Documente Academic
Documente Profesional
Documente Cultură
CMEarticleJPOG JanFeb2015 - Crash Caesarean Section For Fetal Distress
Încărcat de
matahanaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
CMEarticleJPOG JanFeb2015 - Crash Caesarean Section For Fetal Distress
Încărcat de
matahanaDrepturi de autor:
Formate disponibile
CONTINUING MEDICAL EDUCATION
JPOG JAN/FEB 2015
Crash Caesarean Section
for Fetal Distress
5 SKP
Mak Shui Lam, MBBS, MRCOG, FHKCOG, FHKAM (O&G); Kou Kam On, MBBS, MRCOG, FHKCOG, FHKAM (O&G); Ng Ching Wah, RN, RNM, BHS (Nsg), MMid;
Leung Kwok Yin, MBBS, MD, FRCOG, FHKCOG, FHKAM (O&G)
INTRODUCTION
The rate of caesarean delivery for non-reassuring fetal heart tracing ranges from
2.9% to 4.6%1 and increases over the
years.2 A delay in delivery may thus result in hypoxic ischaemic encephalopathy, stillbirth, or neonatal death, depending on the severity and duration of fetal
hypoxia/acidosis.
When life-threatening fetal distress occurs, requiring immediate delivery by abdominal operation, this
type of emergency caesarean section
is referred to as crash caesarean section, as described by MacKenzie and
Cooke.3 It belongs to grade 1 emergency caesarean section according to
the classication system proposed by
Lucas et al.46 It is also the most urgent
type, based on the continuous spectrum suggested by the RoyalCollege
of Obstetricians and Gynaecologists.4
The rate of crash caesarean is estimated to be 0.60.7%.7,8
The classication system proposed
Crash Caesarean Section is the Most Urgent Type of Caesarean Section.
by Lucas et al categorizing the urgency
of caesarean section into four grades is
es and for better communication among
are to be taken care of? It is the aim
shown in Table 1. The Royal College of
medical staff.
of this article to review the risks and
Obstetricians and Gynaecologists advo-
However, crash caesarean sec-
benefits associated with crash caesar-
cates the recognition of a continuum of
tion is not without risks to the mother
ean sections, the alternative manage-
urgency in relation to levels of urgency
or even the baby. The question, then,
ment, and ways to achieve a swift and
for caesarean section, but agrees on the
is what is a reasonable duration for
safe delivery, as well as to explore the
idea that the four dened categories re-
decision-to-delivery interval (DDI) if
medicolegal aspect of the manage-
main useful particularly for audit purpos-
both the maternal and fetal well-being
ment of fetal distress.
37
38
CONTINUING MEDICAL EDUCATION
JPOG JAN/FEB 2015
rologic signs, and asphyxia lasting more
Table 1. Classification of Urgency of Caesarean Section6
than 12 minutes caused irreversible
brain damage and functional decits. To-
Description
tal asphyxia lasting for 12 to 13 minutes
Emergency caesarean section performed when there is
immediate threat to the life of woman or fetus
caused brain damage in primates, and if
Urgent caesarean section performed when there is maternal
or fetal compromise that is not immediately life-threatening
ten lead to the death of the fetus.15
Scheduled caesarean section performed when there is a
need for early delivery but no maternal or fetal compromise
cental abruption complicated by fetal
Elective caesarean section performed at a time that suits the
woman and maternity team
a DDI of 20 minutes was associated
Garde
1
lasting more than 20 minutes, it would ofIn humans, a study of severe plabradycardia by Kayani et al showed that
with substantially reduced cerebral palsy
and neonatal death rates than did a DDI
of 30 minutes.16 Similarly, neonatal and
maternal complications in uterine rup-
MATERNAL AND FETAL RISKS
DURING CRASH CAESAREAN
DELIVERY
tive assessment, review of preoperative
ture with complete fetal extrusion were
tests, and optimization of medical condi-
shown to be low with prompt intervention
tions (eg, eclampsia, adequate preoper-
in a study by Leung et al.17
The rate of complications in crash cae-
ative fasting, appropriate premedication,
In contrast, in a large series of
sarean deliveries has been observed to
and the explanation of anaesthetic risks
17,780 emergency caesarean sections
be higher than that in emergency or elec-
to patients).11 Furthermore, crash cae-
in a national cross-sectional survey in
tive caesarean deliveries. A retrospec-
sarean sections are required in cases of
England and Wales, although the odds
tive study showed that secondary acute
placental abruption, rupture of uterus, or
of an Apgar score < 7 at 5 minutes was
caesarean section following a failed vag-
eclampsia which by themselves carry a
signicantly higher with DDI > 75 min-
inal delivery was associated with more
greater risk of maternal complications
utes, the odds with DDI of 1675 min-
lacerations of the uterine corpus com-
and poorer fetal outcome.
utes, compared with that for DDI < 15
pared with primary elective caesarean
However, a study of a small series
minutes, was not signicantly different.13
section or primary acute caesarean sec-
from a university hospital concluded
More interestingly, a retrospective study
tion without any attempt to deliver vagi-
that emergency caesarean section per-
showed that very short DDI (below 20
nally. Blood loss greater than 1,000 mL
formed in the delivery room may result
minutes) was associated with lower um-
was also signicantly more frequent with
in a DDI of less than 30 minutes, with-
bilical blood pH or Apgar scores.7 There
secondary acute caesarean section.10
out detrimental perioperative effects
are four possible reasons to explain
When a caesarean section is performed
on mother or neonate.12 Another study
these paradoxical results. First, more
in haste by a less experienced doctor and
found that the maternal requirement for
critical conditions, like cord prolapse or
without gentle tissue handling, a greater
special care for a DDI < 15 minutes was
placental abruption, might have been
risk of laceration of the uterine corpus,
not statistically signicantly different from
managed with more urgent actions by
bladder, cervix/vagina, ligaments, and
that for a DDI of 1675 minutes.13
obstetricians. Less critical conditions
10
bowel may be expected. Chances of
might be due to a transient hypoxic ef-
trauma may increase when the baby is
FETAL RISKS WITH DELAYED
DELIVERY
skin lacerations, bone fracture, and birth
fect, which can improve spontaneously. Second, not all cases studied were
not delivered gently enough. Besides,
14
In experiments with rhesus monkeys,
life-threatening fetal distress. Third, fetal
crash caesarean section may leave too
an acute asphyxial episode of less than
encephalopathy may be present before
little time for anaesthetists to thoroughly
8 minutes might not cause brain dam-
labour but be manifested as intrapar-
perform all their tasks concerning preop-
age, an episode of more than 8 but less
tum fetal distress.18 Nevertheless, the
erative preparation, including preopera-
than 10 minutes produced transient neu-
action to expedite delivery in these crit-
CONTINUING MEDICAL EDUCATION
JPOG JAN/FEB 2015
ical conditions is still required to reduce
and Gynaecologists do not provide any
staff at one time without requiring them
further damage to the infant. Fourth, the
time duration constraint on performing
to reply; (3) dedicated operation theatre;
bradycardia-to-delivery
caesarean sections.
(4) providing adequate and trained man-
interval
(BDI),
23,24
which reects the actual duration of fe-
Each caesarean section should be
power during and after ofce hours; and
tal hypoxia, may be more relevant than
performed, considering its own merits
(5) providing general or regional anaes-
DDI in terms of neonatal outcomes.17,19,20
and individual circumstances.23 In cas-
thesia within 10 minutes.25
In a retrospective study of 106 cases of
es of severe fetal distress, caesarean
uterine rupture, signicant neonatal mor-
section should be initiated expeditious-
EXPERIENCE IN HONG KONG
bidity occurred when 18 or more minutes
ly in collaboration with anaesthetic and
A tertiary-wide audit on caesarean sec-
had elapsed between the onset of pro-
other necessary support personnel. In
tion for fetal distress was performed in all
longed deceleration and delivery.17 Be-
addition, reasons for delay should be
nine public hospitals with maternity units
sides, BDI, but not DDI, has been shown
documented in the chart by obstetrical,
in Hong Kong from April to June 1997.
to be inversely correlated with neurolog-
anaesthetic, and nursing personnel.24
Of the 243 cases audited, 42.8% of de-
24
ic outcomes and umbilical arterial pH at
The 30-minute time interval is only used
liveries were achieved beyond 30 min-
delivery.19,20 A retrospective study by Le-
as an audit standard and not as a basis
utes after decision of delivery. The main
ung et al reported that the median BDI in
for judging multidisciplinary team per-
reasons for the long DDI were related to
the group with irreversible causes of fetal
formance for any individual caesarean
preparation for operation (patient stabi-
distress was 5 minutes shorter than the
section.
lization, nursing procedures, obtaining
19
group with reversible causes, while its
Although the 30 minutes is consid-
consent, language barrier), not having
median DDI was only 1 minute shorter.20
ered an auditable standard, it may not
crash caesarean section, patient transfer to the theatre, availability of surgeon,
effective anaesthesia, and operation
Each caesarean section should be performed,
considering its own merits and individual
circumstances
theatre. After improvement measures in
various hospitals were instituted, a second audit in 2000 showed a reduction in
the proportion of deliveries with DDI >
30 minutes to 29.1% because of reduction of the rst three main reasons. About
RECOMMENDATIONS AND
GUIDELINES
always be achievable. MacKenzie and
80% of the DDI was used up before skin
Cooke concluded from their study that
incision. Difculty in dissection of the
The Royal College of Obstetricians
fewer than 40% of intrapartum deliveries
scar because of previous operation, or in
and Gynaecologists and the Ameri-
by caesarean section for fetal distress
delivery because of deeply engaged fetal
can College of Obstetricians and Gy-
were achieved within 30 minutes of the
head or macrosomia was encountered in
necologists recommend that obstetric
decision. The mean DDI for 22 crash
around 10% of cases.
services are to be capable of perform-
caesarean sections was 27.4 minutes.3
From July 2011 to December 2012
ing a caesarean section within a time
On the other hand, an audit conducted
in the public hospital Queen Elizabeth
interval of 30 minutes.21,22 A shorter
at a maternity hospital in Singapore from
Hospital, 94 cases of crash caesarean
time interval of 20 minutes is recom-
February 2003 to January 2004 found
section (1.01% of 9,352 delivery epi-
mended by the German Society for
that the mean DDI for crash caesarean
sodes) were performed for fetal distress,
Gynecology and Obstetrics.7 These two
section was 7.7 minutes, with 100% of
with 93.6% achieving a DDI of 30 min-
time standards are not supported by
25
deliveries made within 17 minutes.
utes. The mean DDI was 20 minutes.
any trials. On the other hand, the Soci-
These excellent results were achieved
There was only one case having an
ety of Obstetricians and Gynaecologists
by (1) following a strict protocol; (2) us-
Apgar score of < 7 at 5 minutes among
of Canada and the Royal Australian and
ing the public announcement system,
those with DDI > 30 minutes. There was
New Zealand College of Obstetricians
instead of paging, to alert all concerned
no signicant correlation between DDI >
39
40
CONTINUING MEDICAL EDUCATION
JPOG JAN/FEB 2015
Table 2. Indications for Crash Caesarean Section
not be exposed to iatrogenic injuries or
mistakes made because of carrying out
the procedure with too much haste.5
Fetal distress with severely abnormal fetal heart rate pattern such as
prolonged bradycardia
Umbilical cord prolapse
Placental abruption associated with abnormal fetal heart rate pattern
Abnormal pH 7.2 on fetal scalp blood sampling
Ruptured uterus
Severe antepartum haemorrhage associated with abnormal fetal
heart rate pattern
In high-risk cases, anticipation and
early detection of fetal heart abnormalities allow an earlier intervention for irreversible causes and a shorter BDI, which
may help improve fetal outcome. It would
also be advisable to have a crash caesarean protocol, communication protocols,
and regular crash caesarean section
drills with feedback to familiarize staff
with the workow.8,28,29 Using a multipha-
30 minutes and Apgar score < 7 at 5 min-
rst instead of crash caesarean section.
sic project of continuous quality improve-
utes (chi-square test; P = 0.621). There
For example, stopping oxytocin infusion
ment, a hospital has recently identied
was also no difference in cord blood pH
can help resolve hypertonic uterine con-
and overcome various systematic and
between DDI within and beyond 30 min-
tractions in the case of iatrogenic uterine
individual barriers, resulting in achiev-
utes (Student t test; P = 0.715). Detailed
hyperstimulation, and use of tocolyt-
ing the 30-minute standard.28 The nal
analysis of the time required in different
ics can also be considered; ephedrine
phase of this project involved making an
steps will be performed and reported
may be given to improve the maternal
overhead announcement of code green
elsewhere.
blood pressure in cases of regional an-
with room identication in the labour and
algesia-induced maternal hypotension
delivery unit whenever emergency cae-
CAREFUL SELECTION OF
CASES
if lateral positioning of the women and
sarean section was required because of
prophylactic intravenous hydration be-
fetal distress.28 This provided immediate
Crash caesarean section is indicated
fore administration of regional analgesia
attention and prioritization of the case,
in cases with immediate threat of fetal
are not effective enough. Amnioinfusion
rapid communication with anaesthetists
death. Reported indications included fe-
can be considered when cord compres-
and operating room staff, and arrival of
tal distress with severe fetal heart abnor-
sion is suspected in the presence of olig-
additional nursing personnel to transport
malities such as persistent bradycardia
ohydramnios and characteristic variable
the patient. The mean DDI dropped from
of more than 3 minutes, cord prolapse,
decelerations on fetal heart rate monitor-
40 minutes to 20 minutes.28 In another
fetal heart abnormalities associated with
ing are noted.
hospital, code red was used to facil-
27
placental abruption or severe antepar-
When an irreversible cause is iden-
itate communication between staff for
tum haemorrhage, pH 7.2 on fetal
tied or suspected, a caesarean delivery
emergency caesarean sections and to
scalp blood sampling, uterine rupture,
should be arranged urgently but not nec-
reduce the DDI.29 However, the authors
and bleeding from vasa praevia (Table
essarily in a crash manner, depending
concluded that restriction of indications
2).
on the clinical conditions of the fetus and
for colour code emergency caesarean
When fetal heart rate abnormalities
the woman. A proportion of emergency
sections is required to avoid unjustied
are detected, it is important to assess
caesarean sections do not have a clear-
maternal and fetal complication.29
and speedily search for the underlying
ly identiable risk factor for the need for
cause,26 preferably within 1 or 2 min-
emergency intervention.8,20
7,19,22,25
utes. When a reversible cause, includ-
The decision-to-delivery interval involves three steps: (1) preparation and
transfer of the patient to the operation
theatre; (2) induction of anaesthesia; and
post-regional anaesthesia, and aorto-
ACHIEVING SAFE AND QUICK
CRASH CAESAREAN DELIVERY
caval compression,26 is identied, in
During crash caesarean section for fetal
To shorten the time required for
utero resuscitation should be attempted
distress, the woman or her baby should
patient preparation in cases of crash
ing iatrogenic uterine hyperstimulation,
(3) skin incision to delivery of baby.
CONTINUING MEDICAL EDUCATION
JPOG JAN/FEB 2015
caesarean section, anticipating the possibility of emergency caesarean section
with earlier preparation involving blood
type and screen test, fasting, and optimization of maternal condition would be of
help. Epidural for pain relief can be considered so that a top-up can be offered if
emergency caesarean section is needed.
Having an experienced operating team
in-house has the advantage of allowing
intervention to take place within a shorter
period of time.30 Prophylactic antibiotic
usage can help offset infectious risk.12
Skipping the Foley catheter placement
can be done with minimal problems if
care is taken to avoid the bladder.31
Minimizing the transfer time to the
operating theatre is of importance. Hospital design should take into consider-
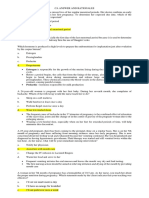
Cardiotocograph Showing Persistent Fetal Bradycardia Leading to Crash Caesarean
Section.
ation a short physical distance of the
operating theatre from the labour ward,
plications.12 Inside their delivery rooms,
epidural analgesia, are good alternatives
or having an operating theatre for cae-
a complete pack of sterile instruments,
to general anaesthesia in emergency
sarean section in the labour ward itself.
necessary anaesthetic equipments, and
caesarean setting, although general an-
Sayegh et al32 conducted a retrospec-
medications are available. However, the
aesthesia still seems to be the method of
tive study reviewing caesarean sections
operation was performed in suboptimal
choice for most anaesthetists in extreme-
performed in a French maternity hospi-
sterile conditions.12
ly urgent settings.36 An audit conducted
tal over a 6-month period. They found a
In the second step to minimize the
at a maternity hospital in Singapore from
mean DDI of 39.5 minutes for emergency
time for anaesthesia induction, it would
February 2003 to January 2004 showed
and urgent caesarean sections. The DDI
be best to have in-house anaesthetic
that the majority of patients (88.8%) had
was mainly inuenced by the time taken to
support. The American Society of Anes-
general anaesthesia for crash caesarean
get the patient into the theatre. The mean
thesiologists and the American College
section, while the rest had successful
decision-to-operating theatre interval ac-
of Obstetricians and Gynecologists sug-
epidural block extension. There was no
counted for 45.6% of the mean DDI in the
gest the availability of a licenced practi-
signicant difference in the DDI or mean
group. The authors highlighted the im-
tioner who is credentialed to administer
cord blood pH with respect to the type of
portance of reducing the decision-to-the-
an appropriate anaesthetic whenever
anaesthesia given. The authors suggest-
atre interval. Tuffnell et al stated that ap-
necessary.
ed that both general anaesthesia and
32
34
proximately 17% of caesarean sections
For the choice of anaesthesia, Dun-
extension of existing epidural block are
had a DDI exceeding 50 minutes, which
phy et al, in their article published in 1991,
acceptable modes of anaesthesia and
could be explained by delays in getting
suggested that regional blockade was
do not delay delivery of the fetus. The au-
the women into the operating room.33 As
associated with longer intervals than did
dit revealed that 100% of deliveries were
previously mentioned, Hillemanns et al
general anaesthesia. However, a more
achieved within the proposed 30-minute
showed that emergency caesarean deliv-
recent review by Dahl et al published in
DDI by implementing a protocol for crash
ery performed in the delivery room result-
2009 suggested that regional anaesthetic
caesarean sections.25
ed in a shortened DDI without detrimental
techniques, such as a single-shot spinal
perioperative maternal or neonatal com-
or a top-up of a well-functioning labour
35
In the third step to reduce the incision-to-delivery
time,
experienced
41
42
CONTINUING MEDICAL EDUCATION
JPOG JAN/FEB 2015
Suggested Measures for Achieving a Safe and Quick Crash Caesarean
Section
A single scalpel can be used for
incision in the skin and rectus sheath
during abdominal wound incision, thus
eliminating the time for changing scal-
Crash caesarean section protocol
Communication protocols
pels to gain entry into the abdomen. A
randomized controlled trial comparing
Good team work
Good collaboration with anaesthetists and staff of the operation
theatre
the use of one versus two scalpels in
Regular crash caesarean section drills
Multiphasic improvement project involving special coding
rate to be signicantly different.37 One
Educational programme for staff
Preparation of patient in labour and before operation
1. Anticipation of the possibility of deterioration in high-risk
cases, with early preparation of patient
2. Early detection of cardiotocographic pathology
3. Consideration of epidural for pain relief in labour
4. In-house support of senior obstetricians, midwives, and
anaesthetists with expertise in dealing with obstetric cases
5. Prophylactic antibiotic usage
6. Skipping Foley catheter placement
Patient transfer to operating theatre
1. Hospital design should take into consideration a short physical
distance of the operating theatre from the labour room
2. Consideration of having an operating theatre for caesarean
section in the labour room itself
patients undergoing elective general
surgery did not nd the wound infection
study showed that scalpels were sterile
after skin incision, supporting the view
that there is no need to discard the skin
scalpel to prevent wound infection.38 The
use of separate surgical knives to incise
the skin and the deeper tissues at caesarean section is not recommended by
the National Institute for Health and Clinical Excellence.5
Once the caesarean section surgery has started, surgeons should refrain from
diverting attention to con-
trol small bleeders or to repair visceral
lacerations. They can return to address
those surgical issues after delivery of
Induction of anaesthesia
1. In-house anaesthetic support
2. Regional anaesthetic techniques (eg, a single-shot spinal or a
top-up of a well-functioning labour epidural analgesia) as good
alternatives to general anaesthesia
the baby.
Incision-to-delivery interval
1. Involvement of experienced surgeons
2. Use of a single scalpel for incision in the skin and rectus sheath
during abdominal wound incision
3. Refraining from diverting attention to control small bleeders
or to repair visceral damage before delivery of the baby
Metzger et al,39 data on the uterine in-
The effect of duration of the interval from uterine incision to delivery
on fetal outcome seems to be unclear.
In a retrospective review by Maayancision-to-delivery interval of 855 cases
revealed that a uterine incision-to-delivery interval of > 2 minutes was associated with more feeding problems and
later hospital discharge compared with
a shorter interval of 2 minutes. Andersen et al40 studied 204 patients un-
surgeons should be assigned to per-
experienced surgeon should be pres-
dergoing caesarean delivery and found
form crash caesarean sections requir-
ent to supervise the performance of the
that, after correction for various factors
ing greater technical skills (eg, in cases
operation. An experienced surgeon is
(including fetal distress, meconium,
suspected to have dense intra-abdom-
expected to use less time for delivery
pre-eclampsia), uterine incision-to-de-
inal adhesions caused by previous
of the baby in these situations. Besides,
livery intervals did not signicantly
caesarean section or laparotomy, or in
the importance of surgical skills training
contribute to Apgar scores or umbilical
morbidly obese patients) or at least an
should be emphasized.
cord blood gases.40
CONTINUING MEDICAL EDUCATION
JPOG JAN/FEB 2015
RISK MANAGEMENT
principle and commitment to good and
cases of fetal distress. Placenta should
Prevention is better than cure. Peri-
evidence-based obstetric practice rath-
be sent for histopathologic investigation.
natal risk management using the con-
er than indulgence in defensive medi-
cept of foreseeability of harm, the
cine.42 However, most emergency cae-
CONCLUSION
harm in this case being fetal distress
sarean deliveries develop during labour
Crash caesarean delivery has always
or poor neonatal outcome, and pre-
in low-risk women and cannot be antici-
been considered as the immediate re-
vention of its development together
pated by prelabour factors.
sort to saving the fetus or mother when
with common sense can help improve
fetal outcome.
DDI is an important and integral
instrumental delivery is not achievable
part of critical conduct interval in acutely
or imminent delivery not expected. It is
The concept of foreseeability of
compromised fetus. Therefore, maternity
indicated in cases with immediate threat
harm, which forms the principle for safe
care units must possess full operational
of fetal death and when an irreversible
obstetric management, was introduced
strength to deliver appropriate care in
cause of fetal distress is identied. To
by Justice Benjamin Cardozo in 1916
acute emergencies. Pierre and Rudigoz43
achieve a swift and safe delivery with
and serves as a road map to obstetrics
suggested that a detailed analysis of ob-
crash caesarean section, numerous
malpractice lawsuits.41 In the case of
stetrical context and of each sequence of
measures could be taken into consider-
MacPherson vs Buick Motor Company,
the DDI is more efcient and realistic for
ation to reduce the time required (1) for
Justice Cardozo wrote that because
evaluation in medical liability cases than
preparation and transfer of the patient to
the operation theatre; (2) for induction of
anaesthesia; and (3) from skin incision
Crash caesarean delivery has always been
considered as the immediate resort to saving
the fetus or mother
to delivery of the baby. It is advisable to
have a crash caesarean protocol, good
team collaboration, and regular drills to
familiarize staff with the workow. Maternity care units must possess the capacity to perform crash caesarean sections
the danger is to be foreseen, there is
an optimal gold standard. In addition, it
within a 30-minute interval. It is prudent
a duty to avoid the injury . . . if [a per-
allows a prophylactic reection for a risk
to have good documentation of every
son] is negligent where a danger is to
management approach in each labour
case that could not reach the 30-min-
be foreseen a liability will follow. In the
ward.
ute target, and risk management should
42
the development
The National Institute for Health
always be considered for every case of
of fetal bradycardia serves as an indica-
and Clinical Excellence emphasized the
fetal distress. The shorter the DDI, the
tion to put the obstetrician on notice of
need to ensure safe birth of the baby in
more desirable it would be to achieve
acute fetal distress. Notice, in this exam-
as good a condition as possible without
this objective. BDI should also be kept
ple, refers to the circumstances in which
causing harm to the woman or her baby
to a minimum. Following the foreseea-
a physician or nurse has sufcient time
through iatrogenic injury or mistakes
bility-of-harm principle and anticipating
to identify the potential for acute fetal
made because of carrying out the proce-
the possibility of deterioration in high-
distress and an ample opportunity to
dure with too much haste.5 The balance
risk cases, together with commitment to
correct or prevent the problem through
between swift and safe delivery should
evidence-based obstetric practice, can
timely intervention. The legal test would
always be kept in mind. When DDI is
help improve fetal outcome in cases of
then be one based on what a reason-
more than 30 minutes, good documen-
fetal distress.
ably prudent obstetrician/nurse would
tation of reasons and fetal condition be-
foresee and would do in light of [that
fore operation may help diminish prob-
information] under the circumstanc-
lems of medicolegal concern. It would be
es.42 Present-day concerns should be
prudent to document arterial and venous
focused on the foreseeability-of-harm
cord blood pH and base excess for all
example by Phelan,
42
About the Authors
Dr Mak is Resident, Dr Kou is Associate Consultant, Ms Ng is
Advanced Practice Nurse, and Dr Leung is Chief of Service, in
the Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Hong Kong.
A list of references can be obtained upon request to the editor.
43
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Premature Rupture of MembranesDocument9 paginiPremature Rupture of MembranesYessica MelianyÎncă nu există evaluări
- Management Placenta PreviaDocument24 paginiManagement Placenta PreviaMuhammad RifaldiÎncă nu există evaluări
- Rle FinalsDocument31 paginiRle FinalsMae Arra Lecobu-anÎncă nu există evaluări
- Nursing SeminarDocument51 paginiNursing SeminarNiceniadas Caraballe100% (1)
- Practice Essentials: Abruptio PlacentaeDocument2 paginiPractice Essentials: Abruptio PlacentaeNurnajwa PahimiÎncă nu există evaluări
- Comprehensive Exam NCM 350Document23 paginiComprehensive Exam NCM 350JustJ ThingsÎncă nu există evaluări
- Ca Answer and RationalesDocument16 paginiCa Answer and RationalesJela Jane ArcalÎncă nu există evaluări
- Abruptio Placentae: (Accidental Hemorrhage, Premature Separation of Placenta)Document25 paginiAbruptio Placentae: (Accidental Hemorrhage, Premature Separation of Placenta)Akashdeep singhÎncă nu există evaluări
- Hypertension in PregnancyDocument34 paginiHypertension in PregnancyROY ALPHYÎncă nu există evaluări
- Third Stage of LabourDocument4 paginiThird Stage of LabourKhazoliyaÎncă nu există evaluări
- Maternal and Child Health Nursing 2 (30 Items)Document11 paginiMaternal and Child Health Nursing 2 (30 Items)hasan ahmdÎncă nu există evaluări
- NCP Drug Study Group 1Document21 paginiNCP Drug Study Group 1Cassandra Grace Muerong Dela CruzÎncă nu există evaluări
- Ob Final ReviewDocument13 paginiOb Final Reviewraquel maniegoÎncă nu există evaluări
- KKPMT IV ICD 10 CAHPTER XV Kehamilan 2020 Ada ICD 9 NyaDocument55 paginiKKPMT IV ICD 10 CAHPTER XV Kehamilan 2020 Ada ICD 9 NyaClarains FriskaÎncă nu există evaluări
- Kode Icd-10 Maternal Dan NeonatalDocument49 paginiKode Icd-10 Maternal Dan NeonatalciptaningtyasÎncă nu există evaluări
- Bleeding Disorders in Pregnancy: Table 1Document7 paginiBleeding Disorders in Pregnancy: Table 1KharismaNisaÎncă nu există evaluări
- NCM 109 Module 3mDocument25 paginiNCM 109 Module 3mKyle ChuaÎncă nu există evaluări
- Fetal DistressDocument3 paginiFetal DistressMaria Donabella OngueÎncă nu există evaluări
- Quiz 1 Maternity NursingDocument230 paginiQuiz 1 Maternity NursingAllaiza CristilleÎncă nu există evaluări
- Nursing DiagnosisDocument16 paginiNursing DiagnosisShemie TutorÎncă nu există evaluări
- Soal-Soal PretesDocument8 paginiSoal-Soal Pretespoker011007Încă nu există evaluări
- School of Health and Allied Health Sciences Nursing Department Self-Directed Learning 5 (Clinical Area)Document3 paginiSchool of Health and Allied Health Sciences Nursing Department Self-Directed Learning 5 (Clinical Area)Margarette BaynosaÎncă nu există evaluări
- Intensive V (Complications)Document117 paginiIntensive V (Complications)darren55Încă nu există evaluări
- Pregnancy Induced Hypertension - Nursing Diagnosis (NANDA)Document12 paginiPregnancy Induced Hypertension - Nursing Diagnosis (NANDA)api-370148988% (43)
- Ceasarean Section LectureDocument40 paginiCeasarean Section LectureamvyellicamaricorcoÎncă nu există evaluări
- Effect of Vitamin D o Placenta AccretaDocument4 paginiEffect of Vitamin D o Placenta AccretaYoga ParipurnaÎncă nu există evaluări
- CoC ExamDocument29 paginiCoC Examanteneh67% (3)
- Care of Mother and Child (Well-Client)Document67 paginiCare of Mother and Child (Well-Client)Jake Padua100% (2)
- Contraction Ring, Uterine Rupture, Precipitate LaborDocument4 paginiContraction Ring, Uterine Rupture, Precipitate LaborJessica Carmela CasugaÎncă nu există evaluări
- Case3 Case StudyDocument6 paginiCase3 Case StudyKrizzia Angela BacotocÎncă nu există evaluări