Documente Academic
Documente Profesional
Documente Cultură
Antiphospholipid Syndrome in Pregnancy: Review of Diagnosis and Treatment
Încărcat de
Dara Dasawulansari SyamsuriDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Antiphospholipid Syndrome in Pregnancy: Review of Diagnosis and Treatment
Încărcat de
Dara Dasawulansari SyamsuriDrepturi de autor:
Formate disponibile
Antiphospholipid syndrome in pregnancy
Howard J. A. Carp
Purpose of review
Antiphospholipid syndrome is widely recognized as a risk factor
for numerous obstetric complications including miscarriage,
intrauterine growth restriction, preeclampsia, fetal death and
preterm labour. The many recent changes in concept regarding
this syndrome, the role of the relevant antibodies, mechanism of
action, diagnosis and treatment are assessed in this review.
Recent findings
In recent years, our understanding of antiphospholipid
syndrome has grown. The antigen has become better defined
and is now thought to be b2 glycoprotein 1. The classical
antibodies, lupus anticoagulant and anticardiolipin antibody are
known to be pathogenic even when passively transferred to
animal hosts. It seems, however, that the pathogenic antibodies
are those directed towards b2 glycoprotein 1, and that those
which are directed to phospholipids without binding to b2
glycoprotein 1 may not be pathogenic, but merely
epiphenomena. The treatment of this condition has also been
changed due to the influence of randomized trials in which
heparin or low molecular weight heparin has replaced the use of
steroids.
Summary
There are numerous pitfalls in managing this condition. As b2
glycoprotein 1 antibodies are not usually tested, the condition
may be over diagnosed or misdiagnosed. Similarly, the results
of treatment are not usually corrected for confounding factors
such as fetal chromosomal aberrations. In the absence of other
confounding factors low molecular weight heparins are
probably the treatment of choice.
Keywords
antiphospholipid syndrome, antiphospholipid antibodies, b2
glycoprotein 1 antibodies, recurrent pregnancy loss, recurrent
miscarriage, heparin, low molecular weight heparins, aspirin,
intravenous immunoglobulin
Curr Opin Obstet Gynecol 16:129135.
2004 Lippincott Williams & Wilkins.
Department of Obstetrics and Gynecology, Sheba Medical Center, Tel Hashomer,
University of Tel Aviv, Israel
Correspondence to Prof. H.J.A. Carp MB BS FRCOG, Department of Obstetrics and
Gynecology, Sheba Medical Center, Tel Hashomer 52621, Israel
Tel: +972 9 9557075; fax: +972 9 9574779; e-mail: carp@netvision.net.il
Current Opinion in Obstetrics and Gynecology 2004, 16:129135
Abbreviations
aPL
APS
b2GP1
ELISA
IVIG
antiphospholipid antibody
antiphospholipid syndrome
b2-glycoprotein 1
enzyme-linked immunosorbent assay
intravenous immunoglobulin
2004 Lippincott Williams & Wilkins
1040-872X
DOI: 10.1097/01.gco.0000124163.64477.a3
Introduction
The most acceptable diagnostic criteria for the antiphospholipid syndrome (APS) are the Sapporo criteria
[1]. These criteria dene the clinical features of
pregnancy loss as either one unexplained fetal death of
a morphologically normal fetus over 10 weeks of
pregnancy, or three or more otherwise unexplained
consecutive abortions prior to 10 weeks. The laboratory
features have been modied and now require a positive
test for lupus anticoagulant, or a medium or high-titre
anticardiolipin IgG or IgM test on at least two occasions,
at least 6 weeks apart, before a positive diagnosis can be
made.
Most of the clinical features are related to thrombosis,
both venous and arterial. The presenting symptom
leading to gynaecological consultation is usually fetal
loss, typically fetal death in the second or third trimesters
[2,3], often after growth retardation. Antiphospholipid
antibodies (aPLs), however, have been implicated in
other forms of pregnancy loss including rst-trimester
miscarriage [4]. Hence the current trend is for gynaecologists to seek these antibodies in any case of unexplained pregnancy loss. The syndrome can be dened as
primary when no other autoimmune disease is present
and secondary in patients with other autoimmune
diseases.
Beyond these guidelines are many controversies as the
syndrome is still not fully dened. This review will
discuss some of the pitfalls which may be encountered in
interpreting this syndrome as well as the clinical features
of the condition.
Laboratory diagnosis
As well as the two main antibody assays, lupus
anticoagulant and anticardiolipin, other aPLs have been
reported to be associated with APS, but their association
remains to be conrmed. Phosphatidylinositol, phosphatidylserine and phosphatidylethanolamine are three
such examples. Recently, b2 glycoprotein 1 (b2GP1)
has been recognized as the cofactor required for lupus
anti-coagulant and anticardiolipin to act. Although antib2GP1 antibodies have high specicity for APS (98%),
their assessment cannot be relied upon in normal clinical
practice as the sensitivity of testing is low (4050%)
[5,6 . .].
There is frequent concordance between lupus anticoagulant and anticardiolipin [7] and anti-b2GP1
antibodies [8]. These antibodies, however, are not
129
130 Maternalfetal medicine
identical. Lupus anticoagulant may react with phospholipids other than cardiolipin or proteins other than
b2GP1, whereas some anticardiolipin and b2GP1 antibodies have no lupus anticoagulant activity.
Lupus anticoagulant was rst described by Colney and
Hartman in 1952 in certain patients with systemic
lupus erythematosus. Lupus anticoagulant seems to be
the most specic test for APS [9]. Its diagnosis in vitro
depends on prolongation of the phospholipid-dependent coagulation tests such as prothrombin time,
recalcication time and the kaolin clotting time. The
activated partial thromboplastin test is the most widely
used diagnostic test, as it is the most readily available.
The dilute Russells viper Venom test seems to be
more sensitive than the previously used kaolin clotting
time [10], and has tended to replace it. It is interesting
that lupus anticoagulant can have seemingly opposing
actions in vitro and in vivo. Prolongation of the
coagulation tests is due to the inhibitory action of
the antibody on the phospholipid reagent, which is
added to tested blood in the laboratory (e.g. thromboplastin in the activated partial thromboplastin test).
Those reagents in vitro take the place of the
thrombocyte membrane and tissue thromboplastin that
accumulate at injured tissues sites in vivo. Thromboplastin is a clotting factor and induces thrombocyte
aggregation.
It was Harris et al. [11] who rst suggested that the
antibody could be examined directly and not indirectly
by its effect on clotting. He introduced a test using the
enzyme-linked immunosorbent assay (ELISA), using
chemically pure cardiolipin as the antigen. This
antibody is therefore known as anticardiolipin antibody.
The test is relatively easy to perform and most
laboratories are able to obtain the standard sera. The
ELISA assay, however, has a number of drawbacks.
The test is not specic when results are low positive.
In general, the higher the anticardiolipin level, the
greater the likelihood of APS [12]. There have been
numerous efforts at standardization, including the
introduction of standard calibrators derived from
monoclonal anticardiolipin antibodies. Anticardiolipin
ELISA is the most frequently performed test in
patients with suspected APS in Europe [13]. In a
survey of 24 centres, however, Tincani et al. [13] found
that when 10 serum samples were evaluated independently by the 24 centres in their study, there was
difculty in getting comparable results. Hence, skill
and experience are necessary in interpreting the
results, and additional features are necessary, such as
repeat positive values 6 weeks apart, a high level of
antibody (above 40 GPL units), concurrent thromboses
and additional antibodies such as lupus anticoagulant
before the diagnosis of APS is made.
Mechanisms of action
Antiphospholipid antibodies have been shown to cause
pregnancy loss directly. Injection of serum from mice
with a high titre of aPL to naive mice induces resorbtion
of pregnancies in the recipient [14], and active immunization with human pathogenic monoclonal anticardiolipin antibody induced the clinical manifestations
of antiphospholipid syndrome in BALB/c mice [15]. It
has been shown that the serum from women with APS is
highly teratogenic to rat embryos in culture and also
affects embryonic growth [16]. Moreover, purication of
the IgG faction of the sera of women with APS directly
affected the embryo and yolk sac, reducing their growth
[17 .].
It has long been known that aPLs require a cofactor
(apolipoprotein H or b2GP1). Today this cofactor is
thought to be the antigen to which aPLs bind. Binding
of aPLs to the b2GP1 forms divalent IgGb2GP1
complexes that have increased afnity for membrane
phospholipid [6 . .]. The physiological function of b2GP1
has not been elucidated, and b2GP1 deciency does not
appear to be associated with disease. Homozygous
b2GP1 null mice also appear anatomically and histologically normal [18]. The binding of aPLb2GP1 to cell
membranes including trophoblast results in injury or
activation. Activation may be cytokine mediated, as IL3, a cytokine which is involved in implantation, has been
reported to be decreased in APS [19]. Administration of
IL-3 prevented fetal loss in experimental APS [20], and
the balance of Th-1/Th-2 cytokines may be altered in
APS [21]. Additionally, tumour necrosis factor-a levels
were found to be signicantly higher in patients with
APS than healthy controls [22].
aPLs are thought to have their actions by one or more of
three main mechanisms: thrombosis, interference with
the prostacycline thromboxane balance, and affecting the
adhesion molecules between trophoblastic elements.
Cellular activation increases the expression of cell
adhesion molecules [23,24], which may promote leukocyte adhesion to the endothelial surface. aPLs have
thrombogenic effects that are mediated by intercellular
cell adhesion molecule-1, vascular cell adhesion molecule-1, and P-selectin [25]. aPLs may disrupt the
annexin-V shield around cells and trophoblasts. Annexin-V is a phospholipid-binding protein with potent
anticoagulant properties [26]. IgG fractions from APS
patients reduce annexin-V on cultured human trophoblasts and endothelial cells [6 . .]. aPL-mediated reduction of annexin-V requires b2GP1 [27]. aPLs with
reactivity against annexin-V induce apoptosis in endothelial cells [28]. Some of these apoptotic (microparticles) have been shown to be stimulated by lupus
anticoagulant [29].
Antiphospholipid syndrome in pregnancy Carp 131
aPLs may also interfere with the protein C antithrombotic pathway. aPLs decrease protein C activation by
thrombomodulin, inhibit activated protein C activity,
and bind to factors Va and VIIIa preventing their lysis by
activated protein C [30].
aPLs have been reported to inhibit arachidonic acid
release [31]. Arachidonic acid release is an essential
prerequisite for prostacycline production. Prostacycline is
a potent physiologic inhibitor of thrombocyte aggregation, and a potent vasodilatator. aPLs have been shown
to increase the concentration of thromboxane, thus
altering the thromboxane/prostacycline balance [32].
Additionally, in a mouse model of experimental APS,
Shoenfeld and Blank [33] infused anticardiolipin to
pregnant mice in order to induce APS. Mice that were
cotreated with a thromboxane receptor antagonist had a
signicant reduction in fetal resorption rate from 45 to
19.8% and an increase in mean placental and embryo
weights. There was also an increased platelet count
(from 597 100 to 1 075 000 platelets/mm3) in treated
mice, indicating the effect of thrombocyte aggregation in
APS.
aPLs, however, may also affect the adhesion molecules
between the elements of syncytiotrophoblast. Cytotrophoblast cells express phospholipids on their surface,
and aPLs may damage the trophoblast unrelated to
thrombosis. This concept is supported by histological
evidence from patients with aPLs and fetal death.
Women with aPLs have decreased vasculosyncitial
membranes, increased synctial knots, substantially more
brosis, hypovascular villi and infarcts than women
without APS [34]. The changes in syncitial membranes
may be secondary to thrombosis, but thrombosis could
also be secondary to placental damage which allows free
transplacental passage of maternal aPLs.
Infection may be one of the mechanisms giving rise to
APS. In certain mouse models, immunization with
Haemophilus inuenzae, Neisseria gonorrhoeae, or tetanus
toxoid resulted in the development of antibodies against
b2GP1 [35 . .]. Infusion of these antibodies into pregnant
mice resulted in APS, including thrombocytopenia,
prolonged activated partial thromboplastin time, and
increased fetal loss. In humans, infection with varicella
has been associated with APS [36]. Although HIV,
hepatitis A, hepatitis B, and hepatitis C are also
associated with an increased prevalence of anticardiolipin antibodies, most of these are not b2GP1 dependent
[37]. The difference between APS and the mere
presence of aPLs may be due to diseases such as
syphilis and Lyme disease, raising antibodies which
recognize phospholipids directly, whereas in APS the
infections raise antibodies which recognize epitopes on
phospholipid-binding proteins such as b2GP1.
Prevalence
The prevalence of APS varies according to the population assessed, and how strict are the criteria used to
assess the antibodies. aPLs have been found in women
with normal pregnancies, but the prevalence is low.
Lupus anticoagulant has been found in 0.2% of women
with normal pregnancies, and anticardiolipin antibodies
in 2% of women [3,38,39]. The author has found a 5%
prevalence of lupus anticoagulant in a group of 360
patients with recurrent miscarriage [40]. In a slightly
larger series of 500 women with recurrent miscarriage,
however, Rai et al. [41] reported a 15% prevalence of
aPLs with b2GP1. Vinatier et al. [42] have reviewed 16
publications on the prevalence of aPLs in recurrent
miscarriage. The prevalence of anticardiolipin antibodies
varied between 4.6 and 50.7% with a mean of 15.5%.
The prevalence of lupus anticoagulant varied between 0
and 14% with a mean incidence of 8.3%. In women with
mid-trimester losses, however, the prevalence has been
reported to be as high as 30% [43].
Clinical features
The features of APS are numerous and range from the
most mild to the most severe. The clinical features can
affect pregnancy only or there may be other associated
autoimmune phenomena. Most of the systemic features
of the syndrome can be explained by vasculopathy and
occlusion of small vessels due to platelet aggregation and
subsequent thrombosis. There may be a history of deep
venous thromboses, arterial thrombosis, pulmonary
embolus, transient ischaemic attacks, stroke, renal
infarcts, and so on. These may lead to subsequent
hypertension, proteinuria and renal failure, amongst
other conditions. Dementia can occur after multiple
cerebral infarcts. There may also be associated Reynauds phenomenon, livido reticularis, pulmonary hypertension, amaurosis fugax, transient ischemic attacks,
hemiplegia, hemiesthesia and Singer neurosis.
Systemic lupus erythematosus is not a prerequisite for
APS, but is often present. Rarely a catastrophic
syndrome may occur with abrupt widespread vascular
occlusion [44].
In pregnancy, aPLs have been implicated to be the
cause of pregnancy loss at all stages of pregnancy,
placental dysfunction in the third trimester, intrauterine
growth restriction and preeclampsia. Each of these may
or may not be associated with thrombocytopenia. The
placenta is small, and usually has a vasculopathy.
APS has also been reported to cause preclinical
pregnancy loss, presenting as infertility. Although Lyden
et al.s [45] classical work on the effects of aPLs on the
development of trophoblasts supports the concept of
an association between aPLs and infertility, most
132 Maternalfetal medicine
authorities have failed to nd an association with
infertility [46].
Most pregnancy losses in APS are in the later stages of
pregnancy. Rai et al. [47] found that fetal heart activity
was present in 86% of recurrently miscarrying women
with APS, but in only 43% of recurrently miscarrying
women without APS; in the others no fetal heart activity
was detected. The author [48] has only found fetal heart
activity in 11% of unexplained recurrent pregnancy loss.
Hence the syndrome seems to be associated with missed
abortions in which a fetal heart was previously detected.
Lockshin [3] has reported that typically pregnancies start
normally, and a fetal heart is detected early in the rst
trimester. Intrauterine growth restriction or second or
third trimester fetal death ensues. The author [49] has
found an increased prevalence of second trimester
miscarriages in APS compared with women with
unexplained recurrent pregnancy losses. Oshiro et al.
[50] have also reported that women with APS tend to
lose their pregnancies a mean of 4 weeks later than
controls. More recently, a study of 366 women with two
or more pregnancy losses [51] showed that in women
with anticardiolipin at medium to high titres and lupus
anticoagulant, 50% of losses were fetal deaths, in contrast
to 10% in women who were anticardiolipin-negative.
Tests of fetal well-being may show signs of fetal
compromise.
There is disagreement as to the incidence of pregnancy
loss in the presence of aPLs. In patients with APS, Rai
et al. [47] have reported the incidence of pregnancy loss
to be as high as 90%. However, Rai et al.s [47] series
was a small series with only 20 patients. There are now
three papers which have compared the use of aspirin
with placebo [5254]. The three papers have been
combined in a metaanalysis [55 . .]. Fifty-two of 61
pregnancies developed normally in the placebo group.
It must be borne in mind, however, that the four trials
may have used different criteria for the laboratory
diagnosis of aPLs. No trial used the strict Sapporo
criteria. None of the above trials assessed b2GP1.
Hence it is difcult to draw any conclusions about the
incidence of pregnancy loss in the presence of aPLs or
APS without treatment.
Treatment
Various regimens of treatment have been used, either
alone or in combinations, for example, aspirin, steroids,
anticoagulants such as unfractionated heparin, and, more
recently, low molecular weight heparins and immunoglobulin. In early trials, treatment was administered for
the presence of anticardiolipin and lupus anticoagulant
alone. Even if the strict Sapporo criteria are used, no
trial of treatment has assessed anti-b2GP1 antibodies.
Additionally, no trial has corrected for fetal causes of
pregnancy loss which may confound the results. The
fetal causes may include structural malformations which
are incompatible with life, and chromosomal aberrations.
In missed abortion, Philipp and Kalousek [56] have
performed 19 embryoscopies on missed abortions. Ten
were morphologically abnormal; only some of these
morphological abnormalities could be explained by
chromosomal aberrations. In sporadic miscarriage, 50
60% of embryos lost will be lost due to karyotypic
aberrations in the embryo. In recurrent miscarriage,
between 29 and 57% of abortuses will be lost due to
chromosomal rearrangements [5759]. In recurrent miscarriage with APS, 2040% of abortuses are also
chromosomally abnormal [5860]. The results of treatment should be interpreted against this background of
uncertainty.
Steroids are used infrequently today due to uncertainty
as to efcacy and the side effects (Cushings syndrome,
acne, osteoporosis, etc.). There have been two randomized controlled trials assessing the effects of steroid
therapy for APS in pregnancy. Cowchock et al. [61]
compared prednisone and aspirin with heparin and
aspirin in a randomized trial of 20 women. The live
birth rate was identical (75%) in both groups. Silver et al.
[62] compared the effect of aspirin with that of aspirin
with the addition of prednisone. The live birth rate was
100% in both groups. In both studies prednisone was
associated with a higher incidence of premature and
growth retarded infants. Neither of these trials corrected
for b2GP1 antibodies, however, nor confounding factors
such as chromosomal aberrations in the aborted fetuses.
There is still a place for steroids in the presence of
vasculitis.
The most commonly used form of treatment today is
heparin together with low-dose aspirin [63 . .]. Three
trials have compared aspirin alone with aspirin with the
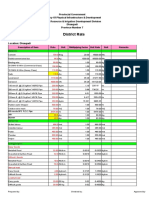
addition of heparin. Both Kutteh et al. [64] and Rai et al.
[65] reported that the live birth rate increased by 36 and
29%, respectively, when heparin was added to the
regimen (Fig. 1). Farquharson et al. [66], in contrast to
previous studies, found the live birth rate to be similar in
both groups (72% with aspirin alone compared with 78%
when heparin was added to the regimen). When the
three trials are combined in a metaanalysis (Fig. 1) there
was a common odds ratio of 2.63 in favour of heparin
(95% CI 1.464.75). As with steroids and also aspirin, the
explanation for the discordant results between Farquarson et al.s trial and the other trials may be due to failure
to correct for b2GP1 antibodies and the loss of
chromosomally abnormal embryos in the subsequent
pregnancy. Additionally, Kutteh et al. [64] used unfractionated heparin, whereas Rai et al. [65] used the low
molecular weight heparin enoxaparin, and Farquharson
et al. [66] used the low molecular weight heparin
Antiphospholipid syndrome in pregnancy Carp 133
Figure 1. Metaanalysis on the beneficial effects on pregnancy of low molecular weight heparin
Kutteh et al. [64]
Rai et al. [65]
Farquharson et al . [66]
Overall RR
0.1
daltaparin. The different types of heparin used may also
explain the discordant results.
Low molecular weight heparins have a number of
advantages over unfractionated heparin: they are more
bioavailable and have a longer half life. Hence only one
injection is required per day, as opposed to two to three
injections of unfractionated heparin for the same effect.
Heparin-induced thrombocytopenia also seems to be less
frequent. The main advantage, however, is that there is
no overlap between the anticoagulant effect and the
antithrombotic effect. There is no bleeding with low
molecular weight heparins; even Caesarean sections can
be safely performed, and there is little need for
monitoring. However, heparin, while increasing the live
birth rate, seems to have little effect on the obstetric
complications such as preeclampsia, intrauterine growth
restriction and preterm labour.
There have recently been three descriptive studies
and two comparative trials of intravenous immunoglobulin (IVIG) in APS. The three descriptive studies
[6769], which used IVIG in addition to other forms
of treatment, reported a subsequent 8090% live birth
rate. The two comparative trials, however, do not
show IVIG to be benecial in terms of live births
compared with prednisone and aspirin [70] or heparin
and aspirin [71]. Although IVIG offers little advantage
in terms of live births, a different picture emerges
when the late complications are considered. Harris
and Pierangeli [72] reviewed the literature and
reported that preeclampsia, intrauterine growth restriction, and premature births were reduced after IVIG
compared with prednisone and aspirin, or heparin and
10
aspirin. Valensie et al. [73] reported on 14 patients
who received IVIG for APS. Only one had preeclampsia with placental abruption; all the other 13
had no maternal or fetal complications. The best
evidence that IVIG lessens the prevalence of late
complications comes from the two comparative trials
mentioned above. In Vaquero et al.s [70] trial the
prevalence of pregnancy-induced hypertension and
gestational diabetes was signicantly lower (P 50.05)
in patients who received IVIG than those receiving
prednisone and aspirin (5% of 41 patients as opposed
to 14% of 22 patients) for each condition. Branch et
al. [71] reported that there were fewer cases of fetal
growth restriction in the IVIG group when compared
with the heparin and aspirin group (14% of seven
patients compared with 33% of nine patients, respectively). There were also fewer admissions to the
neonatal intensive care unit (14% of seven patients in
the IVIG group compared with 44% of nine in the
heparin and aspirin group). IVIG is the only
intervention to lower anticardiolipin levels rather than
to inhibit the actions of aPLs. In Spinnato et al.s [67]
series, three of the four patients with live births had a
concomitant decrease in anticardiolipin IgM levels. In
Kwak et al.s [74] series, aPL titres of both IgG and
IgM were signicantly decreased after each IVIG
infusion. Three pregnancies of six were complicated
by intrauterine growth restriction the development
of which correlated to rising antibody titres.
The prohibitive cost of IVIG probably prevents this
treatment ever becoming a rst-line treatment in APS.
However, it probably has a place as second-line
treatment in patients who are refractory to heparin or
134 Maternalfetal medicine
who continue to suffer the late obstetric complications of
APS.
Conclusion
There are numerous pitfalls in the diagnosis and
treatment of APS, some of which have been mentioned
above.
(1) Patients must be properly dened. Some reports in
the literature summarize patients with only two
pregnancy losses. In these patients there is an 80%
chance that the next pregnancy will result in a live
birth. In any trial which includes patients with two
pregnancy losses, the 80% live birth rate in the
control group will obscure any benecial effect in the
patient with a poor prognosis.
(2) Confounding factors such as fetal chromosomal
aberrations must be included in future trials if the
results of therapy are to be meaningful.
(3) The fact that there is no denite correlation between
antibody levels and fetal death is a problem. Where a
denitive test is available, it would permit withholding unnecessary treatment. It would also enable
modication of treatment as the situation demands
during pregnancy. Hopefully, the test for b2GP1 will
become more specic and may full this role.
References and recommended reading
Papers of particular interest, published within the annual period of review, have
been highlighted as:
.
of special interest
..
of outstanding interest
12 Harris EN, Pierangeli SS. Revisiting the anticardiolipin test and its
standardization. Lupus 2002; 11:269275.
13 Tincani A, Allegri F, Sanmarco M, et al. Anticardiolipin antibody assay: a
methodological analysis for a better consensus in routine determinations. A
cooperative project of the European Antiphospholipid Forum. Thromb
Haemost 2001; 86:575583.
14 Blank M, Cohen J, Toder V, Shoenfeld Y. Induction of anti-phospholipid
syndrome in naive mice with mouse lupus monoclonal and human polyclonal
anti-cardiolipin antibodies. Proc Natl Acad Sci U S A 1991; 88:30693073.
15 Bakimer R, Fishman P, Blank M, et al. Induction of primary antiphospholipid
syndrome in mice by immunization with a human monoclonal anticardiolipin
antibody (H-3). J Clin Invest 1992; 89:15581563.
16 Ornoy A, Yacobi S, Avraham S, et al. The effect of sera from women with
SLE and/or anti phospholipid syndrome on rat embryos in culture. Reprod
Toxicol 1998; 12:185191.
17 Ornoy A, Yacobi S, Tartakover Matalon S, et al. The effects of antiphospholipid antibodies obtained from women with SLE APS and associated
pregnancy loss on rat embryos and placental explants in culture. Lupus 2003;
12:573578.
First paper to show that aPL has embryotoxic effects in addition to thrombotic
effects.
18 Sheng Y, Reddel SW, Herzog H, et al. Impaired thrombin generation in beta
2-glycoprotein I null mice. J Biol Chem 2001; 276:1381713821.
19 Shoenfeld Y, Sherer Y, Fishman P. Interleukin-3 and pregnancy loss in
antiphospholipid syndrome. Scand J Rheumatol Suppl 1998; 107:1922.
20 Fishman P, Falach-Vaknine E, Zigelman R, et al. Prevention of fetal loss in
experimental antiphospholipid syndrome by in vivo administration of
recombinant interleukin-3. J Clin Invest 1993; 91:18341837.
21 Krause I, Blank M, Levi Y, et al. Anti-idiotype immunomodulation of
experimental anti-phospholipid syndrome via effect on Th1/Th2 expression.
Clin Exp Immunol 1999; 117:190197.
22 Bertolaccini ML, Atsumi T, Lanchbury JS, et al. Plasma tumor necrosis factor
alpha levels and the 238A promoter polymorphism in patients with antiphospholipid syndrome. Thromb Haemost 2001; 85:198203.
23 Simantov R, LaSala JM, Lo SK, et al. Activation of cultured vascular
endothelial cells by antiphospholipid antibodies. J Clin Invest 1995; 96:2211
2219.
24 Meroni PL, Raschi E, Camera M, et al. Endothelial activation by aPL: a
potential pathogenetic mechanism for the clinical manifestations of the
syndrome. J Autoimmun 2000; 15:237240.
25 Pierangeli SS, Espinola RG, Liu X, et al. Thrombogenic effects of
antiphospholipid antibodies are mediated by intercellular cell adhesion
molecule-1, vascular cell adhesion molecule-1, and Pselectin. Circ Res
2001; 88:245250.
Wilson WA, Gharavi AE, Koike T, et al. International consensus statement on
preliminary classification for definite antiphospholipid syndrome. Arthritis
Rheum 1999; 42:13091311.
Ruiz-Irastorza G, Khamashta MA, Hughes GRV. Treatment of pregnancy loss
in Hughes syndrome: a critical update. Autoimmun Rev 2002; 1:298304.
Lockshin MD. Antiphospholipid antibody syndrome. JAMA 1992; 268:1451
1453.
Stone S, Khamashta MA, Poston L. Placentation, antiphospholipid syndrome
and pregnancy outcome. Lupus 2001; 10:6774.
Sanmarco M, Soler C, Christides C, et al. Prevalence and clinical
significance of IgG isotype anti-beta 2-glycoprotein I antibodies in antiphospholipid syndrome: a comparative study with anticardiolipin antibodies.
J Lab Clin Med 1997; 129:499506.
Rand JH. The antiphospholipid syndrome. Annu Rev Med 2003; 54:409424.
A review paper which explains the mechanisms of action of aPLs.
29 Combes V, Simon AC, Grau GE, et al. In vitro generation of endothelial
microparticles and possible prothrombotic activity in patients with lupus
anticoagulant. J Clin Invest 1999; 104:93102.
Galli M, Comfurius P, Barbui T, et al. Anticoagulant activity of b2-glycoprotein
I is potentiated by a distinct subgroup of anticardiolipin antibodies. Thromb
Haemost 1992; 68:297300.
30 de-Groot PG, Horbach DA, Derksen RH. Protein C and other cofactors
involved in the binding of antiphospholipid antibodies: relation to the
pathogenesis of thrombosis. Lupus 1996; 5:488493.
Viard JP, Amoura Z, Bach J-F. Association of anti-b2 glycoprotein I
antibodies with lupus-type circulating anticoagulant and thrombosis in
systemic lupus erythematosus. Am J Med 1992; 93:181186.
31 Carreras LO, Vermylen JG. Lupus anticoagulant and thrombosis: possible
role of inhibition of prostacyclin formation. Thromb Haemost 1982; 48:3840.
Carreras LO, Forastiero RR, Martinuzzo ME. Which are the best biological
markers of the antiphospholipid syndrome? J Autoimmun 2000; 15:163172.
32 Robbins DL, Leung S, Miller-Blair DJ, et al. Effect of anticardiolipin/beta2glycoprotein I complexes on production of thromboxane A2 by platelets from
patients with the antiphospholipid syndrome. J Rheumatol 1998; 25:5156.
10 Pengo V, Biasiolo A, Rampazzo P, Brocco T. dRVVT is more sensitive than
KCT or TTI for detecting lupus anticoagulant activity of anti-beta2glycoprotein I autoantibodies. Thromb Haemost 1999; 81:256258.
33 Shoenfeld Y, Blank M. Effect of long-acting thromboxane receptor antagonist
(BMS 180,291) on experimental antiphospholipid syndrome. Lupus 1994;
3:397400.
11 Harris EN, Gharavi AE, Boey ML. Anti-cardiolipin antibodies: detection by
radioimmunassay and association with thrombosis in systemic lupus
erythematosus. Lancet 1983; 2:12111214.
34 Out HJ, Kooijman CD, Bruinse HW, et al. Histo-pathological findings from
patients with intrauterine fetal death and antiphospholipid antibodies. Eur J
Obstet Gynecol 1991; 41:179186.
..
26 Voges D, Berendes R, Burger A, et al. Three-dimensional structure of
membrane-bound annexin V: a correlative electron microscopy-X-ray crystallography study. J Mol Biol 1994; 238:199213.
27 Rand JH, Wu XX, Andree HAM, et al. Antiphospholipid antibodies accelerate
plasma coagulation by inhibiting annexin-V binding to phospholipids: a lupus
procoagulant phenomenon. Blood 1998; 92:16521660.
28 Nakamura N, BanT, Yamaji K, et al. Localization of the apoptosis-inducing
activity of lupus anticoagulant in an annexin V-binding antibody subset. J Clin
Invest 1998; 101:19511959.
Antiphospholipid syndrome in pregnancy Carp 135
35 Blank M, Krause I, Fridkin M, et al. Bacterial induction of autoantibodies to
beta2-glycoprotein-I accounts for the infectious etiology of antiphospholipid
syndrome. J Clin Invest 2002; 109:797804.
The first paper to show that APS may have an infectious cause.
..
36 Manco Johnson MJ, Nuss R, Key N, et al. Lupus anticoagulant and protein S
deficiency in children with postvaricella purpura fulminans or thrombosis. J
Pediatr 1996; 128:319323.
37 Guglielmone H, Vitozzi S, Elbarcha O, et al. Cofactor dependence and
isotype distribution of anticardiolipin antibodies in viral infections. Ann Rheum
Dis 2001; 60:500504.
38 Lockwood CJ, Romero R, Feinberg RF, et al. The prevalence and biologic
significance of lupus anticoagulant and anticardiolipin antibodies in a general
obstetric population. Am J Obstet Gynecol 1989; 161:369373.
39 Harris EN, Spinnato JA. Should anticardiolipin tests be performed in
otherwise healthy pregnant women? Am J Obstet Gynecol 1991;
165:12721277.
40 Carp HJA, Toder V, Mashiach S, et al. Recurrent miscarriage: a review of
current concepts, immune mechanisms and results of treatment. Obstet
Gynecol Surv 1990; 45:657669.
41 Rai RS, Regan L, Clifford K, et al. Antiphospholipid antibodies and beta 2glycoprotein-I in 500 women with recurrent miscarriage: results of a
comprehensive screening approach. Hum Reprod 1995; 10:20012005.
42 Vinatier D, Dufour P, Cosson M, et al. Antiphospholipid syndrome and
recurrent miscarriages. Eur J Obst Gynecol Reprod Biol 2001; 96:3750.
43 Drakeley AJ, Quenby S, Farquharson RG. Mid-trimester loss-appraisal of a
screening protocol. Hum Reprod 1998; 13:19751980.
56 Philipp T, Kalousek DK. Transcervical embryoscopy in missed abortion. J
Assist Reprod Genet 2001; 18:285290.
57 Stern JJ, Dorfman AD, Gutierez-Najar MD. Frequency of abnormal karyotype
among abortuses from women with and without a history of recurrent
spontaneous abortion. Fertil Steril 1996; 65:250253.
58 Ogasawara M, Aoki K, Okada S, et al. Embryonic karyotype of abortuses in
relation to the number of previous miscarriages. Fertil Steril 2000; 73:300
304.
59 Carp HJA, Toder V, Orgad S, et al. Karyotype of the abortus in recurrent
miscarriage. Fertil Steril 2001; 5:678682.
60 Takakuwa K, Asano K, Arakawa M, et al. Chromosome analysis of aborted
conceptuses of recurrent aborters positive for anticardiolipin antibody. Fertil
Steril 1997; 68:5458.
61 Cowchock FS, Reece EA, Balaban D, et al. Repeated fetal losses associated
with antiphospholipid antibodies: a collaborative randomised trial comparing
prednisone with low-dose heparin. Am J Obstet Gynecol 1992; 166:1318
1323.
62 Silver RK, MacGregor SN, Sholl JS, et al. Comparative trial of prednisone
plus aspirin vs. aspirin alone in the treatment of anticardiolipin antibodypositive obstetric patients. Am J Obstet Gynecol 1993; 169:14111417.
63 Tincani A, Branch DW, Levy RA, et al. Treatment of pregnant patients with
antiphospholipid syndrome. Lupus 2003; 12:524529.
A paper which describes current prescribing practice in APS after questioning 16
leading centres.
..
44 Asherson RA, Cervera R, Piette JC, et al. Catastrophic antiphospholipid
syndrome: clues to the pathogenesis from a series of 80 patients. Medicine
2001; 80:123.
64 Kutteh WH. Antiphospholipid antibody-associated recurrent pregnancy loss:
treatment with heparin and low-dose aspirin is superior to low-dose aspirin
alone. Am J Obstet Gynecol 1996; 174:15841589.
45 Lyden T, Vogt E, Ng AK, et al. Monoclonal antiphospholipid antibody
reactivity against human placental trophoblast. J Reprod Immunol 1992;
22:114.
65 Rai R, Cohen H, Dave M, et al. Randomised controlled trial of aspirin and
aspirin plus heparin in pregnant women with recurrent miscarriage associated
with phospholipid antibodies (or antiphospholipid antibodies). BMJ 1997;
314:253257.
46 Backos M, Rai R, Regan L. Antiphospholipid antibodies and infertility. Hum
Fertil 2002; 5:3034.
47 Rai RS, Clifford K, Cohen H, et al. High prospective fetal loss rate in
untreated pregnancies of women with recurrent miscarriage and antiphospholipid antibodies. Hum Reprod 1995; 10:33013304.
48 Carp HJA, Toder V, Mashiach S, et al. Early pregnancy loss: current
concepts of research and treatment. Obstet Gynecol Surv 1990; 45:657
669.
49 Carp HJA, Cohen S, Dulitzki M. Antiphospholipid antibody syndrome and
pregnancy. In: Dasgupta S, editor. Recent advances in obstetrics and
gynaecology. New Delhi: Jaypee Ltd; 1997. Chapter 3, pp 5473.
50 Oshiro BT, Silver RM, Scott JR, et al. Antiphospholipid antibodies and fetal
death. Obstet Gynecol 1996; 87:489493.
51 Loizou S, Byron MA, Englert HJ, et al. Association of quantitative
anticardiolipin antibody levels with fetal loss and time of loss in systemic
lupus erythematosus. Q J Med 1988; 255:525531.
52 Cowchock S, Reece EA. Do low-risk pregnant women with antiphospholipid
antibodies need to be treated? Organizing Group of the Antiphospholipid
Antibody Treatment Trial . Am J Obstet Gynecol 1997; 176:10991100.
66 Farquharson RG, Quenby S, Greaves M. Antiphospholipid syndrome in
pregnancy: a randomized, controlled trial of treatment. Lupus 2002;
100:408413.
67 Spinnato JA, Clark AL, Pierangeli SS, et al. Intravenous immunoglobulin
therapy for the antiphospholipid syndrome in pregnancy. Am J Obstet
Gynecol 1995; 172:690694.
68 Clark AL, Branch DW, Silver RM, et al. Pregnancy complicated by the
antiphospholipid syndrome: outcomes with intravenous immunoglobulin
therapy. Obstet Gynecol 1999; 93:437441.
69 Marzusch K, Dietl J, Klein R, et al. Recurrent first trimester spontaneous
abortion associated with antiphospholipid antibodies: a pilot study of
treatment with intravenous immunoglobulin. Acta Obstet Gynecol Scand
1996; 75:922926.
70 Vaquero E, Lazzarin N, Valensise H, et al. Pregnancy outcome in recurrent
spontaneous abortion associated with antiphospholipid antibodies: a
comparative study of intravenous immunoglobulin versus prednisone plus
low-dose aspirin. Am J Reprod Immunol 2001; 45:174179.
53 Pattison NS, Chamley LW, Birdsall M, et al. Does aspirin have a role in
improving pregnancy outcome for women with the antiphospholipid
syndrome? A randomized controlled trial. Am J Obstet Gynecol 2000;
183:10081012.
71 Branch DW, Peaceman AM, Druzin M, et al. A multicenter, placebocontrolled pilot study of intravenous immune globulin treatment of antiphospholipid syndrome during pregnancy. The Pregnancy Loss Study Group.
Am J Obstet Gynecol 2000; 182:122127.
54 Tulppala M, Marttunen M, Soderstrom-Anttila V, et al. Low-dose aspirin in
prevention of miscarriage in women with unexplained or autoimmune related
recurrent miscarriage: effect on prostacyclin and thromboxane A2 production.
Hum Reprod 1997; 12:15671572.
72 Harris EN, Pierangeli SS. Utilization of intravenous immunoglobulin therapy to
treat recurrent pregnancy loss in the antiphospholipid syndrome: a review.
Scand J Rheumatol Suppl 1998; 107:97102.
55 Empson M, Lassere M, Craig JC, et al. Recurrent pregnancy loss with
antiphospholipid antibody: a systematic review of therapeutic trials. Obstet
Gynecol 2002; 99:135144.
A systematic review of therapeutic trials with aspirin for APS. Also appears in
Cochrane database, and shows that there is no evidence that aspirin has an effect
on the live birth rate.
..
73 Valensie H, Vaquero E, De Carolis C. Normal fetal growth in women with
antiphospholipid syndrome treated with high dose intravenous immunoglobulin (IVIG). Prenat Diag 1995; 15:509517.
74 Kwak JY, Quilty EA, Gilman-Sachs A, et al. Intravenous immunoglobulin
infusion therapy in women with recurrent spontaneous abortions of immune
etiologies. J Reprod Immunol 1995; 28:175188.
S-ar putea să vă placă și
- Practice Bulletin: Antiphospholipid SyndromeDocument8 paginiPractice Bulletin: Antiphospholipid SyndromeSus ArÎncă nu există evaluări
- Acog SDR AntifosfolipidicDocument8 paginiAcog SDR Antifosfolipidicleonar8Încă nu există evaluări
- Dilute Russell's Viper Venom Test (dRVVT) ExplainedDocument15 paginiDilute Russell's Viper Venom Test (dRVVT) ExplainedAngelo GreenÎncă nu există evaluări
- Dr. Sharda Jain: Director: Secretary GeneralDocument91 paginiDr. Sharda Jain: Director: Secretary GeneraljijaniÎncă nu există evaluări
- OSCE Revision OBG DocumentDocument60 paginiOSCE Revision OBG DocumentshreyaÎncă nu există evaluări
- OB - CPG HTN in Pregnancy BEADocument138 paginiOB - CPG HTN in Pregnancy BEAEllieAdlerÎncă nu există evaluări
- Antiphospholipid Syndrome (Aps) and PregnancyDocument36 paginiAntiphospholipid Syndrome (Aps) and Pregnancyskeisham11Încă nu există evaluări
- Postpartum CollapseDocument54 paginiPostpartum Collapsemedical chroniclesÎncă nu există evaluări
- GCT For Dummies - Publish AbleDocument24 paginiGCT For Dummies - Publish AblepcrosleyÎncă nu există evaluări
- Fetal MonitoringDocument6 paginiFetal MonitoringRraouzmaaliÎncă nu există evaluări
- Placenta Praevia, Placenta Accreta and Vasa Praevia Managment and Diagnosis Royal College of ObgDocument26 paginiPlacenta Praevia, Placenta Accreta and Vasa Praevia Managment and Diagnosis Royal College of ObgDiana PanaitÎncă nu există evaluări
- Hypertension in PregnancyDocument20 paginiHypertension in PregnancyFAMED RESIDENTS CESMED100% (1)
- Management of CA Vulva 2Document33 paginiManagement of CA Vulva 2api-3705046Încă nu există evaluări
- 002 Intrapartum Fetal Heart Rate Monitoring 3a - ACOG Bulletin 106 PDFDocument11 pagini002 Intrapartum Fetal Heart Rate Monitoring 3a - ACOG Bulletin 106 PDFale_fearÎncă nu există evaluări
- Hepatitis B in PregnancyDocument17 paginiHepatitis B in PregnancysnazzyÎncă nu există evaluări
- SEIZURE CASE PROTOCOLDocument1 paginăSEIZURE CASE PROTOCOLMarco Paulo Reyes NaoeÎncă nu există evaluări
- Analytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsDocument5 paginiAnalytical Study of Intrauterine Fetal Death Cases and Associated Maternal ConditionsNurvita WidyastutiÎncă nu există evaluări
- Gynecological History Taking and ExaminationDocument17 paginiGynecological History Taking and Examinationnmsiswaridewi100% (1)
- Abnormal Uterine BleedingDocument12 paginiAbnormal Uterine BleedingGilang DermawanÎncă nu există evaluări
- (SLE) and PregnancyDocument60 pagini(SLE) and PregnancyNurfikhaHandayaniÎncă nu există evaluări
- Preterm Prelabour Rupture of MembranesDocument12 paginiPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanÎncă nu există evaluări
- Maternal Collapse During PregnancyDocument57 paginiMaternal Collapse During PregnancytapayanaÎncă nu există evaluări
- Benign and Malignant Ovarian Tumors: Case 1Document14 paginiBenign and Malignant Ovarian Tumors: Case 1Charrie RagadiÎncă nu există evaluări
- Contraction Stress Test complicationsDocument5 paginiContraction Stress Test complicationsPao Ali100% (1)
- POGS PB Dystocia Sept 2022Document6 paginiPOGS PB Dystocia Sept 2022John Piox Badiang100% (1)
- Preterm Postterm Prom1Document35 paginiPreterm Postterm Prom1api-3856051Încă nu există evaluări
- Cholestatic Disease in PregnancyDocument25 paginiCholestatic Disease in Pregnancyarifbotwin100% (1)
- Normal Conduct of LaborDocument62 paginiNormal Conduct of LaborFaye Cabotaje LinganÎncă nu există evaluări
- Abruptio Placentae: Insert or Drag & Drop Your PhotoDocument42 paginiAbruptio Placentae: Insert or Drag & Drop Your PhotoClareen JuanicoÎncă nu există evaluări
- Placenta Previa Experience at Saudi HospitalDocument23 paginiPlacenta Previa Experience at Saudi HospitalGabbyÎncă nu există evaluări
- Deep Vein Thrombosis and Pulmonary Embolism in Pregnancy - Prevention - UpToDateDocument11 paginiDeep Vein Thrombosis and Pulmonary Embolism in Pregnancy - Prevention - UpToDateGabyta007Încă nu există evaluări
- Hypertension and Angina DrugsDocument158 paginiHypertension and Angina DrugsMelissa SalayogÎncă nu există evaluări
- Hypertension in PregnancyDocument34 paginiHypertension in PregnancyMusekhirÎncă nu există evaluări
- Medical Diseases Complicating Pregnancy: by The Name of AllahDocument45 paginiMedical Diseases Complicating Pregnancy: by The Name of Allah'محمد علي' محمد لافيÎncă nu există evaluări
- Poly Hi DR AmnionDocument7 paginiPoly Hi DR Amnionwanwan_adongÎncă nu există evaluări
- Endometrial Hyperplasia: by Dr. Mervat AliDocument48 paginiEndometrial Hyperplasia: by Dr. Mervat AliAsh AmeÎncă nu există evaluări
- OB 1.01 DystociaDocument9 paginiOB 1.01 DystociaRaquel Reyes100% (1)
- Acog 19Document25 paginiAcog 19Janet GoldameirÎncă nu există evaluări
- Mal Presentations Mal PositionsDocument4 paginiMal Presentations Mal PositionsMelissa Aina Mohd YusofÎncă nu există evaluări
- Philippine CPG-2013-uti in Adults-Part1 PDFDocument82 paginiPhilippine CPG-2013-uti in Adults-Part1 PDFVirginia AbalosÎncă nu există evaluări
- Endometrial HyperplasiaDocument12 paginiEndometrial HyperplasiaHenri KnafoÎncă nu există evaluări
- Operative Vaginal Delivery PDFDocument56 paginiOperative Vaginal Delivery PDFFarehan Md IsaÎncă nu există evaluări
- Hormone Regulation of the Menstrual CycleDocument8 paginiHormone Regulation of the Menstrual CycleRj PolvorosaÎncă nu există evaluări
- Planes and Diameters of The PelvisDocument32 paginiPlanes and Diameters of The PelvisRumelle ReyesÎncă nu există evaluări
- Ectopic Pregnancy 2Document9 paginiEctopic Pregnancy 2Kristine VanzuelaÎncă nu există evaluări
- Ob CPCDocument80 paginiOb CPCDonna Meryll Eduave-EsguerraÎncă nu există evaluări
- AUBDocument26 paginiAUByayaslaras96Încă nu există evaluări
- Causes of Fetal DeathDocument3 paginiCauses of Fetal DeathRene Cordova InapanÎncă nu există evaluări
- Operative Vaginal DeliveryDocument6 paginiOperative Vaginal DeliveryCT Johara MusorÎncă nu există evaluări
- 02 Gestational Trophoblastic DiseaseDocument8 pagini02 Gestational Trophoblastic Diseasemisakichan FrandoÎncă nu există evaluări
- Diabetes Acog 2017Document15 paginiDiabetes Acog 2017Holger Vicente Guerrero Guerrero100% (1)
- Green Top Guidelines 13Document29 paginiGreen Top Guidelines 13garfield1Încă nu există evaluări
- Threatened AbortionDocument1 paginăThreatened AbortionKEn PilapilÎncă nu există evaluări
- Forceps Delivery For Gravidocardiac PatientsDocument80 paginiForceps Delivery For Gravidocardiac PatientsTots A. Macahilo-LayawonÎncă nu există evaluări
- Essentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2De la EverandEssentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly Different Volume 2Încă nu există evaluări
- Problem-based Approach to Gastroenterology and HepatologyDe la EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisÎncă nu există evaluări
- Handbook of Current and Novel Protocols for the Treatment of InfertilityDe la EverandHandbook of Current and Novel Protocols for the Treatment of InfertilityMichael H. DahanÎncă nu există evaluări
- Rahayu, 2021Document6 paginiRahayu, 2021Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Colletti 2013Document7 paginiColletti 2013Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Guidlines Pregnancy and Heart DiseaseDocument52 paginiGuidlines Pregnancy and Heart DiseasePanggih Sekar Palupi IIÎncă nu există evaluări
- Atrio-Ventricular Septal Defect in Pregnant Women, How To Deal With It: A Case StudyDocument6 paginiAtrio-Ventricular Septal Defect in Pregnant Women, How To Deal With It: A Case StudyDara Dasawulansari SyamsuriÎncă nu există evaluări
- Furenas, 2020Document9 paginiFurenas, 2020Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Hesselink, 2019Document8 paginiHesselink, 2019Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Heart Disease and Pregnancy: A Review of Physiological Changes and ManagementDocument17 paginiHeart Disease and Pregnancy: A Review of Physiological Changes and ManagementDuy Nguyen CongÎncă nu există evaluări
- E001148 FullDocument6 paginiE001148 FullDara Dasawulansari SyamsuriÎncă nu există evaluări
- Causes and Management of Secondary Postpartum HaemorrhageDocument6 paginiCauses and Management of Secondary Postpartum HaemorrhageDara Dasawulansari SyamsuriÎncă nu există evaluări
- Emergency cesarean in patient with atrial septal defectDocument3 paginiEmergency cesarean in patient with atrial septal defectDara Dasawulansari SyamsuriÎncă nu există evaluări
- Pregnancy in Adults With Repaired/unrepaired Atrial Septal DefectDocument8 paginiPregnancy in Adults With Repaired/unrepaired Atrial Septal DefectDara Dasawulansari SyamsuriÎncă nu există evaluări
- Causes of An Elevated CA 125Document1 paginăCauses of An Elevated CA 125Dara Dasawulansari SyamsuriÎncă nu există evaluări
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument5 paginiEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyDara Dasawulansari SyamsuriÎncă nu există evaluări
- Pregnancy Issues in Women With Atrial Septal Defect: April 2012Document9 paginiPregnancy Issues in Women With Atrial Septal Defect: April 2012Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Tapros - Leuprorelin Asetate - DKI9270700244A1 - 2015Document26 paginiTapros - Leuprorelin Asetate - DKI9270700244A1 - 2015Ananto PrasetyoÎncă nu există evaluări
- Pitfalls in The Diagnosis of Congenital Diaphragmatic HerniaDocument2 paginiPitfalls in The Diagnosis of Congenital Diaphragmatic HerniaDara Dasawulansari SyamsuriÎncă nu există evaluări
- 8 - 11 March 2021: Bali Nusa Dua Convention CenterDocument2 pagini8 - 11 March 2021: Bali Nusa Dua Convention CenterDara Dasawulansari SyamsuriÎncă nu există evaluări
- Bansal 2016Document2 paginiBansal 2016Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Bochdalek Diaphragmatic Hernia PDFDocument4 paginiBochdalek Diaphragmatic Hernia PDFDara Dasawulansari SyamsuriÎncă nu există evaluări
- 4088 FTPDocument10 pagini4088 FTPDara Dasawulansari SyamsuriÎncă nu există evaluări
- Esaso52 04Document8 paginiEsaso52 04Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Congenital Diaphragmatic HerniaDocument15 paginiCongenital Diaphragmatic HerniaDara Dasawulansari SyamsuriÎncă nu există evaluări
- Medind - Nic.in Icb t05 I5 Icbt05i5p445Document4 paginiMedind - Nic.in Icb t05 I5 Icbt05i5p445Ester SibaraniÎncă nu există evaluări
- En 03Document6 paginiEn 03Dara Dasawulansari SyamsuriÎncă nu există evaluări
- Findings From ACGH in Patients With Congenital DiaphragmaticDocument12 paginiFindings From ACGH in Patients With Congenital DiaphragmaticDara Dasawulansari SyamsuriÎncă nu există evaluări
- Late-Presenting Congenital Diaphragmatic HerniaDocument5 paginiLate-Presenting Congenital Diaphragmatic HerniaDara Dasawulansari SyamsuriÎncă nu există evaluări
- Epidemiologic Characteristics of CongenitalDocument5 paginiEpidemiologic Characteristics of CongenitalDara Dasawulansari SyamsuriÎncă nu există evaluări
- Late Versus Early Surgical Correction For Congenital SummaryDocument3 paginiLate Versus Early Surgical Correction For Congenital SummaryDara Dasawulansari SyamsuriÎncă nu există evaluări
- Survival Treted With Very Delayed Surgery, Spontaneous Respiration, and No Chest TubeDocument4 paginiSurvival Treted With Very Delayed Surgery, Spontaneous Respiration, and No Chest TubeDara Dasawulansari SyamsuriÎncă nu există evaluări
- Congenital Diaphragmatic Hernia in 120 Infants TreatedDocument10 paginiCongenital Diaphragmatic Hernia in 120 Infants TreatedDara Dasawulansari SyamsuriÎncă nu există evaluări
- Khatr Khola ISP District RatesDocument56 paginiKhatr Khola ISP District RatesCivil EngineeringÎncă nu există evaluări
- Preferensi Konsumen &strategi Pemasaran Produk Bayem Organik Di CVDocument8 paginiPreferensi Konsumen &strategi Pemasaran Produk Bayem Organik Di CVsendang mÎncă nu există evaluări
- Kidde Ads Fm200 Design Maintenance Manual Sept 2004Document142 paginiKidde Ads Fm200 Design Maintenance Manual Sept 2004José AravenaÎncă nu există evaluări
- Handbook For Magnaflux L10 CoilDocument4 paginiHandbook For Magnaflux L10 CoilmgmqroÎncă nu există evaluări
- NMC Confirmation FormDocument3 paginiNMC Confirmation FormGianina AvasiloaieÎncă nu există evaluări
- Module 4 q2 Smaw-9-10Document15 paginiModule 4 q2 Smaw-9-10Louvre Ferris Salabao TangbawanÎncă nu există evaluări
- Jamec Air FittingsDocument18 paginiJamec Air Fittingsgoeez1Încă nu există evaluări
- Schneider - Cptg010 en (Print)Document16 paginiSchneider - Cptg010 en (Print)el_koptan00857693Încă nu există evaluări
- Sugar Reseach in AustraliaDocument16 paginiSugar Reseach in AustraliaJhonattanIsaacÎncă nu există evaluări
- Regional Ecology Test ScoringDocument14 paginiRegional Ecology Test Scoringaisyah Wardah201Încă nu există evaluări
- Reflective Essay Assignment #8 - Managing Emotions and Coping With StressDocument2 paginiReflective Essay Assignment #8 - Managing Emotions and Coping With StressRej GarbosaÎncă nu există evaluări
- Husqvarna 340/345/350 Operator's ManualDocument47 paginiHusqvarna 340/345/350 Operator's ManualArtur MartinsÎncă nu există evaluări
- MSE 2103 - Lec 12 (7 Files Merged)Document118 paginiMSE 2103 - Lec 12 (7 Files Merged)md akibhossainÎncă nu există evaluări
- IOSA Self Evaluation Form - 31 October 2014Document45 paginiIOSA Self Evaluation Form - 31 October 2014pknight2010Încă nu există evaluări
- PTA Resolution for Donation to School WashroomDocument2 paginiPTA Resolution for Donation to School WashroomMara Ciela CajalneÎncă nu există evaluări
- The Role of Play Therapists in Children's Transitions: From Residential Care To Foster CareDocument11 paginiThe Role of Play Therapists in Children's Transitions: From Residential Care To Foster Caresherry_hoang_1Încă nu există evaluări
- Report Experiment 5 STK1211Document9 paginiReport Experiment 5 STK1211NurAkila Mohd YasirÎncă nu există evaluări
- Baileys in 2009: Case Study Reference No 509-050-1Document17 paginiBaileys in 2009: Case Study Reference No 509-050-1Ernesto KulasinÎncă nu există evaluări
- Euro 4 Standard PDFDocument2 paginiEuro 4 Standard PDFCamellaÎncă nu există evaluări
- Research PaperDocument12 paginiResearch PapershreyanshÎncă nu există evaluări
- SSMT ConplanDocument2 paginiSSMT ConplanJeffrey VillangcaÎncă nu există evaluări
- Steps of Repertorization - 5e097dab9ad98Document18 paginiSteps of Repertorization - 5e097dab9ad98Sowjanya JyothsnaÎncă nu există evaluări
- 1 The Fifth CommandmentDocument10 pagini1 The Fifth CommandmentSoleil MiroÎncă nu există evaluări
- McCubbin, H. I., & Patterson, J. M. (1983) - The Family Stress Process. Marriage & Family Review, 6 (1-2), 7-37Document33 paginiMcCubbin, H. I., & Patterson, J. M. (1983) - The Family Stress Process. Marriage & Family Review, 6 (1-2), 7-37Gimena MottaÎncă nu există evaluări
- 12 2022 Salary Slip SintexDocument1 pagină12 2022 Salary Slip SintexpathyashisÎncă nu există evaluări
- Personal Chiller 6-Can Mini Refrigerator, Pink K4Document1 paginăPersonal Chiller 6-Can Mini Refrigerator, Pink K4Keyla SierraÎncă nu există evaluări
- CWK-IDD-009-CC-2020: Reference Checking Consent and Authorization Form Candidate's Full NameDocument1 paginăCWK-IDD-009-CC-2020: Reference Checking Consent and Authorization Form Candidate's Full NamePopa Alina-ManuelaÎncă nu există evaluări
- Joyforce SDS - PVA Pellet - r2.ENDocument3 paginiJoyforce SDS - PVA Pellet - r2.ENjituniÎncă nu există evaluări
- Secondary AssessmentsDocument12 paginiSecondary Assessmentsapi-338389967Încă nu există evaluări
- Calculation of Lightning and Switching Overvoltages Transferred Through Power TransformerDocument9 paginiCalculation of Lightning and Switching Overvoltages Transferred Through Power TransformerBožidar Filipović-GrčićÎncă nu există evaluări