Educational Objective:
Decreased esophageal body peristalsis and poor relaxation of the LES on manometry
are typical for achalasia. Achalasia presents with progressive dysphagia, chest pain,
food regurgitation and aspiration. Barium swallow shows a dilated esophagus and a
birds beak deformity of the LES.
234
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 41: A 45-year-old Caucasian male undergoes evaluation for intense
fatigability. He denies any chest pain dyspnea, palpitations or lower
extremity edema. He has no other medical problems. His laboratory
values are significant for elevated creatinine phosphokinase (CPK) level.
Which of the following is the most reasonable next step in managing this
patient?
tolerance test
B. 24-hour urinary cortisol excretion
C. Serum prolactin level
D. Serum TSH level
E. Electrocardiogram (ERG)
A. Oral
glucose
Explanation:
The clinical features described above are consistent with hypothyroidism. Thyroid
hormones are responsible for the physiologic function of most organ systems;
therefore, dysfunction of the thyroid gland (hypothyroidism or hyperthyroidism)
leads to widespread organ system manifestations. The skeletal system is involved in
both hyper and hypo-thyroidism. Hypothyroid patients typically complain of the
fatigability described in this patient, and also of muscle pain, and cramping. Biopsy
of these muscles usually shows pale muscle fibers with decreased striation and
deposition of a mucinous material. There is atrophy of the type II muscle fibers. As
with any myopathic process, creatinine phosphokinase (CPK) levels can be increased
in patients with hypothyroidism.
(Choice A) Oral glucose tolerance test is used to diagnose diabetes mellitus. This
patient does not have any features suggestive of diabetes mellitus; i.e. he has no
polyuria, polydipsia, or weight loss. Furthermore the oral glucose tolerance test has
been replaced by fasting blood glucose levels in screening most patients for diabetes
mellitus; the oral glucose tolerance test is reserved only for a selected patient
populations.
(Choice B) The patient described above does not have features of Cushing
syndrome. Symptoms of Cushing syndrome include central obesity, abdominal skin
striae, proximal muscle weakness hypertension and increased supraclavicular
deposition of fat. The 24-hour urine cortisol excretion is a screening test for Cushing
syndrome and is not indicated when a thyroid disorder is suspected.
(Choice C) Hyperprolactinemia presents with hypogonadism in males. In typical
cases of hyperprolactinemia, there is no involvement of muscle system. Although it
is true that serum prolactin levels can be elevated in patients with hypothyroidism,
establishing this patients thyroid status is the best next step in evaluating his
fatigability.
(Choice E) CPK exists in three isoforms: MM, MB and BB. CPK MB is confined to the
cardiac muscle; BB is present in the nervous system and MM is present in the
skeletal muscle. Damage to the respective organ system will elevate the level of that
specific CPK isoform. If this patient did have a myocardial infarction the CPK would
increase and it would be the MB isoform. However the patient has no symptoms
suggestive of ischemic cardiac disease; and the myopathy of hypothyroidism
accounts for the increase in CPK (MM isoform).
Educational Objective:
Hypothyroidism is a common cause of elevated CPK level because of hypothyroid
myopathy. Sometimes it can be the first manifestation of hypothyroidism. The other
common causes of elevated CPK include medications such as HMG Co-A reductase
inhibitors (statins), autoimmune disease (polymyositis / dermatomyositis) and
muscular dystrophies (like Duchenne muscular dystrophy).
235
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 42: A newborn female is hypotensive and hypoactive. She also has labial
fusion and clitoromegaly. The prenatal period and delivery were
uncomplicated. Laboratory investigation reveals increased urinary 17hydroxyprogesterone excretion and decreased 11-deoxycortisone excretion.
Which of the following enzymes is most likely to be deficient in this patient?
hydroxylase
B. 21-hydroxylase
C. 11-hydroxylase
D. Desmolase
E. 5-alpha-reductase
A.
17-
Explanation:
Congenital adrenal hyperplasia (CAH) is a group of disorders that result from defects
in the enzymes of cortisol biosynthesis in the adrenal gland. 21-hydroxylase
deficiency is the most common type of CAH, accounting for 90% of patients. The
enzyme 21-hydraylase catalyzes the conversion of 17-hydroxy-progesterone to 11deoxycortisol in the zona fasciculata, and the conversion of progesterone to
deoxycorticosterone in the zona glomerulosa. When there is a deficiency of 21-
236
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
hydrorlase, the adrenal gland cannot synthesize cortisol efficiently. Low cortisol
levels stimulate ACTH release from the pituitary gland. In this setting, elevated
ACTH levels serve to increase the production of adrenal androgens, because the
accumulating high levels of cortisol precursors are diverted towards the adrenal
androgen biosynthetic pathway (see diagram). The patient described in the vignette
has clinical features of cortisol and aldosterone deficiency (hypotension), and
androgen excess (labial fusion and clitoromegaly).
(Choice A) 17-hydroxylase deficiency accounts for less than 1% of patients with
CAH. 17-hydroxylase converts pregnenolone to 17-hydroxypregnenolone and
progesterone to 17-hydroxyprogesterone. This enzymatic pathway is active in both
the adrenal gland and the gonads. ACTH levels are high as a result of decreased
cortisol production, thus stimulating the formation of deoxycorticosterone and
corticosterone in the adrenals. The result is low renin levels, hypertension, and
hypokalemia. In females, the genitalia are normal at birth. However, these females
have delayed puberty (no production of sex steroid) and are hypertensive (excessive
production of deoxycorticosterone and corticosterone). Males are under virilized and
hypertensive.
(Choice C) 11--hydroxylase converts deoxycorticosterone to corticosterone and 1deoxycortisol to cortisol. Like 21-hydroxylase deficiency, this enzymatic deficiency
presents with ambiguous genitalia and increased androgen levels at birth. Because
the production of deoxycorticosterone (potent mineralocorticoid) is increased, these
patients have features of mineralocorticoid excess (in contrast to the symptoms of
mineralocorticoid deficiency that occur with 21-hydroxylase deficiency).
(Choice D)20, 22-desmolase converts cholesterol to pregnenolone. Because this is
the first enzyme in the steroidogenic pathway, the formation of all steroid hormones
is affected. Cholesterol and cholesterol esters accumulate in the adrenal glands. This
type of CAH is extremely uncommon and usually carries a bad prognosis.
(Choice E) 5-a-reductase deficiency causes ambiguous genitalia in males, as a result
of a defective conversion of testosterone to dihydrotestosterone. This is not a form
of CAH because cortisol production is not affected.
Dihydrotestosterone is responsible for the fusion of the labial folds during normal
male fetal development. Low dihydrotestosterone levels during fetal life leads to
poor labial fusion in males. Depending on the severity of the defect the external
genitalia in males vary from pseudovaginal perineoscrotal hypospadias to labial
fusion with microphallus. At puberty, affected males show signs of virilization, such
as increased muscle mass, deepened voice and phallus enlargement, because these
pubertal features are dependent on testosterone. After puberty, males have a high
testosterone level, with low dihydrotestosterone levels and mildly elevated FSH.
Females with 5--reductase deficiency do not have ambiguous genitalia.
Educational Objective:
21-hydroxylase deficiency is the most common cause of CAH. It may result in
mineralocorticoid deficiency and is accompanied by increased 17hydroxyprogesterone secretion.
237
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 43: A 21-year-old Caucasian male presents to your office with mild jaundice
after a hiking trip. He had a similar episode two years ago after fasting for five
days. His physical examination is unremarkable except for mild jaundice.
Liver studies
Albumin
4.2 mg/dL
Total protein, serum
6.8 mg/dL
Total bilirubin
2.8 mg/dL
Direct bilirubin
0.8 mg/dL
Alkaline phosphatase
90 U/L
Aspartate aminotransferase (SGOT)
26 U/L
Alanine aminotransferase (SGPT)
32 U/L
This patient most likely suffers from:
A. Gilbert syndrome
B. Dubin-Johnson syndrome
C. Acute viral hepatitis B
D. Acute viral hepatitis C
E. Acute alcoholic hepatitis
F. Wilsons disease
Explanation:
The hepatic metabolism of bilirubin occurs in the following four stages: uptake from
the bloodstream; storage within the hepatocyte; conjugation with glucuronic acid;
and biliary excretion. In the normal individual, serum total bilirubin is 0.2-1 mg/dL,
of which <0.2 mg/dL is the direct fraction. Typically, elevated conjugated bilirubin
levels are suggestive of hepatobiliary disease (eg cirrhosis or hepatitis) because the
bilirubin conjugates will reflux back into the plasma when the secretion of
conjugated bilirubin into the bile is slowed. In contrast, elevated unconjugated
bilirubin levels typically indicate increased bilirubin formation (such as that seen in
hemolysis) or a slowing in bilirubin conjugation (such as that seen in this patient,
who has Gilbert syndrome).
Gilbert syndrome is a common familial disorder of bilirubin glucuronidation in which
the production of UDP glucuronyl transferases (enzymes that mediate
glucuronidation of various substances) is reduced. Approximately 9% of individuals
in Western countries are homozygous for this mutation with another 30%
heterozygous and asymptomatic. The diagnosis is suggested in those patients with
no apparent liver disease who have mild unconjugated hyperbilirubinemia thought to
be provoked by one of the classic triggers. Examples of such triggers include
hemolysis, fasting physical exertion, febrile illness stress, and fatigue. Presumptive
diagnosis can be made when the unconjugated hyperbilirubinemia persists with
repeat testing but liver function tests complete blood count, blood smear and
reticulocyte count are normal.
(Choice B) Individuals with the rare Dubin-Johnson syndrome have predominantly
conjugated chronic hyperbilirubinemia that is not associated with hemolysis. For the
diagnosis to be made conjugated hyperbilirubinemia with a direct bilirubin fraction of
at least 50% and an otherwise normal liver function profile must be present.
(Choices C and D) Expected laboratory findings in a patient with acute viral hepatitis
include significant elevations in ALT and AST (with ALT> AST) followed by rises in
bilirubin and alkaline phosphatase.
(Choice E) Alcoholic hepatitis is typically associated with a significant drinking history
and is commonly characterized by an AST:ALT ratio greater than 2:1.
238
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice F) Wilsons disease is the likely diagnosis in a patient younger than 30 years
old with unexplained chronic hepatitis (elevated AST and AST). The presence of low
serum ceruloplasmin and increased urinary copper excretion or Kayser-Fleischer
rings provides diagnostic confirmation.
Educational Objective:
Gilbert syndrome is the likely diagnosis in patients with no apparent liver disease
who have mild unconjugated hyperbilirubinemia that appears provoked by one of the
classic triggers.
239
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 44: A 21-year-old Caucasian male presents to your office complaining of
repeated episodes of palpitations that start and stop abruptly. After
completing a careful work-up, you believe that there is an abnormal muscle
tract in this patients heart that bypasses the AV node. If your diagnosis is
correct, which of the following parts of the patients ECO is most likely to be
affected at baseline?
A.
B.
C.
D.
E.
F.
A
B
C
D
E
F
Explanation:
The patient gives a history consistent with recurrent temporary arrhythmias, and we
come to suspect that these maybe due to an accessory AV conduction pathway (a
bundle of Kent). The presence of such a pathway would allow recurrent temporary
tachyarrhythmias due to an atrioventricular re-entry circuit involving the AV node
and the accessory pathway. The diagram below depicts the most common
anatomical anomaly responsible for Wolff Parkinson-White (WPW) pre-excitation
syndrome and the most common re-entry circuit responsible for paroxysmal narrow
ORS complex (supraventricular) tachycardia in patients with WPW.
In patients with this anatomical abnormality when there is no re-entrant
tachycardia, normal sinus impulses reach the ventricles first via the accessory
pathway and shortly thereafter via the AV node. The accessory pathway preexcites the ventricles, hence the term pre-excitation syndrome. The result is a
shortened PR interval (often less than 12 seconds) with an early hump (delta wave)
at the start of each ORS complex. The ORS complex is wider than normal as well. A
demonstrative EGG is pictured below:
240
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice A) Except during periods of tachycardia, a patient with an accessory AV
conduction pathway should have a normal p-wave.
(Choice B) There are no s-segment changes in WPW syndrome.
(Choice C and D) The ST-segment (choice C) corresponds roughly to the plateau
phase of the ventricular cardiac myocyte action potential and the T-wave (choice D)
corresponds roughly to the repolarization phase of ventricular myocardiocytes action
potentials. Due to changes in the normal geographic sequence of ventricular
depolarization and repolarization in isolated ventricular pre-excitation, there may be
variable ST segment T wave abnormalities, but these are less consistently found
than the usual WPVV triad of ECG abnormalities.
(Choice F)The QT-interval might theoretically be prolonged to the same extent that
the ORS interval is prolonged in a patient with an accessory AV conduction pathway.
However, any QT-interval changes are not seen as consistently as the WPW triad of
ECG abnormalities.
Educational Objective:
An accessory AV conduction pathway can manifest clinically as recurrent paroxysmal
supraventricular tachycardia (PSVT) in an otherwise healthy individual. The baseline
ECG (i.e. not in the setting of PSVT) of a patient with this anatomy generally shows
a triad of abnormalities, which correspond to the ventricular pre-excitation
physiology (Wolff Parkinson-White syndrome): a shortened PR-interval, a delta wave
at the start of the ORS complex, and a widened QRS- interval.
241
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 45: A new drug developed for the treatment of congestive heart failure
demonstrates favorable effects in both animal experiments and human
studies. The drug dilates arterioles and veins and promotes diuresis. The
drug described above is most likely an analog of which of the following
endogenous substances?
Endorphin
B. Transforming growth factor beta (TGF)
C. Brain natriuretic peptide
D. Bradykinin
E. Endothelin
F. Angiotensin II
A.
Explanation:
Nesiritide is a recombinant form of human Brain Natriuretic peptide (BNP) and can
be used in patients with decompensated left ventricular dysfunction leading to
congestive heart failure. In heart failure, especially systolic dysfunction, increased
blood volume within the heart causes stretching of the atria and ventricles beyond
the appropriate stretch to cause maximal contraction by the Prank-Starling
mechanism. This increased stretch causes the release of natriuretic peptides from
the walls of the atria (atrial natriuretic peptide, ANP) and the walls of the ventricles
(Brain Natriuretic Peptide, BNP). Both ANP and BNP activate guanylate cyclase,
which induces an increase of intracellular cyclic GMP. Natriuretic peptides cause
vasodilatation, diuresis/natriuresis (as their name implies) and a decrease in blood
pressure. They counteract endothelin, sympathetic effects and angiotensin II.
(Choice A) Endorphin, as indicated by the name, is an endogenous substance that
acts on the same receptors as narcotic analgesics (ENDO genous mORPHINe). Itis
released by the hypothalamic-pituitary axis and does not play a role in diuresis or
vasodilatation. Itis synthesized in and released from primarily corticotroph cells in
the anterior pituitary.
(Choice B)TGP-3 is a molecule synthesized by most cells in the body. Actions of TGF43 include arrest of the cell cycle (leading to its action as a tumor suppressing
agent), promotion of angiogenesis (leading to its action as an agent allowing tumor
metastases to survive after they become resistant to TGF), and stimulation of
fibroblasts to lay down extracellular matrix proteins (leading to its implication in
atherosclerosis and fibrotic diseases). It does not cause the effects mentioned in the
question stem.
(Choice D) Bradykinin is a hormone produced by the kidney in situations where the
adrenergic and renin-angiotensin aldosterone systems are stimulated. It acts locally
to constrict veins and dilate arterioles to increase renal perfusion. It is metabolized
by ACE and has been implicated as one of the causes of angioedema. This is why
patients on ACE inhibitors are predisposed to angioedema.
(Choices E and F) Endothelin and Angiotensin II both have effects that are opposite
those of brain natriuretic peptide and opposite those presented in the question stem.
They are both potent vasoconstrictors that have the effect of increasing the afterload
which the failing heart has to pump against in the setting of heart failure. It is
believed that endothelin release is mediated by angiotensin II, and this is why the
ACE-I class of drugs has been found to be useful in treating heart failure.
242
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Brain Natriuretic Peptide (BNP) is elevated in patients with heart failure and is often
used as a laboratory test in the clinical setting to determine if a patient is suffering
from a CHE exacerbation. Itis released by the ventricles when they are stretched as
they often are in CHE from systolic dysfunction. It acts along with ANP to cause
vasodilatation (decreased preload) and diuresis. Both ANP and BNP activate
guanylate cyclase, which induces an increase of intracellular cyclic GMP.
243
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 46: Partial gastrectomy is performed on a 32-year-old Caucasian male
because of refractory peptic ulcer disease. The pathologist receives the
tissue and notes significant enlargement of the gastric rugal folds on gross
examination. Microscopy of the gastric mucosa reveals parietal cell
hyperplasia. Which of the following stimuli is the most likely cause of parietal
cell proliferation in this patient?
Acetylcholine
B. Serotonin
C. Somatostatin
D. Gastrin
E. Secretin
F. Transforming growth factor -
A.
Explanation:
Parietal cells are located in the mucosal glands of the fundus and body of the
stomach. They can be easily spotted due to their eosinophilic cytoplasm on H&E
stain. These cells have abundant mitochondria and an intracellular tubulovesicular
system. They secrete gastric acid (HO) and intrinsic factor.
Parietal cells are influenced by a number of substances. Histamine acetylcholine, and
gastrin increase gastric acid secretion while PGE2 inhibits it. Gastrin not only
facilitates HCI secretion, but it also has atrophic affection parietal cells, causing
proliferation and hyperplasia of these cells.
In patients with Zollinger-Ellison syndrome (such as in the patient in the vignette),
excessive gastrin is produced by tumor cells. The excess gastrin increases gastric
acid secretion and induces parietal cell proliferation. Increased acid production leads
to peptic ulcer disease and diarrhea. Parietal cell hyperplasia increases the mass of
fundic glands, visibly enlarging the fundic mucosal folds.
(Choice A) Acetylcholine is a universal neurotransmitter that is present in
parasympathetic postganglionic synapses and in all preganglionic synapses.
Cholinergic receptors are divided into muscarinic (located in smooth muscle and in
glands) and nicotinic (at the neuromuscular junctions).
(Choice B) Serotonin (5HT) is found in GIT, brain, platelets retina and other tissues.
This mediator helps regulate secretion peristalsis, vomiting and control of emotions
by the limbic system.
(Choice C) Somatostatin (growth hormone-inhibiting hormone) is secreted by D cells
of pancreatic islets and 01 mucosa. Somatostatin inhibits gastrin secretion
pancreatic exocrine secretion, gastric secretion and motility, gallbladder contraction
and the absorption of all nutrients.
(Choice E) Secretin is produced by S cells of the small intestine. It increases
bicarbonate production by the pancreas and leads to the secretion of watery,
alkaline pancreatic juice. This substance also inhibits gastric acid secretion and
stimulates pyloric sphincter contraction.
(Choice F)The predominant sources of TGE- are carcinomas but this chemical is
also secreted by macrophages and epithelial cells. TGE- is a potent stimulator of
epithelial growth. In the stomach it causes mucosal-cell hyperplasia, but has little
effect on parietal cells.
Educational Objective:
Gastrin increases gastric acid secretion and stimulates parietal cell proliferation, thus
increasing parietal cell mass (trophic effect). Both these effects are seen in patients
with Zollinger-Ellison syndrome.
244
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 47: An 8-year-old Caucasian male with recurrent pulmonary infections and
otitis media is found to completely lack the cystic fibrosis transmembrane
conductance regulator (CETR) on epithelial surfaces. The contents of which of
the following lumens is most likely to be hypertonic?
A. Pancreatic ducts
B. Small airways
C. Sweat ducts
D. Vas deferens
E. Bile ductules
Explanation:
Cystic fibrosis (CF) results from an autosomal recessive mutation in the CFTR gene.
Effects on ion and water transport are tissue-specific. In most exocrine epithelia, a
normal CFTR will increase chloride conductance (thereby enhancing chloride
reabsorption or secretion depending upon local transmembrane electrochemical
gradients) and inhibit apical sodium resorption. In sweat ducts, however, the CFTR
normally increases luminal membrane sodium resorption. Thus CFTR mutation in
sweat gland ducts decreases both sodium and chloride resorption, causing the sweat
to be abnormally hypertonic in CF patients.
(Choice A) In pancreatic ducts and most other exocrine ducts, the CFTR normally
functions to promote chloride secretion and inhibit sodium resorption. The CFTR also
increases bicarbonate secretion. Mutation of the CFTR would cause an abnormally
high rate of net ion and water resorption, causing isotonic dehydration of the lumen
and contributing to ductal obstruction by thickened mucus. In CF patients the
abnormal acidity of the pancreatic duct fluid may also contribute to obstruction by
promoting mucin precipitation.
(Choice B) In the mucous glands of small pulmonary airways, the CFTR normally
promotes chloride secretion and inhibits sodium resorption by the mucous gland
ductal epithelium. Thus, a CFTR mutation would cause an abnormally high rate of
net ion and water resorption, producing isotonic dehydration of the inner luminal
duct surface and thickened mucus. In small airways, this viscous mucus can cause
airway obstruction and promote infection secondary to mucus plugging and impaired
mucociliary clearance. Histologic examination shows bronchioles distended with thick
mucus and bronchiectasis.
(Choice D) Mutation of the CFTR would cause isotonic dehydration of the contents of
the vas deferens as well. However this choice can also be eliminated based on the
fact that congenital bilateral absence of the vas deferens is commonly associated
with CFTR mutations.
(Choice E) Involvement of the bile duct epithelium by a CFTR mutation would cause
isotonic dehydration of the luminal contents as in most exocrine glands. Bile
canaliculi become plugged by mucinous material potentially resulting in cholestasis,
hepatic steatosis, and biliary cirrhosis.
Educational Objective:
Mutations in the CFTR gene cause isotonic dehydration of the luminal contents of
most exocrine glands. Sweat glands are the exception here CFTR mutations
produce hypertonic luminal fluid containing elevated concentrations of sodium and
chloride.
245
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 48: A 45-year-old alcoholic male with history of hepatitis C infection and HIV
is brought to the hospital with abdominal distention and altered mental status. He
has a musty body odor. Physical examination shows gynecomastia, palmar
erythema, spider angiomata, and asterixis. Abdomen is extremely distended with
dilated periumbilical veins; 3 + bilateral lower extremity edema is present.
Abdominal imaging shows splenomegaly. In this patient which of the following has
similar pathogenicity of gynecomastia?
A. Lower extremity edema
B. Altered mental status
C. Palmar erythema
D. Musty body odor
E. Splenomegaly
F. Esophageal varices
Explanation:
This patient has numerous cirrhotic stigmata that are consistent with cirrhosis of the
liver, including gynecomastia, palmar erythema, spider angiomata, asterixis, ascites,
pedal edema hepatic encephalopathy, and splenomegaly. Cirrhosis of any type
results in the progressive loss of liver functionality.
In the cirrhotic patient, gynecomastia arises from hyperestrinism secondary to the
damaged livers inability to metabolize circulating estrogens. Other manifestations of
hyperestrinism in the cirrhotic patient include palmar erythema, spider angiomas,
and in males, testicular atrophy and decreased body hair.
(Choice A) The liver is the primary site of protein synthesis, and the cirrhotic liver
typically produces insufficient amounts of important proteins such as albumin.
Hypoalbuminemia leads to a decrease in the intravascular oncotic pressure. Fluid
then moves into the extravascular space, and pitting edema in the lower extremities
(eg, pedal edema) results.
(Choices B and D) Altered mental status and musts body odor (fetor hepaticus) are
signs of poor hepatic function and hyperammonemia. In the healthy liver, ammonia
is detoxified to urea, which is then excreted in the urine. Because the cirrhotic liver
has lost this detoxification ability, ammonia accumulates in the blood. Impaired
neuronal function and cerebral edema frequently ensue.
(Choices E and F) Portal hypertension arises from increased hepatic resistance to
portal flow at the sinusoids and causes increased pressure at the portosystemic
collateral veins in the anterior abdomen lower rectum and the lower end of
esophagus where the portal and systemic circulations meet. This phenomenon is
responsible for the esophageal varices, hemorrhoids, caput medusae, and
splenomegaly commonly seen in cirrhotic patients.
Educational Objective:
Hyperestrinism in cirrhosis leads to gynecomastia, testicular atrophy, decreased
body hair, spider nevi and palmar erythema.
246
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 49: A 65-year-old long-time smoker is evaluated for shortness of breath and
cough. Chest X-ray shows a mass in the right upper lobe. Laboratory studies
return with the following values:
Chemistry panel
Serum sodium
Serum potassium
Blood urea nitrogen (BUN)
Serum creatinine
Calcium
136 mEq/L
4.0 mEq/L
20 mg/dL
0.8 mg/dL
14.0 mg/dL
A bone scan is negative. Which of the following is most likely to be elevated in this
patient?
A. Serum phosphorous
B. Parathyroid hormone level
C. Parathyroid hormone related peptide
D. 25 hydroxyvitamin D level
E. Serum prolactin level
Explanation:
This long-term smoker has lung mass and respiratory symptoms that probably
represent cancer; and smoking is a very significant risk factor for squamous cell lung
cancer. This patients labs also demonstrate elevated serum calcium. Answering this
question will depend on your knowledge of a paraneoplastic phenomenon known as
the humoral hypercalcemia of malignancy. This hypercalcemia is caused by factors
usually secreted by non-metastatic cancers. Although other factors maybe
responsible parathyroid hormone-related peptide (PTHrP) is by far the most
significant cause of the humoral hypercalcemia of malignancy. The structure of
PTHrP closely resembles parathyroid hormone (PTH) at the bioactive amino-terminal
region. As a result, PTHrP acts similarly to PTHI although the degree of
hypercalcemia is generally higher with PTHrP production than in primary
hyperparathyroidism.
(Choice A) As a rule of thumb if calcium levels are high, phosphorous levels are low,
and vice versa. Phosphorous is certain to be low in this patient because PTHrP is a
potent inhibitor of phosphorus reabsorption from the proximal renal tubule.
(Choice B) PTHrP causes hypercalcemia, which suppresses the secretion of PTH via
calciums negative feedback.
(Choice D) Serum levels of 25-hydroxvvitamin D reflect the oral intake and
endogenous formation of vitamin D. Neither PTHrP nor PTH have an effect on the
25-hydroxylation step in the liver.
(Choice E) Serum prolactin level is not related to this patients condition.
Educational Objective:
The hypercalcemia associated with squamous cell lung cancer and several other
tumors, is usually due to overproduction of parathyroid hormone-related peptide and
is termed the humoral hypercalcemia of malignancy.
247
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 50: A 45-year-old Caucasian female undergoes left-sided adrenalectomy.
Gross examination of the gland demonstrates a well-defined yellowish tumor in
the adrenal cortex. If the tumor was composed of functional cells from the
outer layer of adrenal cortex the patient would most likely complain or
Weight gain and easy bruising
B. Paresthesia and muscle weakness
C. Excessive hair growth
D. Sweating and tremulousness
E. Diarrhea and flushing
A.
Explanation:
The outer layer of the adrenal gland, the zona glomerulosa, normally produces
aldosterone. The patient in the vignette most likely suffers from primary
hyperaldosteronism (Conns syndrome). Aldosterone-secreting adrenal adenomas
are the most common cause of Conns syndrome (65% of cases). Idiopathic
hyperaldosteronism, including primary adrenal hyperplasia, accounts for 3040% of
cases of Conns syndrome. Hyperaldosteronism produces renal Na retention and
excess K secretion, resulting in hypertension and hypokalemia. Additionally, patients
with Conns syndrome commonly experience a metabolic alkalosis. The hypokalemia
may cause muscle weakness (hypokalemic paresis). Hypokalemic alkalosis may
promote paresthesias.
(Choice A) Weight gain and easy bruising are symptoms of glucocorticoid excess
(Cushings syndrome). Easy bruising results from inhibited collagen and matrix
glycosaminoglycan synthesis, resulting in thinner, weaker skin and connective
tissue. A cortisol-secreting adrenal lesion would have the functionality of the
intermediate layer of the three-layered adrenal cortex, the zona fasciculata.
(Choice C) Excessive hair growth (hirsutism) can result from androgen excess. An
adrenal tumor causing androgen hypersecretion would have the functionality of the
third (innermost) layer of the adrenal cortex, the zona reticularis.
(Choice D) Sweating and tremulousness can be caused by excess circulating
catecholamines, which may result from a pheochromocytoma, the most common
tumor of the adrenal medulla in adults.
(Choice E) Diarrhea and flushing may be seen in carcinoid syndrome, a rare
condition caused most often by a serotonin (5-HT)-secreting tumor derived from
neuroendocrine cells of the gastrointestinal tract.
Educational Objective:
If a hypersecreting-adrenal tumor has the functionality of the outer, intermediate, or
inner layers of the adrenal cortex, the hormone(s) released and clinical syndrome
produced will be aldosterone/Conns syndrome, cortisol/Cushings syndrome, and
androgens/hirsutism and virilization, respectively.
248
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 51: A 6-year-old Caucasian girl is brought to your office by her mother. The
mother says that her daughter is womanly including being exceptionally tall for
her age. Physical examination reveals Tanner Stage 3 breast development and
coarse pubic hair. The childs height is in the 96th percentile. You explain to her
mother that, although this girl is yew tall now, she will ultimately be shorter than
average if she does not get treatment. Which of the following is the physiologic
explanation for the information you provided?
A. Estrogen effect on the long bone diaphysis
B. Estrogen effect on the long bone epiphysis
C. Estrogen effect on the long bone epiphysial plate
D. Somatomedin C effect on the long bone diaphysis
E. Somatomedin C effect on the long bone epiphysial plate
Explanation:
The child described in the vignette is six years old and has already undergone
pubertal changes, as indicated by her Tanner staging. (Also called the sexual
maturity rating, Tanner staging is a systematic, universalized method that uses
female breast and pubic hair development to categorize development.) Precocious
puberty in Caucasian females is defined as the development of secondary sexual
characters at an age less than seven years.
Young bone has several layers; their order from middle to end is diaphysis,
metaphysis, epiphyseal cartilage, and epiphysis. The epiphyseal cartilage, also called
the growth plate, is responsible for linear growth.
Linear growth stops when the epiphyseal growth plate closes, i.e. when the
epiphysis fuses with the metaphysis. Sex steroids initially increase linear growth, but
they also encourage closure of epiphyseal growth plates. Once the growth plates
have closed linear growth is irreversibly stopped. In normal puberty there is a rapid
increase in growth. At the end of this pubertal growth spurt, almost 90% of the final
height is achieved. Although this child is currently taller than her peers the excess
steroids will soon cause epiphyseal growth plate closure: hence, if this patient is not
treated, she will ultimately not meet her full growth potential.
(Choices A and B) in sites other than the epiphyseal growth plate the effect of
estrogen on bone is anabolic because estrogen increases osteoblastic bone
deposition and decreases osteoclastic bone resorption. Low estrogenic states, such
as menopause, are associated with rapid bone loss.
(Choices D and E)The secretion of somatomedin C, more commonly known as
insulin-like growth factor-i (IGF-i), is directly increased when growth hormone is
secreted from the pituitary gland. IGF-i causes the differentiation and proliferation of
chondrocytes in the epiphyseal growth plate, causing an increase in linear growth.
However, unlike estrogen, IGF-1 does not accelerate epiphyseal closure.
Educational Objective:
Sex hormones promote both growth and epiphysial plate closure: hence, precocious
puberty may result in a shorter stature, despite an initial growth spurt. Gigantism is
caused by excessive pituitary production of growth hormone; these patients achieve
enormous heights because, unlike excessive sex steroids, excessive IGF-1 does not
lead to premature closure of the epiphysis.
249
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 52: Animal experiments have shown that chronic, chemical, intravascular inju
results in intimal thickening and collagen deposition. Which of the following cells are
most important in this intimal response?
A. Interstitial fibroblasts
B. Endothelial cells
C. Smooth muscle cells
D. Macrophages
E. Pericytes
Explanation:
The vascular reaction to intimal injury, including endothelial injury, involves
migration of medial smooth muscle cells (SMC) across the internal elastic lamina and
into the intima, followed by SMC proliferation and collagen synthesis to produce a
neointima. The result is often a reactive intimal hyperplasia.
Injured endothelial cells may release growth factors, such as platelet-derived growth
factor (PDOF) that promotes SMC migration and proliferation. They may also express
surface vascular cell adhesion molecules, such as VCAM-1 which allow adherence of
monocytes and lymphocytes and their diapedesis into the intima. These white blood
cells can then release further cytokines and growth factors to promote SMC
migration into and proliferation in the intima, encouraging subsequent fibrogenesis
(elaboration of collagen and extracellular matrix). Finally, when intimal injury is
severe enough to denude the endothelium, there is platelet adhesion to
subendothelial collagen and platelet release of PDGF.
(Choice A) Fibroblasts are infrequently found in the tunica intima of blood vessels. In
response to injury, medial SMC migrate into the intima, and are responsible for
intimal thickening and collagen deposition.
(Choice B) Injured endothelial cells may secrete factors that promote medial SMC
migration and proliferation, including PDGFI FOE, and endothelin-1. However, the
SMC are directly responsible for intimal thickening after intimal injury as a result of
SMC proliferation and synthesis of new collagen, elastin, and proteoglycans.
(Choice D) SMC derived from the media are responsible for intimal thickening. After
injury, these cells migrate, proliferate, and synthesize new connective tissue.
However, tissue macrophages in the intima can contribute to this process as well.
Blood monocytes can be recruited to the intima beneath sites of endothelial injury to
form tissue macrophages.
Educational Objective:
The vascular reaction to endothelial and intimal injury is intimal hyperplasia and
fibrosis, mediated predominantly by reactive SMC that migrate from the media to
the intima.
250
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 53: In certain adults, the myocytes of the cardiac ventricles express mRNA for
natriuretic peptides typically synthesized by the atria. This finding is associated with
which of the following conditions?
A. Hyperplasia
B. Hypertrophy
C. Malnutrition atrophy
D. Sublethal ischemic injury
E. Reperfusion injury
F. Normal aging
Explanation:
Pathologic ventricular hypertrophy is accompanied not only by morphologic changes,
but by changes in gene transcription patterns as well. When there is prolonged
hemodynamic overload, there may be abnormal up-regulation or re-expression of
fetal proteins from both atrial and ventricular myocytes. These alterations in protein
synthesis may be adaptations to improve contractile efficiency and to decrease
ventricular wall stress. In the normal adult heart, A-type natriuretic peptide (ANP) is
secreted by the atria, and in some cases the ventricles in response to volume
overload. B-type natriuretic peptide (BNP) is predominantly secreted by the
ventricles. Volume overload increases the release of both ANP and BNP, facilitating
natriuresis and diuresis. BNP levels can be used for the diagnosis of congestive heart
failure (both systolic and diastolic).
(Choice A) The cardiac myocyte is generally considered a terminally differentiated
cell that can no longer divide. Increased mechanical loads (pressure and/or volume
overload) can increase the sarcomere content and volume of individual ventricular
myocytes (hypertrophy), but do not cause hyperplasia.
(Choice C) Atrophy from malnutrition causes a reduction in the structural
components of the cell. The myocytes of atrophic muscle contain fewer myofilaments
and mitochondria, and less endoplasmic reticulum.
(Choice D) Reversible ischemic injury to cardiac myocytes results in intracellular ATP
depletion glycogen loss, lactate accumulation relaxation of myofibrosis and
mitochondrial swelling. There are no associated increases in ANP or BNP.
(Choice E) Reperfusion injury is thought to result from generation of oxygen-free
radicals and/or local complement activation. ANP and BNP are not elevated in this
condition.
(Choice F) Normal aging of ventricular myocytes results in atrophy and the
progressive accumulation of cytoplasmic granules containing brownish Lipofuscin
pigment.
Educational Objective:
1. Both ventricular hypertrophy and volume overload cause release of both ANP and
BNP from the ventricular myocytes to facilitate natriuresis and diuresis.
2. Reperfusion injury is thought to result from generation of oxygen-free radicals.
251
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 54: A 28-year-old Caucasian female comes to your office complaining of
constant thirst. She also urinates a lot, and her mouth is very often dry. Her
blood glucose level is 80 mg/dL, and her plasma sodium level is 132 mEq/L.
You proceed with the standard water deprivation test in this patient. The urine
osmolality results of the test are presented below.
1 hour 2 hour 3 hour 4 hour 5 hour 6 hour 7 hour 8 hour
130
160
170
285
310
510
510
520
5 units of vasopressin administered
Which of the following is the best treatment for this patient?
Desmopressin
B. Hydrochlorothiazide
C. Indomethacin
D. Low salt, low protein diet
E. Water restriction
A.
Explanation:
Three important causes of polyuria and polydipsia are diabetes mellitus, diabetes
insipidus (Dl), and primary (psychogenic) polydipsia. Diabetes mellitus can quickly
be ruled out in this patient because her blood glucose is normal. Next, one must
decide between Dl and psychogenic polydipsia. Dl is an inability to concentrate the
urine because of either a deficient amount of vasopressin (antidiuretic hormone
[ADH], or an abnormal response to ADH. In a water deprivation study, patients with
Dl will not have a significant change in urine osmolality.
Primary polydipsia, called psychogenic polydipsia in older literature, is simply
excessive (pathologic) water drinking. It is a psychological disorder found more
commonly in women and children and cannot be diagnosed if there is a medical
reason the patient feels thirstyfor instance many medications give patients dry
mouth h In real practice primary polydipsia is a diagnosis of exclusion and should be
diagnosed cautiously. For test purposes however one can identify primary polydipsia
easily: there will be a steady, reliable and prompt increase in urine osmolality during
water deprivation studies and there will be a paltry response to vasopressin
administration. Both results were true for this particular patient. Additionally
patients with primary polydipsia will have low serum sodium and low serum
osmolality. Restriction of water intake normalizes urine output in patients with
primary polydipsia.
(Choice A) The pathology of central Dl is lack of adequate ADH. Desmopressin is a
synthetic form of ADH and the treatment of choice for central Dl.
(Choices B and C) Nephrogenic Dl is caused by a lack of response to ADH.
Hydrochlorothiazide causes increased water absorption from the proximal tubule
(remember ADH acts in the collecting tubule) and is used to treat nephrogenic Dl.
Alternatively indomethacin is sometimes used; it increases water absorption by
decreasing prostaglandin synthesis (prostaglandins inhibit ADH).
(Choice D) Low salt low protein diets are typically used in patients with renal failure.
Educational Objective:
During a water deprivation test most patients with primary polydipsia will
demonstrate a significant increase in urine osmolality. Additionally patients with
primary polydipsia will have low serum sodium and low serum osmolality. Restriction
of water intake normalizes urine output in patients with primary polydipsia.
252
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 55: A 61-year-old male presents to your office with a history of progressive
dyspnea. He can not tolerate moderate exertion and sleeps in a half-sitting
position due to orthopnea. He has also noticed some swelling of his ankles. He
does not smoke or consume alcohol. His past medical history is significant for
hypercholesterolemia and recurrent chest pain. Which of the following do you
expect to be increased in this patient?
A. Cardiac output
B. Renal perfusion
C. Arteriolar resistance
D. Mixed venous oxygen content
E. Lung compliance
Explanation:
The symptoms described in this clinical scenario are strongly suggestive of
congestive heart failure (CHF). Left-sided CHF frequently presents with dyspnea on
exertion, orthopnea (dyspnea while lying flat) and paroxysmal nocturnal dyspnea
(waking from sleep gasping for air). Symptoms of right-sided CHF include lower
extremity edema and hepatomegaly. Most commonly combined left- and rightventricular failure is observed owing to the fact that the most common cause of right
heart failure is left heart failure.
CHE occurs due to a progressive decrease in myocardial contractility (systolic
dysfunction) or due to inability of heart to relax sufficiently to accommodate
incoming blood in diastole (diastolic dysfunction). CHE of both origins ultimately
leads to decreased cardiac output and inadequate oxygen delivery to tissues.
Decreased perfusion of peripheral tissues induces a number of neuroendocrine
compensatory mechanisms, such as:
1. Renin-angiotensin-aldosterone mechanism: Decreased renal perfusion leads to
diminished stretch of glomerular afferent arterioles and increased synthesis of renin.
Increased renin is converted to angiotensin II, which is a potent vasoconstrictor. By
causing vasoconstriction, angiotensin II increases arterial resistance and after load
(Choice C). The failing heart is unable to pump blood to the tissues against the
increased afterload induced by angiotensin II, so tissue perfusion decreases and
more renin is secreted by the kidney creating a vicious circle. Angiotensin II also
stimulates the secretion of aldosterone which functions to increase the circulating
blood volume (preload) and further exacerbate CHR
2. Increased sympathetic output is stimulated by baroreceptors that sense
decreased perfusion. Epinephrine and norepinephrine increase heart rate and
contractility but these neurotransmitters also increase peripheral arterial resistance
thereby increasing afterload.
(Choice A) Cardiac output is decreased in both systolic and diastolic heart failure.
(Choice B) Decreased cardiac output leads to diminished perfusion of the viscera,
including the kidneys. Decreased renal perfusion activates the renin-angiotensinaldosterone mechanism.
(Choice D) As less arterial blood is delivered to peripheral tissues the contact of
tissues with venous blood is increased. Uptake of oxygen from venous blood is
higher, and mixed venous oxygen content is decreased.
(Choice E) Increased pressure in pulmonary circulation results in transudation of
fluid into the lung interstitium and air spaces. This decreases lung compliance and
oxygen diffusion.
253
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Decreased cardiac output triggers a number of compensatory mechanisms. Reninangiotensin-aldosterone activation and increased sympathetic output raise arterial
resistance (afterload) and exacerbate heart failure by making it more difficult for the
failing heart to pump blood to the tissues.
254
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 56: A 46-year-old Caucasian female is hospitalized for recurrent renal colic.
Her past medical history is significant for peptic ulcer disease for which she takes
famotidine daily. Her laboratory values are:
Serum sodium
140 mEq/L
Serum potassium
4.0 mEq/L
Chloride
103 mEq/L
Serum creatinine
0.8 mg/dL
Serum calcium
12.0 mg/dL
Serum phosphorus
2.4 mg/dL
24-hour urinary calcium excretion
350 mg (N 100-300 mg)
Which of the following changes in bone structure is most typical for this patients
condition?
A. Osteoid matrix accumulation around trabeculae
B. Trabecular thinning with fewer interconnections
C. Subperiosteal resorption with cystic degeneration
D. Lamellar bone structure resembling a mosaic
E. Spongiosa filling medullary canals with no mature trabeculae
Explanation:
The clinical features described here are most consistent with primary
hyperparathyroidism. Primary hyperparathyroidism is caused by a parathyroid
adenoma in 80-85% of patients and by parathyroid hyperplasia in the remaining 1O15%. (Parathyroid cancer is a very uncommon cause of primary
hyperparathyroidism.) The excess serum calcium found in hyperparathyroidism
occurs by three mechanisms: (1) an increase in the renal absorption of calcium, (2)
an increase in the gastrointestinal absorption of calcium indirectly, by 1, 25dihydroxjvitamin D formation (parathyroid hormone increases the formation of 1, 25
dihydroxyvitamin D in the kidneys), and (3) an increase in bone resorption by
osteoclast activation. The serum phosphorus in patients with hyperparathyroidism is
usually low because parathyroid hormone decreases phosphate resorption in the
proximal renal tubule.
For unclear reasons cortical or compact bone, in the appendicular skeleton (the
pectoral girdle, the pelvic girdle, and the limbs) is more commonly involved in
hyperparathyroidism. Subperiosteal thinning is a characteristic feature of
hyperparathyroidism. Radiologically this thinning appears as subperiosteal erosions
in the medial side of the second and third phalanxes of the hand, and there is a
granular salt-and-pepper appearance of the skull.
The cardinal clinical manifestations in patients with primary hyperparathyroidism,
are bone loss, renal stones, gastrointestinal upset (ulcers), and psychiatric disorders
(bones, stones, groans and psychic moans). These symptoms are described best
by older textbooks because most cases today are detected before any bone or
kidney symptoms occur. The present practice of routinely measuring calcium in the
chemistry profile allows patients to be diagnosed well before the onset of clinical
symptoms.
(Choice A) Histologically, vitamin D deficiency is characterized by excessive un
mineralized osteoid and widened osteoid seams. Patients with vitamin D deficiency
have low bone mineral densities and are at risk for fractures.
(Choice B) Trabecular thinning with fewer interconnections is characteristic of
osteoporosis. In osteoporosis, the total bone mass is decreased, and normal bone
architecture is disrupted.
255
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice D) A mosaic pattern of lamellar bone with irregular sections of lamellar
bone, linked by cement lines is seen in patients with Pagets disease of the bone.
The cement lines represent previous areas of bone resorption.
(Choice E) Osteopetrosis, also known as marble bone disease is caused by
decreased osteoclastic bone resorption. Histologically, osteopetrosis is characterized
by the persistence of primary; un mineralized spongiosa in the medullary canals. In
normal individuals bone marrow replaces the primary spongiosa.
Educational Objective:
Subperiosteal thinning is a characteristic feature of hyperparathyroidism.
Radiologically, this thinning appears as subperiosteal erosions in the medial sides of
the second and third phalanxes of the hand, and as a granular, salt-and pepper
appearance of the calvarium.
256
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 57: An infant with ambiguous genitalia is born to a 26-year-old woman
following an uncomplicated pregnancy. During the first week of life the infant
develops hypotension and hyperkalemia. Cytogenetic studies reveal a46XX
karyotype. The enzyme deficient in this patient is normally responsible for
which of the following transformations?
Cholesterol Pregnenolone
B. Progesterone 17-hydroryprogesterone
C. Testosterone Dihydrotestosterone
D. Progesterone 11-Deoxycorhcosterone
E. Androstenedione Testosterone
A.
Explanation:
Congenital adrenal hyperplasia (CAH) can result when there is a deficiency of an
enzyme of cortisol and/or aldosterone synthesis. CAH is a heterogenous group of
disorders because different enzymes may be involved. All types of CAH are inherited
in an autosomal recessive fashion. In 90% of cases 21-hydroxIase is the deficient
enzyme.
21-hydroxlase catalyzes both 11-deoxjcorticosterone and 11-deoxqcortisol
synthesis. 11-deoxjcorticosterone is the precursor of corticosterone, which is the
precursor of aldosterone, and 11-deoxytortisol is the precursor of cortisol. In 21hydroxjlase deficiency mineralocorticoid and glucocorticoid synthesis is decreased.
Upstream precursors accumulate as a result, and channel into testosterone synthesis
257
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
instead. Increased testosterone levels lead to ambiguous genitalia in girls
(virilization). Male children have normal genitalia. Salt-wasting occurs due to the
lack of mineralocorticoids. Affected infants often have recurrent vomiting,
dehydration, hypotension, hyponatremia and hyperkalemia. Deficiencies of 11hydroxlase and 17-hydroxlase can also cause CAH.
(Choice A) Desmolase catalyzes the conversion of cholesterol into pregnenolone.
Absence of this enzyme would lead to a complete absence of steroid hormones. An
infant with a total lack of desmolase would not survive.
(Choice B) Synthesis of 17-hydroxyprogesterone from progesterone is catalyzed by
17-hydroxilase. Deficiency of this enzyme leads to mineralocorticoid excess that
manifests with salt retention and hypertension. Patients are phenotypically female.
(Choice C) Dihydrotestosterone (DHT) is a biologically active metabolite of
testosterone formed by 5cc-reductase in the prostate gland testes. Hair follicles and
adrenal glands. Deficiency of (or insensitivity to) DH Tin utero is a cause of androgen
insensitivity syndrome.
(Choice E) Androstenedione is produced in the adrenals and the gonads as an
intermediate in the synthesis of testosterone estrone and estradiol. Impaired
androstenedione synthesis would lead to decreased levels of sex hormones.
Educational Objective:
21-hydroxylase deficiency is the most common form of congenital adrenal
hyperplasia. Affected female infants have ambiguous (virilized) genitalia. Saltwasting (vomiting hypotension and hyperkalemia) occurs due to mineralocorticoid
deficiency.
258
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 58: A 32-year-old Asian female presents to your office complaining of easy
fatigability and exertional dyspnea. Cardiac auscultation reveals an extra
diastolic sound and a diastolic murmur at the apex. You suspect mitral stenosis.
Cardiac catheterization findings are given on the slide below. Which of the
following corresponds to the opening snap (OS) timing in this patient?
A.
B.
C.
D.
E.
A
B
C
D
E
Explanation:
The opening snap (OS) in patents with mitral stenosis is an early diastolic sound due
to tensing of the abnormal mitral valve (MV) leaflets after the valve cusps have
completed their opening excursion. This occurs shortly after the mitral valve opens,
when left ventricular pressure drops below left atrial pressure. From the graph
above, it can be seen that the higher the early diastolic left atrial pressure the closer
the opening snap will tend to be to point B, which corresponds to the A2 component
of the heart sound. The A2-OS interval is inversely correlated with the severity of
mitral stenosis. The more severe the stenosis, the higher the steady state left atrial
pressure in early diastole and the shorter the A2-OS interval.
(Choice A) This point corresponds to the opening of the aortic valve at the end of
isovolumetric ventricular contraction in early systole, when the left ventricular
pressure exceeds the aortic pressure.
(Choice B) Point B corresponds to the closure of the aortic valve at the end of
systole, producing the A2 component of the second heart sound. The aortic valve
closes as soon as left ventricular pressure drops below the aortic pressure.
(Choice D) This is a random point in diastole, when the mitral valve is already
maximally open and ventricular filling is progressing. Note that there is a significant
gradient of pressure between the left atrium and left ventricle during diastole,
consistent with mitral stenosis. Under normal conditions, diastolic left atrial and left
ventricular pressures are nearly equal.
(Choice E) Point E roughly corresponds to the onset of atrial contraction during late
ventricular diastole. The mitral valve is still maximally open. Note the increase in the
gradient of pressure between the left atrium and left ventricle produced by atrial
contraction. This can cause presystolic accentuation of the diastolic murmur of mitral
stenosis.
Educational Objective:
Patients with mitral stenosis due to abnormal mitral valves may have an opening
snap (OS) in early diastole, shortly alter the aortic component of the second heart
sound (A2). The OS occurs shortly after the mitral valve opens.
259
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 59: A 12-year-old Caucasian male is found to have a wide, fixed splitting of
the second heart sound (82) on routine physical examination. He denies any
symptoms. If present, the congenital heart disease in this patient may require
surgical repair to prevent irreversible changes in the:
A. Right ventricle
B. Right atrium
C. Left ventricle
D. Left atrium
E. Pulmonary vessels
F. Coronary vessels
Explanation:
Wide fixed splitting of S2 that does not vary with respiration is a characteristic
auscultatory finding of an atrial septal defect (ASD). ASD creates a left-to-right
shunt because of the high pressure in the left atrium. The result is increased blood
flow through the pulmonary artery. The muscular pulmonary arteries may develop
laminated medial hypertrophy that can become so severe overtime as to increase
the pulmonary vascular resistance above the total systemic vascular resistance. At
this point the original left-to-right intracardiac shunt reverses, and flow becomes
right-to- left. This switch to right-to-left shunting manifests as late-onset cyanosis,
with clubbing and polycythemia. Eisenmenger syndrome is the name for reversal of
shunt flow through a congenital cardiac defect that occurs as a result of chronic
pulmonary hypertension. Overtime the pulmonary vascular sclerosis becomes
irreversible and closure of the cardiac septal defect can no longer be
hemodynamically tolerated by the right ventricle.
(Choices A and B) Pulmonary hypertension produced by an ASD could result in right
ventricular hypertrophy and right atrial enlargement. However, these changes are
not necessarily irreversible. If the pulmonary hypertension is corrected, the right
heart can revert to a more normal morphology.
(Choices C and D) Left ventricular failure is uncommon in patients with ASD. Left
atrial enlargement can be present due to volume overload but the main changes are
in the right side of the heart.
Educational Objective:
Wide fixed splitting of the second heart sound is a characteristic auscultatory finding
in patients with ASD. A hemodynamically significant ASD can produce chronic
pulmonary hypertension as a result of left-to-right intracardiac shunting.
Eisenmenger syndrome is the late-onset reversal of a left-to-right shunt due to
pulmonary vascular sclerosis resulting from chronic pulmonary hypertension. Closure
of the ASD may be required to prevent irreversible pulmonary vascular sclerosis and
a permanent Eisenmenger syndrome.
260
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 60: A 2-year-old female is undergoing evaluation for ambiguous genitalia. The
patient has high blood pressure on three consecutive visits as well as marginally low
serum potassium levels. Which of the following enzymes is most likely to be
deficient in this patient?
A. 17-hydroxqlase
B. 21-hydraqlase
C. 11-hydroxqlase
D. Desmolase
E. 5-alpha-reductase
Explanation:
Congenital adrenal hyperplasia (CAH) is a group of disorders that result from defects
in the enzyme pathway for cortisol biosynthesis in the adrenal gland. CAH can occur
as a result of any of five enzymatic defects (see steroidogenic pathway):
1. 17-hydroxylase
2. 21-hydroxylase (most common)
3. 11-hydroxylase
4. 20, 22-desmolase
261
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
5. 3-3-hydroxysteroid dehydrogenase
11-hydroxylase converts deoxycorticosterone to corticosterone and 11-deoxycortisol
to cortisol. When there is a deficiency of this enzyme the adrenal gland cannot
synthesize cortisol efficiently. Low cortisol levels stimulate pituitary production of
ACTHI which increases the production of adrenal androgens because the high levels
of cortisol precursors are diverted towards the adrenal androgen biosynthetic
pathway (see diagram). Therefore, female patients with 11-hydroxylase deficiency
develop ambiguous genitalia. Due to the block in aldosterone synthesis,
deoxycorticosterone is increased. Deoxycortisone has mineralocorticoid activity,
which leads to the development of low-renin hypertension.
(Choice A) 17-hydroxylase deficiency accounts for less than 1% of patients with
CAH. 17-hydroxylase converts pregnenolone to 17-hydroxypregnenolone and
progesterone to 17-hydroxyprogesterone. This enzymatic pathway is active in both
the adrenal glands as well as the gonads. Decreased cortisol production leads to
increased levels of ACTH thus stimulating the formation of deoxycorticosterone and
corticosterone by the adrenals and causing low-renin hypertension and hypokalemia.
In females, the genitalia are normal at birth. However, these females have delayed
puberty (no production of sex steroid) and are hypertensive (excessive production of
deoxycorticosterone). Males are under virilized and hypertensive.
(Choice B) 21-hydroxylase deficiency is the most common type of CAH accounting
for 90% of patients. The enzyme 21-hydroxylase is responsible for converting 17hydroxyprogesterone to 11-deoxycortisol in the zona fasciculata and progesterone to
deoxycorticosterone in the zona glomerulosa. Patients with 21-hydroxylase
deficiency will have features of androgen excess cortisol deficiency and
mineralocorticoid deficiency (hypotension).
(Choice D) 2022-desmolase converts cholesterol to pregnenolone. Because this is
the first enzyme in the steroidogenic pathway, the formation of all steroid hormones
is affected. Cholesterol and cholesterol esters accumulate in the adrenal glands.
(Choice E) 5--reductase deficiency causes ambiguous genitalia in males, as a result
of the defective conversion of testosterone to dihydrotestosterone. This is not a form
of CAH because cortisol production is not affected. Females with 5-a-reductase
deficiency do not have ambiguous genitalia.
Educational Objective:
11-hydroxylase deficiency typically results in excessive adrenal androgen and
mineralocorticoid production.
262
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 61: Bone mass is an important pathogenetic determinant of fracture risk. On
the graph below, bone mass versus lifetime curves are shown for two healthy,
fracture-free women. Which of the following factors is most consistent with curve
A?
A. Low body mass index (BMI)
B. Smoking history
C. Black race
D. Glucocorticoid therapy
E. Early menopause
Explanation:
Statistically black females have higher bone density than Caucasian females. The
reasons that bone mineral density is generally higher in people of African descent
are not entirely understood. It is known that adipose tissue serves as a site of extraovarian estrogen production: it has been postulated that perhaps black females have
more adipose tissue (fat) than white females. However adipose tissue cannot
account entirely for the differences, as multivariate analyses have shown higher
bone mass in black females even after adjustment for BMI. To confound matters
even more, the risk of fracture in black females is significantly lower than white
females at a given bone density.
(Choice A) Bone density increases with increasing BMI. A bodyweight of less than
127 pounds is a risk factor for low bone density and fragility fractures. Decreased
bone mineral density in low body weight females maybe related to lower estrogen
levels, as there is less adipose tissue to produce estrogen.
(Choice B) Current smoking is a major risk factor for osteoporosis and for
osteoporotic fractures. Smokers have significantly lower bone mineral density
compared to nonsmokers, a fact attributed to the antiestrogenic effect of smoking.
This decrease in estrogen also allows smokers to have a lower incidence of
fibrocystic breast disease and uterine cancer. This cancer reduction should not be an
implied incentive to smoke. The overall health effects of smoking are resoundingly
negative.
(Choice D) Chronic glucocorticoid use is associated with lower bone mineral density
for several reasons. Glucocorticoids decrease the gastrointestinal absorption of
calcium, inhibit collagen synthesis by osteoblasts, decrease gonadotrophin releasing
hormone (leading to hypogonadism), and increase urinary calcium loss. Despite
these adverse effects, life would be simply miserable or nearly impossible for some
patients without chronic steroid therapy. In these patients, glucocorticoid-induced
bone loss is treated by optimization of calcium and vitamin D intake and by the use
of bisphosphonates.
(Choice E) Menopause causes accelerated bone loss due to a decrease in estrogen.
Estrogens have an anabolic effect on bone by increasing osteoblastic activity and
decreasing osteoclastic activity.
Educational Objective:
Remember the risk factors for osteoporosis:
1. Smoking 2. Menopause 3. Corticosteroid therapy 4. Physical inactivity
5. Caucasian race (immutable) 6. Low total body weight 7. Alcohol use
263
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 62: A mutation affecting the trypsinogen molecule has recently been
described. The mutation affects the inactivating cleavage site of the
enzyme. Patients having this abnormality would most likely suffer from:
ulcer
B. Liver cirrhosis
C. Pancreatitis
D. Megaloblastic anemia
E. Gastric cancer
A.
Peptic
Explanation:
All pancreatic enzymes (except amylase and lipase) are synthesized and secreted in
inactive form to protect the pancreas from autodigestion. These inactive proenzymes
are then activated by trypsin in the duodenal lumen. Trypsin is produced from its
own precursor, trypsinogen, by the action of duodenal enterokinase. Activated
trypsin activates other trypsinogen molecules as well as the other proteolytic
enzymes.
The body has protective mechanisms to prevent trypsin from being prematurely
activated. Pancreatic secretory trypsin inhibitor (PSTI) secreted by pancreatic acinar
cells inhibits any trypsin abnormally activated within the pancreas. This protein
prevents trypsin-mediated activation of other proteolytic enzymes and autodigestion
of pancreatic tissue. When the inhibitory capacity of PSTI is exceeded by large
amounts of active trypsin, trypsin itself can serve as its own inhibitor.
Hereditary pancreatitis is a rare disorder that results from a mutation in the gene
that encodes the trypsinogen molecule. This mutation leads to the synthesis of
abnormal trypsinogen that is not susceptible to inhibition by either trypsin or PSTI.
Patients experience recurrent attacks of acute pancreatitis.
(Choices A and E) Peptic ulcer disease and gastric adenocarcinoma are strongly
associated with H. pylon infection.
(Choice B) Liver cirrhosis can be caused by any number of conditions, with
alcoholism and chronic hepatitis B and C being the most common. There is no
association with mutations of the trypsinogen gene.
(Choice D) Megaloblastic anemia is caused by deficiencies of vitamin B 12 and/or
folate. It is also associated with a number of drugs (such as methotrexate and
phenytoin) and some inborn metabolic errors.
Educational Objective:
Trypsin activates all proteolytic pancreatic enzymes including it self. If activated
prematurely (i.e. before reaching the duodenal lumen), it can cause autodigestion of
the pancreatic tissue. A number of inhibitory mechanisms exist to prevent premature
activation of trypsin. A gene mutation that renders trypsinogen insensitive to
inhibition causes hereditary pancreatitis.
264
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 63: A 74-year-old female presented to the ER with the sudden onset of severe
upper back pain. Physical examination shows point tenderness over the thoracic
vertebra. Neurological examination is unremarkable. X-ray of the spine reveals a
compression fracture of a thoracic vertebra. On the graph, area C shows the
normal relationship between the serum concentrations of calcium and parathyroid
hormone. Which of the following areas represent this patients metabolic state?
A. Area A
B. Area B
C. Area C
D. Area D
E. Area E
Explanation:
Osteoporosis is characterized by decreased bone strength resulting from low bone
mass and micro-architectural deterioration of bone tissue. The presence of a fragility
fracturea fracture due to minimal trauma such as after a fall from a standing
heightis strongly suggestive of osteoporosis. The World Health Organization (WHO)
has established a definition of osteoporosis based on bone measurement using dual
x-ray absorptiometry. The WHO defines osteoporosis in postmenopausal females as
a bone density that is 2.5 standard deviations below the mean bone mineral density
for young adult women. There are two different types of bones in the body. The
cortical or compact bone makes up the shafts of long bones and outer envelopes of
all bones. Postmenopausal osteoporosis typically involves cancellous bone, which is
predominantly present in the vertebral column, distal radius, hip, and neck of femur.
In primary osteoporosis, serum calcium and PTH are typically in the normal range.
(Choice A) Area A in the diagram reflects high serum PTH with low serum calcium.
This is usually seen in patients with renal failure or with vitamin D deficiency.
(Choices B and E) Area B reflects primary hyperparathyroidism. Area E shows high
calcium levels in the presence ot low PTH levels, seen in patients with PTHindependent causes of hypercalcemia. The increase in serum calcium suppresses the
secretion of PTH from normal parathyroid glands. Important causes of PTHindependent hypercalcemia include the humoral hypercalcemia of malignancy,
vitamin D toxicity, excessive of ingestion of calcium, thyrotoxicosis, and
immobilization.
(Choice D) In patients with hypoparathyroidism, low PTH levels cause hypocalcemia.
Educational Objective:
Patients with osteoporosis have low bone mass, resulting in increased susceptibility
for fragility fractures. In primary osteoporosis (osteoporosis not caused by a medical
disorder), serum calcium, phosphorus, and PTH levels are typically normal.
265
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 64: A 58-year-old Caucasian male with severe exertional angina is found to
have hypokinesia of the anterior wall of the left ventricle and a left ventricular
ejection fraction of 35% on transthoracic echocardiography. His past medical
history is significant for hypertension, diabetes and hypercholesterolemia. The
patient undergoes coronary artery bypass grafting (CABG) and his condition
improves significantly: hypokinesia is no longer evident and the ejection fraction
increases to 50%. This phenomenon is referred to as:
A. Ischemic preconditioning
B. Myocardial stunning
C. Hibernating myocardium
D. Reperfusion injury
E. Ventricular remodeling
Explanation:
Repetitive ischemia of cardiac myoc4es or persistent hypoperfusion of myocytes can
result in a chronic but reversible loss of contractile function, referred to as
hibernation. In hibernating myocardium, myocardial energy metabolism is reduced
but there is sufficient ATP to prevent contracture. There maybe increased gene
expression of TNF- and NOS (inhibitors of contraction), complex defects in calcium
cycling and excitation-contraction coupling, and/or decreased beta-adrenergic
receptor density. The syndrome of cardiac muscle hibernation can be reversed by
revascularization with CABG surgery or balloon angioplasty. The time-course of
contractile function recovery is variable, occurring within hours to months.
(Choice A) Ischemic preconditioning is the development of resistance to infarction by
cardiac myocytes exposed to prior repetitive non-lethal ischemia. Sublethal ischemic
insults can protect the affected myocardium against subsequent greater ischemic
insults.
(Choice B) Myocardial stunning is a less severe form of ischemia-induced reversible
loss of contractile function than hibernation. Brief ischemic episodes (c 30 minutes)
followed by reperfusion can produce myocardial stunning, and full recovery is usually
over hours to days. In contrast, the patient in the vignette appears to have had a
chronic depression of myocardial contractility. Repetitive stunning can result in
hibernation.
(Choice D) The patient in the vignette experienced a net improvement in myocardial
contractile function with reperfusion; thus reperfusion injury was not the
predominant process here. Reperfusion injury is further myocardial cell damage
beyond that associated with the initial ischemic event. Proposed mechanisms of
reperfusion injury include membrane damage from oxygen free radicals generated
by infiltrating leukocytes during reperfusion, intracellular calcium overload, and
apoptosis.
(Choice E) Ventricular remodeling involves chronic changes in the mass, volume,
shape, and myocyte composition of the heart, as a means of compensating for an
increased hemodynamic load. Normal myocardium adjacent to ischemic,
dysfunctional myocardium would be more likely to undergo remodeling than the
ischemic myocardium itself. In any case, the rapidly of this patients improvement
following revascularization indicates that the previously ischemic myocardium most
likely resumed contraction: remodeling would take significantly longer to exert any
significant effect.
A persistent or repetitive low flow state causes myocardial hibernation that can be
reversed by reperfusion. Myocardial stunning is a less severe form of ischemiainduced reversible loss of contractile function.
266
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Repetitive stunning can result in hibernation. Ischemic preconditioning is the
development of resistance to infarction by cardiac myocytes previously exposed to
repetitive non-lethal ischemia.
Ventricular remodeling involves chronic changes in mass volume. Shape and
myocyte composition of the heart, to compensate for an increased hemodynamic
load.
267
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 65: A 72-year-old Caucasian male has a presystolic sound on cardiac
auscultation that immediately precedes the first heart sound and is best
heard when the patient turns to his left side and holds his breath. The
patients blood pressure is 150/90 mmHg and his heart rate is 74 beats per
minute and regular. He has a long history of hypertension and evidence of
extensive calcinosis around the mitral and aortic valves on chest x-ray. The
extra sound is most likely due
Increased flow velocity through the aortic valve
B. Restricted motion of the aortic valve cusps
C. Restricted motion of the mitral valve cusps
D. Papillary muscle tension after the rapid filling of the ventricles
E. Increased stiffness of the left ventricular wall
A.
Explanation:
An S4 gallop (also known as an atrial sound or atrial gallop) is a presystolic sound on
cardiac auscultation that immediately precedes S1. A left-sided S4 is heard best at
the cardiac apex with the patient in the left lateral decubitus position, and a rightsided S4 is heard best along the lower left sternal border (the tricuspid area) with
the patient in the supine position.
An S4 is heard when there is a sudden rise in end diastolic ventricular pressure
caused by atrial contraction against a ventricle that has reached the limit of its
compliance. Thus, an S4 may be present in any condition that causes a stiff
ventricle. Degenerative mitral annular calcification or aortic valve calcification can be
associated with chronically elevated LV pressures and systemic hypertension. This
patient probably has left ventricular hypertrophy (LVH) associated with hypertensive
heart disease. LVH reduces ventricular compliance and can cause diastolic
dysfunction. A normal atrial contraction is required to generate an S4.
(Choice A) This would tend to produce the murmur of aortic stenosis, an ejectiontype murmur that occurs during systole (after S1 and before A2).
(Choice B) Restricted motion of the aortic valve cusps might be associated with an
aortic ejection click, aortic stenosis, and/or aortic regurgitation. In any event, the
extra sound(s) produced would occur after S1, during systole.
(Choice C) Restricted motion of the mitral valve cusps could result in abnormal
diastolic sounds, like an opening snap and/or a murmur of mitral stenosis (MS). The
opening snap would occur early in diastole. Pre-systolic accentuation (due to atrial
contraction) of an otherwise inaudible murmur of MS could explain the extra sound
heard in this patient. However, isolated MS is generally associated with normal or
reduced left ventricular pressures making degenerative mitral annular calcification as
seen in this patient less likely.
(Choice D)The papillary muscles are not placed under increased tension during
diastolic ventricular filling. They are tensed during ventricular systole, after S1.
Educational Objective:
A presystolic sound on cardiac auscultation that immediately precedes S1 is most
often an S4 gallop. An S4 requires normal atrial contraction and results from rapid
emptying of atrial blood into a ventricle with reduced compliance (stiff ventricle).
268
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 66: A 30-year-old female with type 1 diabetes is being evaluated for anorexia,
weight loss and decreased insulin requirement. Physical examination shows
generalized hyperpigmentation. An ACTH stimulation test fails to elicit an increase in
her serum cortisol levels. Which of the following set of laboratory values is most
likely present in this woman?
Explanation:
The patient described in the vignette has features of primary adrenal insufficiency.
As a patient with type 1 diabetes mellitus (a disorder that results from the
autoimmune destruction of pancreatic -cells), she is prone to develop other
autoimmune disorders, including autoimmune adrenalitis. Autoimmune adrenalitis is
a condition where all three zones of the adrenal cortex are attacked by the bodys
immune system, resulting in primary adrenal insufficiency (primary because the
defect is inherent to the adrenal itself). In primary adrenal insufficiency,
administration of exogenous ACTH does not increase serum cortisol levels.
Autoimmune adrenalitis typically spares the adrenal medulla.
Typical biochemical abnormalities in patients with primary adrenal insufficiency
include hyponatremia, hyperkalemia, hypochloremia, and metabolic acidosis. In
patients with secondary and tertiary adrenal insufficiency (due to defects in the
pituitary and hypothalamus, respectively), a deficiency of mineralocorticoid does not
usually occur. Thus, these patients do not develop hyperkalemia or metabolic
acidosis. Patients with secondary and tertiary adrenal insufficiency will typically
respond with a serum cortisol increase when exogenous ACTH is administered.
(Choices A and D)These choices show biochemical abnormalities characteristic of
mineralocorticoid (i.e. aldosterone) excess. Elevated aldosterone levels lead to
sodium retention, potassium loss, and bicarbonate retention. Thus, hypokalemia and
metabolic alkalosis are common in this condition. Hypernatremia, however, does not
usually occur, due to the phenomenon of aldosterone escape, whereby initial
increases in sodium and chloride resorption lead to intravascular hypervolemia,
which in turn causes release of atrial natriuretic peptide, leading to diuresis and
compensatory sodium loss.
(Choice C) The finding of hyponatremia, hypokalemia, and hypochloremia with
metabolic alkalosis suggests diuretic use. Diuretics lead to urinary loss of sodium,
potassium and chloride, while promoting increased bicarbonate absorption secondary
to volume contraction (contraction alkalosis).
(Choice E) Normal serum sodium in the setting of hypokalemia and metabolic
acidosis is suggestive of renal tubular acidosis (RTA).
Educational Objective: Patients with type 1 diabetes mellitus are prone to develop
other autoimmune endocrinopathies, including Hashimoto thyroiditis, Graves
disease, and Addisons disease (hypoadrenocorticism). These patients are at
increased risk for other non-endocrine autoimmune disorders as well, including
vitiligo and pernicious anemia.
269
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 67: A 33-year-old Hispanic female who recently emigrated from Mexico is
brought to the ER with severe shortness of breath and hemoptysis. She is
A.
treated with diuretics, and begins to feel better. However, she develops rightsided hemiparesis soon after. Based on the history and initial physical
examination, you suspect mitral stenosis is responsible. Which of the following
findings suggests an associated lesion or another diagnosis in this patient?
Right ventricular dilation
B. Increased systolic pulmonary artery pressure
C. Increased pulmonary capillary wedge pressure
D. Tricuspid regurgitation
E. Increased diastolic left ventricular pressure
F. Reduced pulmonary compliance
Explanation:
In isolated mitral stenosis (MS) diastolic pressures in the left ventricle (LV) are
usually near normal. Only pressures proximal to the stenotic mitral valve would be
markedly elevated. When a patient with suspected MS is also found to have an
increased LV end diastolic pressure, the presence of an additional lesion is likely.
Possibilities include rheumatic involvement of the aortic valve (which typically causes
combined aortic stenosis and regurgitation), or infective endocarditis superimposed
on an aortic valve deformed by chronic rheumatic heart disease (RHD). In patients
with RHDI the mitral valve alone is the sole site of involvement in 65% to 70% of
cases. Both the mitral and aortic valves are affected in about 25% of cases. This
patients right-sided hemiparesis may have arisen from an embolic stroke
complicating isolated MS (via atrial dilatation, atrial mural thrombosis and
thromboembolism) or from an aortic valve vegetation generated by endocarditis.
(Choice A) Right ventricular dilatation is found in mitral stenosis that is severe
enough to cause significant pulmonary hypertension.
(Choice B) This finding would be expected in isolated mitral stenosis severe enough
to cause significant pulmonary hypertension via backward transmission of elevated
left atrial pressure.
(Choice C) This finding would be expected in isolated mitral stenosis (MS) severe
enough to cause a significant elevation of left atrial pressure. A properly measured
pulmonary capillary wedge pressure reflects the left atrial transmural pressure at
end diastole, which is elevated in MS, even though left ventricular end diastolic
transmural pressure (LVEDP) may be normal. Note that the wedge pressure does
not reflect LVEDP in patients with MS.
(Choice D) Tricuspid regurgitation may occur as a complication of severe isolated
mitral stenosis, as a consequence of right ventricular dilatation due to pulmonary
hypertension.
(Choice F) Reduced pulmonary vascular compliance may complicate long-standing
pulmonary hypertension induced by isolated mitral stenosis. Pulmonary vascular
endothelial dysfunction and reactive vasoconstriction can result from pulmonary
hypertension. Chronic pulmonary hypertension can also cause reactive hypertrophy
in the walls of pulmonary vessels (pulmonary vascular sclerosis). Both of these
processes reduce pulmonary vascular compliance.
Educational Objective: Isolated mitral stenosis (MS) elevates the left atrial end
diastolic pressure and can therefore cause an elevated pulmonary capillary wedge
pressure (PCWP) pulmonary hypertension, pulmonary vascular sclerosis and
decreased compliance, right ventricular dilatation, and functional tricuspid
regurgitation. Note that in patients with isolated MS, PCWP does not reflect the left
ventricular end diastolic pressure which maybe normal.
270
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 68: A 46-year-old Caucasian female presents to your office because of easy
fatigability and exertional dyspnea. Auscultation of the heart reveals a diminished
first heart sound and an apical holosystolic murmur radiating to the axilla. Lungs
have bibasilar crackles. There is no elevation of jugular venous pressure or
peripheral edema. Which of the following would most likely increase forward-toregurgitant volume ratio in this patient?
A. Decreasing left ventricular preload
B. Increasing left ventricular contractility
C. Decreasing left ventricular afterload
D. Decreasing heart rate
E. Increasing left ventricular volume
Explanation:
This patient has clinical features suggestive of mitral regurgitation with left sided
heart failure. In a patient with mitral regurgitation, some of the blood in the left
ventricle is pumped forward through the aortic valve and is considered the forward
stroke volume (FSV) while some is forced backwards through the incompetent mitral
valve into the left atrium and is considered the regurgitant stroke volume (RSV). If
the systolic retrograde flow resistance between the LV and LA, the preload (LV end
diastolic volume) and the contractility remain the same, the amount of blood that
flows forward and backward is determined by the left ventricular afterload (or
systolic intraventricular pressure). The lower the average LV afterload, the lower will
be the average systolic pressure gradient driving regurgitant flow into the LA and
the lower will be the RSV. Moreover, FSV will be increased. This will increase the
forward-to-regurgitant volume ratio. Thus arterial vasodilator therapy, which acts to
decrease LV afterload, tends to decrease RSV and increase FSV in patients with MR.
(Choice A) LV preload reduction might decrease the regurgitant flow fraction if the
degree of mitral valve incompetence was LV end diastolic volume dependent (eg. in
dilated cardiomyopathy) or if the reduction in LV preload was also accompanied by a
slight decrease in LV afterload. However these effects on the regurgitant flow
fraction would generally be quantitatively less than that of a significant reduction of
afterload.
(Choice B) For a fixed anatomical degree of mitral valve incompetence producing
mitral regurgitation (MR) and at a given left ventricular preload, an increase in LV
contractility would tend to increase LV afterload. The latter would tend to increase
the fraction of each LV stroke volume going into regurgitant flow. Thus an isolated
increase in LV contractility would tend to increase MR. Partly for this reason some
experts recommend chronic beta blocker therapy for patients with significant MR.
(Choice D) A primary decrease in heart rate (HR) would tend to increase LV end
diastolic volume (preload). In the new steady state after recruitment of
cardiovascular reflexes to maintain forward LV output and mean systemic arterial
pressure LV afterload might not be significantly changed. Moreover in some cases of
MR where LV dilatation alone maybe responsible the fraction of regurgitant flow can
increase as the LV dilates further (as preload is increased). Under these conditions a
primary decrease in heart rate could decrease the forward to regurgitant LV output
ratio.
(Choice E) Presumably this choice means increasing LV end diastolic volume or
preload. As explained above increasing LV preload does not significantly alter steady
state LV afterload, the major determinant of the degree of mitral regurgitation.
Moreover LV dilatation alone can contribute to or worsen MR.
271
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
The major determinant of the ratio of forward-to-regurgitant left ventricular (LV)
output in patients with mitral regurgitation (MR) is LV afterload. An increase in
steady state LV afterload tends to decrease this ratio. An increase in steady state LV
end diastolic volume may contribute to or worsen MR.
272
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 69: A 60-year-old Caucasian male presents to your office for a routine checkup. He has no complaints. His blood pressure is 165/110 mmHg, and heart rate is
75/mm. Physical examination reveals a moderately overweight man
(BMI = 28.3 kg/m2) with predominantly central fat distribution. Lab work
demonstrates a blood glucose level of 150 mg/dL. If present, which of the following
is most likely responsible for the resistance of peripheral tissues to the action of
insulin in this patient?
A. High low density lipoprotein (LDL)
B. Low high density lipoprotein (HDL)
C. High free fairy acids (FFA)
D. High serum C-peptide level
E. High serum beta-hydroxybutyrate
F. High homocysteine
Explanation:
One of the important actions of insulin is the facilitation of glucose uptake by
adipocytes and muscle cells. Several genetic and environmental factors can cause
insulin resistance. High free fa1ti acid levels are one environmental factor that
results in insulin resistance. The mechanism by which free fatty acid induces insulin
resistance is unclear. Serine phosphorylation of the insulin receptors beta subunit
could be involved. This phosphorylation of serine interferes with down-stream
signaling because serine kinase, instead of tyrosine kinase, becomes activated.
Serine phosphorylation is a known mechanism of insulin resistance induced by TNEalpha, glucagon, and glucocorticoids. Free fatty acids also act to decrease insulin
secretion, which prevents the compensatory rise of insulin that is required to
overcome insulin resistance. The induction of insulin resistance and beta cell
dysfunction along with high free fatty acids is termed lipo toxicity. Lowering free
fatty acids improves beta cell function and insulin resistance. The other choices
listed do not interfere with insulin secretion or insulin action.
(Choices A and B) LDL is metabolized by receptor-mediated endocytosis, mainly in
the liver. LDL levels are governed by diet, liver production, and receptor-mediated
LDL uptake. Insulin is not directly involved in LDL metabolism. High serum
triglycerides and free fatty acids are commonly seen in insulin resistance and
uncontrolled diabetes mellitus. The surface phospholipids in LDL particles are
replaced by triglycerides in diabetics. The subsequent removal of surface triglyceride
in the liver by hepatic lipase results in highly atherogenic small dense LDL particles.
Serum HDL is generally low in diabetics because the altered cell surface composition
accelerates the clearance of HDL. In contrast to free fatty acids, LDL and HDL do not
alter insulin signaling. (Choice D) C-peptide is secreted in equimolar amount with
insulin from pancreatic beta cells. It is true that increased C-peptide levels are
present in insulin resistance, but C-peptide does not have any biological effect.
(Choice E) Beta hydroxybutyrate is a marker of insulin deficiency and would be
present only in type 1 diabetes mellitus. Patients with type 2 diabetes mellitus do
not have high beta hydroxybutyrate because they do not have absolute deficiency of
circulating insulin. Beta hydroxybutyrates do not interfere with the actions of insulin.
(Choice F) Homocystinemia has been linked to atherosclerosis. Lowering of
homocysteine levels by folic acid treatment has been shown to decrease the
progression of atherosclerosis in some studies. However, high homocysteine levels
do not interfere with insulin action.
Educational Objective: EEA and serum triglycerides are believed to increase insulin
resistance in overweight individuals.
273
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 70: A 40-year-old Caucasian female is hospitalized by a femoral neck fracture
after falling from a standing heightmore specifically, she slipped in the tub. Three
years ago, she was diagnosed with a prolactinoma, but she has refused treatment.
The tumor has not significantly increased in size over the last two years nor has it
caused any visual deficits. The pathophysiology underling this patients
susceptibility to bone fracture is additionally responsible for which of the following?
A. Stomach ulcers
B. Vaginal dryness
C. Kidney stones
D. Hand tremor
E. Swallowing difficulty
Explanation:
Prolactinomas are the most common pituitary tumors. In females prolactinomas
typically cause amenorrhea and galactorrhea. Reproductive dysfunction occurs
because high levels of prolactin suppress gonadotrophin-releasing hormone (GnRH)
from the hypothalamus, leading to hypogonadism, anovulation, and amenorrhea.
The direct effect of prolactin on the breasts causes milk discharge (galactorrhea).
If hyperprolactinemia is not treated, prolonged hypogonadism (low estrogen) causes
accelerated bone loss, exactly as occurs with postmenopausal
osteopenia/osteoporosis. Low bone density puts patients at a high risk for fragility
fractures (fractures sustained with minimal trauma such as fall from standing height,
also called pathological fractures). Low bone density and vaginal dryness are very
frequent sequelae of decreased estrogen.
Other causes of accelerated bone loss include hyperparathyroidism,
hyperthyroidism, chronic glucocorticoid excess, and vitamin D deficiency. All of these
causes of low bone density should be ruled out in patients with significantly low bone
density.
(Choices A and C) Hyperparathyroidism can cause kidney stones, probably as a
result of high serum calcium. Stomach ulcers can occur with isolated
hyperparathyroidism or with the MEN-associated Zollinger-Ellison syndrome of
excess gastrin.
(Choices D and E) Hyperthyroidism causes hand tremors and an enlarged thyroid
that can make it difficulty to swallow.
Educational Objective:
Low bone density is a well known complication of hyperprolactinemia that is
associated with prolactin-induced hypogonadism (ie, low estrogen). Vaginal dryness
is another very common manifestation of estrogen deficiency.
274
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 71: A male patient is being evaluated for progressive shortness of breath. His
flow-volume curve is pictured below. Which of the following pathologic findings is
most likely in this patient?
A. Pulmonary fibrosis
B. Alveolar hyaline membranes
C. Interalveolar wall destruction
D. Intraalveolar hemorrhage
E. Thromboembolic disease
F. Compression atelectasis
Explanation:
This patients flow-volume loop exhibits a marked reduction in expiratory flow rate
compared to the normal loop. Moreover, the patients residual lung volume (RVI at
end expiration) is increased and tidal volume is decreased compared to normal.
These abnormalities are characteristic of chronic obstructive pulmonary disease
(COPD). An obstructive flow-volume loop profile may result from increased bronchial
resistance (e.g. due to anatomic narrowing as in chronic bronchitis) and/or from
decreased lung elasticity (e.g. due to destruction of interalveolar walls as in
emphysema). Decreased lung elasticity also promotes dynamic compression of
otherwise normal airways during expiration, contributing to increased expiratory
airflow resistance in bronchi. The expiratory airflow obstruction in chronic bronchitis
and/or emphysema causes hyperinflation (increased RV) and decreased tidal
volumes.
(Choice A) Pulmonary fibrosis tends to decrease lung volume and compliance,
producing a restrictive pattern in spirometric flow volume loops, as shown by the red
curve below.
Note that in restrictive diseases, tidal volume and residual volume are reduced but
the expiratory flow rate may be normal or only modestly reduced.
275
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice B) Alveolar hyaline membranes tend to reduce lung compliance, causing a
restrictive flow-volume pattern.
(Choice D) Diffuse intraalveolar hemorrhage would tend to dilute alveolar surfactant,
thus increasing alveolar surface tension and promoting alveolar atelectasis. These
changes would reduce lung volumes and lung compliance. A restrictive flow-volume
pattern would likely result.
(Choice E) In thromboembolism, only perfusion is limited; there is no effect on
ventilation. Therefore, pulmonary function tests would not be affected.
(Choice F) Atelectasis due to extrinsic pulmonary compression may occur when part
or all of the pleural cavity is filled by air (as in pneumothorax), fluid, exudate,
and/or blood. Under such conditions, lung volumes and total lung compliance would
likely be reduced, producing a restrictive flow-volume pattern on spirometry.
Educational Objective:
Reduced expiratory air flow velocity, decreased tidal volume, and increased residual
volume together characterize chronic obstructive pulmonary disease (COPD).
Chronic bronchitis and/or emphysematous destruction of interalveolar walls maybe
responsible. In comparison, restrictive lung disorders tend to decrease all lung
volumes without significantly affecting expiratory flow rates.
276
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 72: A 24-year-old male presents to your office complaining of paroxysmal
episodes of breathlessness and wheezing. Sputum microscopy shows many
granule-containing cells and crystalloid masses. The sputum findings suggest
the role of which of the following substances in this patients condition?
B. lL-3
C. lL4
D. lL5
E. y-Interferon
F. TGF-3
A.
lL1
Explanation:
Paroxysmal breathlessness and wheezing in a young patient unrelated to ingestion
of aspirin pulmonary infection, inhaled irritants, stress, and/or and exercise should
raise a strong suspicion for extrinsic allergic asthma. The granule- containing cells in
the sputum are most likely eosinophils and the crystalloid bodies are most likely
Charcot-Leyden crystals (contain eosinophil membrane protein). Chronic eosinophilic
bronchitis in asthmatics involves bronchial wall infiltration by numerous activated
eosinophils, largely in response to IL-5 released by allergen-activated TH2 cells.
(Choice A) Although macrophage IL-i release is involved in asthma pathogenesis, itis
a not specific for this process. IL-i release is a component of almost all inflammatory
processes, and does not necessarily cause eosinophil infiltration.
(Choice B) IL- functions mainly to promote the growth and differentiation of bone
marrow stem cells.
(Choice C) Release of IL-4 by TH2 type helper T-cells is a non-specific pathway
involved in the stimulation of B-cell antibody production. IL- 4 is not chemotactic for
eosinophils, however.
(Choice E) y-Interferon is secreted by helper l-cells and functions to activate
macrophages, thereby promoting adaptive immunity against intracellular pathogens.
It is not directly chemotactic for eosinophils.
(Choice F) Transforming growth factor beta (TGE-3) is growth factor involved in
tissue regeneration and repair.
Educational Objective:
Paroxysmal breathlessness and wheezing in a young patient that is unrelated to
ingestion of aspirin pulmonary infection, inhalation of irritants, stress, and/or and
exercise should raise a strong suspicion for extrinsic allergic asthma. Classic sputum
findings include eosinophils and Charcot-Leyden crystals. Eosinophils are recruited
and activated bylL-5 secreted bVTH2 type helper l-cells.
277
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 73: A 56-year-old male presents to your office with progressive vision
impairment. His past medical history includes diabetes mellitus,
hypertension and gout. Physical examination suggests bilateral clouding of
the lens in this patient. Which of the following metabolic conversions in the
peripheral tissues most likely contributed to this patients current condition?
Galactitol to sorbitol
B. Glucose to sorbitol
C. Fructose to galactitol
D. Glucose to glyceraldehyde
F. Adenine to uric acid
A.
Explanation:
Complications of long-standing diabetes mellitus such as microangiopathy,
retinopathy nephropathy and peripheral neuropathy occur at least in part due to
chronic hyperglycemia that induces a number of metabolic changes. The most
important mechanisms involved in the development of complications are:
1. Advanced glycosylation end products: Glycosylation refers to the attachment of
glucose to amino acid residues in various proteins forming reversible glycosylation
products that slowly stabilize to irreversible products. Glycosylation products
accumulate and cross-links with collagen in blood vessel walls and interstitial tissues
contributing to microangiopathy and nephropathy. Cross-linking of proteins by
glycosylation products also facilitates inflammatory cell invasion and deposition of
LDL in the vascular walls leading to atherosclerosis.
2. Polyol pathway impairment occurs in tissues that do not depend on insulin for
glucose transport (lens, peripheral nerves, blood vessels and kidneys).
Hyperglycemia results in increased intracellular glucose concentrations in these
tissues. Glucose undergoes conversion into sorbitol (Choice B) by aldose reductase,
and sorbitol, in turn, is converted into fructose. Sorbitol and fructose increase the
osmotic pressure in tissues and stimulate the influx of water leading to osmotic
cellular injury. Increased water in lens fiber cells leads to rupture of these cells with
resultant opacification of the lens and cataract formation. Osmotic injury of Schwann
cells contributes to peripheral neuropathy in diabetes.
(Choice A) Aldose reductase coverts galactose into galactitol. If the level of galactose
is increased, such as in galactosemia, more galactitol is produced. Elevated galactitol
levels cause cataracts in patients with galactosemia. Synthesis of galactitol is not
increased in DM.
(Choice C) Galactitol is produced from galactose, not from fructose.
(Choice D) In the hexose monophosphate pathway, glucose is converted to
glyceraldehyde-3-phosphate that can enter glycolysis. This metabolic pathway does
not play any role in development of diabetic complications.
(Choice E) Deficiency of enzyme adenosine deaminase impairs the conversion of
adenosine to uric acid. This enzyme is absent or defective in severe combined
immunodeficiency (SCID).
Educational Objective:
During hyperglycemia, excess plasma glucose is converted to sorbitol by aldose
reductase. Sorbitol accumulates within some cels and attracts water into these
tissues leading to osmotic cellular injury. This mechanism is implicated in the
pathophysiology of cataracts and peripheral neuropathy in diabetes.
278
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 74: A genetically female infant born to a 23-year-old female demonstrates
ambiguous genitalia and a normal-sized uterus. Blood pressure is normal, but
serum testosterone and androstenedione levels are increased. The mother
experienced increased facial hair growth and some voice deepening during
pregnancy. Which of the following is most likely deficient in the newborn?
A. 21-hydroxylase
B. Aromatase
C. 17-hydroxylase
D. 5-reductase
F. HMG CoA reductase
Explanation:
Aromatase is an enzyme that converts androstenedione to estrone and testosterone
to estradiol. These metabolic steps are essential in estrogen synthesis and occur in
numerous tissues including the ovari, testis placenta, brain, liver, muscle and
adipose tissue.
Aromatase deficiency manifests early in embryonal life with high androgen levels
and low estrogen levels in the female fetus. This hormonal imbalance can affect the
mother causing virilization during pregnancy due to the transfer of excess androgens
into the maternal circulation via the placenta. At birth, affected female infants have
ambiguous or male-type external genitalia (female pseudohermaphrodism). Females
with aromatase deficiency have primary amenorrhea and tall stature because
estrogen is necessary for fusion of the epi physes. Males with this defect exhibit tall
stature and osteoporosis with no genital abnormalities.
Increased aromatase levels, on the other hand, lead to estrogen excess causing
gynecomastia in boys and precocious puberty in girls. Patients of both sexes have
short stature due to early closure of the epiphyses.
(Choice A) 21-hydroxqlase deficiency is the most common tqpe of congenital adrenal
hyperplasia (CAH). It presents with ambiguous genitalia in the female fetus and salt
wasting resulting in hypotension, hyponatremia and hyperkalemia.
(Choice C) 1 7-hydroxylase deficiency is a rare form of congenital adrenal
hyperplasia (CAH). Its symptoms include sodium retention hypertension, and
ambiguous genitalia in the male fetus.
(Choice D) Deficiency of 5a-reductase leads to decreased synthesis of
dihydrotestosterone (DHT) in the male fetus. Affected infants have feminized
external genitalia at birth, and experience virilization at puberty.
(Choice E) HMG CoA reductase catalyzes the first step in the cholesterol synthesis
pathway. It is the target of the statin class of lipid-lowering drugs. This enzyme is
not involved in sexual differentiation.
Educational Objective:
Aromatase converts androgens into estrogens in the ovaries, testes, placenta and
other peripheral tissues. Genetic deficiency of this enzyme leads to an inability to
synthesize estrogens. It presents with maternal virilization during pregnancy and
masculinization of the female fetus.
279
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 75: A 50-year-old Caucasian female presents to your office with periodic
flatulence, abdominal pain and explosive diarrhea. After careful history taking,
you suspect lactase deficiency as the cause of this patients symptoms. If your
diagnosis is correct, which of the following is most likely to decrease on lactose
challenge in this patient?
Stool osmotic gap
B. Stool pH
C. Breath hydrogen content
D. D-xylose absorption
E. Cobalamin absorption
A.
Explanation:
Congenital lactase deficiency is a rare autosomal recessive condition caused by a
gene near (but separate from) the lactase gene, with affected newborns exposed to
lactose experiencing explosive watery diarrhea. The more common form of lactose
intolerance is acquired lactase deficiency, which occurs in 80-95% of Native
Americans, 90% of some Asians, 65-75% of Africans and African Americans, and
50% of Hispanics: in these groups, symptoms appear by mid- childhood once
intestinal lactase levels have plummeted. Lastly, some individuals appear to
experience lactose malabsorption secondary to bacterial overgrowth or mucosal
injury of the gastrointestinal tract.
Lactase deficiency by any means causes incomplete hydrolysis of the disaccharide
lactose into the monosaccharides glucose and galactose. The undigested lactose
then accumulates within the gastrointestinal lumen, leading to osmotic diarrhea.
Bacterial fermentation of lactose produces short-chain fatty acids and excess
amounts of hydrogen. The presence of this hydrogen acidifies the stool, lowering its
pH.
The lactose tolerance test entails the oral administration of 50 g of lactose, with
blood levels measured at 0, 60, and 120 minutes. If the blood glucose increases c 20
mg/dL and the individual experiences symptoms (eg, abdominal pain, bloating,
flatulence, diarrhea, or vomiting), the diagnosis of lactose intolerance is confirmed.
(Choice A) At its maximum, stool osmolality approaches serum osmolality
(approximately 290 mOsm/kg). Most stool osmolality is accounted for by sodium
and potassium, with colonic fermentation products composing the remainder (ie, the
stool osmotic gap). When electrolytes comprise most of the luminal osmolality, the
stool osmotic gap is low (c 50 mOsm/kg). When poorly absorbable substances are
present, the stool osmotic gap is large (> 100 mOsm/kg). Therefore, the stool
osmotic gap will be increased in lactase-deficient patients.
(Choice C) Breath hydrogen content increases by more than 20 ppm in lactasedeficient patients and can be measured in exhaled air by gas chromatography.
(Choice D) D-xylose absorption can be diminished in numerous malabsorptive
conditions, including celiac sprue. It is not classically associated with lactose
intolerance.
(Choice E) Cobalamin (vitamin B 12) absorption is hindered in patients with
pernicious anemia. It is not classically associated with lactose intolerance.
Educational Objective:
Lactase-deficient individuals have increased stool osmotic gap, increased breath
hydrogen content, and decreased stool pH upon lactose challenge.
280
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 76: A 64-year-old male with uncontrolled diabetes and hypertension is
evaluated for fatigue. His laboratory studies show a BUN of 75 mg/dL and
creatinine of 5.8 mg/dL. On the graph, area C shows the normal
relationship between serum concentrations of calcium and parathyroid
hormone. Which of the following areas represent this patients metabolic
state?
A. Area A
B. Area B
C. Area C
D. Area D
E. Area E
Explanation:
Parathyroid hormone (PTH) is one of the principal regulators in keeping serum
calcium within a tight normal range. PTH increases serum calcium by increasing
osteoclastic bone resorption, increasing the distal tubular absorption of calcium. and
increasing the formation of 1, 25-dihydroxvitamin D through up-regulation of the
renal enzyme 1-alpha hydroxylase. 1, 25-dihydox vitamin D increases the
gastrointestinal absorption of calcium. When PTH has adequately increased serum
calcium, calcium-sensing receptors present on the parathyroid discourage the
further secretion of PTH in a classic feedback loop.
This patient is in renal failure, as demonstrated by his BUN and creatinine levels. The
activity of renal 1-alpha hydroxylase is decreased in chronic kidney disease which
causes the decreased formation of 125-dihyroxyvitamin
D. The gastrointestinal absorption of calcium is consequently decreased; the
ultimate result is a decrease in serum calcium. Another electrol4e change is the
elevation of phosphorous because chronic renal disease impairs its excretion. The
result of the decrease in 125-dihydroxjvitamin D the decrease in serum calcium, and
the increase in serum phosphorus is an increase in the secretion of parathyroid
hormone, a state termed secondary hyperparathyroidism. Despite excess PTH,
calcium levels remain in the normal to only slightly low range; PTH is unable to
increase the serum calcium because of the deficiency in 1-alpha hydroxylase. Area A
on the graph demonstrates high PTH despite low calcium levels.
(Choice B) Area B in this diagram reflects the effects primary hyperparathyroidism.
Because the production of PTH is not subject to negative feedback in these patients,
high calcium levels are unable to suppress the secretion of PTH.
(Choice D) In patients with hypoparathyroidism, low PTH levels are accompanied by
hypocalcemia and hyperphosphatemia.
(Choice E) Area E shows high calcium levels in the presence of low PTH levels. This
is seen in patients with PTH independent causes of hypercalcemia. Important causes
of PTH-independent causes of hypercalcemia include the humoral hypercalcemia of
malignancy, vitamin D toxicity, excessive ingestion of calcium, thyrotoxicosis, and
immobilization (calcium is resorbed from inactive bones).
281
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Secondary hyperparathyroidism is seen in patients with chronic renal failure. These
patients have an elevated serum PTH accompanied by normal to low serum calcium
levels, and high serum phosphorus levels. Circulating 1, 25 dihydroxy vitamin D
levels are low due to the deficiency of 1-alpha hydroxylase, an enzyme that resides
in the kidneys.
282
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 77: A 40-year-old female presented to the physician for evaluation of
worsening fatigue. She has no other medical problems. She does not use
tobacco, alcohol or drugs. Vital signs are within normal limits. Physical
examination is within normal limits. Laboratory evaluation shows an
alkaline phosphatase level of 180 U/L. Which of the following should be
checked next?
Unconjugated bilirubin level
B. Lactate dehydrogenase level
C. Serum ammonia levels
D. Prothrombin time
E. y-glutamyl transpeptidase
F. Aspartate aminotransferase
A.
Explanation:
Broadly speaking laboratory tests used in the evaluation of hepatobiliary disease
either assess liver functionality (eg, prothrombin time bilirubin, albumin, cholesterol)
or the structural integrity and cellular intactness of the liver (eg, transaminases) or
the biliary tract (eg, alkaline phosphatase, y-glutaryl transferase).
Alkaline phosphatase represents a group of enzymes associated with metabolic
activity in a number of tissues including liver, bone, intestine, kidney, placenta
leukocytes, and some neoplasms. Bone and liver are the primary sources of alkaline
phosphatase with threefold elevation considered a relatively nonspecific finding for
many liver diseases. To clarify the import of a moderately elevated alkaline
phosphatase the hepatic y-glutamyl transpeptidase (GGTP) should be evaluated. Y
glutamyl transpeptidase is an enzyme predominantly present in hepatocytes and
biliary epithelia. While it too can be found in various extrahepatic tissues (organs
such as kidney spleen pancreas heart, lung and brain) GGTP is not present to a
significant extent in bone. It is therefore particularly useful in determining whether
an elevated alkaline phosphatase is of hepatic or bony origin.
(Choice A) Measurement of unconjugated bilirubin (especially in contrast to
conjugated bilirubin) can be of assistance in distinguishing hemolytic conditions from
hepatic dysfunction or bile duct obstruction. This test is not particularly helpful in
following up an elevated alkaline phosphatase.
(Choice B) Lactate dehydrogenase is a relatively nonspecific test that can be of some
assistance in the evaluation of tissue injury or death. It is not the most helpful test
in following up an elevated alkaline phosphatase.
(Choice C) Serum ammonia levels can be of assistance in determining the extent of
liver failure or gastrointestinal bleeding among other conditions. It is not the most
helpful test in following up an elevated alkaline phosphatase.
(Choice D) Prothrombin time is of assistance in assessing coagulative ability and
liver functionality, especially in the acute setting. It is not the most helpful test in
following up an elevated alkaline phosphatase.
(Choice F) Aspartate aminotransferase is of assistance in assessing and monitoring
hepatic damage. It is not the most helpful test in following up an elevated alkaline
phosphatase.
Educational Objective:
A moderately elevated alkaline phosphatase of unclear etiology should be followed
up with y-glutamyl transpeptidase.
283
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 78: A 56-year-old female presents to your office for routine check-up. She
has no present complaints. Her past medical history is significant for a vertebral
compression fracture experienced after a minor trauma one year ago. She has
taken hormone replacement therapy since then. Her laboratory tests reveal
normal serum TSH levels. Which of the following is most likely to be true in this
patient?
A. Increased total T4 pool
B. Increased free T3 level
C. Overactive iodine uptake by the thyroid
D. Decreased conversion of T4 to T3
E. Occult sympathetic hyperactivity
Explanation:
This patient has osteoporosis (hence the fragility vertebral fracture) which is being
treated with hormone replacement therapy containing estrogen and progesterone.
Estrogen has an effect on thyroid hormones, which is detailed in the following
paragraphultimately, estrogen causes an increase in total 14, but thyroid function
remains normal. Similar changes are seen in the hyper-estrogenic state of
pregnancy.
More than 99% of circulating thyroid hormones are bound to plasma proteins. The
main protein responsible for binding circulating thyroid hormone is thyroid binding
globulin (TBG). TBG levels increase with estrogen use because the catabolism of TBG
decreases when estrogen is present. An increase in TBG levels leads to an increase
in total T4 (bound T4 plus free T4) and total T3. However the level of free thyroid
hormones remains normal, so patients remain euthyroid and have normal ISH
levels.
(Choices B and E) As described above, levels of free thyroid hormones, including
free T3, do not change with estrogen. Since the level of free thyroid hormones
remains the same, patients in hyper-estrogenic states (pregnancy and oral
contraceptive pill users) do not experience thyroid symptoms. Occult sympathetic
activity would be found in a hyperthyroid patient.
(Choices C and D) An increase in TBG levels neither leads to increased iodine uptake
by thyroid gland nor to decreased peripheral conversion of T4 to T3. Medications
that can decrease the peripheral conversion of T4 to T3 are propylthiouracil,
glucocorticoids, amiodarone, iopanoic acid, and nonselective beta-blockers.
Educational Objective:
Increase in levels of thyroid binding globulin lead to increase in circulating total T4
and total T3. However the level of free thyroid hormone is normal. Increase in TBG
is typically seen in pregnancy with use of oral contraceptives or with hormone
replacement therapy.
284
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 79: A 10-year-old male is being evaluated for abnormal growth. He is in the
99th percentile for height and 90th percentile for weight. He has long and moist
extremities. Both parents are proportionate and of average height. Serum TSH is
within normal limits. Which of the following is the most likely cause of his
condition?
A. Increased release of insulin from pancreas
B. Increased release of IGF-1 from liver
C. Increased release of IGF-1 from hypothalamus
D. Defective growth hormone receptors
E. Excessive free thyroxine (T4) levels
Explanation:
Growth hormone is a 191-amino-acid hormone secreted from the anterior pituitary.
Growth hormone increases linear growthgrowth of the long bones through
increased production of insulin like growth factor-1 (IGF-1) from the liver. IGF-1
causes bone growth by stimulating the proliferation of cartilage in bone cells.
Alternatively, if there is excess growth hormone before closure of the epiphysis, it is
called gigantism a condition characterized by a tall stature and long limbs; after
closure of the epiphysis, the condition is called acromegaly. Although gigantism
and acromegaly are caused by the same excess hormone, the symptoms not alike.
This patient is young enough that we can be sure that his epiphyses are not yet
closed. It is unlikely that this patient is just a tall kid because his parents are of
average height and he has long limbs; you should suspect gigantism.
(Choice A) The main action of insulin is reduction of blood sugar levels, although it is
true that insulin secretion also causes some ICE-i production from the liver. If insulin
was being hyper-expressed (in a non-insulin resistance state), the patient would
complain of symptoms of hypoglycemiaweakness, headache, nervousness, and/or
syncope that resolve with food ingestion.
(Choice C) Although growth hormone does affect synthesis of ICE-1 from the liver, it
does not affect synthesis of ICE-1 from hypothalamus. ICE-1 that originates from
the hypothalamus is believed to regulate central nervous activity and not to
contribute significantly to a persons linear growth.
(Choice D) Defective growth hormone receptors will lead to decrease in linear
growth and is called Laron dwarfism. In patients with defective receptors, serum
levels of growth hormone will be high with low levels of circulating ICE-1. Growth
hormone acts by binding to the cell surface receptor, which stimulates intracellular
secondary pathway. The secondary pathways involved in growth hormone signaling
are Janus kinase and STAT 5 (JAR-STAT) pathway. Growth hormone releasing
hormone stimulates the release of growth hormone; whereas, somatostatin inhibits
growth hormones release.
(Choice E) Excessive circulating thyroid levels will suppress the TSH secretion from
the pituitary. A slight increase in serum free T4 levels will have a marked effect on
suppression of TSH release. The patient does not have increase free T4 levels
because his TSH is within normal limits.
Educational Objective:
1. Growth hormone increases linear growth by stimulating the production of IGF-1
from the liver.
2. Defective growth hormone receptors will lead to decrease in linear growth and is
called Laron dwarfism. It is characterized by high serum levels of growth hormone in
the presence of low IGF-1 levels.
285
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 80: A 35-year-old alcoholic is hospitalized with severe abdominal pain and
vomiting. The patients condition fails to improve after initial treatment.
Laparotomy reveals a swollen and partially necrotic pancreas. Activation of
which of the following enzymes is most likely responsible for this patients
condition?
Chymotrypsin
B. Trypsin
C. Phospholipase
D. Elastase
E. Lipase
F. Amylase
A.
Explanation:
Pancreatic enzymes are secreted by pancreatic acinar cells as zymogens, inactive
enzyme precursors. Zymogen granules are excreted from the apical surface of acinar
cells by exocytosis. The zymogens then enter the pancreatic ductal system and drain
through the ampulla of Vater into the descending part of the duodenum. There the
duodenal brush border enzyme enterokinase turns trypsinogen into trypsin, its
active form. Once a small quantity of trypsin is produced, it activates most of the
other proteolytic enzymes, such as chymotrypsin, elastase, carboxypeptidase and
others. It addition, trypsin activates trypsinogen to produce more trypsin. This
ability to self-activate allows trypsin to maintain a self-supporting cycle of proteolytic
enzyme activation in the duodenum.
In acute pancreatitis, inflammation and ischemia of pancreatic tissue lead to acinar
cell damage. This triggers abnormal activation of trypsin inside the acinar cells.
Trypsin then activates the other proteolytic enzymes and starts a self-sustaining
cycle of digestion of pancreatic tissues. Pancreatic autodigestion (autolysis) is the
central event in the pathogenesis of acute necrotizing pancreatitis.
(Choices A, C and D) Chymotrypsin, phospholipase A2, and elastase are secreted by
the pancreas as inactive precursors (chymotrypsinogen, pyrophosphokinase A2, and
proelastase) which are subsequently activated by trypsin in the duodenal lumen.
(Choice E) Lipase hydrolase triglycerides into fatty acids and glycerol. It is
synthesized in an active form and does not require activation by trypsin.
(Choice F) Amylase hydrolyzes starch to produce maltose (a glucose-glucose
disaccharide) trisaccharide maltotriose, and limit dextrins. It does not require
activation by trypsin.
Educational Objective:
The abnormal activation of trypsin within the pancreas is a central event in the
pathogenesis of acute necrotizing pancreatitis. All proteolytic pancreatic enzymes are
converted into their active forms by trypsin. Intracellular pancreatic activation of
trypsin leads to activation of other proteolytic enzymes and pancreatic
autodigestion.
286
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 81: A 74-year-old Caucasian female presents to the physicians office for
evaluation of choking spells, dysphagia, and coughing. She suffers from
recurrent pneumonia and has a long hi stow of hypertension, but no other
medical problems. Barium swallow is shown below. Which of the following is
the most likely cause of her symptoms?
A. Degenerative changes of the myenteric plexus
B. Cricopharyngeal motor dysfunction
C. Scarring and traction of the esophagus
D. Retention cyst due to duct obstruction
E. Increased intraluminal pressure in the stomach
Explanation:
Deglutition (swallowing) is a complex process that includes three phases. The oral
phase is voluntary: the food bolus is collected at the back of the mouth and lifted
upwards to the posterior wall of the pharynx. This initiates the pharyngeal phase,
which consists of involuntary pharyngeal muscle contractions that propel the food
bolus to the esophagus. During the esophageal phase, food enters the esophagus
and stretches the walls. Peristalsis begins just above the site of distention and
moves the food downward. Relaxation of the lower esophageal sphincter (LES)
follows, allowing the food bolus to enter the stomach.
Cricopharyngeal muscle dysfunction occurs due to diminished relaxation of
pharyngeal muscles during swallowing. More force is subsequently required to move
the food bolus downward. More intense contractions of the pharyngeal muscles
increase the oropharyngeal intraluminal pressure. With time, the pharyngeal mucosa
will herniate through muscle fibers in the zone of weakness (posterior hypopharynx),
forming a Zenker diverticulum. Remember that when a diverticulum consists only of
mucosa, itis a false or pulsion, diverticulum. A traction diverticulum, alternatively,
consists of all layers of the organ wall.
Cricopharyngeal dysfunction causes symptoms of high dysphagia: difficulty in
swallowing felt at the throat coughing choking and sometimes even nasal
regurgitation. When a Zenker diverticulum forms it can cause food retention with
regurgitation occurring days later. Food aspiration may lead to pneumonia, as
happened in this patient. The diverticulum can be palpated as a lateral neck mass.
(Choice A) Degenerative changes of the myenteric plexus result in achalasia.
(Choice C) Scarring and traction of the esophagus result in true diverticula. True
diverticuli are usually seen at the mid-portion of the esophagus and result from
mediastinal lymphadenitis (tuberculosis fungal infections). The above image shows a
diverticulum at the upper part of the esophagus.
287
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice D) Retention cysts are formed if the duct of a gland is obstructed trapping
secretions. Cricopharyngeal muscle dysfunction is not associated with the formation
of retention cysts.
(Choice E) Mallory-Weiss syndrome describes mucosal tears that occur around the
esophagogastric squamocolumnar junction. These tears are caused by the increased
intraluminal pressure in the stomach that occurs during retching or vomiting.
Educational Objective:
Cricopharyngeal muscle dysfunction is a condition caused by diminished relaxation of
pharyngeal muscles during swallowing. The subsequently increased intraluminal
pressure in the oropharynx causes the mucosa to herniate through the wall at a
point of muscle weakness, forming a Zenker diverticulum. Clinically, patients
(elderly) present with oropharyngeal dysphagia, coughing, choking, and recurrent
aspiration.
288
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 82: A 21-year-old male presents to his physician after noticing that his urine
had a frothy appearance. He also complains of easy fatigability and anorexia. His
past medical history is significant only for an upper respiratory infection several
weeks ago. Physical examination reveals symmetric pitting edema of the ankles.
Which of the following is most likely decreased in this patient?
A. Capillary hydrostatic pressure
B. Interstitial fluid pressure
C. Plasma oncotic pressure
D. Tissue lymphatic drainage
E. Circulating aldosterone level
Explanation:
Frothy, foamy urine may be caused by proteinuria or bile salts in the urine. This
patients history of a recent upper respiratory infection and ankle edema on physical
exam suggest a diagnosis of nephrotic syndrome with associated low serum
albumin. Hypoalbuminemia lowers the plasma oncotic pressure and causes
interstitial edema formation due to net plasma filtration. Minimal change disease
(MCD) is the most common cause of nephrosis in children, and can occur in adults
as well.
(Choice A) A decrease in capillary hydrostatic pressure would tend to decrease net
plasma filtration and interstitial edema formation.
(Choice B) This patients ankle edema is the result of a transudate of plasma into the
interstitial tissues of the ankle. We would therefore expect an increase in the steady
state interstitial fluid pressure in the ankles.
(Choice D) While a primary decrease in lymphatic drainage can cause interstitial
edema, the rate of lymphatic drainage would be increased in this particular patient
because of the accumulation of ankle interstitial fluid.
(Choice E) In nephrotic syndrome, the plasma oncotic pressure is decreased, which
causes net plasma filtration into the interstitium, thus decreasing the effective
circulating intravascular volume. This reduction of the intravascular volume
stimulates a compensatory increase in the activity of the renin-angiotensinaldosterone system. Patients with nephrotic syndrome tend to have elevated
circulating aldosterone levels.
Educational Objective:
Frothy or foamy urine maybe caused by proteinuria. Heavy proteinuria, as in
nephrotic syndrome, can cause regional or generalized interstitial edema because
the decrease in serum albumin and total protein concentrations lowers the plasma
oncotic pressure and increases net plasma filtration in capillary beds.
289
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 83: A 63-year-old Caucasian male presents to the emergency department
with severe dyspnea, orthopnea and fatigue. He suffered a myocardial infarction
six months ago, and has not been compliant with his medications since that
time. On exam, his blood pressure is 170/100 mmHg and his heart rate is 100
beats per minute. Auscultation reveals crackles at the lung bases, an S3 gallop,
and a Il/VI holosystolic murmur over the apex. After initial treatment with
diuretics and vasodilators the patients condition improves significantly. The
next morning, there are no appreciable gallops or murmurs on cardiac exam.
The murmur heard at the time of presentation is most likely explained by:
Thickened and deformed mitral valve cusps
B. Heavily calcified mitral annulus
C. Increased flow rate through the aortic valve
D. Ruptured chorda tendineae
E. Functional mitral regurgitation
A.
Explanation:
This patients symptoms of dyspnea and orthopnea together with bibasilar crackles
are consistent with high pulmonary venous pressure and pulmonary edema in the
dependent lung. The holosystolic murmur heard over the cardiac apex is suggestive
of mitral regurgitation (MR). An 33 gallop reflects an increased left ventricular filling
rate during mid diastole, and can be heard as a consequence of MR.
Treatment with a diuretic tends to reduce left ventricular (LV) preload and therefore
decreases the LV end diastolic volume (EDV). Since the patients murmur and gallop
disappeared following the reduction of LVEDVI his MR was most likely functional
that is, due to transient hemodynamic factors causing LV dilatation and/or papillary
muscle ischemia rather than due to a fixed mitral valve lesion. Acute LV dilatation
can sufficiently separate otherwise normal mitral valve leaflets to permit functional
regurgitation. The most common anatomical abnormality producing mitral
regurgitation is myxomatous degeneration (mitral valve prolapse). Afterload
reduction with a vasodilator decreases the average intraventricular systolic pressure
required to generate a given stroke volume and would tend to reduce MR due to any
cause.
(Choice A) Thickened and deformed mitral valve cusps are fixed anatomical lesions
that typically result from chronic rheumatic heart disease. For this reason, these
lesions are usually only found in older individuals (who may not have had access to
antibiotics while young). Mitral stenosis is the usual result.
(Choice C) Mitral annular calcification, consisting of degenerative calcific deposits in
the fibrous ring of the mitral valve, generally does not impair valvular function.
There is associated regurgitation or stenosis only in rare instances. Mitral annular
calcification is most common in women older than 60, individuals with a history of
myxomatous degeneration of the mitral valve, and individuals with chronically
elevated left ventricular (LV) pressures. Furthermore, whereas the patient in the
vignette had mitral regurgitation that was eliminated by a reduction in LV size
(which also decreases the mitral valve radius), the radius is fixed in patients with a
calcified mitral valve annulus.
(Choice D) An increased rate of flow through the aortic valve could produce a
functional murmur of aortic stenosis, which would be a systolic ejection type murmur
heard best over the aortic area (right upper sternal border).
(Choice E) Chordae tendineae rupture producing severe mitral regurgitation (MR) is
a complication of bacterial endocarditis, and less frequently of connective tissue
diseases or acute myocardial infarction. When papillary muscle or chordae rupture
290
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
occurs in association with myocardial infarction, it is usually an early complication of
the Ml (i.e. occurring within 10 days).
The MR of the patient in the vignette appears to have been precipitated by
medication non-compliance which caused an acute hemodynamic change. Thus
endocarditis and connective tissue disease are more remote possibilities.
Additionally, the murmur of MR due to chordae rupture may not be completely
eliminated by pharmacological manipulations. Chordae rupture results in fixed
anatomic (versus reversible functional) MR.
Educational Objective:
Acute hemodynamic changes can produce functional heart murmurs in the absence
of any fixed valve lesion. Dilatation of the left ventricle in response to increased
preload can result in functional mitral regurgitation which can be eliminated by
preload reduction and reduced by afterload reduction.
291
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 84: A 34-year-old immigrant from South Asia presents to your office
complaining of heart palpitations that are particularly prominent at night.
He also notes that with moderate exertion, he experiences head
pounding accompanied by involuntary head bobbing. He remembers
being diagnosed with a heart murmur years before, but he cannot recall
the type and has never received any treatment. Based on this patients
history, you suspect:
Restricted left ventricular filling
B. Impaired left ventricular contractility
C. Left ventricular outflow obstruction
D. Systolic-diastolic hypertension
E. Widening of the pulse pressure
A.
Explanation:
This patient complains of nocturnal palpitations and head pounding with exertion.
Palpitations may result from forceful ventricular contractions ejecting large stroke
volumes, and head pounding can be due to unusually high amplitude pulsations of
the intracranial arteries with each heartbeat. In voluntary head bobbing can be a
sign of a widened pulse pressure (recall that pulse pressure = peak systolic arterial
pressure end diastolic arterial pressure). The most likely cause of a repetitive,
widened pulse pressure together with unusually large LV stroke volumes and a heart
murmur is aortic regurgitation (AR).
(Choice A) Restriction of left ventricular (LV) filling would result in a reduced LV end
diastolic volume (reduced preload). At a given level of contractility, this would cause
a reduction in stroke volume. Lower stroke volumes result in lower pulse pressures,
whereas this patients symptoms and signs suggest a high pulse pressure.
(Choice B) Impaired left ventricular contractility would cause a reduction in stroke
volume for a given preload, resulting in lower pulse pressures.
(Choice C) Left ventricular outflow tract obstruction, as can result from aortic
stenosis or hypertrophic cardiomyopathy, could cause a murmur but would tend to
reduce stroke volume and thus pulse pressure.
(Choice D) Combined systolic and diastolic hypertension is not necessarily
accompanied by an abnormally large pulse pressure or murmur.
Educational Objective:
The abnormally large (wide) pulse pressure caused by aortic regurgitation (AR) is
responsible for many of the symptoms and signs of AR.
292
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 85: In an animal experiment, the left anterior descending (LAD) coronary
artery is ligated (time 0) and changes in substance levels within the affected
myocardial cells are recorded. At which point on the graph does the affected
myocardium stop contracting?
A.
B.
C.
D.
E.
A
B
C
D
E
Explanation:
The main early biochemical consequence of total myocardial ischemia is cessation of
aerobic glycolysis and initiation of anaerobic glycolysis. This transition occurs within
seconds, and results in inadequate production of high-energy phosphates (e.g. ATPI
creatine phosphate) to sustain cardiac muscle contraction. Loss of contractility and
lactate accumulation begin within 60 seconds of total ischemia.
(Choice B) After 5 minutes of total myocardial ischemia, ATP levels within the
affected cardiac myocytes have fallen to JS% of normal, and lactate levels have
risen significantly.
(Choice C) After 10 minutes of total myocardial ischemia, intracellular ATP levels in
the affected myocytes have been reduced to 50% of normal, and lactate levels are
markedly elevated.
(Choice D) After 20 minutes of total myocardial ischemia, intracellular ATP levels in
the affected myocytes have been reduced to about 25% of normal and lactate levels
are high.
(Choice E) After 30 minutes of total myocardial ischemia, intracellular ATP levels in
the affected myocytes have been reduced to about 15% of normal and lactate levels
are very high. When total ischemia has persisted for 30 minutes, ischemic injury
becomes irreversible. In contrast, when the ischemia lasts less than 30 minutes
myocardial stunning (reversible loss of contractile function) occurs.
Educational Objective:
Loss of cardiac myocyte contractile function occurs within 60 seconds of the onset of
total ischemia, due to immediate cessation of aerobic glycolysis and initiation of
anaerobic glycolysis, with a fall in high-energy phosphates such as ATP and creatine
phosphate. After 30 minutes of total ischemia, when ATP levels in affected myocytes
have dropped to 15% of normal and lactate levels are very high, irreversible
ischemic injury is likely.
293
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 86: A 23-year-old Caucasian male with periodic abdominal pain is diagnosed
with a duodenal mucosal defect on upper gastrointestinal contrast X-ray. Duodenal
mucosal samples taken during endoscopy demonstrate H. pylori colonization.
Which of the following accounts for bacterial colonization in the duodenum of this
patient?
A. Increased bicarbonate secretion
B. past dumping of gastric content
C. Areas of mucosal necrosis
D. Mucosal metaplasia
E. Mucosal inflammation
Explanation:
Most cases of duodenal and gastric ulcers are associated with Helicobacter pylori, a
gram-negative microaerophilic rod that resides between the protective mucus layer
and gastric epithelium in colonized persons. The following bacterial virulence factors
are implicated in the development of chronic gastritis and peptic ulcer disease
(PUD):
1. H. pylori produce urease. This enzyme catalyzes the synthesis of ammonia from
urea, causing an increase in pH.
2. H. pylori possess adhesins. These substances enable the bacteria to adhere to
gastric epithelium.
3. H. pylori secrete proteases and phospholipases. These enzymes break down
gastric mucus.
4. A number of H. pylori surface factors attract both neutrophils and monocytes,
which contribute to epithelial injury.
5. Some of the enzymes of H. pylori irritate the gastric mucosa, causing
inflammation.
All of the above virulence factors allow H. pylori to thrive on the surface of gastric
epithelium; however, H. pylori cannot live on intestinal epithelium. Therefore, the
presence of H. pylori in the duodenum indicates that gastric-type metaplasia of the
intestine is present. It is thought that H. pylori colonization of the stomach increases
gastric acid production, which leads to acidic injury of duodenal mucosa, inducing
gastric metaplasia there. Then, these metaplastic shelters for H. pylon! cause
inflammation in surrounding duodenal epithelium. Alternatively, some researchers
feel that the gastric metaplasia may be pre-existent in some patients.
(Choice A) H. pylori infection is associated with decreased bicarbonate secretion in
the duodenum, which weakens the defense barrier of the duodenal mucosa to
infection.
(Choice B) Fast dumping of acidic gastric contents into the duodenum is sometimes
noted in patients with duodenal ulcers. However, it is not considered a factor of H.
pylori survival in the duodenum.
(Choices C and E) Mucosal inflammation and subsequent mucosal necrosis can result
from the presence of H. pylori in the gastric or duodenal lumen. These mucosal
changes are the result of, not the facilitator for, survival in the duodenum.
Educational Objective:
H. pylori is well-adapted to live in the gastric lumen. This pathogen doesnt colonize
normal duodenal mucosa, only gastric-type mucosa. The full etiology of duodenal
ulcers is still unclear. Areas of gastric metaplasia may be preexistent in the
duodenum or they may develop secondary to acid injury caused by H. pylori
colonization of the stomach.
294
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 87: A 55-year-old Caucasian female presents to your office complaining of
weight gain and easy fatigability. She takes a multivitamin and some over-thecounter medications for constipation. Her blood pressure is 140/96 mmHg, and
heart rate is 55/mm. Physical examination reveals a delayed relaxation of knee
and ankle reflexes. Skin is very dry and thick. Which of the following is the
single best screening test to confirm the diagnosis in this patient?
A. Serum T3 and T4 levels
B. Serum TSH level
C. 24-hour urinary cortisol excretion
D. Dexamethasone suppression test
E. Serum prolactin level
Explanation:
The features described abovefatigue, weight gain, constipation, slowed relaxation
of deep tendon reflexes, and dry, coarse skinare strongly suggestive of primary
hypothyroidism. The pituitary gland secretes thyroid stimulating hormone (TSH) or
thyrotrophin which increases the synthesis and release of thyroid hormones from the
thyroid gland. In turn, the pituitary itself is stimulated by the hypothalamus, which
secretes thyrotrophin-releasing hormone (TRH).
Excessive thyroid hormone release causes inhibition of TSH and TRH production and
release in a classic negative feedback mechanism. Small changes in thyroid hormone
levels lead to marked changes in serum TSH level. In hypothyroidism, the TSH rise
occurs well before a low thyroid hormone level is seen. Some changes also occur at
the level of hypothalamus but TRH is difficult to measure. Thus, serum TSH is the
most sensitive marker for diagnosis of hypothyroidism.
The main caveat for using TSH in the diagnosis of hypothyroidism is that itis not
elevated in patients with hypothyroidism due to TSH deficiency (central
hypothyroidism). Nonetheless central hypothyroidism is relatively uncommon and
there are usually other clinical features that suggest its presence.
(Choice A) T4 levels can be low but within normal limits in early mild primary
hypothyroidism. Since TSH levels rise beforeT4 levels are low TSH is a more
sensitive test. Serum T3 is the last to decline in most patients with hypothyroidism.
(Choices C and D) Twenty-four hour urinary cortisol and the dexamethasone
suppression test are screening tests for Cushing syndrome. The patient described
above does not have any features of Cushing syndrome which include central
295
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
obesity, skin striae rounded facies deposition of supraclavicular fat and proximal
weakness.
(Choice E) Hyperprolactinemia characteristically leads to amenorrhea and
galactorrhea in females. Increased serum prolactin can occur in hypothyroidism due
to the stimulatory effect of elevated hypothalamic TRH, which then stimulates the
pituitary causing excess prolactin production and release.
Educational Objective:
Serum TSH level is the single most important screening test in diagnosing primary
hypothyroidism. Although TSH is not elevated in patients with hypothyroidism in
central hypothyroidism central hypothyroidism is uncommon.
296
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 88: A group of investigators studies the process of bone remodeling in
response to steroid hormones. In animal experiments they note that the
castration of young females (i.e. removal of the ovaries) leads to overexpression of RANK receptors on the surface of some bone cells. Which of
the following is the most likely consequence of the response described by
the investigators?
Increased bone resorption
B. Decreased osteoid formation
C. Decreased mineralization
D. Osteocyte apoptosis
E. Decreased blood flow to the bone
A.
Explanation:
Osteoclasts are derived from the hemopoietic monocyte phagocytic cell lineage. The
differentiation of osteoclasts is mainly governed by the RANK-ligand and by
monocyte colony-stimulating factor, both of which are produced by osteoblasts.
Interaction of RANK-ligand and monocyte colony-stimulating factor on receptors
present in osteoclastic precursors stimulates the development of mature, multi
nucleated osteoclasts. The interaction of RANK with its ligand is decreased by
another protein secreted by the osteoblastthis protein is called osteoprotegerin
(OPG) and it acts as a decoy receptor. Bone turnover is regulated by the ratio of
RANK-ligand to OPO. Bone turnover increases when RANK-L is high and OPO is low.
Similarly, the over expression of RANK receptors on osteoclasts also increases bone
turnover. Parathyroid hormone (PTH) stimulates osteoclasts in an unexpected way.
Osteoclasts do not have PTH receptorsPTH acts on osteoblasts, instead. PTH
stimulates the secretion of monocyte colony-stimulation factor and RANK-ligand by
osteoblasts, thus stimulating osteoclastic precursor to become mature osteoclasts.
(Choices B and C) RANK receptors are not present on osteoblasts, so an increased
expression of the RANK receptor will have no effect on osteoid formation. In normal
subjects, the resorption and formation of bone is tightly coupled. In patients who are
estrogen deficient, resorption is higher than formation; the net effect is bone loss.
(Choice D) Osteocytes are the precursors of osteoblasts. RANK receptors are not
expressed on osteocytes.
(Choice E) Lower estrogen levels lead to increased vascular endothelial growth factor
(VEGE) production locally within the bone. Vascular endothelial growth factor
augments new blood vessel formation and increases blood flow. Mice that have been
spayed will have an increase in bone vascularity due to VEGE, not decreased blood
flow to the bone.
Educational Objective:
The RANK receptor/RANK-ligand interaction is essential for the formation and
differentiation of osteoclasts. The overexpression of RANK receptors in
hypoestrogenic states causes increased bone resorption due to increased
osteoclastic activity. In short, low estrogen means a lower bone mass.
297
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 89: A 27-year-old Caucasian male presents to your office complaining of
repetitive episodes of muscle weakness. He has no significant past medical
history. His blood pressure is 190/110 mmHg while supine and 195/110
mmHg while standing. His heart rate is 70 beats per minute while supine and
72 beats per minute while standing. Laboratory evaluation reveals very low
plasma renin activity. Overactivity of which of the following structures is most
likely responsible for this patients symptoms?
Chromatin cells of the adrenals
B. Extra-adrenal paraganglion cells
C. Zona glomerulosa of the adrenals
D. Zona fasciculata of the adrenals
E. Zona reticulata of the adrenals
F. Juxtaglomerular cells of the kidney
A.
Explanation:
The adrenal glands are situated above the kidneys and consist of an outer cortex
and an inner medulla. The adrenal cortex develops and functions independently from
the adrenal medulla. The mature adrenal cortex consists of three distinct zones: the
outer zona glomerulosa the middle zona fasciculata, and the inner zona reticularis
(Remember GFR). The zona glomerulosa synthesizes mineralocorticoids, the zona
fasciculata predominantly produces cortisol, and the zona reticularis predominantly
produces androgens.
Secretion of aldosterone from the zona glomerulosa is regulated by the reninangiotensin system and potassium. Because the zona glomerulosa lacks 17-ahydroxqlase, it cannot synthesize cortisol or androgens. ACTH from the anterior
pituitary increases the secretion of cortisol and adrenal androgens from the zona
fasciculata and zona reticularis, respectively but there is no substantial effect of
ACTH on aldosterone secretion.
Aldosterones main effect is to stimulate sodium absorption and potassium and
hydrogen ion excretion at the distal renal tubule. Thus overproduction of aldosterone
by tumors or hyperplastic zona glomerulosa cells can result in sodium retention
hypertension hypokalemia, and metabolic alkalosis. Despite this increase in sodium
absorption, however hypernatremia is rarely observed with mineralocorticoid excess,
due to the phenomenon of aldosterone escape. The high aldosterone levels cause
increased renal sodium and water absorption, thus increasing renal blood flow and
GFRI which in turn increase the rate of sodium excretion from the renal tubules.
Furthermore, the increase in intravascular volume stimulates the release of atrial
natriuretic peptide, which causes natriuresis. Thus, hypertension, hypokalemia and
metabolic alkalosis, without marked hypernatremia, characterize mineralocorticoid
excess. Renin levels are typically very low, due to the hypervolemia. The
hypokalemia of hyperaldosteronism can cause profound muscle weakness.
(Choice A and B) Pheochromocytoma is a neuroendocrine tumor of the chromaffin
cells of the sympathetic nervous system (90% arising from the adrenal medulla.
10% arising extra-adrenally along the sympathetic chain). Hypokalemia is not a
feature of pheochromocytoma, and renin levels may actually be increased secondary
to decreased intravascular volume.
(Choice D and E) Hypersecretion of the zona fasciculata or zona reticularis
(secondary to hyperplasia or neoplasia) would lead to Cushing syndrome or adrenal
hyperandrogenism, respectively.
(Choice F) When there is increased renin production by the juxtaglomerular
apparatus aldosterone levels increase. and hypertension can result. This typically
298
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
occurs in the setting of renal artery stenosis, when decreased renal blood flow
stimulates renin release from the juxtaglomerular apparatus. Increased renin levels
cause increased formation of angiotensin I, which is subsequently converted to
angiotensin II. Angiotensin II directly increases blood pressure via vasoconstriction
and indirectly increases blood pressure by stimulating aldosterone release.
Secondary hyperaldosteronism resulting from renal artery stenosis causes
hypokalemia and hypertension. Thus, patients with hypertension secondary to renal
artery stenosis have high renin and aldosterone levels. (Primary aldosteronism
results from adrenocortical adenomas or hyperplasia. Circulating renin levels are
very low in this condition.)
Educational Objective:
The adrenal cortex consists of three distinct zones: the outer zona glomerulosa the
middle zona fasciculata, and the inner zona reticularis (remember GFR). The zona
glomerulosa synthesizes mineralocorticoids (e.g. aldosterone), the zona fasciculata
predominantly produces cortisol, and the zona reticularis predominantly produces
androgens.
299
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 90: An infant born to a 22-year-old female has a small phallus and
hypospadias. His testes are well developed but reside in the inguinal
area. His blood pressure and serum testosterone levels are normal. His
karyotype is 46XY. Which of the following is most likely deficient in this
patient?
hydroxqlase
B. Aromatase
C. 17-hydroxylase
D. 5a-reductase
E. DHEA sulfatase
A. 21-
Explanation:
5a-reductase converts testosterone into dihydrotestosterone (DHT). Testosterone is
responsible for development of the internal male genitalia during embryogenesis,
spermatogenesis, and male sexual differentiation at puberty (such as development
of muscle mass and libido). DHT mediates development of the external genitalia
(penis and scrotum) in the embryo growth of the prostate, facial hair and temporal
recession of the hairline. DHT also amplifies the effects of testosterone due to a
much higher affinity for the testosterone receptor.
There are two types of 5-reductase. Type 1 is present in postpubescent skin, while
type 2 is found in the genitals. Deficiency of 5-reductase type 2 results in
diminished conversion of testosterone to DHT in the tissues. In the male fetus with
this genetic defect, the internal genitalia develop normally under the influence of
testosterone, but the external genitalia do not develop properly due to the lack of
DHT resulting in male pseudohermaphroditism. The genitalia at birth can range from
a small phallus with hypospadias as described in the question to ambiguous or
female-type at birth. Such children may be raised as females until they reach
puberty when high levels of testosterone and the action of Type 1 5a-reductase
results in masculinization evidenced by male-pattern muscle mass, voice deepening,
penile and scrotal growth, and testicular descent.
(Choice A) 21-hydroxylase converts 17-hydroxyprogesterone into 11-deoxcortisol,
and progesterone into 11- deoxycorticosterone. Corticosteroid precursors are
shunted toward androgen production resulting in virilization of the female fetus and
salt wasting.
(Choice B) Aromatase catalyzes the conversion of androgens to estrogens in the
gonads and peripheral tissues. Aromatase deficiency presents with virilization of
female infants; male patients are not phenotypically affected.
(Choice C) Deficiency of 17-hydroxylase results in decreased secretion of cortisol
and sex steroids and an increased level of mineralocorticoids. Clinically it manifests
with sodium retention leading to hypertension and under virilization of male infants
(female-type genitalia).
(Choice E) DHEA sulfate is a weak androgen produced by the adrenal cortex.
Deficiency of DHEA sulfatase does not result in under virilization of the male fetus.
Educational Objective:
5-reductase converts testosterone to dihydrotestosterone (DHT). DHT mediates
development of the external genitalia in the male fetus. Male neonates with 5areductase deficiency are born with feminized external genitalia that typically
masculinize at puberty. Small phallus and hypospadias are commonly found.
300
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 91: Coronarii angiography demonstrates several atherosclerotic lesions in an
asymptomatic 35-year-old Caucasian male. The lesions do not cause significant
coronary flow obstruction. High intraplaque activity of which enzyme would
predispose the patient to myocardial infarction?
A. Prolyl hydroxylase
B. Lysyl oxidase
C. Procollagen peptidases
D. Metalloproteinases
E. Heparinase
Explanation:
Plaque rupture can produce an acute coronary syndrome via superimposed
thrombosis and/or thromboembolism. The likelihood of plaque rupture or other acute
plaque change has more to do with plaque stability than plaque size. Plaque stability
depends upon the mechanical strength of the overlying fibrous cap. A weak fibrous
cap increases the probability of plaque rupture.
During the chronic inflammatory progression of an atheroma, the fibrous cap is
continually being remodeled. The balance of collagen synthesis and degradation
determines the mechanical strength of the cap. Activated macrophages in the
atheroma contribute to collagen degradation by secreting metalloproteinases. Thus,
a high degree of ongoing intimal inflammation can destabilize the mechanical
integrity of plaques through release of these metalloproteinases. High intraplaque
activity of such enzymes predisposes the patient to plaque rupture and a consequent
acute coronary syndrome, including myocardial infarction.
(Choice A) The enzyme prolyl4-hydroxqlase is responsible for the hydroxylation of
proline on procollagen chains, a required step in the formation of a stable collagen
triple helix. Enhanced collagen deposition would strengthen the fibrous cap, thereby
stabilizing the atheroma.
(Choice B) Lysyl oxidase catalyzes the conversion of the amino terminus of lysine
residues to an aldehyde in collagen fibers. Extracellular collagen fibers are
strengthened by this mechanism. Thus, a high activity of lysyl oxidase would favor
atheroma stabilization by strengthening collagen in the fibrous cap.
(Choice C) Procollagen peptidase cleaves the terminal regions of procollagen
molecules exocytose by fibroblasts or SMCI transforming the procollagen into
insoluble tropocollagen. Tropocollagen then aggregates to form collagen fibrils.
The activity of procollagen peptidase is deficient in Ehlers-Danlos syndrome, a
condition characterized by disorganized collagen bundles. These patients have
stretchable skin hypermobile joints short stature, and other connective tissue
defects.
(Choice E) Heparinase is not an endogenous enzyme. However, if it were, an
increase in its activity could conceivably be prethrombotic or thrombogenic,
theoretically predisposing a patient with coronary artery plaques to myocardial
infarction.
Educational Objective:
The likelihood of acute plaque change (especially rupture) producing an acute
coronary syndrome via superimposed thrombosis and/or thromboembolism is most
related to plaque stability. Plaque stability depends significantly on mechanical
strength of the fibrous cap. Inflammatory macrophages in the intima may reduce
plaque stability by secreting metalloproteinases, which degrade collagen.
301
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 92: A 58-year-old Caucasian male is hospitalized by the sudden onset of chest
pain. His blood pressure is 160/110 mmHg, and his heart rate is 90/mm. His BMI is
30.5 kg/rn2. A baseline ECG reveals non-specific ST segment and T wave changes,
and serial troponin measurements are normal. His fasting plasma glucose level is
found to be 160 mg/dL, although he has never been diagnosed with diabetes
mellitus. Which of the following would correlate most with the resistance of tissues
to the action of insulin in this patient?
A. Arm circumference
B. Triceps area skin thickness
C. Waist-to-hip ratio
D. Increase in liver glycogen
F. Urinary ketone excretion
Explanation:
The patient described in this vignette has hypertension obesity and possible type 2
diabetes mellitus. The pathophysiology of type 2 diabetes mellitus involves insulin
resistance along with defective insulin secretion from pancreatic beta cells. Although
still controversial, many researchers believe that insulin resistance is the main defect
in type 2 diabetes mellitus.
Insulin resistance is a heterogenous disorder caused by number of genetic and
environmental factors. Genetic defects include receptor and post-receptor mutations
that result in faulty insulin signaling. Environmental factors that increase insulin
resistance include lack of physical activity and obesity. Increased BMI is very
commonly associated with insulin resistance and type 2 diabetes mellitus. A high
BMI typically connotes a higher body fat content, although a very muscular person
(like a bodybuilder) might have a high BMI, also. There are two different types of fat
in the body: visceral fat and subcutaneous fat. In general, the visceral deposition of
fat (fat surrounding internal organs) has a much stronger correlation with insulin
resistance than does subcutaneous fat. Measuring of the waist-to-hip ratio (VVHR)
indirectly measures the visceral fat to subcutaneous fat as the abdomen contains
mainly viscera and hips have only subcutaneous fat. A high waist hip ratio is
associated with insulin resistance, metabolic syndrome and type 2 diabetes mellitus.
The metabolic syndrome is a group of risk factors that include hypertension,
abdominal obesity, atherogenic dyslipidemia, insulin resistance and other factors.
(Choices A and B) Measuring the whole arm circumference or triceps skin fold
thickness correlates poorly with insulin resistance and type 2 diabetes mellitus.
These parameters indirectly measure muscle mass and/or subcutaneous fat
deposition.
(Choice D) An increase in liver fat suggests insulin resistance; whereas, an increase
in glycogen deposition suggests enhanced insulin action (after glycogen storage
diseases have been excluded). Insulin increases glycogen synthesis in the liver and
in skeletal muscles.
(Choice E) Increase in urine ketone production usually occurs with absolute insulin
deficiency as seen in type 1 diabetes mellitus. Although type 2 diabetics are
relatively deficient in insulin the absence is not complete. In fact patients with type 2
diabetes mellitus generally have high circulating insulin which suppresses
ketogenesis.
Educational Objective:
Visceral obesity as measured by waist-to-hip ratio is an important determinant of
insulin resistance.
302
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 93: A 30-year-old female has had diarrhea and weight loss for several
months. She also has diffuse bone pain and weakness. Her diarrhea
improves with a gluten-free diet. Which of the following is most likely seen
on the laboratory evaluation of this patient?
A.
B.
C.
D.
E.
Serum Ca
increased
decreased
decreased
decreased
normal
Serum phosphorous
decreased
decreased
increased
increased
increased
Serum PTH
increased
increased
decreased
increased
increased
Explanation:
This woman has celiac disease, which is characterized by an increased sensitivity to
a group of dietary proteins present in wheat barley, and rye collectively known as
gluten. In patients who suffer from celiac disease the small intestinal mucosa
becomes inflamed and atrophic in response to gluten, which results in defective
mucosal absorption of nutrients. Celiac disease can also cause vitamin D
malabsorption, which causes rickets in children and osteomalacia in adults.
In vitamin D deficiency, both calcium and phosphorus absorption from the
gastrointestinal tract are markedly decreased. Low levels of 1, 25 dihydroxyvitamin
D, and the ensuing hypocalcemia, cause an increase in parathyroid hormone levels
(secondary hyperparathyroidism). In vitamin D deficiencies, the serum phosphorus
is decreased because there is an increase in urinary excretion of phosphorus induced
by high PTH levels and because phosphorous is not properly absorbed from the
gastrointestinal tract.
(Choice A) An elevated PTH, hypercalcemia, and hypophosphatemia are the values
expected in patients with primary hyperparathyroidism.
(Choice C) In patients with hypoparathyroidism, the decrease in serum PTH level is
accompanied by a decrease in serum calcium and an increase in serum phosphorus.
(Choices D and E) Either of these biochemical scenarios can occur in
pseudohypoparathyroidism and chronic renal failure. Resistance to PTH causes
pseudohypoparathyroidism. The patient will have biochemical features of
hypoparathyroidism (normal to low calcium levels and elevated phosphorous levels)
but will have elevated circulating levels of parathyroid hormone. In chronic renal
failure, high PTH is accompanied by normal to low serum calcium and increase in
serum phosphorus. Low serum calcium is due to the decreased production of 1,25dihydroxivitamin D from the damaged kidneys, resulting in decreased calcium
absorption from the gastrointestinal tract. Chronic renal disease results in impaired
phosphorus excretion leading to hyperphosphatemia.
Educational Objective:
The diarrhea of celiac disease can lead to vitamin D deficiency through
malabsorption. Patients with a vitamin D deficiency have decreased serum
phosphorus increased serum PTH (secondary hyperparathyroidism), and low serum
calcium. They may also have symptoms such as bone pain and muscle weakness.
303
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 94: A one-month-old Caucasian male with a history of persistent jaundice
experiences muscle rigidity, lethargy and seizures. Which of the following
causes of hyperbilirubinemia is most likely to produce this patients neurological
abnormalities?
Absent liver conjugation enzymes
B. Deficient bilirubin excretion into bile canaliculi
C. Impaired canalicular bile transit
D. Increased gut deconjugation of bilirubin
E. Impaired gut reabsorption of bilirubin
A.
Explanation:
The hepatic processing of bilirubin is accomplished in three key steps: 1) carriermediated uptake of bilirubin at the sinusoidal membrane: 2) conjugation of bilirubin
with glucuronic acid by UGT (uridine diphosphate glucuronyl transferase)
in the endoplasmic reticulum: and 3) biliary excretion of the water-soluble, nontoxic
bilirubin glucuronides. Disruption of this process can be fatal, as seen with CriglerNajjar syndrome.
Crigler-Najjar syndrome type 1 is an autosomal recessive disorder of bilirubin
metabolism caused by a genetic lack of the LJGT enzyme needed to catalyze bile
glucuronidation. When bilirubin is not correctly enzymatically processed by the liver,
unconjugated hyperbilirubinemia develops. Indirect bilirubin levels typically
approximate 20-25 mg/dL in these infants, but can rise to as high as 50 mg/dL.
Conjugated bilirubin is water soluble, loosely bound to albumin, and excreted in
urine when present in excess. In contrast, unconjugated bilirubin binds tightly to
albumin and is highly insoluble in water. When bound, this unconjugated bilirubin
cannot be filtered by the glomerulus and is therefore not excreted in the urine,
Instead, the unconjugated bilirubin is gradually deposited into various tissues,
including the brain. These deposits can cause kernicterus (bilirubin encephalopathy),
which is a potentially fatal condition characterized by severe jaundice and neurologic
impairment, as seen in this child.
(Choice B) Dubin-Johnson syndrome is an autosomal recessive disorder
characterized by the absence of a biliary transport protein, MRP2 (multidrug
resistance protein 2), used in the hepatocellular excretion of bilirubin glucuronides
into bile canaliculi. The liver is darkly pigmented as a result, but patients are
typically asymptomatic and suffer no significant adverse effects.
(Choice C) Rotor syndrome is a rare autosomal recessive disorder characterized by
an asymptomatic conjugated hyperbilirubinemia that results from numerous defects
in the hepatic uptake and excretion of bilirubin pigments. Although patients are
often jaundiced, they enjoy normal life expectancies.
(Choice D) High numbers of anaerobes and Staphylococcus aureus can result in the
deconjugation (via removal of glycine and taurine) of bile acids, rendering them less
soluble and therefore less able to form micelles. This deconjugation impedes the
active reabsorption of bile acids into portal circulation at the terminal ileum,
resulting in lipid malabsorption. However, there are no neurologic abnormalities
associated with bilirubin deconjugation in the gut.
(Choice E) Within the colon, bacterial enzymes reduce bilirubin into urobilinogen. A
small fraction of these urobilinogen return to the liver through the enterohepatic
circulation: these will later either re-enter the gastrointestinal tract or be excreted
through the urine. The urobilinogen that remain in the colon are excreted in the
feces as stercobilin, contributing to its dark color. Fortunately, there are no
neurologic abnormalities associated with impaired gut reabsorption of bilirubin.
304
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Crigler-Najjar syndrome is an autosomal recessive disorder of bilirubin metabolism
caused by a genetic lack of the UGT enzyme needed to catalyze bile glucuronidation.
Unconjugated hyperbilirubinemia develops in these infants, causing kernicterus and
often death.
305
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 95: An 8-year-old boy with recurrent episodes of shortness of breath and
wheezing is brought to the physicians office for evaluation. Physical
examination reveals mildly prolonged expirations. A complete blood count
shows eosinophilia. The physician prescribes a pharmacologic receptor
antagonist, and the symptoms improve substantially. The drug most likely acts
at the receptor for:
Serotonin
B. Histamine
C. Leukotriene D4
D. Platelet activating factor
E. Prostaglandin E2
A.
Explanation:
This patients history and physical exam findings are consistent with atopic (extrinsic
allergic) asthma, the most common type of asthma. Atopic asthma usually manifests
in childhood. Of the numerous inflammatory mediators postulated to play a role in
the pathogenesis of allergic asthma, only leukotrienes (LTC4, LTC4, and LTC4) and
acetylcholine produce bronchospasm that is relieved by pharmacologic antagonists.
Leukotrienes are synthesized by mast cells, eosinophils, basophils, and other cell
types that infiltrate the bronchial mucosa in asthmatics. In addition to causing
bronchial constriction and hyperreactivity, leukotrienes also promote mucosal edema
and mucus hypersecretion. Two leukotriene D4 receptor antagonists, zafirlukast and
montelukast, may offer long-term control of atopic asthma by increasing airway
caliber and reducing mucosal inflammation.
Inhaled ipratropium is an antimuscarinic agent that blocks M3 receptors in airway
smooth muscle and submucosal glands. It may offer short term relief of
bronchoconstriction in allergic asthma.
(Choice A) Serotonin does not play a major role in the pathogenesis of atopic
asthma.
(Choice B) Histamine is a bronchoconstrictor released by activated mast cells.
Histamine may contribute to the pathogenesis of asthmatic bronchoconstriction, but
its role appears to be relatively minor given that histamine antagonists lack efficacy
in allergic asthma.
(Choice D) RAE is a secondary inflammatory mediator released by activated mast
cells that may promote bronchospasm and bronchial mucosal cellular infiltration.
However, RAE receptor antagonists have not been shown tube as efficacious as
leukotriene D4 and muscarinic receptor antagonists in the treatment of atopic
asthma.
(Choice E) Although prostaglandins may contribute to the pathogenesis of allergic
asthma, prostaglandin receptor antagonists are less effective therapies than
leukotriene D4 and muscarinic receptor antagonists in the treatment of atopic
asthma.
(Choice E) Although prostaglandins may contribute to the pathogenesis of allergic
asthma, prostaglandin receptor antagonists are less effective therapies than
leukotriene D4 and muscarinic receptor antagonists.
Educational Objective:
Although numerous substances are thought to play a role in the pathogenesis of
allergic asthma, only leukotrienes (LTC4, LTD4, and LTE4) and acetylcholine have
pharmacologic receptor antagonists that offer clear therapeutic benefit.
306
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 96: A 67-year-old Caucasian male presents to your office with right tibial pain
that started three months ago and has increased in intensity overtime. His past
medical history is significant for bilateral hearing impairment, diagnosed one year
ago, and long-term hypertension. Physical examination reveals local tenderness and
a lumpy protuberance over the right tibia. After extensive evaluation you proceed
with bone biopsy. The pathologist calls to tell you that there were numerous
multinucleate cells in the biopsy; some cells had over 100 nuclei that were positive
for tartrate resistant acid phosphatase. Which of the following substances is
essential for the differentiation of the cells described by the pathologist?
A. Fibroblast growth factor (FGE)
B. Transforming growth factor beta (TGF beta)
C. Insulin-like growth factor (IGF)
D. Macrophage colony-stimulating factor (M-CSF)
E. Osteocalcin
Explanation:
This patient has clinical features suggestive of Pagets disease of the bone: the
patient is an older gentleman with pain and deformity in a bony area and hearing
loss suggesting that the disease is affecting not only the patients right tibia, but also
his skull. (There is also a Pagets disease of the breast which is unrelated to the
bone disease.) The primary abnormality in Pagets disease of the bone is excessive
osteoclastic bone resorption. A childhood infection of osteoclasts by a paramyxovirus
might be responsible for Pagets disease. Osteoclasts in Pagets disease are typically
very large and can have up to 100 nuclei (normal osteoclasts have 2-5 nuclei). The
bone turnover is markedly increased in Pagets disease, culminating in chaotic bone
formation.
Osteoclasts are the large multinucleated cells responsible for bone resorption. They
originate from the mononuclear phagocytic cell lineage. Osteoclasts are formed
when several precursor cells fuse, creating a multinucleated, mature cell. The
osteoclastic plasma membrane that faces the calcified surface is called the ruffled
border because it has deep folding. Lysosomal enzymes responsible for bone
resorption are predominantly secreted through the ruffled border. Systemic
hormones, as well as locally-acting cytokines, regulate the function of osteoclasts.
The two most important factors for osteoclastic differentiation are produced by the
osteoblast. These factors are M-CSF (monocyte colony-stimulating factor) and
RANK-L (the receptor for activated nuclear factor kappa beta -ligand). Osteoclast
precursors and mature osteoclasts posses receptors for RANK-L and M-CSF.
(Choice A) Both acidic and basic fibroblast growth factors increase bone formation by
stimulation of the osteoblast. Fibroblast growth factor leads to increased bone matrix
formation. Fibroblast growth factor is also important for neovascularization and for
wound healing. This neovascularization and matrix formation are also important in
fracture repair. Abnormalities in the fibroblast growth factor receptor in the bone
cause a form of congenital dwarfism known as achondroplasia.
(Choice B) Transforming growth factor beta increases the replication of osteoblast
precursors leading to increased formation of mature osteoblasts. Transforming
growth factor beta also increases collagen synthesis and decreases bone resorption
by increasing osteoclastic apoptosis.
(Choice C) Insulin like growth factors (IGF-I and II) are synthesized by various
tissues including the liver and bone. IGF-l levels are much higher postnatally than
IGF-II. IGF-I increases osteoblastic replication and collagen synthesis. IGF-I also
307
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
decreases collagen degradation by inhibiting the enzyme matrix metalloproteinase-1
3 (MMP-13). The net effect of IGF-I on the bone is anabolic.
(Choice E) Osteocalcin is a non-collagenous protein secreted by the osteoblast. It is
used as a marker of bone formation. The exact function of osteocalcin is not known
but it is thought to limit bone mineralization. In mice with deficient osteocalcin, the
bone mass is increased.
Educational Objective:
Osteoclasts originate from hematopoietic progenitor cells. RANK-L and M-CSF play
an important role in osteoclast differentiation. Pagets disease of the bone is caused
by excessive osteoclastic resorption.
308
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 97: A 43-year-old Caucasian male presents to your office with a severalmonth history of pruritus, rash pushing, and abdominal cramps. Small bowel
biopsy demonstrates nests of mast cells within the mucosa. Which of the
following additional findings would you expect most in this patient?
Gastric atrophy
B. Pernicious anemia
C. Gastric hypersecretion
D. Gastric hypomotility
E. Bacterial colonization of the stomach
F. Pancreatic tumor
A.
Explanation:
Gastric acid is secreted by parietal cells located in the mucosal glands of the fundus
and body of the stomach. It is stimulated by the following substances:
1. Histamine acts via H2 receptors and increases intracellular cAMP concentration.
2. Acetylcholine acts via M3 muscarinic receptors, and leads to an increase in
intracellular calcium.
3. Gastrin binds to the gastrin receptor on the surface of parietal cells and increases
intracellular calcium concentration. It also stimulates histamine synthesis and
release by ECL (enterochromaffin-like) cells in the stomach. The latter is the most
potent mechanism of gastrin action.
Intracellular calcium and cAMP activate protein kinases and lead to increased
transport of H+ by H+-K+ ATPase into the gastric lumen.
In systemic mastocytosis, mast cell proliferation occurs in the bone marrow and in
other organs. Increased histamine secretion ensues; as a result, many clinical
symptoms of this disease are mediated by histamine. Gastric acid secretion
increases, which inactivates pancreatic and intestinal enzymes, causing diarrhea.
Other GI symptoms include nausea, vomiting, and abdominal cramps. Gastric
ulcerations may occur.
Other histamine-mediated symptoms of mastocytosis are syncope, flushing
hypotension, tachycardia, and bronchospasm. Skin manifestations, such as pruritus,
urticaria, and dermatographism, are typical.
(Choice A) Gastric mucosal atrophy results from long-standing gastritis, most
commonly associated with H. pylon. It usually clinically silent or manifests with nonspecific symptoms of nausea, vomiting, and epigastric discomfort.
(Choice B) Pernicious anemia is associated with rare autoimmune gastritis. It results
from autoantibody attack of parietal cells / intrinsic factor. If intrinsic factor is not
produced, vitamin B 12 can not be absorbed, causing neurological symptoms.
(Choice D) Gastric hypomotility (gastroparesis) occurs in patients with diabetes
mellitus, uremia, hypothyroidism, and other metabolic disorders. Gastroparesis may
cause constipation, episodic diarrhea, early satiety, and food stasis with subsequent
vomiting.
(Choice E) Colonization of the stomach with the gram-negative rod H. pylori is the
most common cause of chronic gastritis and peptic ulcer disease. It is not associated
with cutaneous pruritus and flushing. Mast cell proliferation is not associated with H
pylon.
(Choice F) Pancreatic tumors may secrete gastrin (Zollinger-Ellison syndrome),
insulin (causing symptoms of fasting hypoglycemia), glucagon (causing diabetes
mellitus and typical rash), and somatostatin (associated with diarrhea, cholelithiasis
and diabetes mellitus). Pancreatic tumors, however, are not known to secrete
histamine.
309
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Systemic mastocytosis is characterized by the abnormal proliferation of mast cells
and increased histamine secretion. Histamine increases the production of gastric acid
by parietal cells. Gastric hypersecretion, therefore, is a common occurrence in
systemic mastocytosis.
310
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 98: A 62-year-old male complains of progressive dyspnea that limits his daily
activities. He has smoked 1-2 packs of cigarettes a day for over 30 years. Physical
examination reveals bilaterally decreased breath sounds and scattered wheezes.
His chest x-ray is shown below. Which of the following parameters is most likely to
be increased in this patient?
A. Expiratory flow rates
B. Carbon monoxide diffusion capacity
C. Lung elastic recoil
D. Forced vital capacity
E. Functional residual capacity
Explanation:
This patients clinical picture is consistent with chronic obstructive pulmonary disease
(COPD). The chest x-ray shows hyperinflated lungs and a flattened diaphragm.
COPD encompasses chronic bronchitis and/or emphysema. Patients with emphysema
often have a barrel-shaped chest and decreased breath sounds on physical exam, as
well as increases in both total lung capacity (TLC) and residual volume (RV). These
spirometry findings are due to destruction of interalveolar walls and diminished lung
elastic recoil which cause air trapping in enlarged distal airspaces. Since the
functional residual capacity (RC) is equal to the expiratory reserve volume (ERV)
plus the RV, and since the FRV is likely to be increased by the air trapping that
characterizes emphysema, FRC will also tend to be increased in emphysematous
patients.
(Choice A) In both types of COPD expiratory airflow rates are reduced. This is
because of the inflammatory and fibrotic narrowing of bronchi in chronic bronchitis
and the decreased lung elastic recoil and increased dynamic airway compression
during expiration in emphysema.
(Choice B)The diffusing capacity of the lung for carbon monoxide (DLCO) depends on
the thickness and total surface area of the alveolar capillary membrane and on the
hematocrit and total volume of the pulmonary capillary blood. In emphysema,
interalveolar wall destruction decreases the alveolar-capillary surface area, reducing
diffusing capacity. In patients with emphysema, DLCO may be decreased even when
there is little evidence of expiratory airflow obstruction by spirometric pulmonary
function testing.
(Choice C) In emphysema, lung elastic recoil is decreased due to destruction of
interalveolar walls.
(Choice D) In CQPDI forced vital capacity is generally decreased due to reduced lung
elastic recoil and/or expiratory airflow obstruction.
311
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
In patients with emphysema, total lung capacity, residual volume, and functional
residual capacity are generally increased, due to decreased lung elastic recoil. Air
trapping in emphysematous patients tends to increase expiratory reserve volume
and there by further contributes to an increased FRO.
312
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 99: A 62-year-old male visits his physician for evaluation of progressive
exertional dyspnea. His past medical history is significant for pneumonia and
hypertension. He has a 30 pack-year smoking history. On physical
examination, breath sounds are decreased bilaterally, and wheezes are heard.
A CT scan of his chest is shown below: Which of the following cell types was
likely a major contributor to this patients lung condition?
A. Eosinophils
B. Mast cells
C. Neutrophils
D. Type I pneumocytes
E. Type II pneumocytes
F. Clara cells
Explanation:
A heavy smoker with exertional dyspnea and airspace enlargement on CT likely has
centriacinar emphysema. The pathogenesis of centriacinar emphysema begins with
oxidative injury to the respiratory bronchioles and activation of resident
macrophages by components of cigarette smoke. Inflammatory recruitment of
neutrophils into these airspaces follows. Neutrophils release neutrophil elastase,
proteinase 3, cathepsin G, and matrix metalloproteinases. Activated macrophages
also release proteases. Stimulated neutrophils generate oxygen free radicals as well,
which inhibit the antiprotease activity of a1-antitrypsin. The resultant net proteaseantiprotease imbalance and oxidant-antioxidant imbalance destroys acinar walls.
Excess neutrophil elastase activity in particular is a major factor in the development
of centriacinar emphysema. (Neutrophil elastase is also important in the
development of panacinar emphysema. Panacinar emphysema most commonly
develops in individuals deficient in a1-antitrypsin, the major inhibitor of neutrophil
elastase.)
(Choice A) Eosinophils play an important role in the late phase component of Type I
immediate hypersensitivity reactions. In the lung, they are recruited to help
generate and sustain the localized inflammatory response that follows exposure to
allergens.
(Choice B) Interstitial pulmonary mast cells play a central role in the pathogenesis of
allergic asthma, particularly via release of histamine and leukotrienes that induce
bronchospasm.
(Choice D) Type I pneumocytes constitute over 95% of the inner epithelial lining of
the alveoli. This cell type is a target in the acinar wall destruction that occurs in
emphysema.
(Choice E) Type II pneumocytes are the source of pulmonary surfactant and the
main cell type responsible for repair of alveolar epithelium after destruction of type I
cells.
(Choice F) Clara cells are non-ciliated, secretory constituents of the terminal
respiratory epithelium. They secrete Clara cell secretory protein (CCSP) which
313
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
inhibits neutrophil recruitment and activation as well as neutrophil dependent mucin
production.
Educational Objective:
The pathogenesis of centriacinar emphysema associated with chronic, heavy
smoking predominantly involves intraalveolar release of proteases, especially
elastase, from infiltrating neutrophils and from alveolar macrophages.
314
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 100: A 72-year-old Caucasian male is hospitalized after complaining of
chronic fatigue and exertional dyspnea. His left ventricular pressure-volume
curve is pictured below (curve 2). Assuming heart failure is responsible for
this patients symptoms which of the following is the most likely cause of this
patients condition?
A. Viral myocarditis
B. Alcoholic cardiomyopathy
C. Amyloidosis
D. Diphtheritic myocarditis
E. High-dose doxorubicin
Explanation:
This patients left ventricular (LV) diastolic pressure-volume curve (#2) shows
reduced LV compliance (= dV/dP), indicating that diastolic dysfunction is
contributing significantly to the patients congestive heart failure. Of the various
etiologies for cardiomyopathy listed here, only amyloidosis can cause restrictive
cardiomyopathy. In restrictive cardiomyopathy due to amyloidosis, there is
infiltration of the myocardium with amyloid, making it stiffer. Diastolic dysfunction is
the predominant mechanism of heart failure in restrictive cardiomyopathy.
Restrictive cardiomyopathies may be idiopathic or due to amyloidosis, sarcoidosis,
metastatic cancer, or products of inborn metabolic errors.
(Choice A) A viral myocarditis may ultimately result in a dilated cardiomyopathy,
with systolic dysfunction as the main mechanism of heart failure.
(Choice B) Alcohol toxicity causes a dilated cardiomyopathy, with systolic
dysfunction as the main mechanism of heart failure.
(Choice D) Diphtheritic myocarditis may ultimately progress to a dilated
cardiomyopathy, with systolic dysfunction as the main mechanism of heart failure.
(Choice E) Certain chemotherapeutic agents, such as doxorubicin (Adriamycin) and
daunorubicin, can cause dose- dependent cardiotoxicity that produces a dilated
cardiomyopathy. Thus, systolic dysfunction would be the main mechanism of heart
failure.
Educational Objective:
Heart failure due to left ventricular (LV) diastolic dysfunction is the result of a
decrease in diastolic LV compliance. Restrictive cardiomyopathy, as can be caused
by amyloidosis, may cause diastolic dysfunction. Infectious myocarditis and
cardiotoxic agents including alcohol and doxorubicin tend to produce a dilated
cardiomyopathy with predominantly systolic dysfunction.
315
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 101: A 60-year-old male has been experiencing exertional chest pain that
remits with rest for the past 6 months. His past medical history is significant for
hypertension, diabetes, and hypercholesterolemia. An exercise stress test is
positive for inducible ischemia. Cardiac catheterization shows 80% occlusion of
the right coronary artery and 60% occlusion of the left coronary artery main
stem. Which of the following types of cells was most likely involved in the initial
pathogenesis of his condition?
Interstitial fibroblasts
B. Endothelial cells
C. Macrophages
D. Pericytes
E. Mast cells
F. Platelets
G. Smooth muscle cells
A.
Explanation:
This patient has a history and presentation consistent with coronary artery
atherosclerosis. The pathogenesis of atherosclerosis is thought to begin with
endothelial cell injury. In the response-to-injury model, chronic endothelial cell
injury may result from hypertension (and related hemodynamic factors)
hyperlipidemia, smoking, diabetes, homocysteine, toxins (including alcohol), viruses,
and/or immune reactions. Such injury results in endothelial cell dysfunction and/or
exposure of subendothelial collagen (endothelial cell denudation).
Endothelial cell dysfunction results in increased permeability, as well as monocyte
and lymphocyte adhesion and migration into the intima. Endothelial denudation and
exposure of subendothelial collagen promote platelet adhesion. Growth factors
produced by monocytes and platelets stimulate medial smooth muscle cell (SMC)
migration into and proliferation in the intima. At the same time, increased
endothelial cell permeability allows LDL cholesterol into the intima, where it is
phagocytosed by the accumulating macrophages and smooth muscle myocytes to
produce foam cells.
The repetitive endothelial injury results in a chronic inflammatory state within the
underlying intima. Cytokine and growth factor release by macrophages and
lymphocytes maintains the inflammation, allows continued deposition of plasma LDL
cholesterol, and stimulates the new intimal SMC to proliferate and to produce more
extracellular matrix, including collagen and proteoglycans. This chronic inflammation
can also result in necrosis of foam cells and release of their lipid contents (including
toxic oxidized LDL from macrophages) into the extracellular matrix of the intima.
As a result, the chronic inflammatory process initiated by endothelial injury may
progress from a fatly streak within the intima (containing mainly lipid-laden foam
cells) to a full1ledged fibrofatty atheroma. A core of lipid debris surrounded by
monocytes, lymphocytes, and a fibrous cap with intermixed SMC causes marked
intimal thickening.
The atherogenic progression described above is summarized in the following
illustrations:
60
USMLE WORLD STEP 1
61
PATHOPHYSIOLOGY
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice A) Fibroblasts are not thought to contribute significantly to the formation of
atheromas. The fibrous tissue including the fibrous capof atheromas is
synthesized by 3MG that have migrated to and proliferated in the intimal layer in
which the plaque forms.
(Choice C) Macrophages do play an important subsequent role in the continued
pathogenesis of felt streaks and atheromas, but they must first be recruited to the
sites of the atheroma lesions by injury to the overlying endothelium.
(Choice D) Pericytes which are particularly numerous around post capillary venules
are pluripotent cells that surround the smallest blood vessels. These cells are not
directly involved in atherosclerosis, which affects large elastic arteries and large and
medium-sized muscular arteries.
(Choice E) Mast cells are not thought to be directly involved in the pathogenesis of
atherosclerotic lesions in the intima of elastic and muscular arteries.
(Choice F) While platelets do play an important role in the continued pathogenesis of
fatty streaks and atheromas, their adhesion to the sites of the atheroma lesions is
dependent upon injury to the overlying endothelium exposing subendothelial
collagen.
(Choice G) The initial pathogenesis of atherosclerosis involves endothelial cell injury.
SMO do play an important subsequent role in the continued pathogenesis of fatty
streaks and atheromas, but they must first be recruited to the sites of the atheroma
lesions by injury to the overlying endothelium that promotes secretion of smooth
muscle chemotactic and growth factors by platelets and monocytes.
Educational Objective:
Atherosclerosis is initiated by repetitive endothelial cell injury, which leads to a
chronic inflammatory state in the underlying intima of large elastic arteries as well
as large and medium-sized muscular arteries.
62
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 102: Some patients with tetralogy of Fallot (TOF) are cyanotic at birth. Others
have relatively mild symptoms and experience only episodic cyanosis and dyspnea.
The severity of symptoms in patients with this disorder largely depends on the
severity of:
A. Right ventricular hypertrophy
B. Ventricular septal defect
C. Pulmonic stenosis
D. Aortic insufficiency
E. Atrial septal defect
Explanation:
TOF is typically characterized by: pulmonic stenosis, ventricular septal detect (VSD)
right ventricular hypertrophy (RVH) and overriding aorta (straddling the VSD). The
major physiologic problem in cyanotic TOE is right-to-left intracardiac shunting which
results from the asymmetric division of the embryonic truncus arteriosus which
causes significant stenosis of the pulmonic outflow tract. The degree of right-to-left
shunting and associated cyanosis depends upon the degree of right ventricular (RV)
outflow obstruction.
In general the VSD in TOF patients is large and nonrestrictive. Because of the
pulmonic stenosis, the pressure in the RV equals that of the left ventricle (LV). Blood
flow follows the path of least resistance. If the pulmonic stenosis is severe the blood
flows from the RV to the LV (right-to-left shunt) across the VSDI and causes
cyanosis. If the systemic vascular resistance exceeds the pulmonary vascular
resistance (determined by the degree of pulmonic stenosis), the blood flows from LV
to RV via the VSD and to the pulmonary vascular bed. These patients are acyanotic.
(Choice B) The VSD in TOE is generally large enough to permit unrestricted flow
between the RV and LV. Thus the VSD is not one of the variables that determines
the severity of the hypoxemia.
(Choice D) Whereas some patients with severe TOF may develop aortic insufficiency,
it is generally not a presenting feature of this condition.
(Choice E) Patients with TOE generally do not have atrial septal defects.
Educational Objective:
In patients with TOF the degree of RV outflow tract obstruction is the major
determinant of the degree of right-to-left intracardiac shunting, and thus of
hypoxemic symptom severity.
63
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 103: A 54-year-old Caucasian female presents to your office with exertional
dyspnea and fatigue. She also describes nocturnal episodes of dyspnea and
orthopnea. After initial evaluation cardiac catheterization was performed that
reveals the following findings (see the diagram below).
The pressure tracings shown in the diagram are most consistent with which of the
following?
A. Aortic stenosis
B. Aortic regurgitation
C. Mitral stenosis
D. Mitral regurgitation
E. Normal findings
Explanation:
This patient presents with nonspecific symptoms consistent with an inadequate
ability to increase cardiac output during exertion as well as elevated pressures in the
pulmonary circulation resulting in a degree of pulmonary edema. The v wave
corresponding to left atrial filling during the patients cardiac catheterization is
abnormal. See graph below.
Note that the peak v wave pressure corresponding to maximal left a trial filling just
prior to the opening of the mitral valve (arrowheads) is elevated. These
abnormalities are indicative of mitral regurgitation, with abnormal retrograde filling
of the left atrium during ventricular systole.
64
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
(Choice A) The major hemodynamic finding in a patient with aortic stenosis would be
a pressure difference (gradient) between the left ventricle and the aorta in the
interval delimited by points A and B on the graph in the explanation under (Choice
D). A corresponds to opening of the aortic valve and B corresponds to its closure.
Left ventricular pressure would be significantly higher than aortic pressure during
the A-B interval.
(Choice B) Aortic regurgitation would tend to elevate both the left ventricular (LV)
and left atrial diastolic pressures above their normal values. However the contour of
the left atrial pressure tracing relative to the LV pressure curve would not be
significantly alteredas it is altered in this patient.
(Choice C) Mitral stenosis affects the hemodynamic profile during cardiac
catheterization as shown below.
Note the pressure gradient between the left atrium and left ventricle during diastole
(arrows).
(Choice E) Only the aortic and left ventricular pressure tracings in this patient have a
grossly normal relationship.
Educational Objective:
An abnormally prominent (regurgitant) left atrial v wave during cardiac
catheterization is a major hemodynamic finding indicative of mitral regurgitation.
65
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 104: Cardiac catheterization is performed in a 7-year-old Caucasian male,
demonstrating the following pattern of oxygen saturation in cardiac chambers
and outflow tracts.
The patient most likely has which of the following findings on physical examination?
A. Decreased femoral-to-brachial blood pressure ratio
B. Fixed splitting of S2 on cardiac auscultation
C. Holosystolic murmur over the left sternal border
D. Mucosal cyanosis and fingernail clubbing
E. Machinery-like murmur over the upper precordium
F. Spike-and-dome carotid pulse upstroke
Explanation:
This patient has undergone cardiac catheterization to detect a possible intracardiac
shunt via the oximetric method. When a shunt is suspected, direct measurement of
the PO2 and O2 saturation (SO2) in both right heart chambers (right atrium [PA]
right ventricle [RV] and the pulmonary artery is performed. In normal individuals
302 is identical in these locations. However, this patient has an abnormal increase in
902 (an oxygen step-up) from the PA to the RV, indicating the presence of a leftto-right shunt. The most likely anatomic explanation is a ventricular septal defect
(VSD)I which would allow left ventricular blood to enter the PV during systole.
VSD is the most common congenital heart disease, accounting for about 25% of
cases. Most pediatric patients have small defects (restrictive defects), which produce
high resistance to flow from the left side to the right side and thereby preserve a
significant pressure gradient between the to ventricles. Turbulent, high-velocity
blood flow across such a small VSD produces a loud holosystolic murmur best heard
over the left sternal border in the third or fourth intercostal space. In larger
(nonrestrictive) VSDs, this systolic murmur may be absent, due to decreased
resistance across the VSD and a lower transseptal pressure gradient.
(Choice A) A decreased femoral-to-brachial blood pressure ratio is found in
congenital coarctation of the aorta.
(Choice B) Fixed, wide splitting of S2 is present in patients with atrial septal defects
(ASD). These lesions may produce SO2 increases from the vena cava to the PA but
would not produce such an oxygen step-up from the PA to the PV.
(Choice D) Mucosal cyanosis and fingernail clubbing could be observed in any of the
cyanotic congenital heart diseases (e.g. transposition of the great vessels, truncus
66
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
arteriosus, tetralogy of Fallot), or as late features of an atrial or ventricular septal
defect (Eisenmengers syndrome). Transposition with a simultaneous VSD could
produce oximetric findings on cardiac catheterization similar to those seen in this
patient. However, transposition accounts for only about 5% of congenital heart
disease cases, and would be a far rarer occurrence than an isolated VSD. Blood flow
across the VSD in tetralogy is usually right to left as a result of pulmonic stenosis,
thus producing an SO2 drop in the left ventricle.
(Choice E) A precordial machinery-like murmur is a continuous murmur that occurs
during both systole and most of diastole, and is heard in patients with patent ductus
arteriosus (PDA).
(Choice F) Spike-and-dome carotid pulse upstrokes are characteristic of hypertrophic
obstructive cardiomyopathy, a condition associated with dynamic left ventricular
outflow tract obstruction during systole. Hypertrophic obstructive cardiomyopathy
would not alter the normally identical SO2 values in right-sided vessels and
chambers.
Educational Objective:
A significant increase in blood oxygen saturation between two right-sided vessels or
chambers indicates the presence of a left-to-right shunt. If such an oxygen step-up
occurs from the IRA to the RV, a VSD is most likely responsible. VSD is the most
common congenital heart disease. Small VSDs produce a holosystolic murmur that is
loudest over the left mid-sternal border. Fixed splitting of S2 is found in patients
with ASD. Aortic coarctation produces a decreased femoral-to-brachial blood
pressure ratio. PDA produces a continuous systolic and diastolic, machinery-like
murmur. The most common congenital heart disease producing early cyanosis is
tetralogy of Fallot.
67
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 105: A 45-year-old Caucasian male presents to your office with abdominal
discomfort and recent weight loss. Stool guaiac testis positive. If detected on
further work-up, an ulcer in which of the following locations is most likely to be
benign?
A. Esophagus
B. Stomach
C. Duodenum
D. Sigmoid colon
E. Rectum
Explanation:
Gastrointestinal ulcers are defined as breaches of the alimentary tract mucosa that
extend through the muscularis mucosae into the submucosa (or beyond). Those
specifically designated as peptic ulcers are chronic lesions in areas exposed to acid
and peptic juices: the most common locations of peptic ulcers include the proximal
duodenum antral stomach, and gastroesophageal junction. Peptic ulcers are
frequently associated with the presence of Helicobacter pylon, which increases the
risk of developing gastric carcinoma five-fold. Colonization with this bacteria does
not similarly elevate the risk of duodenal carcinoma, however. Adenocarcinoma of
the small intestine is an extremely rare neoplasm that appears to arise sporadically.
(Choice A) Esophageal adenocarcinoma is typically associated with an ulcerated
exophytic lesion at the gastroesophageal junction. Similarly, squamous cell
carcinomas originate as plaque-like thickenings of the mucosa that may eventually
become excavated and ulcerated.
(Choice B) Gastric carcinoma is typically associated with a poorly defined, excavated
ulcer bordered by irregular, heaped-up mucosa.
(Choices D and E) Carcinomas of the distal colon tend to be annular lesions that
result in napkin-ring constriction of the bowel, with heaped-up edges and an
ulcerated central region. In addition, ulcerative colitis is associated with an increased
risk of colorectal cancer. Accordingly, ulcers in the sigmoid colon and rectum are
suspect for malignancy.
Educational Objective:
Duodenal ulcers are not associated with an increased risk of carcinoma in the same
location. In contrast, esophageal, gastric, and colorectal cancers are frequently
identified as ulcerative lesions on endoscopy.
68
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 106: Patients with tetralogy of Fallot (TOE) may assume a squatting position
during episodes of severe cyanosis and dyspnea (tet spells). The posture helps
to:
A. Improve respirators muscle work
B. Decrease pulmonary vascular resistance
C. Increase systemic vascular resistance
D. Decrease pulmonary flow
E. Decrease left ventricular work load
Explanation:
Squatting increases the total systemic vascular resistance (SVR). In TOE, the
amount of shunted blood bypassing the lungs decreases as the ratio SVR/PVR
increases (where PVR denotes pulmonary vascular resistance). Thus, increases in
SVR relative to PVR permit a greater fraction of the total cardiac output to pass
through the lungs, improving arterial oxygenation.
(Choice A) Squatting tends to increase intra-abdominal pressure, and thus would not
decrease the work of breathing.
(Choice B) In TOE the PVR is generally determined by the fixed infundibular stenosis
in the right ventricular outflow tract. Thus, although squatting temporarily increases
venous return it would be unlikely to affect PVR in these patients. In normal
individuals, however squatting might decrease PVR somewhat, based on the
increased pulmonary blood volume.
(Choice D) Squatting increases SVR and decreases right-to-left shunting thereby
increasing pulmonary blood flow.
(Choice E) Since squatting simultaneously increases SVR and venous return, left
ventricular (LV) stroke volume and mean arterial pressure both rise. Although there
may also be a degree of reflex bradycardia, the net effect of increased LV preload
and afterload would likely be to increase LV work done per unit time.
Educational Objective:
In patients with TOE, squatting increases SVR and decreases right-to-left shunting,
thereby increasing pulmonary blood flow. Squatting thus counteracts arterial
desaturation during hypoxemic spells.
69
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 107: A 32-year-old Caucasian female who has suffered from progressive
exertional dyspnea over several years dies suddenly. At autopsy her heart has
the following appearance (RV = right ventricle, LV = left ventricle):
This patient most likely suffered from:
A. Essential hypertension
B. Dilated cardiomyopathy
C. Primary pulmonary hypertension
D. Myocardial infarction
E. Acquired aortic stenosis
F. Wolf-Parkinson-White syndrome
Explanation:
The wall of the right ventricle (RV) is at least 2 cm in thickness and is markedly
thicker than that of the left ventricle. In a normal heart, the RV thickness is 3-4 mm
during diastole, and is significantly thinner than the LV wall during diastole (around
1 cm). Thus, this specimen demonstrates right ventricular hypertrophy (RVH).
Cor pulmonale is defined as RVH (with or without congestive right heart failure)
caused by pulmonary hypertension. Pulmonary hypertension can result from disease
of the lung parenchyma or lung vasculature. The most common cause of pulmonary
hypertension is obliteration of segments of the pulmonary vasculature by chronic
obstructive pulmonary disease. However, in young women between the ages of 20
and 40, idiopathic (primary) pulmonary hypertension must be considered. In
primary pulmonary hypertension, there is progressive proliferation of endothelial
cells smooth muscle cells and intimal cells. There is striking medial hypertrophy of
arterioles and small arteries as well as concentric laminar intimal fibrosis. In some
cases the lumina is narrowed to a pinpoint diameter. As with the patient in the
vignette, patients may present first with dyspnea and fatigue. Respiratory distress,
cyanosis and right ventricular hypertrophy ensue with death generally occurring
within 2 to 5 years of the onset of decompensated cor pulmonale.
(Choices A and E) Essential hypertension and aortic stenosis would cause left
ventricular hypertrophy, not right ventricular hypertrophy.
(Choice B) Dilated cardiomyopathy (DCM) typically increases the size of the four
chambers of the heart. As is evident in the above gross specimen this patients left
ventricular cavity is small or normal in size not enlarged. (Normal diameter at the
level of the junction of the mitral valve with its chordae tendineae is 5 cm.)
Moreover the LV here is relatively normal in shape (elliptical with a long axis about
twice that of lateral short axis dimensions) which is not the case with LV dilatation.
(Choice F) Wolf-Parkinson-White syndrome must be suspected in any case of sudden
cardiac death in an otherwise healthy young individual. WPW is an
electrophysiological abnormality of atrioventricular cardiac conduction and does not
bear any consistent association with gross morphological changes to the ventricles.
On histologic exam WPW shows small accessory atrioventricular impulse conduction
pathway(s) anatomically separate from the AV node.
70
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Under normal circumstances, the right ventricular (RV) thickness is between 3-4mm
during diastole, significantly thinner than the left ventricular wall thickness (1 cm).
RVH is a feature of cor pulmonale, a condition caused by pulmonary hypertension
resulting from disease of the lung parenchyma or the pulmonary vasculature. In
young females between the ages of 20 and 40, primary pulmonary hypertension
may be responsible for cor pulmonale.
71
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 108: A 48-year-old Caucasian male presents with chest pain and syncope.
Coronary arteriography demonstrates significant atherosclerotic involvement of
the left anterior descending and circumflex arteries. Which of the following cells
provides major proliferative stimuli for the cellular components of atherosclerotic
plaques?
Neutrophils
B. Eosinophils
C. Mast cells
D. Erythrocytes
E. Platelets
F. B lymphocytes
A.
Explanation:
The pathogenesis of atherosclerotic plaques (atheromas) is thought to begin with
endothelial cell injury, which results in endothelial cell dysfunction and/or exposure
of subendothelial collagen (endothelial cell denudation). Exposure of subendothelial
collagen promotes platelet adhesion, aggregation, and release of factors that
promote migration of smooth muscle cells (SMC) from the media into the intima, as
well as SMC proliferation. These factors include platelet-derived growth factor
(PDGF) and transforming growth factor beta (TGF-13). PDGF is chemotactic and
mitogenic for SMC. TGE-3 is chemotactic for SMC.
(Choice A) Neutrophils do not appear to play a significant role in the chronic intimal
inflammatory process that generates atheromas, nor do they release growth factors.
(Choice B) Eosinophils do not play a significant role in the chronic intimal
inflammatory process that generates atheromas. Rather, they are important in
parasitic infections and IgE-mediated immune reactions.
(Choice D) Erythrocytes are not known to release growth factors or mitogens that
can cause SMC proliferation.
(Choice F) B-lymphocytes are responsible for antibody production. Antibodies or
auto-antibodies do not appear to play a role in the initiation or progression of
atherosclerosis. While cytokines released from B-lymphocytes may play a role in
immune responses, they do not act as growth factors for SMC.
Educational Objective:
In the pathogenesis of atherosclerotic plaques, release of PDGF by platelets
adherent to areas of denuded vascular endothelium is thought to play an important
role in promoting both the migration of SMC from the media into the intima, and
their subsequent proliferation in the intima.
72
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 109: A 56-year-old male presents complaining of progressively worsening
dyspnea. He says that he cannot walk more than few blocks without getting
short of breath, and finds it particularly difficult to sleep while lying flat. He uses
three pillows at night. The patient does not use tobacco, alcohol or drugs. He
has been diagnosed with hypertension, but only takes his medication when he
experiences headaches. His blood pressure today is 170/100mm Hg and his
pulse is 80 beats per minute. On physical examination, there are basilar lung
crackles bilaterally, jugular venous distention, and bilateral trace lower
extremity edema. There is cardiomegaly on chest x-ray, and evidence of left
ventricular hypertrophy on EKG. Echocardiogram shows significant pulmonary
arterial hypertension. Which of the following is the most likely explanation for
this patients pulmonary hypertension?
Mechanical obstruction of the pulmonary arterial tree
B. Hypoxia-induced pulmonary vasoconstriction
C. Obliteration of the pulmonary vascular bed
D. Inflammatory pulmonary vascular reaction
E. Reactive vasoconstriction due to venous congestion
F. Increased volume of flow and pressure in the pulmonary arteries
A.
Explanation:
The patient in the vignette appears to have left sided heart failure (likely due to
long-standing hypertension), which may have eventually led to pulmonary
hypertension and right heart failure.
Chronic hypertension is the most common cause of left ventricular (LV) diastolic
dysfunction or hypertensive heart disease (HHD). HHD is characterized by concentric
LV hypertrophy, which decreases LV diastolic compliance. As a result, steady state
LV filling pressures rise to maintain stroke volume and cardiac output. Pulmonary
venous pressures, and therefore pulmonary arterial pressures, increase as a result,
causing pulmonary hypertension, which promotes the development of right sided
heart failure.
Additional mechanisms have been proposed to explain the pulmonary hypertension
in chronic left-sided heart failure, including dysregulation of pulmonary vascular
smooth muscle tone and structural remodeling of the pulmonary vasculature
secondary to impaired nitric oxide availability and increased endothelin expression. A
form of reactive pulmonary arterial vasoconstriction is thought to result.
(Choice A) Mechanical obstruction of the pulmonary arterial tree occurs in massive
pulmonary embolism. No features of the patients history or physical raise serious
suspicion for pulmonary emboli.
(Choices B and C) Hypoxia-induced vasoconstriction likely underlies the
pathogenesis of pulmonary hypertension secondary to CCPD. Polycythemia and
obliteration of the vasculature follow compounding the increase in pulmonary arterial
pressure. The patient in the vignette appears to have left-sided heart failure
(orthopnea, crackles) in addition to right-sided failure (elevated JVP and peripheral
edema), rather than CCPD. Additionally, because he is nota smoker, CQPD is an
unlikely diagnosis.
(Choice D) Inflammatory pulmonary vascular reactions maybe seen in pulmonary
vasculitides such as Wegeners granulomatosis and Churg-Strauss syndrome. In rare
instances, these may result in secondary pulmonary hypertension.
(Choice F) Flow volume and pressure maybe increased in the pulmonary arteries in
congenital heart diseases that cause left-to-right shunts. A large VSD will quickly
cause pulmonary hypertension at young age, secondary to medial hyper trophy of
73
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
the pulmonary vasculature. An ASD will typically take longer to produce such effects,
due to a lesser degree of volume and pressure overload.
Educational Objective:
Left ventricular dysfunction can lead to increased pulmonary arterial pressure.
Reactive changes in the pulmonary vasculature (e.g. endothelial dysfunction
resulting in vasoconstriction) may also contribute to pulmonary hypertension.
Hypoxia-induced vasoconstriction probably plays the major role in the pathogenesis
of pulmonary hypertension secondary to CC) PD.
74
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 110: A 44-year-old Caucasian male is successfully treated for infective
endocarditis with a long course of antibiotics. Echocardiographic evaluation
reveals significant aortic regurgitation as a consequence of the infection.
Which of the following is the major hemodynamic compensation for this
valvular abnormality?
Increase in left ventricular afterload
B. Increase in left ventricular preload
C. Concentric left ventricular hypertrophy
D. Sustained increase in heart rate
E. Decrease in aortic elasticity
A.
Explanation:
In a patient with relatively acute aortic regurgitation, the major hemodynamic
adaptation to maintain cardiac output is an increase in the left ventricular end
diastolic volume (EDV). Assuming no acute decrease in contractility, this preload
increase allows forward LV stroke volume (FSV) in the new steady state to remain
adequate, although reduced from normal.
(Choice A) Left ventricular (LV) afterload is already increased in acute aortic
regurgitation (AR), and is associated with a greatly increased LV total stroke volume
and a widened pulse pressure. A further increase in afterload would increase the
regurgitant stroke volume and further decrease the LV forward stroke volume (FSV),
thereby further reducing cardiac output. This is why medical stabilization of patients
with severe acute AR may include administration of a vasodilator (nitroprusside) in
addition to an intravenous positive inotropic agent (dopamine or dobutamine). The
vasodilator decreases after load in order to improve the FSV.
(Choice C) Aortic regurgitation subjects the left ventricle (LV) to volume overload,
not pressure overload. The adaptation to volume overload is eccentric hypertrophy,
i.e. chamber dilation (due to increased end diastolic volume, EDV) with
predominantly in series synthesis of new myocardial sarcomeres. Concentric
hypertrophy, the response to pressure overload, involves in parallel deposition of
new sarcomeres, which produces net ventricular wall thickening and a reduction in
ventricular chamber size (decreased EDV). Pressure overload may occur in aortic
stenosis or systemic hypertension.
(Choice D) This patients relatively acute aortic regurgitation (AR) would decrease
the left ventricular forward stroke volume. The acute compensatory response to
maintain cardiac output would include an increase heart rate. Patients with acute AR
are usually tachycardic and poorly tolerant of lower heart rates. However this
answer choice describes a sustained increase in heart rate. As the heart of a patient
who survives acute AR adapts to volume overload, increased left ventricular end
diastolic volume (LVEDV) and eccentric LV hypertrophy result in progressive
increases in LV forward stroke volume. Heart rate therefore returns toward normal in
chronic AR, so that sustained tachycardia is not the major final hemodynamic
compensation.
(Choice E) A decrease in aortic elasticity would tend to increase afterload. An
increase in afterload would further decrease net left ventricular (cardiac) output.
Educational Objective:
An increase in left ventricular preload (LV end-diastolic volume) in association with
eccentric LV hypertrophy is the major lasting hemodynamic compensation to the
volume overload of aortic regurgitation.
75
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 111: A 34-year-old female experiences nausea, abdominal pain and dizziness
after a minor surgical procedure. One year ago, she was diagnosed with systemic
lupus erythematosus (SLE) with significant renal involvement, and she has been on
chronic corticosteroid therapy since that time. Her blood pressure is now 70/40
mmHg and her heart rate is 120 beats per minute. Which of the following changes
in CRH, ACTH, and cortisol are most likely responsible for this patients symptoms?
A.
B.
C.
D.
E.
CRH
Increased
Increased
Increased
Decreased
Decreased
ACTH
Increased
Increased
Decreased
Decreased
Decreased
Cortisol
Increased
Decreased
Decreased
Increased
Decreased
Explanation:
The clinical features described in this vignette are suggestive of central adrenal
insufficiency secondary to long-term pharmacological doses of glucocorticoids.
Patients using pharmacological (i.e. in excess of physiological levels) doses of
glucocorticoids for more than 3 weeks are likely to develop hypothalamic-pituitaryadrenal (HPA) axis suppression. Biochemically HPA axis suppression is characterized
by low CRH, low ACTHI and low cortisol. The level of HPA axis suppression depends
upon the type and potency of glucocorticoid used. More potent glucocorticoids used
for longer durations are more likely to cause suppression, whereas topical
glucocorticoids (i.e. very low systemic doses) are less likely to produce suppression
of the HPA axis.
When pharmacological doses of glucocorticoid therapy are used for more than three
weeks duration, treatment cessation should be gradual (i.e. a steroid taper) to
prevent development of adrenal insufficiency. Rapid withdrawal of glucocorticoids
after prolonged use can cause acute adrenal crisis in patients, especially those under
stressful situations (i.e. infections, surgery). Cortisol plays an important
cardiovascular role during stress. In normal individuals, there is a 3- to 9-fold
increase in the level of endogenous glucocorticoids during stressful situations. In a
patient with a suppressed HPA axis, this response is lacking. The patient in this
vignette shows signs and symptoms of adrenal crisis (likely precipitated by her
surgical procedure), characterized clinically by nausea, vomiting, hypotension, and
tachycardia.
(Choice B) In this choice CRH and ACTH are increased and cortisol is decreased, a
pattern suggestive of a primary adrenocortical problem. Damage to the adrenal
glands by an autoimmune process or infection can lead to primary hypoadrenalism.
This causes an increase in CRH and ACTH via loss of negative feedback inhibition
due to low serum cortisol levels.
(Choice C) In this choice CRH is increased while ACTH and cortisol are decreased, a
pattern suggestive of a primary pituitary problem. ACTH is secreted by the
corticotrophs of the anterior pituitary. Damage to the pituitary gland by tumor,
infarction or infection can cause decreased release of ACTHI which in turn leads to
decreased cortisol production. (ACTH has a trophic effect on adrenocortical cells.)
Decreases in cortisol increase hypothalamic CRH release. Here, however, the
pituitary cannot respond with an increase in ACTH release because it is damaged.
(Choice D) This scenario is suggestive of autonomous production of cortisol from an
adrenal adenoma. Excessive cortisol production from an adrenal adenoma
suppresses CRH and ACTH production by the hypothalamus and pituitary,
respectively.
76
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Educational Objective:
Depression of the entire hypothalamus-pituitary-adrenal axis by glucocorticoid
therapy is the most common cause of adrenal insufficiency.
77
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 112: A 79-year-old male presents to your office with aching bones. He says
that the pain is most pronounced in his back, pelvis, and lower extremities. Pain is
dull and increases after weight bearing activities. He was diagnosed with actinic
keratosis one year ago. and he has been avoiding sunlight religiously. After a
thorough evaluation of this patient, you recommend him to spend about 15 minutes
a day in the outdoors. Which of the following reactions of vitamin D metabolism
underlies your recommendation?
A.
B.
C.
D.
A
B
C
D
Explanation:
On exposure to sunlight1 7-dehydrocholesterol found in the skin (also called
provitamin D3) absorbs ultraviolet-B rays from the sun. Rays with a wavelength
between 290 and 350 nm open up the B-ring of 7-dehydrocholesterol, forming
previtamin D3, which then undergoes thermal isomerization to form vitamin D3, or
cholecalciferol. Excessive sunlight exposure, however, shunts previtamin D3to a
pathway that forms inactive products, such as tachysterol and lumisterol, as a
protective mechanism against excessive vitamin D. Too much vitamin D might cause
electrolyte imbalances, renal stones, renal failure, and ectopic calcium deposition
paradoxically, it might also cause osteoporosis secondary to the excessive
mobilization of bone minerals.
On the other hand, there is no physiological mechanism to protect against too little
vitamin D formation. Inadequate vitamin D is common in older patients and was
even demonstrated in a number of younger hospitalized patients in a recent study.
Factors that discourage vitamin D formation in the skin include dark coloring
(melanin prevents the conversion of 7-dehydrocholesterol to previtamin D3), the use
of sunscreen, old age, and a northern latitude. People living in northern latitudes do
not form sufficient vitamin D, even with exposure to sunlight during winter months.
The very oblique angle of the winter sun at northern latitudes allows penetration of
the atmosphere from only low energy ultraviolet-B rays.
(Choice B) After entering the circulation, vitamin D (D2 and D3) undergoes two
hydroxylation steps to form 1, 25- dihydroxy vitamin D. The first hydroxylation step
occurs in the liver: cytochrome P450 25-hydroxylase converts vitamin D into 25-
78
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
hydroxy vitamin D (calcidiol). The conversion of vitamin D to 25-hydroxy vitamin D
is not tightly regulated; therefore, circulating 25-hydroxy vitamin D measurements
accurately reflect the status of dietary and skin production of vitamin D and can be
used to assess vitamin D deficiency.
(Choices C and D) 25-hydroxy vitamin D is metabolically inactive and is converted to
the active form by the next hydroxylation step which is performed by the kidney
enzyme 1-alpha hydroxylase. Circulating parathyroid hormone (PTH) also augments
the conversion of 25-hydroxy vitamin D to 1, 25-dihydroxy vitamin D. In the case of
1 25- dihydroxy vitamin D excess, kidneys have the enzyme 24-hydroxylase, which
converts 25-hydrcxxyvitamin D to biologically-inactive 24, 25-dihyrox vitamin D.
Educational Objective:
Sunlight exposure catalyses the first reaction in the chain of active vitamin D
synthesis: 7-dehydrocholesterol transforms to cholecalciferol (Vitamin D3). Then,
25-hydroxlation occurs in the liver and the kidney enzyme 1-alpha hydroxylase
catalyzes the final step in the synthesis of active vitamin D.
79
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 113: A 34-year-old male who suffers from severe renal disease has a low
serum calcium level. Further evaluation reveals an increased serum PTH level.
Which of the following reactions of active vitamin D synthesis is most likely
impaired in this patient (see graph)?
A.
B.
C.
D.
A
B
C
D
Explanation:
On exposure to sunlight1 7-dehydrocholesterolor provitamin D3present in the
skin absorbs ultraviolet-B rays from the sun. Rays between wavelengths of 290 and
350 nm open up the B-ring of 7-dehydrocholesterol, forming previtamin D3, which in
turn undergoes isomerization induced by heat to form vitamin D3, or cholecalciferol.
At this point either physiologically-produced D3 or plant-derived D2 will undergo two
hydroxylation steps to form 1, 25- dihydroxyvitamin D, the active form of vitamin D.
(Choice B) The first hydroxylation step occurs in the liver; the cytochrome P450
enzyme 25-hydroxylase converts vitamin D into 25-hydroxyvitamin D (calcidiol).
(Choice D) Twenty-five-hydroxy vitamin D is metabolically inactive and must
undergo one more hydroxylation step to become active; this final step is catalyzed
by the kidney enzyme 1-alpha hydroxylase. Circulating parathyroid hormone (PTH)
also encourages the conversion of 25-hydroxy vitamin D to 1, 25-dihydroxy vitamin
D. If 1, 25-dihydroxy vitamin D excess occurs, kidneys have the enzyme 24hydroxylase, which converts 25-hydroxy vitamin D to biologically inactive 24, 25dihyroxy vitamin D. Excess vitamin D can cause electrolyte imbalances and kidney
problems.
The kidneys play a pivotal role in calcium metabolism. Chronic renal failure impairs
the excretion of phosphorous, so hyperphosphatemia is commonly seen in these
patients. In chronic kidney disease, the conversion of 25-hydroxy vitamin D to 1 ,
25-dihydroxyvitamin D is impaired, so levels of active vitamin D decline. This
stimulates PTH release; a decrease in serum calcium and hyperphosphatemia are
also important in augmenting the increase in PTH.
The compensatory PTH increase in renal failure is called secondary
hyperparathyroidism. High levels of PTH are required to maintain calcium levels in
patients with chronic renal failure. PTH increases serum calcium by the following
three mechanisms:
1. Increasing bone resorption by osteoclastic activation, leading to an increase in
efflux of calcium from bone to circulation
2. Increasing the renal absorption of calcium, and
80
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
3. Increasing the formation of 1, 25-dihydroxy vitamin D.
The secretion of PTH is directly suppressed by circulating levels of 1, 25
dihydroxyvitamin D.
Educational Objective:
One-alpha-hydroxylation transforms calcidiol to calcitriol in the renal tubules. In
chronic kidney disease, the conversion of 25-hydroxyvitamin D to 1,25dihydroxyvitamin D is impaired, leading to decreased circulating levels of 1,25dihydroxyvitamin D. Low levels of the active form of vitamin D cause an increase in
circulating PTHI called secondary hyperparathyroidism. Note that 24, 25dihydrocholecalciferol is an inactive substance.
81
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 114: Liver biopsy of 45-year-old Caucasian female with fatigue that
developed over the course of a year and pale stool reveals dilated bile
canaliculi with green-brown plugs and brawny pigmented hepatic
parenchyma. Which of the following is the most likely associated condition
in this patient?
Seborrhea
C. Osteomalacia
D. Amnesia and confabulations
E. Gastric atrophy
F. Hypochromic anemia
A.
Cardiac
dilation
B.
Explanation:
Cholestasis can arise secondary to hepatocellular dysfunction or biliary obstruction,
whether intrahepatic or extrahepatic. Both obstructive and nonobstructive
cholestasis are characterized by the deposition of bile pigment within the hepatic
parenchyma and the presence of green-brown plugs in the dilated bile canaliculi.
When prolonged, this reduction in bile flow causes intestinal malabsorption and
nutritional deficiencies of the fat-soluble vitamins (A, D, E and K) in particular.
Therefore those conditions associated with fat-soluble vitamin deficiencysuch as
osteomalacia would be most likely in a patient with prolonged cholestasis.
Osteomalacia is one of the most common causes of reduced bone density and, in
adults, is characterized by disordered mineralization of the newly formed bone
matrix.
(Choice A) Cardiac dilation can result from a number of causes, including viral
myocarditis, immunological abnormalities, and familial or genetic factors.
(Choice B) Seborrhea, also termed seborrheic dermatitis, is a chronic inflammatory
condition characterized by the accumulation of scaly, greasy skin on the scalp, face,
ears, and eyelids and eyebrows. Although seborrhea is not associated with
cholestasis, xanthomas (cholesterol deposits in the skin) are.
(Choice D) Amnesia and confabulations are findings commonly associated with
Wernicke-Korsakoff syndrome, a condition seen in thiamine-deficient alcoholics.
(Choice E) Gastric atrophy is commonly associated with chronic gastritis, a condition
that may be caused by H. pylori infection pernicious anemia radiation and
granulomatous conditions.
(Choice F) Hypochromic anemia describes a state in which the circulating red blood
cell mass is reduced below normal limits and demonstrates decreased
hemoglobinization. It can arise secondary to a variety of conditions including iron
deficiency anemia and thalassemia.
Educational Objective:
Digestive disorders such as cholestasis can result in malabsorption and nutritional
deficiencies of the fat-soluble vitamins leading to conditions such as osteomalacia
(which is frequently associated with a deficiency of the fat soluble vitamin D).
82
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 115: A 60-year-oldfemale is being evaluated for weight gain and fatigue.
After the initial laboratory valuation you decide to proceed with a metyrapone
stimulation test. The changes in urinary 17-hydroxy-corticosteroid (17-OHS)
excretion following metyrapone administration are shown on the graph below.
Which of the following is most likely responsible for these findings?
A. Vasopressin overproduction
B. ACTH surge
C. Renin suppression
D. Cortisol surge
E. Aldosterone suppression
Explanation:
Like most hormones cortisol secretion is regulated via a feedback loop. ACTH
stimulates cortisol secretion from the zona fasciculata of the adrenal cortex. ACTH is
itself regulated by CRH and arginine vasopressin from the hypothalamus. Cortisol
suppresses both ACTH and CRH secretion in a negative feedback loop. Decreases in
cortisol lead to increases in ACTH and CRH secretion from the pituitary and
hypothalamus, respectively. Metyrapone testing is indicated when there is suspicion
of an interruption in the hypothalamic-pituitary-adrenal (HPA) feedback loop.
Metyrapone blocks cortisol synthesis by inhibiting the enzyme 11--hydroxylase,
which is responsible for the conversion of 11--deoxycortisol to cortisol (see
enzymatic pathway). Thus with metyrapone administration, serum cortisol levels are
reduced, stimulating pituitary secretion of ACTH. In this setting, the high ACTH level
stimulates the adrenal gland to produce more deoxycortisol (since cortisol cannot be
produced due to inhibition of 11- 3-hydrorylase). Unlike cortisol, 11-deorycotsol
does not cause feedback inhibition of pituitary ACTH production. 11- deoxycortisol
metabolites are measurable in the urine as 11-hydroxy-corticosteroids. If the HPA
axis is normal, administration of metyrapone will cause a significant increase in 11deorvcortisol in serum and 11-hydroxycorticosteroids in urine. The graph shows that
following administration of metyrapone, there is a significant increase in urinary 11hydrox-corticosteroid secretion, indicating a normal HPA axis.
(Choice A) Vasopressin is a hormone secreted by the posterior pituitary that is
responsible for regulating water balance. Vasopressin causes absorption of water
from the distal and collecting tubules in the kidney. Additionally, vasopressin
stimulates pituitary ACTH secretion. However there is no clear feedback loop
between cortisol and vasopressin. Thus vasopressin overproduction is unlikely to be
responsible for increase in 17-hydroxy- corticosteroids in urine.
(Choices C and E) Short-term decreases in cortisol will have minimal effects on renin
production. The renin angiotensin system regulates aldosterone production by the
zona glomerulosa. The zona glomerulosa lacks the enzyme 17-hydroxylase and
therefore cannot synthesize cortisol. There is no significant effect of metyrapone on
the aldosterone pathway.
(Choice D) During metyrapone testing serum cortisol should significantly decrease
not increase.
Educational Objective: An ACTH surge with a resultant increase in steroid halfproduct excretion is a normal reaction to metyrapone administration because
metyrapone blocks the last step of cortisol synthesis.
83
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 116: A 14-year-old female presents to your office complaining of intermittent
shortness of breath. She is unable to link the episodes to specific events or
exposures. Physical examination is normal and her FEV1/FVC ratio is 83%. Which of
the following would be most useful in excluding asthma in this patient?
A. Normal chest X-ray
B. Negative methacholine challenge
C. Absence of eosinophilia
D. Normal serum IgE
E. Negative skin tests to various allergens
Explanation:
This patient is unable to link her symptoms to allergen exposures, the most common
cause of asthma. Moreover, her FEV1/FVC ratio is close to normal (around 80%). In
asthmatics FEV1/FVC is often reduced due to increased expiratory airflow resistance.
The clinical suspicion here is reasonably low, thus, a test to rule out the diagnosis of
asthma would be appropriate.
While there are few, if any, specific tests that can confirm (rule in) a diagnosis of
asthma, bronchial challenge testing is a highly sensitive but non-specific measure
that can help exclude the diagnosis. Bronchial challenge testing assesses bronchial
84
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
hyperreactivity (BHFR) a central pathophysiological feature of asthma. BHR can be
quantified as the concentration of an inhaled aerosolized bronchoconstrictive
substance required to produce a 20% decline in FEV1. Methacholine, a cholinergic
muscarinic agonist, is commonly used as the inhaled test substance.
(Choice A) During an asthma attack, the lungs may appear hyperinflated on chest xray. However, chest x-rays are often normal between attacks. Thus, a normal chest
x-ray would not exclude asthma as a diagnosis here.
(Choice C) Although eosinophil counts may be elevated in asthmatics, the presence
of eosinophilia is not a sensitive or specific indicator of asthma. Sputum eosinophilia
would be a more sensitive test, as eosinophilic infiltration of the bronchial mucosa is
a common pathologic finding in allergic asthma.
(Choice D) Although serum IgE levels are generally elevated in patients with atopic
(extrinsic allergic) asthma, patients with non-immune-mediated asthma have normal
levels of serum IgE. These types of intrinsic asthma can be precipitated by
pulmonary infections (especially viral), aspirin ingestion, cold air, inhaled irritants,
stress, and/or exercise.
(Choice E) Skin tests to various allergens are often reactive in patients with atopic
(extrinsic allergic) asthma, because these patients are inherently predisposed to
develop localized immediate Type I hypersensitivity reactions to a variety of inhaled
and ingested allergens. However, patients with intrinsic asthma would not have this
predisposition to skin test allergen reactivity.
Educational Objective:
Airway challenge testing with methacholine is a highly sensitive but nonspecific
measure that can detect the degree of bronchial hyperreactivity in patients
suspected of having asthma. A negative methacholine challenge test can help to
exclude (rule out) the diagnosis. Chest x-ray, blood eosinophil count, serum IgE
level, and skin reactivity to various allergens are less sensitive; normal findings on
these tests cannot exclude the diagnosis.
85
USMLE WORLD STEP 1
PATHOPHYSIOLOGY
Q NO 117: A 50-year-old female presents with abdominal pain, diarrhea, and
weight loss. She was diagnosed with diabetes mellitus two months ago. Her
serum somatostatin level is highly elevated. Further evaluation reveals biliary
stones. Suppression of which of the following hormones is most likely
responsible for biliary stones?
Secretin
B. Cholecystokinin
C. Glucagon
D. Insulin
E. Gastrin
F. Growth hormone
A.
Explanation:
The term somatostatin was originally applied to the 14-aminoacid cyclic peptide that
is secreted by the hypothalamus and that inhibits the production of growth hormone
from the anterior pituitary gland. Somatostatin is now known to be secreted from
other parts of the central nervous system and from pancreatic delta cells.
Somatostatin secreted from pancreatic delta cells decreases the secretion of
secretin, cholecystokinin, glucagon, insulin, and gastrin. Somatostatinomas are rare
pancreatic islet cell tumors that arise from delta cells. Patients with
somatostatinomas present with hyperglycemia or hypoglycemia, steatorrhea
(excessive fat in the feces), and gallbladder stones. Gallbladder stones form because
of poor gallbladder contractility, which is secondary to inhibition of cholecystokinin
release.
(Choices C and D) Somatostatin decreases the release of glucagon as well as insulin.
However, the secretion of insulin is more profoundly inhibited than is glucagon;
therefore, the net result is hyperglycemia.
(Choice A) Steatorrhea results from the decreased secretion of secretin as well as a
decrease in gastrointestinal motility.
(Choice E) A decrease in gastrin release causes hypochlorhydria.
(Choice F) As indicated above somatostatin does decrease growth hormone secretion
from the normal pituitary gland, and it does so in growth-hormone-secreting
pituitary adenomas. However, somatostatin cannot be used in clinical practice
because of its extremely short half-life. Somatostatin analogs (octreotide and
lanreotide) have a longer plasma half-life and are available for clinical use.
Educational Objective:
Reduced gallbladder contractility, due to decreased cholecystokinin secretion, is
responsible for biliary stones in patients with somatostatinoma.
86
S-ar putea să vă placă și
- SURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1De la EverandSURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1Evaluare: 5 din 5 stele5/5 (2)
- Patho Physio 50qDocument68 paginiPatho Physio 50qRaquel BencosmeÎncă nu există evaluări
- Pharm U WorldDocument421 paginiPharm U Worldjonathan100% (8)
- How to Prepare for the Medical Boards: Secrets for Success on Usmle Step 1 and Comlex Level 1De la EverandHow to Prepare for the Medical Boards: Secrets for Success on Usmle Step 1 and Comlex Level 1Evaluare: 5 din 5 stele5/5 (1)
- Microbiology PDFDocument237 paginiMicrobiology PDFchioÎncă nu există evaluări
- Pathoma DiseasesDocument1 paginăPathoma Diseasesrvar839Încă nu există evaluări
- International Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessDe la EverandInternational Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessRaghav GovindarajanÎncă nu există evaluări
- USMLE World Pharmacology (Uworld Pharm) Flashcards - MemorangDocument4 paginiUSMLE World Pharmacology (Uworld Pharm) Flashcards - Memorangnish0420100% (1)
- U.S. MEDICAL LICENSING EXAM (USMLE) STEP I – Basic Medical Sciences: Passbooks Study GuideDe la EverandU.S. MEDICAL LICENSING EXAM (USMLE) STEP I – Basic Medical Sciences: Passbooks Study GuideÎncă nu există evaluări
- Step 1 Uworld PDFDocument25 paginiStep 1 Uworld PDFRegents Park Business Center100% (1)
- USMLE Step 1: Integrated Vignettes: Must-know, high-yield reviewDe la EverandUSMLE Step 1: Integrated Vignettes: Must-know, high-yield reviewEvaluare: 4.5 din 5 stele4.5/5 (7)
- Pathoma Video ListDocument5 paginiPathoma Video ListLolita A. Hicks100% (1)
- USMLE Step 1 in Final YearDocument11 paginiUSMLE Step 1 in Final YearsehrishÎncă nu există evaluări
- How to Create a Study Plan for the USMLE Step 1De la EverandHow to Create a Study Plan for the USMLE Step 1Evaluare: 4.5 din 5 stele4.5/5 (11)
- MS2 Resources For Step 1Document13 paginiMS2 Resources For Step 1skeebs23Încă nu există evaluări
- 002367889dissecting The USMLE - BookmarkedDocument629 pagini002367889dissecting The USMLE - BookmarkedPharAway100% (6)
- EL Husseiny's Essentials for Molecular BiochemistryDocument260 paginiEL Husseiny's Essentials for Molecular BiochemistryAbdirahman abdallahÎncă nu există evaluări
- PASS Pharm DrillsDocument36 paginiPASS Pharm DrillsSwisskelly1Încă nu există evaluări
- The Usmle Step 1 BibleDocument456 paginiThe Usmle Step 1 Biblesarasha12100% (1)
- Anatomy PDFDocument114 paginiAnatomy PDFkhualabear101100% (1)
- Step 1 Study Schedule and MaterialsDocument10 paginiStep 1 Study Schedule and MaterialstatinÎncă nu există evaluări
- Inflammation and cancer cell developmentDocument12 paginiInflammation and cancer cell developmentJohn PangÎncă nu există evaluări
- NBME 18 NotesDocument15 paginiNBME 18 Noteshector50% (2)
- Goljan - Systemic PathologyDocument326 paginiGoljan - Systemic PathologyAengus Joyce100% (8)
- USMLE Preparation Question BanksDocument3 paginiUSMLE Preparation Question BanksChandan KumarÎncă nu există evaluări
- Usmle World Ed ObjectiveDocument16 paginiUsmle World Ed ObjectiveNisarg Patel100% (3)
- Pass Program CluesDocument851 paginiPass Program Cluesshafat001100% (1)
- Uworld - PEDIATRICSDocument50 paginiUworld - PEDIATRICSNikxy100% (1)
- 4 Week Study PlanDocument9 pagini4 Week Study PlanZamaar MalikÎncă nu există evaluări
- IVMS-Gross Pathology, Histopathology, Microbiology and Radiography High Yield Image PlatesDocument151 paginiIVMS-Gross Pathology, Histopathology, Microbiology and Radiography High Yield Image PlatesMarc Imhotep Cray, M.D.100% (2)
- Goljin ItDocument37 paginiGoljin Itneutralmind100% (1)
- Renal, Urinary, Electrolyte ReviewDocument7 paginiRenal, Urinary, Electrolyte ReviewJorge L CastelarÎncă nu există evaluări
- Busy Medical Student's Guide To Score Higher On Any ExamDocument57 paginiBusy Medical Student's Guide To Score Higher On Any ExamDeus Io Vult100% (5)
- 10 Ways To Succeed With USMLE Step 1Document19 pagini10 Ways To Succeed With USMLE Step 1Zunaira Abdul Ghaffar100% (2)
- 20 Questions Pulmonology ReviewDocument13 pagini20 Questions Pulmonology ReviewSunita Shah0% (1)
- How I Scored A 270 On USMLE Step 1Document7 paginiHow I Scored A 270 On USMLE Step 1sankgupta100% (1)
- Goljan Step 1 PDFDocument3 paginiGoljan Step 1 PDFTrey0% (1)
- Shelf Study TipsDocument114 paginiShelf Study TipsAztecÎncă nu există evaluări
- Setp 1 AdviceDocument101 paginiSetp 1 AdviceStorage Liz100% (1)
- High Yield StudyGuide FINAL PDFDocument6 paginiHigh Yield StudyGuide FINAL PDFRichardÎncă nu există evaluări
- 28-DAY MED STUDY SCHEDULEDocument13 pagini28-DAY MED STUDY SCHEDULEgemazy123100% (3)
- Step 2 Clinical Knowledge (CK) : Sample Test QuestionsDocument59 paginiStep 2 Clinical Knowledge (CK) : Sample Test QuestionsMe back to MeÎncă nu există evaluări
- STEP 2 CK New Free 120 (Q)Document59 paginiSTEP 2 CK New Free 120 (Q)M. Baidar SaeedÎncă nu există evaluări
- Usmle World Step 1 Biochemistry: Question ListDocument85 paginiUsmle World Step 1 Biochemistry: Question ListWajeeh RehmanÎncă nu există evaluări
- Ethics and Biostats Uworld NotesDocument9 paginiEthics and Biostats Uworld NotesNada AK100% (1)
- Step2ck Practice TestDocument67 paginiStep2ck Practice TestAlf CarlÎncă nu există evaluări
- Continuously Updated ALL USMLE DATADocument4 paginiContinuously Updated ALL USMLE DATAflashjetÎncă nu există evaluări
- UWorld Internal Medicine ReviewDocument14 paginiUWorld Internal Medicine Reviewjuli100% (1)
- USMLE Step 1 NotesDocument5 paginiUSMLE Step 1 NotesMarie SantoroÎncă nu există evaluări
- DIT Mnemonics (Complete) FlashcardsDocument31 paginiDIT Mnemonics (Complete) FlashcardsNb + XB = AV100% (1)
- Uworld NotesDocument18 paginiUworld NotesNamRita PrasadÎncă nu există evaluări
- OME StudyGuide 2monthDocument5 paginiOME StudyGuide 2monthVarÎncă nu există evaluări
- The Think Twice Strategy Guide For The USMLE Step 1Document8 paginiThe Think Twice Strategy Guide For The USMLE Step 1Shahriar Kabir DaneÎncă nu există evaluări
- HY PediatricsDocument56 paginiHY PediatricsJamesIwuÎncă nu există evaluări
- Pass ProgramDocument528 paginiPass ProgramEvelyn Lee Russell67% (3)
- Notes Pathoma Webinar PDF PDFDocument84 paginiNotes Pathoma Webinar PDF PDFNosheen Hafeez100% (1)
- Review Goljan Pictures With Notes PDFDocument390 paginiReview Goljan Pictures With Notes PDFsmian08100% (1)
- 240s Study Schedule USMLE Step 2Document6 pagini240s Study Schedule USMLE Step 2Mandeep baggaÎncă nu există evaluări
- Anatomy and Behavioral Kaplan VIdeosDocument4 paginiAnatomy and Behavioral Kaplan VIdeosDiorella Marie López GonzálezÎncă nu există evaluări
- Us Mle Content OutlineDocument34 paginiUs Mle Content OutlineMariela LopezÎncă nu există evaluări
- Step 3 Experience With CCS TipsDocument6 paginiStep 3 Experience With CCS TipsDiorella Marie López González100% (4)
- Anatomy and Behavioral Kaplan VIdeosDocument4 paginiAnatomy and Behavioral Kaplan VIdeosDiorella Marie López GonzálezÎncă nu există evaluări
- NBME Form 1 Sections 1-4 ReviewDocument39 paginiNBME Form 1 Sections 1-4 ReviewDiorella Marie López GonzálezÎncă nu există evaluări
- SampleCCSCasesforUSMLEStep3.Doc (.)Document9 paginiSampleCCSCasesforUSMLEStep3.Doc (.)csquizzardÎncă nu există evaluări
- Https:catalog Uta Edu:pdf:2019-2020 PDFDocument1.135 paginiHttps:catalog Uta Edu:pdf:2019-2020 PDFDiorella Marie López GonzálezÎncă nu există evaluări
- CCS Cases TemplateDocument7 paginiCCS Cases TemplatesaraatifÎncă nu există evaluări
- Pathoma ChecklistDocument3 paginiPathoma ChecklistDiorella Marie López GonzálezÎncă nu există evaluări
- Graber and Wilburs Family Medicine Exami PDFDocument8 paginiGraber and Wilburs Family Medicine Exami PDFDiorella Marie López GonzálezÎncă nu există evaluări
- USMLE Step 1 Comprenhensive Review Part IIDocument72 paginiUSMLE Step 1 Comprenhensive Review Part IIDiorella Marie López González100% (1)
- Family Medicine Review: September 30 - October 5, 2018Document9 paginiFamily Medicine Review: September 30 - October 5, 2018Diorella Marie López GonzálezÎncă nu există evaluări
- Us Mle Content OutlineDocument34 paginiUs Mle Content OutlineMariela LopezÎncă nu există evaluări
- Pathoma ChecklistDocument3 paginiPathoma ChecklistDiorella Marie López GonzálezÎncă nu există evaluări
- USMLE Step 1 Comprenhensive Review Part 1Document75 paginiUSMLE Step 1 Comprenhensive Review Part 1Diorella Marie López GonzálezÎncă nu există evaluări
- Mike's Neuro Block 2 ReviewDocument133 paginiMike's Neuro Block 2 ReviewDiorella Marie López GonzálezÎncă nu există evaluări
- USMLE Step 1 Comprenhensive Review Part 1Document75 paginiUSMLE Step 1 Comprenhensive Review Part 1Diorella Marie López GonzálezÎncă nu există evaluări
- Mike Neuro Review Block 2 Part 1 WquestionsDocument67 paginiMike Neuro Review Block 2 Part 1 WquestionsDiorella Marie López GonzálezÎncă nu există evaluări
- p3085 PDFDocument1 paginăp3085 PDFDiorella Marie López GonzálezÎncă nu există evaluări
- Behavioral Science Terminologies DEFINEDDocument9 paginiBehavioral Science Terminologies DEFINEDDiorella Marie López GonzálezÎncă nu există evaluări
- Broadmann AreasDocument1 paginăBroadmann AreasDiorella Marie López GonzálezÎncă nu există evaluări
- Neoplasia Check ListDocument4 paginiNeoplasia Check ListDiorella Marie López GonzálezÎncă nu există evaluări
- Cell Injury and Adaptation Part 3 Sept 2016Document85 paginiCell Injury and Adaptation Part 3 Sept 2016Diorella Marie López GonzálezÎncă nu există evaluări
- Immuno Review Topic 3Document8 paginiImmuno Review Topic 3Diorella Marie López GonzálezÎncă nu există evaluări
- Class Schedules: Mon May 11 - Fri May 15, 2015 (Port of Spain)Document1 paginăClass Schedules: Mon May 11 - Fri May 15, 2015 (Port of Spain)Diorella Marie López GonzálezÎncă nu există evaluări
- 7610 PiDocument2 pagini7610 PiDiorella Marie López GonzálezÎncă nu există evaluări
- Doctor of Medicine Curriculum - UHSADocument2 paginiDoctor of Medicine Curriculum - UHSADiorella Marie López GonzálezÎncă nu există evaluări
- Nelson GNDocument280 paginiNelson GNNirvair SinghÎncă nu există evaluări
- Urinalysis and Body Fluids2020Document47 paginiUrinalysis and Body Fluids2020MONFOLA100% (1)
- GotaDocument17 paginiGotaAtelos EctasiaÎncă nu există evaluări
- 03 Medication-Related ProblemsDocument13 pagini03 Medication-Related ProblemsRoselyn DawongÎncă nu există evaluări
- Kumpulan Soal GinjalDocument28 paginiKumpulan Soal GinjalTheddyon BhenlieÎncă nu există evaluări
- CBSE Class 10 Life Processes MCQ Practice QuestionsDocument8 paginiCBSE Class 10 Life Processes MCQ Practice QuestionsBasavarajÎncă nu există evaluări
- STPM Biology Trial QuestionsDocument13 paginiSTPM Biology Trial QuestionsThen MoliÎncă nu există evaluări
- Unlock SGCh16Document7 paginiUnlock SGCh16SilaxÎncă nu există evaluări
- Excretory System WorksheetDocument4 paginiExcretory System WorksheetAlexis CastellanosÎncă nu există evaluări
- Ewout JasperDocument400 paginiEwout JasperJohnny AtmanÎncă nu există evaluări
- Genitourinary System: Billy Ray A. Marcelo, RNDocument35 paginiGenitourinary System: Billy Ray A. Marcelo, RNDarell M. BookÎncă nu există evaluări
- Physiology (2 Course)Document9 paginiPhysiology (2 Course)Divine ElyaÎncă nu există evaluări
- Aubf 2020Document447 paginiAubf 2020kurt Allen MacarilayÎncă nu există evaluări
- Excretory Products and Their Elimination: SolutionsDocument10 paginiExcretory Products and Their Elimination: SolutionsEkta ManglaniÎncă nu există evaluări
- Urinary EliminationDocument64 paginiUrinary EliminationMalik100% (2)
- NPNs and Kidney Function TestsDocument10 paginiNPNs and Kidney Function TestsAngelo Jude CobachaÎncă nu există evaluări
- Deogiri College Aurangabad: Examination 2020-2021Document7 paginiDeogiri College Aurangabad: Examination 2020-2021M SuÎncă nu există evaluări
- DPP - Excretory Productes & Their Elimination PDFDocument7 paginiDPP - Excretory Productes & Their Elimination PDFKisna guptaÎncă nu există evaluări
- Final GusDocument57 paginiFinal GusDebbi YuniseraniÎncă nu există evaluări
- IAL - Bio - SB2 - Teaching Plans - 7CDocument21 paginiIAL - Bio - SB2 - Teaching Plans - 7CsalmaÎncă nu există evaluări
- 1851968974biology Class X For Sa-I 2015-16Document99 pagini1851968974biology Class X For Sa-I 2015-16Afandi AmkajaÎncă nu există evaluări
- PhysioEx Exercise 9 Activity 5Document3 paginiPhysioEx Exercise 9 Activity 5Gonzeilo11Încă nu există evaluări
- Chapter19-Birds NotesDocument8 paginiChapter19-Birds Notesapi-195601294100% (1)
- Quiz 4Document6 paginiQuiz 4Andrew DarnelÎncă nu există evaluări
- WBJEE Medical 2016 Biology QuestionsDocument11 paginiWBJEE Medical 2016 Biology QuestionsMarcus RashfordÎncă nu există evaluări
- Urinary SystemDocument59 paginiUrinary SystemSaajid AmraÎncă nu există evaluări
- MeridiansDocument11 paginiMeridiansa2017399883% (6)
- Case Study HyperkalemiaDocument10 paginiCase Study HyperkalemiaJamaica Cerrero100% (1)
- Key Cardiovascular ConceptsDocument18 paginiKey Cardiovascular ConceptsSummer KohistaniÎncă nu există evaluări
- Biomarkers in Progressive Chronic Kidney Disease. Still A Long Way To GoDocument13 paginiBiomarkers in Progressive Chronic Kidney Disease. Still A Long Way To GoconstanzanazarethÎncă nu există evaluări
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesDe la EverandThe Ultimate Guide To Memory Improvement TechniquesEvaluare: 5 din 5 stele5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementDe la EverandTechniques Exercises And Tricks For Memory ImprovementEvaluare: 4.5 din 5 stele4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÎncă nu există evaluări
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 3.5 din 5 stele3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÎncă nu există evaluări
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 5 din 5 stele5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingDe la EverandThe Happiness Trap: How to Stop Struggling and Start LivingEvaluare: 4 din 5 stele4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDe la EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingEvaluare: 5 din 5 stele5/5 (4)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDe la EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingEvaluare: 3.5 din 5 stele3.5/5 (31)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDe la EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsÎncă nu există evaluări
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (41)
- The Tennis Partner: A Doctor's Story of Friendship and LossDe la EverandThe Tennis Partner: A Doctor's Story of Friendship and LossEvaluare: 4.5 din 5 stele4.5/5 (4)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisDe la EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisEvaluare: 5 din 5 stele5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDe la EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisEvaluare: 5 din 5 stele5/5 (8)