Documente Academic
Documente Profesional
Documente Cultură
Testicular Testis
Încărcat de
Gede Mei PutraDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Testicular Testis
Încărcat de
Gede Mei PutraDrepturi de autor:
Formate disponibile
TESTICULAR TUMORS
Ep id emio 1ogic, Et io1ogic, and Path o logic Features
F. K. MOSTOFI,MD
Observations on 6,000 testicular tumors revealed the following: Testicular tumors constitute the fourth most common cause of deaths from neoplasia in the
age group of 15-34 years of age. There is a definite geographic, racial, and age
distribution. The cause of testicular tumors is unknown, but cryptorchidism,
trauma, infections, and genetic and endocrine factors appear to play a role in
their development. Germ cell tumors comprise the large majority of testicular
tumors and present one or more of 4 basic histologic patterns: seminoma,
embryonal carcinoma, choriocarcinoma, and teratoma. In 40% the tumors
show admixtures of 2 or more of these basic cell types. Tumors of specialized
gonadal stroma constitute about 6% of testicular tumors and consist of Leydig
cell, Sertoli cell, and granulosa-theca cell tumors, or admixtures of these. The
most important metastatic tumor of the testes is malignant lymphoma,
initially manifested as testicular tumor.
25 YEARS OF
personal experience and the opportunity
to observe over 7,000 testicular tumors registered in the Testicular Tumor Registry of
the American Registry of Pathology, sponsored by the American Urological Association
at the Armed Forces Institute of Pathology.
This discussion will cover the tumors of germ
cell origin and gonadal stromal tumors and
briefly mention some of the other tumors involving this organ.
HIS PRESENTATION IS BASED ON
EPIDEMIOLOGIC
FINDINGS
The incidence rate of testicular tumors in
the United States is 2.1-2.2 per 100,000
males;3 in Ontario, Canada, it is 2.5 per
100,000 males.l3 The U. S. Census Bureau attributed 0.64% of all male cancer deaths to
testicular tumors, while in England the comparable rate was 0.52y0.In the United States
and Canada, in the 15- to 34-year age group,
deaths from testicular tumors account for
11-13% of all cancer deaths, constituting the
fourth most common cause of death from neoplasia in this age group. A doubling of mortality from testicular tumors from 1944-1947
Presented at the Amcrican Cancer Society's National
Conference on Urologic Cancer, Washington, D. C.,
March 29-31, 1973.
From the Genitourinary Pathology Branch, Armed
Forces Institute of Pathology, Washington, D. C.
Address for reprints: F. K. Mostofi. MD, Armed
Forces Institute of Pathology, Washington, D. C. 20306.
Received for publication August 1, 1973.
(3.2 per 100,000) and from 1958-1962 (6.3) has
been reported in Copenhagen.4 There is evidence that similar doubling of mortality from
testicular tumors has occurred in the United
StateslJl and New Zealand.12
Testicular tumors are rare among the American Negro population, and reports from Africa indicate its extreme rarity among Negroes
there. Low rates have also been reported from
Asia and New Zealand.16
Testicular tumors occur in animals, but
there is considerable species differentiation. In
the horse, teratoma and seminoma are the
most common testicular tumors, while in the
dog, seminoma and Sertoli and Leydig cell tumors are not infrequent, and the incidence increases with old age. Leydig cell tumors are
also common in older rats and mice, but seminomas and teratomas are rare in these animals.
ETIOLOGIC
FINDINGS
The etiology of testicular tumors is unknown. Several factors suggest a causal relationship.
A. Maldescent
I n 2,000 testicular tumors we found 72 that
occurred in undescended testes, an incidence
of 3.6%. Because cryptorchidism is seen in
0.2570 of selectees in the U.S. Army, the
chances are about 14 times greater that a
tumor might develop in an undescended testis
1186
No. 5
TESTICULAR
TUMORSMostofi
than in a normally located testis. Miillerls reported that malignancy in undescended testes
is 10 times greater than in the testes that descended normally. It has been reported that 1
in 80 inguinal testes and 1 in 20 abdominal
testes will become malignant.10J9 It must be
remembered, however, that such studies are of
selected groups, e.g., hospital patients and soldiers, and may not be applicable to the general population. Attention should also be
called to the fact that a tumor may occasionally develop in a normally descended testis of
a patient with a contralateral undescended
testis.
Five factors may be operative in increased
incidence of testicular tumors in cryptorchid
testes: abnormal germ cells, elevated temperature, interference with blood supply, endocrine disturbances, and gonadal dysgenesis.
There is, however, no conclusive evidence as
to which of these factors is responsible for the
high incidence of tumors in such testes.
B. Age
1187
D. Infection
Many patients with testicular tumors have a
history of orchitis of some type, particularly
mumps. It is quite possible that a viral infection of the germ cell may trigger carcinogenesis.
E. Endocrine Abnormalities
A number of factors suggest a strong endocrine role in testicular tumors:16 (a) Induction
of teratomas in fowl by injection of zinc salts
occurs only during pituitary gonadotropin secretion; (b) the peak incidence in testicular
tumors in man is in the period of high androgenic activity; (c) gonadotropins and/or estrogens are produced by a number of testicular
tumors; (d) a number of patients with such tumors show elevation of pituitary gonadotropins, which persists even after orchiectomy; (e)
in tissue culture, androsterone accelerates
growth of certain tumors; and (f) the type of
tumor encountered in the testis varies with
the stage of maturation of the testis.
Testicular tumors are almost entirely limited to 3 age periods: infancy, late adolescence-young adulthood (20-35 years), and 50
years and over.16 The histologic pattern and
behavior of the tumor differ with each period.
For example, no seminomas have been reported in infants; embryonal carcinoma and
teratoma are the most common tumors of infants and children. Their morphological features are somewhat different, and their prognosis is much better than corresponding
tumors in adults. Seminoma, embryonal carcinoma, teratoma, and teratocarcinoma are common in young adults, but seminoma is more
frequent in patients in the fourth decade,
while spermatocytic seminoma and malignant
lymphoma occur in the older age group.
F. Genetic Factors
A high incidence of testicular tumors has
been reported in brothers, identical twins,
monozygous twins, and other members of the
same family. Miiller18 reported that in about
16% of the cases on which sufficient information was available there was a history of malignant disease in the nearest family. There
is also a high incidence of a second testicular
tumor in a patient with a testicular tumor.
C. Trauma
Many patients with testicular tumor give a
history of trauma, and Fergusons reported
that 11% of the 527 testicular tumors had
such a history. Experimental evidence also
suggests a relationship between tumor and
trauma. Trauma is considered a factor in zinc
or copper-induced testicular tumors and in experimental induction of such tumors by transplantation of the genital ridge.m.21 A heavy
and dragging tumorous testis may be susceptible to trauma, and aggravation of an existing
tumor by trauma may facilitate spread of the
tumor.
H. Experimental Induction of Tumors of the
Testis
The Russian scientists697 were the first to
induce teratoma in fowl testes by injection of
zinc chloride and, more recently, of copper
sulfate. The reaction, however, was confined
to 3 months in spring. Stevens20921 has made a
major contribution by producing a reliable
experimental model for testicular tumors. He
has produced testicular teratomas in strain
129 mice by transplantation of the genital
ridge of a 12G-day embryo to the testis of a
mature animal of the same strain. Eighty-five
to 90% of these transplants develop tumors,
G. Abnormal Testes
The high incidence of testicular tumors in
dysgenetic testes would seem to suggest that
such testes are genetically abnormal, but
whether such testes are dysgenetic has not
been settled.
CANCERNovember 1973
1188
but the period in which the embryonic genital
ridge undergoes teratogenesis is very limited.
PATHOLOGIC
FEATURES
Other papers emphasize the fact that as yet
there is no clinically reliable classification of
testicular tumors and the urologist must depend on clinical stage and on histologic appearance of the tumor. Biopsy, generally
accepted for other sites, is absolutely contraindicated in testicular tumors. If a tumor is
suspected, the testis must be removed in toto.
From the pathologists point of view, it is esTABLE1. Pathologic Classification of Testicular
Tumors
~
~~~
I. Germ cell tumors
A. Tumors showing a single cell type
1. Seminoma: typical, anaplastic, and spermatocytic
2. Embryonal carcinoma: adult-type,
infantile-type, and polyembryoma
3. Choriocarcinoma
4. Teratorna
B. Tumors showing more than one histologic
pattern
1. Embryonal carcinoma plus teratoma
(teratocarcinoma)
2. Embryonal carcinoma and seminoma
3. Seminoma and teratoma
4. Other combinations
C. Others
1. Epidermal cysts
2. Retinal anlage tumors
3. Carcinoids
11. Tumors of gonadal stroma
A. Leydig cell tumors
B. Sertoli cell, granulosa cell, theca cell tumors
C. Tumors of primitive gonadal stroma
D. Mixtures of these three
111. Tumors and tumor-like conditions with both
germ cell and gonadal stromal componentsgonadoblastoma
IV. Tumors of adnexae
A. Benign: adenomatoid tumors, adenoma,
soft tissue tumors
B. Malignant: carcinoma, sarcomas
V. Secopdary tumors, malignant lymphomas, and
carcinomas
VI. Unclassified tumors
VII. Tumor-like conditions
A. Granulomatous orchitis
B. Fibromatous periorchitis
C. Sclerosing granuloma
D. Sperm cell granuloma
E. Adrenal rests and hyperplasia
F. Others
Vol. 32
sential to have adequate sampling, especially
of the areas that appear grossly different.
The pathologic classification herein proposed (Table l), is based on the histologic
classification proposed by Friedman and
Moore9 and by Dixon and Moore.6 It is the
tentative World Health Organization classification. In presenting the classification, I
should like to emphasize that any comment
and criticism of the classification is welcome.
Within 2 or 3 years, after a number of international conferences and possible modifications, this classification will become the WHO
classification, and we hope that it will be internationally accepted.
I. Germ Cell Tumors
Germ cell tumors constitute more than 94y0
of testicular tumors.16 In pathologic classification of these tumors it is essential to identify
and designate the basic cell type, determine
whether this is the sole component, and record all the components and their relative
proportions. Sixty percent of testicular tumors
show a single cell pattern, and 40% show
more than 1 cell type. In the latter it is desirable to list the specific types and relative proportions of each component.
A . Tumors Showing a Single Cell Type
1. Seminoma
Seminoma is defined as a germ cell tumor
composed of characteristic large uniform
cells with clear cytoplasm. The cells resemble primordial germ cells, and they are
supported by a fibrovascular stroma with varying amounts of lymphocytic infiltration and a
granulomatous reaction. The tumor is of relatively low malignancy and high radiosensitivity. It occurs in the ovary, where it is designated as dysgerminoma. Seminoma comprises
from 35-71y0 of testicular tumors, the relative
frequency depending on the type of hospital
population under study. Seminomas are more
commonly seen in the fourth and fifth decades
of life, although we have seen this tumor as
early as the 10th year of age. N o cases of seminoma have been confirmed in infants, but it is
a common tumor in the dog.
We recognize 3 subtypes of seminoma: typical seminoma, anaplastic seminoma, and spermacytic seminoma.
a. Typical seminoma
i. Gross features: T h e typical seminoma
and the anaplastic seminoma present essentially the s&e appearance. T h i right testis is
No. 5
involved more frequently than the left. In
85y0 of patients the testis enlarges, sometimes
reaching 10 times the normal size. In 15% the
testis is normal or smaller. The enlargement is
usually diffuse, although occasionally it may
be nodular. The tunica albuginea may be glistening or dull, smooth or rough, thin or thickened. The cut surfaces show a grayish-white,
glistening tissue that is lobulatecl and homogenous. Areas of necrosis and hemorrhage are
infrequent. The tumor is usually demarcated
but not encapsulated; in about half the patients, however, the entire testis is replaced by
a tumor. In about 8% there is extension beyond the capsule to the scrota1 sac, the epididymis, or the spermatic cord.
ii. Histologic features: Typical seminoma is
composed of uniform cells supported by a delicate fibrous stroma with varying amounts of
lymphocytic and granulomatous reaction (Fig.
1). Seminoma cells are large, polyhedral, or
round and have a distinct cell border, clear or
granular cytoplasm, and large centrally located
spherical, hyperchromatic nuclei that have an
irregular nuclear membrane, distinct and
granular chromatin distribution, and 1 or 2
large basophilic nucleoli. The cytoplasm is
clear or granular and contains varying
amounts of glycogen and, rarely, lipid material. Mitotic figures are usually infrequent,
and little variation in size and shape of the
FIG. 1. Typical seminoma of the testis
showing uniform cells
occurring in lobules
separated by fibrovascular stroma and infiltration of scattered
lymphocytes (AFIP
Neg. 73-5740, x210).
TESTICULAR
TUMORSMost of;
1189
cells is encountered. At times the tumor may
be confined to the seminiferous tubules.
Lymphocytic infiltration is seen in almost
all seminomas, but it is marked in only about
20%. The cells consist of mature lymphocytes.
Granulomatous reaction is present in about
half of the cases but is marked in about 20Y0.
It consists of fibroblastic and histocytic reaction with varying numbers of lymphocytes
and foreign body giant cells. The lymphoid
and the granulomatous reaction would seem
to suggest immunologic response of the host
to the tumor. Such reaction indicates good
prognosis.
b. Anaplastic seminoma
Some degree of anaplasia is seen in many
seminomas, but in about 10% the bulk of the
tumor is anaplastic. As already mentioned, no
gross characteristics are evident. Cellular irregularity, with variations in size and shape and
staining of the nuclei, is present, but these features often are difficult to evaluate because fixation may affect the appearance of the cells.
The nuclei are larger and more vesicular than
normally. We found that increased mitotic
activity is the single most important, easily recognizable, and reliable feature (Fig. 2). An average of 3 or more mitotic figures per highpower field would certainly indicate a rapidly
growing neoplasm and would justify the designation of the tumor as anaplastic. We found
1190
CANCER
November 1973
Vol. 32
FIG. 2. Anaplastic
seminoma showing
moderate anaplasia of
cells and increased mitotic activity. At least
four mitotic figures
are seen (H & E. x250;
AFIP Neg. 5182).
that most of the metastasizing seminomas were
anaplastic. Maier and his associates14 showed
that in contrast to typical or classic seminoma,
anaplastic seminoma has a poorer prognosis.
Such seminomas may be difficult to differentiate from solid embryonal carcinoam.
Both typical and anaplastic seminomas may
show tumor giant cells, some of which resemble syncytiotrophoblastic cells. T h e presence
of giant cells in itself does not justify the diagnosis of choriocarcinoma, however.
c. Spermatocytic seminoma
First recognized by Masson15 in 1946, this
tumor is quite different grossly and microscopically from the classic or anaplastic seminoma.
Spermatocytic seminoma comprises 9% of
seminomas. It usually occurs in those over 40
years of age.
i. Gross features: The tumor tends to be
yellowish in color, soft, and slightly mucoid.
Spongy and cystic areas with ragged edges are
quite common, but areas of true necrosis and
hemorrhage are usually small. T h e tumor
usually attains a large size.
ii. Histologic features: In contrast to the
uniform cellularity of typical and anaplastic
seminoma, 3 types of cells can be recognized
in spermatocytic seminoma (Fig. 3). By far the
greatest population consists of medium-sized
cells with a spherical nucleus and a considera-
ble amount of eosinophilic cytoplasm. Scattered in this sea are two other cell types, the
very small lymphocyte-like cells and the huge
mononuclear cells. The cells have a spherical
basophilic glassy nucleus surrounded by a distinct rim of eosinophilic cytoplasm. Giant
cells are usually mononuclear but occasionally
may be binucleated or multinucleated. The
nuclei are spherical, ovoid, or indented and
surrounded by a considerable amont of eosinophilic cytoplasm.
Masson15 called attention to the filamentous
or spireme-like arrangement of the chromatin
in the nuclei of intermediate and large cells
similar to that present in the meiotic phase of
normal primary spermatocytes. T h e chromatin also occurs in regular clumps, and the nuclear membrane is irregularly thickened. Moderate numbers of mitotic figures may be seen
in some fields, and some of these figures are
abnormal.
Typical seminoma has an excellent prognosis and, properly treated, should have a
95-96% 5-year survival. Spermatocytic seminoma also seems to have good prognosis. In
our experience, most of the seminomas that
metastasize and terminate fatally belong to
the category of anaplastic seminoma.
Seminoma usually spreads by the lymphatic
route. In our material, at autopsy, the most
No. 5
TESTICULAR
TUMORS Mostofi
1191
FIG.3. Spermatocytic
seminoma. In contrast
to Figs. 1 and 2, in this
tumor three cell types
are identified: large
cells, intermediate
cells, and small darkstaining cells (AFIP
Neg. 26-9923; x210).
common sites of involvement are the aortic
and iliac lymph nodes (71%), liver (5473,
right and left lung (each 5773, right kidney
(6%), left kidney (37%). right adrenal (9%),
left adrenal (3574, pancreas (2173, peritoneum (22), pleura (17%), and mediastinal
lymph node (17%). Seminoma usually metastasizes as seminoma, but in a few instances it
may metastasize as embryonal carcinoma, teratoma, or choriocarcinoma.
2. Embryonal carcinoma
Embryonal carcinoma is defined as a primary germ cell tumor of the testes in which
the cells have an embryonic and anaplastic
epithelial appearance and a variable pattern
of acinar, tubular, papillary, solid, and/or
reticular structure. Three categories of embryonal carcinoma have been recognized: the
adult type, the infantile type, and polyembryoma.
a. Adult embryo7tal carcinoma
This occurs most frequently in the latter
part of the second decade, in the third decade,
or in older patients. It constitutes 20y0 of testicular tumors; it occurs in the ovary but is
extremely rare. It is a highly malignant
tumor. It is radiosensitive but requires higher
doses than seminoma. It occurs in mice, but
no cases have been reported in dogs and
horses.
i. Gross features: Embryonal carcinoma
usually is the smallest of all testicular tumors,
averaging about 5Occs in volume, but about
40% are less than 2Occs. The tumor replaces
part or all of the testis, distorting the capsular
surface. About 20y0 of them invade the epididymis or the cord. T h e cut surfaces show a
variegated appearance, with grayish-white
granular or smooth soft tissue, extensive areas
of hemorrhage and necrosis, and little or no
evidence of encapsulation.
ii. Histologic features: T h e characteristic
feature of this tumor is that the cells resemble
epithelial cells and are distinctly malignant
and embryonal in appearance (Figs. 4, 5).
There is considerable variation in size, shape,
and arrangement of these cells. They may be
large and pleomorphic without distinct cell
borders. The cytoplasm may be homogeneously amphophilic or vacuolated. The nuclei
may be regular, ovoid, or spherical and have
an irregular and coarse nuclear membrane,
one or more large nucleoli, and varying degrees of nuclear vacuolization. Mitotic figures
and mononuclear and multinuclear giant cells
are frequent. The 5-year survival rate for embryonal carcinoma is 20-30y0.
Embryonal carcinoma metastasizes most frequently to the iliac lymph nodes (about 96%
of cases), each lung (84%), liver (SO%), pleura
1192
CANCER
November 1973
Vol. 32
FIG. 4. Embryonal
carcinoma of the testis. The tumor forms
glandular and tubular
structures (AFIP Neg.
73-5737; x 210).
(46%), bones of the trunk (21%), and gastrointestinal tract (18%). I n 96 7' of autopsy
cases the metastatic lesions are embryonal carcinomas. In 8% there are also associated areas
of teratoma; and in 5%, areas of choriocarcinomas.
b. Infantile embryonal carcinoma
This is also designated as orchioblastoma,
FIG. 5. Embryonal
carcinoma compared
to seminoma. Carcinoma cells (right) are
larger, more pleomorphic, and have an
a m p h o p h y l i c cytoplasm a n d a large
vesicular nucleus with
prominent nucleolus.
The cells form acini.
Seminoma cells (left)
are smaller and have
vacuolated cytoplasm
and small nucleus.
The cells are in lobules, and there are
scattered lym hocytes
(AFIP Neg. !3-5148;
x 210).
No. 5
yolk sac tumor, endodermal sinus tumor, adenocarcinoma of the infantile testis, juvenile
embryonal carcinoma, etc., and constitutes the
most common testicular tumor of infants and
children. It occurs in adults but usually as a
part of a teratocarcinoma. It is also the variant of embryonal carcinoma that is found in
the ovary.
i. Gross features: It has a homogeneous yellowish, mucinous appearance.
ii. Histologic features: T h e principal histologic pattern consists of anastomosing glandular and ductal structures lined by low columnar, cuboidal, or flat epithelium (Fig. 6).
These may form papillary structures, rows and
columns of cells, or solid areas. T h e large,
irregularly shaped nuclei have a variable chromatin distribution and one or more prominent nucleoli. T h e cytoplasm is usually vacuolated, and the cell borders are indistinct.
The cytoplasm contains considerable amounts
of fat, often refractile, as well as glycogen.
Fine or coarse vacuolization of the cells is
present. Some of these vacuoles coalesce to
form larger vacuoles that seem to merge with
the host vascular spaces.
T h e stroma varies in amount and ranges
from fibrous to cellular to primitive mesenchyme. Frequently it is difficult to distinguish
between stroma and the epithelial elements.
FIG. 6. Infantile embryonal carcinoma.
The tumor shows
small and large spaces
lined by cuboidal or
flat epithelial cells.
These alternate with
more solid areas (AFIP
Neg. 71-7615; ~ 1 1 5 ) .
TESTICULAR
TUMORSMostofi
1193
Vascular invasion is not an infrequent finding, but while its presence suggests poor prognosis, a fatal outcome is not necessarily indicated. Careful examination of these tumors
will reveal some teratoid structures in almost
every tumor, usually consisting of a duct lined
by tall columnar epithelium, a nest of cartilage, or an epidermal cyst. In contrast to adult
embryonal carcinoma, which has a grave prognosis, infantile embryonal carcinoma has a 5year mortality of only SO%, and almost all
deaths occur within the first 18 months.16
In a number of embryonal carcinomas, organoid structures are seen that resemble embryos of 1-2 weeks gestation. They may be
spherical, lobular, or cylindrical. They usually
measure less than 1 mm in diameter and consist of a disc, a cavity, and a tubular form surrounded by loose mesenchyme in which syncytiotrophoblastic and cytotrophoblastic cells
may be seen. The disc consists of a single row
of large cells resembling epithelial cells. The
cavity, which simulates an amniotic cavity, is
lined by flattened epithelial cells. The tubular
structures resemble entoderm. Such structures
are found not only in embryonal carcinomas
but in teratocarcinomas also.
Since embryoid bodies are a stage in the development of embryonal carcinoma and since
they have a wide variation in morphological
1194
CANCER
November 1973
structure and are malignant, their presence
should be recorded. We designate the tumor
as embryonal carcinoma. Only if the tumor
consists solely or predominantly of embryoid
bodies may it justifiably be designated as polyembryoma, corresponding to the ovarian
counterpart.
3. Choriocarcinoma
Choriocarcinoma is defined as a highly malignant testicular tumor composed of cytotrophoblastic and syncytiotrophoblastic cells
in which the latter often cap or otherwise
constitute the advancing edge of the tumor.
Pure choriocarcinoma is extremely rare both
in the testes and in the ovary. We have 18
cases in the first 6,000 testicular tumors. The
tumor is almost entirely confined to patients
in the second and third decades of life, but we
have seen it in a 50-year-oldman. The presenting symptoms in these patients are usually referable to metastatic lesions, since there is little enlargement of the testes and very little
pain. No instances have been seen in infants
and children or in lower animals.
a. Gross features
The testis is usually small or of normal size
and may or may not have a nodule. It may be
large and firm, depending on the extent of the
hemorrhage that invariably accompanies testicular choriocarcinoma. In pure form the
tumor presents as a hemorrhagic central mass
Vol. 32
with some grayish-white viable tissue at the
periphery. When choriocarcinoma occurs with
other cell types, the area usually appears
grossly as a hemorrhagic focus in association
with a cystic or solid testicular tumor.
b. Histologic features
In choriocarcinoma two distinct cell types
are seen-syncytiotrophoblastic and cytotrophoblastic cells (Fig. 7). The typical syncytiotrophoblastic cell is readily recognizable. It is
large and multinucleated and has many hyperchromatic, irregular nuclei. The cytoplasm is
either eosinophilic or amphophilic but has
many vacuoles of various sizes. The vacuoles
usually contain a slightly eosinophilic precipitate and occasionally red blood cells. Other
syncytiotrophoblastic cells may be spindled
and have one large, irregular hyperchromatic
nucleus. Cytotrophoblastic cells are fairly uniform and intermediate in size and are closely
packed. The cytoplasm is clear, and the cell
has a distinct border and a sitlgle uniform,
rather moderate-sized vesicular nucleus. The
advancing edge of the growth (whether in relation to vascular spaces of the surrounding
tissue or not) is usually covered by syncytiotrophoblastic cells that cap the cytotrophoblasts. Such an arrangement suggests a villuslike formation, but true villi (as Seen in the
mature placenta, with a core of loose fibro-
FIG. 7. Chorimrcinoma of the testis. Syncytiotrophoblastic cells
cap cytotrophoblastic
elements (AFIP Neg.
70-2213; X190).
No. 5
TESTICULAR
TUMORS
*
Mostofi
vascular tissue covered by elongated hyperchromatic syncytiotrophoblastic cells, with or
without intervening cytotrophoblasts) have
not been observed in choriocarcinoma of the
testis. Hemorrhage is a constant accompaniment of choriocarcinoma, whether in its pure
form or associated with other testicular tumors. Such hemorrhage should not be interpreted as a response to chemotherapy or
radiation therapy.
There is much confusion about what is
called choriocarcinoma. I have mentioned
that pure choriocarcinoma of the testis is extremely rare. Foci of choriocarcinoma or syncytiotrophoblastic cells are not infrequent in
embryonal carcinoma, seminoma, and teratocarcinoma. We have seen over 500 such cases.
Such tumors, in which choriocarcinomatous
elements may be found in association with teratoma, seminoma, or embryonal carcinoma,
should not be designated simply as choriocarcinoma but rather by all the elements that are
present (e.g., seminoma and choriocarcinoma).
Most of the cures of testicular choriocarcinoma reported in the literature and most, if
not all, failures in chemotherapy of. testicular
choriocarcinoma are tumors in this mixed category.
The diagnosis of choriocarcinoma should
not be made without the presence of elevated
chorionic gonadotropins, but such elevation
per se, without histologic evidence of choriocarcinoma, should not lead to the diagnosis
of choriocarcinoma because the elevated hormone level may be due to pituitary effect.
In our 18 cases of pure choriocarcinoma of
the testis all the metastatic lesions consisted of
choriocarcinoma. Metastatic spread appeared
to be principally hematogenous but also lymphatic: to periaortic and iliac lymph nodes
and each lung ( looyo),liver (86y0), intestines
(71%), spleen, adrenal, or brain (56Y0).
4. Teratoma
Teratoma is defined as a complex tumor
showing recognizable elements of more than
one germ layer in various stages of maturation, often arranged in such a manner as
to suggest abortive organ formation. Generally included under teratoma are three rare lesions of the testis: epidermal cysts, carcinoids,
and retinal anlage tumors. It has been postulated that these represent one-sided development of teratoma. When they occur by themselves these lesions should not be diagnosed as
teratoma, monodermal or otherwise, but by
their specific morphological features.
1195
In our material teratomas constitute about
9% of adult testicular tumors. They occur in
male patients of any age but are found frequently during the first, second, and third decades. The 5-year mortality in adult patients is
29%. The ovarian counterpart is the dermoid
cyst.
a. Gross features
The testis is usually enlarged, averaging 70
cc in volume. The tumor offers varying degrees of resistance to cutting. The cut surfaces
reveal cysts of various sizes filled with clear gelatinous, mucinous, or keratohyaline substance. These alternate with various amounts
of solid tissue and islands of firm, translucent
cartilate and spicules of bone.
b. Histologic features
Teratoma shows elements that are derivable
from more than 1 germ layer (Fig. 8): ectoderm, entoderm, and mesoderm. Ectodermal
elements are represented by squamous epithelium, with or without keratinization, and by
neural tissue; entodermal structures, by gastrointestinal, respiratory, and urinary tracts;
and mesodermal elements, by bone, cartilage,
muscle, and lymphoid tissue.
The components of the tumor may be mature or immature. Mature elements may be
differentiated, ranging from benign-appearing
cells to tissues and organs. Immature teratomas consist of primitive neuroectodermal, en- .
todermal, or mesodermal tissue.
The most common elements in the teratoma
are cysts lined by squamous, cuboidal, columnar, or transitional epithelium, cartilage, intestinal tissue, pancreas, liver, bone marrow,
various types of connective tissue, and smooth
and skeletal muscle fibers. If primitive undifferentiated areas are seen we indicate their
existence. Teratomas occurring in adult patients, even when histologically entirely benign, should not be designated as benign since
29% metastasize and terminate fatally in 5
years.
Metastatic lesions observed in patients with
teratoma consist of teratoma and embryonal
carcinoma (each 63y0), and choriocarcinoma
(25y0). The tumor metastasizes most often
through the lymphatics to the following sites:
aortic and iliac lymph nodes (loo%), liver
83%), each lung (720/,), bones of trunk (36y0),
pleura (3573, and intestines (25%).6J4
In infants and children, teratoma constitutes the second most frequent testicular
tumor. Histologically the constituent elements
are mature, and clinically the prognosis is ex-
1196
CANCER
November 1973
Vol. 32
FIG.8. Teratoma of
the testis showing
cystic spaces, some of
which are lined by
columnar epithelium
and others by squamous cells. Note islands
of cartilage (AFIP Neg.
73-4925; ~22).
cellent, as no deaths have been reported from
testicular teratomas in this age group. Teratoma also occurs in horses and rodents.
B. Germ Cell Tumors Showing More Than
One Histologic Pattern
In about 40% of tumors of the testes more
than 1 histologic pattern is observed. The
relationship of these tumors to each other
and the designations used to identify them
have resulted in much confusion in testicular
oncology.
The most frequent association, that of teratoma and embryonal carcinoma, constitutes
24% of all testicular tumors. Teratoma and
embryonal carcinoma and serminoma are seen
in about 6.4%, embryonal carcinoma and seminoma in 50/,, teratoma and seminoma in
about Z%, teratoma, embryonal carcinoma,
and choriocarcinoma in 1yo.le
We use the term teratocarcinoma to designate tumors that consist of teratomas and
embryonal carcinoma, and we specify the elements that are present and the proportions of
each.
Teratocarcinomas are usually the largest of
all testicular tumors, having a volume of
about 85 cc. The cut surfaces show teratomatous and solid areas. They metastasize principally as embryonal carcinoma (80%), but choriocarcinoma and teratoma may also be found.
Metastasis is through lymphatics and the
blood stream to the preaortic and iliac lymph
nodes (92%), each lung (80%), liver (70%),
brain (40y0),and pleura (My0).
The association of 1 cell pattern with another may or may not affect the clinical behavior, treatment, or prognosis. Dixon and
Moore6 have shown that seminoma in association with embryonal carcinoma and teratoma
has no effect on the prognosis but may affect
the mode of therapy. On the other hand, the
association of embryonal carcinoma with teratoma ameliorates the prognosis of embryonal
carcinoma. The presence of choriocarcinoma
with either embryonal carcinoma or teratoma
adversely affects the prognosis of these
tumors.6J6
Some years ago we reported 17 young
men who died from metastatic embryonal
carcinoma, teratocarcinoma, seminoma, or
choriocarcinoma.2 In each case careful examination of the testis showed a distinct
and well-defined scar, usually in the hilar region, and evidence of old hemorrhage. In
some, small foci of seminoma, embryonal carcinoma, or teratoma were also seen. In some
instances intratubular basally situated hyperchromatic cells were found that we believed
were malignant germ cells. I mention this
group to emphasize the need for careful examination of the testes in patients with extra gonadal germ cell tumors.
No. 5
TESTICULAR
TUMORSMostofi
C. Other Tumors
In contrast to their high incidence in
ovaries, dermoid cysts are rarely seen in
testes. Grossly and microscopically they resemble ovarian cysts with sebaceous and
keratohyaline material, teeth, hair, bone, and
cartilage. We have not seen any metastatic
growths from pure dermoid cysts of the testes.
1. Epidermal cysts
The simple epidermal cyst is lined by keratinizing stratified squamous epithelium sup
ported by fibrous tissue. T h e cyst contains keratohyaline material. There are no skin
appendages. We16 have reported 70 cases from
the Testicular Tumor Registry. They occur at
all ages. I should like to emphasize that in all
epidermal cysts it is absolutely essential to examine the apparently uninvolved portions of
the testis carefully because there may be a
small embryonal carcinoma, seminoma, or a
scar. When none of these elements was present
in our cases and the lesion consisted entirely of
pure epidermoid cyst, there was no metastasis
or recurrence.
2. Retinal anlage tumor or melanotic hamartoma
This tumor is primarily a testicula; adnexal
tumor, but we have seen it occasionally originating in the testis. We have seen no instances
of metastasis from retinal anlage tumors.
3. Carcinoid of the testis
Carcinoid of the testis may be primary or
secondary, functional or nonfunctional. I n a
number of cases the tumor is in association
with a teratoma, but whether in the pure
form or as part of a teratoma, its presence
should be recorded.
11. Tumors of Gonadal Stroma
The primitive gonadal stroma, which is the
precursor of Leydig and Sertoli cells in the
testes and granulosa-theca cells in the ovary,
may manifest its oncogenetic potentialities in
either gonad as differentiated Leydig cell
tumor, Sertoli cell tumor, granulosa-theca cell
tumor, undifferentiated gonadal stromal
tumor, or an admixture of any of these.16J'
By far the most common of these tumors can
readily be identified as either pure Leydig cell
or pure Sertoli cell tumor.
A . Leydig Cell Tumor
Leydig cell tumor is defined as a tumor
of the interstitial cells of Leydig.
In 6,000 testicular tumors registered in the
Testicular Tumor Registry the incidence of
testicular Leydig cell tumor is about 3%. T h e
1197
tumor occurs with almost the same frequency
in both Negro and Caucasian races. Spontaneous Leydig cell tumor has been described in
the dog (in which it is quite frequent, especially in older animals), in horses, cows, birds,
rats, and mice.
Enlargement of the testis, with or without
pain, is the most common symptom. Leydig
cells are one of the 2 normally hormone-producing cells in the testes, and their tumors
manifest a variable endocrine symptomology,
from masculinization in children to feminization or no symptoms in adults. All children
with this tumor manifest macrogenitosomia,
with enlarged penis, pubic and facial hair,
and deep voice. Facial acne, precocious skeletal and muscular development, and unusually
early interest in girls are other symptoms. In
adult patients, 2446% manifest gynecomastia. Other related symptoms include loss of libido, feminine distribution of hair, and presence or absence of genital underdevelopment.
Interestingly, .some patients with malignant
Leydig cell tumor and metastasis show an unusual preservation of muscular structure and
absence of cachexia.
1. Gross features
Leydig cell tumor is usually unilateral, but
5-9% are bilateral. I n such cases suspicion
should be raised of adrenogeni tal syndrome.
The 2 sides are about equally involved. The
testis may be diffusely enlarged, or it may
be nodular. The tumor may vary from less
than 1 cm to more than 10 cm in diameter.
It is usually soft but may be firm or even
hard. The cut surfaces are homogeneously
yellowish to mahogany brown and bulging.
Areas of hyalinization and even calcification
may be present.
2. Histologic features
Leydig cell tumors present an amazing
variation in histologic pattern. The most
common cell population is the medium-sized
hexagonal cell with a distinct cell border,
eosinophilic or vacuolar cytoplasm surrounding an irregular round or oval vesicular
nucleus (Fig. 9). The nucleus usually has a
delicate distribution of chromatin and one
small basophilic nucleolus. Occasional large
but regular binucleated and multinucleated
cells are present. Many tumors contain lipid
material and brown lipofuscin pigment. T h e
characteristic feature of Leydig cell is Reinke's
crystals, which are cigar-shaped cytoplasmic
inclusions of various sizes, best demonstrated
by Masson's trichrome, PTAH, and Mallory's
I198
CANCER
November 1973
Vol. 32
FIG.9. Leydig cell
tumor of the testis.
The cells are uniform,
have granular or clear
cytoplasm, and are in
intimate relationship
with thin-walled blood
vessels (AFIP Neg. 735746; x210).
iron-hematoxylin stains. We have found these
crystals in 40% of tumors, and the crystals
have no hormonal activity.
Other tumor cells may be large, finely or
coarsely vacuolated, small and hyperchromatic, or elongated or spindle-shaped, and
they may have eosinophilic or granular cytoplasm. The cells may occur in cords, islands,
or nests, but usually they have a distinct endocrine pattern of vascularity. The stroma is
usually delicate but may show varying degrees
of hyalinization and even calcification.
Leydig cell tumors occur at any age. They
are usually benign, but 10% develop metastasis. In our material the earliest reported metastasis occurred within 4 months, but usually
metastatic lesions are late in development.
Histologic evidences of malignancy are increased mitotic activity, especially abnormal,
extension to the tunica and appendages, and
invasion of vascular spaces, but the most reliable criterion is development of metastatic
foci.
B. Other Gonadal Stromal Tumors
Sertoli cell tumors, theca-granulosa cell tumors, primitive gonadal stromal tumors, and
admixtures of these cell types constitute about
3% of testicular tumors. These tumors are
occasionally associated with gynecomastia, but
most of the reported cases do not show this
feature. The well-differentiated Sertoli cell
tumor is rather common among dogs and
occasionally gives rise to feminizing features.
1. Gross features
The left testis is more frequently involved.
The tumors may vary from 1-17 cm in diameter. They are usually firm, lobulated, well
circumscribed, and yellowish or grayish-white.
2. Histologic features
There is much confusion in the interpretation of the histologic characteristics of
these tumors. Pure Sertoli cell tumors are
readily recognizable, since the cells are
hexagonal or tall and columnar and have
a large spherical or oval nucleus with a
distinct nuclear membrane surrounding a fine
chromatin network and a small solitary basophilic nucleus. The cytoplasm is usually abundant and has large clear vacuoles, often containing fat, but may be scanty and either
eosinophilic or basophilic. Mitotic figures and
giant cells are rare. I n most instances the cells
are arranged in tubular forms that resemble
seminiferous tubules. In other areas the cells
are smaller, more cuboidal, and arranged in
sheets, cords, and follicles reminiscent of granulosa cells (Fig. lo), and in some cases there
are structures resembling Call-Exner bodies.
At times the epithelial cells may have an
abundant ground-glass eosinophilic cytoplasm
and resemble Leydig cells, but they are entirely intratubular. Another cell type is spin-
No. 5
TESTICULAR
TUMORS Mostofi
1199
FIG. 10. Gonadal
stromal tumor. Stertoli-granulosa-likecells
are seen occurring as
solid sheets and as individual cells (AFIP
Neg. 73-57444; x 210).
dle-shaped and has an elongated nucleus and
eosinophilic and sometimes vacuolated cytoplasm. The spindle cells are plumper than the
usual fibroblasts. Pure spindle cell theca-like
tumors are rare, but almost half the tumors
show distinct, often interlacing, spindleshaped cell areas. Areas of hyalinization are
frequent, and a few of the tumors show calcification.
About 10% of the tumors become malignant, but the majority of the patients have
not been adequately followed for 5 or more
years. To date the criteria for malignancy
have not been clearly defined, but in our experience increased mitosis, polymorphism, cellular anaplasia, extension to the capsule or adnexae, and vascular invasion are indicative of
malignancy; the actual demonstration of metastasis, however, remains the indisputable
evidence of malignancy. Almost all metastasis
has occurred within the first 5 months.
111. Metastatic Tumors Initially Manifested
as Testicular Neoplasms
The most common of the metastatic tumors,
initially manifested as testicular neoplasms, is
malignant lymphoma. It constitutes about 1%
of testicular tumors.16 I n contrast to germinal
tumors, which rarely involve the Negro population, malignant lymphoma occurs in both
races. It may occur in any age group, ranging
from 21/*-87 years, but many of the patients
are in the sixth and seventh decades. Enlargement of the testis, with or without pain, is the
chief symptom. In about 25% of the cases
weight loss, anorexia, and weakness are present.
A . Gross Features
The testis is invariably enlarged, and the
enlargement is usually diffuse. The cut surfaces show a bulging, firm, grayish-white,
usually solid tumor with a granular surface and areas of hemorrhage and necrosis.
The tumor is nonencapsulated.
B . Histologic Features
The characteristic feature is extreme cellularity of the tumor (Fig. 11). More than
half of the tumors consist of pure reticulum
cell sarcoma, in about one-third the cells
are obviously lymphocytic, and the remainder
are either lymphoblastic or of mixed type,
with reticulum cells, lymphoblasts, and
lymphocytes. We have seen no instances
of Hodgkins disease occurring primarily
in the testis. Many malignant lymphomas
of the testis are misdiagnosed either as seminoma or embryonal carcinoma. Seminoma
cells are larger and have much more clear or
granular cytoplasm; the nuclei are larger and
more vesicular and have one or more nucleoli.
1200
CANCER
November 1973
Vol. 32
FIG. 11. Malignant
lymphoma,
initially
manifested as testicular tumor. The tumor
is extremely cellular
and infiltrates the interstitium. The cellular population is polymorphous. ranging
from small lymphocytes to reticulum
cells. Note that, in
contrast to Figs. 1-5,
the cells here have
little cytoplasm (AFIP
Neg. 73-5741; x 240).
The cells have a distinct cell border and form
a mosaic pattern. Embryonal carcinoma has a
distinct epithelial appearance and frequently
forms glandular, papillary, or tubular structures. In lymphoma the cells are usually small,
and the nuclei are large and indented. The
scant cytoplasm may form a halo around the
nucleus.
About 20% of patients develop tumor in
the opposite testis. In our experience 90% of
the patients are dead with generalized lymphoma within 2 years.
IV. Adnexal Tumors
Most malignant adnexal tumors are sarcomas. The incidence of these tumors shows
three age peaks: in children, adolescents, and
the older adult age group. The most common
of sarcomas are rhabdomyosarcomas occcuring
in children and young adults-from
5
months-28 years of age.
A. Gross Features
They present as a large intrascrotal mass
ranging up to 20 cm in diameter; They are
circumscribed but not encapsulated, and the
cut surface is grayish white to tan.
B . Histologic Features
Rhabdomyosarcomas present a ,wide range
of histologic patterns, from undifferentiated
cells to myxomatous, spindle cell, and differentiated rhabdomyoblastic tissue. Other
sarcomas-e.g., liposarcomas, leiomyosarcomas, malignant fibrous histiocytomas, mesotheliomas, and mixed mesenchymal tumorsare most often seen in older patients.
Almost all these tumors are primary in testicular adnexae-the tunica and the cordand not in the testes proper.
REFERENCES
1. Axtell, L. M., Cutler, S. J., and Myers, M. H.:
End results in cancer-Report No. 4. Bethesda, Maryland, U. S. Department of Health, Education, and
Welfare, 1972.
2. Auopardi, J. G., Mostofi, F. K.,and Theiss. E. A.:
Lesions of testes observed in certain patients with widesDread choriocarcinoma and related tumors-The sieiificance and genesis of hematoxylin-staining bodies rn
the human testis. A m . J . Pathol. 38:207-225, 1961.
3. Clarke, B. G.: The relative frequency and age incidence of principal urological diseases. J . Urol. 98:
701-705, 1967.
4. Clemmesen, J.: A doubling of morbidity from testis carcinoma in Copenhagen, 1943-1962. ~~t~ Pathof.
&ficrobiol. Stand. 72:34&349, 1968.
5. Dixon, F. J., and Moore, R. A.: Tumors of the
Male Sex Organs. Atlas of Tumor Pathology, fascicles
No. 5
TESTICULAR
TUMORS Mostofi
31b and 32. Washington, D. C., Armed Forces Institute of Pathology, 1952.
6. Dvizhkov, P. P., and Potapova, L. N.: On the carcinogenic properties of metallic zinc and zinc chlorides.
Gig. T r . Prof. Zabol. 12:23-27, 1968.
7. Falin, L. I.: Experimental teratomas testis in the
fowl. A m . J . Cancer 38:199-211, 1940.
8. Ferguson, J. D.: Tumours of the testis. Br. J . Urol.
34:407-421, 1962.
9. Friedman, N. B., and Moore, R. A.: Tumors of
the testis; a report on 922 cases. M i l i t . Surg. W573593, 1946.
10. Gilbert, J. B., asd Hamilton, J. B.: Studies in
malignant testis tumors-incidence and nature of tumors in ectopic testes. Surg. Gynecol. Obstet.
71~731-743, 1940.
11. Grumet, R. F., and MacMahon, B.: Trends in
mortality from neoplasms of the testis. Cancer
11:790-797, 1958.
12. Howden, P. F.: Carcinoma of the testicle. N . 2.
Med. J . 67:215-217, 1968.
13. MacKay, E. N., and Sellers, A. H.: A statistical
review of malignant testicular tumors based on the experience of the Ontario Cancer Foundation Clinics,
1938-1961. Can. Med. Assoc. J . 94889-899, 1966.
1201
14. Maier, J. G., Sulak, M. H., and Mittemeyer, B.
T.: Seminoma of the testis-Analysis of treatment success and failure. A m . J . Roentgenol. Radium Ther.
Nucl. Med. 102:596-602, 1968.
15. Masson, P.: Etude sur le seminome. Rev. Can.
Biol. 5:361-387, 1946.
16. Mostofi, F. K., and Price, E. B., Jr.: Tumors of
the Male Genital System. Atlas of Tumor Pathology,
fascicle 7, series 2. Washington, D. C., Armed Forces
Institute of Pathology, 1973 (In press).
17. Most&, F. K., Theiss, E. A., and Ashley, D. J.
B.: Tumors of specialized gonadal stroma in human
male patient-Androblastoma,
Sertoli cell tumor,
granulosa-theca cell tumor of the testis, and gonadal
stromal tumor. Cancer 12:944-957, 1959.
18. Muller, K.: Cancer Testis. Thesis. Copenhagen,
Munksgaard, 1962.
19. Sauer, H . R., Watson, E. M., and Burke, E. M.:
Tumors of the testicle. Surg. Gynecol. Obstet. 86:
591-603, 1948.
20. Stevens, L. C., Jr.: Embryology of testicular teratomas in strain 129 mice. J . Natl. Cancer Inst.
23~1249-1295, 1959.
21. Stevens, L. C., Jr., and Little, C. C.: Spontaneous
testicular teratomas in an inbred strain of mice. Proc.
Natl. Acad. Sci. 401080-1087, 1954.
S-ar putea să vă placă și
- Neoplasms of TestisDocument26 paginiNeoplasms of TestisFeddyFebriyantoManurungÎncă nu există evaluări
- Epidemiology of Ovarian Cancer: A ReviewDocument24 paginiEpidemiology of Ovarian Cancer: A ReviewWiedya kristiantiÎncă nu există evaluări
- Pathology of Germ Cell Tumors of The TestisDocument14 paginiPathology of Germ Cell Tumors of The TestisAnonymous be1sWu6l6Încă nu există evaluări
- Pathogenesis of Testicular Germ Cell Tumours: Leendert H. J. Looijenga and J. Wolter OosterhuisDocument11 paginiPathogenesis of Testicular Germ Cell Tumours: Leendert H. J. Looijenga and J. Wolter OosterhuisLatansa DinaÎncă nu există evaluări
- 6 Tumors IntroductionDocument101 pagini6 Tumors IntroductionReZky MusliminÎncă nu există evaluări
- Clear Cell CADocument2 paginiClear Cell CAOscar HalumÎncă nu există evaluări
- Oncology Toribio Augene SecFDocument9 paginiOncology Toribio Augene SecFAugene ToribioÎncă nu există evaluări
- Testicular CancerDocument11 paginiTesticular CancercilengsaiÎncă nu există evaluări
- Neoplasia ExamDocument9 paginiNeoplasia ExamYheng Gaosaii100% (1)
- Semi No MaDocument2 paginiSemi No MaDea Prista AgathaÎncă nu există evaluări
- MR 28 Agustus-1Document7 paginiMR 28 Agustus-1BramaÎncă nu există evaluări
- Finger Clubbing and A Lung MassDocument5 paginiFinger Clubbing and A Lung MassSeptinaAyuSamsiatiÎncă nu există evaluări
- TESTICULAR CANCER BookletDocument33 paginiTESTICULAR CANCER BookletCheeBrendaÎncă nu există evaluări
- POGS Practice Bulletin 3 FINALDocument6 paginiPOGS Practice Bulletin 3 FINALAileen TombocÎncă nu există evaluări
- G Path-NeoplasiaDocument60 paginiG Path-Neoplasiachouchou124Încă nu există evaluări
- RPB14150079015Document5 paginiRPB14150079015Ijupbs IjupbsÎncă nu există evaluări
- Jurnal Kanker TestisDocument9 paginiJurnal Kanker TestisDiatni FibriÎncă nu există evaluări
- Testis CancerDocument9 paginiTestis CancerMuhammad Tawfiq ZamriÎncă nu există evaluări
- 624 PDFDocument9 pagini624 PDFTri AryantiÎncă nu există evaluări
- Subject Date Professor Sbobinatore: (Armando Muro) ReviewerDocument10 paginiSubject Date Professor Sbobinatore: (Armando Muro) ReviewerÁngel Parra CominoÎncă nu există evaluări
- Kurman 2013Document6 paginiKurman 2013adevanshi3399Încă nu există evaluări
- Medsci 06 00031 PDFDocument113 paginiMedsci 06 00031 PDFCarolina VillalobosÎncă nu există evaluări
- Asal CA OvarianDocument3 paginiAsal CA OvarianBenyamin Rakhmatsyah TitaleyÎncă nu există evaluări
- Smith 2017Document14 paginiSmith 2017Evelynππ θσυÎncă nu există evaluări
- Testicular CancerDocument12 paginiTesticular Cancerghost_724Încă nu există evaluări
- Lesions Infertile: Precancerous of The Cervix Uteri in WomenDocument2 paginiLesions Infertile: Precancerous of The Cervix Uteri in WomenGede S PutrawanÎncă nu există evaluări
- The Unitarian or Trophoblastic Thesis of CancerDocument32 paginiThe Unitarian or Trophoblastic Thesis of Canceruge9Încă nu există evaluări
- Biochemistry of CrytorchidismDocument21 paginiBiochemistry of CrytorchidismGabrielÎncă nu există evaluări
- ReviewDocument5 paginiReviewerickmattosÎncă nu există evaluări
- Papillary Thyroid CarcinomaDocument9 paginiPapillary Thyroid CarcinomaELinkTulusÎncă nu există evaluări
- Praktikum Reproduksi 2Document46 paginiPraktikum Reproduksi 2Andika Tatag100% (1)
- Navigation Search Cancer (Disambiguation) : (Intrusion On and Destruction of Adjacent Tissues), and SometimesDocument23 paginiNavigation Search Cancer (Disambiguation) : (Intrusion On and Destruction of Adjacent Tissues), and Sometimesmariannec_3Încă nu există evaluări
- CancerDocument14 paginiCancerNano AlmukasabyÎncă nu există evaluări
- Dunn RefDocument47 paginiDunn RefFlorencia Chandrika HalimÎncă nu există evaluări
- Giant Uterine Leiomyoma - Case Report and Review of LiteratureDocument3 paginiGiant Uterine Leiomyoma - Case Report and Review of LiteratureMan ManuelÎncă nu există evaluări
- Testis and EpididymisDocument15 paginiTestis and EpididymisJake MillerÎncă nu există evaluări
- Tumori Testisa PDFDocument14 paginiTumori Testisa PDFVuk MilutinovićÎncă nu există evaluări
- Neoplasma TestisDocument3 paginiNeoplasma TestisFalira MuthiaÎncă nu există evaluări
- CarcinogenicityDocument66 paginiCarcinogenicityNormana ZureikatÎncă nu există evaluări
- Testicular Cancer (Teratoma Testis)Document7 paginiTesticular Cancer (Teratoma Testis)Witha Lestari AdethiaÎncă nu există evaluări
- Presença de Beta III Nas Células de Kulchitsky Sugere Sua Origem Subventricular Do SNCDocument3 paginiPresença de Beta III Nas Células de Kulchitsky Sugere Sua Origem Subventricular Do SNCFedericoDiGiovanniÎncă nu există evaluări
- Adenocarcinoma Borderline OvarioDocument18 paginiAdenocarcinoma Borderline OvarioIsaac MaderoÎncă nu există evaluări
- Metastases To The Thyroid: A Review of The Literature From The Last Decade Chung2012-2Document11 paginiMetastases To The Thyroid: A Review of The Literature From The Last Decade Chung2012-2Pavel GonzálezÎncă nu există evaluări
- Sacrococcygeal Teratoma A Tumor at The Center of EmbryogenesisDocument8 paginiSacrococcygeal Teratoma A Tumor at The Center of EmbryogenesisLuis Ruelas SanchezÎncă nu există evaluări
- Original Research ReportDocument4 paginiOriginal Research ReportSehrish SiddiqueÎncă nu există evaluări
- Neonatal Extra-Renal Wilm's Tumour: Division of Paediatric Surgery, Aga Khan University Hospital, KarachiDocument2 paginiNeonatal Extra-Renal Wilm's Tumour: Division of Paediatric Surgery, Aga Khan University Hospital, Karachidydy_7193Încă nu există evaluări
- Cancers Make Their Own Luck - Theories of Cancer OriginsDocument15 paginiCancers Make Their Own Luck - Theories of Cancer Originszhe zhÎncă nu există evaluări
- Papillary Thyroid CarcinomaDocument17 paginiPapillary Thyroid CarcinomaEster Sibarani100% (2)
- Theories of Endometrial CarcinogenesisDocument14 paginiTheories of Endometrial CarcinogenesisRisti SFÎncă nu există evaluări
- Colon Cancer: Risk Factors and Therapeutic ApproachesDocument11 paginiColon Cancer: Risk Factors and Therapeutic ApproachesCentral Asian StudiesÎncă nu există evaluări
- Near-Infrared Raman Spectroscopy For TheDocument12 paginiNear-Infrared Raman Spectroscopy For TheAlberto Carlos Espinosa GaravitoÎncă nu există evaluări
- NATIONAL CANCER CONTROL PROGRAMM 2 (Prakash)Document19 paginiNATIONAL CANCER CONTROL PROGRAMM 2 (Prakash)angayarkanni100% (1)
- Incidence A N D Case-Control Study: Ovarian CancerDocument7 paginiIncidence A N D Case-Control Study: Ovarian CancerHannah SteinmetzÎncă nu există evaluări
- PG Art 34580-10Document15 paginiPG Art 34580-10Horia MineaÎncă nu există evaluări
- Micrornas and Recent Insights Into Pediatric Ovarian CancersDocument10 paginiMicrornas and Recent Insights Into Pediatric Ovarian CancersingeÎncă nu există evaluări
- Benign Cystic TeratomaDocument3 paginiBenign Cystic TeratomaLisa Dwipurnamasari TobingÎncă nu există evaluări
- Managing The Risk of Cancer in Cowden Syndrome: A Case ReportDocument4 paginiManaging The Risk of Cancer in Cowden Syndrome: A Case ReportKaisun TeoÎncă nu există evaluări
- Biology ProjectDocument6 paginiBiology ProjectBemnet TayeÎncă nu există evaluări
- Animal CellDocument7 paginiAnimal CellLezircYojDapmalÎncă nu există evaluări
- Lecture 1Document39 paginiLecture 1Mohammed SindiÎncă nu există evaluări
- Exercise Cell As The Basic Unit of Living ThingsDocument16 paginiExercise Cell As The Basic Unit of Living ThingsHidayatul ZawawiÎncă nu există evaluări
- Bolo - Dakabadonebuli - Book 2Document152 paginiBolo - Dakabadonebuli - Book 2sasa sasadzeÎncă nu există evaluări
- SHS STEM Bio1 Q1 Week 1 Module 2 Cell Structure and Functions 1Document17 paginiSHS STEM Bio1 Q1 Week 1 Module 2 Cell Structure and Functions 1Dette Dominic Ballano67% (3)
- Horizontal Gene Transfer in Eukaryotic Evolution - Nature Reviews Genetics - 2008Document14 paginiHorizontal Gene Transfer in Eukaryotic Evolution - Nature Reviews Genetics - 2008carlos murciaÎncă nu există evaluări
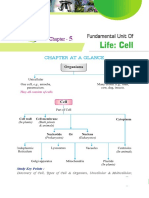
- Chapter at A Glance: Study Key PointsDocument14 paginiChapter at A Glance: Study Key PointssatishÎncă nu există evaluări
- Cells R UsDocument2 paginiCells R Usapi-264011999Încă nu există evaluări
- The Cell Structure and TaxonomyDocument10 paginiThe Cell Structure and TaxonomyKingJayson Pacman06Încă nu există evaluări
- Flashcards - Topic 17 Inheritance - CAIE Biology IGCSEDocument75 paginiFlashcards - Topic 17 Inheritance - CAIE Biology IGCSESabbath the sign of GodÎncă nu există evaluări
- DNA Programming Kit Manual PDFDocument65 paginiDNA Programming Kit Manual PDFavrajamohamedÎncă nu există evaluări
- Biomolecules and Cells NotesDocument81 paginiBiomolecules and Cells NotesLily RobinsonÎncă nu există evaluări
- Expert MdcatDocument4 paginiExpert Mdcathely shahÎncă nu există evaluări
- Science Biology 11-12 Q1Document9 paginiScience Biology 11-12 Q1Zhering RodulfoÎncă nu există evaluări
- Review of Medical Microbiology and Immunology 17th Edition (Medicalstudyzone - Com)Document1.016 paginiReview of Medical Microbiology and Immunology 17th Edition (Medicalstudyzone - Com)FaizÎncă nu există evaluări
- Cell Biology: InstructorDocument20 paginiCell Biology: Instructorahmed mediaÎncă nu există evaluări
- Samuelson - Textbook of Veterinary HistologyDocument710 paginiSamuelson - Textbook of Veterinary HistologyValentina Aguirre LópezÎncă nu există evaluări
- Lab 2 - InstructionsDocument16 paginiLab 2 - InstructionsCazzel AvilesÎncă nu există evaluări
- FET CP 1 Cell Structure & FunctionsDocument220 paginiFET CP 1 Cell Structure & FunctionsFarhat GirangÎncă nu există evaluări
- AS Level Biology Notes 2015 PDFDocument298 paginiAS Level Biology Notes 2015 PDFali hyd100% (1)
- G. Biology PPT Chapter 1-6new1Document238 paginiG. Biology PPT Chapter 1-6new1Alemayehu MelkamuuÎncă nu există evaluări
- Eukaryotic Chromosome Structure PDFDocument2 paginiEukaryotic Chromosome Structure PDFRachelÎncă nu există evaluări
- Choose The Correct AnswerDocument8 paginiChoose The Correct AnswerBLlahniesss Love KenÎncă nu există evaluări
- Neet Question Paper 2021 Code O1Document71 paginiNeet Question Paper 2021 Code O1Deev SoniÎncă nu există evaluări
- Gallery WalkDocument12 paginiGallery WalkPaul Hudson MackÎncă nu există evaluări
- 1.2 Ultrastructure of Cells: ProkaryotesDocument8 pagini1.2 Ultrastructure of Cells: Prokaryotesdavid tsaiÎncă nu există evaluări
- Actividad MitosisDocument6 paginiActividad MitosisVanesaÎncă nu există evaluări
- XXXXXXXXDocument17 paginiXXXXXXXXRicardo LazoÎncă nu există evaluări
- Topic 3 - Cellular Level of OrganizationDocument6 paginiTopic 3 - Cellular Level of OrganizationAdeyinka OluyoleÎncă nu există evaluări
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Evaluare: 3 din 5 stele3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (81)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 4 din 5 stele4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (5)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (45)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (170)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedEvaluare: 4 din 5 stele4/5 (61)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDe la EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesEvaluare: 4.5 din 5 stele4.5/5 (1412)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingDe la EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingEvaluare: 1 din 5 stele1/5 (1)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (59)